- 1School of Geography and Planning, Sun Yat-sen University, Guangzhou, China
- 2Land Consolidation and Rehabilitation Center MNR, Beijing, China
Many studies revealed a significant correlation between low-density built environment and the mental health of older adults in developed countries. However, scholars and decision-makers recently began to pay close attention to the effect of this relationship in high-density built environments and in developing countries. Using point-of-interest (POI) data from Baidu and data on 20 communities in Guangzhou, China, which were collected through a questionnaire survey, this study aimed to examine the relationship between built environment and the mental health of older adults as well as the physiological–psychological mediating paths between the two, so as to enrich the research on population aging in the high-density urban context in developing countries. The findings indicated that facility accessibility and distance to parks significantly positively correlated with the mental health of older adults and the number of public transit stations, and the distance to these stations significantly negatively correlated with the mental health of older adults. Also, the perceptions of community cohesion and community safety had a significant mediating effect between the built environment and the mental health of older adults. Furthermore, the moderating effect analysis results verified the moderating effect of income: with an increase in income, the perception of community cohesion enhanced the protection of the mental health of older adults and reduced the mediating effect of the perception of community safety. The results provided a reference for policy-makers and urban planners in their efforts to plan and build health-supporting communities and a healthy aging society.
Introduction
Population aging is one of the major challenges facing most countries worldwide (1), especially China (2). According to data from the Seventh National Population Census of China conducted in 2020, 264 million are 60 years and older, accounting for 18.7% of the national population and representing an increase of 5.44 percentage points from 2010, when the Sixth National Population Census was completed (seventh national population census). It is predicted that, by 2050, the number of older adults in China will peak at 487 million and account for 34.9% of the total population. China will face tremendous pressure brought about by a large aging population. With the rapid growth of the aging population, the Chinese government has proposed to build a society of “healthy aging,” and protecting the physical and mental health of older adults is a key component of this initiative (3). In reality, however, the mental health of older adults does not present an optimistic outlook. Mental health usually refers to a state of happiness in whichindividuals are aware that they can cope with normal stresses of everyday life, perform work effectively, and contribute to their community (4). According to the National Mental Health Development Report of China (2019-2020), nearly one third of the older adults in China have psychological disorders urgently needing interventions (5). The mental health of older adults has become a topic worthy of deep concern.
Older adults are more likely to experience health-related changes and challenges as age advances, making them potentially more sensitive and susceptible to the residential environment than other age groups (6–8). Experts and scholars from various fields, such as planning, medicine, sociology, and geography, have begun to consider the importance of the community environment with regard to the mental health of older adults (9–12). A growing body of evidence indicates that the community environment may impact the mental health of older adults (13–16). For example, a study on New York residents has indicated that people who live in a lower-quality built environment are more likely to suffer from depression (17). Therefore, building or developing built environment in communities has been gradually incorporated into more public health projects as an important measure to improve the mental health of residents (2).
However, almost all existing research or projects have been conducted in developed countries (1, 11, 17), and limited research evidence pertains to developing countries, such as China. On the one hand, developing countries are also facing the problem of aging (18). On the other hand, the built environment in developing countries is very different from that in developed countries. First, as developing countries are still in the process of urbanization, many people gather in cities for a long time, resulting in a very high population density (19). Second, compared with auto-dependent cities in the West, public transport is the main travel mode of urban residents in most developing countries such as China (20). Moreover, the distance between the daily activities of residents and destinations is still very long, although the development is extensive (21).
Therefore, research data from non-developed countries and low- and medium-income countries may reveal situations that cannot be found in developed countries and offer new insights into the mechanism driving these phenomena. Therefore, Guangzhou, a megacity in China, was chosen for a case study. This study used data collected from a questionnaire survey to investigate how the community environment affected the mental health of older adults in China. This study provided a reference for enriching related research in the context of Chinese cities and for active spatial intervention and cultivation of a healthy aging society.
Background
The built environment refers to the objective material environment built by human beings for daily living, work, and entertainment (22). It mainly includes building units (e.g., houses, schools, and workplaces), open spaces (e.g., parks, squares, and recreational venues), infrastructure (e.g., transportation systems), and public service facilities (shopping malls, stadiums, and libraries) (23). Most researches on the relationship between built environment and mental health focus on the built environment at the community level (24), that is, the level closest to residents (25) in the ecosystem theory, as the built environment at this level encompasses direct interactions with residents (26). Also, abundant literature exists on the effect of the built environment of the community on mental health. Putrik, de Vries (27) found that residents living close to the railway were exposed to a high number of stressors and reported worse mental health. Remes, Lafortune (28) explored the relationship between residential environment and major depressive disorder, and found that women living in deprived areas were more prone to anxiety, while men living in an disadvantageous environment are more likely to have depression. However, a study of young adults conducted in the UK demonstrated that greater loneliness was associated with perceptions of lower collective efficacy and greater neighborhood disorder but not with more objective measures of neighborhood characteristics (29). Studies have also shown that the mental health of older adults is particularly associated with their residential environment, and the relationship between them is still not fully understood (11). A study conducted by Maas, Spreeuwenberg (30) in the Netherlands indicated that compared with older adults living in communities with less green space, those living in areas with more green space were less likely to suffer from depression. Similarly, Zhou, Yuan (31) investigated the linkage between greenness and the well-being of older adults, and found that community greenness was positively correlated to regular social interactions among older adults and hence positively linked to their mental health. Some studies, however, questioned the positive effect of green spaces because of the risk associated with them. These studies argued that green spaces might provide a hideout for criminals, increase crime, and cause stress to nearby residents, which were detrimental to mental health (32). Some studies verified the positive impacts of residence density, street connectivity, housing, and community quality on mental health (33, 34), while others proposed that the impact was negative (35). Furthermore, some studies argued that these relationships were non-linear and that more empirical research was needed to clarify the relations (36).
The built environment may not only be directly related to people's mental state but also affect residents' perception of the environment, thus explaining mental health outcomes to a certain extent (37). The physiological–psychological path is one of the major mechanisms through which the sense of unsafety and disorder increases chronic physical stress on people, thereby damaging mental health. The perception of unsafety is also considered an important source of stress (38, 39). Perceptions of unsafety and high degrees of chaos in the surrounding environment generate feelings of helplessness and fear and directly or indirectly increase the perceptions of suffering and mental stress (40, 41). For example, the lack of public spaces in a community deters residents from interacting with others and engaging in social activities, leading to a higher degree of distrust and fear toward the community (37, 42, 43). Wang, Yuan (44) found that perception of community safety benefited residents' mental health by offering residents a favorable place to interact with their neighbors and participate in neighborhood activities. Robinette, Charles (45) found that people who perceived lower community safety had more health problems 10 years later than those perceiving more community safety. Furthermore, community cohesion is another connection between a built environment and mental health. The built environment of a community can, in some context, provide a free, relaxed space for social interactions, enhance social cohesion within a community, protect the mental health of residents, and hence ease stress. For example, a better perception of community cohesion enhances mutual trust and unity among neighbors (46) and improves mental health and well-being by promoting social and physical activities and buffering against the negative effects of stress (47–49). Therefore, the perception of community cohesion plays an important role as a buffer between a community environment and mental health, that is, it can offset some of the negative effects of an adverse community environment on mental health (e.g., depression) (12, 50). Some researchers attempted to incorporate the perceptions of community cohesion and community safety into models to investigate the relationship between built environment and mental health and found that the perceptions of community cohesion and safety might play a mediating role in the relationship between a built environment and mental health. Existing research, however, merely incorporates the two into the same model. The mediating role of the perception of community cohesion or the perception of community safety as an independent factor has not been established (24).
In addition, previous studies on built environment and the mental health of older adults have been conducted in developed countries in a low-density urban context (1, 11, 17, 51). As a developing country, China has an urban context distinct from that in Western countries, as evidenced by the high population density and high building and transportation network density in China (18, 19, 52). As one of the megacities of China, Guangzhou is representative of the high-density urban context. Its permanent population has been increasing substantially, and the population is rapidly aging (53). Therefore, the impact of the built environment in Guangzhou on older adults may differ from that seen in developed countries that have low population densities. Choosing Guangzhou for this empirical study might help guide countries with high population densities in their strategic planning for building livable cities that help improve the mental health of older adults. This case study might also help optimize public policies that focus on developing a healthy aging society.
Income is prominent, in addition to the environment, among the multiple factors that may affect the mental health of older adults (3). Irrespective of the social environment in China or in the Western countries, older adults with a lower socioeconomic status are more susceptible to the pressure brought about by the environment, and their state of mental health is usually inferior (54). For example, a study conducted by Maas, Verheij (51) in the Netherlands indicated that the relationship between green spaces and anxiety was the strongest among older adults with a lower socioeconomic status. In investigating the impact of the perception of a built environment on depression among older adults in China, Pan, Liu (3) found that monthly income had a significant moderating effect on the significant negative correlation between perceptions of the built environment and depression, in other words, the impact of the perceived built environment on depression weakened among older adults with a higher monthly income. Therefore, we hypothesized that the relationship between perceptions of the built environment (i.e., perceptions of community cohesion and community safety) and the mental health of older adults was moderated by income.
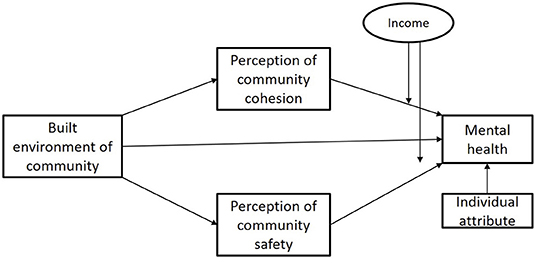
We developed a research framework (Figure 1) based on the environment stress theory to guide the investigation of how the built environment affected mental health through the perception of community cohesion and perception of community safety so as to fill the gap in existing research and enrich research on aging. More specifically, this study aimed to answer the following questions: (1) What is the relationship between a built environment and the mental health of older adults? (2) Does the perception of community cohesion or the perception of community safety have a mediating effect? Is there a difference between the impacts caused by these mediating effects? (3) Are the relationships between the perceptions of community cohesion and community safety and the mental health of older adults moderated by income level?
Data and Methods
Data
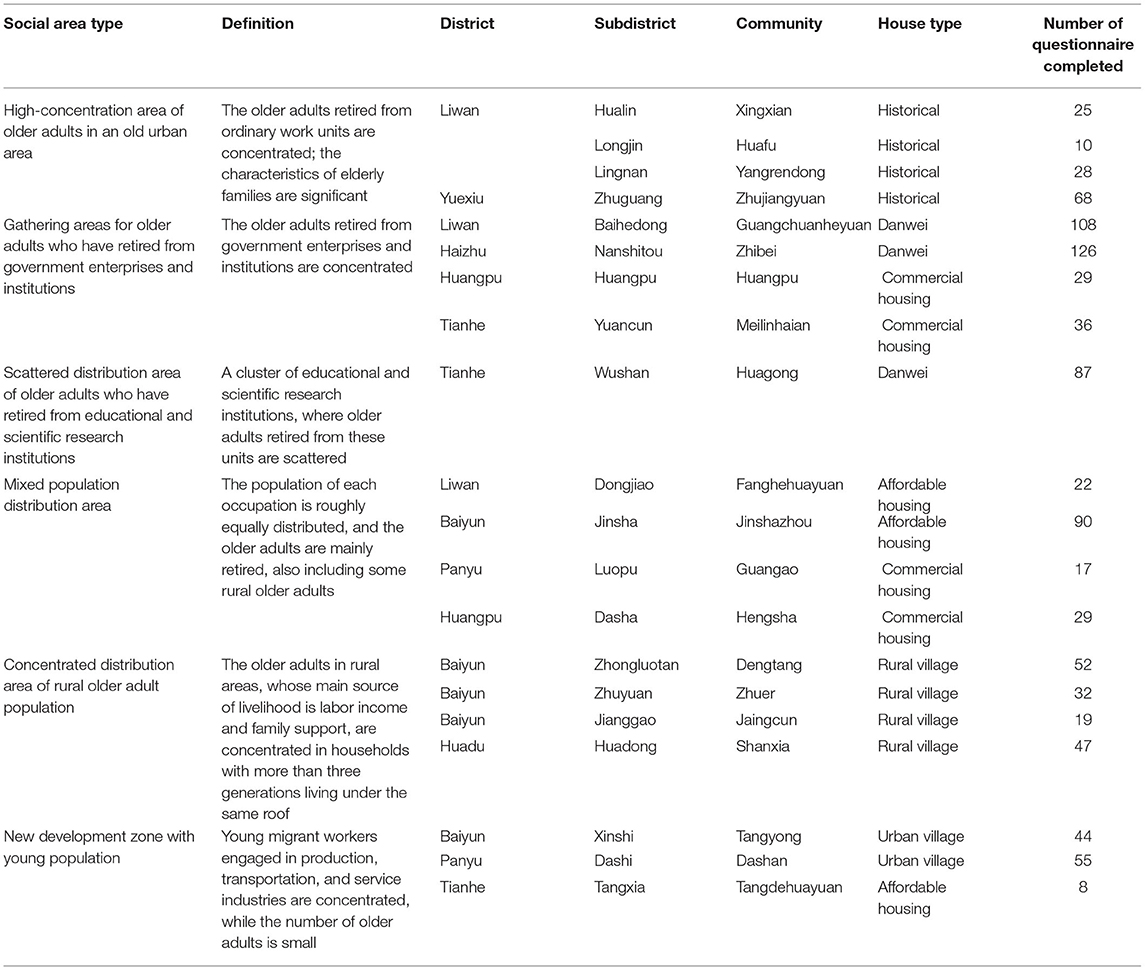
By the end of 2019, 1.7551 million people were aged 60 and above in Guangzhou, accounting for 11.47% of the total population. From December 2018 to April 2019, we conducted a questionnaire survey of older adults aged more than 60 years living in Guangzhou for more than 6 months. A multistage stratified probability proportionate to population size sampling technique (PPS), which enabled each unit to have the probability of being selected in proportion to its size (55), was adopted toselect respondents. First, Guangzhou was divided into six types of social aging areas (Table 1) on the basis of previous findings (56), including concentrated distribution areas of older adults in old neighborhoods; in government agencies, enterprises, and institutions;in urban villages; and in new development areas of a younger generation, scattered distribution areas of retired older adults in education and scientific research units, and mixed population distribution areas. Subsequently, the factor analysis was carried out on the selected 71 variables when defining six types of social aging areas. Five main factors with a cumulative variance contribution rate of 81.04% were extracted in our previous study (56). Thus, 18 subdistricts with the highest scores of five main factors among these six social aging areas were selected. Next, 20 communities with more than 10% of older adults within these 18 subdistricts were selected, covering six housing types: institutional, affordable, historic, rural self-built, commercial, and urban village housing (Table 1; Figure 2). Second, the number of questionnaire in each community was based on the proportion of older adults. The respondents from each sample community were randomly selected.
After the sample communities were determined, we submitted this survey activity and questionnaire to the Institutional Review Board of the School of Geography and Planning, Sun Yat-sen University, for review and approval. Then, we got in touch with the neighborhood committees of the sample communities. The neighborhood committees agreed to let us enter the community after being informed that all the survey data were used for academic research. Next, we conducted face-to-face interviews with each older adult for about 30 min in public places in the community. All respondents involved in this study gave their informed consent and described their feelings and thoughts in the past 4 weeks. They were asked to assess the importance of the built environment in their communities and their satisfaction with each environmental element. The respondents were also asked to evaluate statements about interpersonal relationships and safety in their communities. At the same time, they were also asked to provide some personal and demographic information about themselves and their families, such as income, housing, marital status, and other information. We finally enrolled 1000 study participants and a total of 932 valid questionnaires were completed (Table 1); the completion rate was 93.2%.
Variables
Mental Health
Mental health is defined as a state of emotional well-being. It was measured using mental health parameters in the 36-item Short-Form Health Survey (SF-36) (57). It included eight questions to assess the mental health–related feelings of respondents over the past 4 weeks: “Your mind has been in a healthy state,” “You have felt calm,” “You have felt happy,” “You have been able to concentrate on your work,” “You haven't felt stressed,” “You haven't felt nervous,” “You haven't felt dejected,” and “You haven't felt energetic” (Appendix A). Based on the Likert scale, each question had five options from 1 to 5: strongly disagree, disagree, general, agree, and strongly agree. Considering that the explained variable was basically normally distributed (58) according to previous studies (31, 58, 59), it could be regarded as a continuous variable. Therefore, the total score of mental health was obtained by adding up the scores of each question, ranging from 8 (worst health outcome) to 40 (best health outcome). Cronbach's alpha in the mental health project in this study had good internal consistency (0.923).
Built Environment
The older adults spent more time in the community after retirement and were the most affected by the built environment around the community (60). At the same time, considering the average walking speed of the older adults, the built environment of the community selected in this study was a 1-km buffer zone defined by the location of the community committee (53). In the existing studies, the measurement of the built environment was mostly based on the “5D” proposed by Ewing and Cervero (61), that is, density, diversity, design, accessibility, and distance to destination. Considering the previous findings (22, 53, 62) and the availability of data, we selected “4D” (density, diversity, accessibility, and distance to destination) from “5D” to measure the built environment of a community in this study (Table 2), which could be obtained from the seventh national population census in China and POI data from Baidu.
Mediators: Perception of Community Cohesion and Perception of Community Safety
This study explored two biopsychosocial pathways through which the built environment of the community affected the mental health of the older adults: perception of community cohesion and perception of community safety.
Perception of Community Cohesion
Following previous studies on community social cohesion (63, 64), we measured the perception of community cohesion by asking each respondent on what level they agreed with the four items that “You know a lot of people in the community,” “You have a harmonious relationship in the community,” “You belong to this community,” and “You think the cohesion of this community is very strong.” The respondents were asked to respond to these questions on the Likert scale: strongly disagree = 1; disagree = 2; generally agree = 3; agree = 4; and strongly agree = 5. We treated this variable as a continuous variable, since it was basically normally distributed. Then, we chose the Likert scoring method to calculate the score of perception of community cohesion since it contained the maximum information for the linear regression model (Cronbach's alpha was 0.714 in this study, indicating good internal consistency). The Likert scoring method is used by adding items of the same construct (59, 65). The total score of the perception of community cohesion was generated by adding four items ranging from 4 to 20. Higher scores indicated a better perception of community cohesion.
Perception of Community Safety
We measured with the following questions: “You think the community environment is quiet” and “You think the community has good public security.” Based on the Likert scale, each question had five options, scored from 1 to 5: strongly disagree, disagree, generally agree, agree, and strongly agree. It also contained the maximum information for the linear regression model (Cronbach's alpha = 0.853). The total score of the perception of community safety was generated by adding two items ranging from 2 to 10. Higher scores indicated a better perception of community safety.
Moderator: Income
Previous studies indicated that the perception of community cohesion and safety might have different effects on the mental health of older adults depending on the level of individual income (3, 66). We therefore introduced income into the model as a moderating variable and interacted income with mediating variables to assess the moderating effect of income. We divided the income into four groups by the quartile division method, with the first group (the lowest income level) as the reference group. This was mainly based on two considerations. First, the relationship between the perception of community cohesion and safety and mental health might be non-linear. Second, the income might not be normally distributed.
Individual Covariates
The regression results were adjusted for the following individual covariates: age, sex, education level, marital status, hukou type, monthly income, and living style. Hukou type refers to two types of household: local and non-local hukou, which are separated from population migration and household registration migration. Living style refers to living alone or with spouse or children.
Methods
We estimated the relationship between built environment and mental health using multilevel linear models. Multilevel models were more suitable than single-level models in this case due to the nested characteristics of the data. They can identify differences between groups (communities) or within groups (individuals) and can explain the multi-factor mechanism of health (67). Therefore, they are widely used in existing studies about residents' health (53, 58, 68). The full models were specified as follows:
where Yij represents mental health of older adults i in community j, Wj represents the built environment of community j, Mij represents the perception of community cohesion and safety of older adults i in community j, and Xij represents socioeconomic attributes of older adults i in community j, β0 is the constant, β1, β2, and β3 represent the coefficients of the variables, respectively, and μjand εij represent the random effects at the community and individual levels, respectively.
We also used mediation analysis to test the mediating effect of mediators. Following the approach of Baron and Kenny (69), we used stepwise regression to test the mediation effect with Stata12.0. First, we regressed the mental health on the built environment and covariates (model 1). Second, we regressed two mediators on the built environment and covariates (model 2a−2b). Third, we regressed mental health on the built environment, two mediators, and covariates (model 3a−3b). We used the bootstrap method to test whether the effect of the mediating variable was significant. In addition, we added the interaction term between the income level and the mediating variables to model 3a−3b to obtain the model 4a−4b and used the Wald test to test the significance of the interaction term so as to test the moderating effect of the income level.
Results
Descriptive Statistics
Table 3 demonstrates the profile of the respondents. The respondents were dominated by older adults aged 60–75 years, accounting for about 75% of all respondents. The proportion of men and women was almost equal. The older adults with a local hukou accounted for about 70%, and the proportion of older adults with elementary school and below was the highest (41.416%), followed by those with a junior high school (28.433%); the lowest percentage was those with a college degree or above (2.682%). The average income of the respondents was about 3000 RMB. The older adults living with their children accounted for about 60% of all respondents, and the older adults living alone or with their spouses accounted for about 40%. The average score for the mental health of the older adults was 31.710, and their score of perception of community cohesion and safety was 15.578 and 7.739, respectively.
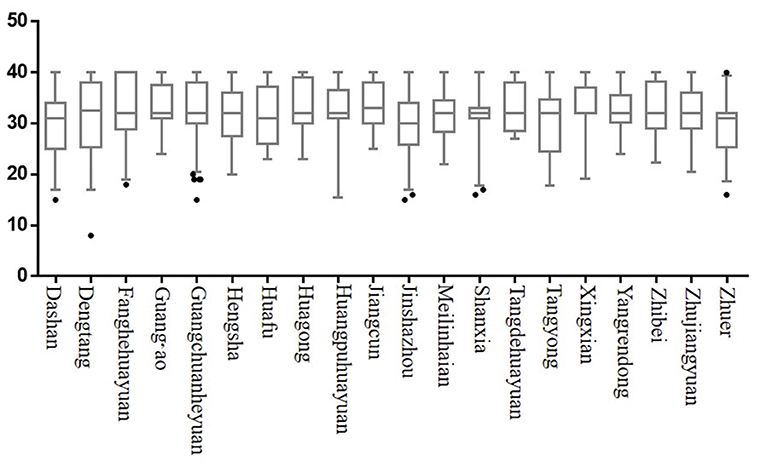
The box diagram in Figure 3 shows the spatial differences in the mental health of the older adults in 20 sample communities in this survey. In the sample distribution, the highest score on mental health appeared in Zhuer village and the lowest in Dengtang village.
Relationship Between Built Environment and Mental Health
We calculated the intra-class correlation coefficient (ICC) of the null model to determine whether multilevel models were necessary. The ICC for the null model (0.1196) indicated that the multilevel models were more suitable than the single-level models. Further, we explored the relationship between built environment and the mental health of older adults. Table 4 shows the results of the multilevel linear regression models. Model 1 was the benchmark model, which estimated the relationship between the built environment and the mental health of older adults after controlling the individual covariates. As for the built environment, facility accessibility (β = 0.005, P < 0.1) and distance to the nearest park (β = 1.389, P < 0.05) were positively correlated to the mental health of older adults. Public transit station accessibility (β = −0.086, P < 0.05) and distance to the nearest public transit station (β = −3.037, P < 0.1) were negatively correlated to the mental health of older adults. As for individual covariates, women were more likely to have better mental health than men. Those who held local hukou, higher education, and higher income were more likely to report better mental health than their counterparts.

Table 4. Relationship between built environment, perception of community cohesion, perception of community safety, and mental health.
Mediating Effect of Perception of Community Cohesion and Safety
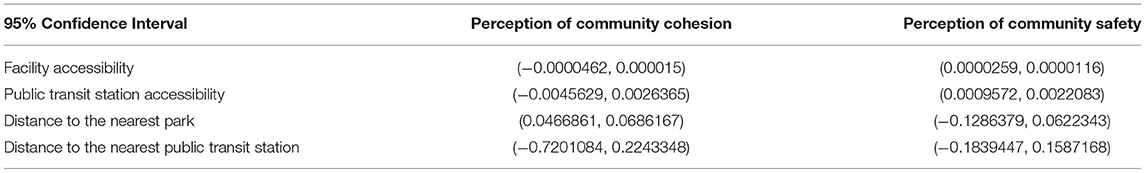
Model 2a−2b estimated the relationship between the built environment and two mediators (perception of community cohesion and perception of community safety).
As shown in Table 4, in model 2a, distance to the nearest park (β = 0.568, P < 0.05) was positively correlated to the perception of community cohesion. Distance to the nearest public transit station (β = −2.712, P < 0.05) was negatively correlated to the perception of community cohesion. Women (β = 0.515, P < 0.05), with local hukou (β = 1.195, P < 0.01) and more income (β = 0.394, P < 0.01), were more likely to perceive community cohesion. In model 2b, mixed land use (β = 4.727, P < 0.01), facility accessibility (β = 0.0003, P < 0.01), and distance to the nearest park (β = 0.617, P < 0.05) were positively correlated to perception of community safety. Park accessibility (β = −0.043, P < 0.05), public transit station accessibility (β = −0.408, P < 0.01), and distance to the nearest public transit station (β = −0.888, P < 0.1) were negatively correlated to perception of community safety. Those having higher income (β = 0.021, P < 0.1) perceived their community as safer. The older adults with high school or technical secondary school education perceived their community less safe.
Relationship Between the Built Environment, Mediators, and Mental Health
Model 3a-3b estimated the relationship between the built environment and the mental health of older adults while taking into account two mediators: perception of community cohesion and safety (Table 5).
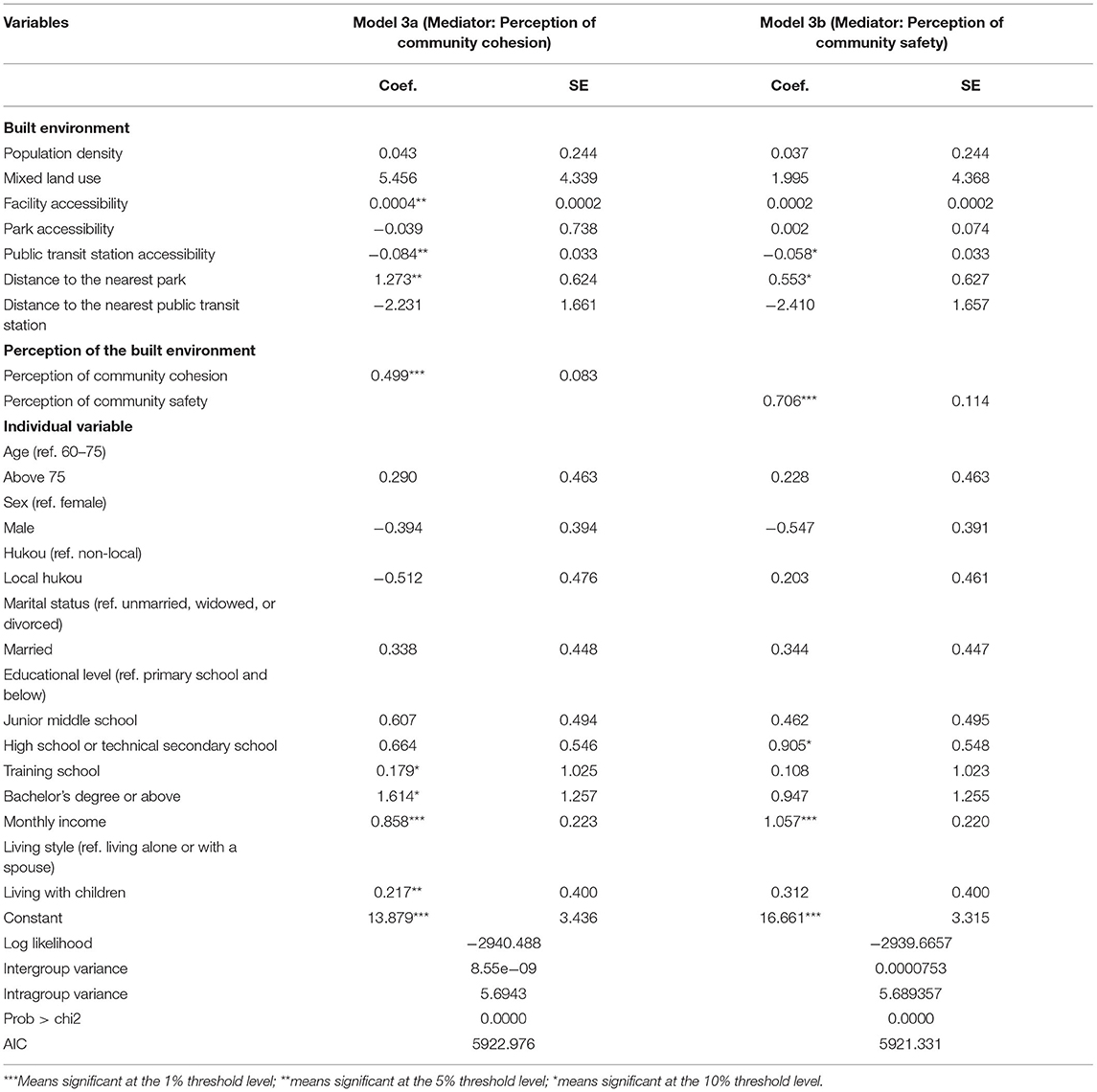
Table 5. Mediation effect of two mediators: perception of community cohesion and perception of community safety.
In model 3a, facility accessibility (β = 0.0004, P < 0.05) and distance to the nearest park (β = 1.273, P < 0.05) positively correlated with mental health. Public transit station accessibility (β = −0.084, P < 0.05) negatively correlated with mental health. Perception of community cohesion (β = 0.499, P < 0.01) positively correlated with the mental health of older adults. The older adults who were highly educated (β = 0.179, P < 0.1; β = 1.614, P < 0.1) and richer (β = 0.858, P < 0.01) reported a higher level of mental health. Those who lived with their children (β = 0.217, P < 0.1) also reported better conditions of mental health.
In model 3b, public transit station accessibility (β = −0.058, P < 0.1) was negatively correlated to mental health, while distance to the nearest park (β = 0.553, P < 0.1) was positively correlated to mental health. Perception of community safety (β = 0.706, P < 0.01) was positively correlated to mental health. The older adults who were well educated (β = 0.905, P < 0.1) and had higher income (β = 1.057, P < 0.01) were more likely to report a high level of mental health. We estimated the mediation effect of the two mediators separately using the bootstrap method (Table 6), revealing that each of the two mediators played a mediating role.
Moderating Effect of the Income Level
We added the interaction items of two mediators (perception of community cohesion and safety) and moderator (income) to the model 4a–4b (Table 7) to test whether the income level had a moderating effect on the relationship between the perception of community cohesion and safety and the mental health of older adults. The Wald test was used to test the significance of interaction terms. The results showed that the relationship between the perception of community cohesion and safety and the mental health of older adults varied with the income level. The Wald test indicated that all the interaction terms in the model 4a−4b passed the significance test.
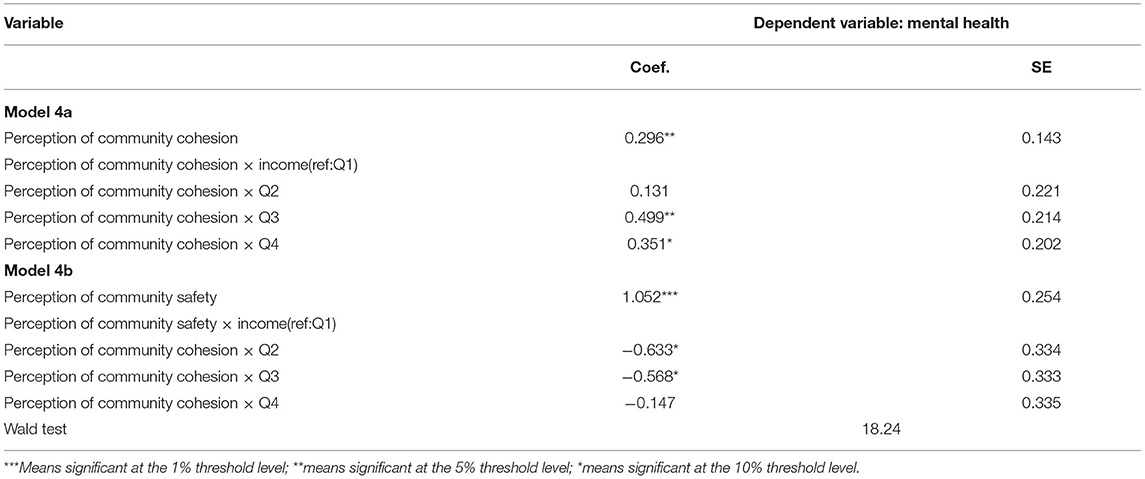
Table 7. Relationship between the perception of community cohesion and safety and mental health: the moderating effect of income.
In model 4a, compared with the first group (lowest income level), the coefficient of the interaction of the third and fourth groups of income and the perception of community cohesion was significant. That is, only when it was higher than the average income level, the income level could moderate the relationship between the perception of community cohesion and mental health. The moderating effect was the strongest at the medium and high income levels.
In model 4b, compared with the first group (lowest income level), the coefficient of the interaction of the second and third groups of income and the perception of community safety was significant. That is, only when it was higher than the average income level, the income level could moderate the relationship between the perception of community safety and mental health. The moderating effect was the strongest at the average income level. In addition, with the increase in income, the moderating effect gradually weakened to an insignificant level.
Discussion
Consistent with previous research findings from developed countries, our study also indicated a significant correlation between the built environment and the mental health of older adults in China (11, 70, 71). The research findings also suggested that both the perception of community cohesion and the perception of community safety had a significant mediating effect between the built environment and the mental health of older adults.
The research results indicated that facility accessibility and distance to parks significantly positively correlated with the mental health of older adults, which was consistent with the findings in the previous literature. With continued urbanization in China, the public facilities gradually improve with the increase in the size of cities. The high degree of facility accessibility around communities increases residents' proximity to recreational venues and public spaces and enhances the frequency of social interactions for older adults (72), which is conducive to improving their state of mental health (73). Distance to parks is an indicator of opportunities for older adults to enjoy green spaces. As important green spaces and public spaces, parks and squares have been shown to improve mental health (31, 74, 75). Parks and squares are important venues for social interactions in everyday life, which act as critical links to help residents maintain interpersonal relations and improve community cohesion, and therefore are conducive to improving the mental health of residents (76–78). The number of public transit stations and the distance to the stations significantly negatively correlated with the mental health of older adults, which was different from the results for developed countries. In megacities such as Guangzhou, the public transportation network shows continuous improvement with the increase in population density. However, if surrounded by too many public transit stations, communities may suffer from noise and exhaust pollution (79), decreasing the willingness of older adults to engage in social interactions, which is not conducive to improving their mental health (80–82). Long-term exposure to exhaust pollution is also detrimental to physical and mental health. Older adults are especially vulnerable to air pollution-related diseases (83–85) as well as depression and anxiety related to air pollution (86).
Our study verified the paths through which the perception of community cohesion and community safety mediated the relationship between the built environment and the mental health of older adults. In other words, creating a built environment that provides residents with opportunities to perceive a harmonious and safe community environment is an important path through which a built environment affects the mental health of residents. The perception of community cohesion has a partial mediating effect between the shortest distance to parks and mental health and many studies have revealed the potential reasons for this effect. For example, older adults are more likely to engage in social interactions in parks. These public spaces help them develop an emotional network among neighbors, ease their negative emotions, and enhance their positive mental state (87, 88). Also, older adults can obtain social support, reinforcing their attachment to the community and sense of belonging in these public spaces. As such, they have a stronger perception of community cohesion and maintain a positive emotional and mental state (58, 77). Interestingly, our research findings suggested that perceived community safety had a mediating effect between the built environment and mental health, which was not reported in previous empirical research in China (37). The relationships between accessibility to facilities, the number of public transit stations and mental health are mediated by the perception of community safety. A higher degree of accessibility to facilities improves the orderliness of areas surrounding a community and makes it more discernable and interesting. It helps keep “more eyes on the streets,” enhances residents' sense of community safety, and eases residents' psychological burden (89). In contrast, when the density of public transit stations exceeds a threshold, a crowding effect occurs (90). A high density of public transit stations and the resulting high population mobility create a noisy and unsafe community atmosphere. To a certain extent, as indicated by the broken windows theory, built environment that lacks order and social control creates distrust and fear among nearby residents (91) and creates pressure and mental stress on residents. This finding is different from the research conclusions for developed countries. The main reason for the difference is that urban residents, including older adults, regardless of their socioeconomic status, in China are likely to live in noisier and more crowded urban areas than residents in developed countries. Given this difference, a high density of public transit stations is not conducive to improving mental health (3).
We also identified the moderating effect of income. The enhancing effect of the perception of community cohesion on mental health was the strongest for older adults who had medium to high levels of income. Older adults with higher levels of income had more options with regard to adjusting their mental state (e.g., travel or recreational activity), reducing the chances of suffering from mental health problems (92, 93). The moderating effect of income was weaker for older adults with lower levels of income because these people, with economic and information accessibility limitations, tended to neglect mental health problems and were more likely to lack the resources needed to cope with these issues (94, 95). With an increase in income, the mediating effect of the perception of community safety that helped improve mental health decreased. Many research findings from developed countries also identified the mechanism underlying this phenomenon: people with a lower socioeconomic status suffered from the inferior built environment (crowdedness and noise) and were more likely to be subject to environmental stress, leading to a worse mental state (66).
This study had the following limitations. First, it was based on an analysis of cross-sectional data, making it difficult to draw a causal relationship between a built environment and the mental health of older adults. Second, the two mediating variables in this study (perception of community cohesion and perception of community safety) were indicators self-reported by the older adults. Hence, more objective measurements should be incorporated in future research. Third, although this study controlled for the socioeconomic characteristics of individuals and families to minimize the impact of self-selection, further experiments are needed to clarify the relationship between a built environment and mental health. Moreover, the research location selected for this case study was Guangzhou, one of the megacities of China. The research results need to be further verified for applicability to small- and medium-sized cities. Finally, the rapid and drastic changes in the built environment of Guangzhou have occurred under the stimulus of rapid urbanization and government policies. At the same time, in Chinese culture and consciousness, the adults still bear important responsibilities in the family. Therefore, considering the particularity of the development environment, government policies, history and culture, and the limited sample size of this study, the research conclusions cannot be extrapolated to other countries to a certain extent.
Conclusions
This study employed a multilevel model and mediating effect analysis to examine the relationship between built environment and the mental health of older adults, as well as the mediating paths between the two. The results indicated a significant relationship between the built environment and the mental health of older adults. Also, the perception of community cohesion and community safety played a mediating role in this relationship. Furthermore, the results from the moderating effect analysis indicated that income moderated the relationship between the perceptions of community cohesion and safety and the mental health of older adults. The research results demonstrated that the built environment of a community played an important role in improving the mental health of older adults in China. We recommend that when governments develop public policies and when planners conduct urban planning, they should fully evaluate and balance the positive and negative effects brought about by infrastructure construction in dense cities. They should also make every effort to adapt to older adults' attachment to spaces and meet their need for social support so as to maximize the positive effect of the built environment on the mental health of older adults and hence effectively cultivate a healthy aging society. In addition, different from a high-density urban environment, a rural environment has the characteristics of low population density, road network, and infrastructure layout. Empirical research should be conducted in the future to compare the differences in the effects of the urban and rural environments on the health of older adults so as to propose strategies for constructing differentiated urban and rural health environment and provide a reference for the policy planning of relevant departments.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions. The datasets presented in this article are not readily available because of institutional copyright issues. Requests to access the datasets should be directed to CZ,emhvdWNzQG1haWwuc3lzdS5lZHUuY24=.
Author Contributions
RZ and CZ developed the main ideas of the study, gathered the data, performed the model construction and estimation, and wrote the manuscript. XH and YL helped to collect and process data. ML participated in revising the manuscript and proofreading the article. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Social Science Foundation of China (17BRK010).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.881169/full#supplementary-material
References
1. Parra DC, Gomez LF, Sarmiento OL, Buchner D, Brownson R, Schimd T, et al. Perceived and objective neighborhood environment attributes and health related quality of life among the elderly in Bogota, Colombia. Soc Sci Med. (2010) 70:1070–6. doi: 10.1016/j.socscimed.2009.12.024
2. Li C, Zhou Y. Residential environment and depressive symptoms among chinese middle- and old-aged adults: a longitudinal population-based study. Health Place. (2020) 66:102463. doi: 10.1016/j.healthplace.2020.102463
3. Pan H, Liu Y, Chen Y. The health effect of perceived built environment on depression of elderly people in rural China: moderation by income. Health Soc Care Community. (2021) 29:185–93. doi: 10.1111/hsc.13081
4. Organization WH. Mental Health Action Plan 2013–2020. Switzerland: World Health Organization Press (2014). p. 5.
5. Fu X, Zhang K, Chen X, Chen Z. China's National Mental Health Development Report (2019-2020). Beijing: Social Sciences Academic Press (2021).
6. Dendup T, Astell-Burt T, Feng X. Residential self-selection, perceived built environment and type 2 diabetes incidence: a longitudinal analysis of 36,224 middle to older age adults. Health Place. (2019) 58:102154. doi: 10.1016/j.healthplace.2019.102154
7. Hu H, Cao Q, Shi Z, Lin W, Jiang H, Hou Y. Social support and depressive symptom disparity between urban and rural older adults in China. J Affect Disord. (2018) 237:104–11. doi: 10.1016/j.jad.2018.04.076
8. Firdaus G. Built environment and health outcomes: identification of contextual risk factors for mental well-being of older adults. Ageing Int. (2016) 42:62–77. doi: 10.1007/s12126-016-9276-0
9. Salvatore MA, Grundy E. area deprivation, perceived neighbourhood cohesion and mental health at older ages: a cross lagged analysis of uk longitudinal data. Health Place. (2021) 67:102470. doi: 10.1016/j.healthplace.2020.102470
10. Ram B, Shankar A, Nightingale CM, Giles-Corti B, Ellaway A, Cooper AR, et al. Comparisons of depression, anxiety, well-being, and perceptions of the built environment amongst adults seeking social, intermediate and market-rent accommodation in the Former London olympic athletes' village. Health Place. (2017) 48:31–9. doi: 10.1016/j.healthplace.2017.09.001
11. Domenech-Abella J, Mundo J, Leonardi M, Chatterji S, Tobiasz-Adamczyk B, Koskinen S, et al. Loneliness and depression among older European adults: the role of perceived neighborhood built environment. Health Place. (2020) 62:102280. doi: 10.1016/j.healthplace.2019.102280
12. Mair C, Diez Roux AV, Morenoff JD. Neighborhood stressors and social support as predictors of depressive symptoms in the chicago community adult health study. Health Place. (2010) 16:811–9. doi: 10.1016/j.healthplace.2010.04.006
13. Wee LE, Tsang YYT, Tay SM, Cheah A, Puhaindran M, Yee J, et al. Perceived neighborhood environment and its association with health screening and exercise participation amongst low-income public rental flat residents in Singapore. Int J Environ Res Public Health. (2019) 16:1384. doi: 10.3390/ijerph16081384
14. van den Berg P, Kemperman A, de Kleijn B, Borgers A. Ageing and loneliness: the role of mobility and the built environment. Travel Behaviour and Society. (2016) 5:48–55. doi: 10.1016/j.tbs.2015.03.001
15. Haseda M, Kondo N, Ashida T, Tani Y, Takagi D, Kondo K. Community social capital, built environment, and income-based inequality in depressive symptoms among older people in Japan: an ecological study from the jages project. Journal of Epidemiology. (2018) 28:108–16. doi: 10.2188/jea.JE20160216
16. Howden-Chapman PL, Chandola T, Stafford M, Marmot M. The effect of housing on the mental health of older people: the impact of lifetime housing history in Whitehall Ii. BMC Public Health. (2011) 11:682. doi: 10.1186/1471-2458-11-682
17. Galea S, Ahern J, Rudenstine S, Wallace Z, Vlahov D. Urban built environment and depression: a multilevel analysis. J Epidemiol Community Health. (2005) 59:822–7. doi: 10.1136/jech.2005.033084
18. Sun B, Yin C. Relationship between multi-scale urban built environments and body mass index: a study of China. Appl Geograp. (2018) 94:230–40. doi: 10.1016/j.apgeog.2018.03.012
19. Kenworthy J, Hu G. Transport and urban form in Chinese Cities:an international comparative and policy perspective with implications for sustainable urban transport in China. Disp - the Planning Review. (2002) 38:4–14. doi: 10.1080/02513625.2002.10556818
20. Gao Y, Kenworthy J. The Urban Transport Crisis in Emerging Economies. Cham: Springer. (2017). p. 33–58.
21. Kelly-Schwartz AC, Stockard J, Doyle S, Schlossberg M. Is sprawl unhealthy? J Planning Edu Res. (2016) 24:184–96. doi: 10.1177/0739456X04267713
22. Saelens BE, Handy SL. Built environment correlates of walking: a review. Med Sci Sports Exerc. (2008) 40(Suppl. 7):S550–66. doi: 10.1249/MSS.0b013e31817c67a4
23. Bonaccorsi G, Manzi F, Del Riccio M, Setola N, Naldi E, Milani C, et al. Impact of the built environment and the neighborhood in promoting the physical activity and the healthy aging in older people: an umbrella review. Int J Environ Res Public Health. (2020) 17:6127. doi: 10.3390/ijerph17176127
24. Guo Y, Liu Y, Lu S, Chan OF, Chui CHK, Lum TYS. Objective and perceived built environment, sense of community, and mental wellbeing in older adults in Hong Kong: a multilevel structural equation study. Landscape Urban Planning. (2021) 209:104058–70. doi: 10.1016/j.landurbplan.2021.104058
25. Hess AL. Review of the ecology of human development: experiments by nature and design, urie brofenbrenner. J Mind Behav. (1981) 2:365–9. doi: 10.1080/00131728109336000
26. Guo Y, Chan CH, Yip PSF. Spatial variation in accessibility of libraries in Hong Kong. Libr Inf Sci Res. (2017) 39:319–29. doi: 10.1016/j.lisr.2017.11.007
27. Putrik P, de Vries NK, Mujakovic S, van Amelsvoort L, Kant I, Kunst AE, et al. Living environment matters: relationships between neighborhood characteristics and health of the residents in a Dutch municipality. J Community Health. (2015) 40:47–56. doi: 10.1007/s10900-014-9894-y
28. Remes O, Lafortune L, Wainwright N, Surtees P, Khaw KT, Brayne C. Association between area deprivation and major depressive disorder in british men and women: a cohort study. BMJ Open. (2019) 9:e027530. doi: 10.1136/bmjopen-2018-027530
29. Matthews T, Odgers CL, Danese A, Fisher HL, Newbury JB, Caspi A, et al. Loneliness and neighborhood characteristics: a multi-informant, nationally representative study of young adults. Psychol Sci. (2019) 30:765–75. doi: 10.1177/0956797619836102
30. Maas J, Spreeuwenberg P, van Winsum-Westra M, Verheij RA, Vries S, Groenewegen PP. Is green space in the living environment associated with people's feelings of social safety? Environ Planning A: Economy Space. (2009) 41:1763–77. doi: 10.1068/a4196
31. Zhou Y, Yuan Y, Chen Y, Lai S. Association pathways between neighborhood greenspaces and the physical and mental health of older adults-a cross-sectional study in Guangzhou, China. Front Public Health. (2020) 8:551453. doi: 10.3389/fpubh.2020.551453
32. Herzog TR, Flynn-Smith JA. Preference and perceived danger as a function of the perceived curvature, length, and width of urban Alleys. Environ Behav. (2001) 33:653–66. doi: 10.1177/00139160121973179
33. Guo Y, Chang SS, Chan CH, Chang Q, Hsu CY, Yip PSF. Association of Neighbourhood social and physical attributes with depression in older adults in Hong Kong: a multilevel analysis. J Epidemiol Community Health. (2020) 74:120–9. doi: 10.1136/jech-2019-212977
34. Liu Y, Dijst M, Faber J, Geertman S, Cui C. Healthy urban living: residential environment and health of older adults in Shanghai. Health Place. (2017) 47:80–9. doi: 10.1016/j.healthplace.2017.07.007
35. Van Dyck D, Cardon G, Deforche B, De Bourdeaudhuij I. Do adults like living in high-walkable neighborhoods? associations of walkability parameters with neighborhood satisfaction and possible mediators. Health Place. (2011) 17:971–7. doi: 10.1016/j.healthplace.2011.04.001
36. Jiang B, Chang C-Y, Sullivan WC. A Dose of nature: tree cover, stress reduction, and gender differences. Landsc Urban Plan. (2014) 132:26–36. doi: 10.1016/j.landurbplan.2014.08.005
37. Tao Y, Yang J, Chai Y. The anatomy of health-supportive neighborhoods: a multilevel analysis of built environment, perceived disorder, social interaction and mental health in Beijing. Int J Environ Res Public Health. (2019) 17:13. doi: 10.3390/ijerph17010013
38. Jenkins R, Meltzer H, Jones P, Brugha T, Bebbington P, Farrell M, et al. Mental health: future challenges. London: The Government Office for Science (2008) 09/01. Report No.
39. Lorenc T, Clayton S, Neary D, Whitehead M, Petticrew M, Thomson H, et al. Crime, fear of crime, environment, and mental health and wellbeing: mapping review of theories and causal pathways. Health Place. (2012) 18:757–65. doi: 10.1016/j.healthplace.2012.04.001
40. De Donder L, Buffel T, Dury S, De Witte N, VertÉ D. Perceptual quality of neighbourhood design and feelings of unsafety. Ageing Soc. (2013) 33:917–37. doi: 10.1017/S0144686X12000207
41. Booth J, Ayers S, Marsiglia F. Perceived neighborhood safety and psychological distress: exploring protective factors. J Sociology Social Welfare. (2014) 39:137–56.
42. Whitley R, Prince M. Fear of crime, mobility and mental health in inner-city London, Uk. Soc Sci Med. (2005) 61:1678–88. doi: 10.1016/j.socscimed.2005.03.044
43. Villanueva K, Badland H, Hooper P, Koohsari MJ, Mavoa S, Davern M, et al. Developing indicators of public open space to promote health and wellbeing in communities. Appl Geograp. (2015) 57:112–9. doi: 10.1016/j.apgeog.2014.12.003
44. Wang R, Yuan Y, Liu Y, Zhang J, Liu P, Lu Y, et al. Using street view data and machine learning to assess how perception of neighborhood safety influences urban residents' mental health. Health Place. (2019) 59:102186. doi: 10.1016/j.healthplace.2019.102186
45. Robinette JW, Charles ST, Gruenewald TL. Vigilance at home: longitudinal analyses of neighborhood safety perceptions and health. SSM Popul Health. (2016) 2:525–30. doi: 10.1016/j.ssmph.2016.06.004
46. Lee YJ, Braun KL, Wu YY, Hong S, Gonzales E, Wang Y, et al. Neighborhood social cohesion and the health of native Hawaiian and other Pacific Islander older adults. J Gerontol Soc Work. (2022) 65:3–23. doi: 10.1080/01634372.2021.1917033
47. Singh GK, Ghandour RM. Impact of neighborhood social conditions and household socioeconomic status on behavioral problems among Us children. Matern Child Health J. (2012) 16:158–69. doi: 10.1007/s10995-012-1005-z
48. Cramm JM, Nieboer AP. Social cohesion and belonging predict the well-being of community-dwelling older people. BMC Geriatr. (2015) 21:30. doi: 10.1186/s12877-015-0027-y
49. Cain CL, Wallace SP, Ponce NA. Helpfulness, trust, and safety of neighborhoods: social capital, household income, and self-reported health of older adults. Gerontologist. (2018) 58:4–14. doi: 10.1093/geront/gnx145
50. Ruijsbroek A, Droomers M, Hardyns W, Groenewegen PP, Stronks K. The Interplay between neighbourhood characteristics: the health impact of changes in social cohesion, disorder and unsafety feelings. Health Place. (2016) 39:1–8. doi: 10.1016/j.healthplace.2016.02.001
51. Maas J, Verheij RA, de Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP. Morbidity is related to a green living environment. J Epidemiol Community Health. (2009) 63:967–73. doi: 10.1136/jech.2008.079038
52. Sun B, Yan H, Zhang T. Built environmental impacts on individual mode choice and bmi: evidence from China. J Transport Geography. (2017) 63:11–21. doi: 10.1016/j.jtrangeo.2017.07.004
53. Zhang R, Liu S, Li M, He X, Zhou C. The effect of high-density built environments on elderly individuals' physical health: a cross-sectional study in Guangzhou, China. Int J Environ Res Public Health. (2021) 18:10250. doi: 10.3390/ijerph181910250
54. Mohai P, Bryant B. Is there a “race” effect on concern for environmental quality? Public Opin Q. (1998) 62:475–505. doi: 10.1086/297858
55. Latpate R, Kshirsagar J, Kumar Gupta V, Chandra G. Probability Proportional to Size Sampling. In: Latpate R, Kshirsagar J, Kumar Gupta V, Chandra G, editors. Advanced Sampling Methods. Singapore: Springer Singapore (2021). p. 85–98. doi: 10.1007/978-981-16-0622-9_7
56. Zhou C, Tong X, Wang J, LAI S. Spatial differentiation and the formation mechanism of population aging in Guangzhou in 2000- 2010. Geographical Res. (2018) 37:103–18. doi: 10.11821/dlxb201612002
57. Ware JE. Jr., Sherbourne CD. The mos 36-item short-form health survey (sf-36) i conceptual framework and item selection. Med Care. (1992) 30:473–83. doi: 10.1097/00005650-199206000-00002
58. Liu Y, Wang R, Xiao Y, Huang B, Chen H, Li Z. Exploring the linkage between greenness exposure and depression among Chinese people: mediating roles of physical activity, stress and social cohesion and moderating role of urbanicity. Health Place. (2019) 58:102168. doi: 10.1016/j.healthplace.2019.102168
59. Zhang L, Zhou S, Kwan MP. A Comparative analysis of the impacts of objective versus subjective neighborhood environment on physical, mental, and social health. Health Place. (2019) 59:102170. doi: 10.1016/j.healthplace.2019.102170
60. Robert S. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. (2003) 25:489–516. doi: 10.1146/annurev.soc.25.1.489
61. Ewing R, Cervero R. Travel and the built environment. J Am Planning Association. (2010) 76:265–94. doi: 10.1080/01944361003766766
62. Pearson AL, Bentham G, Day P, Kingham S. Associations between neighbourhood environmental characteristics and obesity and related behaviours among adult New Zealanders. BMC Public Health. (2014) 14:553. doi: 10.1186/1471-2458-14-553
63. Forrest R, Kearns A. Social cohesion, social capital and the neighbourhood. Urban Stud. (2001) 38:2125–43. doi: 10.1080/00420980120087081
64. Ehsan A, Klaas HS, Bastianen A, Spini D. Social capital and health: a systematic review of systematic reviews. SSM Popul Health. (2019) 8:100425-. doi: 10.1016/j.ssmph.2019.100425
65. Wang R, Liu Y, Lu Y, Zhang J, Liu P, Yao Y, et al. Perceptions of built environment and health outcomes for older chinese in beijing: a big data approach with street view images and deep learning technique. Computers, Environ Urban Systems. (2019) 78:101386–96. doi: 10.1016/j.compenvurbsys.2019.101386
66. Downey L, Van Willigen M. Environmental stressors: the mental health impacts of living near industrial activity. J Health Soc Behav. (2005) 46:289–305. doi: 10.1177/002214650504600306
67. Duncan C, Jones K, Moon G. Context, composition and heterogeneity: using multilevel models in health research. Soc Sci Med. (1998) 46:97–117. doi: 10.1016/S0277-9536(97)00148-2
68. Chen Y, Yuan Y. The neighborhood effect of exposure to blue space on elderly individuals' mental health: a case study in Guangzhou, China. Health Place. (2020) 63:102348. doi: 10.1016/j.healthplace.2020.102348
69. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
70. Andreucci MB, Russo A, Olszewska-Guizzo A. Designing urban green blue infrastructure for mental health and elderly wellbeing. Sustainability. (2019) 11:6425–39. doi: 10.3390/su11226425
71. Beemer CJ, Stearns-Yoder KA, Schuldt SJ, Kinney KA, Lowry CA, Postolache TT, et al. A brief review on the mental health for select elements of the built environment. Indoor Built Environ. (2019) 30:152–65. doi: 10.1177/1420326X19889653
72. Hirsch JA, Diez Roux AV, Rodriguez DA, Brines SJ. Moore KA. Discrete land uses and transportation walking in two us cities: the multi-ethnic study of atherosclerosis. Health Place. (2013) 24:196–202. doi: 10.1016/j.healthplace.2013.09.007
73. Qiu Y, Liu Y, Liu Y, Li Z. Exploring the linkage between the neighborhood environment and mental health in Guangzhou, China. Int J Environ Res Public Health. (2019) 16:3206. doi: 10.3390/ijerph16173206
74. Ettema D, Schekkerman M. How Do spatial characteristics influence well-being and mental health? comparing the effect of objective and subjective characteristics at different spatial scales. Travel Behav Soc. (2016) 5:56–67. doi: 10.1016/j.tbs.2015.11.001
75. Dong H, Qin B. Exploring the Link between neighborhood environment and mental wellbeing: a case study in Beijing, China. Landsc Urban Plan. (2017) 164:71–80. doi: 10.1016/j.landurbplan.2017.04.005
76. Evans GW. The built environment and mental health. J Urban Health. (2003) 80:536–55. doi: 10.1093/jurban/jtg063
77. Liu Y, Wang R, Grekousis G, Liu Y, Yuan Y, Li Z. Neighbourhood greenness and mental wellbeing in guangzhou, china: what are the pathways? Landscape Urban Planning. (2019) 190:103602–11. doi: 10.1016/j.landurbplan.2019.103602
78. de Vries S, van Dillen SM, Groenewegen PP, Spreeuwenberg P. Streetscape greenery and health: stress, social cohesion and physical activity as mediators. Soc Sci Med. (2013) 94:26–33.
79. Lin J, Sun B. Impact of built environment on urban residents' subjective well-being:evidence from the China labor-force dynamics survey. Urban Develop Stud. (2017) 24:69–75. doi: 10.3969/j.issn.1006-3862.2017.12.010
80. Coan JA, Sbarra DA. Social baseline theory: the social regulation of risk and effort. Current Opinion Psychol. (2015) 1:87–91. doi: 10.1016/j.copsyc.2014.12.021
81. Holt-Lunstad J. Why social relationships are important for physical health: a systems approach to understanding and modifying risk and protection. Annu Rev Psychol. (2018) 69:437–58. doi: 10.1146/annurev-psych-122216-011902
82. Leyden KM. Social capital and the built environment: the importance of walkable neighborhoods. Am J Public Health. (2003) 93:1546–51. doi: 10.2105/AJPH.93.9.1546
83. Wang C, Tu Y, Yu Z, Lu R. Pm2.5 and cardiovascular diseases in the elderly: an overview. Int J Environ Res Public Health. (2015) 12:8187–97. doi: 10.3390/ijerph120708187
84. Brook RD, Rajagopalan S, Pope CA. 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. (2010) 121:2331–78. doi: 10.1161/CIR.0b013e3181dbece1
85. Sacks JD, Stanek LW, Luben TJ, Johns DO, Buckley BJ, Brown JS, et al. Particulate matter-induced health effects: who is susceptible? Environ Health Perspect. (2011) 119:446–54. doi: 10.1289/ehp.1002255
86. Pun VC, Manjourides J, Suh H. Association of ambient air pollution with depressive and anxiety symptoms in older adults: results from the Nshap study. Environ Health Perspect. (2017) 125:342–8. doi: 10.1289/EHP494
87. Gascon M, Triguero-Mas M, Martinez D, Dadvand P, Rojas-Rueda D, Plasencia A, et al. residential green spaces and mortality: a systematic review. Environ Int. (2016) 86:60–7.
88. Shanahan DF, Bush R, Gaston KJ, Lin BB, Dean J, Barber E, et al. Health benefits from nature experiences depend on dose. Sci Rep. (2016) 6:28551. doi: 10.1038/srep28551
90. Brown S, Lombard J. Neighborhoods and Social Interaction. New York, NY: John Wiley & Sons, Ltd (2014). p. 91–118.
91. Wood L, Shannon T, Bulsara M, Pikora T, McCormack G, Giles-Corti B. The anatomy of the safe and social suburb: an exploratory study of the built environment, social capital and residents' perceptions of safety. Health Place. (2008) 14:15–31. doi: 10.1016/j.healthplace.2007.04.004
92. Manaugh K, El-Geneidy A. Validating walkability indices: how do different households respond to the walkability of their neighborhood? Trans Res Part D: Trans Environ. (2011) 16:309–15. doi: 10.1016/j.trd.2011.01.009
93. Wu ZJ, Song Y, Wang HL, Zhang F, Li FH, Wang ZY. Influence of the built environment of nanjing's urban community on the leisure physical activity of the elderly: an empirical study. BMC Public Health. (2019) 19:1459. doi: 10.1186/s12889-019-7643-y
94. Wang R, Xue D, Liu Y, Chen H, Qiu Y. The relationship between urbanization and depression in china: the mediating role of neighborhood social capital. Int J Equity Health. (2018) 17:105. doi: 10.1186/s12939-018-0825-x
Keywords: built environment, older adults, mental health, perception of community cohesion, perception of community safety, income
Citation: Zhang R, He X, Liu Y, Li M and Zhou C (2022) The Relationship Between Built Environment and Mental Health of Older Adults: Mediating Effects of Perceptions of Community Cohesion and Community Safety and the Moderating Effect of Income. Front. Public Health 10:881169. doi: 10.3389/fpubh.2022.881169
Received: 22 February 2022; Accepted: 23 May 2022;
Published: 17 June 2022.
Edited by:
Louise Lafortune, University of Cambridge, United KingdomCopyright © 2022 Zhang, He, Liu, Li and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunshan Zhou, emhvdWNzQG1haWwuc3lzdS5lZHUuY24=
 Rongrong Zhang
Rongrong Zhang Xiong He
Xiong He Ying Liu1
Ying Liu1 Ming Li
Ming Li Chunshan Zhou
Chunshan Zhou