- Department of Midwifery, College of Medicine and Health Sciences, Ambo University, Ambo, Ethiopia
Background: Antenatal care is a care given for pregnant women and is taken as a key maternal care service in improving and keeping health of both life outcomes for mothers and newborns. Countries with low antenatal care coverage are the countries with very high maternal mortality ratios.
Objective: Hence, The aim of this study was to determine the level of late initiation of antenatal care visit and associated factors amongst antenatal care follow up in Antenatal care (ANC) services at Gedo General Hospital, Western Oromia Region, Ethiopia, 2021
Methodology: A health facility based cross-sectional study design was conducted from July 10–30, 2021 using primary data review and face-to-face interviews among clients receiving ANC. A total of 347 mothers was selected by simple random sampling and were interviewed while they come to antenatal care follow-up in Gedo general hospital. Data were entered into Epi-data version 4.6 and then changed to SPSS version 23 for the analysis purpose. Those Variables which are P < 0.25 in binary logistic regression were selected as a candidate for multiple logistic regressions to determine independently associated factors. The adjusted odds ratio was employed with 95% CI to illustrate the strength of association and P < 0.05 was used to state a statistical significance.
Result: Among 330 women, about 58.5% of women came for their first ANC visit initiation lately. Being a housewife, having a family size ≥4, and having a distance from the health facility >1 h were higher odds of late first ANC visit initiation as compared to vice versa. Besides, women aged 20–24 years had 0.18 times and 25–29 years had lower odds of late first ANC visit initiation
Conclusion: Majority of women began their first antenatal care initiation lately. Therefore, the provision of awareness on the significance of attending the first antenatal care early via health extension workers is recommended
Introduction
Antenatal care is the care offered for pregnant women and is recognized as a input for maternal service in improving and keeping health outcomes for both lives of mothers and newborns. World health organization (WHO) ANC model recommends a minimum of four ANC contacts, and encourages that the first contact appointment will take place within the first trimester (1). Antenatal care is also referred as the care provided by skilled healthcare providers to pregnant mothers to make sure the health conditions for both mother and baby. ANC is one of the “four pillars” of safe motherhood initiatives, which is used to promote and establish good health during pregnancy and the early postpartum periods (2–4).
Globally, there is a huge difference in the prevalence of late ANC checkup among pregnant mothers that is the prevalence of late ANC in developed countries is 27.5%, and that of developing countries is 88 % (5–8). In spite of ANC service is given without fee and there is high accessibility; low ANC utilization and late registering or booking is still a main problem (9, 10).
Even though, most studies have revealed a lot of factors affecting the utilization of ANC in different contexts, these findings have not been prepared collectively for a factor that affects mothers for late ANC initiation (11). According to a study conducted in Mekelle city, Most of the attendees 109 (48%) made their first visit in their first trimesters and a study done in Jimma town about (51.8%) of the mothers started ANC at late (12–14).
Women who have an inadequate number of ANC visits or start ANC later than the first trimester seem to have higher rates of poor pregnancy outcomes, such as low birth weight and pre-term birth (15, 16). Maternal health complications and lack of prenatal outcomes are often associated with other factors like the non-utilization of antenatal and childbirth services and poor socioeconomic status. Unwanted outcomes are, seen in those mothers who have not done ANC registration due to their delay of antenatal care because of dissatisfaction toward the quality of service pregnant mothers are affected by complications like: preeclampsia, malaria, lack of birth readiness, post-partum hemorrhage due to lack of risk identification at ANC level (17–23).
According to a study done in Niger Delta, Nigeria 73.6% of mothers booked lately (24). According to research conducted in Douala general hospital (DGH), Cameroon From a total of participated women, about 44% of them registered the first ANC visit lately (25). A study done in public health institutions of Axum town, the prevalence of timely ANC initiation of was 27.5%. But, about three fourth of the mothers (72.5%) booked their ANC visit lately (26). A study conducted in Kembata Tembaro Zone in SNNPR also shows that the magnitude of participants who started ANC early was 31.4% while those who registered lately were 68.6%. The finding of the study conducted in northern Ethiopia shows that 59.4% of pregnant mothers began their first visit after the first trimester and in the central zone of the Tigray region the prevalence of late ANC booking at the first visit was 85% (1, 8, 19, 27–29).
According to a study done in Debre Markos town, the magnitude of participants who made their first antenatal care visit after 16 weeks of gestation was found to be 33% (30). A done in Debre Berhan town, the proportion of pregnant women who had ANC booking within the first trimester of pregnancy was 40.6% (31). According to a study done in Ilu Ababor Oromia regional state, the proportion of respondents who initiated ANC lately was 71.2% (32).
There is no study done on the time of ANC initiation amongst pregnant mothers in the selected study area to the best of our knowledge. It is essential to identify the status of ANC late initiation and associated factors to improve maternal and fetal outcomes via sufficient utilization of Antenatal care.
Materials and Methods
Study Setting, Design, Population
The study was conducted in Gedo General Hospital in west Shoa of Oromia regional state west of Ethiopia, which is about 178 kilometers from the capital city, Addis Ababa, and 64 km from Ambo town.it is located at the east of Gedo town 3 km away from the bus station. Gedo General Hospital is a General Hospital owned by the Government. It has four major clinical departments (medical and surgical, pediatrics and Gynecology or Obstetrics) and other minor departments psychiatry, Nice, TB, along with other follow-up and special clinics for specific diseases such as Antiretroviral therapy (ART) and Tuberclosisis (TB). This study was, conducted from May, 15/2021 up to June 15/2021. An institutional-based cross-sectional study design was employed. The source of the population of this study was all pregnant women came for ANC follow-up at Gedo General Hospital and the study population was selected pregnant mothers visiting ANC in Gedo General Hospital during the study period and fulfilling the eligibility criteria. The inclusion criteria for the study were selected pregnant mothers visiting ANC service in Gedo General Hospital during the data collection period.
Sample Size Determination and Sampling Technique
The sample size was determined using a single population proportion formula by considering the proportion of ANC late initiation, which is 71.2% in Ilu Ababora Zone, southwest Ethiopia, 95% significance level of Z α/2 = 1.96, 5% margin of error, and 10% of non-response rate (33).
Hence, the total sample size = 315 + 10 % of none response rate = 347.
A probability systematic random sampling technique was employed by using constant K value (K = N/n, 600/347 = 1.7 ≈ 2), N is the total number of ANC attendants in the last year's quarterly case flow report of the same periods (N = 600). Every two client was interviewed by using a systematic sampling technique. The first client to be interviewed was selected randomly by lottery method from the first two client. The exit interview technique was used to collect data on their clinic days.
Data Collection Tool and Techniques
The data was collected using a pretested structured questionnaire administered face-to-face interview. Pregnant women's knowledge on the advantage and services availability of ANC was asked using 10 questions. The questionnaire was developed from different pieces of literature (33). It was prepared in English and translated to Afan Oromo (local language) for clarification and back to English for data analysis and to check its consistency. The local language version of the questionnaire was used to collect the data. There are four Midwifery student data collectors with supervision turned by the turn supervisor of the investigator who can be closely supervising the process of data collection.
Variables and Operational Definition
Dependent Variable: Late Initiation of ANC (Yes, No)
Independent variables were socio-demographic variables: Maternal Age, Religion, marital status, ethnicity, residence, income, occupation, employment family size, and educational level. Obstetric factors: Gravidity, Parity, GA, Birth interval, previous and current ANC use, number of ANC visits, Maternal medical conditions (DM and Hypertension), Previous mode of delivery, previous CS scar, number of previous CS done. Maternal behavior: chat chewing, drinking alcohol, cigarette smoking.
Data Collection Method and Procedure
Late initiation of antenatal care: Refers to a woman who came for ANC beyond 16 weeks gestation for the first time during the pregnancy (26). Antenatal care is a type of care given for pregnant women and is considered a key maternal service in improving a wide range of health outcomes for women and newborns (29).
Data Processing and Analysis
The collected data was cleaned, edited, coded, and entered into Epi-data V- 4.6 and exported to SPSS version V-23.0 for analysis. After categorizing and defining variables, a descriptive analysis will be employed for each of the independent variables. The results were reported using percentages, tables, and graphs. Bivariate analysis variables that indicate significant association with 95% CI and a P < 0.25 were entered in to multivariable analysis to select the factors associated with the ANC late initiation. The screened variables were fitted to the multivariable logistic regression model through a backward stepwise method to reduce the effects of confounders. Adjusted odds ratio (AOR) was calculated with 95% CI to show the strength of association and P < 0.05 was used to assert statistical significance.
Data Quality Control
The data collected was cleared and checked for completeness of data. The quality of the questionnaire will be secured by pre-testing the tool and training the interviewers and supervisors previous to the real data collection. The pre-test of the questionnaire, which is 5% of the total sample size, was carried out in Ambo health facility- outside of the selected study area. Training was given to interviewers and supervisors on the data collection techniques. The completeness, clarity and consistency of the data collected will be checked by supervisors and investigators.
Ethics Statement
Before the data collection procedure, an ethical clearance letter was taken from the Ambo University department of midwifery ethical committee with the reference number UGC/83/2021, and similarly, permission from Gedo General Hospital was obtained. Oral and written consent was obtained from the responder. The respondents' rights and dignity were also respected. Confidentiality was, kept throughout data collection and the woman has a right to refuse or discontinue any time during the interview. The interview was undertaken in a private area to keep privacy and confidentiality.
Results
Socio-Demographic Characteristics
In this study, 330 pregnant women participated, with a response rate of 95%. Among all respondents about 115 (34.8%) pregnant women were found between the age of 20–24 years. The majority 224 (67.9%) of mothers were protestant by religion. About two-thirds, 309 (93.6%) were married and most of them 228 (69.1%) are literate in educational status. The majority of the respondents were housewives which accounted for 234 (70.9%) (Table 1).

Table 1. Socio-demographic characteristics of pregnant mothers who were attending ANC in the Gedo general Hospital, West Shoa zone, Oromia region, Ethiopia (n = 330).
Time of First Antenatal Care Visit
The proportion of respondents who initiated their first ANC lately was 193 (58.5%) and early first ANC visit initiation was 137 (48.5%) (Figure 1). Moreover, most of the women 155 (47%) used 3rd ANC visit and 128 (38.8%) of them decided with their husband to initiate ANC visit. The majority of the 219 (66.4%) did not Inform when to register 1st ANC and 201 (60.9) did not use ambulance services. The majority of the participants 279 (84.5%) have awareness regarding danger signs and 316 (95.8%) have usage of ANC for birth preparedness (Table 2).
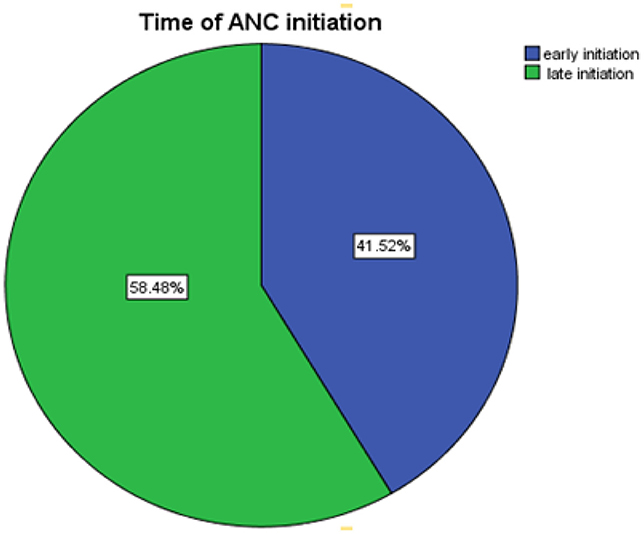
Figure 1. Time the first antenatal care visit initiation who were attending ANC in Gedo General Hospital (n = 330).

Table 2. Obstetric history of pregnant mothers, who were attending ANC in Gedo general hospital (n = 330).
Obstetric History of the Respondents
Two hundred eighty-nine (87.6%) of the respondents were multigravida. Most 293 (88.8%) of the women were part one and above. Among the total respondents, 32 (9.2%) had a history of abortion (Table 2).
Factors Associated With the Late First ANC Visit
On bivariate analysis, factors found to be significantly associated with the late initiation of ANC visit was age, residence, maternal occupation, estimated monthly income, family size, gravidity, distance to the health facility, informed when to register the first ANC visit, Ambulance service, number of ANC visit, awareness of danger sign, awareness of ANC usage for birth preparedness having a history of preterm, On multivariable analysis, age, maternal occupation, family size, distance to the health facility, Ambulance service, were significantly associated with the late booking of the first ANC visit.
The odds of late initiation of ANC for women aged between 20 and 24 years had 0.18 times (AOR: 0.18; 95% CI: 0.05, 0.63) and 25–29 years had 0.24 times (AOR: 0.24; 95% CI: 0.06, 0.90) the odds of those women aged between 15 and 19 years. The odds of late initiation of ANC for women who were housewives in their occupation had 2.22 times (AOR: 2.22; 95% CI: 1.17, 4.19) the odds of those women who were governmental employees. The odds of late initiation of ANC for women who were living within a family size of greater than and equal to four is 2.29 times (AOR: 2.29; 95% CI: 1.24, 4.22) the odds of those living within less and equal to three family size. The odds of late initiation of ANC for women who travel >1 h and above of walking time from their home to health facility had 5.52 times (AOR: 5.52; 95% CI: 2.71, 11.22) the odds of those who travel <1 h and above of walking time. The odds of late initiation of ANC for women who got Ambulance service had 0.38 times (AOR: 0.38; 95% CI: 0.21, 0.68) the odds of those women who did not get Ambulance service (Table 3).
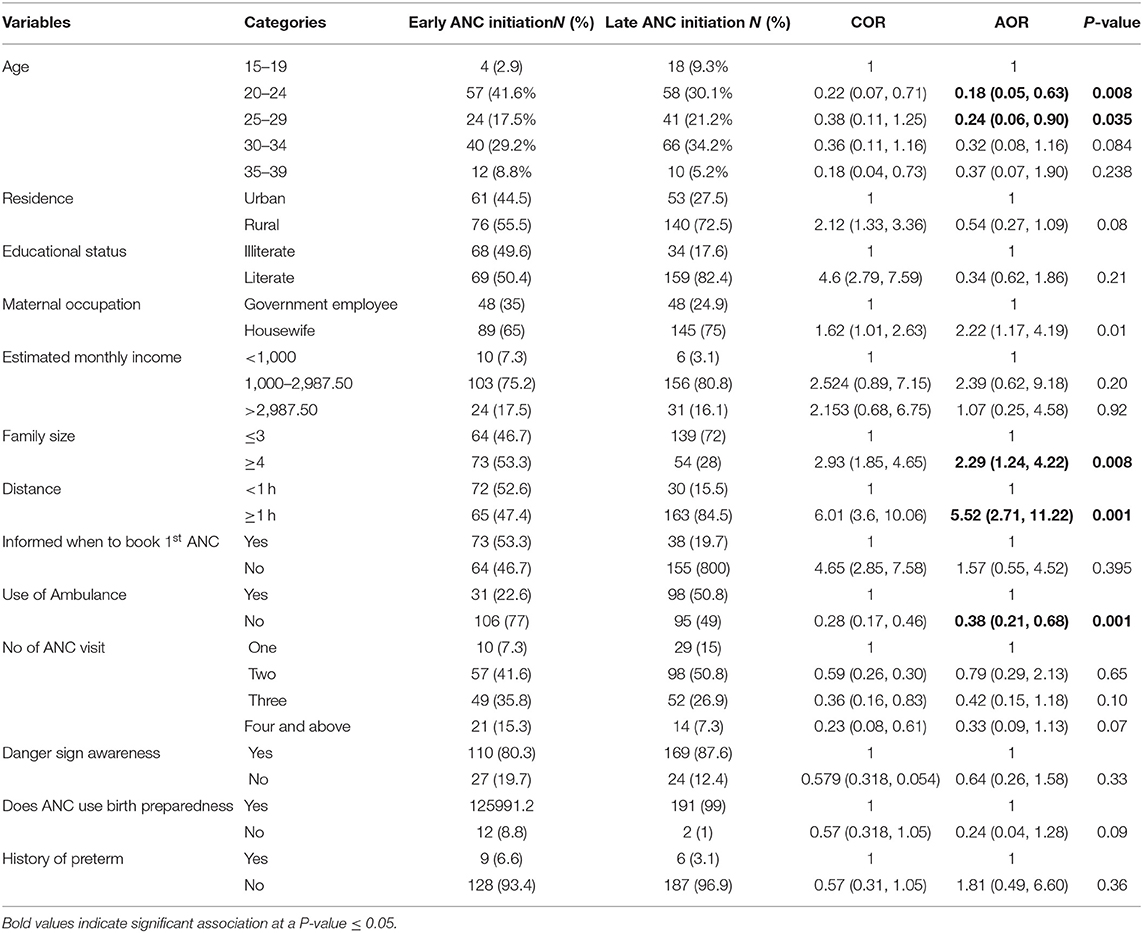
Table 3. Multivariable model of the factors for late ANC initiation among pregnant women attending Gedo Primary Hospital, West Shoa Zone, Oromia region, Ethiopia, 2021.
Discussion
The results of this study showed that among 330 women, about 58.5 % of women came for their first ANC visit initiation lately or registered first ANC visit after 16 weeks of gestation. The finding of this study is almost higher than when compared to with a study done in Douala general hospital (DGH), Cameroon 44 % (25), Debre Markos, 33.4 % (30). This is might be due to socio-demographic differences and health care service awareness. But the prevalence of women who started for their first ANC visit lately is significantly lower than Nigeria 73.6% (24), Axum town (72.5%) (26), Kembata Tembaro Zone (68.6%) (27), Ilu Ababor (71.2%) (33), East Wollega 81.5% (23). This is because of the high distribution of health posts and the promotion of maternal health care utilization by health extension workers.
Furthermore, the magnitude of respondents who registered lately in this study is lower than the Ethiopian demographic health survey 2019 report of 72% or only 28% of women had their first ANC visit during the first trimester (34). This may be due to this study being at a specific hospital in which total populations are different when we compare with the national and gap in the year of study and a lot of strategies and work has been done since then to improve maternal health services.
In this study, teenagers mothers were utilized late ANC than older women. This finding is similar with the studies done in Zambia (35), Nigeria (36), and the United Kingdom (37). This might be young teenagers women may have lack of knowledge, single, unwanted pregnancy, did not experienced with pregnancy when compared with women aged >20 years (35–37). Women who were housewives in their occupation were came lately to ANC visit as compared to those mothers who were governmental employees. This finding was similar with other studies done in North West of Ethiopia (38). The probable justification might be that those women who were governmental employee might have better access of knowledge, peer pressure, awareness and understanding about early ANC services (39).
Mothers who were living with high family size were came lately ANC visit initiation as compared to those who were living with less and equal to three family size. This study is in line with the study done in Rwanda (40) and Illu Abbabora, Ethiopia (33). This might be due to lack of economy which increases as the number of family size increases in developing country. Another reason might be most women overtake their time on other workload activities to develop their family to fulfill their basic needs rather than considering about their pregnancy checkup early.
Regarding distance, Women who travel >1 h and above of walking time from their home to the health facility had 5.52 times higher odds of late first ANC visit initiation as compared to those who travel <1 h and above of walking time. This study is in line with a study done in Zambia, Bahirdar Zuria Wereda, Ethiopia (35, 41). The possible reason might be those women living in a low income country utilize their time in day to day activity for survival of them self's and their family rather than considering their health checkup until they feel some symptoms. The other reason might be due to lack of transport and uncomfortable road for vehicles due to most valley land or unsuitable geographical area.
Limitations of the Study
First, the nature of this study design is subject to selection bias and measurement bias. Women who were at private clinic were not included which led to a lack of generalization was recognized as a limitation of the study.
Conclusions
In this study, the majority of women started their first antenatal care initiation lately. Women's age, being housewives, having a large family size, and long-distance from a health facility were factors identified for late first ANC initiation. Based on the findings of this study, Ambo Zonal Health Office and Cheliya Wereda Health Office should strengthen the provision of training for health extension workers to teach pregnant mothers about early ANC initiation by going home to home. Provision of education and communication for young mothers and their partners by health professionals at a hospital during morning health education and Provision of additional Hospital or ambulance for the community to reach easily and timely at health facility service.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Statement
An ethical clearance letter was obtained from the Ambo University Department of Midwifery Ethical Committee with the reference number UGC/83/2021. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
KD and BD conceptualized the idea, wrote the original draft, supervised the overall study, analyzed data, prepared the manuscript, drafted or revised the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are grateful to Gedo General Hospital for their guidance and support during the data collection period. We also thank data collectors (Alemu Girma, Junedin Aman, Getahun Tilahun, and Ademe Kasahun) and study participants for their huge contribution to the success of the achievement for this study.
Abbreviations
ANC, Antenatal Care; AOR, Adjusted Odd Ratio; CI, Confidence Interval; EDHS, Ethiopian Demographic and Health Survey; FANC, Focused Antenatal care; IMR, Infant Mortality Rate; MMR, Maternal Mortality Rate; WHO, World Health Organization.
References
1. Grum T, Brhane E. Magnitude and factors associated with late antenatal care booking on first visit among pregnant women in public health centers in central zone of Tigray Region, Ethiopia: a cross sectional study. PLoS ONE. (2018) 13:e0207922. doi: 10.1371/journal.pone.0207922
2. Tekelab T, Chojenta C, Smith R, Loxton D. Factors affecting utilization of antenatal care in Ethiopia: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0214848. doi: 10.1371/journal.pone.0214848
3. Downe S, Finlayson K, Tunçalp Ö, MetinGülmezoglu A. What matters to women: a systematic scoping review to identify the processes and outcomes of antenatal care provision that are important to healthy pregnant women. BJOG. (2016) 123:529–39. doi: 10.1111/1471-0528.13819
5. Geta MB, Yallew WW. Early initiation of antenatal care and factors associated with early antenatal care initiation at health facilities in southern Ethiopia. Adv Public Health. (2017) 2017:1–6. doi: 10.1155/2017/1624245
6. Kisuule I, Kaye DK, Najjuka F, Ssematimba SK, Arinda A, Nakitende G, et al. Timing and reasons for coming late for the first antenatal care visit by pregnant women at Mulago hospital, Kampala Uganda. BMC Preg Childbirth. (2013) 13:1–7. doi: 10.1186/1471-2393-13-121
7. Ebonwu J, Mumbauer A, Uys M, Wainberg ML, Medina-Marino A. Determinants of late antenatal care presentation in rural and peri-urban communities in South Africa: a cross-sectional study. PLoS ONE. (2018) 13:e0191903. doi: 10.1371/journal.pone.0191903
8. Wolde F, Mulaw Z, Zena T, Biadgo B, Limenih MA. Determinants of late initiation for antenatal care follow up: the case of northern Ethiopian pregnant women. BMC Res Notes. (2018) 11:1–7. doi: 10.1186/s13104-018-3938-9
10. Zegeye AM, Bitew BD, Koye DN. Prevalence and determinants of early antenatal care visit among pregnant women attending antenatal care in Debre Berhan Health Institutions, Central Ethiopia. Afr J Reprod Health. (2013) 17:130–6.
11. Ali SA, Dero AA, Ali SA, Ali GB. Factors affecting the utilization of antenatal care among pregnant women: a literature review. J Preg Neonatal Med. (2018) 2:14–45. doi: 10.35841/neonatal-medicine.2.2.41-45
12. Berhe KK, Welearegay HG, Abera GB, Kahsay HB, Kahsay AB. Assessment of antenatal care utilization and its associated factors among 15 to 49 years of age women in AyderKebelle, Mekelle City 2012/2013; a cross-sectional study. Am J Adv Drug Deliv. (2014) 62:75. Available online at: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.678.1745&rep=rep1&type=pdf
13. Asifere WN, Tessema M, Tebeje B. Clients' satisfaction with health care providers' communication and associated factors among pregnant women attending antenatal care in Jimma town public health facilities, Jimma zone, southwest. Int J Pregnancy Child Birth. (2018) 4:223–30. doi: 10.15406/ipcb.2018.04.00113
14. Sema A, Alemayehu T, Belay Y, Desalew A, Tekle Y, Roba KT. Late initiation of antenatal care and its associated factors among pregnant women in dire Dawa, Eastern Ethiopia. EAJHBS. (2020) 4:47–58. Available online at: https://www.researchgate.net/publication/344037425_Late_Initiation_of_Antenatal_Care_and_Its_Associated_Factors_among_Pregnant_Women_in_Dire_Dawa_Eastern_Ethiopia
15. Kebede DB, Belachew YB, Selbana DW, Gizaw AB. Maternal satisfaction with antenatal care and associated factors among pregnant women in Hossana town. Int J Reprod Med. (2020) 2020:2156347. doi: 10.1155/2020/2156347
16. Ftwi M, Gebretsadik GG, Berhe H, Haftu M, Gebremariam G, Tesfau YB. Coverage of completion of four ANC visits based on a recommended schedule in Northern Ethiopia: a community-based cross-sectional study design. PLoS ONE. (2020) 15:e0236965. doi: 10.1371/journal.pone.0236965
17. Gejea T, Abadiga M, Hasen T. Maternal satisfaction with delivery services of government hospitals in Ambo Town, West Shoa Zone, Oromia Region, Ethiopia, 2020. Patient Prefer Adherence. (2020) 14:1225. doi: 10.2147/PPA.S251635
18. Awasthi MS, Awasthi KR, Thapa HS, Saud B, Pradhan S, Khatry RA. Utilization of antenatal care services in dalit communities in Gorkha, Nepal: a cross-sectional study. J Pregnancy. (2018) 2018:1–8. doi: 10.1155/2018/3467308
19. Bekana M, Negash S, Yusuf L. Client satisfaction on antenatal care service by pregnant women in public and private hospitals in Addis Ababa, Ethiopia: a cross-sectional comparative descriptive study. J Gynecol Reprod Med. (2020) 4:1–8. doi: 10.33140/JGRM.04.01.06
20. Tadese E, Mirkuzie W. Quality of Antenatal services of public health facilietes Northest Ethiopia. BMC Health Serv Res. (2013) 13:443. doi: 10.1186/1472-6963-13-443
21. Selgado MB, Dukele YH, Amamo DD. Determinants of focused antenatal care service satisfaction in public health facilities in Ethiopia 2018: a mixed study design. JPHE. (2019) 11:158–69. doi: 10.5897/JPHE2019.1154
22. Gulema H, Berhane Y. Timing of first antenatal care visit and its associated factors among pregnant women attending public health facilities in Addis Ababa, Ethiopia. Ethiop J Health Sci. (2017) 27:139–46. doi: 10.4314/ejhs.v27i2.6
23. Ejeta E, Dabsu R, Zewdie O, Merdassa E. Factors determining late antenatal care booking and the content of care among pregnant mothers attending antenatal care services in East Wollega administrative zone, West Ethiopia. Pan Afr Med J. (2017) 27:184. doi: 10.11604/pamj.2017.27.184.10926
24. Ndidi EP, Oseremen IG. Reasons were given by pregnant women for late initiation of antenatal care in the Niger Delta, Nigeria. Ghana Med J. (2010) 44:47–51. doi: 10.4314/gmj.v44i2.68883
25. Tolefac PN, Halle-Ekane GE, Agbor VN, Sama CB, Ngwasiri C, Tebeu PM. Why do pregnant women present late for their first antenatal care consultation in Cameroon? Matern Health Neonatol Perinatol. (2017) 3:1–6. doi: 10.1186/s40748-017-0067-8
26. Gebresilassie B, Belete T, Tilahun W, Berhane B, Gebresilassie S. Timing of first antenatal care attendance and associated factors among pregnant women in public health institutions of Axum town, Tigray, Ethiopia, 2017: a mixed design study. BMC Pregnancy Childbirth. (2019) 19:1–1. doi: 10.1186/s12884-019-2490-5
27. Tekelab T, Berhanu B. Factors associated with late initiation of antenatal care among pregnant women attending antenatal clinic at public health centers in Kembata Tembaro zone, southern Ethiopia. Sci Technol Arts Res J. (2014) 3:108–15. doi: 10.4314/star.v3i1.17
28. Weldemariam S, Damte A, Endris K, Palcon MC, Tesfay K, Berhe A, et al. Late antenatal care initiation: the case of public health centers in Ethiopia. BMC Res Notes. (2018) 11:1–6. doi: 10.1186/s13104-018-3653-6
29. Tufa G, Tsegaye R, Seyoum D. Factors associated with timely antenatal care booking among pregnant women in remote area of bule Hora District, Southern Ethiopia. Int J Womens Health. (2020) 12:657–66. doi: 10.2147/IJWH.S255009
30. Ewunetie AA, Munea AM, Meselu BT, Simeneh MM, Meteku BT. DELAY on first antenatal care visit and its associated factors among pregnant women in public health facilities of Debre Markos town, North West Ethiopia. BMC Pregnancy Childbirth. (2018) 18:173. doi: 10.1186/s12884-018-1748-7
31. Kolola T, Morka W, Abdissa B. Antenatal care booking within the first trimester of pregnancy and its associated factors among pregnant women residing in an urban area: a cross-sectional study in DebreBerhan town, Ethiopia. BMJ Open. (2020) 10:e032960. doi: 10.1136/bmjopen-2019-032960
32. Gashaw BT, Magnus JH, Schei B. Intimate partner violence and late entry into antenatal care in Ethiopia. Women Birth. (2019) 32:e530–7. doi: 10.1016/j.wombi.2018.12.008
33. Tola W, Negash E, Sileshi T, Wakgari N. Late initiation of antenatal care and associated factors among pregnant women attending antenatal clinic of Ilu Ababor Zone, southwest Ethiopia: a cross-sectional study. PLoS ONE. (2021) 16:e0246230. doi: 10.1371/journal.pone.0246230
34. Ethiopian Public Health Institute Federal Federal Ministry of Health Addis Ababa Ethiopia and and The DHS Program ICF. Mini Demographic and Health Survey 2019—Key Indicators. (2019). Rockville, MD: Elsevier Ltd.
35. Sinyange N, Sitali L, Jacobs C, Musonda P, Michelo C. Factors associated with late antenatal care booking: population based observations from the 2007 Zambia demographic and health survey. Pan Afr Med J. (2016) 25:109. doi: 10.11604/pamj.2016.25.109.6873
36. Emelumadu OF, Ukegbu AU, Ezeama NN, Kanu OO, Ifeadike CO, Onyeonoro UU, et al. Socio-demographic determinants of maternal health-care service utilization among rural women in Anambra state, South East Nigeria. Ann Med Health Sci Res. (2014) 4:374–82. doi: 10.4103/2141-9248.133463
37. Baker EC, Rajasingam D. Using trust databases to identify predictors of late booking for antenatal care within the UK. Public Health. (2012) 126:112–6. doi: 10.1016/j.puhe.2011.10.007
38. Mulat G, Kassaw T, Aychiluhim M. Antenatal care service utilization and its associated factors among mothers who gave live birth in the past one year in Womberma Woreda, north west Ethiopia. Epidemiology. (2015). S2:1. doi: 10.4172/2161-1165.S2-003
39. Abame DE, Abera M, Tesfay A, Yohannes Y, Ermias D, Markos T, et al. Relationship between unintended pregnancy and antenatal care use during pregnancy in Hadiya Zone, Southern Ethiopia. J Reprod Infertil. (2019) 20:42.
40. Manzi A, Munyaneza F, Mujawase F, Banamwana L, Sayinzoga F, Thomson DR, et al. Assessing predictors of delayed antenatal care visits in Rwanda: a secondary analysis of Rwanda demographic and health survey 2010. BMC Pregnancy Childbirth. (2014) 14:290. doi: 10.1186/1471-2393-14-290
Keywords: late initiation, antenatal care, pregnant, women, Gedo Hospital, Ethiopia
Citation: Debelo BT and Danusa KT (2022) Level of Late Initiation of Antenatal Care Visit and Associated Factors Amongst Antenatal Care Attendant Mothers in Gedo General Hospital, West Shoa Zone, Oromia Region, Ethiopia. Front. Public Health 10:866030. doi: 10.3389/fpubh.2022.866030
Received: 30 January 2022; Accepted: 25 May 2022;
Published: 20 June 2022.
Edited by:
Li Chen, Augusta University, United StatesReviewed by:
Tolulope Olumide Afolaranmi, University of Jos, NigeriaAnthony Pascual Calibo, Food and Nutrition Research Institute (DOST—FNRI), Philippines
Copyright © 2022 Debelo and Danusa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kababa Temesgen Danusa, a2FiZXRlbWVzZ2VuQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Bikila Tefera Debelo
Bikila Tefera Debelo Kababa Temesgen Danusa
Kababa Temesgen Danusa