
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 14 March 2022
Sec. Environmental Health and Exposome
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.861836
This article is part of the Research Topic The Built Environment and Public Health: New Insights View all 44 articles
Introduction: Health deterioration among frail older adults is a public health concern. Among the multi-dimensional factors, the neighborhood built environment is crucial for one's health. Although the relationship between the built environment and health in the general population has been thoroughly investigated, it has been ignored in the case of frail older adults, who may have difficulties in their daily basic living skills. A path analysis is constructed to model the proposed theoretical framework involving the neighborhood built environment and health among frail older adults. This study thus aims to investigate the environmental influences on health, and to validate the theoretical framework proposed for health and social services.
Methods: This study used secondary data collected in Hong Kong. A sample of 969 older community dwellers aged 60 or above were frail with at least one activity of daily living. Demographic information, neighborhood built environment data, service utilization, and health conditions were collected from these participants and their caregivers. A path analysis was performed to examine the proposed theoretical framework.
Results: The health condition was of general concern, including frailty and incapacities in daily activities in frail older adults. Besides psychosocial factors, service use, and caregivers' care quality, the built environment had a significant impact on the health of older adults as well. Specifically, more facilities offering services and groceries, a shorter distance to the nearest metro station, and more greenery exposure are associated with a better-expected health condition among frail older adults.
Discussion: The proposed theoretical framework successfully supplements past negligence on the relationship between the built environment and the health of frail older adults. The findings further imply that policymakers should promote the usability of transit and greenery in neighborhoods and communities. In addition, service utilization should be improved to meet the basic needs of frail older adults in the communities.
In Hong Kong, adults aged 60 and over represented more than one-sixth of the total population, while the prevalence of aging is estimated to exceed 30% in 2041 (1). Among this aging population, the prevalence of frailty with underlying health conditions is reportedly more than 50% (2, 3). Frail older adults are identified as being weak, with complex medical problems, impaired mental abilities, compromised ability for independent living, and often in need of assistance for daily activities (4). Worsening health and preventive risk factors have traditionally been priorities in public health policy for frail older adults (5, 6). Declining health is a complex state involving multi-dimensional aspects (7). Commonly used indices measuring health conditions include frailty level, activities of daily living, and instrumental activities of daily living. The frailty level refers to physical, psychological and social aspects (8). Activities of daily living refer to a person's basic functional status in daily living (e.g., eating); while instrumental activities of daily living requires a higher extent of functional skills (e.g., financial management) in daily living scenarios (9).
Among all the preventive factors for deteriorating health, several critical components are the necessity to facilitate improvement in the health of frail older adults. The health promotion system will not function well without these critical components: the neighborhood built environment, and two intermediate factors—service utilization and caregivers' quality of life. Studies have shown that the neighborhood built environment among potential risk factors plays a decisive role cause declining health in frail older adults (10). The significance of the neighborhood built environment in health studies has drawn the noticeable attention of public health and gerontology scholars over the past few decades (11, 12). For example, a deficiency of environmental greenery has been reported to adversely affect residents' health and daily living capacities (13). The paucity of social services facilities is considered to compromise one's living conditions, while deficits in mobility and transportive approaches limit people's walkability and physical mobility (14, 15). On the contrary, sufficiently available greenery, social service and grocery facilities, and transit in a sustainable society with well-designed urban planning are greatly beneficial to the physical, psychological, and social aspects of human beings in their daily living scenarios (10). Moreover, professional services, such as Integrated Home Care Services, have been initiated and planned by the Hong Kong government and Social Welfare Department for frail older adults (16). Despite the expected values of services provided in the neighborhood built environment, the services do not fully meet the needs of frail older adults and are poorly utilized by the targeted frail aging population if their caregivers are not involved (17). Frail older adults commonly have impaired independent living abilities and are dependent on assistance to perform their daily activities (18). Caregivers are the main workforce among formal and informal caregivers to take care of frail older adults and support their frailty in their physical mobility, psychological stability, and social interactions (19). Therefore, with the aids from caregivers in the family, frail older adults are able to access the resources in the neighborhood environment and take advantages of services that are available to them in the communities. In this sense, caregivers' quality of life determines their care quality and eventually benefit the frail older adults. Poor quality of life is generally associated with low care quality provided and declining health among frail older adults (18).
To sum, the existing literature fails to tackle two prominent concerns in this proposed framework integrating neighborhood built environment factors, intermediate factors, and health outcomes of frail older adults. First, there has been less recognition of the importance of the built environment in the neighborhood in relation to the intermediate variables and the health outcomes of frail older adults. Second, factors contributing to the health conditions of frail older adults have been investigated sporadically without comprehensive theoretical guidance. Therefore, this study aims to 1) investigate whether the neighborhood built environment influences the service use and health; 2) validate a theoretical framework proposed to interpret frail older adults' health conditions that take into account environmental factors, social services use, and caregivers' quality of life by using the path analysis method.
The relationship between the neighborhood built environment and frail older adults' health has been weakly established due to critical negligence of intermediate components linking the neighborhood environment and health. To best develop a practical conceptual framework, that balances between robustness and parsimony in theoretical development, the Andersen's Model and Stress-Adaptation Model are integrated into our proposed theoretical framework with two essential intermediate components: service use and caregiver's quality of life.
The Andersen's Model is commonly known as the Andersen healthcare utilization model. This model has been an essential framework for diagnosing factors associated with the use of healthcare services (20). This overarching health model underscores the importance of service use to sustain community health and offers potential policy and clinical implications in promoting frail older adults' health conditions. The health condition of frail older adults, according to the Andersen's Model, comprises three aspects: frailty, activities of daily living (ADL), and instrumental activities of daily living (IADL). Frailty in older adults is often accompanied with a lower level of physical and social activities, worse body control, slowed cognitive reactions, physical and cognitive fatigue, and unforeseen weight loss (21). Besides frailty, these older adults also suffer from challenges in their daily life. ADL and IADL are the major indices to measure such challenges. ADL mainly refers to self-care tasks, which are the necessary things that people have to do daily, from getting up in the daytime till going to bed in the nighttime. Given various versions of ADL measurements, the ADL items are commonly identified as in the following: get up from bed or out of a chair, get dressed, personal and toilet hygiene, bathing and showering, eating, walking, climbing stairs, and other responses to safety (22, 23). On the other hand, IADL was identified for older community dwellers and its items relate to one's independent living abilities that enable one to walk out of home or take care of oneself independently, such as cooking for oneself, taking medicines on time, doing grocery or laundry, paying bills and going to banks on one's own (23, 24).
The Andersen's Model categorizes influential factors into three parts: predisposing factors, enabling factors, and need factors. Predisposing factors usually refer to sociodemographic characteristics that direct one's perception of service utilization. Enabling factors refer to resources or capacities that influence service utilization. Need factors refer to one's needs and demands for services due to illness or impairment (e.g., positive or negative attitude) (25, 26). In the context of older adults with frailty and inabilities in daily activities, our “predisposing factors” should at least include demographic information such as age, gender, educational level, and living arrangement. It is indicated that older adults from diverse demographic groups have different behaviors in service use. For example, female older adults are more aware of using available services to benefit their health, whereas males receive services when they desperately need them (27). Old olds, in general, use the services more often than young olds (28). Studies also show that people with a higher level of educational attainment are more likely to use services (29). The “enabling factor” refers to caregivers' perceptions of stress in their daily caregiving. Since caregivers frequently perceive caregiving stress, counseling and respite services may help alleviate their anxiety and psychological burden (30). The “need factor” refers to the needs for services provided to both frail older adults and their caregivers. The need for services is crucial in the process of service utilization. Community and social services sometimes may not appropriately address the actual expressed needs from both frail older adults and caregivers, leading to unmet needs and worsened life experiences among the population as well as the low cost-effectiveness of community services (25). More frequent service use is found among older adults and their caregivers with high service needs (31). Frail older adults have basic needs for assistance with their daily living activities, such as dining, bathing, and mobility, as well as some activities that require an advanced cognitive functioning level, such as financial management and commuting (9). Even though the neighborhood built environment was not explicitly included in the earlier version of the Andersen's Model, recent empirical studies emphasized the necessity to associate service utilization with environmental factors in building a sustainable society (32). Neighborhoods with functioning social organizations and desirable accessibility show high utilization of services for frail older adults with complex needs dwelling at home (33). In addition, the built environment, such as transportation and green spaces, affect local health care utilization and residents' health and wellbeing (34).
In sustaining a decent level of health, according to the Stress-Adaptation Model, the caregiver's quality of life (QoL) is another crucial intermediate component as the caregiver is an irreplaceable agent in our proposed health framework. For daily activities, frail older adults who have lost their independent living abilities heavily depend on caregivers in their daily activities (18). Caregivers, being the backbone among all formal and informal caregivers, have extra responsibilities beyond their own personal life, such as providing emotional support, accompanies in daily dining, toileting, commute, and activities, contacting medical professionals, tracking treatment and medications, coordinating care with other family members, keeping family and relatives informed, making financial and legal arrangement (35). Consequently, these caregivers suffer greatly from physical exhaustion, psychological stress, and social isolation as their lives are occupied by daily care responsibilities (36). Moreover, caregiving stress and burden lead to dissatisfaction with the support or services provided (37), or unwillingness to seek the services because they prioritize the services for frail older adults over the ones for themselves (38). Besides, stressed caregivers broadly report a low QoL (39). More importantly, some caregivers with deteriorated QoL develop severe mental disturbance, such as depression or anxiety, which further cause mental breakdown and inabilities to care for their frail older family members any longer (40, 41). Therefore, The intertwined QoL of caregivers and the health of frail older adults can easily develop a vicious cycle, in which worse QoL leads to declined health owing to worse care quality, whereas a miserable health condition increases more caregiving stress that adversely affects QoL (18). The Stress-Adaptation Model also assumes caregivers, who inevitably experience high levels of stress with a lower QoL, may have compromised quality of care and expect an adverse health outcome among their frail care recipients (42). Empirical studies demonstrate that improved QoL of caregivers results in better care and reduced incidences of frailty and functioning incapacities in the daily activities of their frail care recipients (18, 43, 44).
In summary, by adopting the Andersen's Model and the Stress-Adaptation Model, our proposed theoretical framework incorporates the neighborhood built environment while involving intimate caregiver partners to interpret the potential factors influencing the health condition of frail older adults. The intermediate variables, service uses and caregivers' QoL, associated with health outcomes can be jointly attributed to individual and environmental factors. Neighborhood built environmental factors also contribute to improved use of services and better QoL of caregivers. Improved use of services and QoL of caregivers are found associated with greenery, social service and grocery facilities, whereas the distances to the transit discourage service use and lower caregiver's QoL (13, 17). Supported by the aforementioned Andersen's Model for health services and the Stress-Adaptation Model on caregivers' QoL, this study aims to gain a clear understanding on how the neighborhood built environment influences the service use and health.
This study used secondary data derived from a large project undertaken in Hong Kong. The study with the original data investigates the health condition and service needs of Hong Kong older community dwellers and their family caregivers in 2018 (45). Participants were recruited from all districts in Hong Kong via (1) the community centers, and (2) companies and social organizations. Structured questionnaires administered by trained researchers were distributed to collect quantitative information. Demographics and health conditions of both the family caregiver and the CR in each dyad were interviewed and reported by the caregivers.
A total of 969 family caregivers were selected for this study by our preset criteria, which include 1) the CRs (care recipients—older adults) were aged 60 or above, 2) the CRs had one or more difficulties in both the Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) lists since the past 3 months, and 3) they were the primary family caregivers of the CRs. On the other hand, the CRs aged below 60, had no difficulty in ADL and/or IADL, or had no caregiver were excluded from our study.
The measurements in this study cover outcome variables, intermediate variables, neighborhood variables, and individual variables following an integration of the Andersen's Model and the Stress-Adaptation Model (Figure 1).
The health conditions in this study included two major components: activities of daily functioning and frailty level. To begin with activities of daily functioning, ADL being one of the essential scales measured one's abilities in engaging in activities of daily living, comprising personal hygiene, toileting, eating, etc. whereas, IADL measured one's abilities in performing more advanced or instrumental activities of daily living, including financial management, food preparation, laundry, etc. (46, 47). ADL included 6 items on a two-point scale (1—need assistance to do it; 0—can do it independently); and IADL included 11 items on a two-point scale (1—need assistance to do it; 0—can do it independently). Second, to measure one's frailty level, the frailty scale was used to consist of 16 items that separately evaluated physical, cognitive, psychological and social aspects of frailty, such as falling history, memory loss, depressiveness, and insufficient social support. The frailty scale used a three-point Likert scale including options of 0 (no such symptom), 1 (sometimes), and 2 (very much likely). Lower scores in the above-mentioned three scales indicated better conditions of ADL, IADL, and frailty.
Two critical intermediate variables that lead to sustainable health conditions included quality of life (QoL) and service use. The QoL was measured based on the perceived adaptation level of caregivers to balance their life and care tasks. The QoL used a one-item question with 6 options ranging from 1 (well-balanced life) to 6 (hardly balanced life). A lower score indicated better QoL.
Service use condition was evaluated using a six-point scale with two options (1—have used the service; 0—have not used the service). Services covered community-provided paid and unpaid programs that facilitate emotional support, rehabilitation, counseling, nursing skills, financial assistance, and employment training for older adults and their caregivers. A higher score indicated more frequent use of services.
The neighborhood built environment variables refer to the physical and built environment in the proximity of the residence. First, the physical and built environment consisted of the commonly interactive environment such as greenery in the living environment, social service facilities (e.g., retail, banks, post offices, rehabilitation and daycare centers, etc.), grocery (e.g., markets, shopping, restaurants, etc.), transit (e.g., buses, metro, taxis, etc.), and greenery (green spaces in public area, parks, and open grounds). While each participant's residential place was recorded as coordinates in the GIS system, the neighborhood built environment was analyzed in the vicinity of the given coordinates (48). For instance, the service facilities were measured by counting the number of facilities in the vicinity of 1,000 m. The grocery variable also recorded the total amount of markets, shopping, restaurants within the 1 km range away from each participant. For transit, the distance of the nearest metro station to one's residence was calculated. The greenery index was measured using google street view photos at a 100-meter interval covering each resident's neighborhood in a radius of 1 km. Within each extracted panoramic photo, the proportion of greenery area over the overall area in pixels was calculated using the machine learning technique (49–52).
Caregiving stress measured the stress and burden perceived during one's caregiving experiences. Caregiving burden and stress were measured using the short version of the Zarit Burden Interview (ZBI-4) (53, 54). ZBI consisting of 4 items on the ratings of the 5-point scale (1—“never” to 5—“very often”) had scores ranging from 4 to 20. Higher scores indicated greater stress perceived.
Service need was measured using a need list of items whether the older adults wanted to address. The items in the need list included nine common illnesses such as arthritis, mild cognitive impairment, high blood pressure, etc. Two options were provided: 1—need for services, and 0—no need for service.
The covariate variables for caregivers included age (in years), gender (1—female, 2—male), and education attainment (1—none, 2—primary diploma, 3—secondary diploma, 4—college diploma, 5—graduate diploma or above). On the other hand, the older adults (CRs) had their age (in years), gender (1—female, 2—male), and homestay (0—living separately, 1—living together with the caregiver) were collected.
Descriptive statistics of the covariate, individual, environmental, and intermediate variables of both older adults and their caregivers were analyzed. To have a comprehensive view on the overall model, a path analysis was used to explore the relationships between the outcome, intermediate, environmental, individual, and covariate variables. Path analysis is a form of multiple regression statistical analysis method to modeling relationships between multiple dependent variables and multiple layers of independent variables. Partial regression coefficients were estimated for causal relationships between variables. Being a subtype of structural equation modeling, the exogenous and endogenous effects were both analyzed for detecting variances overly explained by covariate variables. The exogenous and endogenous effects were eventually eliminated according to the preliminary results showing that the variances explained by covariate variables majorly contributed to the path analysis model. We used R (version 4.1.0) to estimate this path analysis model with the adjusted maximum likelihood method.
According to the descriptive statistics in our findings, the older adults had an average age of 81-year-old (SD = 8.33), more males (62.4%) than females, tended to live together with their family members (95.0%). For their caregivers, the average age was 70.1 (SD = 10.8), there were more female caregivers (80.5%; including spouses and daughters). Educational attainment of caregivers were predominantly secondary school or below (90.2%) (Table 1).
At the individual level, ZBI was scored 12.5 (SD = 5.18), indicating moderately high caregiving stress perceived by the caregivers. The service need from the older adults was counted around 4 (SD = 1.78), indicating a moderate need for services. At the environment level within 1 km range of the participants' residence, there were 10 (M = 10.1, SD = 7.67) facilities providing various social services, 28 (M = 28.5, SD = 26.2) places for groceries, 606 meters of distance away from the nearest metro station (SD = 959), 26.6% of greenery exposure in the neighborhood (SD = 16.9%). At the intermediate level, caregivers' QoL score was 3.07 (SD = 2.02), indicating a moderate level of life quality. Their service use condition was 1.07 (SD = 1.13), indicating a low level of service use.
The health conditions of the older adults were generally moderately worrying. Their frailty was scored 14.5 (SD = 4.40), indicating a moderate frailty level. They had moderately high scores in both ADL (M = 4.51, SD = 1.73) and IADL (M = 7.11, SD = 2.53).
A correlational analysis was performed to examine collinearity between independent variables and verify the validity of using these variables in the same model (Figure 2). Collinearity is a critical issue to avoid as it can cause biased estimations in path analysis using any regression method. The correlational result showed that the absolute value of correlational coefficients among all variables ranged between 0 and 0.52, indicating mild to moderate collinearities. For the inherently highly correlated neighborhood built environment variables, their correlational coefficients were still acceptable ranging from 0.44 to 0.81. Therefore, these independent variables were all included conditionally in our path analysis.
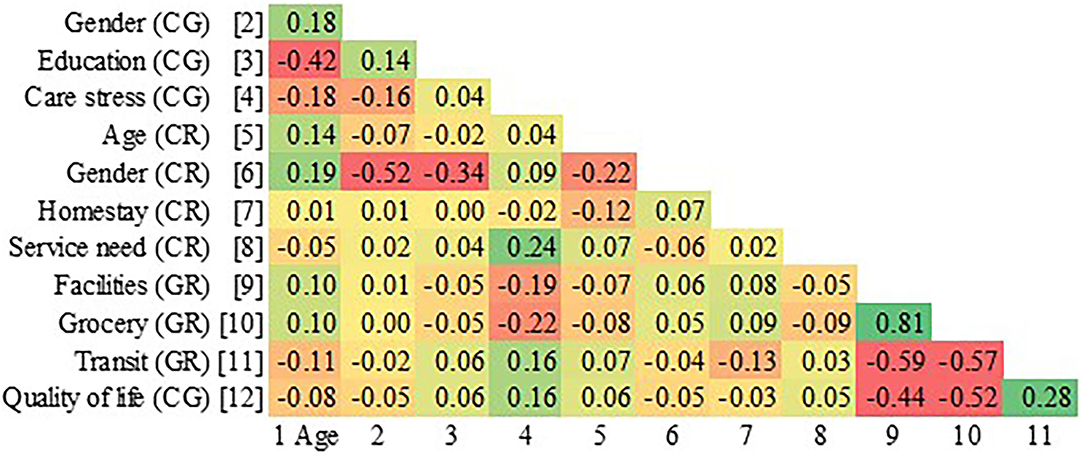
Figure 2. Correlational matrix. CG, caregiver; CR, care recipient/frail older adults; GR, both frail older adults and caregivers.
The path analysis model was preliminarily evaluated with the goodness-of-fit estimations (Table 2). The path analysis used the unconstrained and box-constrained optimization in the maximum likelihood estimation. This path analysis indicated a robust model (p < 0.001). To measure the model fit, we used various indices, including Akaike's information criteria (24090.99), Bayesian information criteria (24236.44), Sample-size adjusted Bayesian information criteria (24144.33), root mean square error of approximation (0.078), standardized root mean square residual (0.046), comparative fit index (0.957), and Tucker-Lewis index (0.873). All these indices were at an acceptable level.
The results analyzed the direct effects of all paths within the path analysis model. Coefficients for all paths were shown in Tables 3, 4. The statistical framework, only showing significant paths, was demonstrated in Figure 3. There were two major layers in this path analysis: 1) environment, individual, and covariate variables predicting intermediate variables (Table 3); and 2) intermediate variables predicting outcome variables (Table 4).
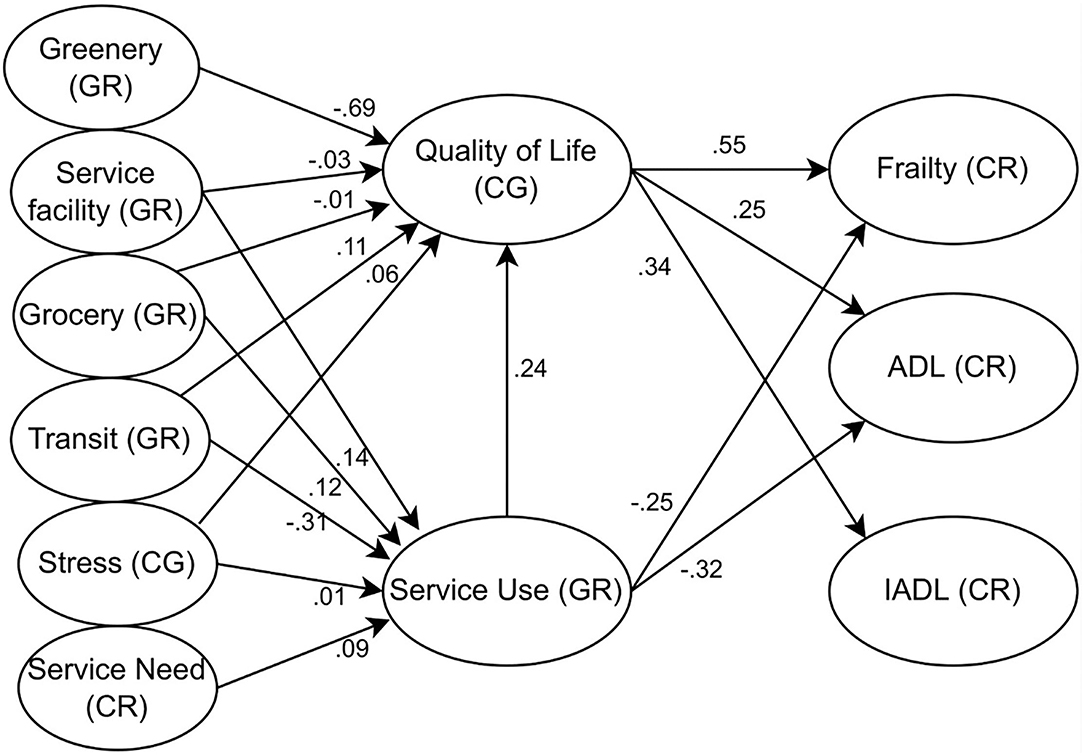
Figure 3. Statistical model. CG, caregiver; CR, care recipient/frail older adults; GR, both frail older adults and caregivers.
In the first layer, shown in Table 3, a higher level of caregivers' QoL was predicted when there were a few more facilities providing social services (B = −0.03, P = 0.034), more grocery shops and markets (B = −0.01, P = 0.009), a shorter distance to the nearest metro station (B = 0.11, P = 0.012), and more greenery exposure (B = −0.69, P = 0.023). A higher level of QoL can be observed among caregivers who were older (B = −0.02, P < 0.001), or males (B = −0.66, P < 0.001). More serve use was associated with more facilities (B = 0.14, P = 0.019), more grocery (B = 0.12, P = 0.045), and a shorter distance to an adjacent metro station (B = −0.31, P = 0.037). Education attainment was insignificantly associated with QoL when controlling for other variables. Service use condition by both older adults and their caregivers were associated with stronger needs for services (B = 0.09, P < 0.001), higher caregiving stress (B = 0.01, P = 0.03). More frequent utilization of services was associated with older adults who were relatively older (B = 0.06, P = 0.012), female (B = −0.05, P = 0.033), and living independently (B = −0.03, P = 0.045).
In the second layer, shown in Table 4, outcome variables were found associated with intermediate and covariate variables. First, a lower frailty level of older adults was associated with a better QoL (B = 0.55, P < 0.001), and a higher frequency of service use (B = −0.25, P = 0.044), younger age (B = 0.06, P = 0.022), females (B = 0.05, P = 0.012), or living together with family members (B = −0.04, P = 0.006). Second, a better ADL functional level was associated with a better QoL (B = 0.25, P < 0.001), and a higher frequency of service use (B = −0.32, P = 0.028), younger age (B = 0.10, P = 0.028), females (B = 0.07, P = 0.042), or living together with family members (B = −0.09, P = 0.010). Last, a better IADL functional level was associated with a better QoL (B = 0.34, P < 0.001), and a lower frequency of service use (B = 0.17, P = 0.045), younger age (B = 0.12, P = 0.038), females (B = 0.09, P = 0.031), or living together with family members (B = −0.11, P = 0.049).
The underlying theoretical framework addressing our research questions was developed based on an integration of the Andersen's Model and the Stress-Adaptation Model including layers of critical components that predict the multi-dimensional health outcome of frail older adults. The Andersen's Model assumes that available services that meet the basic needs of frail older adults and their caregivers are beneficial to their frailty and activities of daily living (20). Application of the Stress-Adaptation Model in aging studies emphasizes the caregiver's role in the caregiving scenario living with a frail older adult and identifies the importance of caregiving stress on the health of older adults (42). Our findings fill in the theoretical gap. First, our findings add new knowledge and extend the application of the Andersen's Model by proposing that the neighborhood built environment factors serve an equivalent weight as individual factors in our proposed framework. Specifically, our findings indicate that the provision of greenery, the feasibility of transit, the density of grocery and social service facilities all evidently improve the acceptance rates of service provided, consequently affecting frail older adults' health outcomes (12). Second, our proposed framework explains the health model more powerfully by involving frail older adults' caregivers. The integration of the Stress-Adaptation Model avoids biased conclusion that can be potentially generated from the Andersen's Model concerning only the party of frail older adults regarding their health conditions. This proposed theoretical framework helps us easily appreciate the daily living scenarios, in which frail older adults and caregivers are generally interdependent. This framework best interprets why home-dwelling frail older adults rely heavily on family caregivers to facilitate their daily lives and promote desirable health status (45).
Policy implications for urban planning underscore the use of transit and greenery in neighborhoods and communities. To begin with, public transportations within walking distance should be the priority in urban planning in encouraging service use and enhancing QoL for community dwellers, who depend on transportations to facilitate service utilization and daily shopping for the maintenance of their basic needs. Both older adults and caregivers have substantially more frequent service use when convenient metro or bus stations are available near their homes (55). Improved QoL is found among older adults who have a desirable transit network, whereas scarcity of necessary transportations near home or close to destinations leads to impaired QoL and a lower potential to meet the needs for daily activities of frail older adults (56–58). In future urban planning for the aging communities with a high density of frail older adults, new bus stops/routes can be established and elevator-assisted metro exists built close to the frail population in order to facilitate their access to services that address their daily needs and health issues (59). Second, sustainable planning on urban greenery improves people's QoL. Humans are naturally attached to environmental greenery, which brings a sedative state and uplifts one's subjective mood. Empirical studies discover that greenery is vital in improving caregivers' life quality, enhancing their care quality, and further promoting frail older adults' health (13, 60). Green spaces also promote the quality of physical activities, such as cycling, hiking and tai chi, and positively reinforce more “green activities” (61, 62). Policymakers in future urban planning can involve environmental greenery and transit for sustainable service delivery and community development. Future environmental greenery planning should extend to small open spaces in the communities and even with the indoor settings in service facilities, which benefit both frail older adults and caregivers.
Our findings inform practices in social services. Improving service use is crucial in preventing frailty and difficulties in daily living. Neighborhood service facilities are imperative to address public health issues and to promote a sustainable age-friendly society. For instance, early screening and home-visiting services provided by the communities are the most fundamental priorities before any long-term services can be scheduled and delivered to the people in need. Accessible early screening for dwelling frail older adults can detect early signs of chronic diseases (e.g., cognitive impairment) that compromises one's capacity in ADL and IADL (e.g., dining, showering, walkability, etc.) and raises risks of emotional exhaustion, incontinence and accidental falls (49, 63). Household or home-visiting services help identify chronic diseases in a timely manner and confirm potential needs for community services. Neighborhood rehabilitation centers are also beneficial in meeting various urgent disease-related needs (17). Service use also benefits families of frail older adults and their caregivers altogether. Improved QoL indicating considerate self-care empowers caregivers to better care for their family members (including frail older adults). Neighborhood daycare and respite centers allow caregivers to have more leisure time beyond their daily care and improve the quality of life and care performance. Support groups sharing similar experiences among caregivers alleviate their emotional breakdown and empower their role identity in providing care. Sustainable social policies should promote diverse and useful social services to meet the basic needs of frail older adults in their daily living activities, followed by training sessions for community workers to ensure that services can be saturated in the target communities. Current social services should still emphasize meeting ADL needs rather than IADL needs as our findings indicate no association between service use and frail older adults' IADL. More advanced community services, such as commute services or financial education services, are not of maximum benefits when the frail older adults are having trouble walking outside freely, taking transportations, or engaging in services that require basic commuting and traveling abilities. Therefore, more basic services, such as home-visiting daycare, chores, and rehabilitation services are needed to support one's ADL difficulties in the preliminary stage of community services.
Among all the limitations in this study, a small sample size being the biggest challenge limits the capacity of making a comparison analysis between gender subgroups, or separately investigating the service use model in populations of frail older adults and caregivers, respectively. Moreover, the measurement of the neighborhood built environment does not address a full spectrum of characteristics of these environmental elements. For instance, distances to the service facilities and grocery stores can be recorded for analysis as this information determines the feasibility of the services provided in the communities. Furthermore, the greenery is found with its significance, yet it is surprisingly not associated with service use. This phenomenon could be due to the fact that the nature of the existing social services does not rely much on environmental greenery. Further investigation is necessary to explore how small green spaces, such as community cornered green or plants in facilities, can stimulate people in need to use services more frequently. Last, the generalizability of this study might be questionable if no future studies validate the theoretical framework in societies of other cultural or social backgrounds (64–68).
Given that the neighborhood built environment factors are absent from the existing knowledge of frail older adults' health status, this study, conducted in Hong Kong with a sample size of 969, uses path analysis to investigate the significance of the urban planning for developing the neighborhood built environment and promotion in service uses. The analysis adopts a comprehensive perspective using the Andersen's health model for frail older adults and the Stress-Adaptation Model for caregivers. The results indicate the neighborhood built environment plays a critical role in promoting the frailty level and assisting capacities for daily living for frail older adults. In particular, more facilities offering services and groceries, a shorter distance to the nearest metro station, and more greenery exposure are associated with a better-expected health condition among frail older adults. In addition, service utilization and caregivers' QoL are indispensable to bridge the limited knowledge for us to understand how the neighborhood built environment can affect one's health. Implications are suggested to involve transit and greenery for urban planning policies, and involve more home-visiting services in the community practice.
The availability of the dataset presented analyzed in this study is not readily available because it belongs to the projects in Kerry Group Service Limited and Sau Po Centre on Ageing. Requests to access these datasets should be directed to Shuangzhou Chen, Y2hlbnNodWFuZ3pob3VAaGt1Lmhr.
The studies involving human participants were reviewed and approved by Human Research Ethics Committee for Non-Clinical Faculties from the University of Hong Kong, Hong Kong (E1808017). The patients/participants provided their written informed consent to participate in this study.
SC is responsible for conceptualization, formal analysis, investigation, methodology, project administration, preparing the original draft, and revisions. TW is responsible for conceptualization, investigation, reviewing, and editing. ZB is responsible for conceptualization, investigation, methodology, project administration, reviewing, and editing. VL is responsible for funding acquisition, data curation, and supervision. All authors agree to be accountable for the content of the work. All authors contributed to the article and approved the submitted version.
This study received funding from the Hong Kong Kerry Group Service Limited (RS180122). The funder was not involved in the study design, collection, analysis, interpretation of data, and the writing of this article or the decision to submit it for publication. The funder had the following involvement with the study: evaluating the original commissioned grant research titled “The profile and service needs of elderly carers.” The funder had not involved in monitoring, evaluating, or providing further funding for this study.
VL, director of Center of Aging, in collaboration with the Hong Kong Council of Social Service were commissioned by the Hong Kong Kerry Group.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to express gratitude toward the contribution of coordinating the project by the Hong Kong Council of Social Service, including Ms. Rachel Szeto, Ms. Crystal Cheng, Ms. Emily Leung, Ms. Rachel Szeto, Ms. Katie Wong, and Ms. Bianca Choi as well as recruitment and interviews conducted by workers from the network of District Elderly Community Centers and Neighborhood Elderly Centers. Special thanks to statistical and GIS support from Olivia Yao, Ivy Zhang, Yanhua Chen, and Sandy Kim.
1. Census Statistics Department. Thematic Report: Older Persons. Hong Kong (2016). Available online at: https://www.statistics.gov.hk/pub/B11201052016XXXXB0100.pdf (accessed December 02, 2021).
2. Santos-Eggimann B, Cuenoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. (2009) 64A:675–81. doi: 10.1093/gerona/glp012
3. Yu R, Wong M, Chong KC, Chang B, Lum CM, Auyeung TW, et al. Trajectories of frailty among Chinese older people in Hong Kong between 2001 and 2012: an age-period-cohort analysis. Age Ageing. (2017) 47:254–61. doi: 10.1093/ageing/afx170
4. Torpy JM, Lynm C, Glass RM. Frailty in older adults. JAMA. (2006) 296:2280. doi: 10.1001/jama.296.18.2280
5. Bai X, Liu C, Baladon L, Rubio-Valera M. Multidimensional determinants of the caregiving burden among Chinese male caregivers of older family members in Hong Kong. Aging Ment Health. (2018) 22:986–95. doi: 10.1080/13607863.2017.1330872
6. Gyasi RM, Phillips DR. Gender, self-rated health and functional decline among community-dwelling older adults. Arch Gerontol Geriatr. (2018) 77:174–83. doi: 10.1016/j.archger.2018.05.010
7. Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. (1998) 13:623–49. doi: 10.1080/08870449808407422
8. Cesari M, Prince M, Thiyagarajan JA, De Carvalho IA, Bernabei R, Chan P, et al. Frailty: an emerging public health priority. J Am Med Dir Assoc. (2016) 17:188–92. doi: 10.1016/j.jamda.2015.12.016
9. Chan ML, Eng CW, Gilsanz P, Whitmer RA, Mungas D, Meyer O, et al. Prevalence of Instrumental Activities of Daily Living (IADL) difficulties and associated cognitive predictors across racial/ethnic groups: findings from the KHANDLE study. J Gerontol B Psychol Sci Soc Sci. (2021) gbab163. doi: 10.1093/geronb/gbab163. [Epub ahead of print].
10. Moore T, Kesten J, López-López JA, Ijaz S, McAleenan A, Richards A, et al. The effects of changes to the built environment on the mental health and well-being of adults: systematic review. Health Place. (2018) 53:237–57. doi: 10.1016/j.healthplace.2018.07.012
11. Rachele JN, Sugiyama T, Davies S, Loh VHY, Turrell G, Carver A, et al. Neighbourhood built environment and physical function among mid-to-older aged adults: a systematic review. Health Place. (2019) 58:102137. doi: 10.1016/j.healthplace.2019.05.015
12. Renalds A, Smith TH, Hale PJ. A systematic review of built environment and health. Fam Community Health. (2010) 33:68–78. doi: 10.1097/FCH.0b013e3181c4e2e5
13. Kondo J M, Fluehr McKeon T, Branas C. Urban green space and its impact on human health. Int J Environ Res Public Health. (2018) 15:445. doi: 10.3390/ijerph15030445
14. Su S, Pi J, Xie H, Cai Z, Weng M. Community deprivation, walkability, and public health: highlighting the social inequalities in land use planning for health promotion. Land Use Policy. (2017) 67:315–26. doi: 10.1016/j.landusepol.2017.06.005
15. Yang L, Liu J, Liang Y, Lu Y, Yang H. Spatially varying effects of street greenery on walking time of older adults. ISPRS Int J Geo Inf. (2021) 10:596. doi: 10.3390/ijgi10090596
16. Chou K-L, Chi I. Comparison between elderly chinese living alone and those living with others. J Gerontol Soc Work. (2000) 33:51–66. doi: 10.1300/J083v33n04_05
17. Fu YY, Chui EWT, Kan WS, Ko L. Improving primary level home and community care services for older people: the case of Hong Kong: improving care services for community-dwelling older people. Int J Soc Welf. (2018) 27:52–61. doi: 10.1111/ijsw.12271
18. Ringer T, Hazzan AA, Agarwal A, Mutsaers A, Papaioannou A. Relationship between family caregiver burden and physical frailty in older adults without dementia: a systematic review. Syst Rev. (2017) 6:55. doi: 10.1186/s13643-017-0447-1
19. Liao M-Y, Yeh C-J, Liao C-C, Lee S-H, Yang S-F, Lee M-C %J EGM. Effects of receiving and providing family support on mortality in non-frail, pre-frail and frail older adults in Taiwan: a 12-year follow-up longitudinal study. Eur Geriatr Med. (2018) 9:679–85. doi: 10.1007/s41999-018-0094-7
20. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
21. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. (2019) 394:1365–75. doi: 10.1016/S0140-6736(19)31786-6
22. Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. (1983) 31:721–7. doi: 10.1111/j.1532-5415.1983.tb03391.x
23. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. (1969) 9:179–86. doi: 10.1093/geront/9.3_Part_1.179
24. Graf C. Functional decline in hospitalized older adults: it's often a consequence of hospitalization, but it doesn't have to be. AJN Am J Nurs. (2006) 106:58–67. doi: 10.1097/00000446-200601000-00032
25. Smith G. Patterns and predictors of service use and unmet needs among aging families of adults with severe mental illness. Psychiatr Serv. (2003) 54:871–7. doi: 10.1176/appi.ps.54.6.871
26. Bradley EH, McGraw SA, Curry L, Buckser A, King KL, Kasl SV, et al. Expanding the andersen model: the role of psychosocial factors in long-term care use. Health Serv Res. (2002) 37:1221–42. doi: 10.1111/1475-6773.01053
27. Allin S, Grignon M, Le Grand J. Subjective unmet need and utilization of health care services in Canada: what are the equity implications? Soc Sci Med. (2010) 70:465–72. doi: 10.1016/j.socscimed.2009.10.027
28. Andersen RM. National health surveys and the behavioral model of health services use. Med Care. (2008) 46:647–53. doi: 10.1097/MLR.0b013e31817a835d
29. Calsyn RJ, Winter JP. Predicting four types of service needs in older adults. Eval Program Plann. (2001) 24:157–66. doi: 10.1016/S0149-7189(01)00006-4
30. Sun Q, Lu N, Jiang N, Lou VWQ. Intention to use respite services among informal care-givers of frail older adults in China: the role of care needs change. Ageing Soc. (2021) 41:101–20. doi: 10.1017/S0144686X20000628
31. Anker-Hansen C, Skovdahl K, McCormack B, Tonnessen S. The third person in the room: the needs of care partners of older people in home care services-A systematic review from a person-centred perspective. J Clin Nurs. (2018) 27:E1309–26. doi: 10.1111/jocn.14205
32. Park G, Evans GW. Environment and Health. In: Llewellyn CD, McManus C, Weinman J, Petrie KJ, Newman S, Ayers S, editors. Cambridge Handbook of Psychology, Health and Medicine. 3rd ed. Cambridge: Cambridge University Press (2019). p. 32–6. Available from: https://www.cambridge.org/core/books/cambridge-handbook-of-psychology-health-and-medicine/environment-and-health/5EFD17A6D38DF80147BE8D3C0989235B
33. Brault MA, Brewster AL, Bradley EH, Keene D, Tan AX, Curry LA. Links between social environment and health care utilization and costs. J Gerontol Soc Work. (2018) 61:203–20. doi: 10.1080/01634372.2018.1433737
34. Cerletti P, Eze IC, Keidel D, Schaffner E, Stolz D, Gasche-Soccal PM, et al. Perceived built environment, health-related quality of life and health care utilization. Devleesschauwer B, editor. PLoS ONE. (2021) 16:e0251251. doi: 10.1371/journal.pone.0251251
35. Máximo RDO, Lopes IC, Brigola AG, Luchesi BM, Gratão ACM, Inouye K, et al. Pre-frailty, frailty and associated factors in older caregivers of older adults. Rev Saúde Pública. (2020) 54:17. doi: 10.11606/s1518-8787.2020054001655
36. Gilhooly KJ, Gilhooly MLM, Sullivan MP, McIntyre A, Wilson L, Harding E, et al. A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatr. (2016) 16:106. doi: 10.1186/s12877-016-0280-8
37. Lopez Hartmann M, De Almeida Mello J, Anthierens S, Declercq A, Van Durme T, Cès S, et al. Caring for a frail older person: the association between informal caregiver burden and being unsatisfied with support from family and friends. Age Ageing. (2019) 48:658–64. doi: 10.1093/ageing/afz054
38. Casado BL, van Vulpen KS, Davis SL. Unmet needs for home and community-based services among frail older Americans and their caregivers. J Aging Health. (2011) 23:529–53. doi: 10.1177/0898264310387132
39. Lien YF, Huang HM. Challenges in intergenerational caregiving for frail older people: a multiple case study. Nurs Health Sci. (2017) 19:81–7. doi: 10.1111/nhs.12314
40. Kim SS, Hayward RD, Reed PG. Self-transcendence, spiritual perspective, and sense of purpose in family caregiving relationships: a mediated model of depression symptoms in Korean older adults. Aging Ment Health. (2014) 18:905–13. doi: 10.1080/13607863.2014.899968
41. Yang F, Ran M, Luo W. Depression of persons with dementia and family caregiver burden: finding positives in caregiving as a moderator. Geriatr Gerontol Int. (2019) 19:414–8. doi: 10.1111/ggi.13632
42. Dorsey K, Purcell S. Roy's adaptation model: principles and general applications. In: Psychiatric and Mental Health Nursing. Boston, MA: Springer US (1990). p. 188–96. Available online at: http://link.springer.com/10.1007/978-1-4899-3011-8_9 doi: 10.1007/978-1-4899-3011-8_9 (accessed January 20, 2022).
43. Amir G, William M, Kristin KW, Tomomi N, Kaname U. Impact of caring for persons with Alzheimer's disease or dementia on caregivers' health outcomes: findings from a community based survey in Japan. BMC Geriatr. (2016) 16:122. doi: 10.1186/s12877-016-0298-y
44. Wells jo N, Cagle CS, Bradley P, Barnes DM. Voices of Mexican American caregivers for family members with cancer: on becoming stronger. J Transcult Nurs. (2008) 19:223–33. doi: 10.1177/1043659608317096
45. Lou VWQ, Lau BHP, Cheung KSL. Positive aspects of caregiving (PAC): Scale validation among Chinese dementia caregivers (CG). Arch Gerontol Geriatr. (2015) 60:299–306. doi: 10.1016/j.archger.2014.10.019
46. Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. (1969) 9:179–186. doi: 10.1097/00006199-197005000-00029
47. Hindmarch I, Lehfeld H, de Jongh P, Erzigkeit H. The Bayer Activities of Daily Living Scale (B-ADL). Dement Geriatr Cogn Disord. (1998) 9:20–6. doi: 10.1037/t58459-000
48. Zagorskas J. GIS-based Modelling and estimation of land use mix in urban environment. Int J Educ Learn Syst. (2016) 1. Available online at: https://www.iaras.org/iaras/filedownloads/ijes/2016/008-0044.pdf.
49. Yang L, Ao Y, Ke J, Lu Y, Liang Y. To walk or not to walk? Examining non-linear effects of streetscape greenery on walking propensity of older adults. J Transp Geogr. (2021) 94:103099. doi: 10.1016/j.jtrangeo.2021.103099
50. Chen J, Lu W, Xue F. “Looking beneath the surface”: a visual-physical feature hybrid approach for unattended gauging of construction waste composition. J Environ Manage. (2021) 286:112233. doi: 10.1016/j.jenvman.2021.112233
51. Chen J, Liu D. Bottom-up image detection of water channel slope damages based on superpixel segmentation and support vector machine. Adv Eng Inform. (2021) 47:101205. doi: 10.1016/j.aei.2020.101205
52. Lu W, Chen J, Xue F. Using computer vision to recognize composition of construction waste mixtures: a semantic segmentation approach. Resour Conserv Recycl. (2022) 178:106022. doi: 10.1016/j.resconrec.2021.106022
53. Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O'Donnell M. The Zarit burden interview: A new short version and screening version. Gerontologist. (2001) 41:652–7. doi: 10.1093/geront/41.5.652
55. Liu Z, Kemperman A, Timmermans H. Influence of neighborhood characteristics on physical activity, health, and quality of life of older adults: a path analysis. Front Public Health. (2021) 9:783510. doi: 10.3389/fpubh.2021.783510
56. Beil K, Hanes D. The influence of urban natural and built environments on physiological and psychological measures of stress— a pilot study. Int J Environ Res Public Health. (2013) 10:1250–67. doi: 10.3390/ijerph10041250
57. Cheng L, De Vos J, Zhao P, Yang M, Witlox F. Examining non-linear built environment effects on elderly's walking: a random forest approach. Transp Res Part Transp Environ. (2020) 88:102552. doi: 10.1016/j.trd.2020.102552
58. Yang L, Chau K, Szeto W, Cui X, Wang X. Accessibility to transit, by transit, and property prices: spatially varying relationships. Transp Res Part Transp Environ. (2020) 85:102387. doi: 10.1016/j.trd.2020.102387
59. Yang L, Chu X, Gou Z, Yang H, Lu Y, Huang W. Accessibility and proximity effects of bus rapid transit on housing prices: heterogeneity across price quantiles and space. J Transp Geogr. (2020) 88:102850. doi: 10.1016/j.jtrangeo.2020.102850
60. He H, Lin X, Yang Y, Lu Y. Association of street greenery and physical activity in older adults: a novel study using pedestrian-centered photographs. Urban For Urban Green. (2020) 55:126789. doi: 10.1016/j.ufug.2020.126789
61. Wu J, Zhao C, Li C, Wang T, Wang L, Zhang Y. Non-linear relationships between the built environment and walking frequency among older adults in Zhongshan, China. Front Public Health. (2021) 9:686144. doi: 10.3389/fpubh.2021.686144
62. Yao W, Chen F, Wang S, Zhang X. Impact of exposure to natural and built environments on positive and negative affect: a systematic review and meta-analysis. Front Public Health. (2021) 9:758457. doi: 10.3389/fpubh.2021.758457
63. Arenas-Castañeda PE, Aroca Bisquert F, Martinez-Nicolas I, Castillo Espíndola LA, Barahona I, Maya-Hernández C, et al. Universal mental health screening with a focus on suicidal behaviour using smartphones in a Mexican rural community: protocol for the SMART-SCREEN population-based survey. BMJ Open. (2020) 10:e035041. doi: 10.1136/bmjopen-2019-035041
64. Bao Z, Laovisutthichai V, Tan T, Wang Q, Lu W. Design for manufacture and assembly (DfMA) enablers for offsite interior design and construction. Build Res Inf. (2021) 1–14. doi: 10.1080/09613218.2021.1966734
65. Bao Z, Lu W, Hao J. Tackling the “last mile” problem in renovation waste management: a case study in China. Sci Total Environ. (2021) 790:148261. doi: 10.1016/j.scitotenv.2021.148261
66. Bao Z, Lu W. A decision-support framework for planning construction waste recycling: a case study of Shenzhen, China. J Clean Prod. (2021) 309:127449. doi: 10.1016/j.jclepro.2021.127449
67. Bao Z, Lee WM, Lu W. Implementing on-site construction waste recycling in Hong Kong: barriers and facilitators. Sci Total Environ. (2020) 747:141091. doi: 10.1016/j.scitotenv.2020.141091
Keywords: older adults, public health, neighborhood built environment, path analysis, Hong Kong
Citation: Chen S, Wang T, Bao Z and Lou V (2022) A Path Analysis of the Effect of Neighborhood Built Environment on Public Health of Older Adults: A Hong Kong Study. Front. Public Health 10:861836. doi: 10.3389/fpubh.2022.861836
Received: 25 January 2022; Accepted: 16 February 2022;
Published: 14 March 2022.
Edited by:
Yu Ye, Tongji University, ChinaCopyright © 2022 Chen, Wang, Bao and Lou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhikang Bao, dTMwMDQ3MDBAaGt1Lmhr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.