- 1Department of Pediatric Dentistry, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia
- 2Department of Pediatric Dentistry and Dental Public Health, Faculty of Dentistry, Alexandria University, Alexandria, Egypt
- 3Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
- 4Medical Faculty, Istanbul Medipol University, Istanbul, Turkey
- 5City Quay Dental Practice and Implant Centre, Dundee, Scotland
- 6Department of Education, University of Kashmir, Srinagar, India
- 7Faculty of Dentistry, Alexandria University, Alexandria, Egypt
- 8Faculty of Dentistry, National Ribat University, Khartoum, Sudan
- 9College of Dentistry, Ajman University, Ajman, United Arab Emirates
- 10Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Syrian Private University, Damascus, Syria
- 11General Courses, King Abdulaziz University, Jeddah, Saudi Arabia
- 12Faculty of Engineering, King Abdulaziz University, Jeddah, Saudi Arabia
- 13King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
- 14Department of Child Dental Health, Obafemi Awolowo University, Ile-Ife, Nigeria
- 15Department of Preventive and Community Dentistry, Faculty of Dentistry, Obafemi Awolowo University, Ile-Ife, Nigeria
- 16Schulich School of Medicine and Dentistry, University of Western Ontario, London, ON, Canada
- 17Department of Dental Surgery, Oman Dental College, Muscat, Oman
- 18UCSI University, Kuala Lumpur, Malaysia
- 19Laboratory of Cereal Plant Pathology, National Institute for Argonomic Research, Settat, Morocco
- 20Division of Imaging Science and Technology, School of Medicine, University of Dundee, Dundee, Scotland
- 21Western Cape Education Department, Cape Town, South Africa
- 22International Medical Centre, Jeddah, Saudi Arabia
- 23Schools of Awqaf, Jerusalem, Israel
- 24Gothenburg University, Gothenburg, Sweden
- 25Health Education Services, Lansing, MI, United States
The use of cigarettes among adolescents and young adults (AYA) is an important issue. This study assessed the association between regular and electronic-cigarettes use among AYA and factors of the Capability-Motivation-Opportunity-for-Behavior-change (COM-B) model. A multi-country survey was conducted between August-2020 and January-2021, Data was collected using the Global-Youth-Tobacco-Survey and Generalized-Anxiety-Disorder-7-item-scale. Multi-level logistic-regression-models were used. Use of regular and electronic-cigarettes were dependent variables. The explanatory variables were capability-factors (COVID-19 status, general anxiety), motivation-factors (attitude score) and opportunity-factors (country-level affordability scores, tobacco promotion-bans, and smoke free-zones) controlling for age and sex. Responses of 6,989-participants from 25-countries were used. Those who reported that they were infected with COVID-19 had significantly higher odds of electronic-cigarettes use (AOR = 1.81, P = 0.02). Normal or mild levels of general anxiety and negative attitudes toward smoking were associated with significantly lower odds of using regular-cigarettes (AOR = 0.34, 0.52, and 0.75, P < 0.001) and electronic-cigarettes (AOR = 0.28, 0.45, and 0.78, P < 0.001). Higher affordability-score was associated with lower odds of using electronic-cigarettes (AOR = 0.90, P = 0.004). Country-level-smoking-control policies and regulations need to focus on reducing cigarette affordability. Capability, motivation and opportunity factors of the COM-B model were associated with using regular or electronic cigarettes.
Introduction
International associations recommend monitoring, screening, and preventing tobacco smoking among children and adolescents (1). Chronic exposure to tobacco is associated with bacterial proliferation, reduced periodontal immunity, and head and neck cancer (2, 3). Electronic cigarettes also deliver nicotine similar to cigarette smoking (4) and were suggested to cause cancer by affecting cell proliferation, periodontal cell migration, cytotoxicity, oxidative stress, apoptosis, and DNA maturation (5, 6). In addition, smoking affects oral and pharyngeal tissues causing irritation, stimulation of microbial growth, reduced periodontal tissue immunity, enhanced alveolar bone resorption, and delayed healing (3, 7). However, research is needed to identify differences between the use of regular and electronic cigarettes regarding determinants and effects.
In order to understand cigarette use, causes and control, multiple complex behavioral interventions need to be addressed. The Capability, Opportunity and Motivation for Behavior change (COM-B) framework (8) offers a structured approach for planning evidence-based interventions that could explain behavioral changes associated with cigarette use and control (8–12). The COM-B framework suggests that people engage in a behavior if they have the Capability (physical and psychological), the Opportunity, when the surrounding environment is physically and socially convenient and the Motivation to adopt this behavior. Within this framework, we conceptualized that the capability factors that may be associated with smoking during the study period include anxiety (13–15) and stresses caused by the COVID-19 pandemic (16) which are assumed to increase the risk of cigarettes' use (17, 18). Also, health problems such as COVID-19 infection may reduce the ability to smoke. Smoking is assumed to decrease in communities where there are legislative controls such as reducing access to cigarettes which decrease the opportunities to engage in smoking (18). The global variation in success of global strategies to control tobacco (18) emphasize the need for global evidence to inform tobacco control programs. Multi-country studies can shed light on person- and country-level factors associated with health problems. At the same time, assessing individual factors such as attitudes toward smoking can guide the development of tobacco cessation counseling activities.
The aim of this study was to assess the capability, opportunity and motivation factors associated with using regular and electronic cigarettes among adolescents and young adults (AYA) in several countries. The hypothesis of the study was that use of cigarettes was associated with capability, opportunity or motivation.
Materials and methods
Design and ethical consideration
A multi-country, online survey was conducted between August 2020 to January 2021. Ethical approval was obtained from the Research Ethics Committee of the Faculty of Dentistry, King Abdulaziz University in Saudi Arabia with Proposal No. 90-08-20. The study was conducted in accordance with the Helsinki Declaration (19).
Participants
Participants were included if they were adolescents or young adults aged 11–23 years, if they/their parents consented to participate, if they were able to read the language of the survey, and if they had access to an electronic device with an Internet connection to access the survey. Exclusion criteria were children of younger age (below 11 years old), older adults (above 23 years-old), and children not living in the participating countries during the study period.
Sample size for estimating the prevalence of using regular or electronic cigarettes was based on the global prevalence of tobacco smoking for AYA. The prevalence ranged from 4.8 to 36.6% (20). The estimated sample size ranged from 71 to 356 participants. To calculate the sample size required to assess the factors associated with smoking, we used an online calculator for multilevel logistic regression models showing that with level 1 units (participants per country) at least = 50 and level 2 units (countries) = 25, the study would be able to detect at least moderate effect size (Cohen's d = 0.5) with power of 0.90 (21). Convenience sampling was used like in previous studies based on online surveys (22). Through snowball sampling, study participants were recruited and asked to distribute the survey link to others in their networks.
Patient and public involvement
During the formation of the study survey tool, public and community members were contacted to seek their feedback. Also, a group of AYA who were not excluded from further analysis were interviewed for their opinion about the questionnaire. They were also involved in disseminating the survey to ensure reaching different level of the community.
Study instrument development and validation
A questionnaire was developed with three sections. The first section assessed the socio-demographic information of the participant (age at last birthday, sex, and educational level) and parents' educational level.
The second section assessed participants' history of COVID-19 infection. Each participant was asked to identify if they had a history of diagnosed COVID-19 by checking a yes, no or do-not-know response. Also, the section included questions that assessed the psychological status of respondents using the Generalized Anxiety Disorder 7-item scale (GAD-7). The scale describes the frequency of seven items assessing general anxiety in the last 2 weeks (during the pandemic) on a 4-point scale ranging from 0: not at all to 3: nearly every day. The total score was the sum of points of all items ranging from 0 to 21. The cut-off points were 5, 10, and 15 for mild, moderate, and severe anxiety, respectively (23, 24). The scale had been validated for use in many of the countries included in the study (25, 26). The section also included five items specially developed for the study assessing respondents' attitude toward smoking asking participants whether they agreed with the following statements: that smoking leads to addiction, that it should be banned in children younger than 18 years old, that smokers are at greater risk of catching COVID-19, that they are at greater risk of having more severe COVID-19 manifestations and that it has harmful effects on the body. These items had three-point responses (agree, not sure, and disagree). The attitude score was created by recoding responses into agree (code 1) and others (code 0) and adding the points. Higher scores indicated more negative attitude toward smoking.
The third section enquired about regular and electronic cigarette use during the pandemic using the Global Youth Tobacco Survey (23). It asked about the current use of regular or electronic cigarettes (yes/no), the frequency of use (daily, weekly, monthly or less than monthly), changes in the frequency of use during the pandemic (less, same, or more than before) and the increase in nighttime use.
The questionnaire was developed in Arabic and translated into English, Turkish, Malay, and French by native researchers who were invited to collaborate with the core study team. The content validity index (CVI) for each version was calculated (27). The CVI for the Arabic and English versions was 0.87 based on evaluation by nine dentists, 0.97 for the Turkish version based on evaluation by seven dentists, 0.80 for the Malay version based on evaluation by five dentists and 0.88 for the French version based on evaluation by five dentists. Each version was pilot tested on 10 participants to ensure clarity and appropriate use of terms. The questionnaire was uploaded to the online platform SurveyMonkey® and the settings were managed to ensure that responses were anonymous and that responses could be submitted only once from the same electronic device. Cronbach alpha was used to assess the internal consistency of the GAD-7 and the attitude items. The Cronbach alpha of GAD-7 = 0.90 and that of the attitude to smoking scale = 0.63.
Study procedure
At the beginning of the survey, participants were required to identify if they belonged to the age groups: 11–14, 15–18, or 19–23 year old (1, 28). Participants who were 11–14 or 15–18-year-old were directed to a form recording the parent's consent for their participation. At the end of the form, the consenting parent was asked to invite their child to respond to the survey without supervision and to assure the child of the confidentiality of their responses. Participants who were 19–23-year-old were able to consent before proceeding to the survey. The purpose of the study was explained to the participants, and they were assured that they were free to withdraw from the survey at any time.
The core team (King Abdulaziz University, Saudi Arabia, and Alexandria University, Egypt) invited collaborators in their own network to collect data in different countries. Repeated invitations were sent to ensure maximum coverage since data could only be collected by country-collaborators. Interested collaborators received the study protocol, ethical approval, and timeline for the study. A customized link and a responses-tracking link were created for each collaborator in the language of interest. Recruitment was also done through social media.
Statistical analysis
There were two dependent variables for the study: the use of regular cigarettes and the use of electronic cigarettes. We used multi-level logistic regression analysis to account for the clustering of participants within countries. Level 1 factors were related to participants: participant's age and sex (confounders), COVID-19 infection status, GAD-7 score (capability factors) and attitude score (motivation factor). Level 2 factors represented opportunity factors measured at country level. Data for these factors were publicly available and obtained from the latest statistics included in the World Health Organization report on the tobacco pandemic in 2021 (29). These factors included the affordability score, which is the percentage of per capita gross domestic product required to buy 2,000 cigarettes of the most popular brand (29) with higher values indicating less affordable tobacco products. There was also a score ranging from 0 to 2 assessing the bans on tobacco promotion on television (29) including tobacco brands and tobacco products with higher score indicating greater compliance with bans. The last opportunity factor included a smoke-free zones score (29) assigning a point when smoking was banned in educational facilities except universities, in universities, restaurants and public transportation with a score ranging from zero to 4 with greater scores indicating greater availability of smoke-free areas. Level 1 and level 2 factors were fixed effect variables, and country of residence was entered as a random effect variable. We used robust estimation to address violations of model assumptions, fitted a random intercept and selected variance component as random effect covariance type. Adjusted odds ratios (AORs), 95% confidence intervals (CIs), and P values were calculated. We also used −2 log likelihood (−2LL) as a measure of deviance to assess the model goodness of fit with smaller values indicating better fit. We reported the −2LL for the unconditional model (without fixed effect variables) and for the conditional model where the fixed effect variables were included and calculated the difference between these two values then tested the significance of the difference using chi square test. We fitted unadjusted models where individual variables were introduced followed by adjusted models were all variables were introduced and mutually adjusted for each other. IBM SPSS for Windows version 22.0 (IBM Corp., Armonk, N.Y., USA) was used for analysis. Significance level was set at 5%.
Results
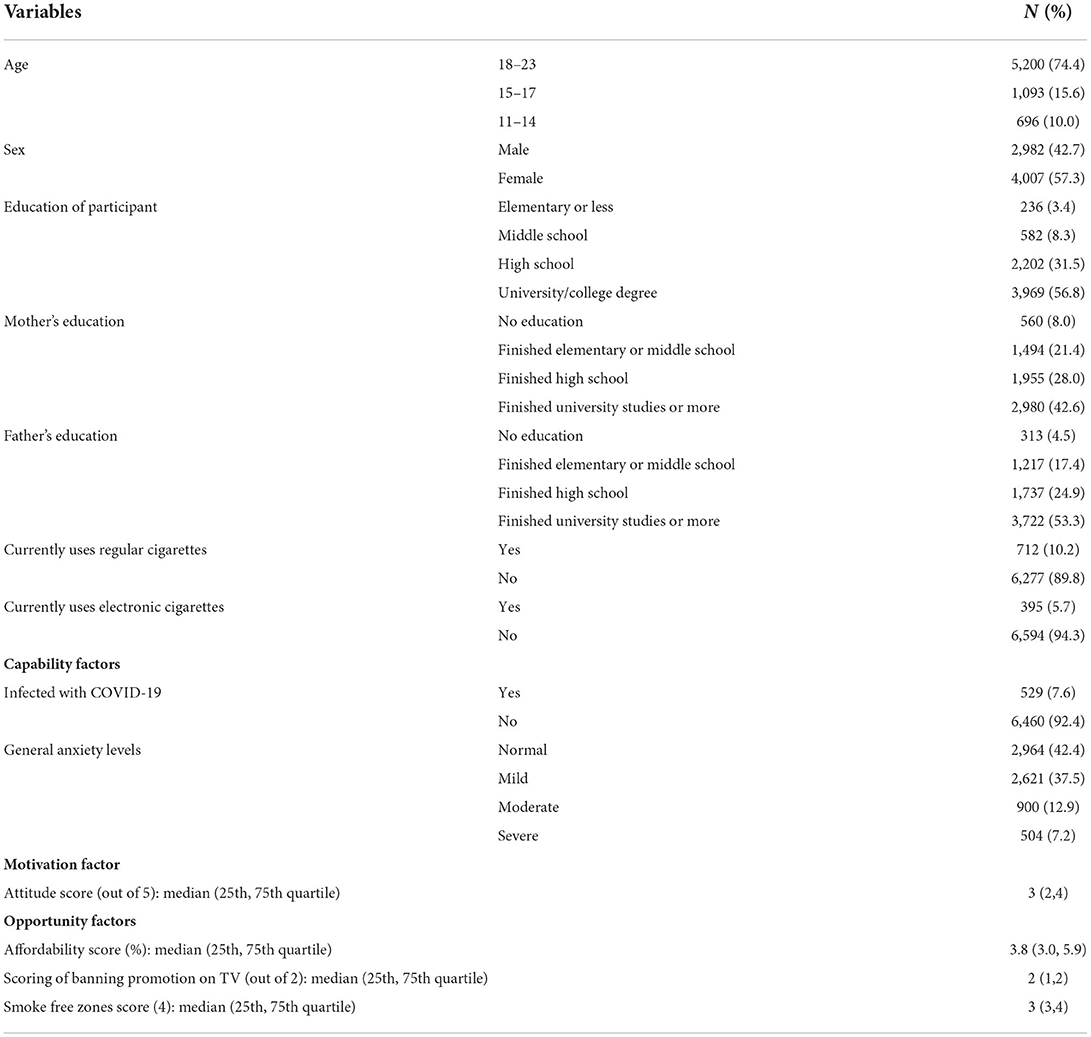
Complete data were available for 6,989 participants from 25 countries (Supplementary Table 1). Table 1 shows that most participants were 18–23 years old (74.4%), females (57.3%), with a university/college degree (56.8%). Most participants' parents had university degrees (42.6% of mothers and 53.3% of fathers). Also, 529 (7.6%) participants were infected with COVID-19, 712 (10.2%) currently used regular cigarettes and 395 (5.7%) currently used electronic cigarettes.
Also, 2,964 (42.4%) of the participants had normal anxiety and 504 (7.2%) had severe anxiety. The median scores for attitude toward smoking scale = 3 out of 5, for banning promotion on television = 2 out of 2, and for smoke free zones = 3 out of 4. The median affordability score was 3.8%.
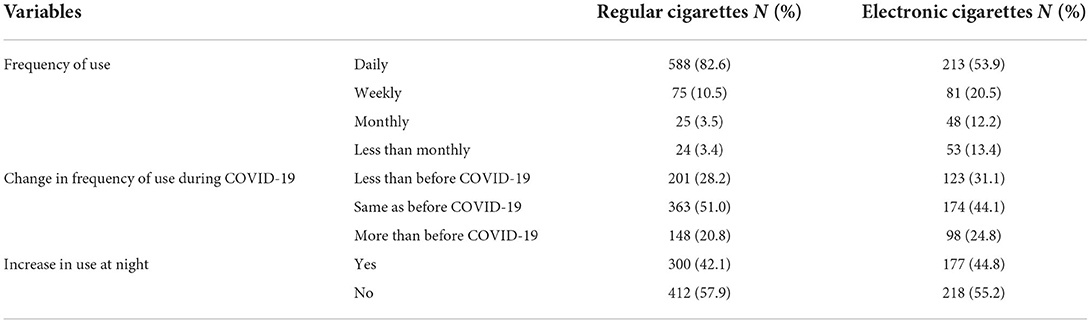
Table 2 shows that daily use was reported by 588 (82.6%) of regular cigarettes users and 213 (53.9%) electronic cigarettes users. Also, 363 (51.0%) and 174 (44.1%) participants reported the same frequency of using regular and electronic cigarettes as before the pandemic, 201 (28.2%) and 123 (31.1%) reported less frequent use during the pandemic; and 300 (42.1%) and 177 (44.8%) participants reported increased use of regular and electronic cigarettes at night.
Table 3 shows the factors associated with the current use of regular and electronic cigarettes in 25 countries. Participants who were 18–23-years-old and 15–17-years-old had significantly higher odds of using regular (AOR = 5.70, P < 0.001 and AOR = 2.28, P =0.005) and electronic cigarettes (AOR = 2.88, P < 0.001 and AOR = 2.25, P =0.002) than respondents who were 11–14-years-old. Male respondents had significantly higher odds of using regular (AOR = 5.96, P < 0.001) and electronic (AOR = 2.31, P < 0.001) cigarettes than females. Those who got infected with COVID-19 reported significantly higher odds of using electronic cigarettes (AOR = 1.81, P = 0.02). Having normal or mild levels of general anxiety were associated with significantly lower odds of using regular (AOR = 0.34 and 0.52, P < 0.001) and electronic (AOR = 0.28 and 0.45, P < 0.001) cigarettes. A higher score of negative attitudes toward smoking was associated with significantly lower odds of regular and electronic cigarettes use (AOR = 0.75 and 0.78, P < 0.001). A higher affordability score was associated with significantly lower odds of using electronic cigarettes (AOR = 0.90, P = 0.004). The fixed effect variables explained 23.9% of the random variation among countries in using regular cigarettes and 32.1% in using electronic cigarettes.
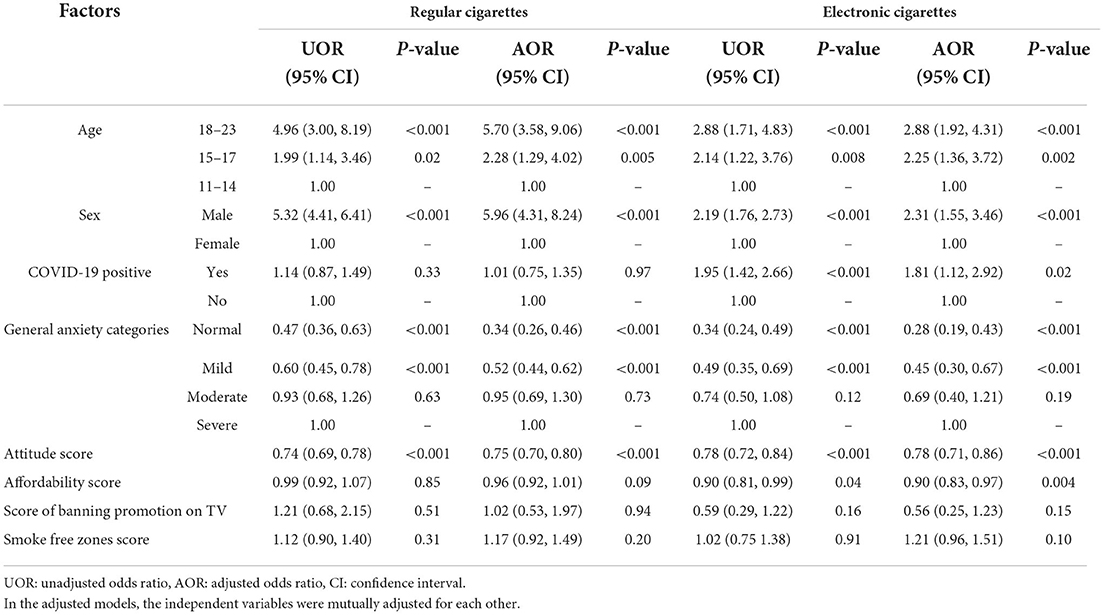
Table 3. Factors associated with using cigarettes and electronic cigarettes in AYA in 25 countries (N = 6,989).
Variance estimate of unconditional model for regular cigarettes = 0.67 and for electronic cigarettes = 1.217, full model variance estimate = 0.51 and 0.826, respectively. Regarding goodness of fit, the deviance decreased from 40818.4 in the unconditional to 37424.7 in the conditional model where using regular cigarettes was the dependent variable and from 44525.3 to 42732.0 where using electronic cigarettes was the dependent variable with significant differences in both cases indicating improvement in model fit after adding the fixed effect variables.
Discussion
The study showed that most current users of regular and electronic cigarettes reported either the same or lower level of use as before the pandemic. Older participants and males had higher odds of using regular and electronic cigarettes. Those with normal or mild anxiety and with negative attitude toward smoking had lower odds of reporting smoking. Participants with a history of COVID-19 infection and those from countries where electronic cigarettes were more affordable had higher odds of using electronic cigarettes. The components of COM-B were, thus, associated with the use of regular and electronic cigarettes.
One of the strengths of this study is the evidence generated on regular and electronic cigarettes use among AYA in several countries. Previous studies on using regular and electronic cigarettes during the pandemic had minor focus on AYA (30–32) or were restricted to only one country (16, 33–36) making it difficult to compare countries with different tobacco control policies. The use of the COM-B model as a conceptual framework for the study allowed the identification of individual and country-level factors that may be associated with smoking.
Despite the unique perspective offered by the present study, there were some limitations. First, there may be a social desirability bias in reporting smoking with potential for underestimating the level of smoking regular and electronic cigarettes. Second, the survey did not distinguish between the use of nicotine-containing and non-nicotine containing electronic cigarettes and this needs to be addressed in future studies. Third, because of COVID-19, data were collected electronically. The convenience sample may, therefore, not be representative of the profile of AYA in the countries included in the study as participants' recruitment was skewed toward those with access to the internet. Fourth, the study is cross-sectional and cannot prove causality; it can only suggest associations. Fifth, the attitude score was based on five items and this may possibly explain the relatively low level of internal consistency indicated by the Cronbach alpha (37) which might have also been reduced by the presence of more than dimension in the items assessing general attitude toward smoking and attitude toward the association of smoking and COVID-19 infection. Future studies assessing attitudes toward smoking may need to include a greater number of items to increase consistency. Despite the study limitations, there were important highlights from the study.
First, we found that a history of COVID-19 infection was associated with higher odds of using electronic cigarettes but not using regular cigarettes. This agrees with Gaiha et al. (16) who reported a significant association between smoking electronic cigarettes and history of COVID-19 infection. A recent meta-analysis of patients hospitalized for COVID-19 found no significant association between COVID-19 infection and smoking (38). However, this disagrees with some population-based studies (39). One possible explanation may be that AYA with a history of COVD-19 infection may opt to use electronic than regular cigarettes with the understanding that it would have less effect on their health. There are few studies that highlighted the interaction between smoking and COVID-19 (17). However, the association between electronic cigarette smoking and COVID-19 infection especially in AYA needs to be explored further. Electronic cigarettes smoking is associated with elevated chemokine CXCL8, extracellular matrix proteins and markers of mitochondrial dysfunction which decreases cellular viability and integrity. It also interferes with cellular mechanisms resulting in increased oxidative stress, inflammation, infections and airway remodeling in the lungs of device users (3, 38, 40–43). What is not known is whether this damage is worse for electronic cigarette smokers than it is for regular cigarette smokers; or if the damage is worse in AYA who smoke electronic cigarettes than it is for older smokers. These knowledge gaps need to be explored further. The study finding suggests that AYA who smoke electronic cigarettes should be counseled on the risk of contracting infection when sharing vaping devices (44).
Second, participants with severe anxiety had higher odds of using regular and electronic cigarettes. This agrees with studies reporting higher frequency of smoking to cope with stresses caused by the COVID-19 pandemic and the associated precautionary measures (45–47). These studies, however, mainly focused on adults and elderlies. We highlight that AYA equally need attention for psychological stress management even if they are less likely to have COVID-19 related deaths. Support provided to AYA should focus on helping them cope and maximize their resilience against surrounding stressors.
Third, less affordability of electronic cigarettes was associated with lower odds of smoking. Affordability is relevant for AYA because they may be less financially independent than adults (48). The rapid increase in electronic cigarette smoking among adolescence was associated with its affordability and availability (49–51). Further taxation of cigarettes during stressful events may be suggested to help reduce the risk of AYA using cigarettes to cope with stresses. However, it is important to note that capability and motivation factors may have stronger association with using electronic cigarettes than opportunity factors based on the present findings.
Fourth, banning tobacco promotion on television seemed to have a strong but non-significant negative association with using electronic cigarettes in the present study. This may be attributed to the impact of role modeling (52) on AYA.
The findings have implication for controlling tobacco smoking in AYA. At the individual level, educating AYA to manage stress without resorting to smoking, and promoting a negative attitude toward smoking may help control smoking. At a country level, it is important to ensure greater financial obstacles so that AYA are less able to afford tobacco products and to reduce the promotion of tobacco through advertisements in addition to exploring other policies. Adopting the MPOWER policies can help control smoking during the pandemic. The MPOWER package includes monitoring tobacco use and prevention policies (M), protecting populations from tobacco (P), offering help to quit tobacco (O), warning about the risks associated with tobacco (W), enforcing bans on tobacco promotion (E) and raising taxes on tobacco products (R). The package was created by the World Health Organization to help governments address the tobacco pandemic based on the framework convention for tobacco control (18). Enforcing the components of MPOWER may help reshape the surrounding environment, thus reducing the opportunities to engage in smoking as a behavior. The evidence generated in the present study supports the adoption of the MPOWER strategies to control smoking associated with stressful events. Further studies are needed to assess the impact of other MPOWER strategies on smoking, and smoking prevalence in AYA compared to other age groups.
Conclusion
The higher odds for AYA to smoke in association with anxiety highlight the need for action to reduce the capability, opportunity and motivation of AYA to smoke during stressful events. The adoption of the MPOWER strategies may provide the framework for governments to address the structural determinants of smoking thereby supporting global tobacco control efforts.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Research Ethics Committee of the Faculty of Dentistry, King Abdulaziz University, Jeddah Saudi Arabia. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
HS, WA, MQ, and ME: conceptualization. MQ and ME: formal analysis. HS, MQ, NAA, JA, NQ, SQ, AH, NM, RO, NA-K, RJ, AB, MS, MF, OA, NG, RA, NAM, HE, MA, BS, RM, NA, SS, SA, and ME: investigation. HS, MQ, and ME: methodology. HS, WA, and ME: project administration and writing—original draft. HS, WA, NA-K, MF, and ME: writing—review & editing. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to acknowledge Zahid Imran and Shaween Al-Tabany for collecting data. We also want to thank EditWorld for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.875801/full#supplementary-material
References
1. American Academy of Pediatrics. Adolescent Sexual Health. Available online at: https://www.aap.org/en/patient-care/adolescent-sexual-health/ (accessed April 10, 2021).
2. Agarwal A, Garg C, Ganesh MS, Reddy S. Molecular mechanisms of tobacco induced oral and oropharyngeal cancer: results of a tissue microarray and immunohistochemistry-based study from a tertiary cancer center in India. Indian J Pathol Micr. (2020) 63:7–12. doi: 10.4103/IJPM.IJPM_783_18
3. Zhang Y, He J, He B, Huang R, Li M. Effect of tobacco on periodontal disease and oral cancer. Tob Induc Dis. (2019) 17:40. doi: 10.18332/tid/106187
4. Reuther WJ, Brennan PA. Is nicotine still the bad guy? Summary of the effects of smoking on patients with head and neck cancer in the post-operative period and the uses of nicotine replacement therapy in these patients. Br J Oral Maxillofac Surg. (2014) 52:102–5. doi: 10.1016/j.bjoms.2013.11.003
5. Pisinger C, Døssing M. A systematic review of health effects of electronic cigarettes. Prev Med. (2014) 69:248–60. doi: 10.1016/j.ypmed.2014.10.009
6. Sonnenberg A, Hüsmert N. Effect of nicotine on gastric mucosal blood flow and acid secretion. Gut. (1982) 23:532–5. doi: 10.1136/gut.23.6.532
7. Mishra A, Chaturvedi P, Datta S, Sinukumar S, Joshi P, Garg A. Harmful effects of nicotine. Indian J Med Paediatr Onco. (2015) 36:24–31. doi: 10.4103/0971-5851.151771
8. Michie S, van Stralen MM, West R. The behavior change wheel: a new method for characterizing and designing behavior change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
9. Michie S, Atkins L, West R. The Behavior Change Wheel: A Guide to Designing. London: Silverback Publishing (2014).
10. Michie S, West R. Behavior change theory and evidence: a presentation to government. Health Psychol Rev. (2013) 7:1–22. doi: 10.1080/17437199.2011.649445
11. Minian N, Corrin T, Lingam M, de Ruiter WK, Rodak T, Taylor VH, et al. Identifying contexts and mechanisms in multiple behavior change interventions affecting smoking cessation success: a rapid realist review. BMC Public Health. (2020) 20:918. doi: 10.1186/s12889-020-08973-2
12. West R, Michie S. A Brief Introduction to the com-b Model of Behavior and the Prime Theory of Motivation. Qeios. doi: 10.32388/WW04E6
13. Buckner JD, Vinci C. Smoking and social anxiety: the roles of gender and smoking motives. Addict Behav. (2013) 38:2388–91. doi: 10.1016/j.addbeh.2013.03.007
14. Evatt DP, Kassel JD. Smoking, arousal, and affect: the role of anxiety sensitivity. J Anxiety Disord. (2010) 24:114–23. doi: 10.1016/j.janxdis.2009.09.006
15. Moylan S, Jacka FN, Pasco JA, Berk M. How cigarette smoking may increase the risk of anxiety symptoms and anxiety disorders: a critical review of biological pathways. Brain Behav. (2013) 3:302–26. doi: 10.1002/brb3.137
16. Gaiha SM, Cheng J, Halpern-Felsher B. Association between youth smoking, electronic cigarette use, and covid-19. J Adolesc Health. (2020) 67:519–23. doi: 10.1016/j.jadohealth.2020.07.002
17. Vardavas CI, Nikitara K. Covid-19 and smoking: a systematic review of the evidence. Tob Induc Dis. (2020) 18:20. doi: 10.18332/tid/119324
18. World Health Organization. Who Framework Convention on Tobacco Control. Available online at: https://www.who.int/fctc/text_download/en/ (accessed October 1, 2021).
19. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. (2001) 79:373–4.
20. World Health Organization. Who Global Report on Trends in Prevalence of Tobacco Use 2000–2025, Third Edition. (2019). Available online at: https://www.who.int/publications/i/item/who-global-report-on-trends-in-prevalence-of-tobacco-use-2000-2025-third-edition (accessed April 10, 2021).
21. Nemes S, Jonasson JM, Genell A, Steineck G. Bias in odds ratios by logistic regression modeling and sample size. BMC Med Res Methodol. (2009) 9:56. doi: 10.1186/1471-2288-9-56
22. Sarich P, Cabasag CJ, Liebermann E, Vaneckova P, Carle C, Hughes S, et al. Tobacco smoking changes during the first pre-vaccination phases of the covid-19 pandemic: a systematic review and meta-analysis. EClinicalMedicine. (2022) 47:101375. doi: 10.1016/j.eclinm.2022.101375
23. Centers for Disease Control Prevention. Global Youth Tobacco Survey (Gyts) — Overview. Available online at: https://nccd.cdc.gov/GTSSDataSurveyResources/Ancillary/Documentation.aspx?SUID=1&DOCT=1 (accessed April 10, 2021).
24. Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the generalized anxiety disorder screener (Gad-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
25. Islam MS, Rahman ME, Moonajilin MS, van Os J. Prevalence of depression, anxiety and associated factors among school going adolescents in Bangladesh: findings from a cross-sectional study. PLoS ONE. (2021) 16:e0247898. doi: 10.1371/journal.pone.0247898
26. Mossman SA, Luft MJ, Schroeder HK, Varney ST, Fleck DE, Barzman DH, et al. The generalized anxiety disorder 7-item scale in adolescents with generalized anxiety disorder: signal detection and validation. Ann Clin Psychiatry. (2017) 29:227–34a.
27. Yusoff MSB. Abc of content validation and content validity index calculation. Edu Med J. (2019) 11:49–54. doi: 10.21315/eimj2019.11.2.6
28. Hardin AP, Hackell JM. Age limit of pediatrics. Pediatrics. (2017) 140:1–3. doi: 10.1542/peds.2017-2151
29. World Health Organization. Who Report on the Global Tobacco Epidemic 2021: Addressing New and Emerging Products. Available online at: https://www.who.int/teams/health-promotion/tobacco-control/global-tobacco-report-2021 (accessed October 1, 2021).
30. Ferastraoaru D, Hudes G, Jerschow E, Jariwala S, Karagic M, de Vos G, et al. Eosinophilia in asthma patients is protective against severe covid-19 illness. J Allergy Clin Immunol Pract. (2021) 9:1152–62.e3. doi: 10.1016/j.jaip.2020.12.045
31. Gendall P, Hoek J, Stanley J, Jenkins M, Every-Palmer S. Changes in tobacco use during the 2020 covid-19 lockdown in New Zealand. Nicotine Tob Res. (2021) 23:866–71. doi: 10.1093/ntr/ntaa257
32. Rebollar Álvarez A, Nuez Vicente C, Lozano Polo A, Pérez Ríos M, Pola Ferrández E, Furió Martínez AM, et al. [Tobacco use in Spain during covid-19 lockdown: an evaluation through social media.]. Rev Esp Salud Publica. (2021) 95:1–11.
33. Chen DT, Kyriakos CN. Cigarette and E-cigarettes dual users, exclusive users and covid-19: findings from four UK birth cohort studies. Int J Environ Res Public Health. (2021) 18:1–12. doi: 10.3390/ijerph18083935
34. Ferrante G, Camussi E, Piccinelli C, Senore C, Armaroli P, Ortale A, et al. Did social isolation during the Sars-CoV-2 epidemic have an impact on the lifestyles of citizens? Epidemiol Prev. (2020) 44(5–6 Suppl 2):353–62. doi: 10.19191/ep20.5-6.S2.137
35. Hopkins DB, Al-Hamdani M. Young Canadian E-cigarette users and the covid-19 pandemic: examining vaping behaviors by pandemic onset and gender. Front Public Health. (2020) 8:620748. doi: 10.3389/fpubh.2020.620748
36. Kreslake JM, Simard BJ, O'Connor KM, Patel M, Vallone DM, Hair EC. E-cigarette use among youths and young adults during the covid-19 pandemic: United States, 2020. Am J Public Health. (2021) 111:1132–40. doi: 10.2105/AJPH.2021.306210
37. Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. (2011) 2:53–5. doi: 10.5116/ijme.4dfb.8dfd
38. Farsalinos K, Niaura R, Le Houezec J, Barbouni A, Tsatsakis A, Kouretas D, et al. Editorial: nicotine and Sars-CoV-2: covid-19 may be a disease of the nicotinic cholinergic system. Toxicol Rep. (2020) 7:658–63. doi: 10.1016/j.toxrep.2020.04.012
39. Haddad C, Bou Malhab S, Sacre H, Salameh P. Smoking and covid-19: a scoping review. Tob Use Insights. (2021) 14:1179173x21994612. doi: 10.1177/1179173X21994612
40. Guan W-J, Ni Z-Y, Hu Y, Liang W, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
41. McAlinden KD, Eapen MS, Lu W, Chia C, Haug G, Sohal SS. Covid-19 and vaping: risk for increased susceptibility to Sars-CoV-2 infection? Eur Clin Respir J. (2020) 56:2001645. doi: 10.1183/13993003.01645-2020
42. Patanavanich R, Glantz SA. Smoking is associated with covid-19 progression: a meta-analysis. Nicotine Tob Res. (2020) 22:1653–6. doi: 10.1093/ntr/ntaa082
43. Tizabi Y, Getachew B, Copeland RL, Aschner M. Nicotine and the nicotinic cholinergic system in Covid-19. FEBS J. (2020) 287:3656–63. doi: 10.1111/febs.15521
44. Majmundar A, Allem JP, Cruz TB, Unger JB. Public health concerns and unsubstantiated claims at the intersection of vaping and covid-19. Nicotine Tob Res. (2020) 22:1667–8. doi: 10.1093/ntr/ntaa064
45. García-Álvarez L, Fuente-Tomás L, Sáiz PA, García-Portilla MP, Bobes J. Will changes in alcohol and tobacco use be seen during the covid-19 lockdown? Adicciones. (2020) 32:85–9. doi: 10.20882/adicciones.1546
46. Rogers AH, Shepherd JM, Garey L, Zvolensky MJ. Psychological factors associated with substance use initiation during the covid-19 pandemic. Psychiatry Res. (2020) 293:113407. doi: 10.1016/j.psychres.2020.113407
47. Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during covid-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. (2020) 17:1–13. doi: 10.3390/ijerph17114065
48. Xiao JJ, Chatterjee S, Kim J. Factors associated with financial independence of young adults. Int J Consum Stud. (2014) 38:394–403. doi: 10.1111/ijcs.12106
49. Fauzi R, Areesantichai C. Factors associated with electronic cigarettes use among adolescents in Jakarta, Indonesia. J Health Res. (2020). doi: 10.1108/JHR-01-2020-0008
50. Hrywna M, Bover Manderski MT, Delnevo CD. Prevalence of electronic cigarette use among adolescents in New Jersey and association with social factors. JAMA Netw Open. (2020) 3:e1920961. doi: 10.1001/jamanetworkopen.2019.20961
51. Perikleous EP, Steiropoulos P, Paraskakis E, Constantinidis TC, Nena E. E-cigarette use among adolescents: an overview of the literature and future perspectives. Front Public Health. (2018) 6:86. doi: 10.3389/fpubh.2018.00086
Keywords: smoking, anxiety, MPOWER, adolescents, young adults
Citation: Sabbagh HJ, Abdelaziz W, Quritum M, AlKhateeb NA, Abourdan J, Qureshi N, Qureshi S, Hamoud AHN, Mahmoud N, Odeh R, Al-Khanati NM, Jaber R, Balkhoyor AL, Shabi M, Folayan MO, Alade O, Gomaa N, Alnahdi R, Mahmoud NA, El Wazziki H, Alnaas M, Samodien B, Mahmoud RA, Abu Assab N, Saad S, Alhachim SG and El Tantawi M (2022) Cigarettes' use and capabilities-opportunities-motivation-for-behavior model: a multi-country survey of adolescents and young adults. Front. Public Health 10:875801. doi: 10.3389/fpubh.2022.875801
Received: 15 February 2022; Accepted: 27 June 2022;
Published: 22 July 2022.
Edited by:
Sheikh Alif, Monash University, AustraliaReviewed by:
Haewon Byeon, Inje University, South KoreaDaniel Rodriguez, La Salle University, United States
Copyright © 2022 Sabbagh, Abdelaziz, Quritum, AlKhateeb, Abourdan, Qureshi, Qureshi, Hamoud, Mahmoud, Odeh, Al-Khanati, Jaber, Balkhoyor, Shabi, Folayan, Alade, Gomaa, Alnahdi, Mahmoud, El Wazziki, Alnaas, Samodien, Mahmoud, Abu Assab, Saad, Alhachim and El Tantawi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heba Jafar Sabbagh, aHNhYmJhZ2hAa2F1LmVkdS5zYQ==
 Heba Jafar Sabbagh
Heba Jafar Sabbagh Wafaa Abdelaziz2
Wafaa Abdelaziz2 Nada AbuBakr AlKhateeb
Nada AbuBakr AlKhateeb Joud Abourdan
Joud Abourdan Ahmed H. N. Hamoud
Ahmed H. N. Hamoud Nada Mahmoud
Nada Mahmoud Nuraldeen Maher Al-Khanati
Nuraldeen Maher Al-Khanati Abdulrahman Loaie Balkhoyor
Abdulrahman Loaie Balkhoyor Morenike Oluwatoyin Folayan
Morenike Oluwatoyin Folayan Noha Gomaa
Noha Gomaa Nawal A. Mahmoud
Nawal A. Mahmoud Bahia Samodien
Bahia Samodien Nour Abu Assab
Nour Abu Assab Sherin Saad
Sherin Saad Sondos G. Alhachim
Sondos G. Alhachim Maha El Tantawi
Maha El Tantawi