
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 18 April 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.856809
This article is part of the Research TopicGlobal Surgery: The Next Frontier in Global Public HealthView all 15 articles
Background: Partner involvement in maternal health services utilization remains a major public challenge in the developing world. Strategies of involving men in maternal health services are a critical and proven intervention for reducing maternal and neonatal mortality by ensuring safe delivery and reducing complications during childbirth. Moreover, the husbands' involvement during pregnancy helps their spouses to make timely decisions and avoid maternal delays, especially first and second delays. Although birth and complication readiness have been studied in developing countries such as Ethiopia, almost all previous researchers were focused primarily on women participants. Therefore, we aimed to investigate factors associated with husband involvement in birth preparedness and complication readiness plan in Haramaya Health and Demographic Surveillance site, Eastern Ethiopia.
Methods: A community-based cross-sectional study was conducted from March 1 to 30, 2020 among men whose wives were pregnant in Haramaya Health and Demographic Surveillance (HDSS) site in Eastern Ethiopia. The calculated sample size was 653, however while contacting 653 husbands only 630 had given the full interview, hence 630 respondents were remained in the analysis. Participants were approached through a systematic sampling technique. Data were collected using a pre-tested structured questionnaire through a face-to-face interview, and entered into Epidata version 3.1 and analyzed using SPSS version 22 (IBM SPSS Statistics, 2013). The prevalence was reported using proportion with 95% Confidence Interval (CI) and summary measures. Predictors were assessed using a multivariable logistic regression analysis model and reported using an adjusted odds ratio (AOR) with 95%CI. Statistical significance was declared at p < 0.05.
Results: Overall, the prevalence of the husband's plan to participate in birth preparedness and complication readiness was 59.6% (95%CI:56–64%). In the final model of multivariable analysis, predictors like husband's knowledge of birth preparedness and complication readiness [AOR = 4.18, 95%CI:2.05, 8.51], having a discussion with spouse on the place of delivery [AOR = 6.84, 95% CI: 4.17, 11.22], husband's knowledge of danger signs during labor and delivery [AOR = 3.19, 95 % CI: 1.52, 6.71], and making a postpartum plan[AOR = 2.30, 95 % CI: 1.38, 3.85] were factors statistically associated with husband's plan to participate in birth preparedness.
Conclusions: This study pointed out that two in every five husbands failed to plan birth preparedness and complication readiness. As a result, all stakeholders should emphasize male partners' education in terms of birth preparedness and complication readiness, as well as knowledge of danger signs during labor and delivery. They should also encourage male partners to discuss a place of delivery and have a postpartum plan in place to reduce potential complications related to labor and delivery.
Globally, approximately 287,000 mothers die each year as a result of pregnancy and childbirth complications. The vast majority of these maternal deaths (99%) occur in developing countries, with Sub-Saharan Africa alone accounting for 66% (1). These deaths are the result of complications during pregnancy, childbirth, or postpartum. Studies have shown that making a birth plan that includes birth-preparedness and complication readiness measures for pregnant women, their spouses, and their families are found to be a key strategy that can reduce the number of women dying from such complications (1, 2).
Birth preparedness and complication readiness (BPCR) is a comprehensive package aimed at promoting timely access to skilled maternal and neonatal services, as well as encouraging pregnant women and their families to actively prepare for and make decisions about delivery (2). This stems from the fact that every pregnant woman is at risk of unexpected and life-threatening complications that could result in death or injury to herself or her infant (3). According to various research reports, pregnancy and childbirth are still regarded solely as women's issues in Sub-Saharan Africa because husbands have tremendous control over the women's decision process both socially and economically (4–7). On the contrary, evidence has shown that involving men in maternal health care has positive outcomes such as reduced maternal morbidity and mortality due to a sufficient birth plan, thereby avoiding care-seeking delays due to obstetric emergencies (8–11), increased institutional deliveries (5, 9, 10) and postnatal service utilization (9, 12). With these all interventions, three phases of maternal delay can be averted.
Literature has shown that numerous factors affect the husband's involvement in the process of BPCR planning during pregnancy and childbirth. For instance, previous research report identified local factors (societal perception such as considering childbirth as a natural process, pregnancy and childbirth are women's role, preference for traditional birth attendance's care and novelty of the idea of husband's involvement in pregnancy and birth care) as barriers of husband's plan to participate in BPCR (13–15). In Sub-Saharan Africa like Ethiopia, despite its public health importance for birth outcomes, male participation in maternal and child health (MCH) remains low, and having a male partner (MP) present in the labor room during delivery is utterly impossible in many settings (9, 11, 16), even in a limited area like urban setting, where male partners have been supportive to their spouses, there are unwelcoming, intimidating, and unsupportive health systems, presenting a missed opportunity, which embarrasses their commitment (13, 17). Similarly, researchers have reported that factors such as poor timely action by family, which leads to a great deal such as looking for a source of money and potential blood donors in case of emergency, finding for transportation, and reaching the appropriate referral facility remain a major challenge in Africa (14, 18).
In Ethiopia, husbands have strong decision-making power over their spouses both at the community and at the household level, and traditionally women have little independence in decisions making process. Cultural barriers, knowledge of recognizing potential complications, and facility service factors all contribute to the husband's involvement in birth preparation and complication readiness planning (19). According to previous studies conducted in limited areas of Ethiopian regions, husband disapproval for antenatal care accounts for 15.5% of the factors influencing antenatal care, and only 21% of pregnant women were accompanied by their husbands to visit the ANC clinic (13). As a result, male participation in birth preparation and complication preparation will be critical in reducing maternal mortality (20). Male involvement allows men to encourage their wives to use obstetric services, and the couple will be better prepared for birth complications. This would result in a reduction in all three phases of delay: delay in deciding to seek care, delay in getting to care, and finally delay in receiving care. In developing countries, the male partner can play an important role, particularly in the first and second stages of delay, and thus positively impact birth outcomes (21–23).
In Ethiopia, in the last decade, various studies have been conducted to assess the practice of birth preparation and complication readiness among mothers; with little attention have been given to the level of the husband's involvement in birth preparation. Moreover, although numerous factors associated with male involvement in BPCR have been identified in the various research report (13, 14, 24, 25), in Ethiopia, husbands' participation in the BPCR received little policy attention (23). In addition, the majority of the previous studies were facility-based and primarily focused on emergency obstetric care and other routine services (26). Therefore, this study was aimed to investigate husbands' participation in BPCR and its associated factors among husbands whose wives were pregnant in the Haramaya HDSS site, Eastern Ethiopia.
A community-based cross-sectional study was conducted from March 1 to March 30, 2020, in four kebeles (the smallest administrative unit) in Ethiopia, namely Biftu-Geda, Ifa-Oromia, Gobe-Chala, and Kuro found in Haramaya districts, which were located 500 km away from Addis Ababa, capital city Addis Ababa. The 2007 national census reported the total population for this District is 271,018, of whom 138,282 were men and 132,736 were women (27). The Haramaya Health and Demographic Surveillance Site which is maintained by Haramaya University was established in the year 2018 GC. The site was established on 12 rural kebeles of Haramaya district. The site constitutes 93,363 residents and 1,712 pregnant women (28).
All husbands whose wives were pregnant in the Haramaya HDSS site during the study period were considered as source population. The study population consisted of all systematically selected husbands whose wives were in their third trimester of pregnancy in the Haramaya district HDSS site's selected kebeles. Husbands who were not staying with their wives during pregnancy and childbirth and, those who were critically ill and unable to provide the required information during data collection were excluded from the study.
In this study, the maximum required sample size was calculated using the single population proportion formula by considering the following assumptions. Taking the prevalence of husband involvement in BPCR (45%, P=0.45) from previous a study conducted in Wolaita Sodo town, Southern Ethiopia (23), a 95% confidence level (Zα/2 =1.96), to increase the representativeness of the sample size and to boost the precision, 4%(α = 0.04) tolerable margin of error was considered. Thus,
By adding a 10% contingency for the non-response rate, the calculated sample size was 653, however while contacting 653 husbands only 630 had given the full interview, hence 630 respondents were remained in the analysis.
In this study, two-stage sampling was used. Initially, a simple random sampling technique was used to select four kebeles from a total of 12 rural kebeles of the Haramaya HDSS site. To do so, the Haramaya HDSS database maintained by Haramaya University was used as a sampling frame to identify a list of pregnant women in each kebele. The total number of pregnant women who are living with their spouse in these four kebeles is 1,332, of which Biftu-Geda, Gobe-Chala, Kuro, and Ifa Oromia have 343, 364, 351, and 274 pregnant women respectively (28). Then, the house of pregnant women was traced to identify the study participants (Households with the husbands of pregnant women). The calculated sample size was proportionally allocated to the four selected kebeles. The systematic sampling technique was employed to select the households, and the first house was selected using lottery methods. For absent participants, rescheduling was done to conduct the interview again. If the selected household does not fulfill the inclusion criteria, the next household was substituted for our study and if more than one candidate was available in the single household, one of them was interviewed by lottery method. Accordingly, a total of 653 sample sizes was proportionally allocated to each kebele to obtain the required numbers of an individual to be included in the estimated sample from each aforementioned kebeles. Then, the Kth interval was calculated for all selected kebeles (Kth = 1,332/653 = ≈2). The sequence of the “kth” interval was 2 for all selected kebeles. Therefore, every second eligible participant was interviewed, and data were collected until the required sample size was obtained (Figure 1).
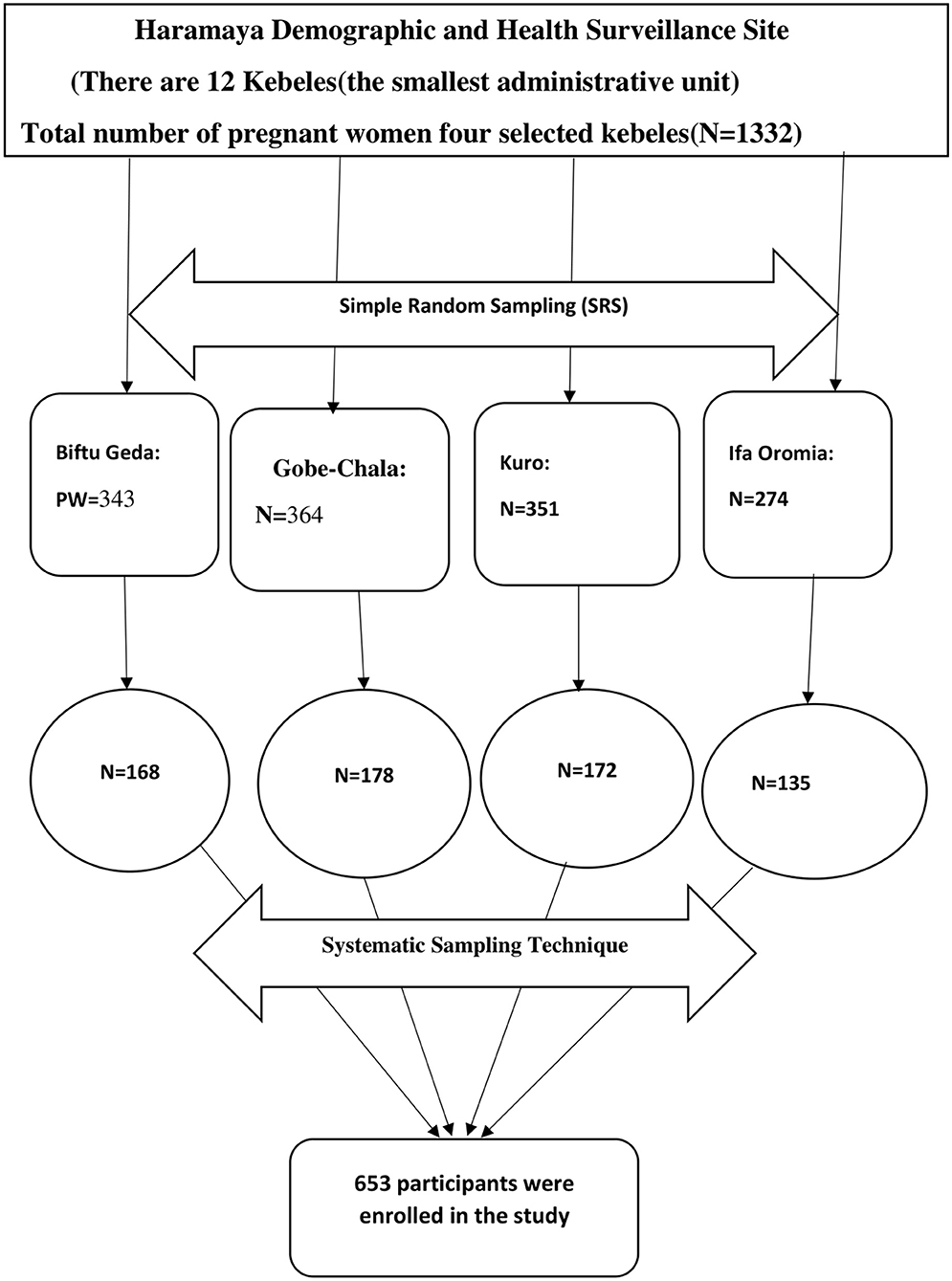
Figure 1. The schematic diagram of the sampling procedure for the study on husbands' plan to participate in birth preparedness and Complication Readiness in Haramaya Health and Demographic Surveillance System Site, Eastern Ethiopia.
The data were collected through a face-to-face interview with a pretested structured questionnaire developed after a review of the literature (29). The questionnaires asked about socioeconomic and demographic information, knowledge of danger signs during pregnancy, labor and delivery, and postnatal care, knowledge of BPCR, and plans to participate in birth preparedness and complication readiness. Ten Bachelor of Science (BSc) nurses were collected the data after a five-day training on the tools and survey methods.
Dependent variable: In this study, the outcome variable was husbands' plan to participate in birth preparedness and complication readiness (Yes/No). The outcome variable was dichotomized as 1 and 0. Thus, it was recoded into binary outcomes as “good participation = 1” and “poor participation = 0”. Independent variables: In this study, the explanatory variables were categorized as: demographic and socioeconomic characteristics (age, religion, number of children and occupation, level of education, and marital status), obstetric related factors: Knowledge of husbands on key danger signs of pregnancy, labor and the postpartum period, knowledge of husbands on birth preparedness and complication readiness.
Birth preparedness and complication readiness: is a strategy to encourage husbands to know the signs of obstetric complications and emergencies, to choose a preferred birthplace and attendant at birth, to arrange for transportation to the skilled care site in the event of emergence, to save or arrange alternate funds for the cost of the emergence, and to accompany her to the emergence care. identifying a blood donor and preparing clean clothes for the mother and child (30). Husbands' plan to participate in BPCR: was measured by nine items, those who responded 'yes' scored 1 and if 'No' scored 0 then the respondents who were scored above the mean value of the indicators of BPCR (23). Good participation in BPCR: Those husbands who practiced five and above elements of nine items (23). Poor participation in BPCR: Husbands who practiced four or fewer elements of nine items (23).
Knowledge of danger signs: According to WHO, there are 10 danger signs of pregnancy, delivery, and postnatal period. Better knowledge: In this study, the respondents who knew greater than or equal to five danger signs during pregnancy, delivery, and postnatal period which is above the mean value (danger signs assigned from 1 to 10) were categorized as ‘have better knowledge” (31). Good knowledge: The respondent who knew below the mean value (<5 danger signs) were considered as “have a good knowledge” (31). Poor knowledge: In this study, the husband's poor knowledge about danger signs can be defined as if the respondent did not know any listed danger signs, they were considered as “poor knowledge” (31).
Husband's knowledge of BPCR: According to the WHO, there are 9 items to assess the components of BPCR. Better knowledge: In this study, if the husbands mentioned five and above components of BPCR items, which is the mean value (component assigned 1- 9), they categorized as “have better knowledge” (31). Good knowledge: The respondents who knew below mean value (<5 components) of the nine BPCR items, they considered as “have good knowledge” (31). Poor knowledge: In this study, if the respondents did not know any components of Birth preparedness and complication readiness, we categorized them as “ have poor knowledge” (31).
The questionnaire was initially prepared in English and then translated into the local languages by a bilingual expert (Afaan Oromoo language). Then, it was translated back into an English version to ensure its consistency. The data collectors and field supervisors received training on the data collection tool and procedures. Before the actual study data collection, the pretest was conducted among 3% of husbands whose wives were pregnant in similar settings. The investigators and experienced field research supervisors provided regular supervision.
First, the collected data were checked for completeness, consistency. Then, they were cleaned, coded, and entered into EpiData version 3.1 for further analysis. The entered data were exported to SPSS version 22 for analysis. Descriptive and summary statistics were conducted and reported using frequency tables and figures. The outcome variable was recoded into binary outcome as “good participation = 1” and “poor participation = 0”. A binary logistic regression model was fitted to check for an association between independent variables and the outcome variable. The model fitness was checked by Hosmer-Lemeshow statistics and Omnibus tests. A multivariable analysis was performed to identify the true predictors of the husband's plan to participate in the BPCR plan. A multi-collinearity test was carried out to check the presence of correlation between independent variables by using the standard error and co-linearity statistics, and no collinearity effects were detected. Thus, the value of the Variance Inflation Factor (VIF) was 0.951. The direction and strength statistical association was measured by odds ratio (OR) along with the 95% confidence interval (CI). A p < 0.05 was considered to declare statistical significance both in bi-variable and multivariable analysis.
A total of 630 husbands were enrolled in this study, with a response rate of 96.5 %. The age of the study participants ranged from 18 to 60 years with a mean age of 31.7 (SD = ±7.4). The majority of the study participants, 387 (61.4%) were between the ages of 30 and 39 years. Four hundred-thirty (68.3%), two hundred-forty (38.1%), and five hundred-eight-four (92.7%) of the husbands were farmers, had no formal education, and were married in monogamous marriages, respectively. More than half of the participants, 356 (56.5 %) had 1–4 children in their family (Table 1).
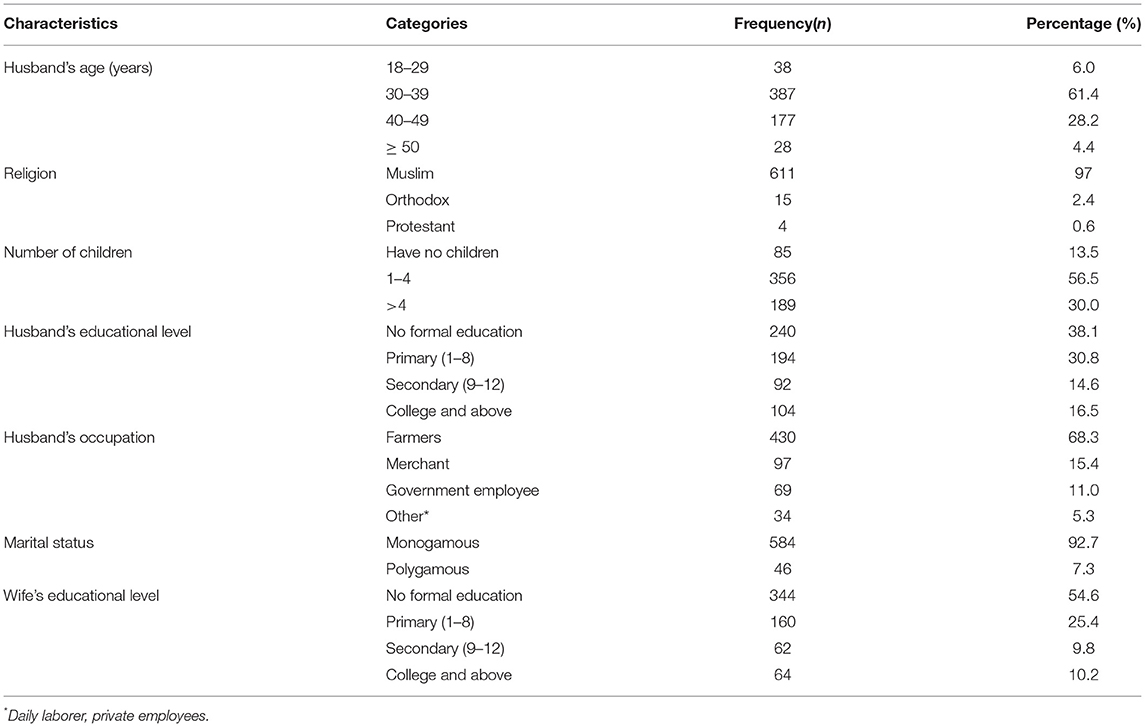
Table 1. Socio-demographic characteristics of husbands whose wives were pregnant in Haramaya HDSS site, Eastern Ethiopia, 2020.
Regarding obstetric danger signs, more than half of the respondents, 352 (55.9%) mentioned five and more danger signs during delivery and around 195(31.0%) of them listed five and more danger signs during the postnatal period. Similarly, nearly half 272(43.2%) of the husbands had responded to five and more BPCR components. Five hundred ninety-seven (94.8%) of the participants had awareness of the significance of ANC during pregnancy (Table 2).
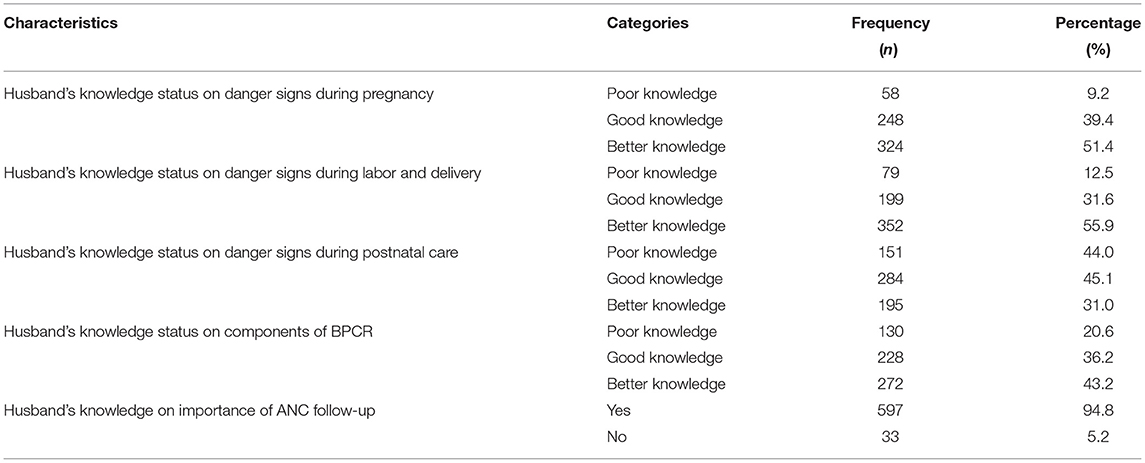
Table 2. Knowledge of obstetric danger signs related factors among husbands whose wives were pregnant in Haramaya HDSS site, Eastern Ethiopia, 2020.
In this study, the respondents were also assessed for their source of information about birth preparation and complication readiness. Accordingly, of the total 630 study participants enrolled in this study, more than half (57.16%) of them were heard from health care providers followed by media (Radio/TV) (18.53%), family/friends (12.41%), reading printed materials (7.17%), and the remaining 4.73% of the heard from other sources in their life (Figure 2).
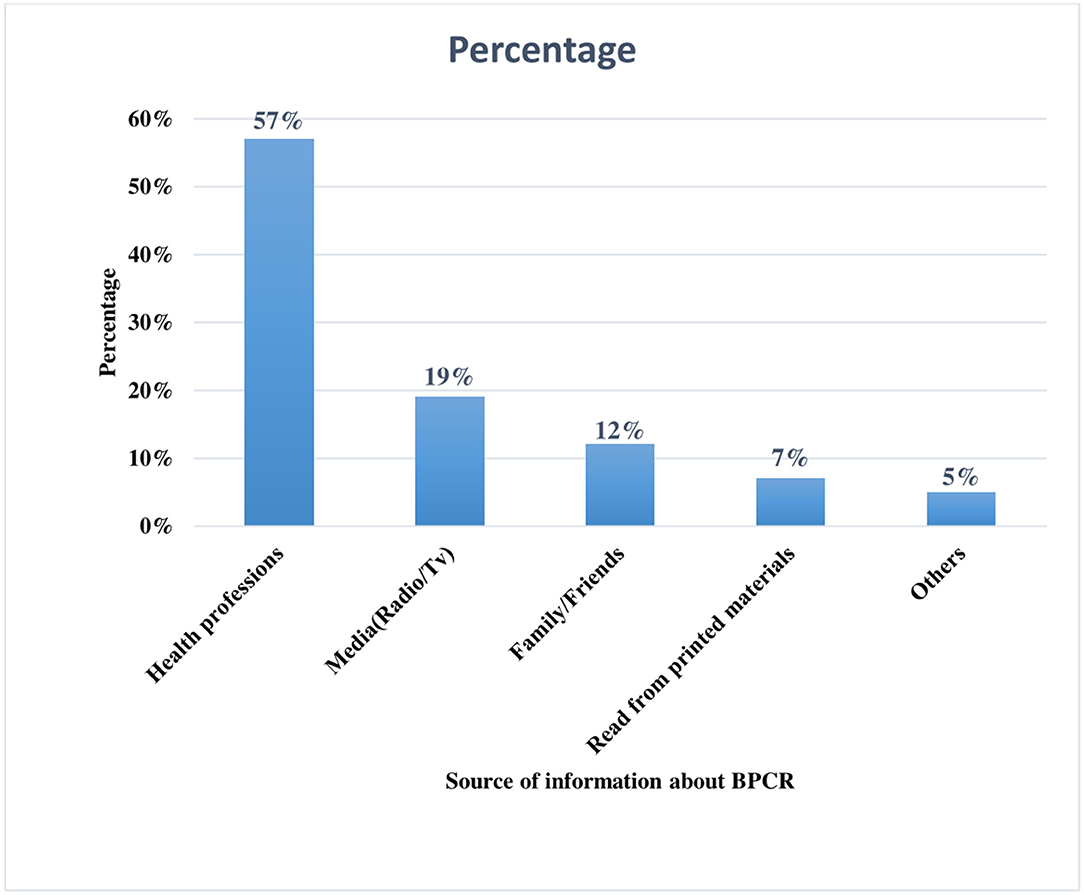
Figure 2. Source of information about birth preparedness and complication readiness Haramaya Health and Demographic Surveillance System site, Eastern Ethiopia, 2020.
In this study, the husband's status of birth preparation and complication readiness plan during labor, delivery, and postpartum were assessed. Accordingly, of the 630 husbands who participated in the study, nearly half, 334(53.0%) of the respondents were made a plan for the place of delivery, and three hundred-four (48.3%) of them identified skilled birth attendants during labor and delivery. Nearly two-thirds (64.9%) of the respondents stated that they save money for delivery. Almost one-third (33.0%) of husbands had a plan for blood donation and 302 (47.9%) had a plan to accompany their wives during labor and delivery. Likewise, two hundred sixty-seven (42.4%) of the husbands made a transportation plan, and nearly half (49.7%) of them made a postpartum plan during their current pregnancy (Table 3).
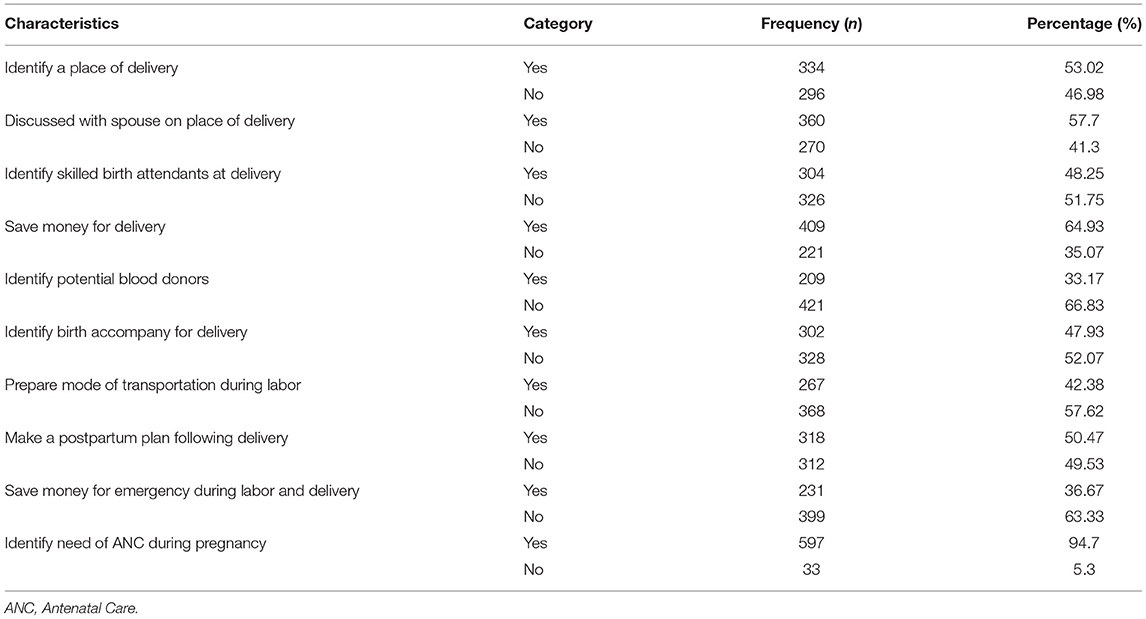
Table 3. Husband's plan to participate in birth preparedness and complication readiness plan in Haramaya HDSS site, Eastern Ethiopia, 2020.
Moreover, in this study, only 379(60.2%) of husbands had a plan for birth preparedness and complication readiness in the current pregnancy. Of 379 husbands who had birth preparedness and complication readiness plan, around 226 (59.6%) of the husbands had a good participation plan while the remaining 153 (40.4%) of them had a poor participation plan. Thus, the overall proportion of husbands' plans to participate in birth preparedness and complication readiness was 59.6% (95%CI:56–64%) (Figure 3).
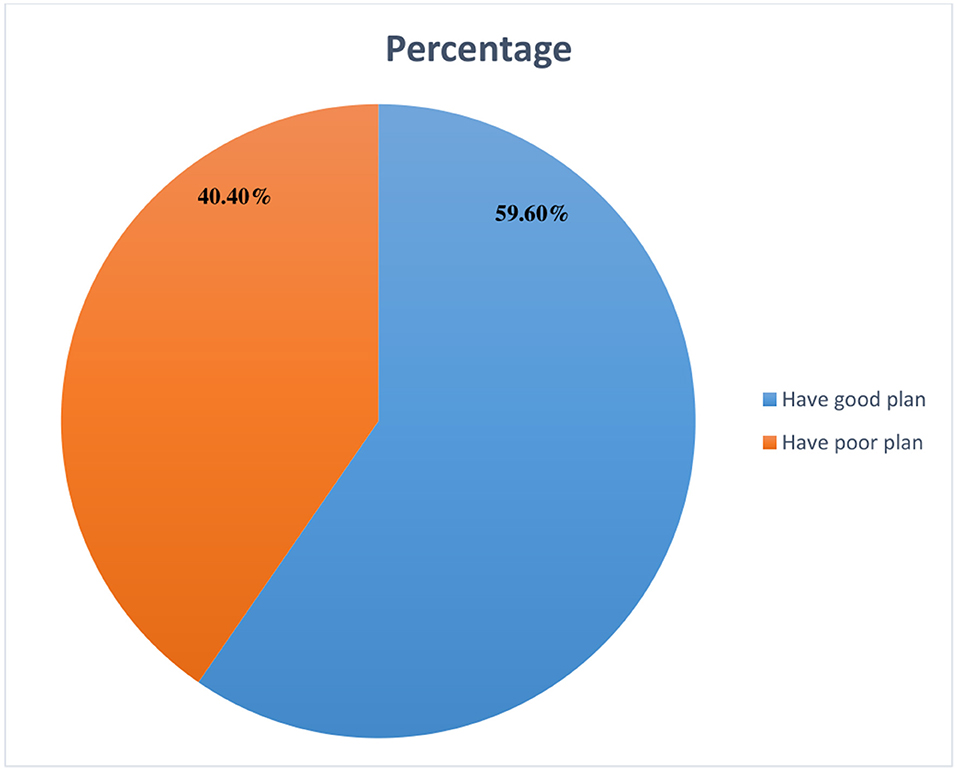
Figure 3. Husband's plan to participate in birth preparedness and complication readiness plan in Haramaya Health and Demographic Surveillance System site, Eastern Ethiopia, 2020.
In the bi-variable analysis, predictor variables such as: husband's educational level, husband's occupational status, the importance of ANC, husband's knowledge status on BPCR, knowing danger signs during pregnancy, husband's knowledge of BPCR, husband's knowledge of danger signs during labor and delivery, having a discussion with spouse on the place of delivery, having government support in BPCR and making a plan for PNC follow-up were significantly associated with husband's plan to participate in BPCR in the current pregnancy.
However, in the final model of multivariable logistic regression analysis, predictor variables like husband's knowledge of BPCR, husband's knowledge status of danger signs during labor and delivery, having a discussion with spouse on the place of delivery, and making postpartum plan following delivery were factors remained significantly associated with husband participation in BPCR. Accordingly, husbands who had better knowledge about BPCR were 4.2 times more likely to participate in BPCR than those husbands who had poor knowledge (AOR = 4.18, 95% CI: 2.05, 8.51). Similarly, the likelihood of participating in the BPCR plan was nearly four times higher among husbands who had good knowledge about BPCR than those husbands who had poor knowledge (AOR = 3.99, 95% CI: 2.20, 7.25).
Moreover, the odds of participating in the BPCR plan were 3.19 times higher among husbands who had better knowledge about birth preparedness and complication readiness plan than their counterparts (those husbands who had poor knowledge) (AOR = 3.19, 95% CI; 1.52, 6.71). Likewise, husbands who had good knowledge of danger signs during labor and delivery were nearly three times more likely to participate in BPCR than those who had poor knowledge of birth plan (AOR = 2.84, 95% CI; 1.34, 6.02). Additionally, participants who discussed with their spouse the place of delivery were 6.8 times more likely to participate in BPCR than those who did not discuss the place of delivery with their wives (AOR = 6.84, 95% CI; 4.17, 11.22). Moreover, husbands who had a postpartum plan with their wives were 2.3 more likely to participate in BPCR than those who did not make plans anymore (AOR = 2.3, 95% CI: 1.38, 3.85) (Table 4).
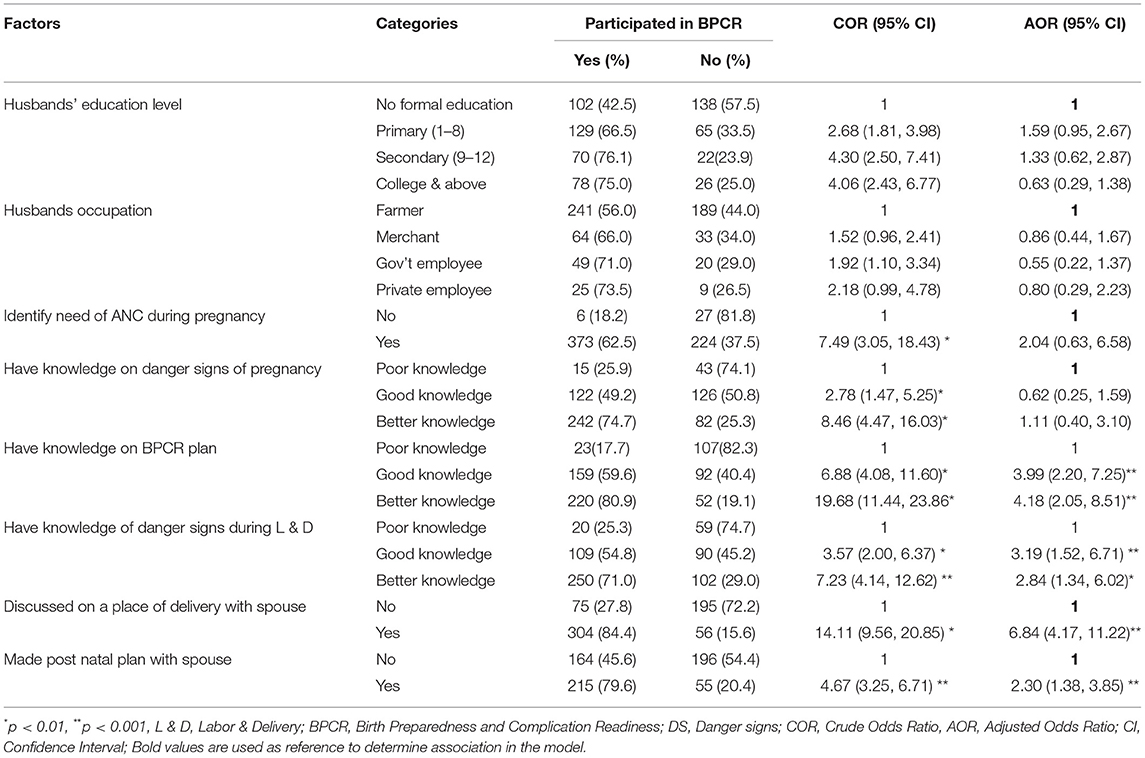
Table 4. Bi-variable and multivariable logistic regression analysis of factors associated with husband's participation in BPCR in Haramaya HDSS site, Eastern Ethiopia, 2020.
This study assessed the husband's plan to participate in birth preparedness and complication readiness and its associated factors in the Haramaya district HDSS site, Eastern Ethiopia. It revealed that the overall prevalence of husbands' plans to participate in BPCR was 59.6%. Thus, approximately two out of every five husbands failed to plan for BPCR. Husband's knowledge of BPCR, husband's knowledge status on danger signs during labor and delivery, having a discussion with spouse on the place of delivery and making postpartum plan were identified as predictors of husband's plan to participate in BPCR.
In this study, around 59.6% of husbands were intended to participate in BPCR during the current pregnancy. Similar findings were reported in a study conducted in the Tigrai region of Northern Ethiopia (60.4 %) (20) and Mekelle Town of Northern Ethiopia (60.9%) (31). The similarities could be due to the fact that the two studies use a similar strategy for safe motherhood and have a similar social structure. However, the current prevalence of husband's plan to participate in BPCR was much higher than previous studies conducted in different settings like Axum, Northern Ethiopia (46.6 %) (18), Bale, Southeast Ethiopia (41.6 %) (32), Nepal (44.36 %) (33), and secondary analysis of DHS data in selected African countries (45.7 %) (5). The possible justification for these disparities might be attributed to differences in sample size, methods of assessment, and the time gaps of the study period. Another possible explanation is that the current study population has better access to information on maternal health care. On contrary, this finding was relatively lower than studies conducted elsewhere such as Gulu district (65.4 %) (12), India (81%) (34), and Nepal (82.6 %) (35). The possible reasons could be due to a variety of socio-demographic factors in the current study setting such as a low level of educational status and socio-economic status of the study participants.
In the final model of multivariable analysis, the husband's knowledge of danger signs during labor and delivery was found to be associated with the husband's plan to participate in BPCR. Thus, those husbands who had a good and better knowledge of danger signs during labor and delivery were 3.19 and 2.84 times more likely to participate in the BPCR plan than those who had poor knowledge, respectively. These results are supported by findings from previous studies conducted in Ethiopia like Burayu (26), Jimma (36), Kofele (37), and other countries such as Nepal (35), and India (38). The possible justification is because knowing about danger signs encourages husbands to seek healthcare service and to participate in BPCR; as improving husbands' awareness and skills could make them involved more in their wives' health status. Moreover, having awareness about potential danger signs of pregnancy may help the husbands to accompany their wives to visit health facilities earlier (39). Moreover, men who are aware of the danger signs of pregnancy and childbirth may become gatekeepers, ensuring that their spouse receives appropriate care in pregnancy-related emergencies (15). Furthermore, when men can recognize danger signs, it makes it easier for women to access health care services, especially in emergencies (9, 12).
Furthermore, in this study, the husband's knowledge status of the birth plan was found to be an independent predictor of BPCR. Accordingly, those husbands with good and better knowledge of BPCRs were 4.18 times and 3.99 times more likely to participate in BPCR than those husbands with poor knowledge respectively. These findings are also supported by studies conducted in Burayu (26) and Nepal (40). This could be because knowing the process of birth preparedness and complication readiness enables husbands to participate in the issues that are beneficial to their spouses. Similarly, the husband's discussion status with their spouse was significantly associated with the husband's plan to participate in BPCR. Thus, those participants who discussed with their wives the place of delivery were 6.84 times more likely to participate in BPCR than those who did not involve in the discussion process. This is in harmony with the findings of the study conducted in Wolaita Sodo, Southern Ethiopia (23). The possible reasons that might be attributed to the household's joint decisions are more powerful because discussing with the husbands could have a positive impact on maternity care services.
Finally, the study pointed out that participants who had made a postpartum plan with their wife were 2.30 times more likely to participate in BPCR than those who had not made a plan. The findings are also in line with a study conducted in Wolaita Sodo, Southern Ethiopia (23), where a higher proportion of husbands who participated in the process of BPCR were observed in those husbands who had no postpartum plan. The possible explanation is that having no postpartum plan was a significant risk factor that endangered or led to the mother's death due to the first two delays in providing care, which is seeking care and reaching a health facility. As a result, preparing for delivery and postpartum care, as well as dealing with unexpected problems, as soon as possible can save the mother's life. Finally, it is very crucial to give more emphasis on BPCR as pregnancy-related complications continue to be a major cause of maternal deaths in Sub-Saharan Africa. Appropriate preparation for birth preparedness and complications readiness by women, male partners, families, and the community has the potential to lower these preventable risk factors. Moreover, policies, programs, and practices could focus on improving male partners' level of knowledge about complications related to pregnancy and childbirth, and the importance of preparing, and planning for childbirth (9, 14).
In this study, due to the nature of the study design, it would be impossible to determine the causal relationship between the variable and the outcome in the analysis. Moreover, as it only involves a participant from rural residences, conclusions for urban could be drawn.
According to this study, approximately two out of every five husbands failed to plan for BPCR. Husband participation in BPCR was significantly associated with knowledge of BPCR, knowledge of danger signs during labor and delivery, discussion status on the place of delivery, and making a postpartum plan. Therefore, all stakeholders should give more emphasis on male partners' education in terms of birth preparedness and complication readiness, as well as knowledge of danger signs during labor and delivery. It is also very crucial to encourage male partners to discuss a place of delivery and have a postpartum plan in place to reduce potential complications related to labor and delivery. Moreover, we also recommend further community-based longitudinal studies triangulated by qualitative methods to identify and explore predictors of a husband's involvement in BPCR.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by ethical approval was obtained from Institutional Health Research Ethics Review Committee (IHRERC) of Haramaya University, College of Health and Medical Sciences. The patients/participants provided their written informed consent to participate in this study.
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Haramaya University provided financial support for this study. However, the funding agency had no role in the collection, analysis, and interpretation of the data as well as the writing-up of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors are very thankful to Haramaya University, heads and staff of HDSS, the study participants, data collectors, and field supervisors.
1. WHO UNICEF UNFPA World Bank Group the United Nations Population Division. Trends in Maternal Mortality: 1990 to 2015. Sexual and reproductive Health (2015). Available online at: https://www.afro.who.int/sites/default/files/2017-05/trends-in-maternal-mortality-1990-to-2015.pdf
2. McPherson R, Khadka N, Moore J, Sharma M. Are Birth-preparedness Programmes Effective? Results From a Field Trial in Siraha District, Nepal. J Health Popul Nutr. (2007) 24:479–88.
3. JHPIEGO. Maternal and Neonatal Health (MNH) Program: Birth Preparedness and Complication Readiness: A Matrix of Shared Responsibility. Baltimore, MD: USAID (2001).
4. Chattopadhyay A. Men in maternal care: evidence from India. J Biosoc Sci. (2012) 44:129–53. doi: 10.1017/S0021932011000502
5. Ditekemena J, Koole O, Engmann C, Matendo R, Tshefu A, Ryder R, et al. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reprod Health. (2012) 9:32. doi: 10.1186/1742-4755-9-32
6. Ganle JK, Dery I. 'What men don't know can hurt women's health': a qualitative study of the barriers to and opportunities for men's involvement in maternal healthcare in Ghana. Reprod Health. (2015) 12:93. doi: 10.1186/s12978-015-0083-y
7. Iliyasu Z, Abubakar IS, Galadanci HS, Aliyu MH. Birth preparedness, complication readiness and fathers' participation in maternity care in a northern Nigerian community. (2010) 14:21–32.
8. August F, Pembe AB, Mpembeni R, Axemo P, Darj E. Men's Knowledge of Obstetric Danger Signs, Birth Preparedness and Complication Readiness in Rural Tanzania. PLoS ONE. (2015) 10:e0125978. doi: 10.1371/journal.pone.0125978
9. Kakaire O, Kaye DK, Osinde MO. Male involvement in birth preparedness and complication readiness for emergency obstetric referrals in rural Uganda. Reprod Health. (2011) 8:12. doi: 10.1186/1742-4755-8-12
10. Mullany B, Becker S, Hindin M. The Impact of Including Husbands in Antenatal Health Education Services on Maternal Health Practices in Urban Nepal: Results from a Randomized Controlled Trial. Health Educ Res. (2007) 22:166–76. doi: 10.1093/her/cyl060
11. Yargawa J, Leonardi-Bee J. Male involvement and maternal health outcomes: systematic review and meta-analysis. J Epidemiol Community Health. (2015) 69:604–12. doi: 10.1136/jech-2014-204784
12. Tweheyo R, Konde-Lule J, Tumwesigye NM, Sekandi JN. Male partner attendance of skilled antenatal care in peri-urban Gulu district, Northern Uganda. BMC Pregnancy Childbirth. (2010) 10:53. doi: 10.1186/1471-2393-10-53
13. Teklesilasie W, Deressa W. Barriers to husbands' involvement in maternal health care in Sidama zone, Southern Ethiopia: a qualitative study. BMC Pregnancy Childbirth. (2020) 20:1–8. doi: 10.1186/s12884-019-2697-5
14. Boltena MT, Kebede AS, El-Khatib Z, Asamoah BO, Boltena AT, Tyae H, et al. Male partners' participation in birth preparedness and complication readiness in low- and middle-income countries: a systematic review and meta-analysis. BMC Pregnancy Childbirth. (2021) 21:556. doi: 10.1186/s12884-021-03994-0
15. Alio AP, Lewis CA, Scarborough K, Harris K, Fiscella K. A community perspective on the role of fathers during pregnancy: a qualitative study. BMC Pregnancy Childbirth. (2013) 13:60. doi: 10.1186/1471-2393-13-60
16. Påfs J, Musafili A, Binder-Finnema P, Klingberg-Allvin M, Rulisa S, Essén B. 'They would never receive you without a husband': Paradoxical barriers to antenatal care scale-up in Rwanda. Midwifery. (2015) 31:1149–56. doi: 10.1016/j.midw.2015.09.010
17. Singh D, Lample M, Earnest J. The involvement of men in maternal health care: cross-sectional, pilot case studies from Maligita and Kibibi, Uganda. Reprod Health. (2014) 11:68. doi: 10.1186/1742-4755-11-68
18. Baraki Z, Wendem F, Gerensea H, Teklay H. Husbands involvement in birth preparedness and complication readiness in Axum town, Tigray region, Ethiopia, 2017. BMC Pregnancy Childbirth. (2019) 19:180. doi: 10.1186/s12884-019-2338-z
19. CSA-Ethiopia I.C.F. International. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. New York, NY: CSA and ICF (2016). p. 59.
20. Gebrehiwot H, Gebregziabher W, Gidey G. Assessment of husbands' participation on birth preparedness and complication readiness in Enderta Woreda, Tigray region, Ethiopia, 2012. J Women's Health Care. (2013) 3:2167–420.
21. Bhusa CK BS. Social Factors Associated with Involvement of Husband in Birth Preparedness Plan and Complication Readiness in Dang District. Nepal J Commun Med Health Educ. (2018) 8:636. doi: 10.4172/2161-0711.1000636
22. Iliyasu Z, Abubakar IS, Galadanci HS, Aliyu MH. Birth preparedness, complication readiness and fathers' participation in maternity care in a northern Nigerian community. Afr J Reprod Health. (2010) 14:21–32.
23. Tadesse M, Boltena AT, Asamoah BO. Husbands' participation in birth preparedness and complication readiness and associated factors in Wolaita Sodo town, Southern Ethiopia. Afr J Prim Health Care Fam Med. (2018) 10:e1–8. doi: 10.4102/phcfm.v10i1.1471
24. Narang H, Singhal S. Men as partners in maternal health: an analysis of male awareness and attitude. Int J Reprod Contrac Obst Gynecol. (2013) 2:388–93. doi: 10.5455/2320-1770.ijrcog20130925
25. August F, Pembe AB, Kayombo E, Mbekenga C, Axemo P, Darj E. Birth preparedness and complication readiness–a qualitative study among community members in rural Tanzania. Glob Health Action. (2015) 8:26922. doi: 10.3402/gha.v8.26922
26. Gize A, Eyassu A, Nigatu B, Eshete M, Wendwessen N. Men's knowledge and involvement on obstetric danger signs, birth preparedness and complication readiness in Burayu town, Oromia region, Ethiopia. BMC Pregnancy Childbirth. (2019) 19:515. doi: 10.1186/s12884-019-2661-4
27. CSA. Population Projection of Ethiopia for All Regions at Wereda Level from 2014–2017. Addis Ababa: CSA (2013). p. 58.
29. Wai KM, Shibanuma A, Oo NN, Fillman TJ, Saw YM, Jimba M. Are Husbands Involving in Their Spouses' Utilization of Maternal Care Services?: A Cross-Sectional Study in Yangon, Myanmar. PLoS ONE. (2015) 10:e0144135. doi: 10.1371/journal.pone.0144135
30. Del Barco RC. Monitoring Birth Preparedness and Complication Readiness. Tools and Indicators for Maternal and Newborn Health 2004. Baltimore, MD: JHPIEGO (2004). p. 330.
31. Haftom Gebrehiwot Weldearegay. Determinant Factors of Male Involvement in Birth Preparedness and Complication Readiness at Mekelle Town; a community Based Study. Sci J Public Health. (2015) 3:175. doi: 10.11648/j.sjph.20150302.14
32. Kassahun F, Worku C, Nigussie A. Ganfurie G. Prevalence of male attendance and associated factors at their partners antenatal visits among antenatal care attendees in Bale Zone, South East Ethiopia. Int J Nurs. Midwifery. (2018) 10:109–20. doi: 10.5897/IJNM2018.0323
33. Bhusal CK, Bhattarai S. Social factors associated with involvement of husband in birth preparedness plan and complication readiness in Dang District, Nepal. J Commun Med Health Educ. (2019) 08.
34. Singh A, Ram F. Men's involvement during pregnancy and childbirth: Evidence from rural ahmadnagar. Populat Rev. (2009) 48. Available online at: https://muse.jhu.edu/article/264738/pdf
35. Dutta M, Kapilashrami M, Tiwari V. Knowledge, Awareness And Extent Of Male Participation In Key Areas Of Reproductive And Child Health In An Urban Slum Of Delhi. Perspectives and Issues. Health Popul.(2014)27:49–66.
36. Debelew GT, Afework MF, Yalew AW. Factors affecting birth preparedness and complication readiness in Jimma Zone, Southwest Ethiopia: A multilevel analysis. Pan Afr Med J. (2014) 19:272. doi: 10.11604/pamj.2014.19.272.4244
37. Tafa A, Dejene H, Ebrahim J, Gebrie M, Wakgari N. Birth preparedness and complication readiness plan among antenatal care attendants in Kofale district, South East Ethiopia: a cross sectional survey. Divers Equal Health Care. (2018) 15:23–9. doi: 10.21767/2049-5471.1000152
38. Jungari S, Paswan B. What he knows about her and how it affects her? Husband's knowledge of pregnancy complications and maternal health care utilization among tribal population in Maharashtra, India. BMC Pregnancy Childbirth. (2019) 19:1–12. doi: 10.1186/s12884-019-2214-x
39. Thapa DK, Niehof A. Women's autonomy and husbands' involvement in maternal health care in Nepal. Soc Sci Med. (2013) 93:1–10. doi: 10.1016/j.socscimed.2013.06.003
Keywords: husband participation, birth preparedness, complication readiness, associated factor, Ethiopia
Citation: Sufian S, Kure MA, Dheresa M, Debella A, Balis B and Roba KT (2022) Husbands' Plan to Participate in Birth Preparedness and Complication Readiness in Haramaya Health and Demographic Surveillance System Site, Eastern Ethiopia: A Community-Based Cross-Sectional Study. Front. Public Health 10:856809. doi: 10.3389/fpubh.2022.856809
Received: 17 January 2022; Accepted: 21 March 2022;
Published: 18 April 2022.
Edited by:
Rosnah Sutan, National University of Malaysia, MalaysiaReviewed by:
Ranjit Kumar Dehury, University of Hyderabad, IndiaCopyright © 2022 Sufian, Kure, Dheresa, Debella, Balis and Roba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adera Debella, YWtzYW5hZGVyYTYyQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.