
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health, 02 June 2022
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.859469
This article is part of the Research TopicReviews in Infectious Diseases – Surveillance, Prevention and TreatmentView all 5 articles
 Tesfanesh Lemma1*
Tesfanesh Lemma1* Mulualem Silesh1
Mulualem Silesh1 Birhan Tsegaw Taye1
Birhan Tsegaw Taye1 Kelem Desta1
Kelem Desta1 Tebabere Moltot Kitaw1
Tebabere Moltot Kitaw1 Tiwabwork Tekalign2
Tiwabwork Tekalign2Background: HIV disclosure among children refers to when the caregiver is having disclosed to the child that he or she has HIV specifically. Disclosure significantly improved adherence to treatment and quality of life among children living with HIV/AIDS. Even though, the benefits of disclosure are considerable, informing a child of his or her own HIV status is often delayed. There is a dearth of studies on HIV serostatus disclosure among children in Ethiopia. Therefore, this study aimed to assess the pooled prevalence of HIV serostatus disclosure and associated factors among children living with HIV in Ethiopia.
Methods and Materials: Using a combination of search terms and Boolean operators, studies were retrieved from Pub Med/MEDLINE, EMBASE, CINAHL, Science Direct, Scopus, Web of Science, Cochran library, and Google Scholar. Five authors independently assessed the quality of each study using the modified Newcastle Ottawa Scale (NOS) for cross-sectional studies. STATA Version 11 software was used for statistical analyses. The random-effects (Der Simonian and Laird) method was used for the meta-analysis. The heterogeneity test was carried out with the help of I-squared (I2) statistics. A leave-one-out sensitivity analysis was carried out.
Results: A total of 12 articles with 3,410 participants were included in this systematic review and meta-analysis. The pooled prevalence of HIV serostatus disclosure among children was 36.87% (95% CI: 29.30, 44.44; I2 = 95.8%). Children aged older than 10 years (p = 0.003) and caregivers with primary and above education (p < 0.001) were factors significantly associated with HIV serostatus disclosure among children.
Conclusions: The finding of this study showed that HIV serostatus disclosure among children is relatively low. Therefore, developing clear guideline on HIV serostatus disclosure among children, strengthening public health education or community awareness creation about HIV/AIDS to promote the benefits of disclosure and extensively provision of counseling by health care providers are essential to enhance HIV serostatus disclosure among children.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021239035.
Human immunodeficiency virus infection/Acquired immune deficiency Syndrome (HIV/AIDS) is still a major public health problem around the world (1). Globally, in 2020, there were 37.7 million (30.2−45.1 million) people living with HIV (PLWH) and 1.7 million children (0–14 years) have been infected with HIV and 99,000 children have died of HIV (2, 3); about 20.7 million PLWH live in Eastern and Southern Africa (4). Besides, Ethiopia has achieved great progress in combating the HIV/AIDS epidemic over the last decade, HIV was still one of public health problem in the country; the prevalence remains extremely high in urban areas, with estimates indicating a 3% prevalence rate compared to <1% nationally (5). In Ethiopia nearly 620,000 adults and children were living with HIV; of which 44,000 were children <15 years old in 2020. In addition, 13,000 of adults and children died due to AIDS (6).
HIV disclosure among HIV-infected children refers to when the caregiver has disclosed to the child that he or she has HIV infected (7, 8). Disclosing one's HIV-positive serostatus can help both HIV-positive people and public health preventive initiatives (9). In HIV-positive children, disclosure enhanced clinical outcomes such as viral suppression, drug adherence, retention in care, and HIV knowledge (10–12). However, one of the most difficult decisions for parents is whether or not to tell their children about their HIV status (9).
According to World Health Organization (WHO) guidelines on HIV counseling for children under the age of 12, children of school age should be informed of their HIV-positive status (13). HIV status disclosure significantly improved adherence to treatment and quality of life among children living with HIV/AIDS (14). Furthermore, disclosing HIV-positive serostatus has advantages for children, parents, and family dynamics (15). However, disclosing a child's HIV status has its own set of difficulties (16). Disclosure requires providing persons with access to appropriate physical and psychological support, which is a critical component of secondary prevention (17). Many people have their own particular disclosure strategies and objectives, which are carefully considered to achieve beneficial results (18).
Treatment must be scaled up even more, especially for HIV-infected children. Globally, only 54% (37%−69%) of children (0–14 years old) were receiving ART at the end of 2020 (3). Also, only 38% of them were on antiretroviral therapy (ART) in Ethiopia (19). HIV disclosure can improve social support, antiretroviral adherence, and healthcare attendance for people living with HIV (20, 21). Despite this, children's HIV disclosure remained low. According to one systematic review, in low- and middle-income countries the overall rate of HIV-positive status disclosure to HIV-infected children was low, which ranges from 1.7 to 41% (7).
Furthermore, disclosure of HIV status among children living with HIV has both beneficial and challenging aspects (7). Developing countries have a lower rate of HIV-positive status disclosure than developed countries (22). Even though, the benefits of disclosure are considerable, informing a child of his or her own HIV status is often delayed (23). This systematic review and meta-analysis sought to fill the gaps in the Ethiopian literature by estimating the pooled effect of disclosure status among children living with HIV in Ethiopia. We believe that our findings will be relevant to those involved in designing interventions to improve HIV serostatus disclosure among HIV-infected children.
• To assess the HIV serostatus disclosure and its predictors among children living with HIV in Ethiopia.
• To determine the pooled prevalence of HIV serostatus disclosure among children in Ethiopia.
• To identify the predictors of HIV serostatus disclosure among children in Ethiopia.
The protocol was registered with in PROSPERO (https://www.crd.york.ac.uk/), registration number (ID: CRD42021239035). This systematic review and meta-analysis were conducted under the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (24, 25). All published articles were searched from major international databases like PubMed /MEDLINE, EMBASE, CINAHL, Science Direct, Scopus, Web of Science, Cochran library, and Google Scholar. A second search was done by using all identified keywords and index terms across all included databases. Also, the reference list of all identified reports and articles was searched for additional studies. The search was performed using key terms such as HIV Disclosure, Disclosure of HIV, HIV positive status disclosure, HIV status disclosure, Disclosure of HIV status, HIV related disclosure, Disclosure of HIV serostatus, Children, Young children's, pediatrics, childhood, children's, pediatrics, pediatric and Ethiopia. The searching periods were from October 1 to 31, 2021.
Study participants included HIV positive children who were booked in ART clinic in Ethiopia. This study included all published and unpublished observational (cross-sectional and case–control) studies on the HIV serostatus disclosure among children in Ethiopia. This review included studies done until November 1, 2021, and was written in the English language.
The data were extracted by three independent authors (TL, MS, and BT) using a data extraction format prepared in a Microsoft Excel 2010 spread sheet. The extracted data were: the first author's name, publication year, study area, region, study design, sample size, sampling method, HIV serostatus disclosure, and associated factors with their odds ratio. The quality of each study was assessed using the modified Newcastle-Ottawa Scale (NOS) for cross-sectional studies (26). The tool's key components were methodological quality, comparability, outcomes, and statistical analysis of each original study, which were graded from five to two and three stars, respectively. The NOS included three categorical criteria with a maximum score of 10 points. Studies with a medium score (50% of quality evaluation criteria) and above were included in the analysis (27). The quality of each study was evaluated independently by five authors (TL, MS, TT, KD, and TM) and any disagreements were resolved by discussion and consensus.
To assess the existence of publication bias, funnel plots were used and Egger's test was computed. A p-value < 0.05 was used to declare the statistical significance of publication bias. I2 test statistics were used to check the heterogeneity of studies. I2 test statistics of < 50, 50–75, and > 75% were declared as low, moderate, and high heterogeneity respectively (28).
HIV serostatus disclosure.
Determinants of HIV serostatus disclosure. The only factor identified as a significant factor in the two and above studies was included in this review and meta-analysis.
STATA version11 software was used to conduct the analysis. The heterogeneity test was conducted by using I-squared (I2) statistics. The pooled prevalence of HIV serostatus disclosure was carried out using a random-effects (Der Simonian and Laird) method. To minimize the potential random variations between studies; the sources of heterogeneity were analyzed using subgroup analysis, and meta-regression. A sensitivity analysis was also conducted.
Initially, a total of 4,529 studies were retrieved from the databases and manual searching. From this, 1,848 duplicates were found and removed. Their title screened the remaining 1,146 articles, and abstract 636 irrelevant studies were removed. Sixty-six full-text articles were assessed for eligibility, and 52 of them were excluded due to not reporting the outcome of interest, and two articles with poor methodological quality. Finally, a total of 12 studies fulfilled the inclusion criteria and enrolled in the study (Figure 1).
A total of 12 (29–40) articles with 3,410 participants were included in this systematic review and meta-analysis. All the included studies were cross-sectional studies and the sample size ranged from 172 (33) to 428 (39). Most studies were conducted in the Amhara region. Among the included studies, HIV serostatus disclosure among children ranged from 16.3 (33) to 60.6 (35).
By including the 12 published research articles we had estimated the pooled prevalence of HIV serostatus disclosure among children in Ethiopia. Accordingly, the overall estimated pooled prevalence of HIV serostatus disclosure among children with a random-effects model was 36.87% (95% CI: 29.3, 44.4) with a heterogeneity index (I2) of 95.8% (p < 0.001; Figure 2).
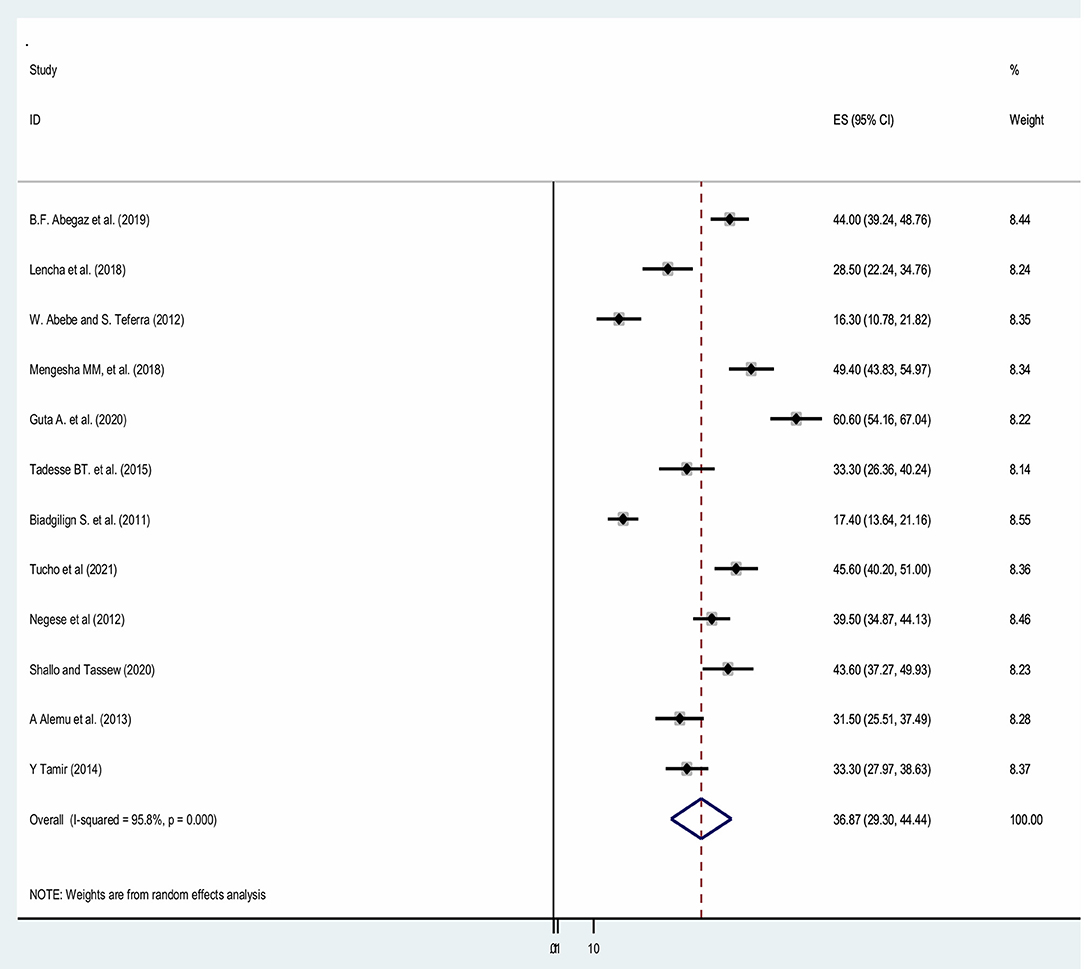
Figure 2. Forest plot showing the pooled prevalence of HIV serostatus disclosure among children in Ethiopia.
Subgroup analyses revealed a marked variation across regions. Based on the subgroup analysis result, the highest (54.92%; 95% CI: 43.95, 65.90), I2 = 74.4%) seen in Dire Dawa region and the lowest (16.83%; 95% CI: 12.92, 20.75), I2 = 0%) seen in Addis Ababa (Figure 3).
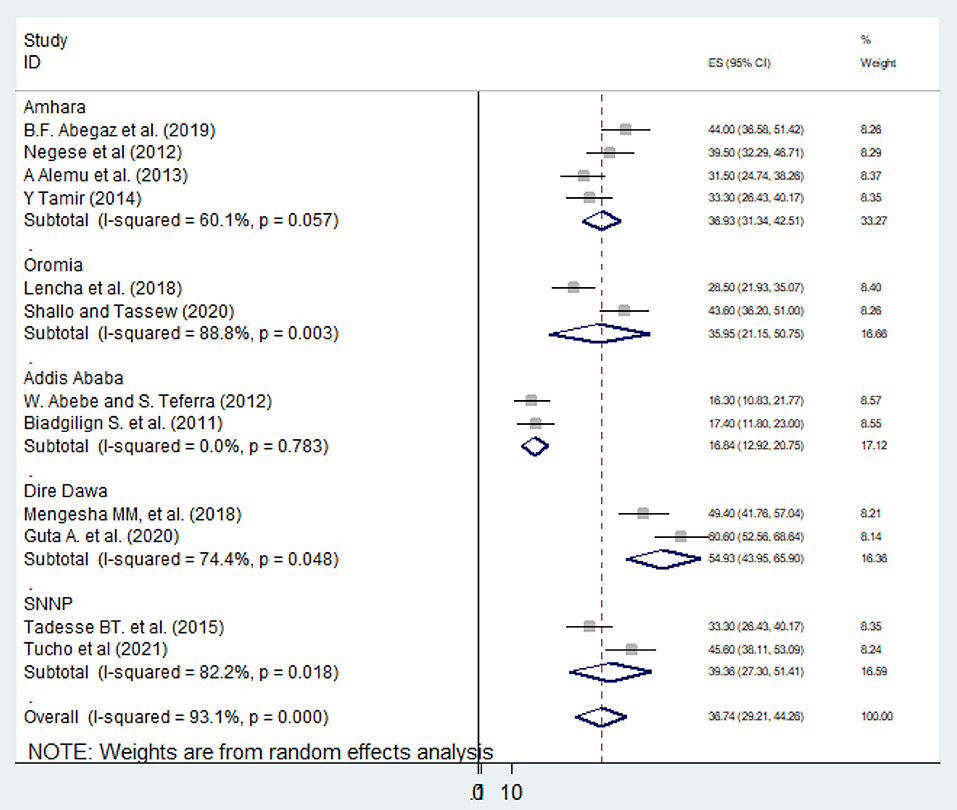
Figure 3. Subgroup analysis of the prevalence of HIV serostatus disclosure among children in Ethiopia.
Meta-regression was conducted to identify the source of heterogeneity using sample size and publication year as a covariates. It was indicated that there is no effect of sample size on heterogeneity between studies. But, the year of publication showed that there is heterogeneity between the studies (Table 1). The presence of publication bias was checked using the Egger's test, and a graphical Funnel plot, the result of egger's test was found significant (p < 0.001), as a result of estimating the number of missing studies that might exist in a meta-analysis we conducted Duval and Tweedie's trim and fill analysis, but is not significant. Also, visual inspection of the funnel plot indicated asymmetrical distribution showing publication bias (Figure 4).
All studies have been included in the review, then a sensitivity analysis performed by study quality by leave-one-out studies step by step to evaluate the effect of a single study on the overall effect estimate. The result indicated removing a single study did not have a significant influence on pooled prevalence (Figure 5).
Six variables were extracted to identify factors associated with HIV serostatus disclosure among children. Of these, age of children and educational status of caregivers were found to be significantly associated with HIV serostatus disclosure among children (Table 2).
Children whose aged older than 10 years were 11 times more likely to know their HIV positive status compared to their counterparts (AOR = 11.15, 95% CI: 4.82–11.98), p = 0.003, I2: 66.2%, the heterogeneity test (p < 0.001). Those caregivers of HIV-positive children with primary and above education were three times more likely to have disclosed HIV status to their children compared to those with no formal education (AOR = 3.21, 95% CI: 1.01–10.18), p = <0.001, I2: 93.8%, the heterogeneity test (p < 0.001).
In this systematic review and meta-analysis, the overall pooled prevalence of HIV serostatus disclosure among children was 36.87% (95% CI: 29.30, 44.44). This result is relatively low, because according to WHO guidelines children of school age should be informed of their HIV-positive status (13). According to the results of the subgroup analysis, the highest prevalence of HIV serostatus disclosure among children was found in the Dire Dawa region (54.92%), while the lowest prevalence of disclosure rate was found in Addis Ababa (16.83%). The possible variation might be due to the difference in study period; because community awareness about HIV and related information improve over time which might increase the disclosure by the caregivers. Also, socio-cultural difference might have role for the difference between these studies.
In the current study, child age was significantly associated with HIV serostatus disclosure. Children whose aged older than 10 years were 11 times more likely to know their HIV positive status compared to their counterparts (AOR = 11.15, 95% CI: 4.82–11.98), p = 0.003, I2: 66.2%, the heterogeneity test (p < 0.001). This is consistent with a review conducted in Sub-Saharan Africa (7, 41). This might be because the caregivers may have believed that the older children were mature enough to understand the illness and recognize the complex causes and consequences of the illness. Also, children in these age groups were more interested in knowing why they were taking medication and what their illness was like.
Furthermore, parental/care giver's educational status also significantly associated with HIV serostatus disclosure among children. Those caregivers of HIV-positive children with primary and above education were three times more likely disclosed the HIV status to their children compared to those care givers with no formal education (AOR = 3.21, 95% CI: 1.01, 10.18), p = <0.001, I2: 93.8%, the heterogeneity test (p < 0.001). This is consistent with the review conducted in resource-limited settings (42). This could be because caregivers with a higher educational level have been exposed to more information about disclosure which allowing them to understand the importance of disclosure and well prepared to handle the disclosure process.
This review showed that HIV serostatus disclosure among children in Ethiopia was not sufficient enough which is difficult to achieve the global target of HIV free generation and sustainable development goal 3 which aims to ensure healthy lives and promote wellbeing for all at all ages, including people living with HIV. Therefore, this review informed the following recommendations; first, healthcare providers should give more attention on the purpose of disclosure to infected children. Furthermore, public health education/ community education should be strengthen to promote HIV/AIDS as a shared burden which eventually enhance community/familial acceptance of living with HIV infected children. Finally, further studies are needed to identify other determinants of HIV serostatus disclosure practices among children in resource-limited countries.
The strength of this review were the study was conducted using a very thorough systematic search, with an international standardized protocol for the search strategy and internationally approved tools for a critical appraisal system for each study's quality assessment. However, only three regions and two administrative cities out of nine regional states were included in this analysis that might reduce its representativeness for the country. Also, lack of studies.
According to the findings of this study, only one-third of caregivers disclosed their child's HIV serostatus. Age of infected children and the educational status of care givers were found to be significantly associated with HIV serostatus disclosure among children. As a result, authors suggest that designing strategies by developing clear guideline on HIV serostatus disclosure among children, strengthening parental/caregiver health education/training or community awareness creation about HIV disclosure and HIV/AIDS related information to promote the benefits of disclosure and extensively provision of counseling by health care providers are essential to enhance HIV serostatus disclosure among children.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.859469/full#supplementary-material
1. Osingada CP, Okuga M, Nabirye RC, Sewankambo NK, Nakanjako D. Disclosure of parental HIV status to children : experiences of adults receiving antiretroviral treatment at an Urban Clinic in Kampala, Uganda. AIDS Res Treat. (2017) 2017:3458684. doi: 10.1155/2017/3458684
4. UNAIDS. Global HIV & AIDS statistics - 2020 fact sheet. Ending the Aids Epidermics. Luxembourg (2020), p. 8.
6. UNAIDS. HIV and AIDS Estimates Adults and children living with Country factsheets ETHIOPIA | 2020 HIV. New York (2020), p. 1–6.
7. Britto C, Mehta K, Thomas R, Shet A. Prevalence and correlates of HIV disclosure among children and adolescents in low- and middle-income countries: a systematic review. J Dev Behav Pediatr. (2016) 37:496–505. doi: 10.1097/DBP.0000000000000303
8. Wiener L. Disclosure of an HIV diagnosis to children: history, current research, and future directions. J Dev Behav Pediatr. (2008) 28:155–66. doi: 10.1097/01.DBP.0000267570.87564.cd
9. Conserve DF, Hill C, Groves AK, Maman S, Hill C. Effectiveness of interventions promoting HIV serostatus disclosure to sexual partners: a systematic review. AIDS Behav. (2016) 19:1763–72.
10. Adefalu MO, Florence M, Issa BA, Adefalu AA. Does disclosure of HIV/AIDS status to children with HIV/AIDS affect their does disclosure of HIV/AIDS status to children with HIV/AIDS affect their mental health? J Psychiatry. (2016) 20:1. doi: 10.4172/2378-5756.1000399
11. Ozoya OO. Perspectives and practice of hiv disclosure to children and adolescents by health-care providers and caregivers in sub-Saharan Africa : a systematic review. Front Public Health. (2016) 4:166. doi: 10.3389/fpubh.2016.00166
12. Vreeman RC, Scanlon ML, Marete I, Mwangi A, Inui TS. Characteristics of HIV-infected adolescents enrolled in a disclosure intervention trial in western Kenya. AIDS Care. (2015) 27(sup1):6–17. doi: 10.1080/09540121.2015.1026307
13. WHO. Guideline on HIV Disclosure Counselling For Children Up to 12 years of Age. Geneva: WHO (2011).
14. Bulali RE, Kibusi SM, Mpondo BCT. Factors associated with HIV status disclosure and its effect on treatment adherence and quality of life among children 6 – 17 Years on antiretroviral therapy in Southern Highlands Zone, Tanzania : unmatched Case Control Study. Int J Pediatr. (2018) 2018:8058291. doi: 10.1155/2018/8058291
15. Tenzek KE, Herrman AR, May AR, Feiner B, Allen M. Examining the impact of parental disclosure of HIV on children: a meta-analysis. West J Commun. (2013) 77:323–39. doi: 10.1080/10570314.2012.719092
16. Beck-sague CM. Disclosure of their HIV status to infected children : a review of the literature. J Trop Pediatr. (2013) 59:84–9. doi: 10.1093/tropej/fms052
17. Conserve DF, Groves AK, Maman S. Effectiveness of interventions promoting HIV serostatus disclosure to sexual partners: a systematic review. AIDS Behav. (2015) 19:1763–72. doi: 10.1007/s10461-015-1006-1
18. Take K, Messages H. Disclosure of HIV-positive status : towards the development of guidelines, strategies and interventions. The issue and why it ' s important. Toronto (2014).
19. USAIDS. PEPFAR 2021 Country and Regional Operational Plan (COP/RO) Guidance for all PEPFAR Countries. Washington, DC (2021).
20. Evangeli M, Wroe AL. HIV disclosure anxiety: a systematic review and theoretical synthesis. AIDS Behav. (2017) 21:1–11. doi: 10.1007/s10461-016-1453-3
21. Nichols J, Steinmetz A, Paintsil E. Impact of HIV-status disclosure on adherence to antiretroviral therapy among HIV-infected children in resource-limited settings : a systematic review. AIDS Behav. (2017) 21:59–69. doi: 10.1007/s10461-016-1481-z
22. Berhe TM, Lemma L, Alemayehu A, Ajema D, Glagn M, Dessu S. HIV-positive status disclosure and associated factors among HIV-positive adult patients attending art clinics at public health facilities of Butajira Town, Southern Ethiopia. AIDS Res Treat. (2020) 2020:7165423. doi: 10.1155/2020/7165423
23. Madiba S, Diko C. The consequences of delaying telling children with perinatal hiv about their diagnosis as perceived by healthcare workers in the eastern cape; a qualitative study. Children. (2020) 7:289. doi: 10.3390/children7120289
24. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:332–6. doi: 10.1136/bmj.b2535
25. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. (2009) 62:1–34. doi: 10.1016/j.jclinepi.2009.06.006
26. Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Cross sectional study Newcastle - Ottawa Quality Assessment Scale. PLoS ONE. (2016) 11:1–2. doi: 10.1371/journal.pone.0147601
27. Kassa BG, Ayele AD, Belay HG, Tefera AG, Tiruneh GA, Ayenew NT, et al. Postpartum intrauterine contraceptive device use and its associated factors in Ethiopia: systematic review and meta-analysis. Reprod Health. (2021) 18:1–12. doi: 10.1186/s12978-021-01273-x
28. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
29. Abegaz BF, Walle TA, Tilahun AD, HIV. positive status disclosure and associated factor among HIV infected children in pediatric ART clinics in Gondar town public health facilities, North West Ethiopia, 2018. J Infect Public Health. (2019) 12:873–7. doi: 10.1016/j.jiph.2019.05.018
30. Lencha B, Ameya G, Minda Z, Lamessa F, Darega J. Human immunodeficiency virus infection disclosure status to infected school aged children and associated factors in bale zone, Southeast Ethiopia: cross sectional study 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Pediatr. (2018) 18:1–8. doi: 10.1186/s12887-018-1336-z
31. Alemu A, Berhanu B, Emishaw S. Challenges of caregivers to disclose their children's HIV positive status receiving highly active anti retroviral therapy at pediatric anti retroviral therapy clinics in Bahir Dar, North West Ethiopia. J AIDS Clin Res. (2013) 4:11. doi: 10.4172/2155-6113.1000253
32. Tamir Y. Disclosure status and associated factors open access among children living with HIV in East Gojjam, Northwest of Ethiopia 2014. Qual Prim. Care. (2015) 23:223–30.
33. Abebe W, Teferra S. Disclosure of diagnosis by parents and caregivers to children infected with HIV: prevalence associated factors and perceived barriers in Addis Ababa, Ethiopia. AIDS Care. (2012) 24:1097–102. doi: 10.1080/09540121.2012.656565
34. Mengesha MM, Dessie Y, Roba AA. Perinatally acquired HIV-positive status disclosure and associated factors in Dire Dawa and Harar, Eastern Ethiopia: a health facility-based cross-sectional study. BMJ Open. (2018) 8:e019554 doi: 10.1136/bmjopen-2017-019554
35. Guta A, Areri HA, Anteab K, Abera L, Umer A. HIV-positive status disclosure and associated factors among children in public health facilities in Dire Dawa, Eastern Ethiopia: a cross-sectional study. PLoS ONE. (2020) 15:1–12. doi: 10.1371/journal.pone.0239767
36. Tadesse BT, Foster BA, Berhan Y, Tang JW. Cross sectional characterization of factors associated with pediatric HIV status disclosure in southern Ethiopia. PLoS ONE. (2015) 10:1–9. doi: 10.1371/journal.pone.0132691
37. Biadgilign S, Deribew A, Amberbir A, Escudero HR, Deribe K. Factors associated with HIV/AIDS diagnostic disclosure to HIV infected children receiving HAART: a multi-center study in Addis Ababa, Ethiopia. PLoS ONE. (2011) 6:1–6. doi: 10.1371/journal.pone.0017572
38. Tucho WA, Tekelehaimanot AN, Habte MB. Disclosure status and associated factors among children on antiretroviral therapy in Ethiopia. Pediatr Health Med Ther. (2021) 12:299–306. doi: 10.2147/PHMT.S314259
39. Negese D, Addis K, Awoke A, Birhanu Z, Muluye D, Yifru S, et al. HIV-positive status disclosure and associated factors among children in North Gondar, Northwest Ethiopia. Isrn Aids. (2012) 2012:1–7. doi: 10.5402/2012/485720
40. Shallo SA, Tassew M. Hiv positive status disclosure and its associated factors among children on antiretroviral therapy in west shoa zone, western ethiopia, 2019: a mixed method cross-sectional study. J Multidiscip Healthc. (2020) 13:507–17. doi: 10.2147/JMDH.S258851
41. Doat A, Negarandeh R. Disclosure of HIV status to children in Sub-Saharan Africa : a systematic review. Medicina. (2019) 55:1–12. doi: 10.3390/medicina55080433
Keywords: children, disclosure, HIV, serostatus disclosure, Ethiopia
Citation: Lemma T, Silesh M, Taye BT, Desta K, Kitaw TM and Tekalign T (2022) HIV Serostatus Disclosure and Its Predictors Among Children Living With HIV in Ethiopia: A Systematic Review and Meta-Analysis. Front. Public Health 10:859469. doi: 10.3389/fpubh.2022.859469
Received: 21 January 2022; Accepted: 03 May 2022;
Published: 02 June 2022.
Edited by:
Claudio Fenizia, University of Milan, ItalyReviewed by:
Yoshan Moodley, Stellenbosch University, South AfricaCopyright © 2022 Lemma, Silesh, Taye, Desta, Kitaw and Tekalign. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tesfanesh Lemma, dGVzZml0aW1udEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.