
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 15 June 2022
Sec. Aging and Public Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.869239
Background: Disability and medical expenses caused by musculoskeletal disorders in China had a great impact on the global health and economy. Rehabilitation is essential for dealing with musculoskeletal disorders. However, China's musculoskeletal rehabilitation needs remain unknown. This study aimed to examine the secular trends for musculoskeletal rehabilitation needs in China from 1990 to 2030.
Methods: Data on musculoskeletal rehabilitation needs were extracted from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) repository. Estimated annual percentage changes (EAPCs) were calculated to reflect fluctuations in the age-standardized rates. The Bayesian age-period-cohort models were used to project rehabilitation needs.
Results: The number of prevalent cases and years lived with disability (YLD) counts in need of musculoskeletal rehabilitation increased greatly in China from 1990 to 2019. There will be 465.9 million Chinese people in need of rehabilitation, with the age-standardized prevalence rate increasing to 21,151.0 [2.5–97.5% predictive interval (95% PI) 14,872.6–27,429.3] per 100,000 persons in 2030. Similarly, the YLD counts will increase to 40.1 million, with the age-standardized YLD rate increasing to 1,811.2 (95% PI 1,232.5–2,390.0) per 100,000 persons in 2030.
Conclusions: Increasing trends in musculoskeletal rehabilitation needs were found from 1990 to 2019, which will be anticipated through 2030. Rehabilitation is suggested to be integrated into primary care settings.
According to the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2017, musculoskeletal disorders become one of the three leading contributors to years lived with disability (YLDs) in China (1). Musculoskeletal disorders cause physical impairment, psychological incapacity, and organizational dysfunction, which lead to productivity reduction and high medical costs, placing great health and financial burdens on individuals, communities, and societies (1, 2).
Rehabilitation is essential for relieving pain, improving physical mobility, and strengthening psychological functioning (3, 4). Moreover, rehabilitation helps to reduce health expenditure by avoiding or shortening hospital stay (5). The profound disease and economic burdens caused by musculoskeletal disorders call for appropriate rehabilitation provision. It is necessary to have a deep understanding of musculoskeletal rehabilitation needs before health service planning and targeted program interventions.
The GBD 2019 study comprehensively analyses the prevalence, incidence, and YLDs of 369 diseases and injuries in 204 countries and territories between 1990 and 2019. Standardized methods for data screening, cleaning, and generation were reported in the previous GBD studies (6–8). Briefly, the GBD project inputs data from censuses, disease registries, vital statistics, civil registration, satellite monitors, health service records, and other sources (6–8). Data bias was examined and adjusted by cross-validation using the GBD's Bayesian meta-regression tool, DisMod-MR 2.1. The estimates in the GBD project were updated annually by adding newly available data and using more appropriate methodologies (6–8).
Low back pain (International Classification of Disease [ICD]-10 code M54.3-54.5, and ICD-9 code 724) is pain referred to the low back which continues for 1 day or longer (6). Neck pain (ICD-10 code M54.2 and ICD-9 code 723.1) is pain referred to the neck that lasts for at least 1 day (6). Osteoarthritis (ICD-10 code M16-19 and ICD-9 code 715), is the most common type of arthritis, presenting as long-term inflammation, malfunction, and anatomical damages in the joints (6). Rheumatoid arthritis (ICD-10 codes M05-08 excluding M07 and ICD-9 codes 714.0–714.9) refers to a systemic autoimmune dysfunction that leads to pain, swelling, and shape changes in joints and can concur with multiple manifestations (6). For estimating rehabilitation needs, seven health conditions, namely, low back pain, neck pain, osteoarthritis, rheumatoid arthritis, fractures, amputation, and other injuries, which caused the largest number of YLDs and rehabilitation was the primary management strategy, were selected in the GBD project (6). The selection process of health conditions used a stepwise method. First, 20 health conditions that resulted in the most numbers of YLDs were identified. Second, only those conditions for which rehabilitation was the necessary and key intervention was retained. Subsequently, a primary list was reviewed and discussed by professionals invited by the World Health Organization. Lastly, the list was modified if other health conditions necessitated rehabilitation and needed to be included (6). Details on the process for estimating the rehabilitation needs were reported in a previous study (6).
To our knowledge, only one study has provided an overall view of musculoskeletal rehabilitation needs at the global and regional levels using data from the GBD study 2019 (6). Although rehabilitation needs were calculated, this study did not analyze secular changes of musculoskeletal rehabilitation needs. Therefore, the shifting patterns of musculoskeletal rehabilitation needs remain unclear. The secular trends over the past decades represent changing patterns of disease epidemiology, and the disease projection in the following decades will also be valuable for disease prevention and the design of coping strategies (9). Disability and medical expenses caused by musculoskeletal disorders in China could have a great impact on global health and economy. Therefore, this study aimed to (1) examine the secular trends for prevalence and YLDs of musculoskeletal rehabilitation needs by sex, age, and category in China from 1990 to 2019, (2) assess the associations between musculoskeletal rehabilitation needs and China's societal development, and (3) project China's musculoskeletal rehabilitation needs to 2030.
This is a cross-sectional study using secondary data.
In this cross-sectional study, we obtained data on prevalence, YLDs, and age-standardized prevalence and YLD rates of musculoskeletal disorders in need of rehabilitation in 19 countries of the G20 excluding the European Union from 1990 to 2019 by age, sex, year, and health condition from the GBD repository (https://vizhub.healthdata.org/rehabilitation/) (10). We included all ages of participants from both sexes. In the GBD project, the 95% uncertainty interval (UI) for each estimate was determined by the 25th and 975th draws in the 1,000 ordered draws, respectively. To assess the associations between musculoskeletal rehabilitation needs and societal development in China, we obtained the sociodemographic index from the GBD project. The sociodemographic index is a composite indicator, which incorporates income per head, total fertility rates younger than 25 years, and the average duration of educational attainment in individuals aged above 15 years (11). To project rehabilitation needs, we also retrieved rehabilitation need data by health condition, 5-year age groups (from 0–4 to 85 years, 18 age groups in total), and year between 1990 and 2019 from the GBD repository. The Chinese population data by 5-year age groups (from 0–4 to 85 years, 18 age groups in total), and by year between 1990 and 2030 were extracted from the United Nations Department of Economics and Social Affairs Population Dynamics (https://population.un.org/wpp/Download/Standard/Population/) (12).
In this study, the estimated annual percentage change (EAPC) and its 95% confidence interval (CI) were generated to reflect fluctuations in the age-standardized rate (9, 13). The lower bound of an EAPC greater than zero indicates that the age-standardized rate increases, whereas the upper bound of an EAPC less than zero suggests that the age-standardized rate decreases and the 95% CI of an EAPC including zero supports that the age-standardized rate remains unchanged during the study period (14).
We used the World (WHO 2000–2025) Standard population to standardize the prevalence and YLDs in need of rehabilitation (15). In the previous studies, the age-period-cohort (APC) model, Joinpoint regression model, smooth spline model, generalized additive model, and Poisson regression model have been widely used in disease trend analyses or projections (9, 16–18). The prevalence and YLDs data in China were divided into two parts according to their years (data in the year 1990–2013, and 2014–2019). The training data (data in the year 1990–2013) were used to train the Bayesian age-period-cohort (BAPC) model, Joinpoint regression model, smooth spline model, generalized additive model, and Poisson regression model. The predicted results were compared with those in the testing data (data in the year 2014–2019). The mean absolute percentage error (%) = was estimated to evaluate model accuracy (9), where n, yo, and yp presented the sample size, observed values, and predicted values, respectively. As the mean absolute percentage errors for both prevalent cases and YLDs in the BAPC model were the smallest (Supplementary Figure 1) among these five models, the BAPC model was selected to project the prevalence and YLDs in need of rehabilitation through 2030.
In an APC model, for age group i in period j, the logarithm of the number of disease cases λij is calculated by:
where μ, αi, βj, and γk refer to the intercept, age, period, and cohort effects, respectively (9, 19, 20). The cohort index k is calculated based on the age group index i, period index j, and the ratio of year span of each age group to period. In this study, the age index i ranged from 1 to I = 18, and the ratio of year span of each age group to period is equal to 5. Therefore, k = 5*(18−i)+j. In this study, the BAPC model with integrated nested Laplace approximations was used to predict rehabilitation needs through 2030 (20). For smoothing consideration, independent mean-zero normal distributions on the second differences of all time effects were assumed in a BAPC model (20). In particular, the age effects are defined as:
where kα is the variance parameter (20). To address the possible overdispersion, for a specific age group i, with a t period(s) in the following year(s), an independent random effect zij ~ N (0) was added to the model (1):
(20).
In a BAPC model, the period effect at period i + 1 is assumed to have a distribution as follows:
(20).
Data analyses were conducted in RStudio Version 1.3.1093 and R packages ggplot2 (21), Rcan (22), BAPC (23), and INLA (www.r-inla.org) (24, 25). The p-values < 0.05 were treated as statistically significant.
In China, the number of prevalent cases of musculoskeletal disorders in need of rehabilitation increased greatly from 186.0 (95% UI 173.7–199.2) million to 322.1 (95% UI 301.7–343.0) million from 1990 to 2019, with a significant increase in YLD counts from 17.6 (95% UI 12.5–23.3) million to 28.1 (95% UI 19.9–38.5) million during the same period. The age-standardized prevalence rate in China decreased from 17,966.3 (95% UI 16,799.9–19,142.9) per 100,000 persons to 17,225.4 (95% UI 16,211.4 to 18,325.4) per 100,000 persons, with an EAPC of −0.10% (95% CI −0.13 to −0.07%) annually. Likewise, age-standardized YLD rate in China decreased from 1707.7 (95% UI 1,225.3–2,269.2) per 100,000 persons to 1,496.8 (95% UI 1073.5–2025.7) per 100,000 persons, with an EAPC of −0.34% (95% CI −0.45 to −0.23%) annually (Table 1). However, there was an overall increase in the rank in terms of age-standardized prevalence rate, from last in 1990 to 18th, ahead of South Africa among 19 countries of the G20 in 2019. Similarly, in terms of age-standardized YLD rate, the rank of China stabilized at 18th, followed by South Africa during the full period (Supplementary Figures 2, 3; Supplementary Table 1).
In both 1990 and 2019, low back pain was the major cause of total prevalent cases among the G20 countries. In 2019, the greatest contributor to total prevalent cases in China was low back pain (28.4%), followed by osteoarthritis (26.7%), neck pain (21.1%), fractures (20.3%), other injuries (12.4%), amputation (8.4%), and rheumatoid arthritis (1.0%). The proportions of prevalent cases by category increased in China, from 0.2% for rheumatoid arthritis to 8.8% for osteoarthritis, except a decrease of 12.1% for low back pain between 1990 and 2019 (Figure 1). The EAPCs increased for fractures (0.31%; 95% CI 0.24–0.39%), other injuries (0.14%; 95% CI 0.04–0.23%), osteoarthritis (0.38%; 95% CI 0.31–0.44%), and rheumatoid arthritis (0.35%; 95% CI 0.02–0.68%), remained stable for neck pain (0.06%; 95% CI −0.01–0.13%) and amputation (−0.03%; 95% CI −0.15–0.08%), and decreased for low back pain (−0.76%; 95% CI −0.82 to −0.71%) (Table 1).
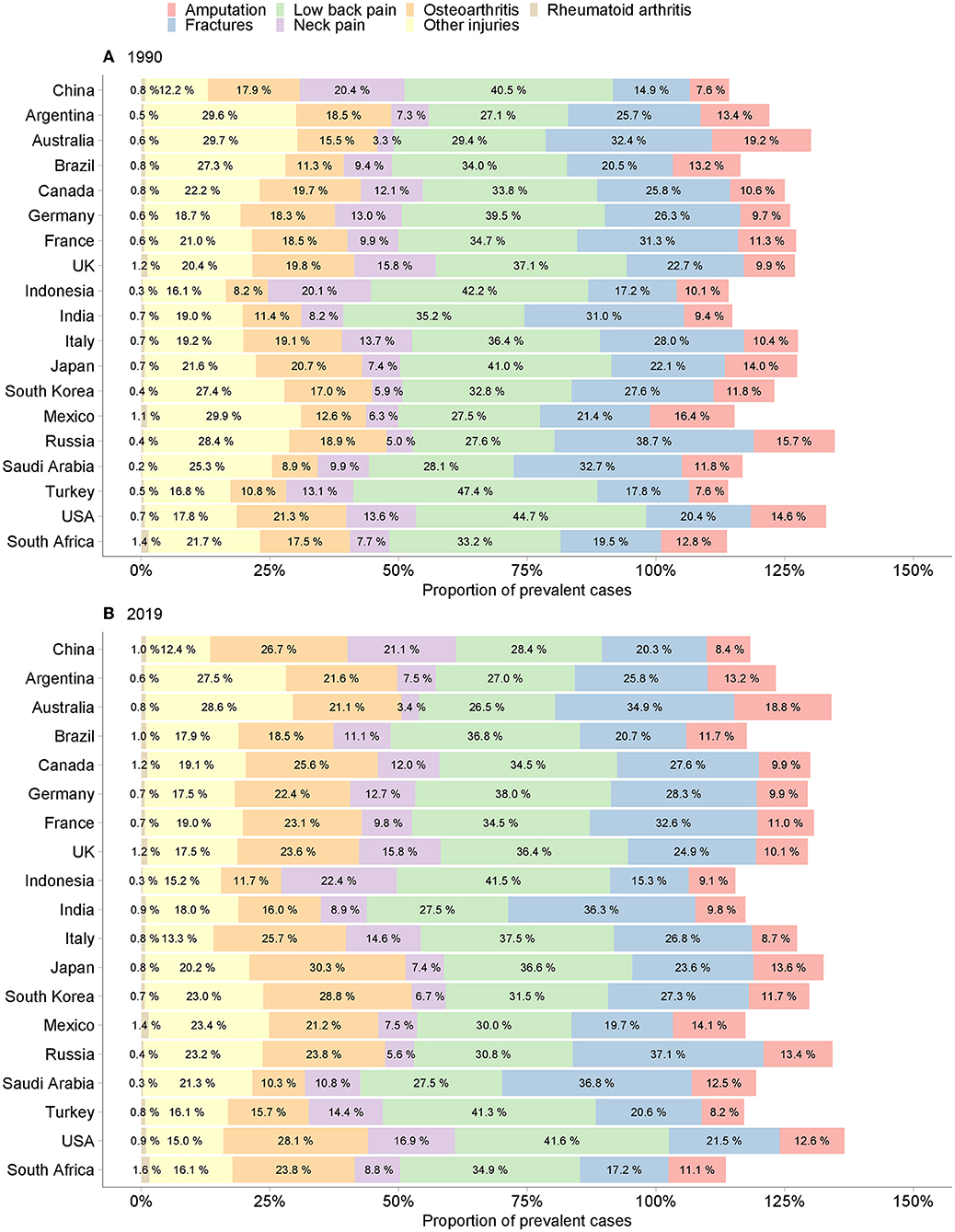
Figure 1. Proportion of prevalent cases of musculoskeletal rehabilitation needs in the G20 countries. (A) 1990. (B) 2019.
Likewise, low back pain was also the main contributor to total YLD counts across the G20 countries. In 2019, low back pain accounted for 36.8% of the total YLD counts, followed by neck pain (24.2%), osteoarthritis (16.8%), fractures (13.4%), other injuries (3.9%), amputation (2.8%), and rheumatoid arthritis (2.0%) in China. From 1990 to 2019, the proportions of YLD counts by category in China increased by 0.5, 2.5, 3.8, and 6.5% for rheumatoid arthritis, neck pain, fractures, and osteoarthritis, but decreased by 0.6, 0.9, and 11.8% for other injuries, amputation, and low back pain, respectively (Supplementary Figure 4). The EAPCs increased for osteoarthritis (0.40%; 95% CI 0.12–0.68%), remained stable for neck pain (0.06%; 95% CI −0.16–0.28%), fractures (0.06%; 95% CI −0.27–0.38%), and rheumatoid arthritis (0.37%; 95% CI −0.40–1.15%), and decreased for low back pain (−0.75%; 95% CI −0.92 to −0.59%), other injuries (−1.01%; 95% CI −1.55 to −0.47%), and amputation (−2.39%; 95% CI −2.99 to −1.79%) (Table 1).
During the entire study period, both age-standardized prevalence and YLD rates of low back pain, neck pain, osteoarthritis, and rheumatoid arthritis were higher in women, whereas those of fractures, other injuries, and amputation were higher in men. The age-standardized prevalence rates increased faster in women for osteoarthritis (0.49%; 95% CI 0.43–0.55%), and other injuries (0.18%; 95% CI 0.08–0.28%) but increased faster in men for fractures (0.45%; 95% CI 0.37–0.52%), and decreased faster in men for low back pain (−0.80%; 95% CI −0.86 to −0.74%) (Supplementary Figure 5). The age-standardized YLD rates decreased faster in women for amputation (−2.65%; 95% CI −3.31 to −1.98%), and other injuries (−1.10%; 95% CI −1.68 to −0.52%), but decreased faster in men for low back pain (−0.79%; 95% CI −0.97 to −0.62%) (Supplementary Figure 6).
Overall, musculoskeletal rehabilitation needs increased with age. Notably, sharp increasing trends in prevalence rates were found in fractures, other injuries, and amputation in people aged 90 years and over. The prevalence rates peaked at 75 years for neck pain and 75–80 years for rheumatoid arthritis in both sexes (Supplementary Figure 7). The trends in YLD rates resembled those of prevalence rates (Supplementary Figure 8).
With increasing sociodemographic index, the age-standardized prevalence rate of low back pain decreased curvilinearly, whereas that of neck pain increased curvilinearly, and that of osteoarthritis increased in a zigzag pattern. The age-standardized prevalence rate of fractures, other injuries, and amputation approached the lowest level when the sociodemographic index increased to 0.57 in 2005. However, the age-standardized prevalence rate of rheumatoid arthritis peaked when the sociodemographic index was 0.66 in 2015 (Figure 2H; Supplementary Tables 2–4). The non-linear associations between the age-standardized YLD rate and the sociodemographic index were in line with those of associations between the age-standardized prevalence rate and the sociodemographic index (Figure 2; Supplementary Tables 2–4).
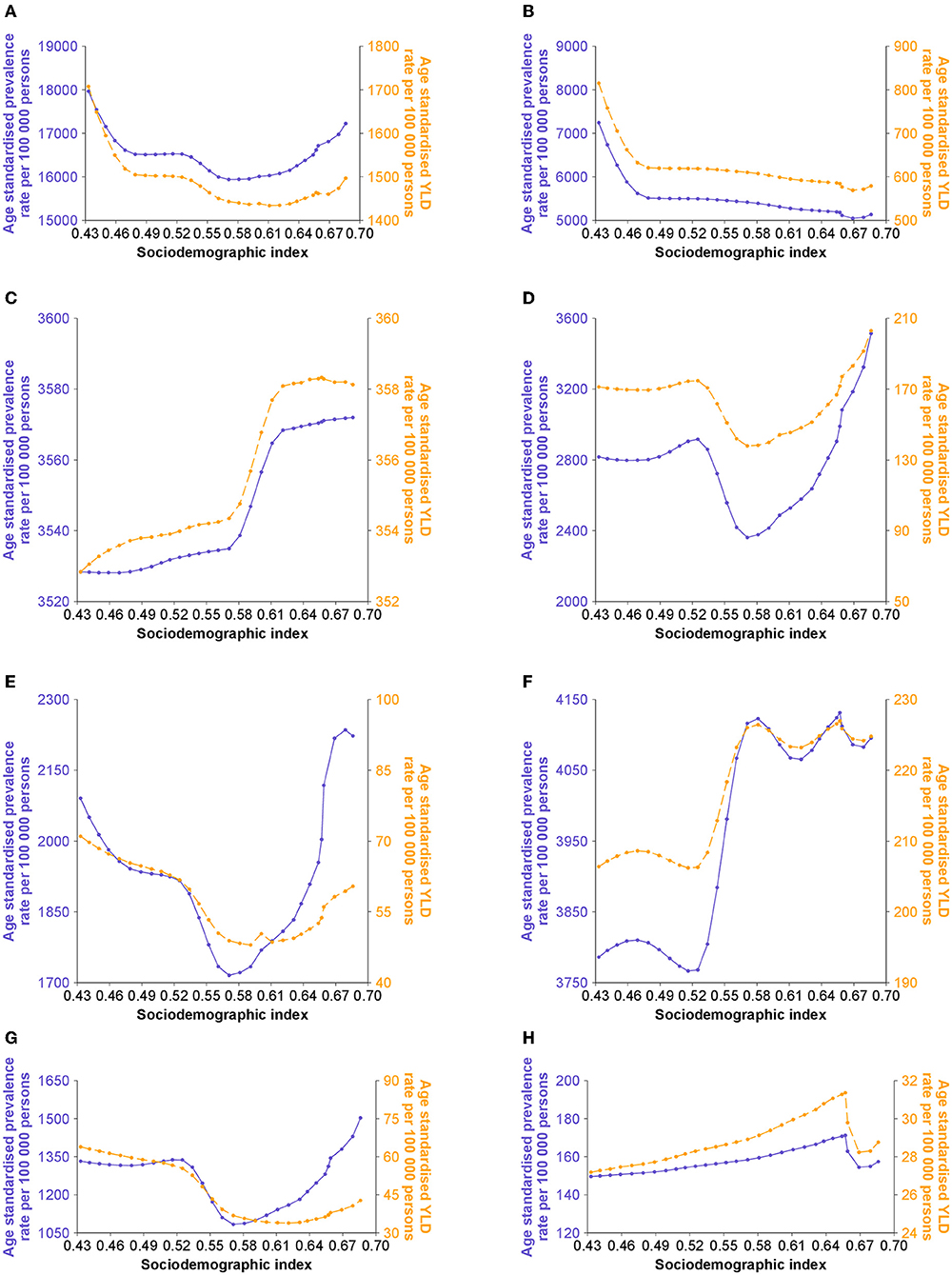
Figure 2. Age-standardized rates of musculoskeletal rehabilitation needs by sociodemographic index in China. (A) Musculoskeletal disorders. (B) Low back pain. (C) Neck pain. (D) Fractures. (E) Other injuries. (F) Osteoarthritis. (G) Amputation. (H) Rheumatoid arthritis.
The number of Chinese people in need of musculoskeletal rehabilitation will increase markedly from 342.0 million in 2020 to 465.9 million in 2030, with the age-standardized prevalence rate increasing from 18,410.7 [2.5–97.5%; predictive interval (95% PI) 17,729.7–19,091.7] per 100,000 persons in 2020 to 21,151.0 (95% PI 14,872.6–27,429.3) per 100,000 persons in 2030, with an EAPC of 1.39% (95% CI 1.26–1.53%). Similarly, the number of YLD counts will increase significantly from 29.7 million in 2020 to 40.1 million in 2030, with the age-standardized YLD rate increasing from 1,595.5 (95% PI 1,535.1–1,656.0) per 100,000 persons in 2020 to 1,811.2 (95% PI 1,232.5–2,390.0) per 100,000 persons in 2030, with an EAPC of 1.27% (95% CI 0.82–1.73%). Between 2020 and 2030, both age-standardized prevalence and YLD rates will increase for low back pain, fractures, and amputation, but will remain stable for neck pain, osteoarthritis, and rheumatoid arthritis (Figure 3; Supplementary Figure 9; Table 2).
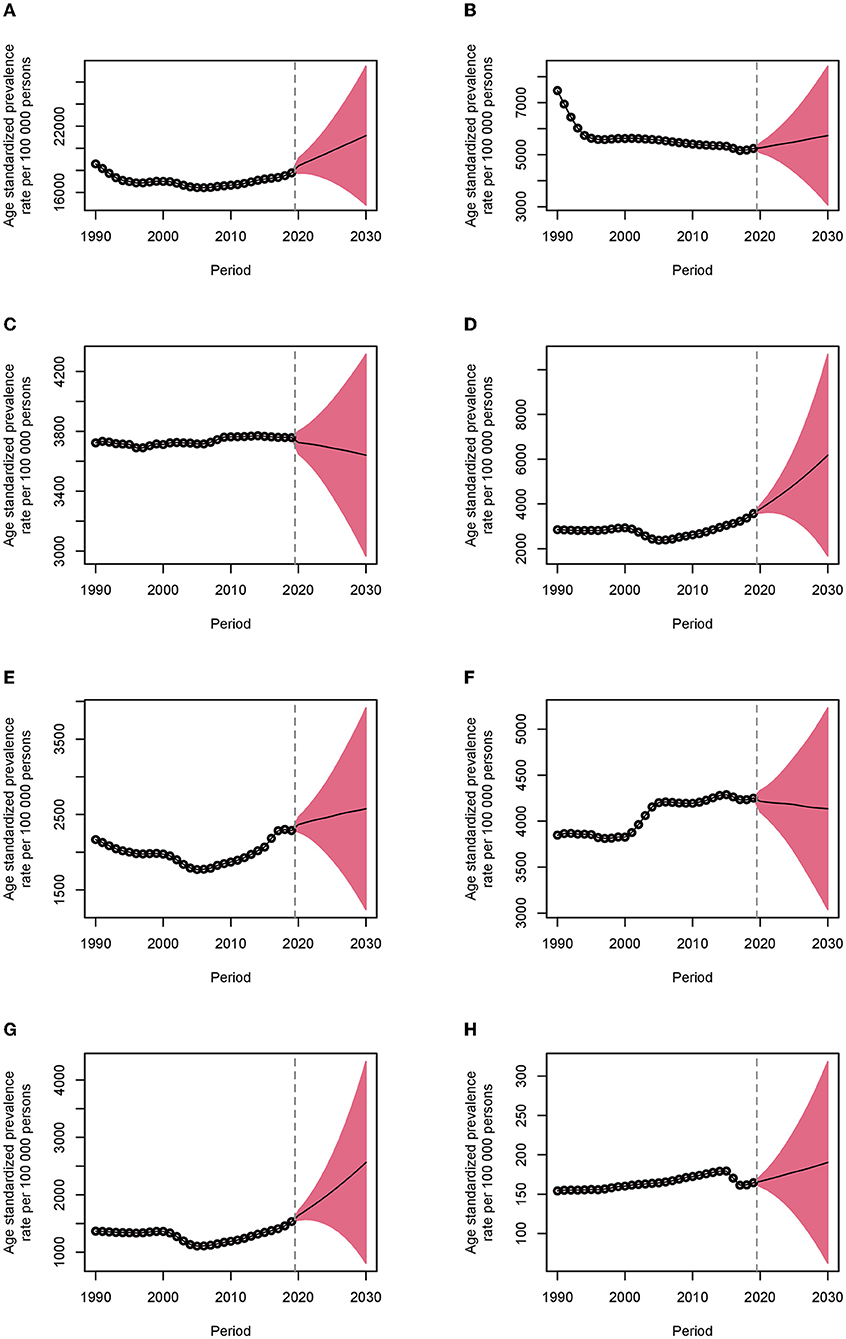
Figure 3. Age-standardized prevalence rates of musculoskeletal rehabilitation needs in China from 1990 to 2030. The dots indicate the observed rates, and the fan plot presents the predicted values with 2.5 and 97.5% quantiles. The solid line indicates the predicted mean values. The vertical dashed line shows when the prediction begins. (A) Musculoskeletal disorders. (B) Low back pain. (C) Neck pain. (D) Fractures. (E) Other injuries. (F) Osteoarthritis. (G) Amputation. (H) Rheumatoid arthritis.
To our knowledge, this is the first study to present secular trends in musculoskeletal rehabilitation needs from the past to the future in China. Between 1990 and 2019, the number of prevalent cases and YLDs of musculoskeletal disorders that would benefit from rehabilitation increased remarkedly in China. Particularly, in 2019, musculoskeletal disorders contributed to 19.14% of total YLD counts (7). In addition, musculoskeletal disorders were ranked second to first among the leading 22 diseases and injuries that caused the largest number of YLD counts (1). The increasing trends were projected to continue through 2030 by using the BAPC models. This could be partly explained by population growth and aging (14). Notably, from 1990 to 2019, the number of Chinese people increased considerably from 1,183.0 to 1,441.9 million, and the number of people aged 65 and older increased greatly from 66.8 to 165.9 million, with its share more than doubling from 5.6 to 11.5% (12). In the same vein, from 2020 to 2030, the Chinese population will grow from 1,447.5 to 1,473.1 million, and the number of people aged 65 and older will increase significantly from 173.7 to 249.2 million, with its share increasing greatly from 12.0 to 16.9% (12).
Particularly, low back pain accounted for ~40% of total YLD counts due to musculoskeletal disorders in 2019. In fact, low back pain was also the primary cause of YLDs in more than 120 countries and the leading contributor to economic burdens globally (26). For example, the US government spends more than US$100 billion annually on treating patients with low back pain (27). Although there were no latest reports on the Chinese medical expenditure on low back pain, given that China has the largest number of people in the world, the medical expenses and economic loss caused by low back pain are expected to be enormous. Furthermore, there were 322.1 million Chinese people with musculoskeletal disorders who would benefit from rehabilitation in 2019, indicating that approximately one in every seven, which will increase to nearly one in every three individuals will benefit from musculoskeletal rehabilitation in 2030. This challenges the common belief that only a few people with specific disabilities need rehabilitation (6).
In terms of both age-standardized prevalence and YLD rates of musculoskeletal disorders, China was ranked from lowest to second-lowest among the G20 countries over the full study period. In addition to the largest population, this could be explained by a more remarkable improvement in life expectancy at birth in China than that in other countries. For example, from 1980 to 2019, life expectancy at birth in China increased significantly from 64.4 to 77.6 years, whereas that in the USA only increased slightly from 74.0 to 78.9 years (11). As such, it is possible that a generally higher proportion of younger people was found in China than that in other countries during the study period. As supported by the World Bank report, the share of people aged 65 and older in the total population was lower in China than that in the UK, the USA, Australia, and Russia from 1990 to 2019 (28). Therefore, age-standardized prevalence and YLD rates of musculoskeletal disorders in China tended to be lower than those in other countries since the burdens of musculoskeletal disorders increase with age (29). In fact, the disease burdens increase with age could not only be found in China but also in all other countries of the G20. Given that rehabilitation needs have increased considerably in the most recent 3 years, and the continuing increasing trends of rehabilitation needs projected by the BAPC models in the following decade, rehabilitation needs in China should not be neglected, and urgent action should be undertaken by the Chinese decision-makers and health professionals.
Sex disparities in rehabilitation needs were also observed. In this study, rehabilitation needs due to fractures, other injuries, and amputation were higher in men, whereas those of low back pain, neck pain, osteoarthritis, and rheumatoid arthritis were higher in women. This phenomenon could be partly attributed to complex traumatic, anatomic, and hormonal effects on the progression of musculoskeletal disorders. For example, men report more rehabilitation needs due to fractures, as men often suffer more serious traumas, such as vehicle accidents, vocational excessive bone loading and recreational injuries (30), although women after menopause are at a higher risk of fractures resulting from reduced bone mass, decreased estrogens, and a higher fall rate (31). However, the impact of sex differed in some countries. For example, men in Turkey and Saudi Arabia have higher rehabilitation needs due to low back pain than women, which was consistent with the previous studies (32, 33). The reason might be that more original studies included in the GBD study 2019 were conducted on the healthcare staff rather than the general population. Therefore, it should be the occupation rather than gender that affects rehabilitation needs because more men might involve in tasks, e.g., transferring patients or lifting objects requiring greater physical demands (33). In addition, men showed higher rehabilitation needs due to osteoarthritis in South Africa, which might be attributed to a higher proportion of included studies that investigated cervical and lumbar spine osteoarthritis because men had a higher risk of osteoarthritis in these sites (34).
Generally, age-standardized prevalence and YLD rates of musculoskeletal orders increased with the sociodemographic index, which was noted in all 19 countries of the G20. Over the last 30 years, rapid development has been observed in the Chinese economy (35). As reported in previous studies, risk factors for musculoskeletal orders, such as sedentary behavior, reduced physical activity, an unhealthy diet, high body mass index, smoking, and alcohol consumption are more common in people with better socioeconomic status (14, 29, 36). Particularly, a growing number of workers spend the majority of their time in the office with less body exercise, resulting in increasing burdens of low back and neck pain (37). Interestingly, an overall negative relationship was observed between age-standardized rates of low back pain and sociodemographic index, which might reveal the combined effects of the risk factors, population growth, and aging (38). Therefore, to manage the disease burdens more effectively, coping strategies should be multisectoral, including counteracting the effects of risk factors, monitoring fertility rates and live births, and tracking mortality and morbidity. Such efforts will help to promote the wellbeing of Chinese people and benefit societal development.
High rehabilitation needs pose a major challenge to Chinese health systems. In China, the primary care settings mainly provide basic clinical treatment and public healthcare (39). However, rehabilitation is often marginalized as a natural process of recovery, rather than an essential resolution to deal with body disabilities (40). One feasible method to meet high musculoskeletal rehabilitation needs is to counter this view and integrate rehabilitation into Chinese primary care settings, in which early rehabilitation can considerably reduce the prevalence and disability of persistent musculoskeletal symptoms. For example, strength training and exercise programs for osteoarthritis can greatly improve joint stability and function (41). To provide better rehabilitation services in primary care, more professional training should be organized for health professionals, such as physicians, nurses, and community health workers to identify rehabilitation needs and deliver rehabilitation care appropriately (6), given that such training is often insufficient (39). Additionally, trained occupational and physical therapists should also be employed to better guide the implementation of interventions (6). To achieve this, the rehabilitation workforce should be given adequate remuneration and opportunities for career promotion. Furthermore, with the help of new technologies, online rehabilitation programs are encouraged to supplement the limited rehabilitation resources and improved the accessibility of rehabilitation services, especially in remote areas (42).
There were several limitations in this study. First, there might be an underestimation of trends in rehabilitation needs, as the understanding and diagnostic criteria for musculoskeletal disorders may have been improved overtime. However, this potential bias was adjusted for during the cause list of diseases mapped to ICD codes. Second, only seven health conditions contributing to the largest number of YLDs and necessitating rehabilitation care were included. However, other categories of musculoskeletal disorders, for example, gout, which might also need rehabilitation services, were excluded. Third, we obtained aggregate data at the national level from the GBD repository, in which data at the subnational level were not available. Therefore, we failed to compare rehabilitation needs among different provinces or between urban and rural areas, which facilitated more specific strategies for rehabilitation initiatives, given that disparities existed in medical resource allocation and health service provision across China (1, 29). Fourth, for the diagnosis of musculoskeletal disorders, although data were adjusted for case definition and outliers were removed, potential overlap might still exist in data from primary healthcare institutions or hospitals. Lastly, to achieve the goals described in the Healthy China 2030 (43), the launch of campaigns focusing on the healthy lifestyles and body fitness in the future may lead to decreases in rehabilitation needs, which may bias our predicted results. Given that we went through rigorous model selection procedures and used data from a relatively long period (1990–2019), this study not only advances our knowledge of the secular trends in musculoskeletal rehabilitation needs but also serves as a baseline for future resource distributions and disease control for China and other countries, as this is the first time to predict rehabilitation needs from the past to the future at the national level.
China's musculoskeletal rehabilitation needs have increased substantially over the last three decades. There will be continuing increasing trends in musculoskeletal rehabilitation needs from 2020 to 2030. Rehabilitation services are suggested to be integrated into Chinese primary care settings.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
NC, DF, and JW interpreted the results. NC drafted the manuscript. DF and JW supervised the study. All authors contributed to the critical revision of the manuscript for important intellectual content and approved the final manuscript as submitted.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the Institute for Health Metrics and Evaluation and its partners for their efforts to make the data accessible to the public.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.869239/full#supplementary-material
APC, age-period-cohort; BAPC, Bayesian age-period-cohort; CI, confidence interval; EAPC, estimated annual percentage change; GBD, Global Burden of Diseases, Injuries, and Risk Factors Study; ICD, International Classification of Disease; UI, uncertainty interval; YLDs, years lived with disability.
1. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
2. Briggs AM, Woolf AD, Dreinhöfer K, Homb N, Hoy DG, Kopansky-Giles D, et al. Reducing the global burden of musculoskeletal conditions. Bull World Health Organ. (2018) 96:366–8. doi: 10.2471/BLT.17.204891
3. de Sire A, Agostini F, Lippi L, Mangone M, Marchese S, Cisari C, et al. Oxygen-ozone therapy in the rehabilitation field: state of the art on mechanisms of action, safety and effectiveness in patients with musculoskeletal disorders. Biomolecules. (2021) 11:356. doi: 10.3390/biom11030356
4. Hayden JA, Wilson MN, Stewart S, Cartwright JL, Smith AO, Riley RD, et al. Exercise treatment effect modifiers in persistent low back pain: an individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br J Sports Med. (2020) 54:1277–8. doi: 10.1136/bjsports-2019-101205
5. Karlsson Å, Berggren M, Gustafson Y, Olofsson B, Lindelöf N, Stenvall M. Effects of geriatric interdisciplinary home rehabilitation on walking ability and length of hospital stay after hip fracture: a randomized controlled trial. J Am Med Dir Assoc. (2016) 17:e9–15. doi: 10.1016/j.jamda.2016.02.001
6. Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease Study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2021) 396:2006–17. doi: 10.1016/S0140-6736(20)32340-0
7. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
8. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
9. Liu Z, Xu K, Jiang Y, Cai N, Fan J, Mao X, et al. Global trend of aetiology-based primary liver cancer incidence from 1990 to 2030: a modelling study. Int J Epidemiol. (2021) 50:128–42. doi: 10.1093/ije/dyaa196
10. Global Global Burden of Disease Collaborative Network Institute for Health Metrics Evaluation. WHO Rehabilitation Need Estimator. (2021). Available online at: https://vizhub.healthdata.org/rehabilitation/ (accessed May 12, 2021).
11. GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1160–203. doi: 10.1016/S0140-6736(20)30977-6
12. United Nations Department of Economics Social Affairs Population Dynamics. World Population Prospects 2019. (2019). Available online at: https://population.un.org/wpp/Download/Standard/Population/ (accessed October 15, 2021).
13. Li X, Cao X, Guo M, Xie M, Liu X. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: systematic analysis for the Global Burden of Disease Study 2017. BMJ. (2020) 370:m3150. doi: 10.1136/bmj.m234
14. Jin Z, Wang D, Zhang H, Liang J, Feng X, Zhao J, et al. Incidence trend of five common musculoskeletal disorders from 1990 to 2017 at the global, regional and national level: results from the Global Burden of Disease Study 2017. Ann Rheum Dis. (2020) 79:1014–22. doi: 10.1136/annrheumdis-2020-217050
15. National Cancer Institute Surveillance Epidemiology End Results Program. World (WHO 2000-2025) Standard. Available online at: https://seer.cancer.gov/stdpopulations/world.who.html (accessed October 16, 2021).
16. Lee TC, Dean CB, Semenciw R. Short-term cancer mortality projections: a comparative study of prediction methods. Stat Med. (2011) 30:3387–402. doi: 10.1002/sim.4373
17. Guido D, Leonardi M, Mellor-Marsá B, Moneta MV, Sanchez-Niubo A, Tyrovolas S, et al. Pain rates in general population for the period 1991-2015 and 10-years prediction: results from a multi-continent age-period-cohort analysis. J Headache Pain. (2020) 21:52. doi: 10.1186/s10194-020-01108-3
18. Nowakowski A, Wojciechowska U, Wieszczy P, Cybulski M, Kamiński MF, Didkowska J. Trends in cervical cancer incidence and mortality in Poland: is there an impact of the introduction of the organised screening? Eur J Epidemiol. (2017) 32:529–32. doi: 10.1007/s10654-017-0291-6
19. Clayton D, Schifflers E. Models for temporal variation in cancer rates. II: age-period-cohort models. Stat Med. (1987) 6:469–81. doi: 10.1002/sim.4780060406
20. Riebler A, Held L. Projecting the future burden of cancer: Bayesian age-period-cohort analysis with integrated nested Laplace approximations. Biom J. (2017) 59:531–49. doi: 10.1002/bimj.201500263
21. Wickham H, Chang W, Henry L, Pedersen TL, Takahashi K, Wilke C, et al. Package ‘ggplot2'. (2021). Available online at: https://cran.r-project.org/web/packages/ggplot2/ggplot2.pdf (accessed June 26, 2021).
22. Laversanne M, Vignat J, Unit CS. Package ‘Rcan'. (2020). Available online at: https://cran.r-project.org/web/packages/Rcan/Rcan.pdf (accessed June 15, 2021).
23. Riebler A, Held L. BAPC Package. (2017). Available online at: https://r-forge.r-project.org/R/?group_id=2054 (accessed June 25, 2021).
24. Rue H, Riebler A, Sørbye SH, Illian JB, Simpson DP, Lindgren FK. Bayesian computing with INLA: a review. Annu Rev Statistics Appl. (2017) 4:395–421. doi: 10.1146/annurev-statistics-060116-054045
25. Rue H, Lindgren F, Niekerk Jv, Krainski E, Fattah EA. R-INLA Project. (2021). Available online at: https://www.r-inla.org/ (accessed July 10, 2021).
26. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
27. Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. (2006) 88 (Suppl. 2):21–4. doi: 10.2106/JBJS.E.01273
28. The World Bank. Population Ages 65 and Above (% of Total Population). (2019). Available online at: https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?end=2019&start=1990 (accessed June 25, 2021).
29. Wu D, Wong P, Guo C, Tam LS, Gu J. Pattern and trend of five major musculoskeletal disorders in China from 1990 to 2017: findings from the Global Burden of Disease Study 2017. BMC Med. (2021) 19:34. doi: 10.1186/s12916-021-01905-w
30. Farr JN, Melton LJ 3rd, Achenbach SJ, Atkinson EJ, Khosla S, Amin S. Fracture incidence and characteristics in young adults aged 18 to 49 years: a population-based study. J Bone Miner Res. (2017) 32:2347–54. doi: 10.1002/jbmr.3228
31. Sànchez-Riera L, Wilson N. Fragility fractures and their impact on older people. Best Pract Res Clin Rheumatol. (2017) 31:169–91. doi: 10.1016/j.berh.2017.10.001
32. Alsiddiky AM, Algarni N, Alluhaidan A. Prevalence and associated factors of low back pain among clinicians of a major referral hospital. Med J Malaysia. (2015) 70:12–7. Available online at: http://www.e-mjm.org/2015/v70n1/low-back-pain.pdf
33. Al Amer HS. Low back pain prevalence and risk factors among health workers in Saudi Arabia: a systematic review and meta-analysis. J Occup Health. (2020) 62:e12155. doi: 10.1002/1348-9585.12155
34. Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. (2005) 13:769–81. doi: 10.1016/j.joca.2005.04.014
35. Bekkers E, Koopman RB, Rêgo CL. Structural change in the Chinese economy and changing trade relations with the world. China Econ Rev. (2021) 65:101573. doi: 10.1016/j.chieco.2020.101573
36. Safiri S, Kolahi AA, Cross M, Hill C, Smith E, Carson-Chahhoud K, et al. Prevalence, deaths, and disability-adjusted life years due to musculoskeletal disorders for 195 countries and territories 1990-2017. Arthritis Rheumatol. (2021) 73:702–14. doi: 10.1002/art.41571
37. Ye S, Jing Q, Wei C, Lu J. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: a cross-sectional study. BMJ Open. (2017) 7:e014914. doi: 10.1136/bmjopen-2016-014914
38. Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. (2020) 8:299. doi: 10.21037/atm.2020.02.175
39. Li X, Lu J, Hu S, Cheng KK, De Maeseneer J, Meng Q, et al. The primary health-care system in China. Lancet. (2017) 390:2584–94. doi: 10.1016/S0140-6736(17)33109-4
40. Xiao Y, Zhao K, Ma ZX, Li X, Qiu YP. Integrated medical rehabilitation delivery in China. Chronic Dis Transl Med. (2017) 3:75–81. doi: 10.1016/j.cdtm.2017.02.003
41. Nguyen C, Lefèvre-Colau MM, Poiraudeau S, Rannou F. Rehabilitation (exercise and strength training) and osteoarthritis: a critical narrative review. Ann Phys Rehabil Med. (2016) 59:190–5. doi: 10.1016/j.rehab.2016.02.010
42. Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS. Telerehabilitation: review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol. (2017) 4:e7. doi: 10.2196/rehab.7511
43. World Health Organization. Healthy China. Available online at: https://www.who.int/teams/health-promotion/enhanced-wellbeing/ninth-global-conference/healthy-china (accessed October 20, 2021).
Keywords: rehabilitation, musculoskeletal disorders, prevalence, years lived with disability, prediction
Citation: Chen N, Fong DYT and Wong JYH (2022) Trends in Musculoskeletal Rehabilitation Needs in China From 1990 to 2030: A Bayesian Age-Period-Cohort Modeling Study. Front. Public Health 10:869239. doi: 10.3389/fpubh.2022.869239
Received: 04 February 2022; Accepted: 29 April 2022;
Published: 15 June 2022.
Edited by:
Sahar Saeedi Moghaddam, Tehran University of Medical Sciences, IranCopyright © 2022 Chen, Fong and Wong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel Yee Tak Fong, ZHl0Zm9uZ0Boa3UuaGs=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.