- 1Department of Occupational Science and Occupational Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
- 2Krembil Research Institute, University Health Network, Toronto, ON, Canada
- 3Centre for Research in Occupational Safety and Health, Laurentian University, Sudbury, ON, Canada
- 4School of Public Health, Shanghai Jiao Tong University, Shanghai, China
- 5Department of Population Medicine, The University of Guelph, Guelph, ON, Canada
- 6Medical Laboratory Professionals Association of Ontario, Hamilton, ON, Canada
Objectives: The overall objective of this proposed project is to examine the impact of the COVID-19 pandemic on the mental health, functioning and wellbeing of medical laboratory technologists (MLT) and medical laboratory technicians/assistants (MLT/A) in Ontario, Canada.
Methods: A cross-sectional study included a self-reported questionnaire for MLT and MLT/A in Ontario. The questionnaire included questions about demographics and occupational characteristics. Questions about mental health, functioning, well-being and psychosocial work environments were also included using validated questionnaires.
Results: There were 551 MLT and 401 MLT/A in the analytic sample. Most of the respondents were women. The mean age and standard deviation of the overall sample were 42.0 ± 11.8. MLT demonstrated higher quantitative demands, possibilities for development, and organizational justice compared to MLT/A. The scores of work pace, emotional demands, role conflicts, job insecurity, insecurity over working conditions and negative acts were higher for MLT/A than MLT. The WHODAS 2.0 scores of the respondents were 20.80 ± 6.68, higher than approximately 92% average people. For both groups, most respondents scored the COPSOQ-III domains as worse since COVID-19.
Conclusion: The study provides preliminary evidence regarding the workplace mental health outcomes of medical laboratory professionals in Ontario, Canada. The findings suggest that MLT and MLT/A experience psychosocial work conditions that impact mental health, functioning and disability. Accordingly, additional research is necessary to understand the experiences of medical laboratory professionals.
Introduction
In Canada, Medical Laboratory Technologists (MLT) and Medical Laboratory Technicians/Assistants (MLT/A) are the sixth-largest groups of healthcare professionals. MLT job duties include laboratory analyses, where physicians use the results to evaluate and make informed decisions about their patients' health and possible treatment (1). Working with MLT, MLT/A work responsibilities include conducting medical laboratory testing and maintaining equipment. During the COVID-19 pandemic, MLT and MLT/A have been responsible for the processing of COVID-19 tests (2). In Ontario, MLT and MLT/As are experiencing increased workloads because of the COVID-19 pandemic, leading to deleterious health outcomes, including burnout (3–6). In addition, Ontario is facing a severe shortage of MLT in 2019, the Medical Laboratory Professionals' Association of Ontario (MLPAO) indicated a significant labor shortage of MLT in Ontario (7). According to the MLPAO (2), 70% of labs that entered COVID-19 were already short-staffed. Furthermore, 44% of MLT will retire in the next 4–8 years (7). The situation is worse in rural and remote areas, where nearly half (45%) of employment opportunities are located. The shortage is ongoing as 39% of openings have been on the market for more than 12 months. Moreover, the healthcare system cannot meet this labor shortage. The increased workload exacerbates this situation and leads to increased work exhaustion, job dissatisfaction, and turnover rates. This leads to mental health illness and stress creating a constant cycle of increased workload, poor mental health, staff illness and absences, and staff shortages (8).
Poor psychosocial health safety has been associated with adverse health outcomes among workers (6). Key workplace factors that can influence psychological wellbeing include collegial relationships, workplace supports and resources, autonomy, working conditions, and opportunities for and attainment of achievements. An example of a health outcome is job stress. In a study with 4,613 laboratory professionals, 96.1% reported feeling “a little bit to a lot of stress” (9). Respondents also reported feeling overwhelmed by their workload, having little control over their work schedule, and feeling anxious about work. Another study found that the likelihood of high job stress for MLT is 36%, compared to nurses and nurse supervisors (67%) and MLT/A (64%) (10). Occupational burnout is another negative workplace health outcome, which is caused by prolonged job stress and leads to physical and emotional exhaustion. Factors associated with burnout and job stress are understaffing and high workloads. Burnout has been studied extensively in many health care groups, including doctors (5, 11, 12), nurses (6, 9, 12), occupational and physical therapists (8, 13–15), psychologists and social workers (4). However, there is a dearth of evidence examining burnout among MLT and MLT/A, particularly in Canada. Other areas of psychosocial wellbeing include support resources, job satisfaction, and emotional demands. Moreover, these factors can impact functioning, biopsychosocial health, job satisfaction, productivity, and work performance (9).
Several studies discuss the significant impact of COVID-19 pandemic on the mental health of individuals, causing stress, anxiety, depressive symptoms, insomnia, denial, anger, and fear (16, 17). More specifically, the mental health of frontline health workers during the COVID-19 pandemic have been widely reported and include symptoms of psychological distress, burnout, anxiety and stress (18–21). The pandemic has increased workplace demands and stressors to healthcare professionals as they had to adapt to increased workloads, new work practices including telehealth and personal protective equipment, increased risks to infection, and redeployment (18). In a national U.S. survey looking at cardiac catheterization laboratory (CCL) nurses and technologists during the COVID-19 pandemic, there was an increase in anxiety/stress (80%), fear (39%), depression (36%), and anger (38%) (22). Furthermore, in a study with healthcare professionals, they found that the increasing number of cases, shortage of medical staff, build-up of working hours and the latent risk of infection were among many factors that increased internal stress (23). In a survey of 348 Ontario laboratory professionals, 87% reported experiencing burnout after a year of testing 24/7 (24).
The literature suggests that prolonged exposure to deleterious mental health and functional outcomes is associated with negative physical and mental health outcomes (24–28).
The literature also suggests that the COVID-19 pandemic has negative effects on mental health (17). The impact of the pandemic on MLT and MLT/A mental health and functioning includes but is not limited to their psychosocial work environment (e.g., work stress, job satisfaction, work productivity, quality of work-life, and work demands) and their means of coping, which remains poorly understood. Thus, the overall objective of this proposed project is to examine the impact of the COVID-19 pandemic on the mental health, functioning and wellbeing of medical laboratory technologists (MLT) and medical laboratory technicians/assistants (MLT/A) in Ontario.
Methods
Design
A cross-sectional study included a self-reported questionnaire for MLT and MLT/A in Ontario, Canada. The questionnaire was developed in close collaboration with the MLPAO, medical laboratory professionals and a comprehensive literature review. The questionnaire included questions about MLT and MLT/A mental health, wellbeing and psychosocial work environments, roles and demographics, and occupational characteristics using validated questionnaires. The research project was approved by the research ethics board at the University of Toronto. All the data will be collected and securely stored on REDCap (29) servers at the University of Toronto. The study received ethical approval from the University of Toronto Research Ethics Board (ID censored for peer-review).
Sample
MLT and MLT/A were invited to complete an anonymous questionnaire and informed consent stating the study's objectives, description, respondents' rights as research participants. In addition, the respondents were provided with two electronic reminders 2 and 4 weeks after the launch of the questionnaire to those who had not responded to the survey. The MLPAO is a provincial organization that represents the interests of medical laboratory professionals with government, health care professionals, regulatory bodies and academic institutions (24). The questionnaire and all reminders were distributed electronically by the MLPAO.
All MLT and MLT/A who met the following eligibility criteria were invited to participate in the current study: (1) actively registered with the College of Medical Laboratory Technologists of Ontario (only for MLT who are a regulated health care profession in the province), (2) Ontario was their clinical practice location, (3) employed and working as of March 11, 2020 (start date of the global pandemic) and (4) position as an MLT or MLT/A providing direct or indirect clinical patient care. In total, there were 553 MLT and 401 MLT/A that met the study's eligibility criteria. We applied a sample size calculation (30) to determine the sample size that was adequate to detect small to moderate differences in the level of job stress and burnout as perceived for MLT and MLT/As working across Ontario, Canada.
Measures
The questionnaire included items from the Copenhagen Psychosocial Questionnaire, third edition (COPSOQ-III) English version, an instrument designed for assessing psychosocial conditions in the workplace (31). The present study used 48 questions from the COPSOQ-III middle version, to measure mental health, participation and engagement in MLT and MLT/A. The COPSOQ-III looks at the following domains: work demands, work organization and job contents, interpersonal relations and leadership, work-individual interface, social capital, health and wellbeing and negative acts. Twenty-seven dimensions were assessed across these domains, including but not limited to social support, job security, burnout, and stress. For each COPSOQ-III dimension, Likert Scale–type items were measured and scaled to the interval of 0–100. Response options vary by scale values and scale direction. For example, Very satisfied (100), Satisfied (75), Neither/Nor (50), Unsatisfied (25), Very unsatisfied (0). Psychometric properties of the COPSOQ-III were assessed in various countries, including Canada (31). In an international study looking at the COPSOQ-III psychometric properties, ceiling effects were present for the dimensions Sense of Community at work (30%), Social Support from Colleagues (21%), Social Support from Supervisor (25%), Meaning of Work (25%) and Quality of Work (26%). Furthermore, floor effects were present for dimensions such as Job Insecurity (19%). The COPSOQ-III also has Canadian standardized used to compare to our population. As this portion of the study is cross-sectional, it is unknown if the results are influenced by COVID-19. To this end, following each domain, the participant answered the question: “Since COVID-19, my current response is ‘better than, ‘the same as', or ‘worse than' before the pandemic.”
The World Health Organization Disability Assessment Schedule (WHODAS) 2.0 was used to measure functioning and disability in MLT and MLT/A. This 36-item questionnaire covers 6 domains of functioning: 1 = cognition, 2 = mobility, 3 = self-care, 4 = getting along, 5 = life activities, and 6 = participation (32). The WHODAS 2.0 uses a Likert-like scale and scores for each item  ranges
ranges rom 1 (none) to 5 (extreme). Psychometric properties of the WHODAS 2.0 have been assessed in various countries, including Canada (33, 34). In addition, the factor structure is consistent across different health populations such as psychiatric illnesses, sclerosis, stroke, and alcohol dependency.
rom 1 (none) to 5 (extreme). Psychometric properties of the WHODAS 2.0 have been assessed in various countries, including Canada (33, 34). In addition, the factor structure is consistent across different health populations such as psychiatric illnesses, sclerosis, stroke, and alcohol dependency.
Data Analysis
All statistical analyses were performed using R software (Version 4.1.0 for Windows) (35). Demographic information was summarized using descriptive statistics including percentages, means and standard deviations. The current status of mental health, functioning, and wellbeing, and the impact of the COVID-19 pandemic on MLT and MLT/A was examined using descriptive and inferential statistics. To examine the differences in COPSOQ domains, we dichotomized the scores into “low” and “high” by using the median values of the distribution (36). Analysis of variance (ANOVA) and t-test were used to examine differences between groups. Comparisons between some groups were made using Fisher's exact analysis due to the small number of certain groups. The sample size varied for some analyses because of missing data on covariates, and the numbers were indicated in the tables. Statistical significance was set at p < 0.05.
Results
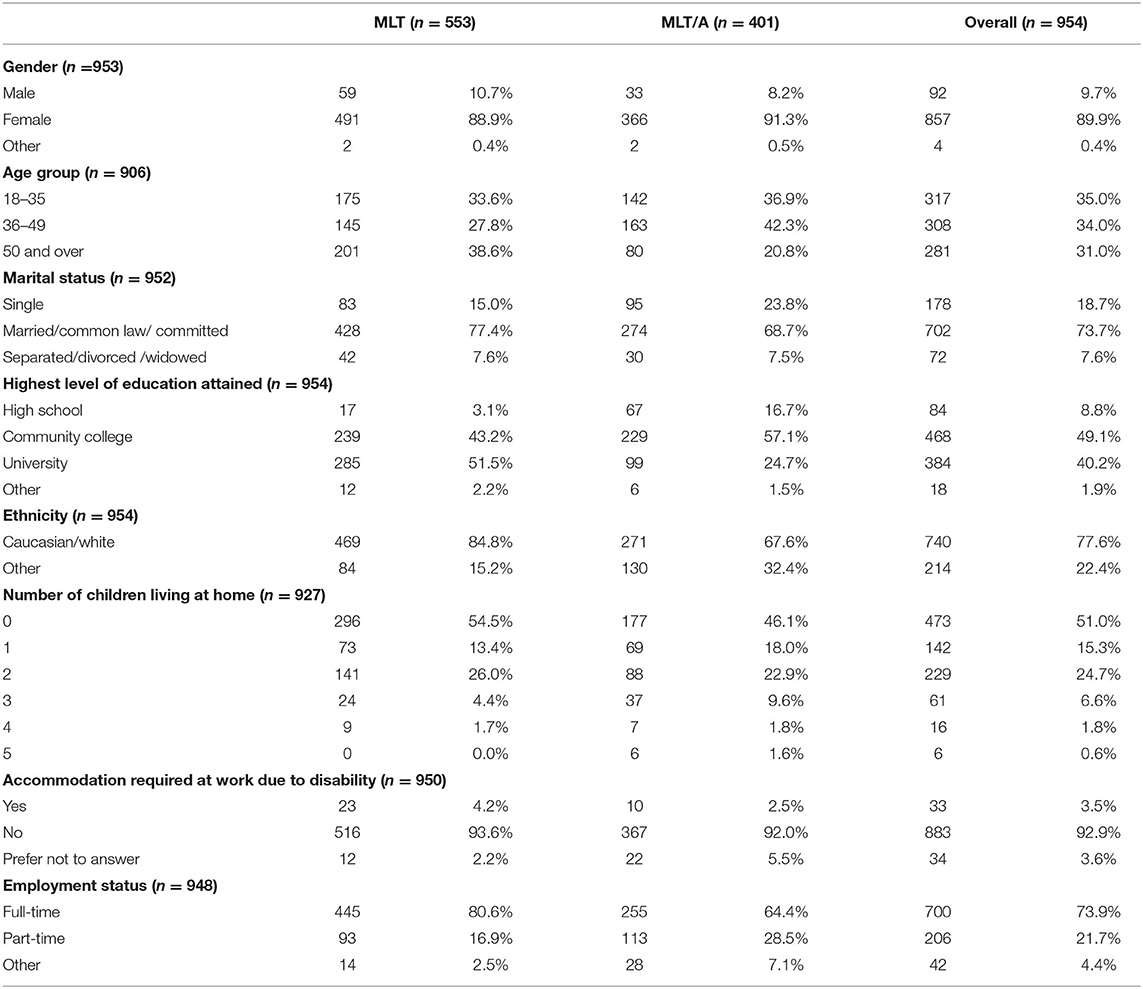
The study's response rate was 79.6% (954/1198). The majority (89.9%) of the respondents, including 88.9% MLT and 91.3% MLT/A, self-identified as women. The mean age and standard deviation of the overall sample, MLT and MLT/A were 42.0 ± 11.8, 43.9 ± 12.3, 39.5 ± 10.5, separately. High proportion (77.6%) of Caucasian/white was the characteristic for the considered study population (accounting for 84.8% MLT and 67.6% MLT/A). Table 1 summarizes the main demographic characteristics of the study population.
COPSOQ Scales
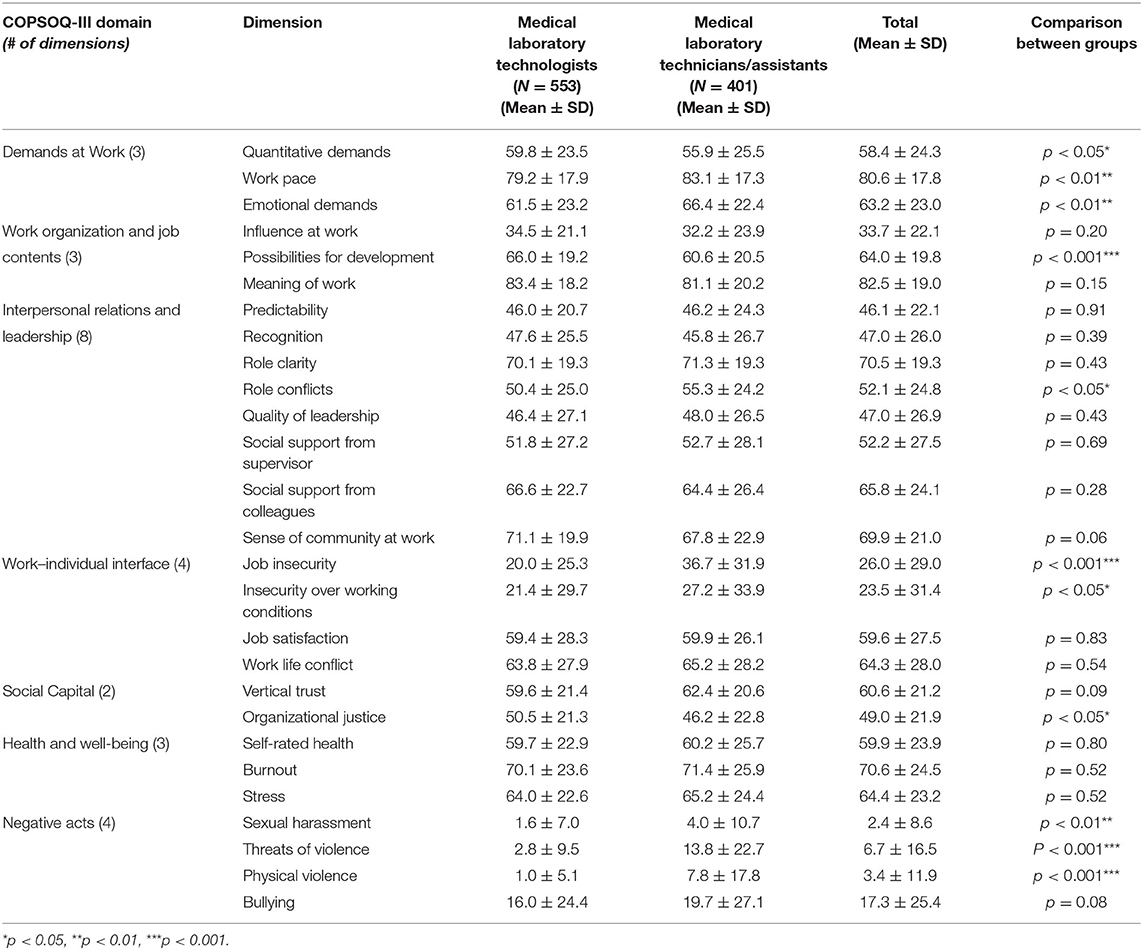
The mean values for the COPSOQ III scales and a comparison of psychosocial factors based on the domains and dimensions of COPSQQ-III among the respondents were presented in Table 2.
Demands at Work
The results showed that the scales of “quantitative demands” were significantly higher for the group of MLT (59.8 ± 23.5) than MLT/A (55.9 ± 25.5). High work pace (79.2 ± 17.9) and emotional demands (61.5 ± 23.2) for the group of MLT were determined, but they were lower than those for MLT/A (83.1 ± 17.3 and 66.4 ± 22.4, respectively).
Work Organization and Job Contents
The values of the “possibilities for development” dimension were higher for MLT (66.0 ± 19.2) than MLT/A (64.0 ± 19.8). Values of influence at work and meaning of work didn't have any distinction between the two groups.
Interpersonal Relations and Leadership
Compared to MLT (50.4 ± 25.0), the values of role conflicts for MLT/A were significantly higher (55.3 ± 24.2). Besides role clarity and role conflicts, other six dimensions (predictability, recognition, quality of leadership, social support from supervisor, social support from colleagues, sense of community at work) presented relatively lower scores than general Canadian workers.
Work-Individual Interface
The categories “job insecurity” and “insecurity over working conditions” for MLT/A were rated high (36.7 ± 31.9 and 27.2 ± 33.9), while MLT rated these two dimensions within the relatively normative range (20.0 ± 25.3 and 21.4 ± 29.7).
Other Domains
MLT hold significantly higher scores (50.5 ± 21.3) in organizational justice than MLT/A (46.2 ± 22.8). MLT/A experienced more sexual harassment, threats of violence and physical violence than MLT.
WHODAS 2.0 Scores
Table 3 demonstrates the scores of the WHODAS 2.0 among respondents across the six domains. We found that a mean and standard deviation score of 20.80 ± 6.68 on the WHODAS 2.0 was the best score for describing the MLT and MLT/A population, 20.38 ± 6.34 for MLT and 21.59 ± 7.22 for MLT/A, separately. The participant scores were higher than ~92% of the WHODAS 2.0 population norms across the general population of 10 countries (e.g., China, India, Slovakia).
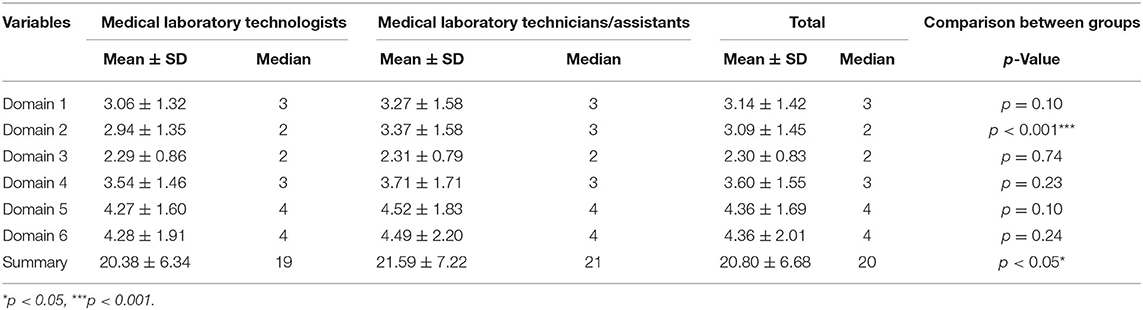
Table 3. A comparison of the functional scores among respondents across the six domains of the WHODAS 2.0.
The scores of MLT/A in Domain 2 (Mobility-moving and getting around) were higher than MLT (t = −3.4358, df = 398.62, p < 0.001). The summary scores also presented the same result (t = −2.1145, df = 410.96, p < 0.05).
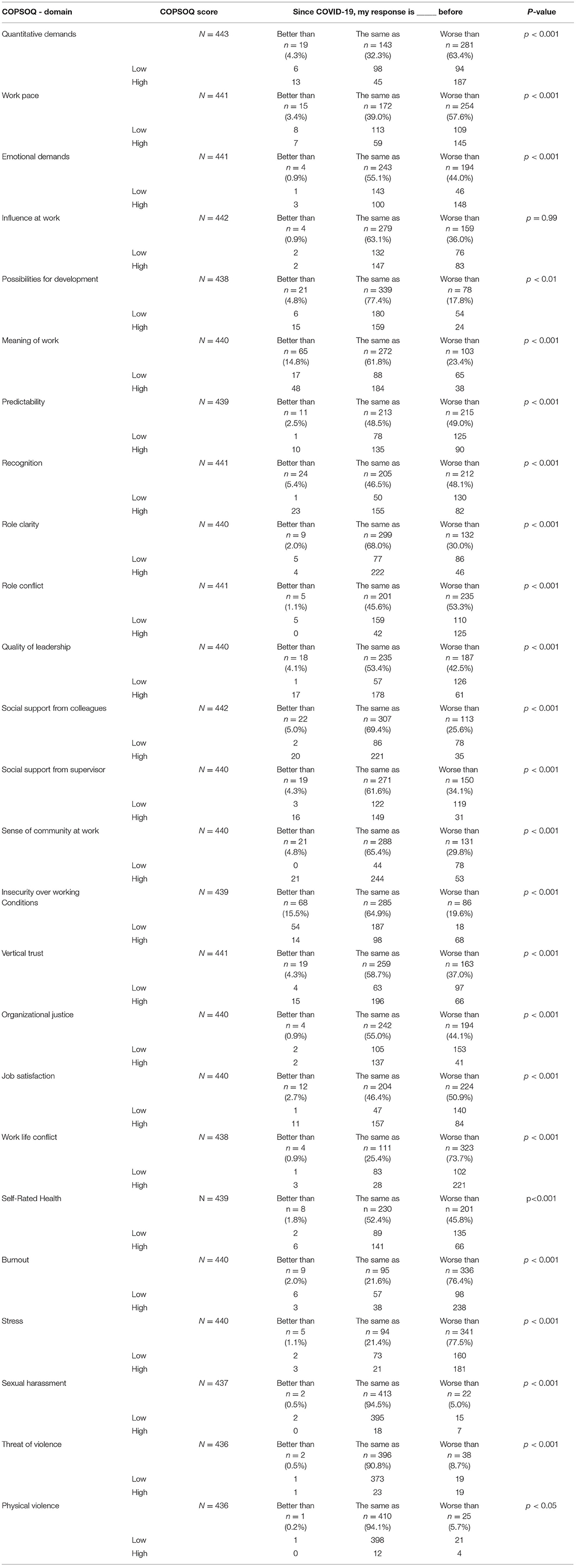
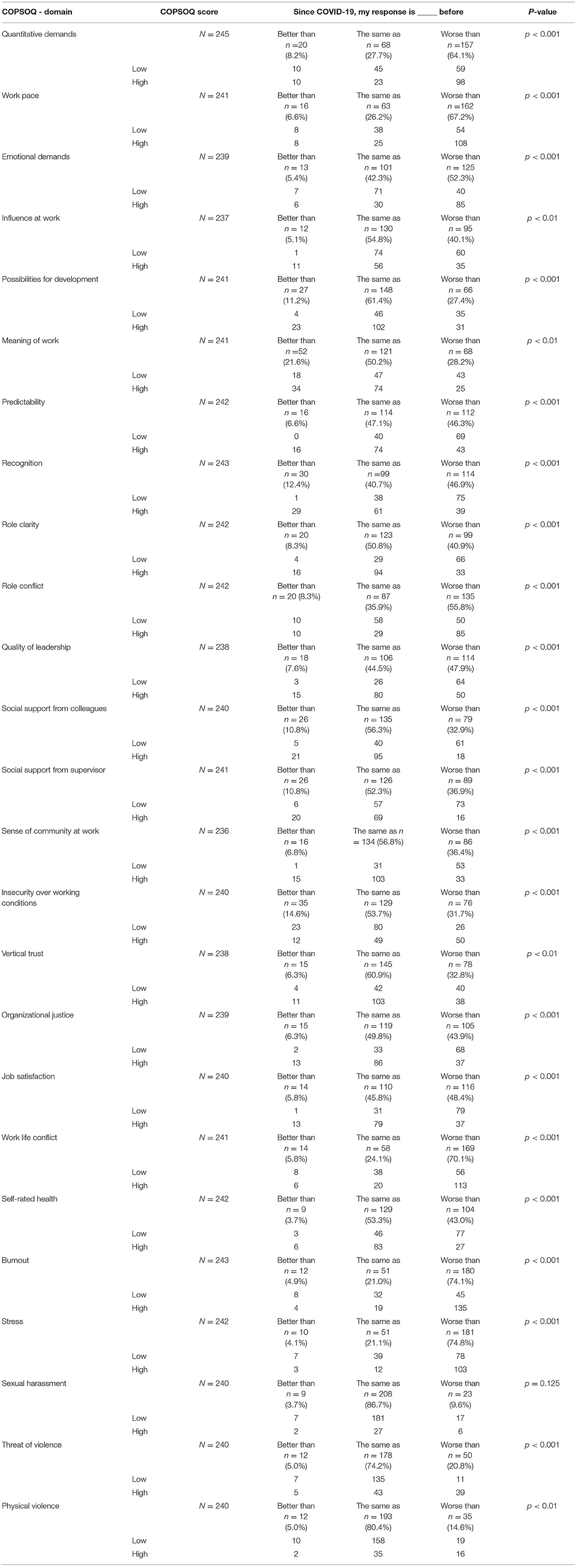
Impact of COVID-19
The impact of the COVID-19 pandemic was also assessed in Tables 4, 5. Table 4 presents a cross-tabulation of COPSOQ III scores and COVID-19 among MLTs. While cross-tabulation of COPSOQ III scores and COVID-19 among technicians is found in Table 5. For both groups, the majority of the respondents reported the COPSOQ-III domains as “worse than” since COVID-19.
In addition, respondents with poor psychological status (e.g., the low group for meaning of work; high group for work pace) were more likely to experience greater pressure under the influence of the epidemic. For example, we found that 33.3% (n = 84) MLT with high job satisfaction reported that their job satisfaction was worse than before the start of the pandemic, while 74.5% (n = 140) MLT with low job satisfaction reported that their job satisfaction was worse than before the start of the pandemic (P < 0.001). Furthermore, we found that 67.22% of MLT/A indicated that they felt worse about work pace than before the start of the pandemic, especially those who experienced faster work pace initially.
Discussion
The main findings of this study found scores of work pace, emotional demands, role conflicts, job insecurity, insecurity over working conditions and negative acts were higher for MLT/A than MLT. The purpose of the study is to examine the current mental status, functioning and disability of medical laboratory professionals in Ontario and the impact of the COVID-19 pandemic on their mental health. This is the first study to examine the psychosocial risk factors of medical laboratory professionals in Ontario, Canada. The health care workers are working at the scenes and are not patient-facing. However, they are the backbone of the healthcare system in providing critical services in general medical laboratory technology, diagnostic typology, and clinical genetics (37). The fact that most of the medical laboratory professions were women, which was larger than other healthcare workers, like doctors, occupational therapists might account for some high scores in COPSOQ because early studies showed that women were more likely to suffer from mental health problems, e.g., depression, anxiety and burnout, considered because job status could also influence mental health problems. For example, Labrague et al. showed that health workers like nurses who worked part-time reported higher fear scores than full-time workers, thus affecting their psychological and emotional wellbeing and work performance (38). The characteristic of part-time work, including temporary and unstable, also increase job insecurity and leaves little room for career development. Therefore, the high proportion of part-time jobs in MLT/A may also be an important reason for this population's prominent psychological health problem.
In addition, negative behaviors like physical violence and sexual harassment in the workplace was also common among laboratory professions, especially among MLT/A group. These kinds of behaviors will affect an individual's work performance or create an intimidating, hostile, or offensive environment (39). Studies focused on nurses have found that greater work demands and less trust and justice were associated with nurses' experiences of violence (40). Manageable workloads and greater understanding of MLT and MLT/A work responsibilities and a more supportive work environment may reduce negative health outcomes acts for medical laboratory professions.
The high sense of job insecurity and insecurity over working conditions was present, especially in the group of MLT/A; heavy demands of workload, including high quantitative and emotional demands and fast work pace were also reflected in medical laboratory professions, especially MLT. This reflected the current problems in the medical laboratory system: inadequate working conditions, high workload, growing competition among healthcare workers and less safety at work. Health workers in such circumstances are experiencing increased pressures at their workplace due to high working demands or do not have enough time to complete the tasks and feel insecure, despite giving maximum effort.
In addition, respondents with poor psychological status (e.g., the low group for meaning of work; high group for work pace) were more likely to experience greater pressure under the influence of the epidemic, which led to further deterioration of their mental health. For example, we found a third MLT with high job satisfaction reported that their job satisfaction was worse than before the start of the pandemic, while almost three quarters of MLT with low job satisfaction reported feeling worse. This vicious circle suggested the importance of early intervention and early treatment for medical laboratory professions.
We found that the mean scores of WHODAS 2.0 in MLT and MLT/A were higher than approximately 92% of the WHODAS 2.0 population norms across the general population of 10 countries, indicating the extent of disability associated with a psychiatric condition among medical laboratory workers was quite serious than average people. When disability limits a person's daily activities, it is clinically significant to consider the impact (i.e., possible mental problems) disability may cause. Moreover, there is evidence that the increase in the WHODAS 2.0 score was associated with increased comorbidities, in particular those related to mental (depression) and physical health (41).
Strengths and Limitations
Mental Health, functioning and disability were significant health concerns for medical laboratory professionals in Ontario. At the same time, they did not receive the same attention as other healthcare workers, e.g., doctors or nurses. To raise awareness on this occupational group, we worked closely with the Medical Laboratory Professionals' Association of Ontario (MLPAO) to recruit participants across the province to represent the diversity of the workforce across geography and workplace settings (e.g., hospitals, private laboratories, etc.). Therefore, the sample is well representative of this group in Ontario. We used the COPSOQ-III and WHODAS 2.0, two internationally well-known questionnaires to measure the results, giving a better reference value for our results. Our study also covered a comparison in the mental status before and after COVID-19 in this occupational group, which has not been examined in any previous studies.
We also acknowledge other potential limitations. First, this was a cross-sectional study, so that causality could not be established. Second, the study participants (MLT and MLA/T) were emailed a link to the survey using REDCap at one certain time. As a result, this may lead to bias in that the credibility and validity of email patterns were not as high as face-to-face interviews. In addition, there are different versions of COPSOQ-III that may raise questions about the reliability of the results when comparing the results with other studies. Furthermore, the study did not evaluate or examine other conditions of COVID-19, such as issues regarding families and restrictions. As a result, this limitation does not allow us to capture the full impact of Covid-19.
Conclusion
The study provides preliminary evidence regarding the workplace mental health outcomes of medical laboratory professionals in Ontario, Canada. The implications of the pandemic reflected on mental health and functioning, specifically the limitations on their psychosocial work environments, have led this study to examine these effects. The scores of work pace, emotional demands, role conflicts, job insecurity, insecurity over working conditions and negative acts were higher for MLT/A than MLT. In terms of their functioning, we observed scores that are higher than the 92% of the normed population. There is a need for robust studies that examine a larger sample across time. The findings may also provide information for governments and employers to address strategies to improve the mental health of laboratory medical professionals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by University of Toronto Research Ethics Board. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The Medical Laboratory Professionals' Association of Ontario funded the Article Processing Charge.
References
1. Bandali K, Zhu L, Gamble PAW. Canada's health human resource challenges: what is the fate of our healthcare heroes? Healthc Manage Forum. (2011) 24:179–83. doi: 10.1016/j.hcmf.2011.04.001
2. Medical Laboratory Professionals' Association of Ontario. Report: medical laboratory professionals at a breaking point – two-year analysis. (2022). Available online at: https://www.mlpao.org/_files/ugd/691355_870e5fae53f34d0cba723820bac97c13.pdf
3. Maunder RG, Heeney ND, Strudwick G, Shin HD, O'Neill B, Young N, et al. Burnout in Hospital-Based Healthcare Workers during COVID-19. Ontario: Science Briefs of the Ontario COVID-19 Science Advisory Table (2021).
4. Roslan NS, Yusoff MSB, Asrenee AR, Morgan K. Burnout prevalence and its associated factors among Malaysian healthcare workers during COVID-19 pandemic: an embedded mixed-method study. Healthcare. (2021) 9:1–90. doi: 10.3390/healthcare9010090
5. West CP, Dyrbye LN, Sinsky C, Trockel M, Tutty M, Nedelec L, et al. Resilience and burnout among physicians and the general US working population. JAMA Net Open. (2020). 3:e209385–96. doi: 10.1001/jamanetworkopen.2020.9385
6. Woo T, Ho R, Tang A, Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J Psychiatr Res. (2020) 123:9–20. doi: 10.1016/j.jpsychires.2019.12.015
7. Medical Laboratory Professionals' Association of Ontario. Medical Laboratory Shortage. Hamilton, ON (2019).
8. Bainbridge L, Davidson K, Loranger L. Burnout Among Alberta physiotherapists: A White Paper (2017).
9. Dyrbye LN, Shanafelt TD, Johnson PO, Johnson LA, Satele D, West CP, et al. cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs. (2019) 18:1–57. doi: 10.1186/s12912-019-0382-7
11. Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians. JAMA. (2018) 320:1131–51. doi: 10.1001/jama.2018.12777
12. Sanghera J, Pattani N, Hashmi Y, Varley KF, Cheruvu MS, Bradley A, et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—a systematic review. J Occup Health. (2020) 62:1–16. doi: 10.1002/1348-9585.12175
13. Painter J, Akroyd D, Elliot S, Adams RD. Burnout among occupational therapists. Occup Ther Health Care. (2003) 17:63–78. doi: 10.1080/J003v17n01_06
14. Poulsen AA, Meredith P, Khan A, Henderson J, Castrisos V, Khan SR. Burnout and work engagement in occupational therapists. Br J Occup Ther. (2014) 77:156–64. doi: 10.4276/030802214X13941036266621
15. Scanlan JN, Hazelton T. Relationships between job satisfaction, burnout, professional identity and meaningfulness of work activities for occupational therapists working in mental health. Aust Occup Ther J. (2019) 66:581–90. doi: 10.1111/1440-1630.12596
16. Sanchez-Gomez M, Giorgi G, Finstad GL, Urbini F, Foti G, Mucci N, et al. COVID-19 pandemic as a traumatic event and its associations with fear and mental health: a cognitive-activation approach. Int J Environ Res Public Health. (2021) 18:1–14. doi: 10.3390/ijerph18147422
17. Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
18. Smallwood N, Karimi L, Bismark M, Putland M, Johnson D, Dharmage SC, et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: a cross-sectional survey. Gen Psychiatry. (2021) 34:1–11. doi: 10.1136/gpsych-2021-100577
19. Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: A multinational cross-sectional study. PLoS ONE. (2021) 16:1–18. doi: 10.1371/journal.pone.0238666
20. Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. (2020) 290:113129–33. doi: 10.1016/j.psychres.2020.113129
21. Chor WPD, Ng WM, Cheng L, Situ W, Chong JW, Ng LYA, et al. Burnout amongst emergency healthcare workers during the COVID-19 pandemic: a multi-center study. Am J Emerg Med. (2021) 46:700–2. doi: 10.1016/j.ajem.2020.10.040
22. Estes BA, Varghese JJ, Jacques J, Naidu SS. Logistical, financial, and psychological impact of the COVID-19 pandemic on cardiac catheterization lab nurses and technologists: A US National Survey. J Invasive Cardiol. (2021) 33:E9–15. doi: 10.5709/ce.1897-9254.433
23. Pazmiño Erazo EE, Alvear Velásquez MJ, Saltos Chávez IG, Pazmiño Pullas DE. Factors associated with psychiatric adverse effects in healthcare personnel during the COVID-19 pandemic in Ecuador. Revista Colombiana de Psiquiatría. (2021) 50:166–75. doi: 10.1016/j.rcpeng.2020.12.001
24. Medical Laboratory Professionals' Association of Ontario. About The MLPAO (2021). Available online at: https://www.mlpao.org/about
25. Booker LA, Sletten TL, Alvaro PK, Barnes M, Collins A, Chai-Coetzer CL, et al. Exploring the associations between shift work disorder, depression, anxiety and sick leave taken amongst nurses. J Sleep Res. (2020) 29:1–9. doi: 10.1111/jsr.12872
26. Cocker F, Joss N. Compassion fatigue among healthcare, emergency and community service workers: a systematic review. Int J Environ Res Public Health. (2016) 13:1–18. doi: 10.3390/ijerph13060618
27. Duarte J, Pinto-Gouveia J. The role of psychological factors in oncology nurses' burnout and compassion fatigue symptoms. Eur J Oncol Nurs. (2017) 28:114–21. doi: 10.1016/j.ejon.2017.04.002
28. Hall LH, Johnson J, Watt I, Tsipa A, O'Connor DB. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS ONE. (2016) 11:1–12. doi: 10.1371/journal.pone.0159015
29. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:1–24. doi: 10.1016/j.jbi.2019.103208
30. Taherdoost H. Determining sample size; how to calculate survey sample size. Int J Econ Manag Syst. (2017) 2:237–9.
31. Burr H, Berthelsen H, Moncada S, Nübling M, Dupret E, Demiral Y, et al. The third version of the copenhagen psychosocial questionnaire. Saf Health Work. (2019) 10:482–503. doi: 10.1016/j.shaw.2019.10.002
32. Ustun TB, Kostanjsek N, Chatterji S, Rehm J. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). Geneva: World Health Organization (2010). p. 1–88.
33. MacLeod MA, Tremblay PF, Graham K, Bernards S, Rehm J, Wells S. Psychometric properties and a latent class analysis of the 12-item world health organization disability assessment schedule 20 (WHODAS 20) in a pooled dataset of community samples International. Int J Methods Psychiatr Res. (2016) 25:243–54. doi: 10.1002/mpr.1523
34. Pösl M, Cieza A, Stucki G. Psychometric properties of the WHODASII in rehabilitation patients. Qual Life Res. (2007) 16:1521–31. doi: 10.1007/s11136-007-9259-4
35. Chan BKC. Data Analysis Using R Programming. In: Biostatistics for Human Genetic Epidemiology. Sunnyvale, CA: Springer International Publishing (2018). p. 47–122.
36. Slany C, Schütte S, Chastang JF, Parent-Thirion A, Vermeylen G, Niedhammer I. Psychosocial work factors and long sickness absence in Europe. Int J Occup Environ Health. (2014) 20:16–25. doi: 10.1179/2049396713Y.0000000048
37. Canadian Institute for Health Information. Medical Laboratory Technologists. Canadian Institute for Health Information (2021).
38. Labrague LJ, Santos JAA. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. (2021) 29:395–403. doi: 10.1111/jonm.13168
39. Nukala M, Freedman-Weiss M, Yoo P, Smeds MR. Sexual harassment in vascular surgery training programs. Ann Vasc Surg. (2020) 62:92–7. doi: 10.1016/j.avsg.2019.05.011
40. Park M, Cho SH, Hong HJ. Prevalence and perpetrators of workplace violence by nursing unit and the relationship between violence and the perceived work environment. J Nurs Scholarsh. (2015) 47:87–95. doi: 10.1111/jnu.12112
Keywords: medical laboratory technologists, medical laboratory assistants/technicians, medical laboratory professionals, mental health, occupational health, Canada
Citation: Nowrouzi-Kia B, Dong J, Gohar B and Hoad M (2022) Examining the Mental Health, Wellbeing, Work Participation and Engagement of Medical Laboratory Professionals in Ontario, Canada: An Exploratory Study. Front. Public Health 10:876883. doi: 10.3389/fpubh.2022.876883
Received: 16 February 2022; Accepted: 01 June 2022;
Published: 15 July 2022.
Edited by:
Judie Arulappan, Sultan Qaboos University, OmanReviewed by:
Nicola Mucci, University of Florence, ItalyCeyda Sahan, Dokuz Eylül University, Turkey
Copyright © 2022 Nowrouzi-Kia, Dong, Gohar and Hoad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Behdin Nowrouzi-Kia, behdin.nowrouzi.kia@utoronto.ca; orcid.org/0000-0002-5586-4282
 Behdin Nowrouzi-Kia
Behdin Nowrouzi-Kia Jingwen Dong4
Jingwen Dong4 Basem Gohar
Basem Gohar