- 1Department of School Health, Yunnan Provincial Center for Disease Control and Prevention, Kunming, China
- 2Public Health School, Kunming Medical University, Kunming, China
- 3Public Health School, Dali University, Dali, China
- 4School of Economics and Management, Kunming University of Science and Technology, Kunming, China
- 5Cardiac Ultrasound Department, Kunming Children's Hospital, Kunming, China
- 6City College, Kunming University of Science and Technology, Kunming, China
- 7Office, Dali Centers for Disease Control and Prevention, Dali, China
- 8School of Economics and Management, Xi'an Jiaotong University, Xi'an, China
- 9Society and People School, Renmin University of China, Peking, China
- 10Infection Control Department, The First People's Hospital of Kunming, Kunming, China
Objectives: To provide us with some evidence to develop more targeted stroke intervention strategies, improve the health awareness of stroke among children, and advocate the health promotion campaign of “small hands holding big hands” among parents and children, we have conducted a health education program on stroke among primary school students in Dali.
Methods: This study has applied stratified random cluster sampling in Dali of Yunnan, China. We compared the improvement of students' knowledge of stroke before and after our health education program in primary school students of Dali in October 2020. Data were collected through 3 rounds of survey by using the same questionnaire.
Results: There were 215 participants aged 7–8 years old sampled in the first phase of the study and 145 participants in the follow-up study. The knowledge of stroke among the participants was relatively low in the pre-intervention survey. After the health education, all the indicators on stroke knowledge were improved. The correct rates in stroke definition, sequelae, and “1-2-0” identification were increased from 0 to 66.05%, to 53.95% and 64.19%, respectively, in both pre-intervention and post-intervention surveys. The correct rate of stroke knowledge was about 4.83–92.41% 3 months after the intervention. The mean score of the questionnaire was 4.25 ± 0.19 in the pre-intervention survey, and that was 15.85 ±0.27 in the post-intervention one. The mean score was 14.02 ± 0.28 post-3-month test. The score in the 3-month survey after the intervention was 11.55% lower than that in the post-intervention score.
Conclusions: The effect of stroke-related knowledge in the health education program for children is improved significantly and this can last for 3 months but it also had attenuation. We should repeat pertinent health education among students.
Introduction
According to the WHO, cardiovascular diseases (CVDs) are the leading cause of death globally, with an estimated 17.9 million lives taken each year. Also, the cause of over four out of five CVD deaths is attributed to heart attacks and strokes (1). Today, China bears a heavy burden of CVD (2). In 2018, the crude death rate of stroke was 149.49/100,000 among Chinese residents, accounting for 22.33% of the total number of deaths. Stroke was ranked as the third leading cause of death in China (3). A study has shown that the incidence of stroke was 6.2% among Bai Ethnic people aged over 35 years in Jianchuan County, Dali of Yunnan in 2018 (4), which was higher than that of adults in China. The rapid changes in lifestyle and dietary habits have made younger people more vulnerable to stroke in recent years (5). Children who had experienced early childhood stroke were at particular risk of alterations in cognitive functions (6). Moreover, epidemiological evidence of stroke burden among Dali residents was lacking. Only patient-specific studies have shown that the factors associated with stroke in Dali residents were age, blood glucose, blood lipids, daily barometric pressure, and daily air temperature (7, 8). Therefore, it is important to improve children's knowledge of stroke and its prevention.
Health education among primary school students has proved to be significantly effective in many studies (9–11). The students were in the critical age of forming the right health concepts with strong learning acceptance, moreover, their health literacy could affect that of the whole family (9, 12, 13). In the Netherlands, students can play a vital role when a stroke occurs by recognizing the signs of a stroke and calling 911 immediately (14). Less research was carried out and reported in China. The reported studies in foreign countries have mainly adopted FAST (Face, Arm, Speech, and Time) to capture a memory in stroke education (15). However, this did not work well due to the language barrier among Chinese adults (16). There have been no related studies on the methods of stroke health education and its effectiveness evaluation among ethnic children.
This study has selected the children as our study population and Dali prefecture as our survey location. It was the first intervention to improve children's stroke awareness in Yunnan. The study aimed to explore the methods of stroke health education for children and to improve children's awareness of stroke health. It is expected to provide us with some evidence for developing more targeted stroke intervention strategies in Yunnan.
Materials and methods
Study design
The study was a follow-up study with data that were generated from the Students' Surveys carried out in Dali of Yunnan from October 2020 to January 2021. The survey was conducted in Dali City of Yunnan province. According to the list of primary schools in Dali City, the survey school was randomly sampled by the end number of the random selecting banknotes. The survey grades and classes were also randomly sampled in the survey school by the end number of the random selecting banknotes. The study participants were recruited by cluster sampling from a sample primary school in Dali City, Yunnan, taking both representativeness and randomness into account. All the students in grades 1 and 2 were eligible to be recruited for our study. We provided stroke health education for the recruited students, and evaluated the educational effect before and after intervention in 2020 and that in 3 months after intervention in 2021. The surveyed students remained consistent from October 2020 to January 2021. Those who were not willing to sign the informed consent were excluded. All participants and/or their parents/guardians provided written informed consent before the survey. There were 215 participants aged 7–8 years old in the first phase of the study. Affected by the epidemic of COVID-19, the follow-up study used an online survey tool WJX.cn (http://www.wjx.cn) to collect data. The contents were kept the same in different surveys of this study. In the follow-up survey, only 145 students met the deadline for the online questionnaire.
Data collection
Data were collected through a questionnaire, which was designed by the research group and used in all the study surveys to measure the participants' understanding of stroke. The questionnaire mainly collects information about the participants' demographic features, their knowledge about stroke and its sources, such as its definition, attacking organ, risk factors, symptoms, identification (three-step method of identification of various problems), treatments, related sequelae, and meanings of about 120 “strokes”. The full score of this questionnaire was 22, with 7 on risk factors of stroke, 5 on typical symptoms, 2 on treatment methods, 4 on sequelae, and 4 on “Stroke 120”.
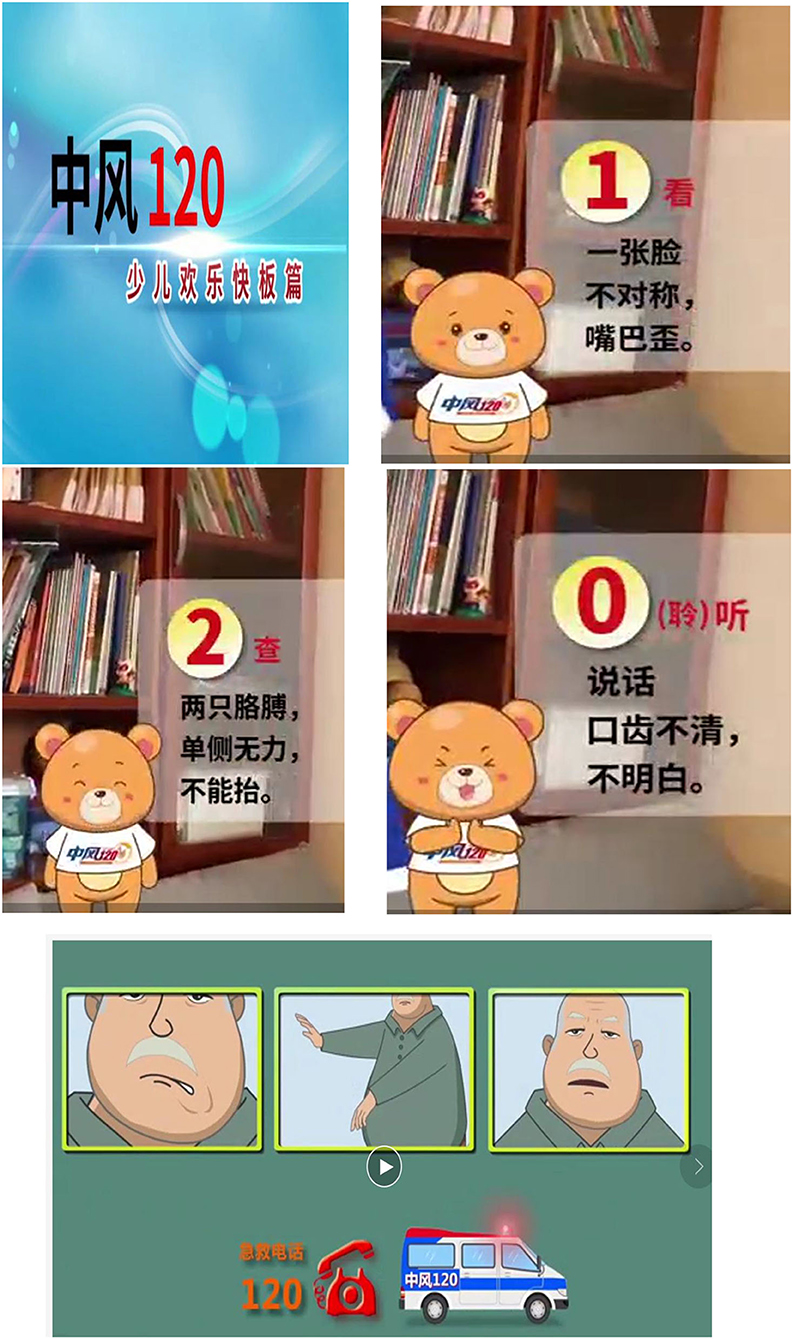
Before the intervention, students filled out the pre-intervention questionnaire, from which we generated our baseline data. Then, participants watched a cartoon educational video, “Stroke 1-2-0” (1-2-0 indicated a three-step identification method) (Figure 1). The message delivered in this video included the following: “1” face droop, “2” arm weakness, “0” speech affected/slurred,” and “120” to call the ambulance. After watching the video, some participants shared their personal experiences about stroke, and what they would have done differently based on their new knowledge learned. After this, a professional investigator performed 1-2-0 again and introduced the meaning of stroke, its risk factors, symptoms, treatments, and related sequelae. The Q and A was finally added to enhance the students' understanding of stroke.
Assessment of the improvement in students' knowledge was carried out twice by the same questionnaires. One was carried out immediately after the education (post-intervention), and the other was 3 months after intervention (follow-up). The three-month follow-up questionnaire was given without noticing and collected data online by a web application of “questionnaire star”. The students had limited time of answering the questions. The students' completion times were studied qualitatively before and after the field intervention (pre-intervention and post-intervention).
Statistical analyses
The primary data analysis was conducted in 2021. All data were analyzed using SPSS 21.0 software. Differences in the mean score of survey questionnaires were compared using the ANOVA test. The correct answer rates for the questionnaire in different surveys (pre-intervention, post-intervention, and follow-up after 3 months) were calculated and stratified by gender, ethnicity, and grade subgroups. Univariate methods were not used to estimate P-value for differences by gender, ethnicity, and grade because high statistical power was achieved from the large sample sizes. Statistical significance was defined as P < 0.05.
Results
Population demography
A total of 215 children of 7- and 8-year-old primary school students were included and intervened, and they completed both pre-intervention and post-intervention questionnaires in October 2020. All of those who had received the intervention and completed survey questionnaires were included in the analysis, with 113 boys and 102 girls. The average age was 7.59 ± 0.49 years old. There were 84 students of Han people, 92 Bai ethnic people, and 39 people of other ethnicities. No significant difference was observed in the distribution of participants between boys and girls (P > 0.05), and only 145 of them completed the follow-up questionnaire in January 2021.
Baseline data in pre-intervention
As shown in Table 1, the Chi-square test found a significant difference in terms of treatments among the students whose mothers held different jobs (x2 = 6.15, P = 0.05) in pre-intervention. There were no differences in other indicators. The students' knowledge of stroke was relatively poor in pre-intervention, especially in its definition, sequelae, and “1-2-0” identification. No one knew them.
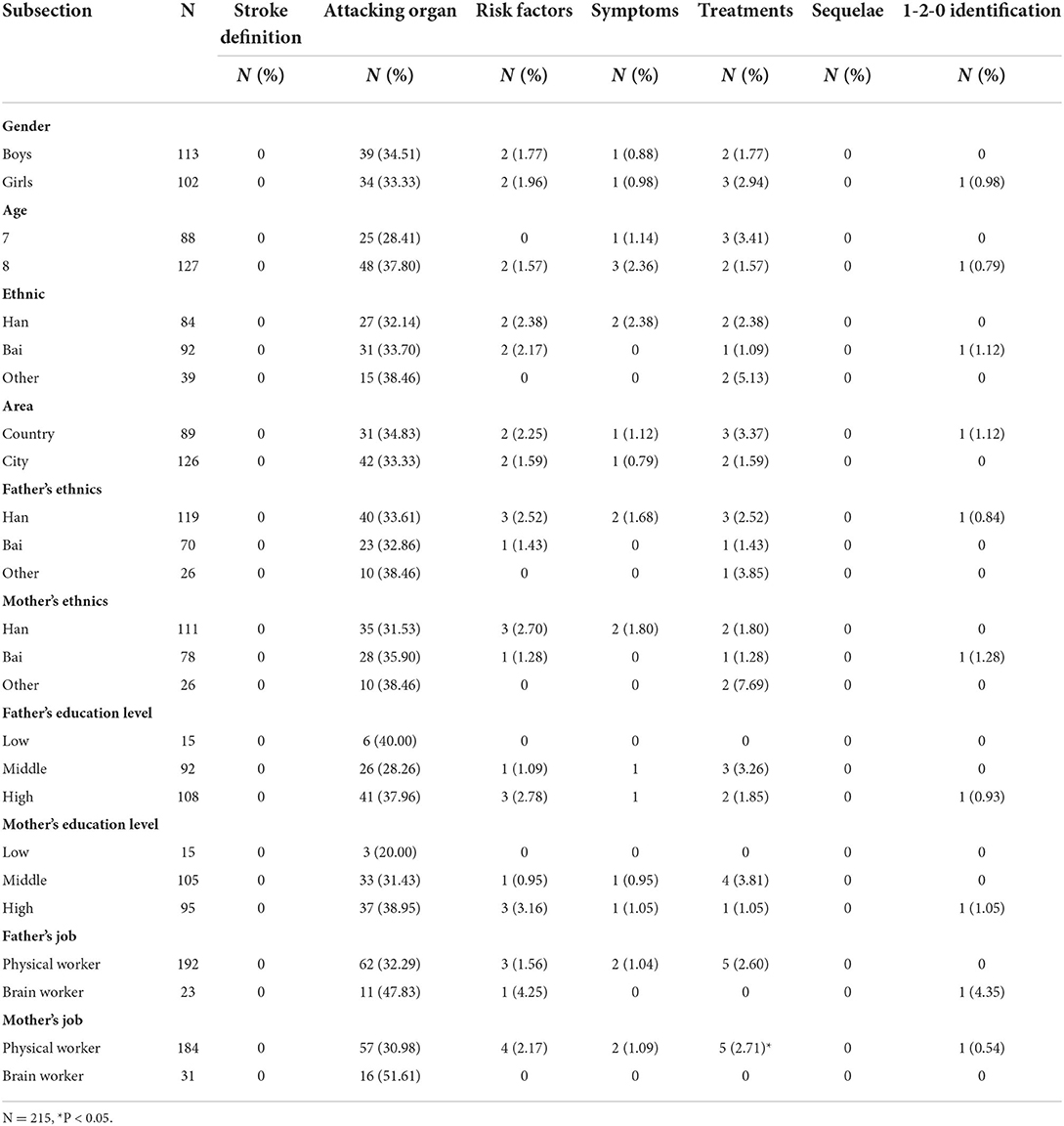
Table 1. The correct rate of stroke knowledge of primary school students in pre-intervention in Dali, Yunnan, China.
Assessment of the stroke knowledge levels in pre-intervention, post-intervention, and follow-up in 3-month surveys
Students took an average of 20 min to finish the questions at the beginning of the survey. Then, the time of answering the same questions took an average of 10 min in the post-intervention survey. The time of answering the questionnaire in the post-intervention survey was way shorter than that in pre-intervention. The speed of the response to the stroke questions post-intervention was quicker than that of pre-intervention.
The Chi-square test found a significant difference in the students' levels of stroke-related knowledge in pre-intervention, post-intervention, and follow-up surveys (P < 0.01).
As shown in Figure 2, after the health education, all the indicators of stroke knowledge were improved. The correct rates of the questionnaires in two post-intervention surveys were higher than that in pre-intervention, especially in the immediate post-intervention survey. However, the correct rate in the follow-up survey was lower than that in the immediate post-intervention one. The correct rate of stroke knowledge was about 4.83–92.41% (the rate is of different questions) 3 months after the intervention. The indicators that achieved better intervention effect were stroke definition, stroke organ, and the meaning of 1-2-0.
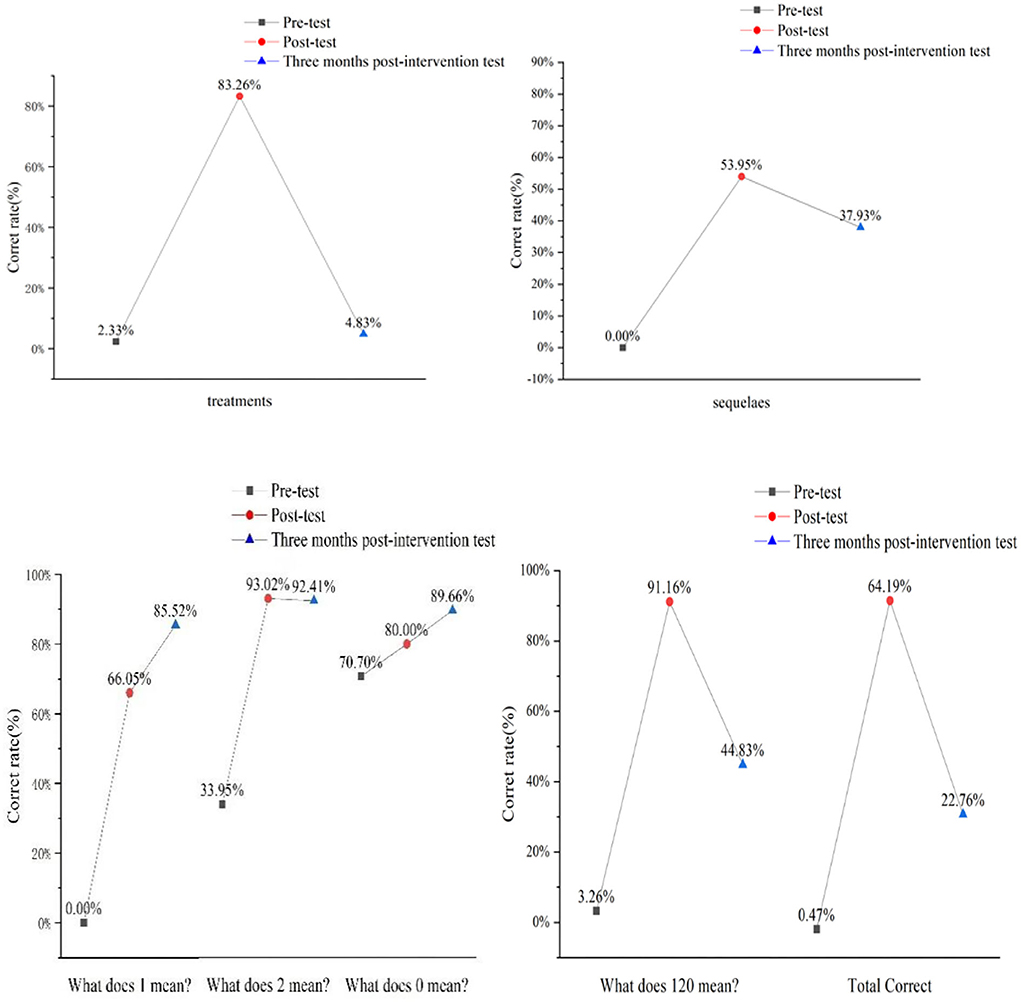
Figure 2. Assessment of the stroke knowledge in pre-intervention, post-intervention, and follow-up surveys.
Health education effect
As shown in Table 2, the ANOVA test found a significant difference in all indicators to measure stoke knowledge of in three surveys. The mean score of the overall questionnaire in pre-intervention was 4.25 ± 0.19., which increased to 15.85 ± 0.27 in the post-intervention. Then, it dropped to 14.02 ± 0.28 in the 3-month follow-up test. The mean score in the 3-month follow-up test was 11.55% lower than that in the post-intervention score. Despite that, the students' knowledge of stroke was improved after our intervention (F = 681.21, P < 0.01), especially in terms of stroke risk factors, symptoms, sequelae, and 1-2-0 identification. In the follow-up survey, the mean scores were also low in terms of stroke attacking organs, its treatments, and “1-2-0” identification (Table 2).
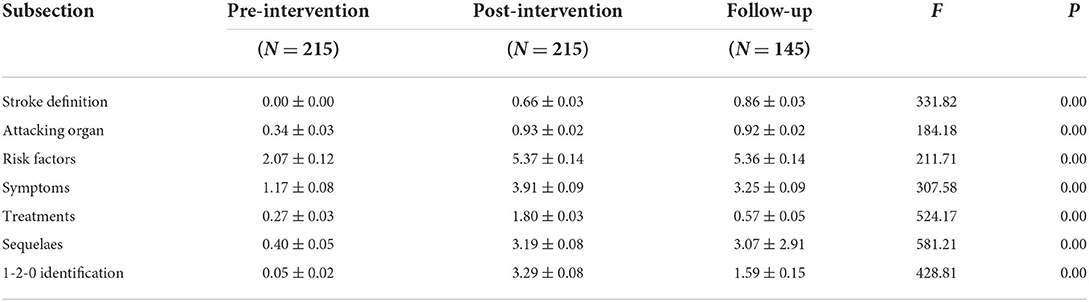
Table 2. The pre-intervention, post-intervention, and follow-up evaluation of stroke knowledge score of primary school students for stroke in Dali, Yunnan, China (means ± SD).
Source of health information
The top three sources of health knowledge were television (57.22%), doctors (55.83%), and teachers or school bulletin boards (55.56%).
Discussion
This study was the first to conduct a localized health educational intervention for primary children in Dali City of Yunnan, China. It has generated some useful information to inform health education on stroke for children and provide insights into preventing and controlling children's stroke in Yunnan ethnic prefectures.
It is evident from our study results that students' knowledge has been greatly improved in terms of stroke and its identification. For example, the correct rates of stroke definition, sequelae, and “1-2-0” identification were increased from 0 to 66.05%, to 53.95 and 64.19%, respectively, after the intervention. In addition, the correct rate of stroke definition kept increasing to 85.52% in 3 months after the intervention. However, the improvement was not observed 3 months after the intervention. The correct rates of sequelae and “1-2-0” identification were decreased to 37.93 and 22.76%, respectively, in 3 months after the intervention. The mean score in the follow-up survey was 11.55% lower than that in the post-intervention one. This decrease could be explained by Ebbinghaus' memory curve. This indicated that the health education program on stoke had attenuation despite the effects achieved among children. The correct rate of stroke knowledge was about 4.83–92.41% in 3 months after the intervention, which was lower than that in the study of Shigehatake (56%) (16) and Li X in Shanghai (84.4%) (17). Therefore, we should repeat pertinent health education programs among students.
The materials used in this health education program was presented in cartoons and hip-hop song. The study found that the manner of delivering stroke health education to children was essential to ensure the effectiveness of health education. Age-targeted education can significantly raise the awareness of stroke in children. In the following study, we will pay attention to making the health education materials match the cognitive characteristics of children in the context of local culture (18, 19).
Meanwhile, we should also note that the top three sources of health knowledge were television (57.22%), doctors (55.83%), and teachers or school bulletin boards (55.56%). This indicated that the principal role of doctors, teachers, or school bulletin boards cannot be ignored in children's health education. School health education has traditionally been an effective public health strategy to help children develop a proper health concept. A study also confirmed that school health education had always been a good option for students to receive health education (20, 21). Because chronic diseases have a long progressing trajectory, children should be the priority group for future intervention in chronic disease prevention. We should carry out child-targeted health education on disease control and prevention in schools, and facilitate children to develop a healthy lifestyle, which would further eliminate their risk behaviors as early as possible and reduce the incidence of chronic diseases in young adults.
This study found that it was important to develop child-friendly health education materials in the future. Thus, how to develop a series of educational electronic animations and pamphlets for children will be the focus of future research.
Limitations
This study has a few limitations. Our study did not have a control group to measure the actual intervention effects, so the evaluation results had certain limitations. We will further expand the study population and scope in the future study and to provide generate robust evidence for the importance of stroke health education in children.
Conclusion
In conclusion, this study is the first one that utilized the successive follow-up data of 7–8 school-aged children of Bai ethnicity in Dali City of Yunnan, China. Especially, this study compared the effect of health education on stroke before and after intervention, even 3 months after intervention. The study revealed our intervention had significantly improved the knowledge of stroke among Bai ethnicity of 7–8 years old children of Yunnan, China.
In view that a number of benefits of conducting health education among children, such as effectively improving the health awareness of stroke, reducing high-risk behaviors, and enhancing the healthy lifestyle of the family, we should develop a health education model that could fit in with the psychology development of children and local culture to raise children's awareness on stroke prevention and control.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The survey was approved by the Medical Research Ethics Committee of Yunnan Preventive Medical Institute. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
YJY: conducted data collection, intervention, statistical analysis and manuscript design, writing, and editing. JD: conducted field survey, collected data, provided suggestions, and manuscript preparation. JQM: field survey, advised, conceived, and designed the work, and edited the final version of the manuscript. ZZS, SZ, and LTC: coordinated survey fields and advised. YL: analyzed data and drew figures. XW and HYQ: conducted field survey, collected data, ill-disposed data, and analyzed data. JJC: provided suggestions, assisted in an English manuscript, and edited the manuscript. FL: analyzed data and provided suggestions. YPY: coordinated survey fields and conducted this study. YJY, JD, and JQM have full access to all the data in this study and takes primary responsibility for the final content. All authors have read and approved the final version of the manuscript.
Funding
This study was supported by the Academic Leader of Medical Science in Yunnan (Grant No. D-2018007), the 16th batch of young and middle-aged academic and technical leaders in Kunming (Grant No. KMRCD-2018011), Xishan Prefecture Science and Technology Bureau Project (Grant No. 34 Xikezi), and the National Natural Science Foundation of China (71764014).
Acknowledgments
The authors are grateful to the participants for their involvement in the survey. The authors also thank the team at the Department of School Health and Chronic Disease Control and Prevention, Yunnan Center for Disease Control and Prevention; Kunming University of Science and Technology; Kunming Children's Hospital; and the technical support of all team members in the survey. The assistance from the Dali Centers for Disease Control and Prevention is highly appreciated.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization (WHO). Cardiovascular Disease Overview. Available online at: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (accessed on December 12, 2021).
2. Chinese Cardiovascular Health and Disease Report Writing Group. China report 2020 profile of cardiovascular health and disease. Chin J Cycle. (2021) 4:521–45. doi: 10.3969/j.issn.1672-5301.2021.07.002
3. Center for Chronic Non-communicable Disease Control and Prevention Chinese Center for Disease Control and Prevention National National Health Statistical Information Center of Health and Family Planning Commission. China Death Surveillance Data Collection 2019. Beijing: China Science and Technology Press (2020).
4. Shen J, Cai L, Wang X, Liu Y, He L. Zuo J. Stroke prevalence and its impact on househould economic condition among rural Bai ethnic minority in Yunnan province. Chin Public Health. (2021) 37:710–2. doi: 10.11847/zgggws1133536
5. Yang Y, Min J, Chang L, Chai J, Song Z, Zha S, et al. Prevalence trends of hypertension among 9-17 aged children and adolescents in Yunnan, 2017-2019: a serial cross-sectional surveillance survey. BMC Public Health. (2021) 21: 338. doi: 10.1186/s12889-021-10258-1
6. Abgottspon S, Thaqi Q, Steiner L, Slavova N, Grunt S, Steinlin M, Everts R. Impact of age at pediatric stroke on long-term cognitive outcome. Neurology. (2021) 98:e721–9. doi: 10.1212/WNL.0000000000013207
7. Hongyang X, Xiaoshan D, Xitong Y, Rong M, Guangming W. Logistic regression analysis of risk factors for stroke patients in Dali residents. J Dali Univ. (2018) 3:63–6. doi: 10.3969/j.issn.2096-2266.2018.08.014
8. Jishuai Z. A Study on the Correlation Between Meteorological Elements in Dali City and the Occurrence of Stroke Events in Residents (Dali, China: Dali University) (2021).
9. Marto JP, Borbinha C, Filipe R, Calado S, Viana-Baptista M. Impact of Stroke Education on Middle School Students and Their Parents: A Cluster Randomized Trial. Int J Stroke. (2017) 12:401–11. doi: 10.1177/1747493016677980
10. Wiilliams O, Leighton-Herrmann Quinn E, Teresi J, et al. Improving community stroke preparedness in the HHS (Hip-Hop Stroke) randomized clinical trial. Stroke. (2018) 49:972–9. doi: 10.1161/STROKEAHA.117.019861
11. Ishigami A, Yokota C, Nishimura K, Ohyama S, Tomari S, Hino T, et al. Delivering knowledge of stroke to parents through their children using a manga for stroke education in elementary school. J Stroke Cerebrovasc Dis. (2017) 26:431–7. doi: 10.1016/j.jstrokecerebrovasdis.2016.10.005
12. Zhao J, Cai X, Li Y, et al. A Preliminary Study on the Practice of Health Science Popularization Education in Primary and Secondary Schools Conducted by Medical Students. J. Shaoyang Univ. (Nat. Sci. Ed.). (2020) 76:79–83.
13. Ottawa C, Sposato LA, Nabbouh F. et al. Stroke outcomes research canada (sorcan -wwwsorcanca) stroke preparedness in children: translating knowledge into behavioral intent: a systematic review and meta-analysis. Int J Stroke. (2015) 10:1008–13. doi: 10.1111/ijs.12628
14. Kabbani MR, Smith AL, Borgert AJ, et al. Abstract WP225: What do kids know? an assessment of stroke awareness in scholl-aged children. Stroke. (2017) 48:AWP225. doi: 10.1161/str.48.suppl_1.wp225
15. Kleindorfer DO, Miller R, Moomaw CJ. et al. Designing a message for public education regarding stroke: does fast capture enough stroke? Stroke. (2007) 38:2864–8. doi: 10.1161/STROKEAHA.107.484329
16. Jing Z, Xutong L, Xiaochuan L, Xu Y, Xu J, Xu A, et al. Changing the strategy and culture of stroke awareness education in China: implementing Stroke 1-2-0. Stroke Vasc Neurol. (2020) 5:374–80. doi: 10.1136/svn-2019-000324
17. Li X, Liu Y, Vrudhula A, Liu R, Zhao J. Middle school students effectively improve stroke knowledge and pass them to family members in China using stroke 1-2-0. Front Neurol. (2020) 11:203. doi: 10.3389/fneur.2020.00203
18. Kovách I, Megyesi BG, Barthes A, Oral HV, Smederevac-Lalic M. Knowledge use in education for environmental citizenship—results of four case studies in Europe (France, Hungary, Serbia, Turkey). Sustainability. (2021) 13:11118. doi: 10.3390/su131911118
19. Williams O, DeSorbo A, Noble J, et al. Child-mediated stroke communication: findings from hip hop stroke. Stroke. (2012) 43:163–9. doi: 10.1161/STROKEAHA.111.621029
20. Zhang X, Long X, Zhang H, et al. Survey on access to health knowledge among pupils based on factor analysis and association rules. Chin Health Educ. (2021) 37:405–8. doi: 10.16168/j.cnki.issn.1002-9982.2021.05.005
Keywords: stroke, health education, effect, children, evaluation, ethnic
Citation: Yang Y, Dai J, Min J, Song Z, Zha S, Chang L, Chai J, Yang Y, Liu Y, Zhang X, Wu X, Gong Y, Wang X, Li F and Qin H (2022) Evaluation of stroke health education for primary school students in Dali, China. Front. Public Health 10:861792. doi: 10.3389/fpubh.2022.861792
Received: 25 January 2022; Accepted: 30 June 2022;
Published: 02 August 2022.
Edited by:
Amelia Kekeletso Ranotsi, Maluti Adventist College, LesothoReviewed by:
Neeti Rustagi, All India Institute of Medical Sciences Jodhpur, IndiaLiguang Tian, Chinese Center for Disease Control and Prevention, China
Copyright © 2022 Yang, Dai, Min, Song, Zha, Chang, Chai, Yang, Liu, Zhang, Wu, Gong, Wang, Li and Qin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunjuan Yang, eW5jZGN5eWpAMTI2LmNvbQ==; Jing Dai, MTU0MTgwODBAcXEuY29t; Jieqing Min, MjQxNDc4NjNAcXEuY29t
†These authors have contributed equally to this work
 Yunjuan Yang
Yunjuan Yang Jing Dai4*†
Jing Dai4*† Yuwen Gong
Yuwen Gong Xin Wang
Xin Wang