- 1Center for Health Promotion and Prevention Research, University of Texas Health Science Center Houston, Houston, TX, United States
- 2Northwest Portland Area Indian Health Board, Portland, OR, United States
- 3Alaska Native Tribal Health Consortium, Anchorage, AK, United States
- 4Inter Tribal Council of Arizona, Inc., Phoenix, AZ, United States
- 5Center for Health Promotion and Prevention Research, University of Texas Health Science Center Houston, San Antonio, TX, United States
- 6College of Medicine, Florida International University, Miami, FL, United States
Background: American Indian and Alaska Native (AI/AN) youth experience serious disparities in sexual and reproductive health, including the highest teen birth rate among racial/ethnic groups, and disproportionate rates of sexually transmitted infections (STI), including HIV. A growing number of evidence-based programs (EBPs) that integrate the strengths and cultural teachings of Native communities exist. Yet, multiple factors, including lack of trained personnel, limited resources, and geographic isolation, may hinder their adoption and implementation. Innovative implementation strategies that facilitate the adoption and implementation of sexual health EBPs in Native communities may help reduce these disparities.
Methods: We applied Implementation Mapping, a systematic planning framework that utilizes theory, empirical evidence, and community input, to adapt a theory-based, online decision support system, iCHAMPSS (CHoosing And Maintaining Effective Programs for Sex Education in Schools), to support underlying dissemination and implementation processes unique to Native communities. We used an iterative design process, incorporating input from Native practitioners and academicians, to ensure that the adapted decision support system reflects cultural identification, community values, and experiences.
Results: Grounded in diffusion of innovations, organizational stage theory, and social cognitive theory, the Healthy Native Youth Implementation Toolbox supports Native practitioners through five phases (Gather, Choose, Prepare, Implement, and Grow) to adopt, implement, and maintain a culturally-relevant, age-appropriate sexual health EBP. The Toolbox provides tools, ready-to-use templates, and guidance to plan, implement, and grow a culturally-relevant adolescent health program with their Tribe or community. Hosted within the Healthy Native Youth website (www.healthynativeyouth.org), the Toolbox comprises: (1) a curriculum portal with access to 15 culturally-relevant, age-appropriate evidence-based health promotion programs for AI/AN youth; (2) a “resource library” comprising 20+ support tools, templates, and links to external resources, and (3) “stories from the field” comprising testimonials from experienced Native educators, who have implemented sexual health programs.
Conclusion: There is a continued need to design, test, and evaluate D&I strategies that are relevant to Native communities. The Healthy Native Youth Implementation Toolbox contributes to the dissemination and implementation of evidence-based, culturally-relevant sexual health education programs in diverse Native communities. Implementation Mapping provided a systematic approach to guide the adaptation process and integrate community voice with the ultimate goal of enhancing sexual health equity among AI/AN youth.
Introduction
The federal government recognizes 574 distinct American Indian/Alaska Native (AI/AN) tribes that represent 2% of the United States (U.S.) population (1). Overall, the AI/AN population is young, with 30% under 18 years-old compared to 24% of the U.S. total population (2). As a result, the need for adolescent health promotion resources is particularly relevant in Native communities.
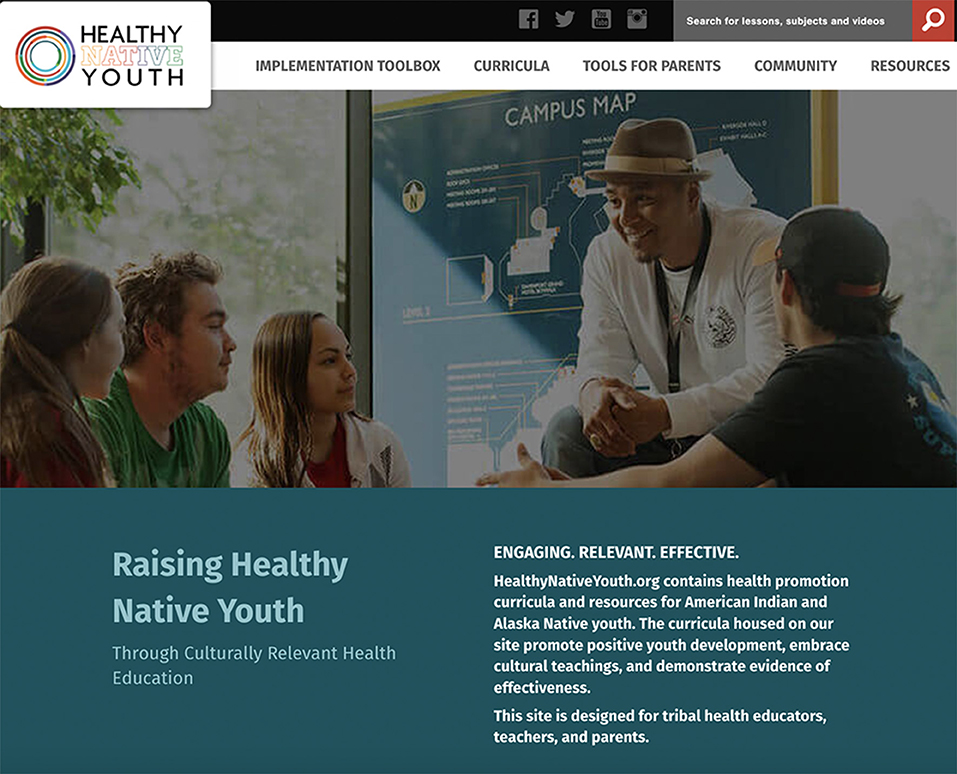
Despite recent declines in teen birth rates in the U.S., racial and ethnic disparities persist (3). AI/AN females ages 15–19 years have the highest teen birth rate among racial/ethnic groups (3) and the highest repeat teen birth rate (4). AI/AN youth are also disproportionately affected by sexually transmitted infections (STI), including HIV (5, 6). These health disparities may be ameliorated by the implementation of effective, culturally-relevant sexual health education programs (7). A growing number of evidence-based programs (EBPs) (8) that integrate the strengths and cultural teachings of Native communities have been developed or adapted for AI/AN youth (9–14). In 2016, our research team, in collaboration with AI/AN advisors, developed the Healthy Native Youth website (www.healthynativeyouth.org) to increase access to these culturally-relevant EBPs (15). The portal allows users to filter and compare curricula on multiple dimensions to determine best-fit and includes implementation materials free-of-charge. Yet, solely increasing access to culturally-relevant EBPs may be insufficient to increase their use (7). Multiple barriers exist and AI/AN health educators often lack the resources to navigate the adoption and implementation process. Adolescent sexual health is a sensitive topic, and many Native communities lack the community readiness and resources to broach the issue. Varying Tribal review and school board approval processes may create delays in program adoption and implementation (16). Pervasive poverty often results in personnel turnover or temporary closures for AI/AN youth-serving agencies, which may compromise implementation fidelity and program sustainability (7). Geographic challenges, including remote villages and reservations, may impact program implementation and access to resources (1, 7). Finally, as in other locations, AI/AN communities may face competing priorities, perceived lack of administrative or parental support, and lack of specialized training in sexual health, including limited knowledge of where to find culturally-relevant EBPs or limited self-efficacy to implement them (17, 18). Innovative strategies that facilitate the adoption and implementation of sexual health EBPs in Native communities are needed to reduce these health disparities.
iCHAMPSS (CHoosing And Maintaining Effective Programs for Sex Education in Schools) is a theory-based online decision support system designed to address barriers to the dissemination and implementation (D&I) of sexual health EBPs in Texas schools (17, 19). Decision support systems are computer-based systems designed to facilitate a wide variety of decision tasks, including information gathering and analysis, alternative evaluation, and decision implementation (20). Grounded in D&I theories (21–23), iCHAMPSS comprises 60+ tools to provide step-by-step guidance to overcome D&I barriers for sexual education (www.ichampss.org). Demonstrated to impact critical determinants for adopting and implementing a sexual health EBP in Texas schools (24), iCHAMPSS serves as a promising implementation strategy to adapt for AI/AN communities.
To explore the potential of adapting iCHAMPSS, we conducted usability testing with AI/AN practitioners (n = 36) across the U.S. Overall, participants rated iCHAMPSS as acceptable, easy to use, credible, appealing, more helpful than current resources, and impactful of EBP adoption, implementation, and sustainability (25). However, using iCHAMPSS also significantly increased participants' perceived barriers to adopting an EBP. Some participants found the amount of information overwhelming and certain steps and tools, such as presenting a School Health Advisory Council (SHAC) recommendation letter to the School Board, were unfamiliar for Native communities. Sexual health education occurs in diverse settings in AI/AN communities, including schools, after-school programs, clinics, and community centers. Thus, the steps involved in the adoption and implementation of sexual health EBPs in Texas schools may not adequately reflect the steps involved in Native communities. Qualitative feedback from the usability testing provided tangible adaptation recommendations such as inclusion of culturally-relevant EBPs, provision of culturally appropriate assessment tools, integration of Tribal review and approval processes, and resources to adapt EBPs (25). Previous studies in AI/AN communities also suggest that embedding implementation within a consortium or learning community may enhance sustainability (26). Overall, findings indicated the potential for an adapted iCHAMPSS to address D&I barriers for sexual health EBPs in AI/AN communities.
In this “Methods” paper we describe how we applied Implementation Mapping to adapt iCHAMPSS to facilitate the adoption and implementation of sexual health EBPs in AI/AN communities. Implementation Mapping is a systematic approach for developing or adapting strategies to increase the adoption, implementation, and maintenance of evidence-based interventions, practices, or policies (27). It provides a step-by-step process, based in theory, empirical evidence, and community input, to identify the relevant determinants, mechanisms, and strategies for effecting change. The resulting Healthy Native Youth Implementation Toolbox (www.healthynativeyouth.org/implementation-toolbox/) is an online implementation strategy to increase the adoption and implementation of culturally-relevant, age-appropriate sexual health EBPs in Native communities with the ultimate goal of improving sexual health equity among AI/AN youth.
Methods
iCHAMPSS decision support system
iCHAMPSS is a web-based, interactive, self-paced decision support system that guides individuals through the process of adopting, implementing, and maintaining sexual health EBPs in Texas schools (Figure 1). iCHAMPSS comprises: (1) a “staging tool” to provide tailored guidance based on a community's level of readiness to implement a sexual health EBP, and (2) a “resource tools library” comprising 60+ support tools to enable successful completion of tasks within each implementation step. Tools include: step overviews, success stories (video testimonials from individuals who have adopted, implemented, or maintained a sexual health education EBP), facts and tips (e.g., a selection guide to identify EBPs), helpful links to online resources outside of iCHAMPSS, and templates that can be tailored to fit a school's or community's needs (19).

Figure 1. The iCHoosing And Maintaining Effective Programs for Sex Education in Schools (iCHAMPSS) online decision support system.
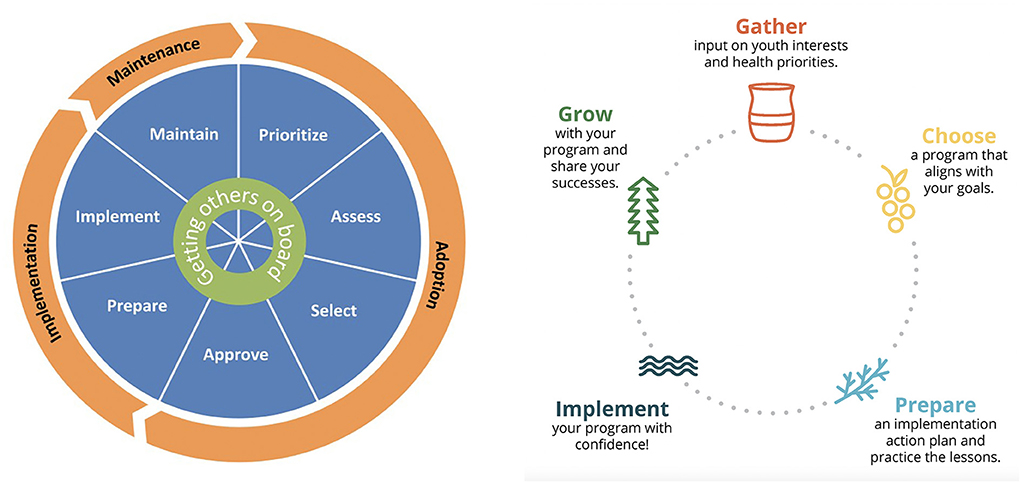
iCHAMPSS was developed using the original Intervention Mapping process (28). Guided by Diffusion of Innovation (21), Organizational Stage Theory (22), and Social Cognitive Theory (23), literature review findings on individual- and organizational-level factors that influence the adoption and implementation of sexual health EBPs in schools, and in-depth interviews with school district personnel, the research team developed adoption, implementation, and maintenance outcomes and performance objectives to delineate the specific actions needed to support sexual health EBPs in Texas schools. The resulting conceptual model, CHAMPSS (CHoosing And Maintaining Effective Programs for Sex Education in Schools), provides the theoretical foundation for the web-based iCHAMPSS, and includes three phases: “adoption,” “implementation,” and “maintenance,” which are further divided into seven steps: (1) prioritize, (2) assess, (3) select, (4) approve, (5) prepare, (6) implement, and (7) maintain EBPs. A core element, “Generate support” (i.e., connecting with other supporters of EBPs and adolescent sexual health), extends across all seven steps. Each step comprises two to six sub-steps or critical tasks to move program planners through the process (Figure 2) (17). The model is circular (Figure 3), reflecting that planners may enter the model at any step, depending on their level of readiness. They may also complete one step but then realize they need to revisit a previous step.
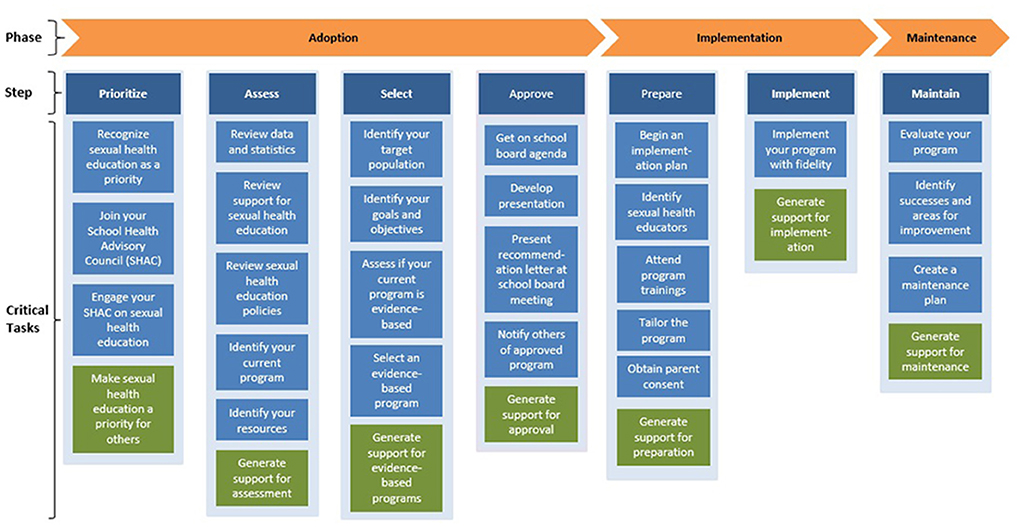
Figure 2. Phases, steps, and critical tasks in the CHAMPSS model (19).
iCHAMPSS incorporates theory-based methods and implementation strategies as step-specific tools to influence the determinants of adoption and implementation. For example, our success story video testimonials use modeling to influence planners' knowledge, skills, and self-efficacy to adopt, implement, or maintain a sexual health EBP. A detailed description of the development process is described elsewhere (17, 19).
The CHAMPSS model extends previous dissemination pragmatic models and frameworks (29–34) by providing greater focus on individual- and organizational-level determinants for the adoption, implementation, and maintenance of sexual health EBPs, and greater detail by operationalizing the steps needed to adopt, implement, and maintain sexual health EBPs in schools. The result is a pragmatic model with greater utility for practitioners, which is a recognized “model practice” by the National Association of County and City Health Officials (35).
Participatory planning approach
Community-based Participatory Research Planning (CBPR) is an important component of Implementation Mapping. CBPR principles involve engaging with community partners to better understand the complex intervention context and to facilitate integration of real-world and academic knowledge to increase the potential effectiveness of interventions and implementation strategies (27, 36). Participatory planning is especially important in partnering with AI/AN communities to ensure the integration of Native-informed practice models and conceptual frameworks (37–39). The core planning group for the adaptation process comprised adolescent health educators and researchers at the Northwest Portland Area Indian Health Board (NPAIHB), the Alaska Native Tribal Health Consortium (ANTHC), the Inter Tribal Council of Arizona, Inc. (ITCA), and the University of Texas Health Science Center (UTHealth); hereafter, referred to as “we”. This group has collaborated for over a decade to adapt and develop online interventions and resources to promote adolescent sexual health in Native communities (11, 40, 41), including the Healthy Native Youth website (www.healthynativeyouth.org), which provides a “one-stop-shop” for Tribal youth advocates to access culturally-relevant curricula and resources (15). The Healthy Native Youth team also hosts monthly Community of Practice virtual gatherings to share resources with Native practitioners.
We used an iterative design process incorporating input from Native practitioners and academicians, to ensure that the adapted decision support system reflects cultural identification, community values, and experiences. During the planning phase (Implementation Mapping Tasks 1 and 2), we convened an Expert Advisory Group to provide high-level guidance on adaptation of the conceptual model and parameters for use for the adapted system. The group comprised researchers in Native adolescent health and representatives from Tribal Epidemiology Centers, the National Indian Health Board, the State of Alaska Adolescent Health Program, and other Native community-based organizations. During the design phase (Implementation Mapping Tasks 3 and 4), we conducted formative feedback sessions with our Healthy Native Youth AI/AN Adolescent Sexual Health Workgroup to obtain input on the adapted model, proposed tools, and website design mock-ups. The workgroup comprises Tribal health educators, advocates, teachers, counselors, academics, and representatives from additional national organizations including the United National Indian Tribal Youth, Inc. (UNITY), Big Brothers, Big Sisters, and Boys & Girls Club of America Native Services. As we began feasibility testing (Implementation Mapping Task 5), we solicited feedback on features and tools from each Toolbox phase during consecutive Healthy Native Youth Community of Practice sessions. Participants included Tribal health educators, teachers, parents, and prevention specialists. Overall, these groups met virtually online using Zoom software eight times between November 2020 and June 2022. We used interactive activities (e.g., Jamboard), chat feed discussions, and polling to obtain feedback on the adapted model, tools, and the website's features, tone, and feel.
Implementation Mapping
Informed by the Intervention Mapping process and implementation science, Implementation Mapping provides step-by-step guidance for selecting, designing, or adapting implementation strategies to guide implementation efforts (27, 28). Implementation Mapping has been applied to improve the adoption, implementation, and sustainability of evidence-based programs, practices, and policies in real-world settings, including clinics, schools, and community-based service agencies (27, 42, 43). Implementation Mapping involves five specific tasks: (1) conduct a needs assessment and identify program adopters and implementers; (2) state adoption and implementation outcomes and performance objectives, identify determinants, and create matrices of change objectives; (3) choose theoretical methods and select or design implementation strategies; (4) produce implementation protocols and materials; and (5) evaluate implementation outcomes. These five tasks are iterative with the planning group circling back to previous tasks throughout to ensure all adopters and implementers, outcomes, determinants, and objectives are addressed (27). In this project, we applied Implementation Mapping (IM) to adapt iCHAMPSS to facilitate the adoption and implementation of culturally-relevant sexual health EBPs in AI/AN communities.
Results
IM Task 1. Conduct an implementation needs assessment
In IM Task 1, planners conduct a needs and assets assessment to identify barriers and facilitators of implementation. It is important to involve all agents including adopters, implementers, and those responsible for maintaining the evidence-based interventions to identify actions needed to implement the program and determinants (barriers and facilitators) of implementation (27).
To inform the adaptation process, we conducted a needs and asset assessment to identify barriers and facilitators for the adoption, implementation, and maintenance of sexual health EBPs in AI/AN communities. Given limited D&I research within Native communities, we conducted: (1) a broad scoping review to identify common barriers and effective implementation strategies to disseminate and implement health promotion EBPs in AI/AN, Native Hawaiian/Pacific Islander (NH/PI), and Canadian Indigenous communities, and (2) key informant interviews with experienced sexual health educators to identify factors specific to the D&I of sexual health EBPs in AI/AN communities.
Scoping review
Partnering with a research librarian, we identified research questions (What are the main barriers encountered in the D&I of EBPs in Indigenous communities? What implementation strategies have been used in Indigenous communities for EBP adoption, implementation and/or maintenance?), relevant electronic publication databases of PubMed, EMBASE, and Medline, formulated database search strategies, and developed a data abstraction form. To encompass a broad range of studies, EBPs were defined as any evidence-based or evidence-informed intervention or program disseminated or implemented in AI/AN, NH/PI, and/or Canadian Indigenous communities to improve health or behavioral outcomes for any age range. “Dissemination” and “Implementation” were defined in accordance with the 2016 National Institute of Health definitions (44). Barriers were classified into nine barrier categories within a broader socio-ecological framework (45). For comparability with D&I research in non-Indigenous communities, we categorized and coded implementation strategies according to the SISTER (School Implementation Strategies, Translating ERIC Resources) taxonomy of implementation strategies developed to facilitate the adoption, use, and maintenance of EBPs in school-based settings (46, 47). A detailed description of our scoping review methodology is described elsewhere (48).
Twenty-one studies met our inclusion criteria, representing community-based programs in diverse Tribal communities and settings. The programs encompassed a variety of health domains, including chronic disease and injury, substance misuse, wellness and illness prevention, and historical trauma, delivered among adults and/or children and youth. Key entities who were crucial to planning program implementation included decision makers in healthcare, school, community, organizations, academics, and government. Most cited barriers (n = 38) sorted into the category of “Social determinants of health,” which included barriers related to socioeconomic, geographic, and structural challenges, and the impact of historical oppression and trauma. Specific barriers related to program adoption included limited funding, competing demands, and lack of program integration with cultural values. These barriers created challenges in obtaining buy-in and support from key decision makers and community members. Barriers related to program implementation and maintenance included high attrition among program participants, high personnel turnover, limited evaluation skills among program implementers, and lack of technical assistance. These barriers have implications for ensuring implementation fidelity and sustaining community participation and support.
The most commonly reported SISTER implementation strategy (identified in 86% of studies) was: “Build partnerships (i.e., coalitions) to support implementation,” followed by “Capture and share local knowledge” (81%), “Tailor strategies” (71%), and “Conduct local consensus discussion” (52%). Four SISTER strategies, previously recognized as being highly important for D&I success in non-Indigenous settings were represented in the top 10 strategies (47). These were, “Conduct ongoing training,” “Monitor the progress of the implementation effort,” “Provide ongoing consultation/coaching,” and “Make training dynamic.” Four SISTER strategies previously described as most feasible for successful D&I in non-Indigenous settings were also represented in the top 10 (47). These were: “Capture and share local knowledge,” “Make training dynamic,” “Distribute educational materials,” and “Facilitation/Problem solving” (48).
Key informant interviews
NPAIHB, ANTHC, and ITCA team members invited five sexual health educators from their respective regions to share their experience adopting, implementing and maintaining sexual health education EBPs with AI/AN youth. The interviews were conducted via Zoom; they lasted about 45 min, and were audio-recorded for transcription. Participant characteristics were collected in a brief post-interview survey. Participants received a $20 e-gift certificate in appreciation of their time. We developed an interview guide based on the adoption, implementation, and maintenance steps outlined in the CHAMPSS model. Closing questions focused on recommendations to adapt iCHAMPSS for use in Native communities (see interview guide in Supplementary materials). For data analysis, we developed a codebook based on the interview guide to categorize each step in the adoption, implementation, and maintenance process as an analytic unit. We used ATLAS.ti to code the 15 key informant interviews according to the codebook. New codes were created based on emerging themes in each category and further broken down into subthemes.
Our key informants comprised nine women, three men, and one gender non-conforming individual. Two did not disclose their gender. The majority self-identified as AI/AN, with two also selecting Asian/Pacific Islander; four participants self-identified as non-Hispanic White. Five participants listed their primary role as a health educator; others included community representatives, clinical staff, a school administrator, youth mentor, and parent. Combined, participants had over 32 years' involvement in decision-making around or implementing sexual health education.
High rates of teen pregnancy and STIs were cited as key factors for prioritizing sexual health education in Native communities. Participants recommended engaging community partners, including community and Tribal leaders, elders, representatives from youth-serving agencies, parents, and youth throughout the planning process to build community support and reduce individual burden. Framing sexual health from a holistic health perspective and integrating culture as a protective factor helped to increase comfort and support for sexual health education. Compiling and sharing local data on adolescent health priorities and resources helped to generate support and guide program selection. Effective communication with key decision-makers, including Tribal Council and/or school board members, engaging youth voice, and preparing required paperwork, such as a memorandum of agreement, facilitated program approval.
Successful implementation of an approved program was influenced by the facilitator's community presence, visibility, and relationship with schools and community-based programs. Participants emphasized the need for pre-planning and effective communication with site leadership regarding program logistics (e.g., supplies, space, and co-facilitators) to avoid potential barriers. Integrating digital resources helped overcome geographic challenges. Effective teaching strategies included becoming comfortable with sexual health topics, being flexible, open-minded, culturally aware, and receptive to community and youth needs. Acknowledgment of diverse backgrounds and values within the classroom, encouraging youth voice, developing and enforcing classroom rules, and integrating self-care were identified as key factors for creating a supportive environment for facilitators and youth. Engaging youth as peer educators, providing incentives, and tailoring activities, such as inviting Tribal elders and clinicians as guest speakers, helped sustain youth involvement. Participants recommended engaging youth in reflecting on what worked well and what could be improved, and celebrating program successes with youth.
Successful maintenance of a sexual health program relied on ongoing, open communication with community members throughout the year. Sharing successes and lessons learned helped sustain interest and support. Seeking opportunities for community collaboration and input helped tailor programs to better reflect community-specific needs. Ongoing engagement with youth through cultural activities and events helped to maintain the excitement and “buy-in.” Given high personnel turnover, participants emphasized the need for ongoing training, technical assistance, and peer support to sustain and grow their program.
Recommendations for adapting iCHAMPSS for Native educators included greater representation of Native cultures and people through graphics, imagery, color schemes, and art. Participants appreciated the inclusion of videos to convey information, and recommended easy access to technical assistance or a program point of contact for implementation support. Overall, participants recommended simplifying the CHAMPSS model, and adapting the tools to reflect relevant processes in Native communities.
Prioritizing barriers and facilitators
With input from our Expert Advisory Group, the planning group synthesized findings from the needs and asset assessment to prioritize important and changeable barriers and facilitators for implementing culturally-relevant sexual health EBPs in AI/AN communities. Importance relates to how causally related a given barrier or facilitator is to implementation; changeability relates to the ease or difficulty of changing that factor (49). We chose to frame the prioritized list in the positive—that is, even when a barrier was identified, we stated it in terms of the change that needed to happen to improve implementation outcomes. We used these key recommendations to inform planning for IM Task 2 (Table 1).
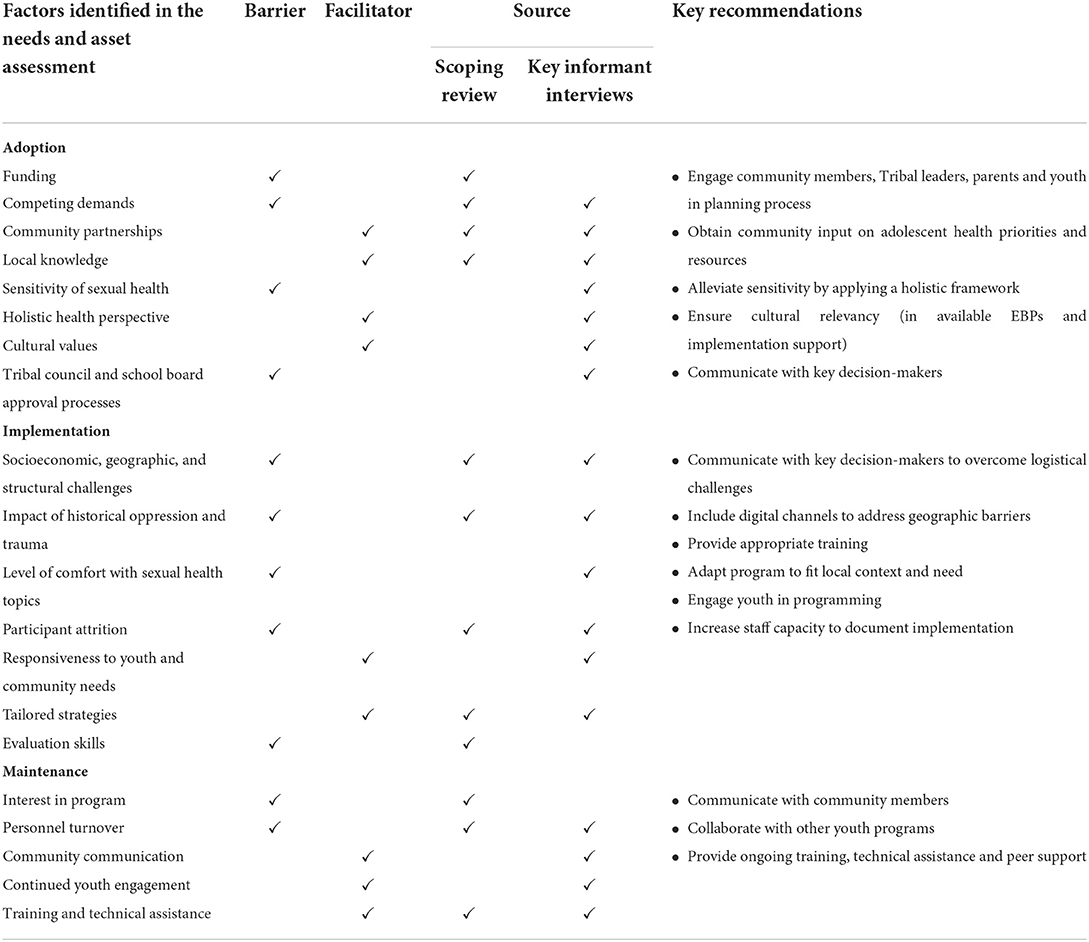
Table 1. Implementation Mapping Task 1: Identified barriers and facilitators for adopting, implementing, and maintaining culturally-relevant, evidence-based sexual health education programs in AI/AN communities.
IM Task 2. Identify adoption and implementation outcomes, performance objectives, determinants, and change objectives
In IM Task 2, implementation planners state adoption and implementation outcomes and performance objectives, identify determinants, and develop matrices of change objectives. Adoption and implementation outcomes are statements that describe the goal of program adoption, implementation, and maintenance. Performance objectives describe the specific steps, or sub-behaviors, that adopters and implementers must perform to meet that overall adoption or implementation goal. Performance objectives make clear “who has to do what” for the program to be adopted, implemented, and maintained. For example, for adopters, one question is: “What do [adopters] have to do to make the decision to use [the program]?” (27).
The planning group used findings from our needs and asset assessment and Expert Advisory Group feedback to adapt the adoption and implementation outcomes and performance objectives from the CHAMPSS model to better reflect the values and experiences of AI/AN communities. Table 2 lists the adoption and implementation outcomes and performance objectives for the Healthy Native Youth Implementation Toolbox.
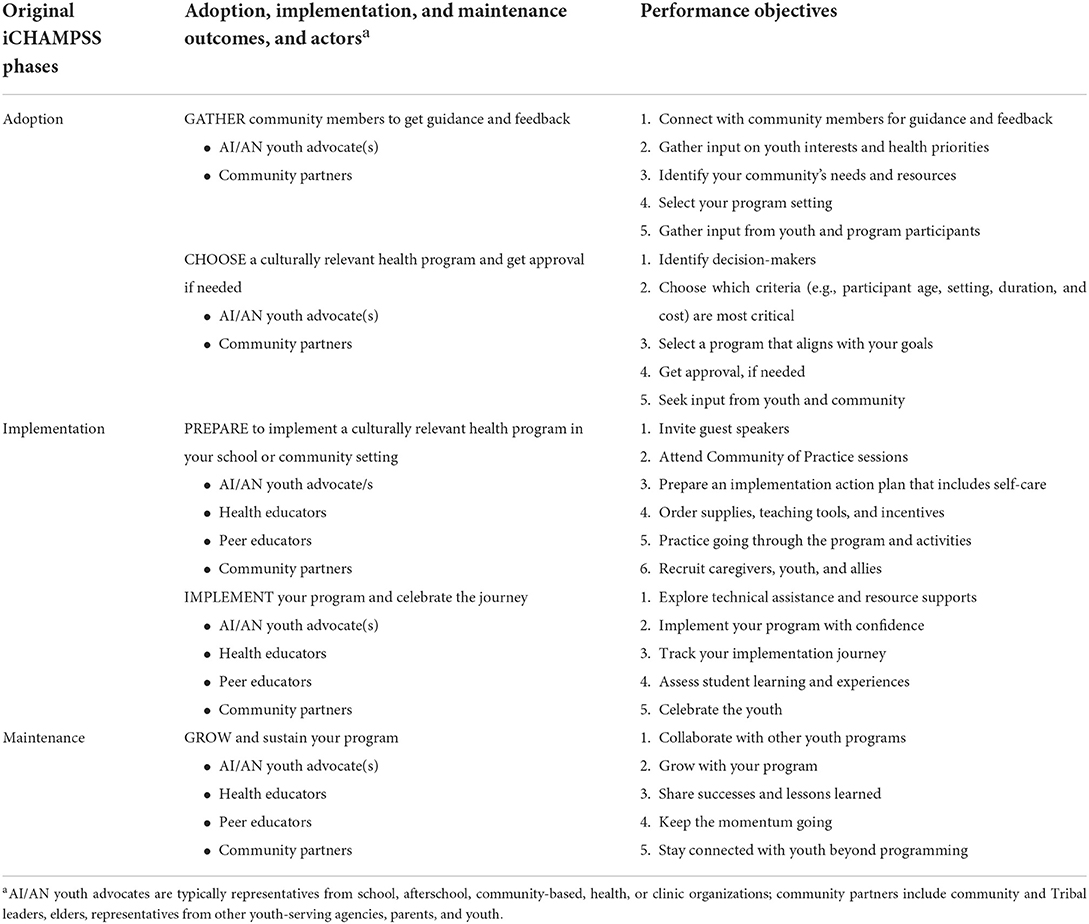
Table 2. Implementation Mapping Task 2: Adapted adoption, implementation, and maintenance outcomes, actors, and performance objectives.
Findings from Task 1 emphasized the importance of building partnerships, as well as capturing and sharing local knowledge, to support EBPs in AI/AN communities. Feedback from our Expert Advisory Group and key informant interviews reiterated the importance of collaborative processes, community involvement, and inclusion of youth voice throughout the planning process. Recommendations were to simplify the model, with a focus on community capacity-building and collective decision-making with the community and youth. Recognizing the diverse settings in which sexual health programs are implemented in AI/AN communities and the diverse profiles of Tribal health educators, we expanded key partners beyond the school system, and identified AI/AN youth advocate(s) (e.g., representatives from school, afterschool, community-based, health, or clinic organizations) and community members, including community and Tribal leaders, elders, representatives from youth-serving agencies, parents, and youth as key actors for program adoption, implementation, and maintenance. Additional actors for implementation include Tribal health educators and peer advocates for specific program delivery.
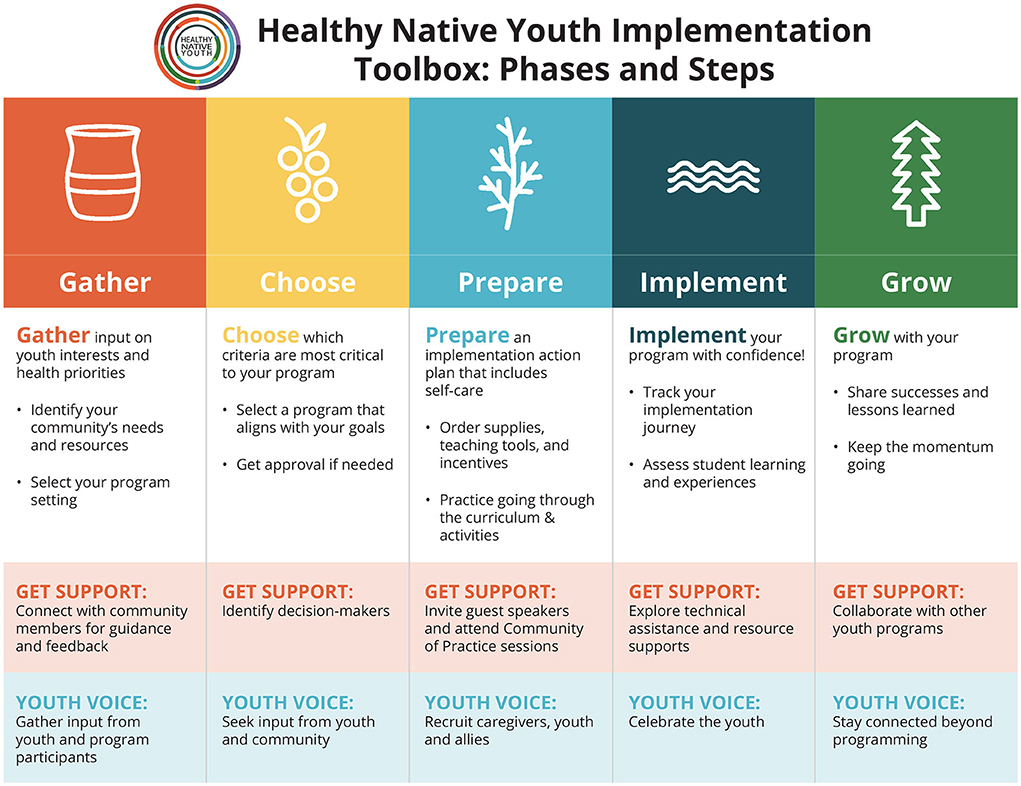
To simplify the tasks involved in program adoption, we combined two CHAMPSS' steps, “Prioritize” and “Assess,” into a single phase, titled “GATHER,” and two CHAMPSS' steps, “Select” and “Approve,” into a single phase, titled “CHOOSE.” GATHER recognizes the importance of community members coming together to share their learning, visionary wisdom, and perspectives. It recognizes Tribal communities as experts and engages with them as partners to gather input on adolescent health priorities and desired health skills. Taking a strengths-based, holistic approach, the model recognizes that adolescent sexual health represents one aspect of overall physical, mental, emotional, social, and spiritual health (50, 51). The GATHER phase performance objectives describe the specific steps that program adopters must take to identify youth interests and health priorities in their community.
“CHOOSE” recognizes the role of shared decision-making in selecting a health program that best aligns with these interests and health priorities. The CHOOSE phase performance objectives describe the steps that program adopters must take to select a culturally-relevant, age-appropriate, evidence-based health promotion program, and get approval from key decision-makers in a school or community setting, such as the school principal, clinic director, school board, health committee or Tribal council. Given varying tribal review and school board approval processes, these steps engage partners with decision-makers early in the planning process to better understand program constraints and requirements from their perspective.
For program implementation, we modified the CHAMPSS steps, “Prepare” and “Implement,” to help implementers plan and deliver a culturally-relevant program. The “PREPARE” phase performance objectives describe the steps needed to plan program implementation and gain support from key decision-makers. Inviting guest speakers, for example Tribal elders, recruiting peer educators, and integrating cultural activities, help to engage youth and community members, and increase program transparency. Integrating self-care planning for implementers and youth helps to reduce personnel burnout and create a supportive learning environment. “IMPLEMENT” focuses on program delivery with a shift from traditional fidelity and assessment to an emphasis on reflection, listening, and feedback. The IMPLEMENT phase performance objectives describe the steps needed to implement the program successfully and collect feedback to guide future program adjustments.
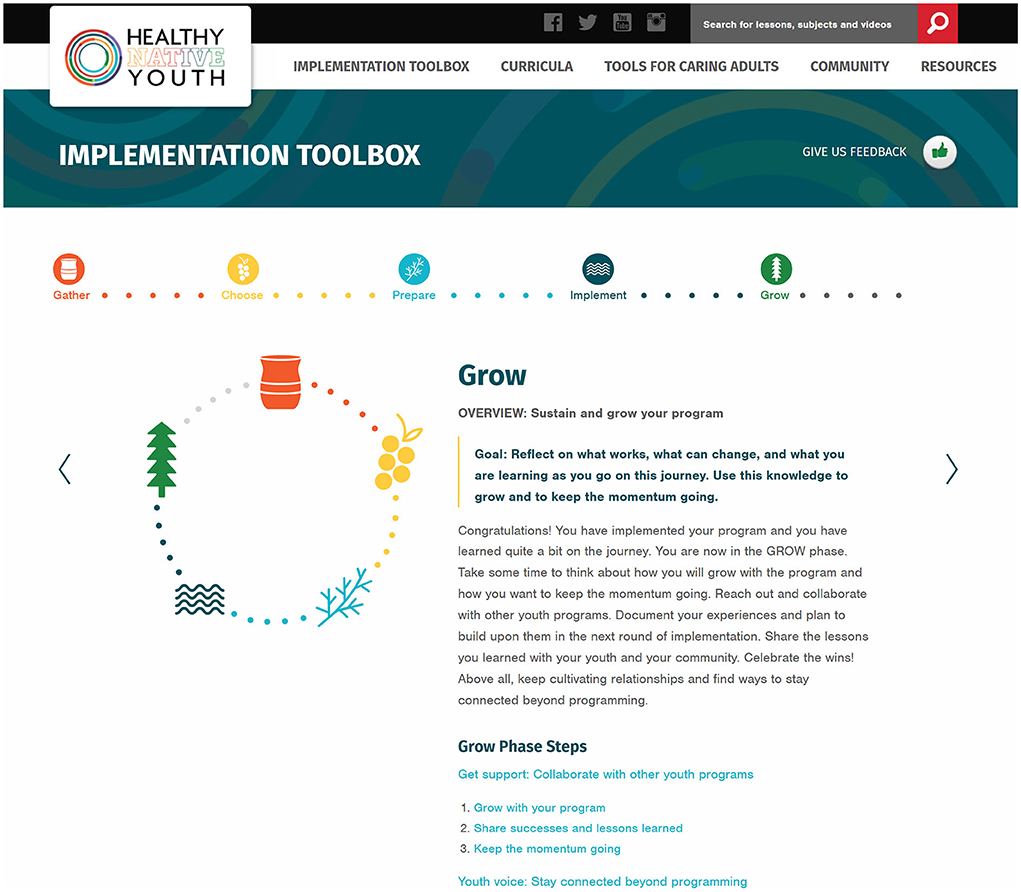
For program maintenance, we modified the CHAMPSS step, “Maintain,” to inform our “GROW” phase. “GROW” recognizes the importance of reflection and collaboration to nourish and sustain your program. The GROW phase performance objectives describe the steps that planners must take to grow and sustain their program by sharing successes with community members, and cultivating relationships across other youth programs and services to keep youth engaged.
The critical elements, “Get support” (i.e., connecting with other supporters of EBPs and adolescent health) and “Youth Voice” are integrated throughout the planning process in the first and final performance objectives of each phase. These elements underscore the importance and value placed in Native communities on building partnerships, capturing and sharing local knowledge, and ensuring inclusive participation throughout the adoption, implementation, and maintenance process.
As in the original CHAMPSS model, the Toolbox conceptual model is circular (Figure 3), indicating that partners may enter the model at any phase depending on their community's readiness or experience implementing sexual health EBPs, or they may enter the planning process at the beginning to adopt a new sexual health program. Figure 4 presents the “rolled-out” version of the model, illustrating the five phases (Gather, Choose, Prepare, Implement, and Grow) and phase-specific steps in the adapted Healthy Native Youth Implementation Toolbox model.
After we identified the performance objectives for each phase, we reviewed findings from Task 1 and the original CHAMPSS planning documents to identify important and changeable personal determinants for adopters and implementers. Determinants answer the question of “why?” For example, “Why would an implementer deliver the program as planned?” These may be constructs from health promotion theories, such as Social Cognitive Theory (23) or Theory of Planned Behavior/Reasoned Action Approach (52), or from implementation science frameworks. They are modifiable factors internal to the adopters and implementers that influence their adoption and implementation behavior (27). In developing the CHAMPSS model, we identified awareness/knowledge, attitudes, skills and self-efficacy, outcome expectations, and perceived norms as important and changeable determinants for sexual health EBP adopters and implementers (17, 19). The planning group agreed that these determinants were also relevant for adopters and implementers in AI/AN communities. Thus, we used these determinants to complete the final step in IM Task 2, develop matrices of change objectives.
Matrices cross performance objectives with personal determinants to produce change objectives. They answer the question: “What has to change in this determinant to bring about this performance objective?” Change objectives are the discrete changes required in each relevant determinant to influence achievement of the performance objective (27). Table 3 presents the matrix of change objectives for the Toolbox adoption phase, GATHER. The first performance objective is for the AI/AN youth advocate and community partners to “PO1: Connect with community members for guidance and feedback” and the corresponding change objective for the determinant, Awareness/Knowledge, is “List venues and organizations from which to engage youth and adult community members who understand and care about adolescent health priorities.” These matrices of change objectives formed the blueprints for adapting or developing new implementation methods and strategies in IM Task 3.
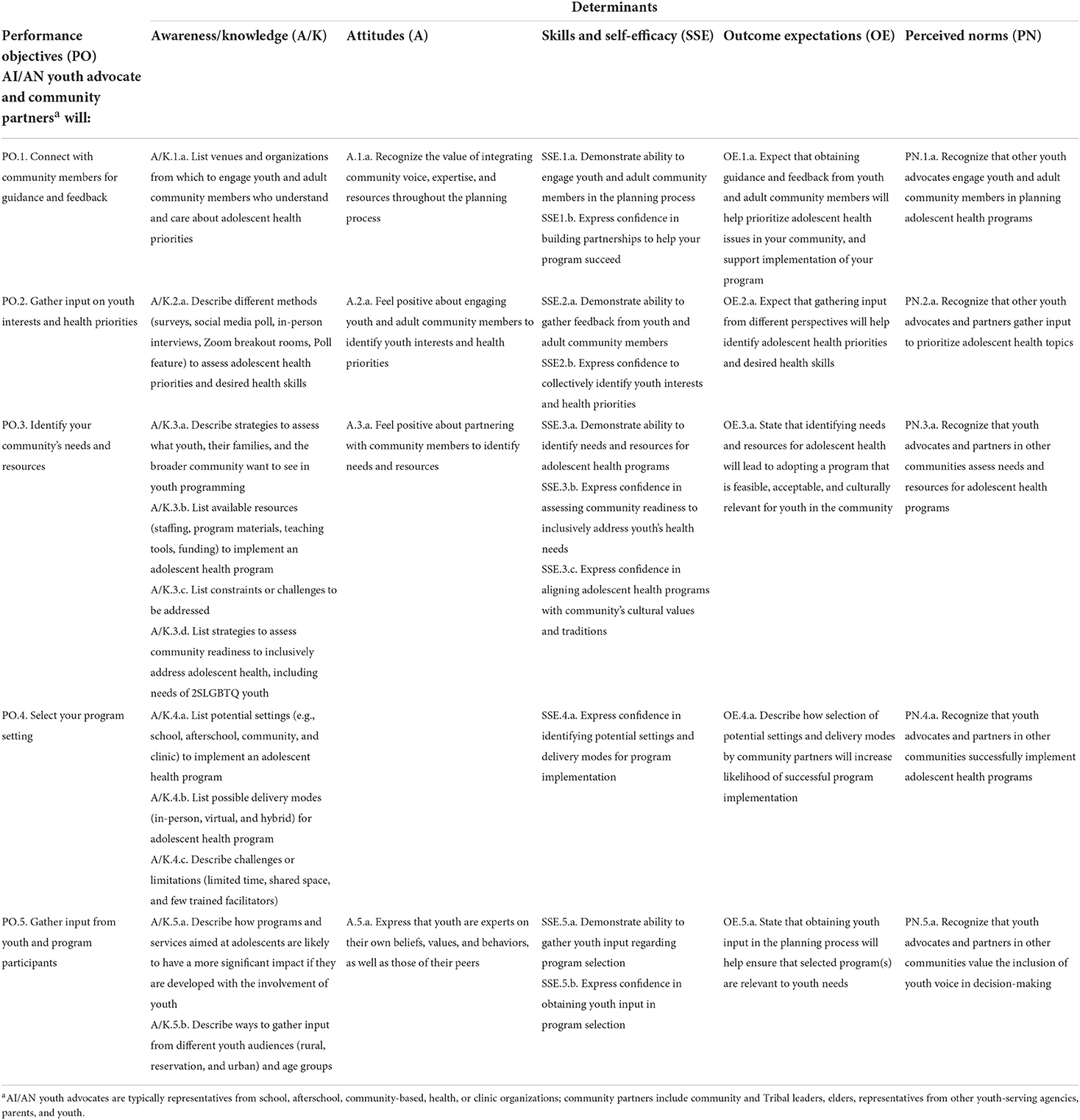
Table 3. Implementation Mapping Task 2: Example matrix of change objectives for adoption outcome, “GATHER community members to get guidance and feedback.”
IM Task 3. Select theoretical methods and design implementation strategies
In IM Task 3, planners choose theory- or evidence-based methods to in?uence the determinants identified in Task 2. They also select or design implementation strategies to operationalize those methods. Theory-based methods are techniques to influence determinants of implementation (27, 28). These methods can focus either at the individual level (the knowledge, attitudes, and skills of the implementer), or at the organizational level aimed at influencing organizational change directly (e.g., creating strong organizational leadership). Methods are important as they represent the underlying mechanism for change for an implementation strategy. Methods originate from behavioral, organizational, and community change theories, such as Social Cognitive Theory (23), the Elaboration Likelihood Model (53), Organizational Development Theory (54), and Models of Community Organization (55). These theories also specify “parameters” or situations under which a method is used appropriately. Implementation strategies refer to the ways in which program planners operationalize methods to influence determinants and change objectives for a specific adopter and task (small-scale strategies) or to the overall package of strategies influencing adoption, implementation, and maintenance (27).
In IM Task 3, we reviewed the theory-based methods and implementation strategies used in iCHAMPSS to guide decisions regarding the adaptation or development of culturally-relevant implementation strategies for the Healthy Native Youth Implementation Toolbox. During formative feedback sessions, our Healthy Native Youth AI/AN Adolescent Sexual Health Workgroup provided input on the acceptability and feasibility of specific implementation strategies to promote sexual health EBPs in Native communities.
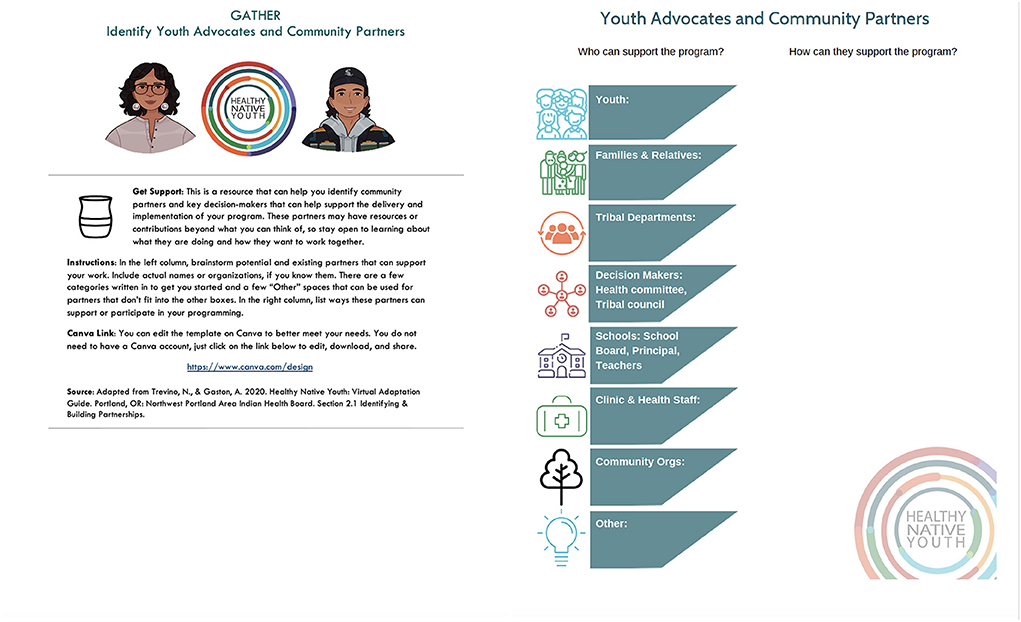
In iCHAMPSS, we used multiple methods, including elaboration, persuasive communication, modeling, shifting perspective, goal-setting, and technical assistance to influence change objectives for the adoption, implementation, and maintenance of sexual health EBPs. The corresponding implementation strategies included step overviews, success stories, facts and tip sheets, ready-to-use templates, and helpful links (19). Reviewing these strategies, as well as existing culturally-relevant strategies developed by the planning group, such as the NPAIHB's Adolescent Health Tribal Action Plan (50), the Healthy Native Youth: Virtual Adaptation Guide (56), and strategies from the Native STAND Dissemination, Implementation and Evaluation project, we developed a list of possible methods and implementation strategies for the Toolbox. Table 4 provides examples of methods, parameters, and implementation strategies for steps in the GATHER phase. For example, in “PO.1. Get support: Connect with community members for guidance and feedback,” we used the methods of active learning (from the Elaboration Likelihood Model) (53) and enhancing network linkages (from Theories of Social Networks and Social Support) (57) to influence awareness/knowledge, skills, and self-efficacy related to connecting with community members. The associated implementation strategy was a customizable worksheet template to identify youth advocates and community partners.
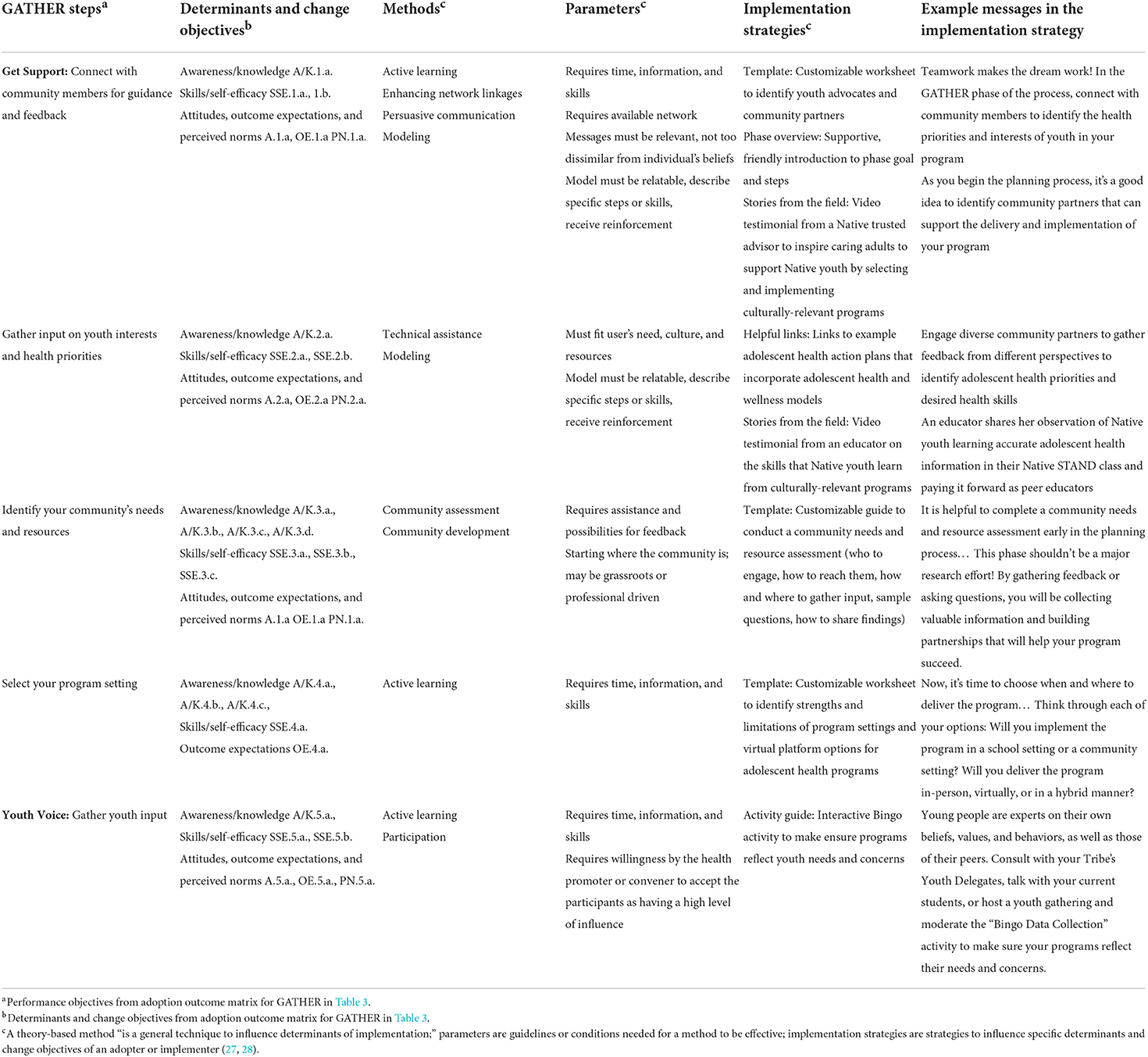
Table 4. Partial Implementation Mapping Tasks 3 and 4: Steps, determinants, methods, parameters, implementation strategies, and example messages from the Healthy Native Youth Implementation Toolbox GATHER phase.
After reviewing possible methods and implementation strategies for all five Toolbox phases with our Healthy Native Youth AI/AN Adolescent Sexual Health Workgroup, we identified a common set of implementation strategies or “tool types.” These included phase overviews, templates, examples, activity guides, helpful links to resources (including Healthy Native Youth Community of Practice recorded sessions), tips, and stories from the field (video testimonials from experienced AI/AN sexual health educators). Healthy Native Youth's Curriculum Portal and Request Technical Assistance feature were also identified as important implementation strategies. Table 5 provides a description of each “tool type,” including its related determinants, methods, purpose, and delivery mode.
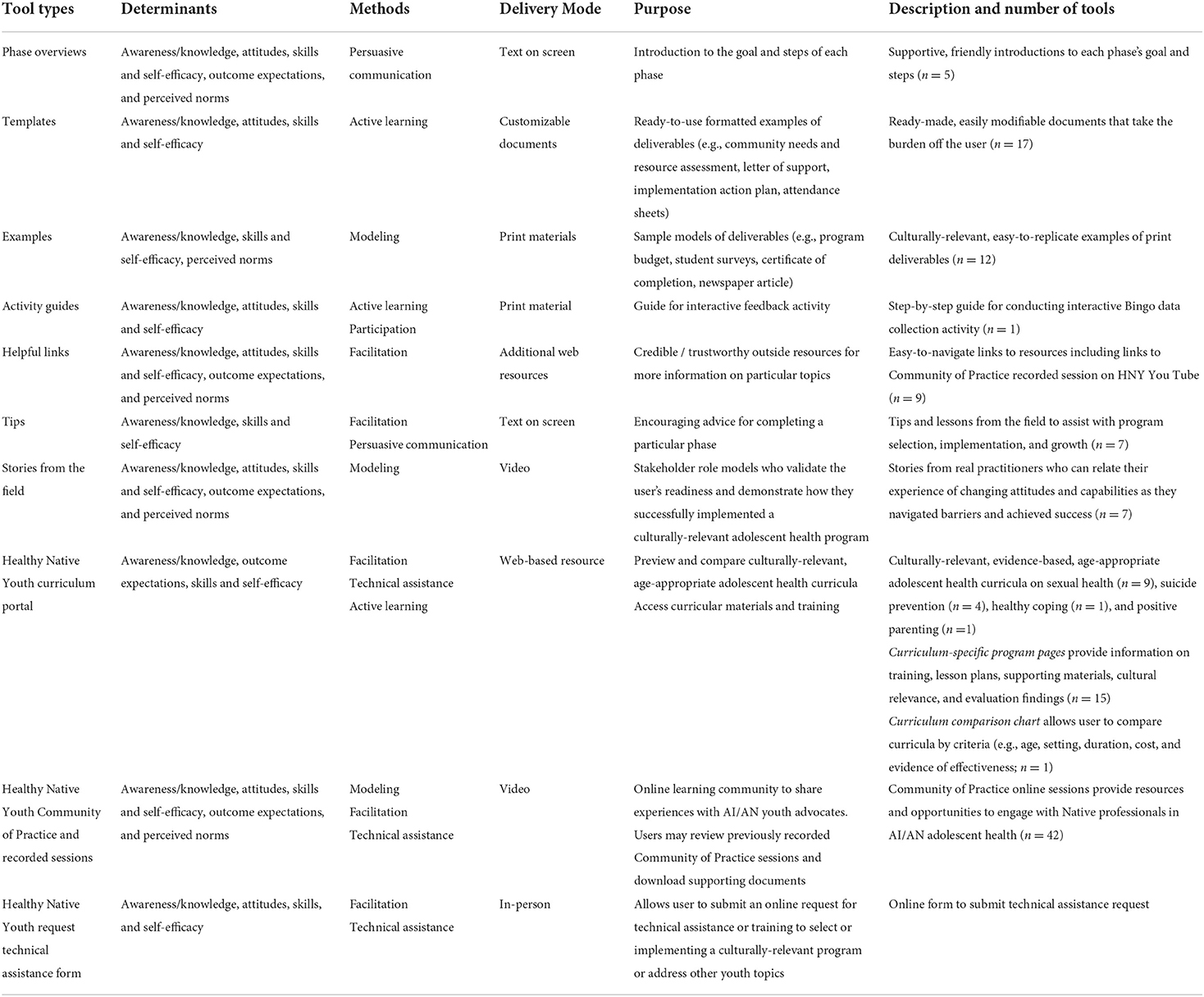
Table 5. Implementation Mapping Tasks 3 and 4: Healthy Native Youth Implementation Toolbox tool types: Determinants, methods, delivery mode, purpose, and description.
IM Task 4. Produce implementation protocols and materials
In IM Task 4, planners produce implementation protocols, activities and/or materials. Similar to Step 4 in Intervention Mapping, this requires planners to create design documents, draft content, pretest and refine content, and produce final materials. Design documents are shared between planners and production teams, and they are created for each document or other materials that are a part of the implementation strategy (27).
In Task 4, the planning group developed design documents and drafted content to guide production of the Healthy Native Youth Implementation Toolbox and its supporting tools. The design documents provided detailed instructions for program designers to produce the Toolbox, including specific content, messages, and tools for each Toolbox phase. We shared proposed tools and website design mock-ups with our Healthy Native Youth AI/AN Adolescent Sexual Health Workgroup to obtain feedback prior to final production.
Website development
We partnered with the original Healthy Native Youth website design team to develop and integrate the Toolbox into the existing website. Utilizing an user-centered design process, the website designers created “use cases” to determine different user experiences interacting with the Toolbox, and wire frames to guide feedback with the planning group during website development. To increase accessibility, the Toolbox is designed to be viewed on desktop, laptop, tablet, and mobile devices.
The Implementation Toolbox is accessed via the Healthy Native Youth website (www.healthynativeyouth.org; Figure 5). The home page includes links to an Introduction, which orients users to the purpose of the Toolbox, and two features, “Where Do I Start?” and “The Big Picture,” which are tailored to the user's experience or need. The “Where do I start?” feature is tailored for users who have already started the process of implementing youth programs and may have specific goals. The user can select from a list of nine activities, each relating to one of the five phases, such as, “I want to engage youth in the planning process,” “I want to do a community needs assessment,” or “I want to select a health curriculum,” and be directed to the relevant phase and tools. “The Big Picture” feature provides a concertina-style overview of the five phases and their respective steps and tools, so that users may select their own entry point into the Toolbox. The “ulu” icon (an all-purpose knife traditionally used by Inuit, Iñupiat, Yupik, and Aleut women) indicates links to relevant tools. “The Big Picture” feature was designed for easy viewing on mobile devices (Figure 6).
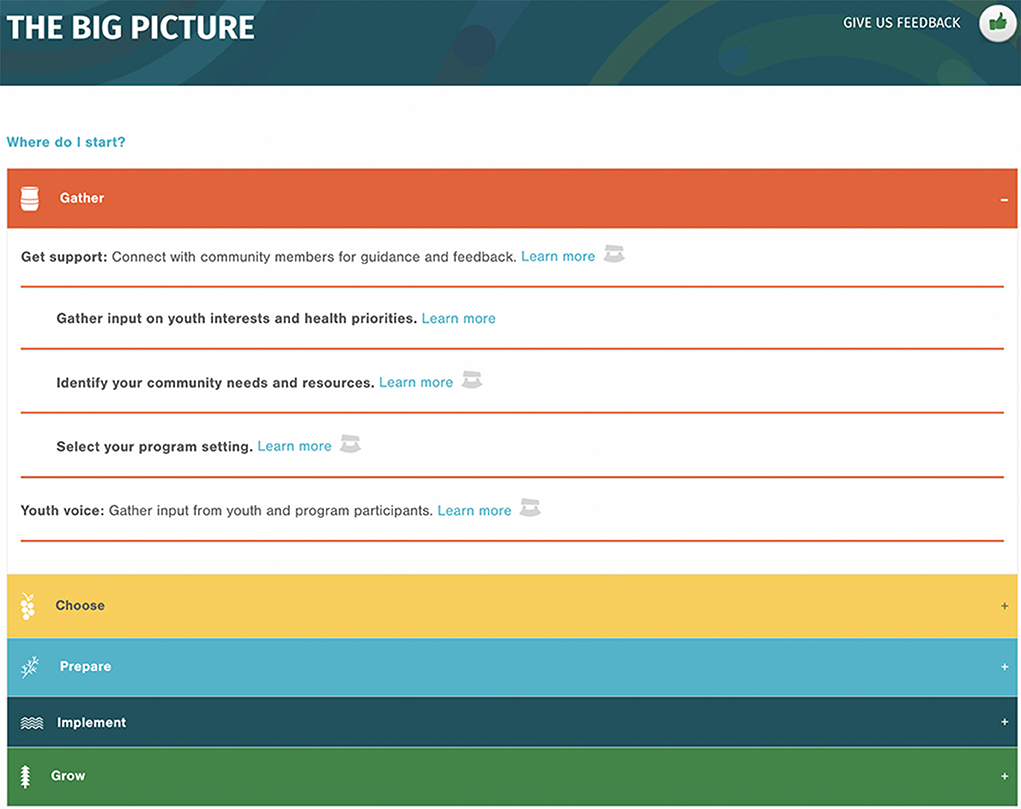
Figure 6. Screen capture of the Healthy Native Youth Implementation Toolbox: The Big Picture feature.
Within the Toolbox, each phase has its own Phase Overview page that orients the user to the goal and steps for that phase, including steps for Get Support and Youth Voice. Each overview page leads to step-specific pages with links to relevant tools (templates, examples, activity guide, tips, helpful links, or success stories) to successfully complete the phase. A radio button panel across the top of each page indicates the user's overall progress through the phases and steps (Figure 7).
Tools development
The planning group developed design documents for each tool that specified its purpose, delivery mode, content, and messages. The tone of the messages is user-friendly, strength-based, and supportive. Table 3 (sixth column) provides example of specific messages for tools in the GATHER phase. The NPAIHB graphic design team developed Indigi-icons, reflective of Native values, to represent each phase in the planning process (Figure 4). Each tool includes the Indigi-icon for its respective phase and simple instructions on how to use the tool. Figure 8 presents the customizable template from the GATHER phase to create a youth advocates and community partners map.
Healthy Native Youth's Curriculum Portal is an important tool for the CHOOSE phase as it provides free access to culturally-relevant, age-appropriate evidence-based curricula designed or adapted for AI/AN youth. The portal currently includes nine curricula related to sexual health, four related to suicide prevention, and two related to healthy coping and positive. Curriculum-specific program pages provide information on training, lesson plans, supporting materials, cultural relevance, and evaluation findings. The Curriculum Comparison Chart allows users to compare curricula by criteria (e.g., age, setting, duration, cost, and evidence of effectiveness) to select a curriculum that best aligns with their community's goals. Evidence of effectiveness follows the Center for Disease Control and Prevention's (CDC) classification of evidence-based practices: emerging practice, promising practice, leading practice, best practice, and/or tribal best practice (8) (Figure 9).
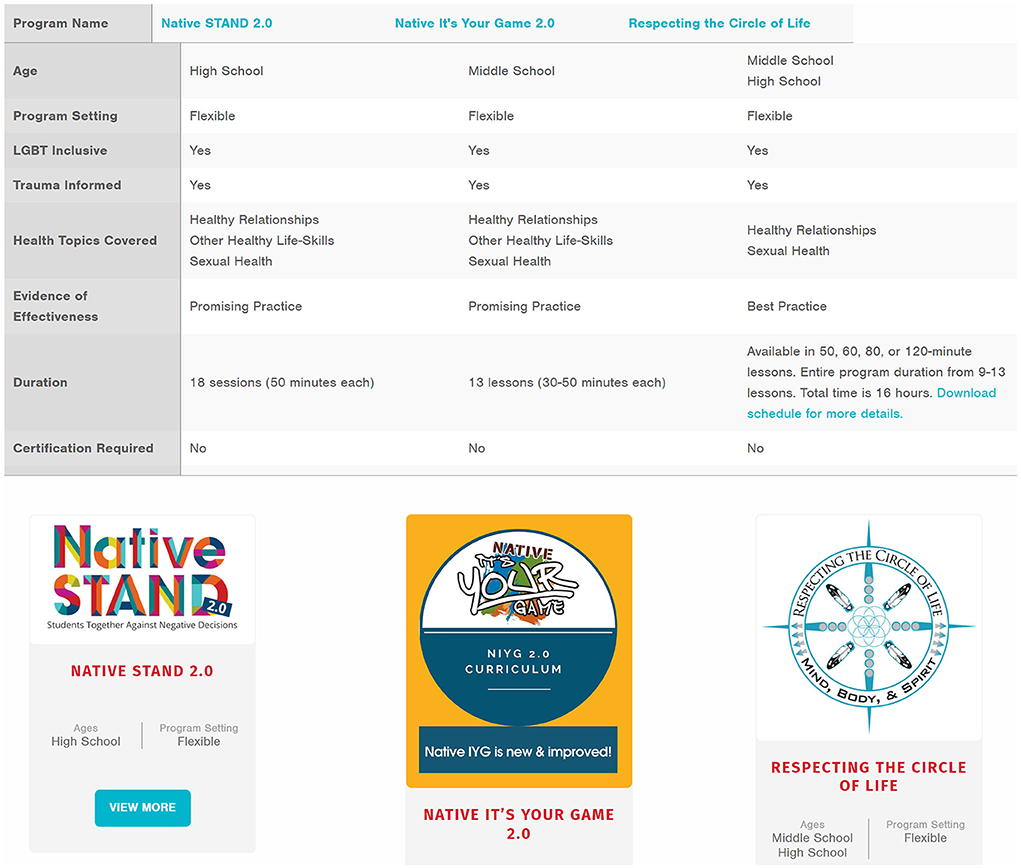
Figure 9. Healthy Native Youth curriculum portal resources, including curriculum comparison chart and example curricula.
Finally, the Healthy Native Youth Community of Practice and Request Technical Assistance features provide peer and technical support from the Healthy Native Youth Collective Partnership to help AI/AN youth advocates adopt and implement culturally-relevant health programs. The Healthy Native Youth SMS text messaging series provides additional resources for directly for youth and trusted adults. See Supplementary material for a comprehensive list of current Toolbox tools by phase. Table 6 provides a side-by-side summary of adaptations by Implementation Mapping task from the original iCHAMPSS decision support system to the adapted Healthy Native Youth Implementation Toolbox.
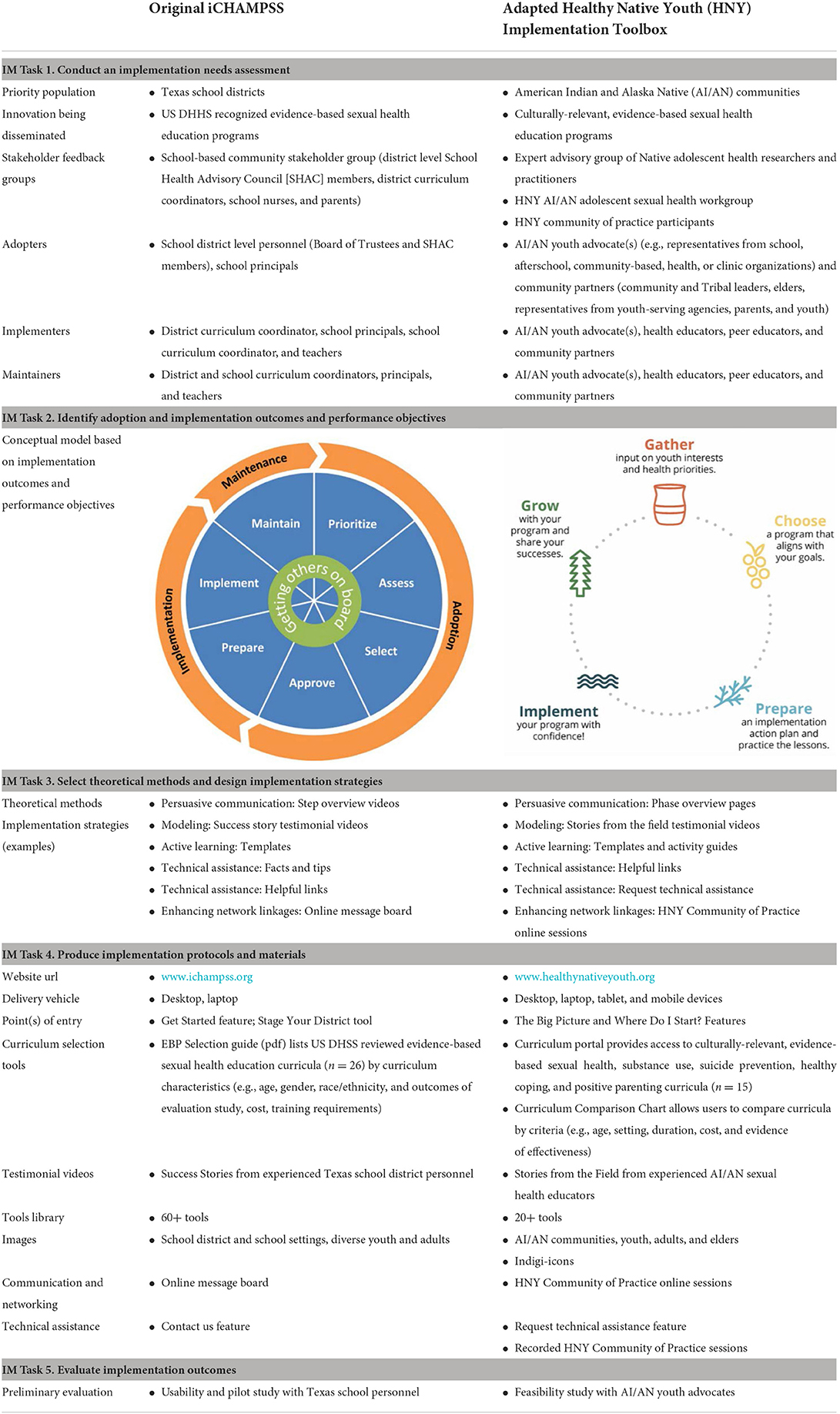
Table 6. Summary of Adaptations from iCHAMPSS to the Healthy Native Youth Implementation Toolbox by Implementation Mapping Task.
We launched the Healthy Native Youth Implementation Toolbox in December, 2021. We have sequentially shared the GATHER, CHOOSE, PREPARE and IMPLEMENT, and GROW phase tools with AI/AN youth advocates at four, online Community of Practice sessions. The feedback from practitioners has been positive, with comments including: “very user friendly,” “helpful, easy to understand,” “concretely helpful tools,” “visually great,” “ease of access.” We also received feedback that, “Downloadable tools and templates in the Big Picture were hard to find.” We are also actively disseminating the Toolbox via Healthy Native Youth's e-newsletter, Twitter, and Facebook page and Indiancountryecho.org. Based on feedback, we are compiling a list of features for the Healthy Native Youth Implementation Toolbox version 2.0, which will include a searchable “tools library” to help users locate the tools they need.
IM Task 5. Evaluate implementation outcomes
In IM Task 5, planners develop an evaluation plan that describes expected implementation outcomes for adoption, implementation, and/or maintenance (27). To inform evaluation planning, we are conducting a feasibility study to obtain feedback from AI/AN youth advocates on their experience using the Toolbox, and to assess its preliminary impact on individual and community-level determinants for implementing culturally-relevant sexual health EBPs in AI/AN communities. Using a convenience sample, pre/post-test design, we have recruited 29 individuals from AI/AN youth-serving organizations across the U.S. to trial the Toolbox for a 6-month period. We will use pre- and post-test survey data to assess changes in stage of community readiness to adopt/implement/maintain a sexual health EBP; individual knowledge and attitudes toward culturally-relevant sexual health EBPs; perceived support of an EBP by various groups (e.g., parents and Tribal leaders); self-efficacy to complete each Toolbox step, and network connections to advocate for culturally-relevant sexual health EBPs. Post-test survey items adapted from previous usability instruments will assess acceptability, ease of use, utility, credibility, motivational appeal, and perceived helpfulness (24, 25, 58, 59). Additional items request recommendations for future enhancements. Findings will inform the development of Toolbox Version 2.0 and provide preliminary data for a future multisite effectiveness-implementation trial.
Discussion
Limited tools exist to help AI/AN communities adopt, implement, and maintain culturally-relevant, age-appropriate, evidence-based adolescent sexual health education programs. We used the systematic planning approach, Implementation Mapping, to adapt an existing online decision support system, iCHAMPSS, to better support sexual health education D&I processes in Native communities. The resulting conceptual model that underlies the Healthy Native Youth Implementation Toolbox is reflective of the values and experiences of AI/AN communities. More importantly, the Toolbox provides guidance and decision support to Tribal health advocates on each phase of the process, sharing adaptable ready-to-use templates, relatable examples, and stories from the field. Many health educators tasked with selecting and implementing a culturally-relevant, age-appropriate sexual health program do not have formal training in public health or research methods. Developing approachable language and visuals, offered in phased bite-size pieces, is critical to meet the needs of diverse program champions, who in turn must navigate diverse delivery settings. Many of the tools and templates now featured in the Toolbox had already been used in the field by Tribal health educators, but were not logically sequenced or offered with accompanying tips or examples. Consolidating these tools and resources into a comprehensive Toolbox was a critical next-step to support AI/AN health advocates and community partners to navigate the planning process.
Using Implementation Mapping to guide the adaptation process had multiple advantages and helped address several challenges previously identified in the implementation science literature. Prior research has highlighted the need for methods that improve the selection and tailoring of implementation strategies for a given setting (60), and that articulate the causal pathways through which implementation strategies are effective (61). Implementation Mapping provided a systematic approach to select, adapt, and create implementation strategies that are tailored to the cultural values and realistic experiences of Native communities. In Tasks 1 and 2, we identified barriers and facilitators unique to the D&I process of sexual health EBPs in Native communities, and developed culturally-relevant behavioral outcomes and performance objectives to guide the adaptation process. In Tasks 3 and 4, we selected theory-based methods that would influence the personal determinants of Native adopters and implementers, and designed culturally-relevant tools and messages to facilitate the D&I process. The explicit linkage of determinants to methods to tools articulates the proposed mechanism of change that underlies the Toolbox.
Prior research has also highlighted the critical role of community engagement to accelerate and improve the implementation of EBPs. Community-engaged D&I research can help improve health inequities through incorporating unique perspectives from communities, that have been historically left out of the research process (62, 63). Collaborative planning is a fundamental principal of Implementation Mapping (27). Our adaption process involved a multi-disciplinary research team together with input from diverse partners ranging from national experts to educators on the ground to capture the unique experience of implementing sexual heath EBPs in Native communities. We are continuing to collect feedback from users to guide further development of the Toolbox to ensure higher reach, satisfaction, and sustained implementation outcomes. Continued training and technical assistance will be also critical to successfully support uptake and use.
Developing culturally-relevant implementation strategies requires collaboration with AI/AN practitioners and academicians, as well as responsiveness to Native-informed practice models and conceptual frameworks (37, 38). Interventions must also align with organizational capacity and community readiness to be sustainably implemented (39). Our adaptation process was informed by cultural sensitivity adaptation frameworks and principles (37, 64–68), and included changes to surface and deep structures (65). Surface structure adaptations involved matching materials and messages to observable characteristics of AI/AN communities (e.g., images, people, and locations), while deep structure involved incorporating cultural, social, environmental, and psychological processes unique to the dissemination and implementation of sexual health EBPs in Native communities. We used an iterative design process, incorporating input from diverse Native partners, to ensure that the final product reflects cultural identification, community values, and needs.
Although using Implementation Mapping had multiple advantages, it was not without its challenges. These included the time required to identify relevant outcomes and performance objectives that reflected the values and processes involved in adopting, implementing, and maintaining sexual health educations programs in Native communities. This process took over a year to complete, with iterative feedback from our advisory groups and community members. It then took 6 months to translate these objectives into supportive, accessible messaging and tools that would resonate with our intended audience. Lessons learned along the way included the critical role that NPAIHB, ANTHC, and ITCA's collective experience partnering with AI/AN communities played in grounding the adaptation process from a holistic, strengths-based perspective, and the importance of collaborating with experienced AI/AN creatives for website development and graphic design to ensure that Toolbox features, language, and imagery were relevant and engaging for Native practitioners.
Alongside these lessons learned, several limitations should be noted. First, the Toolbox represents an adaption of an existing online decision support system rather than the development of a new program using ethnographic and grounded theory approaches. Thus, it does not meet the ideal of a culturally-based, culturally congruent, and culturally grounded practice emerging from AI/AN world views (37). Second, for our scoping review, although the similarity with findings from previous studies indicates some validity across cultural settings, our coding, or limited D&I research in these settings, may have failed to identify implementation strategies that are unique to Native communities. Third, the limited practitioner sample for our key informant interviews and feedback during the adaptation process means that the generalizability of the conceptual model and implementation strategies are unknown. Finally, the feasibility and efficacy of the Toolbox are yet to be established. Findings from our feasibility study will provide feedback to further refine the Toolbox, and future studies should focus on a rigorous evaluation to assess its impact on the adoption, implementation, and maintenance of sexual health EBPs in Native communities.
Conclusion
There is a continued need to design, test, and evaluate D&I strategies that are relevant to Native communities. The Healthy Native Youth Implementation Toolbox contributes to the dissemination and implementation of evidence-based, culturally-relevant sexual health education programs in diverse Native communities. The Toolbox moves beyond simply providing access to EBPs to help Native communities successfully navigate the adoption and implementation process. Implementation Mapping provided a systematic approach to guide the adaptation process and integrate community voice with the ultimate goal of improving sexual health equity among AI/AN youth.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board at the University of Texas Health Science Center at Houston, Committee for the Protection of Human Subjects (CPHS), and the Alaska Area Institutional Review Board. Appropriate tribal approval was obtained in Alaska through the Alaska Native Tribal Health Consortium. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
All authors made substantial contributions to the conception, design of the work, acquisition, analysis, interpretation of the data, and drafted the work or critically revised it for important intellectual content, provided final approval of the manuscript, and agreed to be accountable to all aspects of the work.
Funding
This work was funded by the Indian Health Service HIV Program and the Secretary's Minority AIDS Initiative Fund and by the National Institute on Minority Health and Health Disparities NIH/NIMHD 1R21MD013960-01A1. Native iCHAMPS: An Innovative Online Decision Support System for Increasing Implementation of Effective Sexual Health Education in Tribal Communities. PIs: CM, RS, and MP.
Acknowledgments
We are grateful to our AI/AN adolescent health colleagues and partners across the U.S. who provided feedback to support the development of the Healthy Native Youth Implementation Toolbox.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.889924/full#supplementary-material
References
1. Office of Minority Health. Profile: American Indian/Alaska Native. (2022). Available online at: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=62 (accessed February 27, 2022).
2. U. S. Census Bureau. Facts for Features: American Indian and Alaska Native Heritage Month: November 2021. (2022). Available online at: https://www.census.gov/newsroom/facts-for-features/2021/aian-month.html (accessed February 27, 2022).
3. Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2017. NCHS Data Brief. (2018) 318:1–8.
4. Gavin LE, Warner LS, O'Neil ME, Duong LM, Marshall C, Hastings PA, et al. Vital signs: repeat births among teens — United States, 2007–2010. Morb Mortal Wkly Rep. (2013) 62:249–55.
5. Centers for Disease Control and Prevention. HIV in the United States by Race/Ethnicity: HIV Incidence. Available online at: https://www.cdc.gov/hiv/group/racialethnic/other-races/incidence.html (accessed August 22, 2022).
6. Indian Health Service and Centers for Disease Control and Prevention. Indian Health Surveillance Report - Sexually Transmitted Diseases 2015. Rockville, MD: U.S. Department of Health and Human Services (2018).
7. Kaufman CE, Schwinn TM, Black K, Keane EM, Big Crow CK. The promise of technology to advance rigorous evaluation of adolescent pregnancy prevention programs in American Indian and Alaska Native tribal communities. Am J Public Health. (2016) 106:S1:S18–20. doi: 10.2105/AJPH.2016.303335
8. Spencer LM, Schooley MW, Anderson LA, Kochtitzky CS, DeGroff AS, Devlin HM, et al. Seeking best practices: a conceptual framework for planning and improving evidence-based practices. Prev Chronic Dis. (2013) 10:130186. doi: 10.5888/pcd10.130186
9. Craig Rushing S, Gaston A, Kaufman C, Markham C, Jessen C, Gorman G, et al. Using technology to promote health and wellbeing among American Indian and Alaska Native teens and young adults. In: Dyson LE, Grant S, Hendricks M, editors, Indigenous People and Mobile Technologies. Routledge, Taylor & Francis Group. (2016). p. 163–78.
10. Tingey L, Chambers R, Patel H, Littlepage S, Lee S, Lee A, et al. Prevention of sexually transmitted diseases and pregnancy prevention among Native American youths: a randomized controlled trial, 2016-2018. Am J Public Health. (2021) 111:1874–84. doi: 10.2105/AJPH.2021.306447
11. Shegog R, Craig Rushing S, Jessen C, Lane T, Gorman G, Torres J, et al. Native It's Your Game: improving psychosocial protective factors for HIV/STI and teen pregnancy prevention among youth in American Indian/Alaska Native communities. J Appl Res Child. (2017) 8:3.
12. Hafner SP, Craig Rushing S. Sexual Health, STI and HIV risk, and risk perceptions among American Indian and Alaska Native emerging adults. Prev Sci. (2019) 20:331–41. doi: 10.1007/s11121-018-0920-7
13. Skye M, McCoy T, Kelley A, Singer M, Rushing SC, Donald C, et al. Effectiveness of Native STAND: a five-year study of a culturally relevant sexual health intervention. Adolescents. (2021) 1:321–34. doi: 10.3390/adolescents1030024
14. Kaufman CE, Whitesell NR, Keane EM, Desserich JA, Giago C, Sam A, et al. Effectiveness of circle of life, an HIV-preventive intervention for American Indian Middle School Youths: a group randomized trial in a Northern Plains Tribe. Am J Public Health. (2014) 104:e106–12. doi: 10.2105/AJPH.2013.301822
15. Craig Rushing S, Stephens D, Shegog R, Torres J, Gorman G, Jessen C, et al. Healthy Native Youth: Improving access to effective, culturally-relevant sexual health curricula. Front Public Health. (2018) 6:225. doi: 10.3389/fpubh.2018.00225
16. Jernigan VBB, Jacob T, Styne D. The adaptation and implementation of a community-based participatory research curriculum to build tribal research capacity. Am J Public Health. (2015) 105:S424–32. doi: 10.2105/AJPH.2015.302674
17. Hernandez BF, Peskin MF, Shegog R, Markham CM, Johnson K, Ratliff EA, et al. Choosing and maintaining programs for sex education in schools: the CHAMPSS model. J Appl Res Child. (2011) 2:1–33.
18. Peskin MF, Hernandez BF, Johnson K, Addy RC, Markham CM, Shegog R, et al. Sexual health education from the perspective of school staff: implications for adoption and implementation of effective programs in middle school. J Appl Res Child. (2011) 2:1–38.
19. Peskin MF, Hernandez B, Gabay E, Cuccaro P, Li D, Ratliff E, et al. Using Intervention Mapping for program design and production of iCHAMPSS: an online-decision support system to increase adoption, implementation, and maintenance of evidence-based sexual health programs. Front Public Health. (2017) 5:203. doi: 10.3389/fpubh.2017.00203
20. Bhargava HK, Power DJ, Sun D. Progress in web-based decision support technologies. Decis Support Syst. (2007) 43:1083–95. doi: 10.1016/j.dss.2005.07.002
22. Butterfoss D, Kegler M, Francisco V. Mobilizing organizations for health promotion: theories of organizational change. In: Glanz K, Rimer BK, Viswanath K, editors, Health Behavior and Health Education: Theory, Research and Practice, 4th edition. San Francisco, CA: Jossey-Bass (2008). p. 335–62.
23. Bandura A. Social Foundations of Thought and Action. Englewood Cliffs, NJ: Prentice Hall (1986).
24. Hernandez BF, Peskin MF, Shegog R, Gabay EK, Cuccaro PM, Addy RC, et al. iCHAMPSS: Usability and psychosocial impact for increasing implementation of sexual health education. Health Promo Pract. (2017) 18:366–80. doi: 10.1177/1524839916682004
25. Markham CM, Torres J, Craig Rushing S, Gorman G, Jessen C, Gaston A, et al. Usability and psychosocial impact of decision support to increase sexual health education in American Indian and Alaska Native communities. J Health Dispar Res Pract. (2018) 11:7.
26. Walker SC, Whitener R, Trupin EW, Migliarini N. American Indian perspectives on evidence-based practice implementation: results from a statewide tribal mental health gathering. Adm Policy Ment Health. (2015) 42:29–39. doi: 10.1007/s10488-013-0530-4
27. Fernandez ME, ten Hoor G, van Lieshout S, Ruiter RAC, Markham CM, Biedas RS, et al. Implementation Mapping: using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:158. doi: 10.3389/fpubh.2019.00158
28. Bartholomew Eldredge LK, Markham CM, Ruiter RAC, Fernández ME, Kok G, Parcel GS. Planning Health Promotion Programs: An Intervention Mapping Approach, 4th edition. San Francisco, CA: Jossey-Bass (2016).
29. Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, Stillman L, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. (2008) 41:171–81. doi: 10.1007/s10464-008-9174-z
30. Collins CB, Edwards AE, Jones PL, Kay L, Cox PJ, Puddy RW, et al. comparison of the interactive systems framework (ISF) for dissemination and implementation and the CDC division of HIV/AIDS prevention's research-to-practice model for behavioral interventions. Am J Community Psychol. (2012) 50:518–29. doi: 10.1007/s10464-012-9525-7
31. Wingood GM, DiClemente RJ. The ADAPT-ITT model: a novel method of adapting evidence-based HIV interventions. J AIDS. (2008) 47(Suppl.1):S40–6. doi: 10.1097/QAI.0b013e3181605df1
32. Hawkins JD, Catalano RF, Arthur MW, Egan E. Testing communities that care: the rationale, design and behavioral baseline equivalence of the community youth development study. Prev Sci. (2008) 9:178–90. doi: 10.1007/s11121-008-0092-y
33. McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, et al. Adapting evidence–based behavioral interventions for new settings and target populations. AIDS Educ Prev. (2006) 18(Supp.):59–73. doi: 10.1521/aeap.2006.18.supp.59
34. Wandersman A, Imm P, Chinman M, Kaftarian S. Getting to outcomes: a results-based approach to accountability. Eval Program Plann. (2000) 23:389–95. doi: 10.1016/S0149-7189(00)00028-8
35. National Association of County and City Health Officials. Model Practice Database. Available online at: http://archived.naccho.org/topics/modelpractices/search.cfm (accessed March 1, 2022).
36. Kang E, Foster ER. Use of implementation mapping with community-based participatory research: development of implementation strategies of a new goal setting and goal management intervention system. Front Public Health. (2022) 10:834473. doi: 10.3389/fpubh.2022.834473
37. Gray JS, Rose WJ. Cultural adaptation for therapy with American Indians and Alaska Natives. J Multicult Couns Devel. (2012) 40:82–92. doi: 10.1002/j.2161-1912.2012.00008.x
38. Chino M, Debruyn L. Building true capacity: indigenous models for indigenous communities. Am J Public Health. (2006) 96:596–9. doi: 10.2105/AJPH.2004.053801
39. Peters DH, Adam T, Alonge O, Agyepong IA, Tran N. Implementation research: what it is and how to do it. Br Med J. (2013) 347:bmj.f6753. https://doi.org/10.1136/bmj.f6753
40. Shegog R, Craig Rushing S, Gorman G, Jessen C, Torres J, et al. NATIVE-It's Your Game: adapting a technology-based sexual health curriculum for American Indian and Alaska Native youth. J Prim Prev. (2016) 38:27–48. doi: 10.1007/s10935-016-0440-9
41. Sacca L, Craig Rushing S, Markham CM, Shegog S, Peskin MF, Hernandez B, et al. Assessment of the reach, usability, and perceived impact of “Talking is Power”: a parental sexual health text-messaging service and web-based resource to empower sensitive conversations with American Indian and Alaska Native teens. Int J Environ Res Public Health. (2021) 18:9126. doi: 10.3390/ijerph18179126
42. Roth IJ, Tiedt MK, Barnhill JL, Karvelas KR, Faurot KR, Gaylord S, et al. Feasibility of implementation mapping for integrative medical group visits. J Altern Complement Med. (2021) 27:S71–80. doi: 10.1089/acm.2020.0393
43. Ibekwe LN, Walker TJ, Ebunlomo E, Ricks KB, Prasad S, Savas LS, et al. Using implementation mapping to develop implementation strategies for the delivery of a cancer prevention and control phone navigation program: a collaboration with 2-1-1. Health Promot Pract. (2022) 23:86–97. doi: 10.1177/1524839920957979
44. National Institutes of Health. Dissemination and Implementation Research in Health. (2016). Available online at: https://grants.nih.gov/grants/guide/pa-files/PAR-16-238.html (accessed March 1, 2022).
45. Kok G, Gottlieb NH, Commers M, Smerecnik C. The ecological approach in health promotion programs: a decade later. Am J Health Promot. (2008) 22:437–42. doi: 10.4278/ajhp.22.6.437
46. Cook CR, Lyon AR, Locke J, Waltz T, Powell BJ. Adapting a compilation of implementation strategies to advance school-based implementation research and practice. Prev Sci. (2019) 20:914–35. doi: 10.1007/s11121-019-01017-1
47. Lyon AR, Cook CR, Locke J, Davis C, Powell BJ, Waltz TJ. Importance and feasibility of an adapted set of implementation strategies in schools. J Sch Psychol. (2019) 76:66–77. doi: 10.1016/j.jsp.2019.07.014
48. Sacca L, Shegog R, Hernandez B, Peskin M, Craig Rushing S, Jessen C, et al. Barriers, frameworks, and mitigating strategies influencing the dissemination and implementation of health promotion interventions in Indigenous communities: a scoping review. Implement Sci. (2022) 17:18. doi: 10.1186/s13012-022-01190-y
49. Fernandez ME, Damschroder L, Balasubramanian B. Understanding barriers and facilitators for implementation across settings. In: Weiner BJ, Lewis CC, Sherr K, editors, Practical Implementation Science. New York, NY: Springer Publishing Company (2023). p. 97–132. doi: 10.1891/9780826186935.0005
50. NPAIHB. Adolescent Health Tribal Action Plan. Available online at: https://www.healthynativeyouth.org/wp-content/uploads/2021/03/Adolescent-Health-Tribal-Action-Plan-2020-Final.org/wp-content/uploads/2021/03/Adolescent-Health-Tribal-Action-Plan-2020-Final. (accessed March 1, 2022).
51. Alaska. Adolescent Health Tribal Action Plan. Available online at: https://www.healthynativeyouth.org/wp-content/uploads/2021/03/2020-AK-Adolescent-Health-Action-Plan-Final-10222020.pdf (accessed March 1, 2022).
52. Fishbein M, Ajzen I. Predicting and Changing Behaviour: The Reasoned Action Approach. New York, NY: Psychology Press (2010).
53. Petty R, Cacioppo JT. Communication and Persuasion: Central and Peripheral Routes to Attitude Change. New York, NY: Springer Science & Business Media (2012).
54. Cummings TG, Worley CG. Organization Development and Change. 10th ed. Mason, OH: South-Western Cengage Learning (2014).
55. Eng E, Rhodes SD, Parker E. Natural helper models to enhance a community's health and competence. In: Di Clemente RJ, Crosby RA, Kegler MC, editors, Emerging Theories in Health Promotion Practice and Research. 2nd ed. San Francisco, CA: Jossey-Bass (2009). p. 303–30.
56. Trevino N, Gaston A. Healthy Native Youth: Virtual Adaptation Guide. Portland, OR: Northwest Portland Area Indian Health Board. Available online at: https://www.healthynativeyouth.org/wp-content/uploads/2021/02/8.-Virtual-Adaptation-Guide.pdf (accessed March 1, 2022).
57. Holt-Lunstad J, Uchino B. Social support and health behavior. In:Glanz K, Rimer B, Viswanath K, editors, Health Behavior: Theory, Research and Practice. 5th ed. San Francisco, CA: Jossey-Bass (2015). p. 183–204.
58. Escobar-Chaves SL, Shegog R, Moscoso-Alvarez MR, Markham C, Tortolero-Luna G, Peskin M, et al. Cultural tailoring and feasibility assessment of a sexual health middle school curriculum: a pilot test in Puerto Rico. J Sch Health. (2011) 81:477–84. doi: 10.1111/j.1746-1561.2011.00617.x
59. Markham C, Shegog R, Leonard A, Bui T, Paul M. +CLICK: Harnessing web-based training to reduce secondary transmission among HIV-positive youth. AIDS Care. (2009) 21:622–31. doi: 10.1080/09540120802385637
60. Powell BJ, Beidas RS, Lewis CC, Aarons GA, McMillen JC, Proctor EK, et al. Methods to improve the selection and tailoring of implementation strategies. J Behav Health Serv Res. (2017) 44:177–94. doi: 10.1007/s11414-015-9475-6
61. Lewis CC, Klasnja P, Powell BJ, Lyon AR, Tuzzio L, Jones S, et al. From classification to causality: advancing understanding of mechanisms of change in implementation science. Front Public Health. (2018) 6:136. doi: 10.3389/fpubh.2018.00136
62. Schlechter CR, Del Fiol G, Lam CY, Fernandez ME, Greene T, Yack M, et al. Application of community–engaged dissemination and implementation science to improve health equity. Prev Med Rep. (2021) 24:101620. doi: 10.1016/j.pmedr.2021.101620
63. Pinto RM, Park S, Miles R, Ong PN. Community engagement in dissemination and implementation models: a narrative review. Implement Res Pract. (2021) 1:1–18. doi: 10.1177/2633489520985305
64. Kumpfer KL, Alvarado R, Smith P, Bellamy N. Cultural sensitivity and adaptation in family-based prevention interventions. Prev Sci. (2002) 3:241–6. doi: 10.1023/A:1019902902119
65. Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. (1999) 9:10–21.
66. Kreuter M, Lukwago SN, Bucholtz DC, Clark EM, Sanders-Thompson VS. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. (2003) 30:133–46. doi: 10.1177/1090198102251021
67. Santisteban DA, Muir-Malcom JA, Mitrani JB, Szapocznik J Integrating the study of ethnic culture and family psychology intervention science. In: Liddle HA, Santisteban DA, Levant RF, Bray JH, editors, Family Psychology: Science-Based Interventions. Washington, DC: American Psychological Association (2001). p. 331–51. doi: 10.1037/10438-016
Keywords: adolescent, sexual health promotion, American Indian and Alaska Native, interventions, dissemination and implementation research, Implementation Mapping
Citation: Markham CM, Rushing SC, Manthei J, Singer M, Jessen C, Gorman G, Peskin MF, Hernandez BF, Sacca L, Evans GS, Luna-Meza C, Merritt Z and Shegog R (2022) The Healthy Native Youth Implementation Toolbox: Using Implementation Mapping to adapt an online decision support system to promote culturally-relevant sexual health education for American Indian and Alaska Native youth. Front. Public Health 10:889924. doi: 10.3389/fpubh.2022.889924
Received: 04 March 2022; Accepted: 03 October 2022;
Published: 31 October 2022.
Edited by:
Byron J. Powell, Washington University in St. Louis, United StatesReviewed by:
Erica Lau, University of British Columbia, CanadaSheila Patel, RTI International, United States
Copyright © 2022 Markham, Rushing, Manthei, Singer, Jessen, Gorman, Peskin, Hernandez, Sacca, Evans, Luna-Meza, Merritt and Shegog. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christine M. Markham, Y2hyaXN0aW5lLm1hcmtoYW1AdXRoLnRtYy5lZHU=
 Christine M. Markham
Christine M. Markham Stephanie Craig Rushing
Stephanie Craig Rushing Jane Manthei2
Jane Manthei2 Michelle Singer
Michelle Singer Cornelia Jessen
Cornelia Jessen Melissa F. Peskin
Melissa F. Peskin Lea Sacca
Lea Sacca Ross Shegog
Ross Shegog