- 1Department of Child Health Development, Capital Institute of Pediatrics, Beijing, China
- 2Community Health Association of China, Beijing, China
- 3School of Social Development and Public Policy, Beijing Normal University, Beijing, China
- 4Research Center for Health and Social Policy, Beijing Normal University, Zhuhai, China
Background: Studies have not provided clear enough evidence on the direct association between cigarette smoking and poverty. This study aims to assess the association of householder smoking with near-poverty households, and the potential mediating effect of NCDs.
Methods: A cross-sectional survey was conducted from November 2019 to October 2020 in relatively underdeveloped regions in China. In total, 2,409 households were investigated in areas under the jurisdiction of 24 primary health care (PHC) institutions of eight provinces. Pearson's χ2-test was performed, and multivariable logistic regression and extended probit regression models were fitted to examine the association between householder smoking and near-poverty households. Moreover, generalized structural equation modeling was used to explore the mediating effect of NCDs.
Results: After adjusting for all other potential confounding factors, compared with households headed by never-smokers, households headed by smokers exhibited significantly elevated risks of being near poverty, with an odds ratio of 2.01 (95% CI: 0.48–0.91). We also found that living in rural areas and having a low education level both had a negative effect on being near poverty. Additionally, NCDs had a significantly positive mediating effect, with a 31.57% effect of householder smoking on near-poverty status mediated by NCDs; the indirect effect was estimated to be 0.17 (95% CI: 0.04–0.31).
Conclusions: Householder smoking significantly elevated the risk of the household being near poverty, and suffering NCDs had a positive mediating effect.
Introduction
Cigarette smoking is a major public health problem and remains the leading preventable cause of death and disability in China and other countries, killing more than 8 million people a year around the world (1). In 2020, it was estimated that there were approximately 1.3 billion tobacco users worldwide, with the vast majority living in low- and middle-income countries or in more disadvantaged socioeconomic groups (1, 2). China is the world's largest producer and consumer of tobacco, accounting for more than 44% of the world's total cigarette consumption (3). It is estimated that one million people die of tobacco-related diseases in China every year, with the majority of those individuals in their productive years. Unfortunately, this number is estimated to exceed three million per year by the end of 2050 if the smoking epidemic is not controlled (4, 5).
Additionally, even though the global percentage of people living in extreme poverty declined from 36% in 1990 to 10% in 2015, more than 700 million people now live in extreme poverty (6). “End poverty in all its forms everywhere” is the first goal of United Nations Sustainable Development. Studies have found that noncommunicable diseases (NCDs), associated with mortality and prolonged disability, have negative impacts at the individual, community, and societal levels (7) and could expose individuals to poverty through lost productivity, unemployment and long-term medical expenses (8, 9). Meanwhile, studies have also found that cigarette smoking is one of the main risk factors driving the growing epidemic of NCDs, including cancers and cardiovascular and respiratory diseases (10, 11). However, early studies have not provided clear enough evidence on the direct association between cigarette smoking and poverty. Evidence is accordingly required to clarify the association of cigarette smoking with poverty and its underlying mechanisms, underpinning the rationale for integrating tobacco control policies with poverty alleviation strategies.
At the macro level, multiple studies have demonstrated that tobacco use imposes an economic burden through a reduction in productivity and an increase in the cost of medical treatment (12). For example, Pearce et al. (13) reported that in 2012, tobacco use contributed to an estimated USD 7.9 billion, USD 402 million, and USD 138 million in lost productivity in China, Brazil, and South Africa, respectively. Cigarette smoking accounted for approximately USD 289-332.5 billion in medical expenses over the period 1964–2014 in the United States (14), while in Indonesia, tobacco-related treatment costs were estimated at nearly USD 2.2 billion (15). The Directorate General for Health and Consumers study (16) reported that the estimated costs attributed to cigarette smoking in the European Union amounted to approximately USD 714.9 billion in 2009, and a global estimated economic burden of smoking was approximately USD 1.44 trillion in 2012 (17).
At the micro level, there have been few studies about cigarette smoking and poverty. Liu et al. (18) estimated cigarette smoking's impact on poverty through excessive medical spending and direct spending on cigarettes. Wei et al. (19) conducted a population-based study and demonstrated that smoking can significantly reduce the income of Chinese urban residents, resulting in immense negative impacts on society. In the traditional Chinese family structure, the householder is often male and males have much higher smoking rates than females (5). Moreover, householders often shoulder a heavy burden and play a central role in households' economic status. However, to our knowledge, no study has assessed the association between householder smoking and poverty and its underlying mechanisms. To fill this research gap, we conducted a cross-sectional study and assessed the association of householder smoking with near-poverty households and the mediating effect of NCDs in relatively underdeveloped regions in China.
Methods
Study Design and Participants
We conducted a cross-sectional questionnaire-based survey in relatively underdeveloped regions in China from November 2019 to October 2020, and the participants were enrolled using a stratified multistage sampling method. According to per capita GDP levels, we first chose 12 cities/counties that had relatively lower per capita GDP in eight province-level regions in China (North China: Fuping and Pingshan in Hebei Province; Central China: Nanyang in Henan Province, Macheng and Qichun in Hubei Province; Eastern China: Linqing and Wuli in Shandong Province; Southwest China: Luzhou in Sichuan Province, Kaili in Guizhou Province; Northwest China: Yulin in Shanxi Province; Northeast China: Harbin and Wuchang in Heilongjiang Province). Then, in each city/county, two primary health care (PHC) institutions were randomly selected as our investigation units, for a total of 24 PHC institutions.
Next, with the coordination of local health professionals in PHC institutions, approximately 100 households were selected in areas under the jurisdiction of each PHC institution. The participants were not sampled randomly but were directly selected based on the following: (1) living in local communities for at least 6 months; (2) willing to participate in this study; (3) the householder was aged over 40; (4) near-poverty households and nonpoor households were included; and (5) smokers and never-smokers were included.
Data Collection and Measures
The selected householders had a face-to-face interview with the local health professionals of the PHC institutions, and prior to the interview, investigators received professional training to ensure data collection quality. A validated interviewer-administered questionnaire was used to obtain information about the household's basic situation (household income, size of household and residence location), demographic characteristics of the householder (sex, age, education level, marital status, and income level), and the householder's smoking status, whether the householder suffered from NCDs or not and so on. All measures were self-reported in the study.
Poverty Status
In 2019, the Chinese government defined the poverty as yearly per capita income <3,747 Yuan (or US $1.49 per day). In our study, we further defined near-poverty as 200% of the poverty level definition (7,494 Yuan) and categorized household poverty status as near-poverty (yearly per capita income <7,494 Yuan) or nonpoor (yearly per capita income of 7,494 Yuan or above).
Smoking Status
Smoking status was categorized as smoker (including current smoker and former smoker) or never-smoker. Participants were asked: “Have you smoked in the last month?” When the respondent answered “yes”, the individual was categorized as a “current smoker”; if the respondent answered “no”, he or she was then asked, “have you ever smoked?” If the respondent answered “yes”, the individual was considered to be a “former smoker”; if the answers to both questions were “no”, the respondent was considered a never-smoker.
Noncommunicable Diseases (NCDs)
Noncommunicable disease status were determined by the following question: “Have you ever been diagnosed with noncommunicable diseases, such as hypertension, diabetes, COPD, CHD, strokes, cancer and so on?” Respondents who replied “yes” were categorized as having NCDs.
Respondent Characteristics
We controlled for an array of demographic and socioeconomic statuses that have been previously shown to be associated with cigarette smoking and poverty. The basic household situation included the household's residential location (rural or urban) and household size (number of household members). Demographic characteristics of the householder included the following: sex (male or female); age group (40–50 years, 50–60 years, 60–70 years, ≥70 years); educational level (illiterate, primary, junior high, senior high/vocational, college and above), marital status (single, married, divorced/widowed) and alcohol use (yes or no). We also asked, “Does raising cigarette prices influence tobacco use?” (yes or no). All covariates were categorical variables.
Statistical Analysis
The database was established using Epidata 3.1 and transferred into Stata/MP 16.0 software for analysis. Categorical (nominal/ordinal) variables were described using frequencies and percentages. Pearson's χ2-test was performed to assess differences in the characteristics between near-poverty and nonpoor households for the categorical variables. Both univariate and multivariate logistic regression models were used to determine the association between householder smoking and near-poverty households. The covariates were adjusted in the multivariable logistic regression model. Moreover, to accommodate endogenous covariates, we fitted an extended probit regression model (20) using the response to “Does raising cigarette prices influence tobacco use?” as the instrumental variable of smoking status to examine the association. In addition, we used generalized structural equation modeling to evaluate the mediating effect of NCDs.
Results
Demographic Characteristics
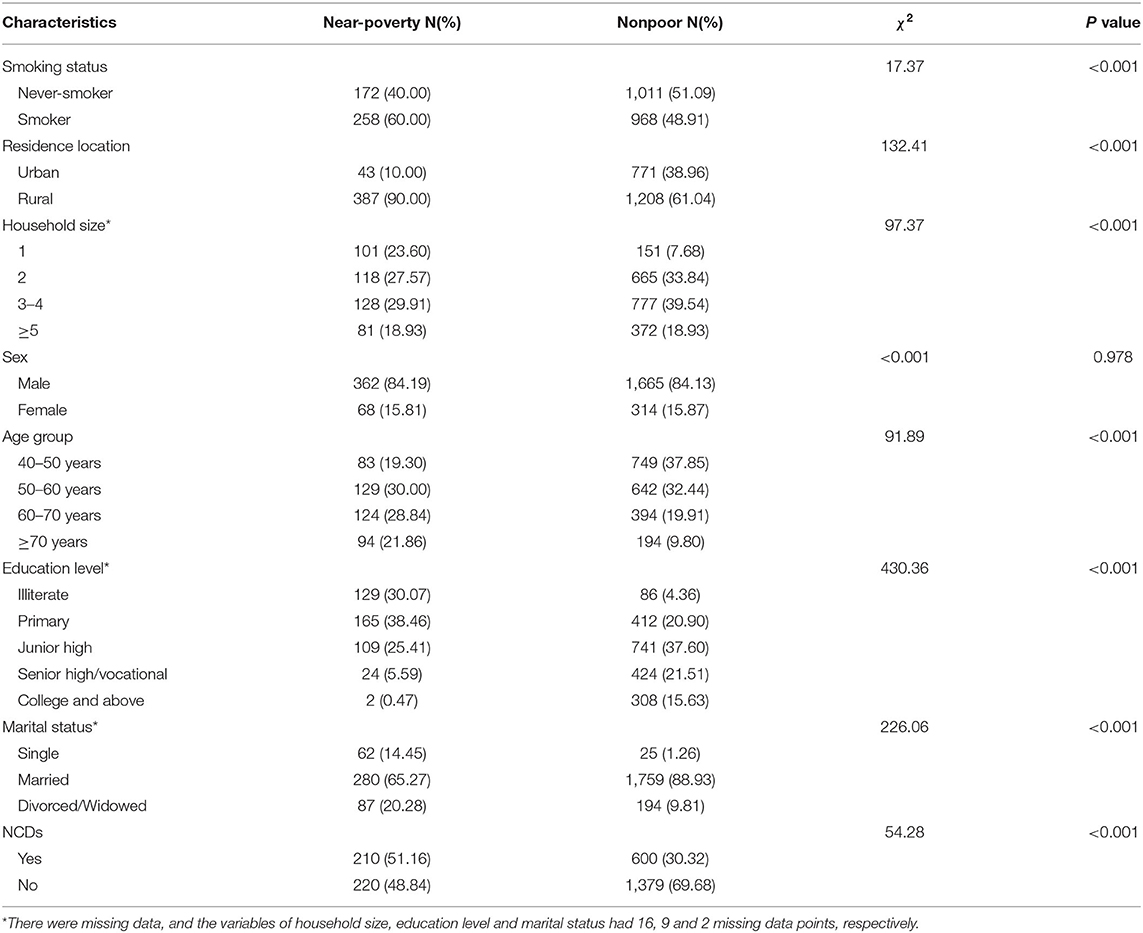
The study included 1,595 households from rural areas and 814 households from urban areas. Of the 2,409 households, 430 (17.85%) households were near-poverty, and 1,979 (82.15%) households were nonpoor. A total of 1,183 (49.11%) householders were never-smokers, while 1,226 (50.89%) householders were smokers. The ages of the householders ranged from 40 to 80 years, with an average age of 55.52 ± 10.42 years. Table 1 compares the basic household situations and the householders' demographic characteristics according to poverty status. Near-poverty households were more likely to be in rural areas and to have only one member in the household. For householders from near-poverty households, the smoking rate was higher than that in householders from nonpoor households (60.00 vs. 48.91%, P < 0.001). NCDs were reported to be more prevalent among near-poverty householders (51.16%) than nonpoor householders (30.32%). Furthermore, near-poverty householders tended to be older, to be single or divorced/widowed, and to have a lower education level. In terms of householder sex, there were no considerable differences between the two categories of households (84.19 vs. 84.13% male).
Association of Householder Smoking With Near-Poverty Household
Table 2 shows the association of householder smoking with near-poverty status among households in relatively underdeveloped regions of China. The results of Models 1–3 all suggest that householder smoking significantly increased the risk of households being near poverty (P < 0.05). As shown in Models 1–2, compared to households headed by never-smokers, households headed by smokers had an approximately 50% increase in the probability of household being near poverty, with odds ratios of 1.57 (95% CI: 1.27–1.94) and 1.49 (95% CI: 1.14–1.95), respectively. In Model 3, we found that the correlation between the errors of our two equations was significantly negative, so the unobservable factors that increased the householder smoking rates decreased the probability of households being near poverty. The results of Model 3 revealed that households headed by smokers had a two times higher risk of being near poverty than households headed by never-smokers, with an odds ratio of 2.01 (95% CI: 0.48–0.91).
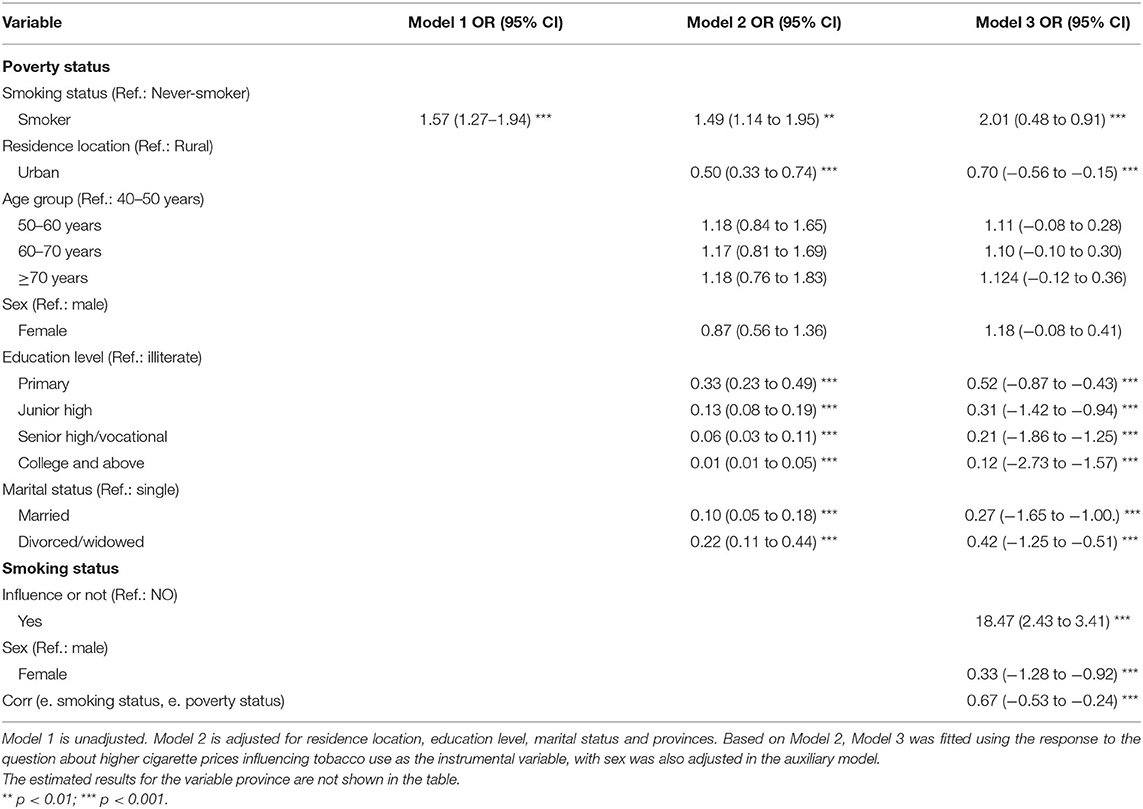
Table 2. Unadjusted and adjusted odds ratios of the association of near-poverty status with householder smoking.
Table 3 presents the average treatment effect (ATE) of householder smoking on near-poverty status and the average potential-outcome means (PO means) of the two smoking status based on Model 3. When all householders were never-smokers, we estimated that the average probability of households being near poverty was 12.14% (95% CI: 0.10–0.14), which would rise to 25.23% (95% CI: 0.22–0.28) when all householders were smokers. The average probability of households being near poverty increased by 12.99% (95% CI: 0.09–0.17) when all householders were smokers vs. when all householders were never-smokers.
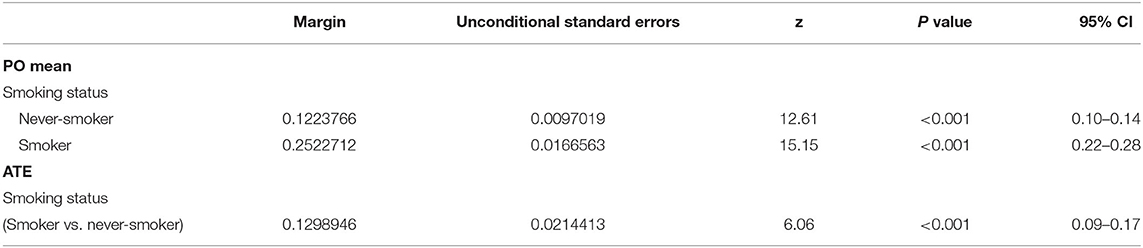
Table 3. Estimates of ATE of householder smoking on being near poverty and PO means of the two smoking status.
Moreover, households in rural areas had higher odds of being near poverty than households in urban areas (OR = 0.70, 95% CI: −0.56 to −0.15). Additionally, we also found that the higher the education level of the householder was, the lower the predictive probability of the household being near poverty in both rural and urban areas. However, regarding different education levels, households headed by smokers all had higher probabilities of being near poverty than households headed by never-smokers (Figure 1).
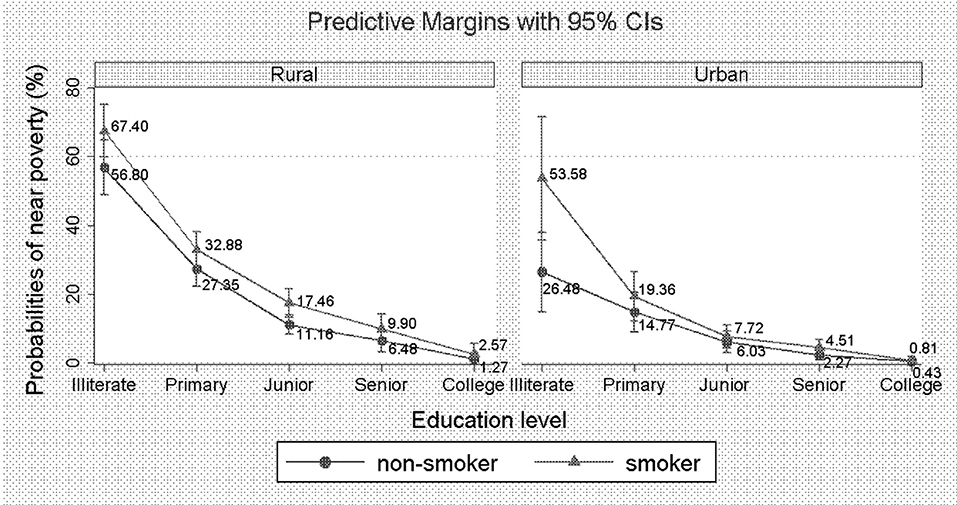
Figure 1. Predictive probabilities of being near poverty across different education levels and smoking status.
Mediating Effect of NCDs Between Householder Smoking and Near-Poverty Status
Figure 2 presents the path diagram of the generalized structural equation model estimation used to evaluate the mediating effect of NCDs between householder smoking and near-poverty status. As shown in Table 4, smokers had an increased risk of suffered from NCDs compared with never-smokers, and the direct effect of smoking on NCDs was estimated to be 0.33 (95% CI: 0.13–0.53). Householders who had NCDs had an increased probability of being near poverty, and the direct effect was estimated to be 0.53 (95% CI: 0.28–0.77). There was a significant positive indirect effect of householder smoking on households being near-poverty status (coefficient: 0.17; 95% CI: 0.04–0.31). In addition, we also observed that the direct and total effects of householder smoking on near-poverty status were estimated to be 0.38 (95% CI: 0.14–0.62) and 0.55 (95% CI: 0.28–0.82), respectively, which were both significant. Overall, we estimated that 31.57% of the total effect was mediated by NCDs.
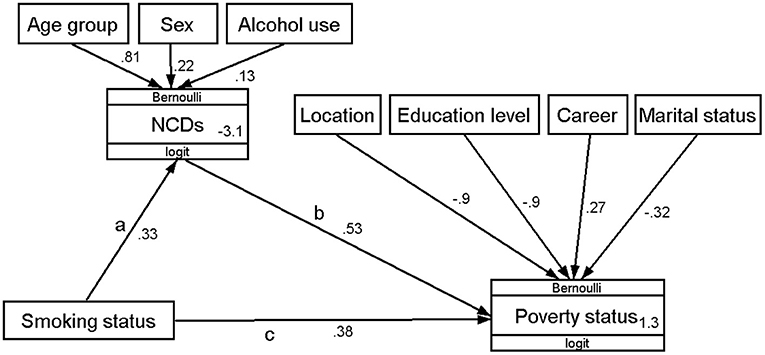
Figure 2. Path diagram of generalized structural equation model estimation of the mediating effect of NCD's between householder smoking and near-poverty status. Path c is the direct effect before taking into account the effect of NCDs. Path a and b make up the mediating pathway, with the mediating effect usually being described in the literature as the product of co-efficient (ab). Age group, sex, and alcohol use were adjusted as confounding variables of NCDs. Residence location, education level, career, and marital status were adjusted as the confounding variables of being near poverty.
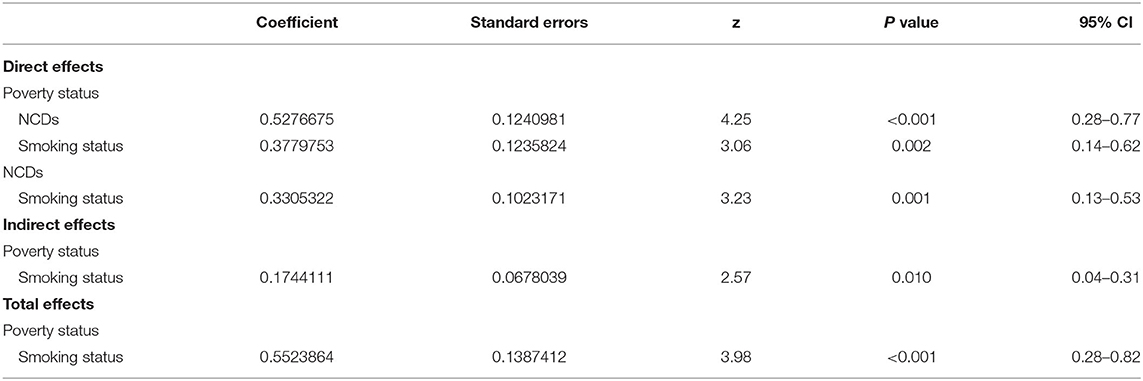
Table 4. Generalized structural equation model estimation results of the mediating effect of NCDs between householder smoking and near-poverty status.
Discussion
In this study, we observed a strong association between householder smoking and household being near-poverty status that persisted after adjusting for basic household situation and sociodemographic factors. In line with previous studies (19, 21), our results indicated that householder smoking elevated the probability of households being near poverty after adjustment for relevant covariates and potential confounds, which contributed evidence on the direct association between householder smoking and near-poverty status at the micro level.
Moreover, our study revealed a higher impact of smoking on poverty than in a previous study (19). Possible reasons are as follows. First, near-poverty status was used as the income criterion in this study, which was defined as 200% of the poverty level definition. Second, the study was conducted in relatively underdeveloped regions in China, particularly rural regions where residents have higher rates of smoking and poverty than residents of urban areas (22). Third, participants interviewed in this study were aged over 40, and studies have shown that adverse effects of smoking are cumulative and delayed, which would be gradually shown after smokers become middle-aged (14, 18). Meanwhile, we also found that the effect of householder smoking on household near-poverty status was more significant in households with householders aged over 50 than in households with householders under 50 years old.
The purchasing of cigarettes imposes a financial burden on low-income smokers and their families, but tobacco-related diseases, such as NCDs, exact an even greater cost and plunge those already on the margins into poverty. This study revealed that NCDs had a significantly positive mediating effect between householder smoking and household being near-poverty status, which offered evidence to consider the underlying mechanisms of the observed association. Potential explanations include the toxic effects of smoking on the human body, including but not limited to endothelial dysfunction, inflammation, and cancer, leading to a higher chance of developing NCDs (23, 24). Furthermore, NCDs result in reduced workforce participation and productivity, which has a direct bearing on household income (12, 19). Additionally, it has been suggested that NCDs significantly increase outpatient and hospitalization rates and medical expenditures, diverting household funds from basic necessities such as food, education and health care and further increasing the risk of poverty (25, 26). However, the causality of householder smoking and poverty is complex, and further studies should be carried out to provide more evidence.
Our study indicated that cigarette smoking has a strong association with near-poverty status, so from a policy perspective, controlling tobacco use and reducing smoking prevalence are not only important public health issues but are also closely related to poverty alleviation. As the most populated developing country in the world, China has made remarkable progress in poverty alleviation; however, problems of “sickness poor” and “poverty due to illness” remain the biggest barriers to consolidating achievements in poverty alleviation. Therefore, it is recommended to integrate tobacco control strategies with national poverty alleviation policies, which will be helpful in overcoming economic and political obstacles in the implementation of existing tobacco control measures. Additionally, we also found that NCDs mediated the association between householder smoking and near-poverty status, so it is recommended to strengthen health education and expand the coverage of medical insurance, which will be useful to lighten near-poverty households' financial burden and solve near-poverty households' inclination toward poverty because of illness. Furthermore, worldwide evidence has shown that raising tobacco taxes had the single greatest impact on the reduction of tobacco consumption (27, 28), and studies have demonstrated that low-income smokers were more price-sensitive and could reap greater health gains from increased taxes and higher prices of cigarettes (29, 30). It is also recommended to gradually increase the tobacco tax rate and prices to curb the tobacco epidemic.
We also noted that a low educational level of the householder was significantly associated with a higher probability of being near poverty. Previous studies have shown that less-educated individuals and individuals with lower socioeconomic status were more likely to be smokers (31, 32). In addition, studies have demonstrated that individuals with lower socioeconomic status also benefitted less from smoking prevention information (33, 34). Therefore, interventions aimed at preventing addiction to smoking among lower-educated individuals and individuals with lower socioeconomic status are recommended, including improving the educational and cognitive levels of individuals in relatively underdeveloped regions and promoting publicity campaigns about the hazards of smoking. In addition, due to lower awareness about the hazards of smoking and the benefits of smoking cessation aids and smoking cessation programs, individuals with lower socioeconomic status were less likely to quit smoking (35, 36). Hence, in future smoking cessation interventions, smokers with lower education and socioeconomic status should be given more attention.
The strengths of our study include the nationally representative survey. A broad range of data from relatively underdeveloped regions in China was collected, supplementing the empirical research conclusions on the relationship between householder smoking and household being near-poverty status. Moreover, in the study of the effects of householder smoking on near-poverty status, data endogeneity was unavoidable, and an extended probit regression model with the instrumental variable was used to overcome endogeneity problems. In addition, we used generalized structural equation modeling to evaluate the mediating effect of NCDs, providing evidence to consider the underlying mechanisms of the association between householder smoking and near-poverty households. However, there are also several limitations in this study. First, this study is a retrospective self-reported survey, and recall bias may be inevitable; however, prior studies have found that self-reported smoking status and health conditions had reasonable validity (37, 38). Second, the analysis was based on cross-sectional analyses, which limited our ability to make causal inferences about the association of householder smoking with being near poverty, and longitudinal association should be explored in future studies. Third, although we attempted to adjust several potential confounders, the analysis of the relationship of smoking and NCDs might miss potential important confounding variables due to lack of information such as diet and physical activity information.
Conclusions
In conclusion, householder smoking significantly elevated the risk of households being near poverty, and suffering NCDs had a positive mediating effect between householder smoking and near-poverty status. We also found that a lower educational level and living in rural areas were significantly associated with a higher probability of being near poverty.
What Is Already Known on This Subject?
• At the macro level, tobacco use imposes an economic burden through a reduction in productivity and an increase in the cost of medical treatment.
• At the micro level, few studies estimate the impact of cigarette smoking on poverty by reducing the income of Chinese urban residents and excessive medical spending.
What This Study Adds?
• At the micro level, householder smoking significantly elevated the risk of households being near poverty.
• Suffering from NCDs has a positive mediating effect on the relationship between householder smoking and households being near poverty.
Data Availability Statement
The datasets presented in this article are not readily available because data involves personal privacy issues. Requests to access the datasets should be directed to HY, eWFuZ2h1aW1pbjg1QDEyNi5jb20=.
Ethics Statement
This study was approved by the Ethics Committee of the Capital Institute of Pediatrics, Beijing (ID: SHERLL2020017). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CJ, BC, and HY conceptualized the study. The questionnaire was developed by CJ, BC, and AG and refined with input from HY. Data collection in the field was coordinated by BC and AG and supervised by HY and JS. HY, JS, and XC contributed substantially to data analyses and interpretation of the results under the guidance of CJ. HY drafted the manuscript. CJ and BC revised the manuscript critically for intellectual content. All authors approved the final version of the manuscript.
Funding
This work was supported by the Capital Institute of Pediatrics's Research Foundation (QN-2020-21) and the Capital's Funds for Health Improvement and Research (CFH 2020-3-1132).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We gratefully acknowledge the coordination of 24 PHC institutions that participated in this study and we thank the data collectors for their support. Additionally, we appreciate the heads of households and their households and all health workers involved in this study for their sustained support.
References
1. World Health Organization. (2020). Tobacco. Available online at: https://www.who.int/news-room/fact-sheets/detail/tobacco (accessed June 17, 2021).
2. Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. (2012) 1248:107–23. doi: 10.1111/j.1749-6632.2011.06202.x
3. Yang G, Wang Y, Wu Y, Yang J, Wan X. The road to effective tobacco control in China. Lancet. (2015) 385:1019–28. doi: 10.1016/S0140-6736(15)60174-X
4. World Health Organization. Regional Office for the Western Pacific. (2017). The bill China Cannot Afford: Health, Economic and Social Costs of China's Tobacco Epidemic. WHO Regional Office for the Western Pacific. Available online at: https://apps.who.int/iris/handle/10665/255469. (accessed June 17, 2021).
5. Chen Z, Peto R, Zhou M, Iona A, Smith M, Yang L, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. (2015) 386:1447–56. doi: 10.1016/S0140-6736(15)00340-2
6. United Nations. Sustainable Development Goals, Goal 1: End Poverty in all its Forms Everywhere. Available online at: https://www.un.org/sustainabledevelopment/poverty/ (accessed 19 July, 2021).
7. Bloom DE, Dan C, Jane-Llopis E, Prettner K, Stein A, Feigl A. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Disease in Low- and Middle-Income Countries, PGDA Working Papers. Program on the Global Demography of Aging. (2011) p. 7511
8. Jaspers L, Colpani V, Chaker L, van der Lee SJ, Muka T, Imo D, et al. The global impact of non-communicable diseases on households and impoverishment: a systematic review. Eur J Epidemiol. (2015). 30:163–88. doi: 10.1007/s10654-014-9983-3
9. Chaker L, Falla A, van der Lee SJ, Muka T, Imo D, Jaspers L, et al. The global impact of non-communicable diseases on macro-economic productivity: a systematic review. Eur J Epidemiol. (2015) 30:357–95. doi: 10.1007/s10654-015-0026-5
10. Gallucci G, Tartarone A, Lerose R, Lalinga AV, Capobianco AM. Cardiovascular risk of smoking and benefits of smoking cessation. J Thorac Dis. (2020) 12:3866–76. doi: 10.21037/jtd.2020.02.47
11. GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. (2017) 389:1885–906. doi: 10.1016/S0140-6736(17)32559-X
12. Ekpu VU, Brown AK. The economic impact of smoking and of reducing smoking prevalence: review of evidence. Tob Use Insights. (2015) 8:1–35. doi: 10.4137/TUI.S15628
13. Pearce A, Sharp L, Hanly P, Barchuk A, Bray F, de Camargo Cancela M, et al. Productivity losses due to premature mortality from cancer in Brazil, Russia, India, China, and South Africa (BRICS): a population-based comparison. Cancer Epidemiol. (2018) 53:27–34. doi: 10.1016/j.canep.2017.12.013
14. National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US) (2014).
15. Kristina SA, Endarti D, Wiedyaningsih C, Fahamsya A, Faizah N. Health care cost of noncommunicable diseases related to smoking in Indonesia, 2015. Asia Pac J Public. (2018) 30:29–35. doi: 10.1177/1010539517751311
16. DG SANCO. A Study on Liability and the Health Costs of Smoking: Updated Final Report. London: GHK. (2012).
17. Goodchild M, Nargis N. Tursan d'Espaignet E. Global economic cost of smoking-attributable diseases. Tob Control. (2018) 27:58–64. doi: 10.1136/tobaccocontrol-2016-053305
18. Liu Y, Rao K, Hu TW, Sun Q, Mao Z. Cigarette smoking and poverty in China. Soc Sci Med. (2006) 63:2784–90. doi: 10.1016/j.socscimed.2006.06.019
19. Wei H, Zhong Z, Yang L, Yao T, Huang S, Mao Z. Impact of smoking on the income level of Chinese urban residents: a two-wave follow-up of the China Family Panel Study. BMJ Open. (2020) 10:e036939. doi: 10.1136/bmjopen-2020-036939
20. StataCorp LLC. Stata Extended Regression Models Reference Manual Release 16. Texas: Stata Press (2019) p. 134.
21. Shusted CS, Kane GC. Linkage Between Poverty and Smoking in Philadelphia and Its Impact on Future Directions for Tobacco Control in the City. Population Health Manag. (2020) 23:68–77. doi: 10.1089/pop.2019.0006
22. Hu TW, Mao Z, Liu Y, de Beyer J, Ong M. Smoking, standard of living, and poverty in China. Tob Control. (2005) 14:247–50. doi: 10.1136/tc.2004.010777
23. Rezk-Hanna M, Benowitz NL. Cardiovascular Effects of Hookah Smoking: Potential Implications for Cardiovascular Risk. Nicotine Tob Res. (2019) 21:1151–61. doi: 10.1093/ntr/nty065
24. Münzel T, Hahad O, Kuntic M, Keaney JF, Deanfield JE, Daiber A. Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes. Eur Heart J. (2020) 41:4057–70. doi: 10.1093/eurheartj/ehaa460
25. Xin Y, Qian J, Xu L, Tang S, Gao J, Critchley JA. The impact of smoking and quitting on household expenditure patterns and medical care costs in China. Tob Control. (2009) 18:150–5. doi: 10.1136/tc.2008.026955
26. Efroymson D, Pham HA, Jones L, FitzGerald S. Thu le T, Hien le TT. Tobacco and poverty: evidence from Vietnam. Tob Control. (2011) 20:296–301. doi: 10.1136/tc.2010.039735
27. Hu TW, Mao Z, Shi J, Chen W. The role of taxation in tobacco control and its potential economic impact in China. Tob Control. (2010) 19:58–64. doi: 10.1136/tc.2009.031799
28. Chaloupka FJ, Straif K, Leon ME. Effectiveness of tax and price policies in tobacco control. Tob Control. (2011) 20:235–8. doi: 10.1136/tc.2010.039982
29. Choi SE. Are lower income smokers more price sensitive?: the evidence from Korean cigarette tax increases. Tob Control. (2016) 25:141–6. doi: 10.1136/tobaccocontrol-2014-051680
30. Nargis N, Ruthbah UH, Hussain AK, Fong GT, Huq I, Ashiquzzaman SM. The price sensitivity of cigarette consumption in Bangladesh: evidence from the International Tobacco Control (ITC) Bangladesh Wave 1 (2009) and Wave 2 (2010) Surveys. Tob Control. (2014) 23:i39–47. doi: 10.1136/tobaccocontrol-2012-050835
31. Huisman M, Kunst AE, Mackenbach JP. Inequalities in the prevalence of smoking in the European Union: comparing education and income. Prev Med. (2005) 40:756–64. doi: 10.1016/j.ypmed.2004.09.022
32. Mathur C, Stigler MH, Perry CL, Arora M, Reddy KS. Differences in prevalence of tobacco use among Indian urban youth: the role of socioeconomic status. Nicotine Tob Res. (2008) 10:109–16. doi: 10.1080/14622200701767779
33. Mercken L, Moore L, Crone MR, De Vries H, De Bourdeaudhuij I, Lien N, et al. The effectiveness of school-based smoking prevention interventions among low- and high-SES European teenagers. Health Educ Res. (2012) 27:459–69. doi: 10.1093/her/cys017
34. Patnode CD, O'Connor E, Whitlock EP, Perdue LA, Soh C. Primary care-relevant interventions for tobacco use prevention and cessation in children and adolescents: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. (2013) 158:253–60. doi: 10.7326/0003-4819-158-4-201302190-00580
35. Siahpush M, McNeill A, Hammond D, Fong GT. Socioeconomic and country variations in knowledge of health risks of tobacco smoking and toxic constituents of smoke: results from the 2002 International Tobacco Control (ITC) Four Country Survey. Tob Control. (2006) 15:iii65–70. doi: 10.1136/tc.2005.013276
36. Young-Hoon KN. A longitudinal study on the impact of income change and poverty on smoking cessation. Can J Public Health. (2012) 103:189–94. doi: 10.1007/BF03403811
37. Gilpin EA, Pierce JP, Cavin SW, Berry CC, Evans NJ, Johnson M, et al. Estimates of population smoking prevalence: self-vs proxy reports of smoking status. Am J Public Health. (1994) 84:1576–9. doi: 10.2105/AJPH.84.10.1576
Keywords: cigarette smoking, poverty, noncommunicable diseases (NCDs), extended probit regression, generalized structural equation model
Citation: Yang H, Chen B, Guo A, Song J, Cheng X and Jin C (2022) Association of Householder Smoking With Poverty and the Mediating Effect of NCDs in Relatively Underdeveloped Regions in China. Front. Public Health 10:858761. doi: 10.3389/fpubh.2022.858761
Received: 09 February 2022; Accepted: 04 April 2022;
Published: 19 May 2022.
Edited by:
Han C. G. Kemper, Amsterdam University Medical Center, NetherlandsReviewed by:
Yayi Prabandari, Gadjah Mada University, IndonesiaNorsham Juliana, Universiti Sains Islam Malaysia, Malaysia
Copyright © 2022 Yang, Chen, Guo, Song, Cheng and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chenggang Jin, Y2dqaW4yMDA1QDEyNi5jb20=
 Huimin Yang
Huimin Yang Bowen Chen1
Bowen Chen1 Xi Cheng
Xi Cheng Chenggang Jin
Chenggang Jin