- Edward via College of Osteopathic Medicine–Auburn, Biomedical Affairs and Research, Auburn, AL, United States
The COVID-19 pandemic has led to diminished sleep and increased stress, anxiety, and burnout for many health professionals and health professions students. One simple approach that may be effective for bolstering personal well-being is consciously cultivating gratitude. Gratitude is positively associated with physical health, psychological health, hope, sleep, and health behavior engagement; and randomized studies indicate that gratitude interventions can improve psychological well-being and sleep. The primary aim of this study was to assess the impact of practicing Tiny Habits® on self-reported gratitude, as measured by the 6-Item Gratitude Questionnaire (GQ-6). In January 2021, 154 adult participants with GQ-6 <35/42 were randomized to one of 3 groups: Tiny Habits for Gratitude (n = 50), Tiny Habits Control (n = 52), and Inactive Control (n = 52). Both Tiny Habits groups chose 3 Tiny Habits Recipes to practice daily and participated in the free, email-based 5-Day Program with automated daily check-in emails and personalized feedback from a Certified Tiny Habits Coach. The Recipes for the Tiny Habits for Gratitude group focused on cultivating gratitude, while those for the Tiny Habits Control group did not. Post-intervention, the mean change in GQ-6 scores in the Tiny Habits for Gratitude (Δ = ↑6.9 ± 5.6; n = 37/50, 74%; p< 0.001, Cohen's d = 0.85) and Tiny Habits Control (Δ = ↑5.6 ± 4.1; n = 31/52, 60%; p = 0.009, Cohen's d = 0.71) groups were greater than that of the Inactive Control group (Δ = ↑2.5 ± 4.4; N = 42/52, 81%). At 1 month, the mean change in GQ-6 scores in the Tiny Habits for Gratitude group (Δ = ↑7.0 ± 5.3; N = 28/50, 56%) was greater than that of the Inactive Control group (Δ = ↑2.9 ± 5.4; N = 39/52, 72%; p = 0.002, Cohen's d = 0.78). These findings suggest that practicing Tiny Habits Recipes and participating in the 5-Day Program can significantly increase gratitude in the short term and focusing specifically on gratitude during this process can sustain the increase in gratitude for up to 1 month. Implementation is quick, simple, and free. This has significant implications for healthcare education stakeholders.
Introduction
Recent societal and environmental events have negatively impacted the health and wellness of many health professionals and health professions students. This is well illustrated by the impact of the COVID-19 pandemic on healthcare education stakeholders across the globe. For healthcare professionals, particularly those working on the frontlines, the pandemic brought about a significant increase in work demands, uncertainty regarding best treatment practices, emotional exhaustion from caring for severely ill patients and consoling families who have lost loved ones, and heightened concern regarding contracting and further spreading the disease themselves. The result for many has been diminished sleep and increased stress, anxiety, and burnout (1–14). Due to COVID-19-related restrictions, the requisite shifts from in-person to online learning, and the resulting decrease in social support and interaction, similar negative effects have been seen in health professions students (15–20). In addition to the negative impact of these stressors on health professionals, there are negative implications for patient safety as well (21). While effective institution- and policy-based approaches to mitigate the negative impact of such events are worth exploring, implementation is often slow and complex. In the meantime, there are actions that individuals can take to bolster their personal well-being and resiliency in the face of such challenges. One simple approach that may be effective for many is to practice and cultivate gratitude.
Gratitude can be defined as “a life orientation (i.e., worldview) toward noticing and appreciating the positive in the world” (22). It is experienced when one recognizes that (1) they have obtained a positive outcome and that (2) there is an altruistic external source (e.g., another individual, god, nature, happenstance) that is responsible for the positive outcome (23). Gratitude can be conceptualized as a state of being, a personality trait, an emotion, an attitude, or a coping mechanism (23). When viewed as a state of being, gratitude is more context-based; it is felt more during specific events. In contrast, gratitude as a trait refers to how often and intensely one experiences the state of gratitude (24). Levels of state and trait gratitude vary from person to person and often fluctuate within an individual over time (24, 25).
Higher levels of gratitude are associated with enhanced well-being and prosocial behavior. Cross-sectional studies have found that gratitude is positively associated with self-reported physical health (26), psychological health (26–28), hope (29, 30), sleep quality and quantity (31, 32), and engagement in health behaviors (26). A few studies have assessed gratitude and related outcomes in healthcare education stakeholders. Looking at nurses in South Korea (N = 646) during the COVID-19 pandemic, Lee et al. (33) found that gratitude was negatively associated with perceived stress. Prior to the pandemic, a study by Shi and Du (34) involving 1,392 medical students in China found that gratitude was positively associated with perspective taking and empathic concern, two components of emotional intelligence which have been found to be positively associated with prosocial behavior (35). This link between gratitude and prosocial behavior is corroborated elsewhere in the literature (28).
Systematic reviews and meta-analyses of randomized studies indicate that gratitude interventions provide meaningful health and wellness benefits. A meta-analysis by Davis et al. (36) indicated that gratitude interventions, such as keeping a daily or weekly gratitude journal or expressing gratitude to others, had a small positive effect on psychological well-being. Cregg and Cregg (37) found in their meta-analysis a modest effect of gratitude interventions in terms of reducing symptoms of depression and anxiety when assessed post-intervention and up to 1 month thereafter, and a systematic review by Boggiss et al. (38) suggested that gratitude interventions improve subjective sleep quality. Lastly, in a series of meta-analyses, Dickens (39) found that gratitude interventions provide many positive benefits with small to medium effect sizes regarding well-being, happiness, and depressive symptoms when assessed post-intervention and at delayed follow-up (ranging from 1 week to 6 months). It should be noted that the outcomes that were found to be significant, as well as the corresponding effect sizes, depended upon the comparison group. As a general trend, benefits and effect sizes were smaller when gratitude interventions were compared to a positive control (e.g., listing daily acts of kindness), larger when compared to a negative control (e.g., listing daily hassles), and somewhere in between when compared to a neutral control (e.g., measurement only or listing daily activities) (36, 37, 39). The benefits of gratitude interventions outlined above focus on comparison to neutral control groups.
A few mechanisms have been proposed regarding the beneficial effects of gratitude on psychological well-being and sleep. Fredrickson's (40, 41) broaden-and-build theory posits that gratitude, like other positive emotions (e.g., joy, love), broadens one's “momentary thought-action repertoire” and builds one's “enduring personal resources.” In other words, positive emotions enable individuals to pursue a wider range of novel or creative thoughts and actions in the moment (e.g., prosocial or reciprocal altruistic behaviors), resulting in an increase in one's social resources (e.g., more friendships and social bonds) and psychological resources, such as hope (30) and resilience (33). Building on Fredrickson's model, Alkozei et al. (42) suggest that, by increasing the experience of positive memories for past events, gratitude broadens one's ability to interpret seemingly negative or ambiguous situations with a more positive valence, thereby promoting psychological well-being. This is in opposition to negative emotions (e.g., fear, anxiety) which narrow one's momentary thought-action repertoire, promoting reflexive and adaptive responses (e.g., fight or flight) to threatening situations (40, 41). As for sleep, a cross-sectional study by Wood et al. (32) with over 400 participants found that gratitude predicted better subjective sleep quality and sleep duration, and less sleep latency and daytime dysfunction. Mechanistically, the authors proposed that gratitude mediates the relationships observed by promoting positive vs. negative pre-sleep cognitions.
In order to be a viable option for healthcare education stakeholders, simple, attractive, and effective gratitude-boosting interventions are needed. Several interventions, such as regularly writing a gratitude list (“counting one's blessings”), keeping a gratitude journal, or writing and delivering a letter of gratitude to an individual, have been shown to boost gratitude (39). Given that healthcare education stakeholders are often overworked with little time, physical energy, or mental energy to spare, particularly during the pandemic (9), effective interventions that are quick and easy to perform are needed. Further, interventions that individuals are intrinsically motivated to perform would lend themselves to habit formation and increased engagement (43). Although existing interventions that are supported in the literature are relatively easy and take little time to perform, the options are limited, and it is possible to create and test interventions that are simpler still. The ideal intervention is one that is effective and appealing to the individual, can be tailored to fit seamlessly into their personal routine, takes minimal time and energy to perform, and allows for easy revision, as needed, in the face of barriers or changes in routine.
The Tiny Habits® Method (44) is a simple, systematic and evidence-based approach to designing new behaviors into one's existing routine. The Tiny Habits Method was created by BJ Fogg, PhD via derivation from the Fogg Behavior Model (45). The Method involves creating a specific form of implementation intentions (46) called Tiny Habits Recipes, as follows: “After I Anchor Moment, I will Tiny Behavior.” The Anchor Moment is some reliable behavior in one's existing routine that is used to prompt the new target behavior. The Tiny Behavior is the target behavior of interest but scaled back, if needed, such that it takes very little time (i.e., <30 s) and effort to perform. Here's an example Recipe related to gratitude: “After I brush my teeth in the morning, I will think of one thing for which I am grateful.” Immediately after the Tiny Behavior, a planned Celebration is performed. The Celebration can be anything that the individual can think, say, and/or do in the moment (e.g., think, “It feels great to be grateful!” and do a fist pump) to generate positive emotions and the feeling of success. The purpose of the Celebration is to reinforce the Tiny Behavior and the Anchor Moment–Tiny Behavior relationship, thereby increasing the automaticity—the defining feature of habits (47)—with which the Tiny Behavior is performed after the Anchor Moment. Practitioners of the Method are encouraged to focus on behaviors that they truly “want” to do, as opposed to those that they feel they “should” or “need to” do (44). The Tiny Habits Method is supported in the literature as follows. Implementation intentions have been shown to facilitate action and goal achievement (46) by enhancing the mental accessibility of cues (Anchor Moments) and strengthening the link between cues and planned responses (Tiny Behaviors) (48, 49). Further, previous studies show that small, simple behaviors are performed more consistently and are more readily formed into habits (47, 50), as are behaviors that are pleasurable and intrinsically motivated (43, 51).
Materials and Methods
A randomized controlled study was performed to assess changes in gratitude scores (primary outcome) in a Tiny Habits for Gratitude group as compared to a Tiny Habits Control group and an Inactive Control group. Change in hope (secondary outcome) was also assessed, as hope and gratitude have been shown to be positively associated (29, 30).
Sample
A power analysis was performed using PASS 14.0 (NCSS, LLC. Kaysville, Utah) to determine the number of participants needed to detect variation in group means accounting for 10% of the total observed variance. Using an alpha level = 0.05 and 85% power, analysis results indicated that a total sample size of 102 participants (N = 34 per group) was needed. To account for attrition, the target sample size was set at 150 participants (N = 50 per group).
Inclusion criteria required participants to be ≥18 years of age and to have a baseline score <35/42 on the Gratitude Questionnaire 6-Item (GQ-6), a validated gratitude assessment (28). The GQ-6 cut-point was set at <35 to avoid the ceiling effect (52).
Assessments
The participants responded to the following assessments at three timepoints: before the intervention (time 1 = baseline), directly after the intervention (time 2 = post-intervention), and approximately 1 month after the intervention (time 3 = follow-up).
Gratitude Questionnaire 6-Item
The GQ-6 is a validated, self-administered tool for assessing gratitude. It consists of 6 statements with responses classified on a 7-point Likert-type scale ranging from 1 = strongly disagree to 7 = strongly agree. Two of the 6 items are reverse scored. Possible scores range from 6 to 42, with higher scores signifying higher gratitude (28).
Adult Hope Scale
The AHS is a validated, self-administered tool for assessing hope, defined as “a cognitive set that is based on a reciprocally derived sense of successful (a) agency (goal-directed determination) and (b) pathways (planning of ways to meet goals)” [(53), 571]. It consists of a total of 12 items with responses classified on an 8-point Likert-type scale ranging from 1 = definitely false to 8 = definitely true. Four of the items serve as “filler.” Scores are derived from the remaining 8/12 items and range from 8 to 64, with higher scores signifying higher hope [(53), 571].
Procedures
The assessments were built and administered via Qualtrics (Qualtrics, Provo, UT), an online survey tool. The baseline assessment included age and sex, and all 3 assessments captured participants' first names and email addresses, such that individual responses could be linked across all 3 timepoints. Recruitment was performed via posts on social media (e.g., Twitter, Facebook) on a rolling basis. After clicking the link, potential participants first viewed an information letter detailing the study, including potential benefits as well as risks, which were minimal. Those meeting inclusion criteria were then randomized (1:1:1) to one of three groups using the “randomizer” feature in Qualtrics.
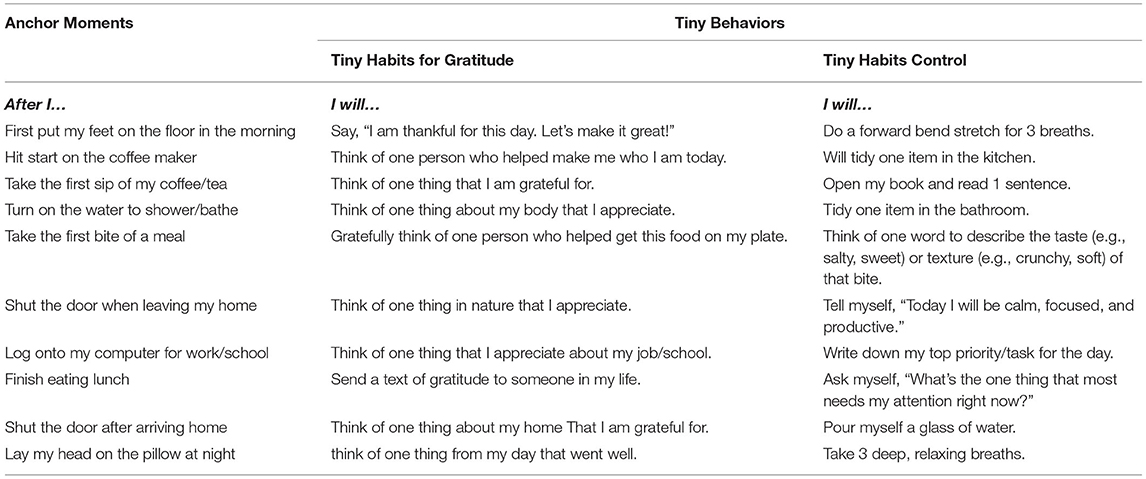
Participants who were randomized to one of the Tiny Habits groups then selected 3 Tiny Habits Recipes from a list of 10 to practice. The Recipes for both groups included the same Anchor Moments but differed on the Tiny Behaviors. The Tiny Behaviors presented to the Tiny Habits for Gratitude group focused on gratitude, while those presented to the Tiny Habits Control group did not. See Table 1. These two groups also participated in the Tiny Habits 5-Day Program (54). This free, email-based, semi-automated program includes (1) daily check-in emails with additional guidance for applying the Method and (2) personalized input and feedback from a certified Tiny Habits Coach, as needed. These participants were encouraged to practice their Recipes, revising them as needed, during the 5-Day Program and beyond. Total daily time commitment for completing the 3 recipes and fully participating in the 5-Day Program is estimated to be <2 min and <5 min, respectively. There was no intervention for the Inactive Control group. Post-intervention (time 2) and follow-up (time 3) assessments were emailed to all participants ~1 week and 5 weeks after enrollment (time 1). No incentives were offered to participants.
Statistical Analysis
Participant age, gratitude (GQ-6) scores, and hope (AHS) scores at baseline, as well as change in gratitude and hope scores from baseline to post-intervention and from baseline to 1-month follow-up, were described using sample means and standard deviations by group. Analysis of Variance (ANOVA) models were utilized to test for statistically significant differences among population means across groups for these variables, with Bonferroni post-hoc analysis performed as needed. The assumptions of normality of residuals and homogeneity of variance were examined with normal probability plots and residual plots respectively. Sex was described by frequency and percentage of female participants by group, and Chi square test of homogeneity was used to assess for statistically significant differences regarding sex across groups.
Ethics Statement
This study was pre-approved by the Edward via College of Osteopathic Medicine (VCOM) Institutional Review Board (IRB; Board Reference #2020-038).
Results
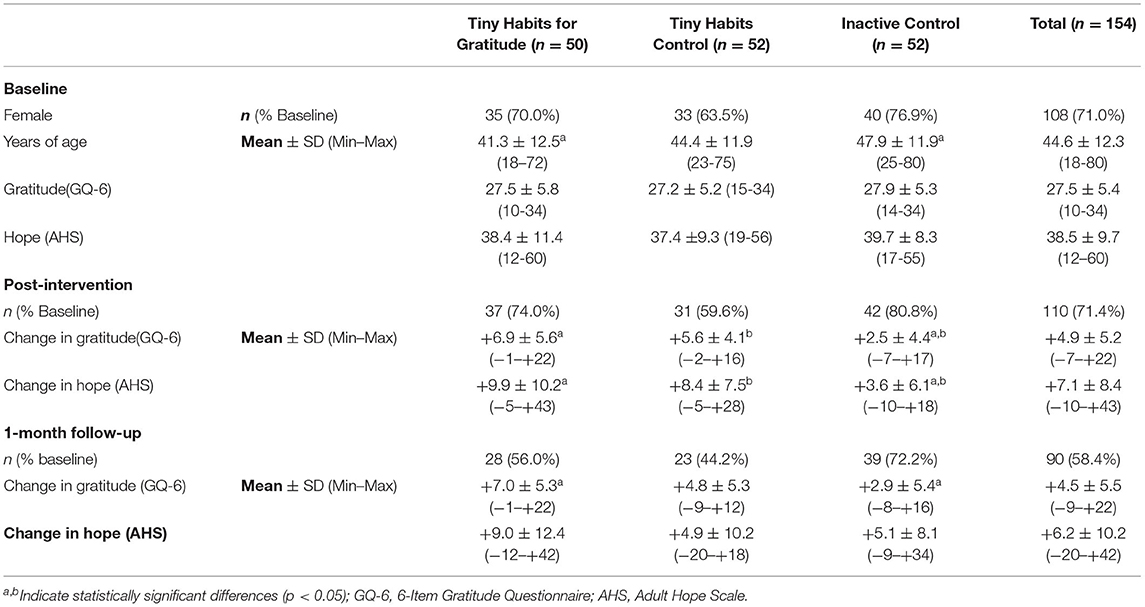
Between January 5th−22nd, 2021, 400 individuals expressed interest in participating in the study. A total of 154 met inclusion criteria, completed the baseline assessment, and were randomized to one of the three groups: Tiny Habits for Gratitude (n = 50), Tiny Habits Control (n = 52), or Inactive Control (n = 52). A total of 108/154 (71.0%) participants were female. Frequency of female sex did not differ statistically between groups (p = 0.32). Overall participant mean years of age (±standard deviation) was 44.6 (±12.3). Examination of age by treatment group revealed a significant difference in mean years of age by group (p = 0.02). Post-hoc examination among groups indicates that the Tiny Habits for Gratitude group (41.3 ± 12.5) was statistically lower in mean age compared to the Inactive Control group (47.9 ± 11.9; p = 0.01). At baseline, overall mean gratitude (GQ-6) and hope (AHS) scores (±standard deviation) were 27.5 (±5.4) and 38.5 (±9.7), respectively, with no statistical difference between groups (p = 0.85 and p = 0.50).
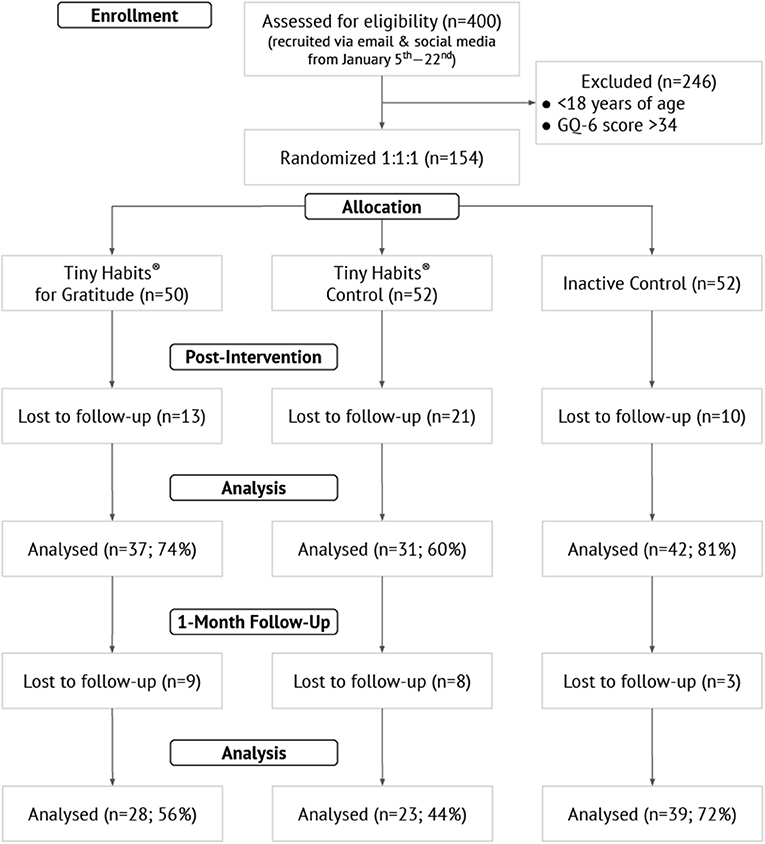
Of the 154 participants randomized, 110 (71%) completed the post-intervention assessment and 90 (58%) completed the 1-month follow-up assessment. Comparing those who completed either the post-intervention or follow-up assessment (n = 116; 75%) to those who did not complete either assessment (n = 38), there was no statistical difference regarding mean years of age (44.9 ± 11.2 vs. 44.4 ± 14.9; p = 0.91) or sex (74.1 vs. 59.5% female; p = 0.069). Figure 1 is a flow diagram illustrating progression through the phases of the trial. Table 2 contains group-level demographic and outcomes data.
Gratitude
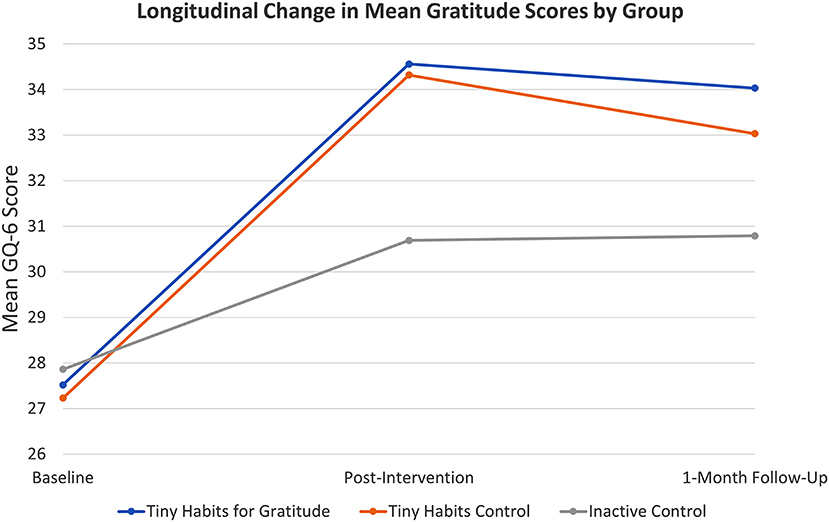
Post-intervention phase, ANOVA and Bonferroni post-hoc tests indicated that the mean change in GQ-6 scores in the Tiny Habits for Gratitude group (Δ = ↑6.9 ± 5.6; N = 37/50, 74%) and in the Tiny Habits Control group (Δ = ↑5.6 ± 4.1; N = 31/52, 60%) were both significantly greater than that of the Inactive Control group (Δ = ↑2.5 ± 4.4; N = 42/52, 81%) with p< 0.001 and p = 0.009, respectively. Measuring the standardized difference between the sample means for Tiny Habits for Gratitude group and Inactive Control group at this time, we observe Cohen's d = 0.85. Measuring the standardized difference between the sample means for Tiny Habits for Control group and Inactive Control group, we observe Cohen's d = 0.71. At 1 month, the mean change in GQ-6 scores in the Tiny Habits for Gratitude Group (Δ = ↑7.0 ± 5.3; N = 28/50, 56%) was statistically significantly greater than that of the Inactive Control group (Δ = ↑2.9 ± 5.4; N = 39/52, 72%, with a p = 0.002 and Cohen's d = 0.78. No other statistically significant differences were noted in relation to GQ-6 scores (see Figure 2).
Hope
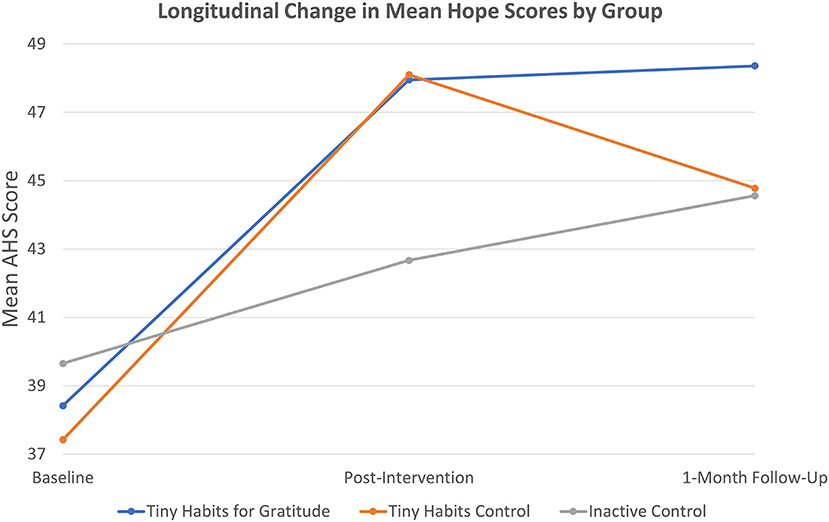
Post-intervention, ANOVA and Bonferroni post-hoc tests indicated that the mean change in AHS scores in the Tiny Habits for Gratitude group (Δ = ↑9.9 ± 10.2; N = 37/50, 74%) and in the Tiny Habits Control group (Δ = ↑8.4 ± 7.5; N = 31/52, 60%) were statistically significantly greater than that of the Inactive Control group (Δ = ↑3.6 ± 6.1; N = 42/52, 81%) with p< 0.001 and p = 0.015, respectively. For these comparisons, Cohen's d = 0.76 comparing the Tiny Habits for Gratitude group to Inactive Control and Cohen's d = 0.70 comparing the Tiny Habits Control group to Inactive Control effect sizes. No other statistically significant differences were noted in relation to AHS scores (see Figure 3).
Discussion
The findings of this study suggest that practicing Tiny Habits Recipes and participating in the Tiny Habits 5-Day Program can significantly increase hope and gratitude in the short term, and that focusing specifically on gratitude in the process can sustain the increase in gratitude for up to 1 month thereafter. Congruent with previous studies (36, 37, 39), greater differences were seen when the intervention (Tiny Habits for Gratitude) group was compared to a neutral (Inactive) vs. positive (Tiny Habits) control group. For instance, relative to the Inactive Control group, the Tiny Habits for Gratitude group exhibited statistically significant increases in gratitude scores post-intervention and at 1-month follow-up, with a large and medium-to-large effect size, respectively. And there were no statistical differences between the two Tiny Habits groups in this regard. Further, both Tiny Habits groups exhibited greater increases in hope and gratitude scores post-intervention, relative to the Inactive Control group, but only the Tiny Habits for Gratitude group exhibited sustained increases in gratitude at 1-month follow-up. This suggests that positive psychology interventions, in general, may increase hope and gratitude in the short term but, for sustained effects to be realized, such interventions may need to be focused on the domain of interest (e.g., gratitude). Overall, the results indicate that this is an effective intervention for boosting gratitude. Implementation is simple and takes very little time, and the 5-Day Program is free for all individuals who wish to take part. This has significant implications for healthcare education stakeholders, especially now.
Due to the threats and demands of the COVID pandemic, for example, many health professionals have reported diminished sleep and increased stress, anxiety, and burnout (1–14), and similar negative effects have been seen in health professions students (15–20). These effects may limit the time and physical or mental resources available to regularly engage in new behaviors (e.g., start an exercise routine, meditate, go to bed earlier) that could help promote well-being and resilience. Most individuals, however, can easily design 3 Tiny Habits Recipes for gratitude into their daily routine, with assistance from a Tiny Habits Coach in the 5-Day Program. This simple behavioral intervention can have an outsized effect in terms of boosting gratitude, which is good in and of itself and may also lead to other changes and benefits, such as improved psychological well-being and subjective sleep quality (36–39). Further, the Tiny Habits Method can also be utilized to promote consistent engagement in other gratitude interventions that have been shown to be effective. For instance, if one wanted to keep a daily gratitude journal, a Tiny Habits Recipe such as, After I finish eating breakfast, I will open my gratitude journal and write, “Today I am grateful for __________.” could be utilized. Increased gratitude may lead to additional health behavior change (26), and the Tiny Habits Method can be applied to any behavior domain (e.g., diet, physical activity, patient safety) of the individual's choosing, thereby providing the potential for additional benefit.
Limitations
This study is not without limitations. The total sample size (N = 154) was relatively small, and a significant percentage of participants did not complete the post-intervention (28.6%) and 1-month follow-up (41.6%). Furthermore, a greater percentage of participants in the Tiny Habits groups were lost to follow-up relative to the Inactive Control group, which may bias the results. This was also an intention-to-treat analysis, in which all data available were analyzed whether or not participants completed the intervention protocol (i.e., performing their 3 Tiny Habits Recipes daily) as instructed. This is good in terms of external validity. However, completing a per-protocol analysis would strengthen internal validity. Lastly, the study was not conducted in healthcare professions stakeholders and may not generalize to this population. That said, there is no reason to believe that it would not, given the findings of previous studies regarding gratitude and healthcare professions stakeholders (33, 34).
Future Outlooks
Practicing gratitude in general, and practicing Tiny Habits for gratitude specifically, can be a simple and effective self-care strategy to promote well-being and resilience. Future studies should consider (1) focusing on healthcare education stakeholders specifically in order to better assess the implications for this cohort and (2) incorporating per-protocol analysis to strengthen internal validity.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by IRB of Edward via College of Osteopathic Medicine. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JH conceived of the idea, designed the study, oversaw implementation, coached participants in the Tiny Habits for Gratitude group, and drafted the manuscript. DR performed power analysis, statistical analysis, produced figures, and gave feedback on the article. Both authors approved of the article in its final form.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Tiny Habits Coaches Geoff Grivitz and William Flautt for helping coach participants in the Tiny Habits Control group and Student Doctor Vandana Chaudhary (VCOM-Virginia) for assisting with the literature review for the Introduction of the article.
References
1. Demartini B, Nisticò V, D'Agostino A, Priori A, Gambini O. Early psychiatric impact of COVID-19 pandemic on the general population and healthcare workers in Italy: a preliminary study. Front Psychiatry. (2020) 11:561345. doi: 10.3389/fpsyt.2020.561345
2. Giusti EM, Pedroli E, D'Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, et al. The psychological impact of the COVID-19 outbreak on health professionals: A cross-sectional study. Front Psychol. (2020) 11:1684. doi: 10.3389/fpsyg.2020.01684
3. Ghahramani S, Lankarani KB, Yousefi M, Heydari K, Shahabi S, Azmand S, et al. Systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Front Psychiatry. (2021) 12:758849. doi: 10.3389/fpsyt.2021.758849
4. Di Monte C, Monaco S, Mariani R, Di Trani M. From resilience to burnout: psychological features of italian general practitioners during COVID-19 emergency. Front Psychol. (2020) 11:567201. doi: 10.3389/fpsyg.2020.567201
5. Zhang X, Wang J, Hao Y, Wu K, Jiao M, Liang L, et al. Prevalence and Factors Associated with burnout of frontline healthcare workers in fighting against the COVID-19 pandemic: evidence from China. Front Psychol. (2021) 12:680614. doi: 10.3389/fpsyg.2021.680614
6. Xia L, Chen C, Liu Z, Luo X, Guo C, Liu Z, et al. Prevalence of sleep disturbances and sleep quality in chinese healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry. (2021) 12:646342. doi: 10.3389/fpsyt.2021.646342
7. Zakeri MA, Rahiminezhad E, Salehi F, Ganjeh H, Dehghan M. Burnout, anxiety, stress, and depression among iranian nurses: before and during the first wave of the COVID-19 pandemic. Front Psychol. (2021) 12:5491. doi: 10.3389/fpsyg.2021.789737
8. Barello S, Caruso R, Palamenghi L, Nania T, Dellafiore F, Bonetti L, et al. Factors associated with emotional exhaustion in healthcare professionals involved in the COVID-19 pandemic: an application of the job demands-resources model. Int Arch Occup Environ Health. (2021) 94:1751–61. doi: 10.1007/s00420-021-01669-z
9. Barello S, Palamenghi L, Graffigna G. Stressors and resources for healthcare professionals during the COVID-19 pandemic: lesson learned from Italy. Front Psychol. (2020) 11:2179. doi: 10.3389/fpsyg.2020.02179
10. Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinical Medicine. (2020) 24:100424. doi: 10.1016/j.eclinm.2020.100424
11. van Roekel H, van der Fels IMJ, Bakker AB, Tummers LG. Healthcare workers who work with COVID-19 patients are more physically exhausted and have more sleep problems. Front Psychol. (2020) 11:625626. doi: 10.3389/fpsyg.2020.625626
12. Yeung NC, Wong EL, Cheung AW, Yeoh EK, Wong SY. Feeling anxious amid the COVID-19 pandemic: factors associated with anxiety symptoms among nurses in Hong Kong. Front Psychol. (2021) 12:748575. doi: 10.3389/fpsyg.2021.748575
13. Wang W, Song W, Xia Z, He Y, Tang L, Hou J, et al. Sleep Disturbance and Psychological Profiles of Medical Staff and Non-Medical Staff During the Early Outbreak of COVID-19 in Hubei Province, China. Front Psychiatry. (2020) 11:733. doi: 10.3389/fpsyt.2020.00733
14. Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. (2020) 11:306. doi: 10.3389/fpsyt.2020.00306
15. Xiong P, Ming W-K, Zhang C, Bai J, Luo C, Cao W, et al. Factors influencing mental health among Chinese medical and non-medical students in the early stage of the COVID-19 pandemic. Front Public Health. (2021) 9:603331. doi: 10.3389/fpubh.2021.603331
16. Zhang J-Y, Shu T, Xiang M, Feng Z-C. Learning burnout: evaluating the role of social support in medical students. Front Psychol. (2021) 12:625506. doi: 10.3389/fpsyg.2021.625506
17. Stacey A, D'Eon M, Madojemu G. Medical student stress and burnout: before and after COVID-19. Can Med Educ J. (2020) 11:e204–5. doi: 10.36834/cmej.70305
18. Zheng Q, Lin X, He L, Freudenreich T, Liu T. Impact of the perceived mental stress during the COVID-19 pandemic on medical students' loneliness feelings and future career choice: a preliminary survey study. Front Psychiatry. (2021) 12:666588. doi: 10.3389/fpsyt.2021.666588
19. Gao J, Wang F, Guo S, Hu F. Mental health of nursing students amid coronavirus disease 2019 pandemic. Front Psychol. (2021) 12:699558. doi: 10.3389/fpsyg.2021.699558
20. Hong J, Jung I, Park M, Kim K, Yeo S, Lee J, et al. Attitude of medical students about their role and social accountability in the COVID-19 pandemic. Front Psychiatry. (2021) 12:645340. doi: 10.3389/fpsyt.2021.645340
21. Hall LH, Johnson J, Watt I, Tsipa A, O'Connor DB. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS ONE. (2016) 11:e0159015. doi: 10.1371/journal.pone.0159015
22. Wood AM, Froh JJ, Geraghty AWA. Gratitude and well-being: a review and theoretical integration. Clin Psychol Rev. (2010) 30:890–905. doi: 10.1016/j.cpr.2010.03.005
23. Emmons RA, McCullough ME. Counting blessings versus burdens: an experimental investigation of gratitude and subjective well-being in daily life. J Pers Soc Psychol. (2003) 84:377–89. doi: 10.1037/0022-3514.84.2.377
24. McGuire AP, Szabo YZ, Murphy KM, Erickson TM. Direct and indirect effects of trait and state gratitude on health-related quality of life in a prospective design. Psychol Rep. (2020) 123:2248–62. doi: 10.1177/0033294119868784
25. Chopik WJ, Newton NJ, Ryan LH, Kashdan TB, Jarden AJ. Gratitude across the life span: age differences and links to subjective well-being. J Posit Psychol. (2019) 14:292–302. doi: 10.1080/17439760.2017.1414296
26. Hill PL, Allemand M, Roberts BW. Examining the pathways between gratitude and self-rated physical health across adulthood. Pers Individ Dif. (2013) 54:92–6. doi: 10.1016/j.paid.2012.08.011
27. Wood AM, Joseph S, Maltby J. Gratitude predicts psychological well-being above the big five facets. Pers Individ Dif. (2009) 46:443–7. doi: 10.1016/j.paid.2008.11.012
28. Mccullough ME, Emmons RA, Tsang J-A. The grateful disposition: a conceptual and empirical topography. J Pers Soc Psychol. (2002) 82:112–27. doi: 10.1037/0022-3514.82.1.112
29. Witvliet CV, Richie FJ, Root Luna LM, Van Tongeren DR. Gratitude predicts hope and happiness: a two-study assessment of traits and states. J Posit Psychol. (2019) 14:271–82. doi: 10.1080/17439760.2018.1424924
30. McCullough ME. Savoring life, past and present: Explaining what hope and gratitude share in common. Psychol Inq. (2002) 13:302–4. Available online at: https://www.jstor.org/stable/1448873
31. McClintock CH. Opening the heart: a spirituality of gratitude. Spiritual Clin Pract. (2015) 2:21–22. doi: 10.1037/scp0000060
32. Wood AM, Joseph S, Lloyd J, Atkins S. Gratitude influences sleep through the mechanism of pre-sleep cognitions. J Psychosom Res. (2009) 66:43–8. doi: 10.1016/j.jpsychores.2008.09.002
33. Lee J-Y, Kim M, Jhon M, Kim H, Kang H-J, Ryu S, et al. The association of gratitude with perceived stress among nurses in Korea during COVID-19 outbreak. Arch Psychiatr Nurs. (2021) 35:647–52. doi: 10.1016/j.apnu.2021.10.002
34. Shi M, Du T. Associations of emotional intelligence and gratitude with empathy in medical students. BMC Med Educ. (2020) 20:116. doi: 10.1186/s12909-020-02041-4
35. Wang H, Wu S, Wang W, Wei C. Emotional intelligence and prosocial behavior in college students: a moderated mediation analysis. Front Psychol. (2021) 12:713227. doi: 10.3389/fpsyg.2021.713227
36. Davis DE, Choe E, Meyers J, Wade N, Varjas K, Gifford A, et al. Thankful for the little things: a meta-analysis of gratitude interventions. J Couns Psychol. (2016) 63:20–31. doi: 10.1037/cou0000107
37. Cregg DR, Cheavens JS. Gratitude interventions: effective self-help? a meta-analysis of the impact on symptoms of depression and anxiety. J Happiness Stud. (2020) 22:413–45. doi: 10.1007/s10902-020-00236-6
38. Boggiss AL, Consedine NS, Brenton-Peters JM, Hofman PL, Serlachius AS. A systematic review of gratitude interventions: effects on physical health and health behaviors. J Psychosom Res. (2020) 135:110165. doi: 10.1016/j.jpsychores.2020.110165
39. Dickens LR. Using gratitude to promote positive change: a series of meta-analyses investigating the effectiveness of gratitude interventions. Basic Appl Soc Psych. (2017) 39:193–208. doi: 10.1080/01973533.2017.1323638
40. Fredrickson BL. Gratitude, like other positive emotions, broadens and builds. The Psychology of Gratitude. (2004) 368:145–66. doi: 10.1093/acprof:oso/9780195150100.003.0008
41. Fredrickson BL. What good are positive emotions? Rev Gen Psychol. (1998) 2:300–19. doi: 10.1037/1089-2680.2.3.300
42. Alkozei A, Smith R, Killgore WDS. Gratitude and subjective wellbeing: a proposal of two causal frameworks. J Happiness Stud. (2018) 19:1519–42. doi: 10.1007/s10902-017-9870-1
43. Judah G, Gardner B, Kenward MG, DeStavola B, Aunger R. Exploratory study of the impact of perceived reward on habit formation. BMC Psychol. (2018) 6:62. doi: 10.1186/s40359-018-0270-z
44. Fogg BJ. Tiny Habits: The Small Changes That Change Everything. Kindle. Boston, MA: Houghton Mifflin Harcourt (2019).
45. Fogg BJ. A behavior model for persuasive design. In Proceedings of the 4th International Conference on Persuasive Technology Persuasive'09. New York, NY, USA: ACM (2009). doi: 10.1145/1541948.1541999
46. Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Advances in Experimental Social Psychology. (2006) 38:69–119. doi: 10.1016/S0065-2601(06)38002-1
47. Verplanken B. Beyond frequency: habit as mental construct. Br J Soc Psychol. (2006) 45:639–56. doi: 10.1348/014466605X49122
48. Webb TL, Sheeran P. How do implementation intentions promote goal attainment? A test of component processes. J Exp Soc Psychol. (2007) 43:295–302. doi: 10.1016/j.jesp.2006.02.001
49. Judah G, Gardner B, Aunger R. Forming a flossing habit: an exploratory study of the psychological determinants of habit formation. Br J Health Psychol. (2013) 18:338–53. doi: 10.1111/j.2044-8287.2012.02086.x
50. Lally P, van Jaarsveld CHM, Potts HWW, Wardle J. How are habits formed: modelling habit formation in the real world. Eur J Soc Psychol. (2010) 40:998–1009. doi: 10.1002/ejsp.674
51. Phillips LA, Chamberland P-É, Hekler EB, Abrams J, Eisenberg MH. Intrinsic rewards predict exercise via behavioral intentions for initiators but via habit strength for maintainers. Sport, Exercise, and Performance Psychology. (2016) 5:352–64. doi: 10.1037/spy0000071
52. Chyung SY, Hutchinson D, Shamsy JA. Evidence-based survey design: Ceiling effects associated with response scales. Perform Improv Advis. (2020) 59:6–13. doi: 10.1002/pfi.21920
53. Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, et al. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol. (1991) 60:570–85. doi: 10.1037/0022-3514.60.4.570
54. Let Tiny Habits change your life (2020). Available online at: https://tinyhabits.com/join/ [Accessed January 6, 2022]
Keywords: gratitude, habits, Tiny Habits, self-care, COVID-19, stress, burnout, healthcare professionals (HCPs)
Citation: Hollingsworth JC and Redden DT (2022) Tiny Habits® for Gratitude-Implications for Healthcare Education Stakeholders. Front. Public Health 10:866992. doi: 10.3389/fpubh.2022.866992
Received: 31 January 2022; Accepted: 04 April 2022;
Published: 16 May 2022.
Edited by:
Channing R. Ford, Jacksonville State University, United StatesReviewed by:
Kristen Helms, Alabama College of Osteopathic Medicine, United StatesStarla Meighan, Alabama College of Osteopathic Medicine, United States
Copyright © 2022 Hollingsworth and Redden. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joshua C. Hollingsworth, amhvbGxpbmdzd29ydGhAYXVidXJuLnZjb20uZWR1
 Joshua C. Hollingsworth
Joshua C. Hollingsworth David T. Redden
David T. Redden