- 1Medical College, Xijing University, Xi'an, China
- 2Department of Psychiatry, Wuhan Fourth Hospital, Puai Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 3Research Center for Psychiatric Diseases, Tehran University of Medical Sciences, Tehran, Iran
During the pre-operation period, surgical candidates experience situations that stimulate psychological anxiety leading to stress during and after surgery which is known as preoperative anxiety. This condition can cause psychological and physiological adverse effects on both children and adults. Due to the high prevalence and adverse effects of preoperative anxiety, different treatments have been evaluated including pharmacological and non-pharmacological approaches. As pharmacological treatments may cause adverse effects such as breathing problems, drowsiness, interfering with anesthetic drugs, and prolonged recovery, non-pharmacological interventions are becoming more popular. These methods include cognitive-behavioral therapy, music therapy, pre-op preparation video, aromatherapy, hypnosis, guided imagery relaxation therapy, and massage. In this study, the most popular non-pharmacological approaches to preoperative anxiety are reviewed focusing on more recent evidence provided by clinical studies. The reviewed clinical evidence on the mentioned methods shows the efficacy of non-pharmacological interventions for the treatment of preoperative anxiety, so they can be used in patients of different ages and types of disease and surgery.
Introduction
Anxiety is defined as an unpleasant sense associated with fear, tension, and nervousness (1). Surgery as a major trauma can cause anxiety. During the period of pre-operation, surgical candidates experience situations that stimulate psychological anxiety leading to stress during and after surgery. The anxiety secondary to disease, hospitalization, and planned surgery is called preoperative anxiety (2, 3). The most common cause of preoperative anxiety is waiting for surgery, concern about the operation results, separation from family, postoperative pain anticipation, loss of independence, and fear of surgery and death (4).
The prevalence of preoperative anxiety varies widely and it has been reported to range from 40 to 60%among young children patients and 11–80% among adult ones (4–6). In a study, 23.99% of patients experienced severe preoperative anxiety (4). Different causes are proposed for preoperative anxiety such as the fear of the unknown, fear of being sick, and fear of death (7). Various factors are associated with preoperative anxiety. These factors are classified as sociodemographic factors, psychosocial variables, and surgery and anesthesia-related factors such as previous surgical experience, having information about the surgical process, and anesthesia (4, 7). Age is a protective factor of preoperative anxiety as each 1 year increase in age reduces five percent of the chance of preoperative anxiety. Females are at higher risk and levels of anxiety than men and educated persons experience higher levels of anxiety (8). Married patients have greater emotional supports so they experience lower anxiety levels (9). The significance of the surgery is associated with anxiety as higher levels of anxiety are reported in patients who had a greater surgical procedure (10). History of cancer is an important risk factor for preoperative anxiety (4). Previous psychiatric diseases, such as depression and anxiety may influence the extent of preoperative anxiety (11, 12).
Preoperative anxiety can cause psychological and physiological adverse effects on both children and adults. Also, it can interfere with the process of surgery and can put patients in danger during the surgical process (13). Maladaptive behaviors, emergence delirium, and preoperative anxiety are common among children undergoing surgery and these phenomena are related as maladaptive behavioral responses like sleep and eating disturbances and enuresis are common adverse events among children with preoperative anxiety (6, 14–16). A 10 point increase in the state anxiety scores in children may result in a 12.5% increase in the probability of the new-onset maladaptive behavior happening after the operation (16).
The increased need for postoperative analgesics, prolonged hospital stay, and recovery are common among adults (17, 18). Besides, it can trigger autonomic and endocrine systems which cause hemodynamic instability (19). Moreover, severe preoperative anxiety is associated with impaired wound healing and postoperative complications like nausea, vomiting, and pain (20–22). There is a significant inverse relationship between anxiety and recovery and effectiveness of anesthesia (23).
Preoperative anxiety is a matter of concern for many health professionals including anesthesiologists and surgeons, and nurses at the recovery unit, ICU, and ward. It is considered a major morbidity factor during and after the surgical process (24, 25). It is also known as a financial burden on the healthcare system (26). The mentioned costs are considered to be attributed to the prolonged recovery and hospital stay and increased need for anesthetic and analgesic drugs (27).
Due to the high prevalence and adverse effects of preoperative anxiety, treatment is necessary. Till now, two types of interventions for preoperative anxiety are identified pharmacological and non-pharmacological. Pharmacological interventions include sedatives and anti-anxiety drugs. Midazolam, diazepam, ketamine, and fentanyl are the most common anxiolytics (28). As pharmacological treatments have adverse effects such as breathing problems, drowsiness, interfering with anesthetic drugs, and prolonged recovery, non-pharmacological interventions are becoming more commonly used. It is reported that non-pharmacological interventions are more commonly used by anesthesiologists compared to pharmacologic ones in both pediatric and adult anesthesia procedures. For example, in a survey from Korean anesthesiologists, 46.3% preferred non-pharmacological interventions compared to 39.0% preferring medications and 14.6% of no preference for pediatric anesthesia (29). In another report from the UK 95% of anesthesiologists reported the use of communication with the patient and reassurance as their most popular method to reduce preoperative anxiety in the adult population (30).
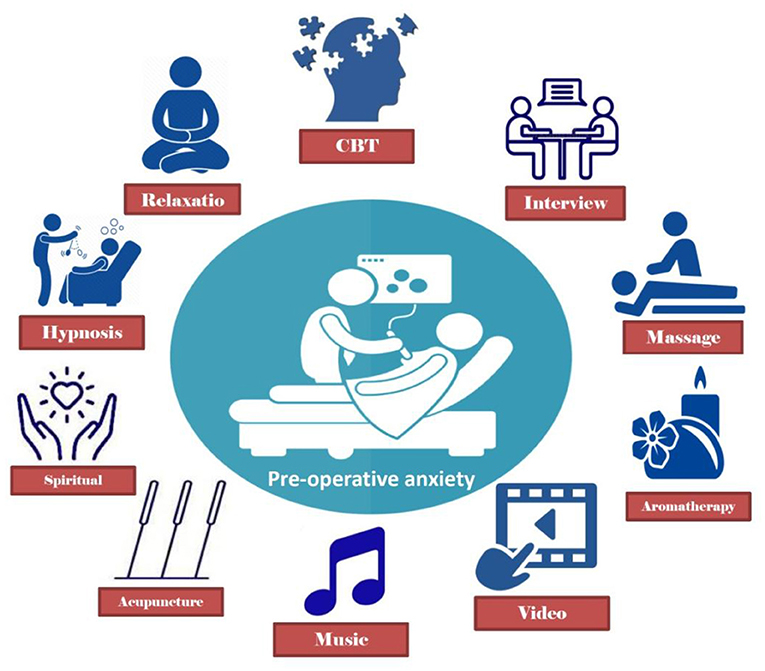
Non-pharmacological interventions include, but are not limited to, interviews with patients performed by healthcare providers, communicating strategies, religious or spiritual activity, music, visits from relatives, acupuncture, various distraction, and patient education (Figure 1) (31–44). Various clinical studies are conducted to evaluate the efficacy of these non-pharmacological interventions (Table 1). In this study, the most popular non-pharmacological approaches to preoperative anxiety are reviewed focusing on more recent evidence provided by clinical studies.
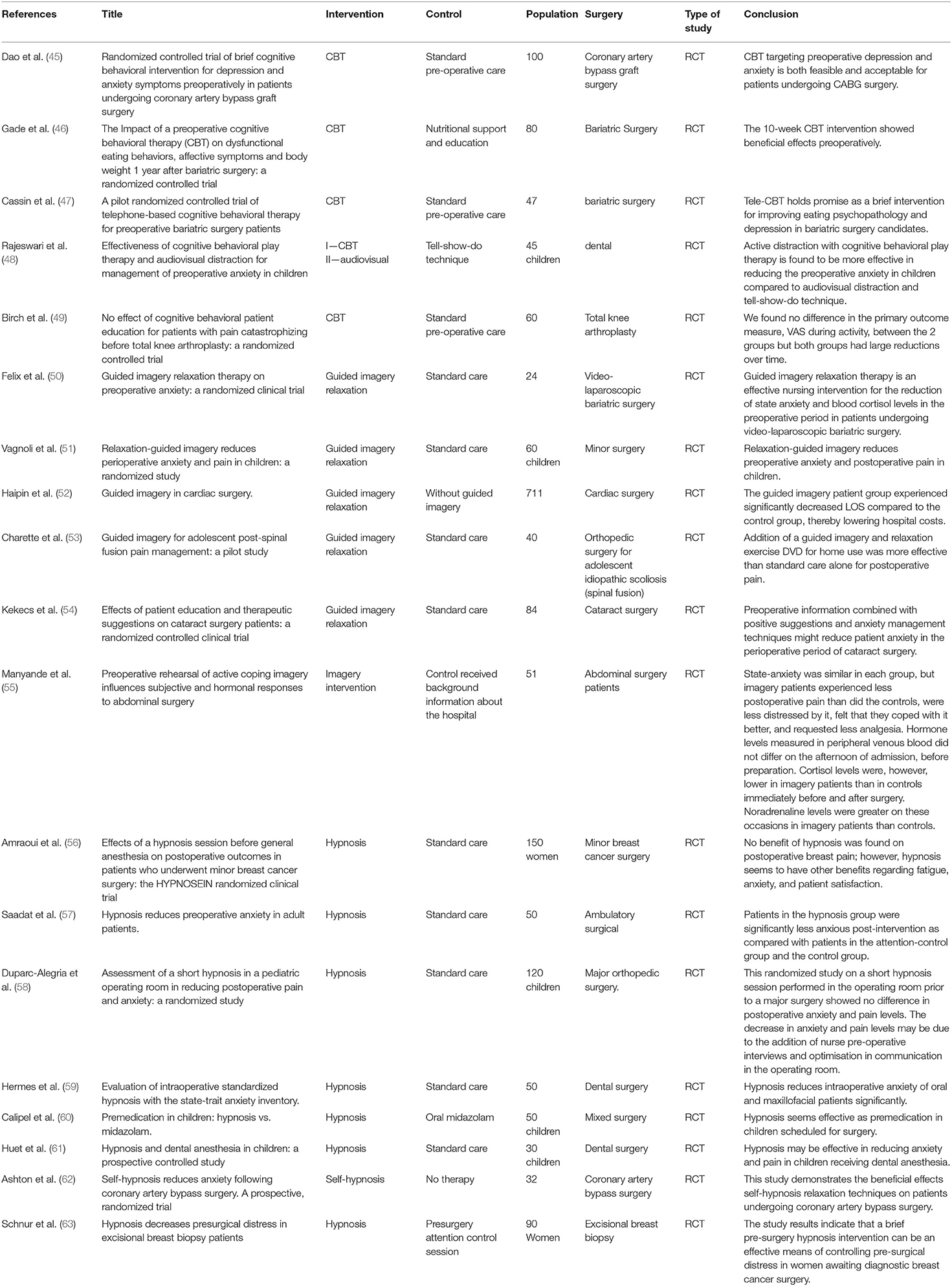
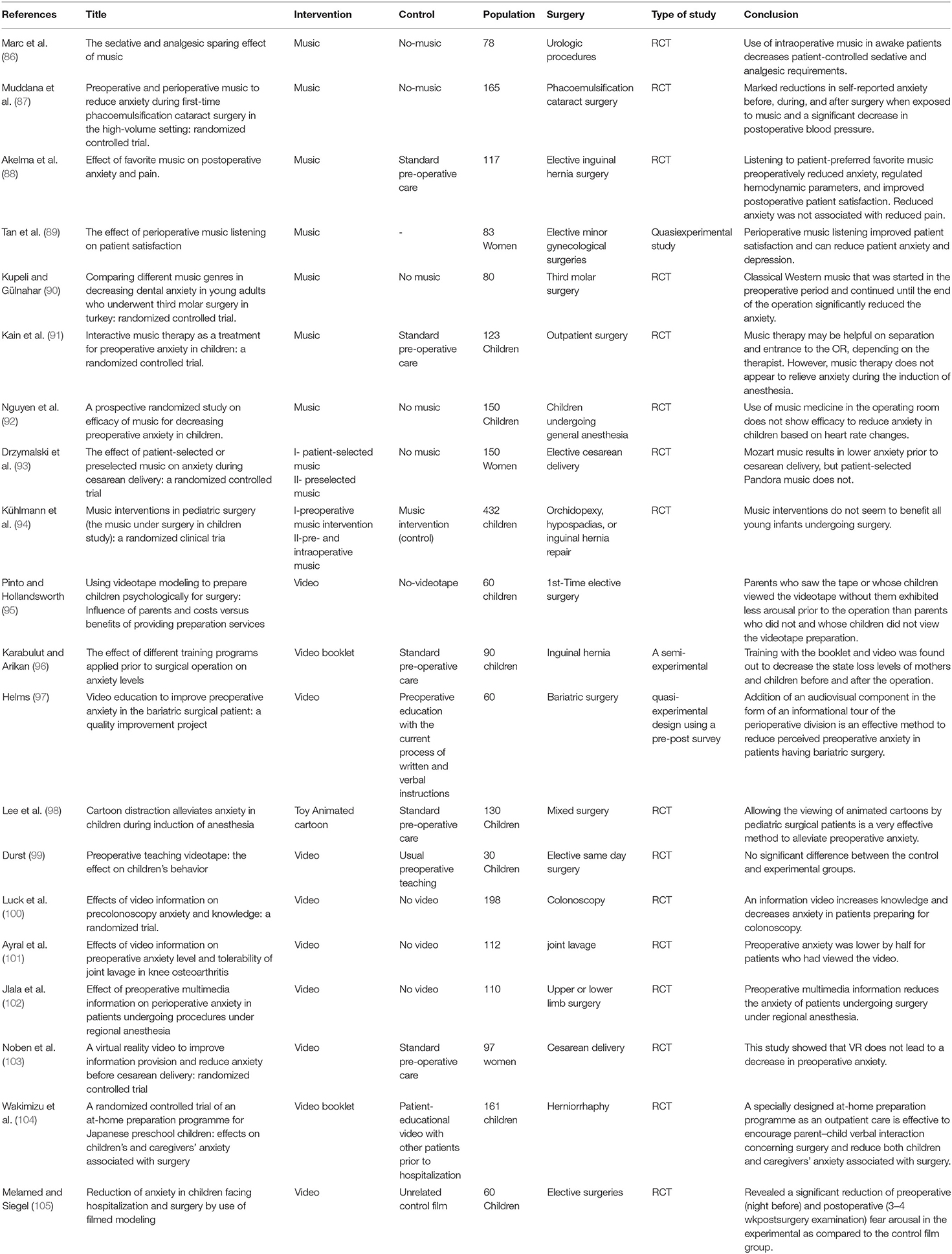
Table 1. Clinical studies on cognitive behavioral therapy (CBT), guided imagery relaxation and hypnosis in preoperative anxiety.
Methods
This study was performed as a narrative literature review, aimed to comprehensively gather and summarize the available information in the scientific literature on the non-pharmacologic treatments for preoperative anxiety. The databases of PubMed, Scopus, and web of knowledge, as well as google scholar search engine, were searched for the relevant articles. The searching terms included “preoperative anxiety,” “treatment,” and “trial” from inception to 2020. All studies reported outcomes for non-pharmacologic treatments are reviewed. This study reviewed the latest clinical trials of 10 types of non-pharmacological interventions. The used key terms of treatments, interventions, approaches, and therapy used as synonyms through the text and means the mentioned 10 types of non-pharmacological l interventions aiming the reduction of preoperative anxiety. We will review the clinical evidence about the interview, conversation and communication strategies, cognitive-behavioral therapy, spiritual/religious interventions, music therapy, pre-operation preparation video, aromatherapy, massage, meditation, and guided imagery relaxation therapy, hypnosis, and acupuncture in the treatment of the preoperative anxiety. Animal, and in-vitro studies as well as clinical studies on drug therapy for preoperative anxiety were excluded. Two reviewers, independently, checked the studies for eligibility and extracted data from each study. For each study type of non-pharmacologic intervention, type of intervention in control group, sample size, population, type of surgery, and results were extracted. After that, we have discussed the availability, limitations, acceptability, needed education and equipment, acceptability and popularity of these interventions.
Interview, Conversation, and Communication Strategies
Interview and communication strategies are considered the most common strategy used by anesthesiologists for controlling preoperative anxiety in some studies (30). Different studies have evaluated the efficacy of these strategies in reducing preoperative anxiety. A report evaluating 230 patients undergoing breast and abdominal surgeries by State-Trait Anxiety Inventory (STAI) regarding their preoperative anxiety showed that surgeon communication with the patients and their communication abilities was associated with reduced anxiety scale (64). They have used predefined question prompt lists for the consultation session held 1-3 weeks before the surgical schedule. Another study on a structured communication between patients and anesthesiologists showed reduced anxiety and fear of anesthesia, particularly in younger patients compared to standard interview techniques (65). Notably, the structured interview had a significantly shorter duration compared to the routine sessions. Evidence also supports the positive effect of preoperative patient-doctor communication on pre-operative anxiety (66, 67).
Cognitive-Behavioral Therapy
Cognitive Behavioral Therapy (CBT) is defined as science-based behavioral and cognitive interventions. Behavioral interventions aim to increase adaptive behaviors and decrease maladaptive ones. Cognitive interventions change abnormal beliefs, self-statements, and cognitions. CBT is the gold standard psychotherapeutic treatment of anxiety disorders (68–71). Exposure and cognitive therapy are the most commonly used CBT methods. Imaginal, in vivo (in real life), and interoceptive are three forms of exposure. Cognitive therapy is based on changing the distorted thoughts by using some techniques such as recognizing inaccurate thinking, controlling automatic thoughts, and changing abnormal thoughts (72).
Catastrophizing (such as magnification, rumination, and helplessness), anxiety, and depression are associated with increased postoperative pain (73). Proper evaluation and identifications of these factors in the patient in the perioperative period may help reduce anxiety and promote recovery (74). For example, the modified Yale Preoperative Anxiety Scale (mYPAS) and State-Trait Anxiety Inventory for Children (STAIC) is reported as a significant predictor of anxiety in children (75).
Perioperative Pain Self-management (PePS) intervention based on principles of CBT is a feasible intervention for preventing chronic pain and long-term opioid use (76). A brief Managing Anxiety and Depression using Education and Skills (MADES) intervention (a type of CBT) before coronary artery bypass graft surgery had several beneficial effects in the intervention group compared to usual treatment in control (45). This CBT improved depression and anxiety symptoms and quality of life (45). Moreover, it reduces the length of hospital stay (45) (Table 1).
A randomized controlled trial showed that a 10 week CBT intervention before bariatric surgery, significantly reduced the pre-operative anxiety and depression symptoms (46). Moreover, telephone-based cognitive behavioral therapy (Tele-CBT) improved depression and psychopathology of eating in candidates of bariatric surgery (47). To reduce preoperative anxiety in children, active distraction with cognitive-behavioral play therapy is more effective than the tell-show-do technique, and audiovisual distraction (48). The CBT-based pain education was not more effective than usual care after total knee arthroplasty in reducing pain and improving physical activity (49).
Spiritual/Religious Interventions
Multiple studies have evaluated the association between religiousness and anxiety with different results in varying communities and cultures (77–79). It is shown that religiousness may be negatively correlated with the level of preoperative anxiety (36, 80). It is also shown that preoperative spiritual/religious training can reduce anxiety in Muslim patients undergoing coronary artery bypass grafting (81). The intervention consists of 5 sessions of 45–60 min in 5 consecutive days presenting relevant Islamic supplication (Zikr) and the holy Quran verses based on Richards and Bergin's (2000) spiritual therapy technique.
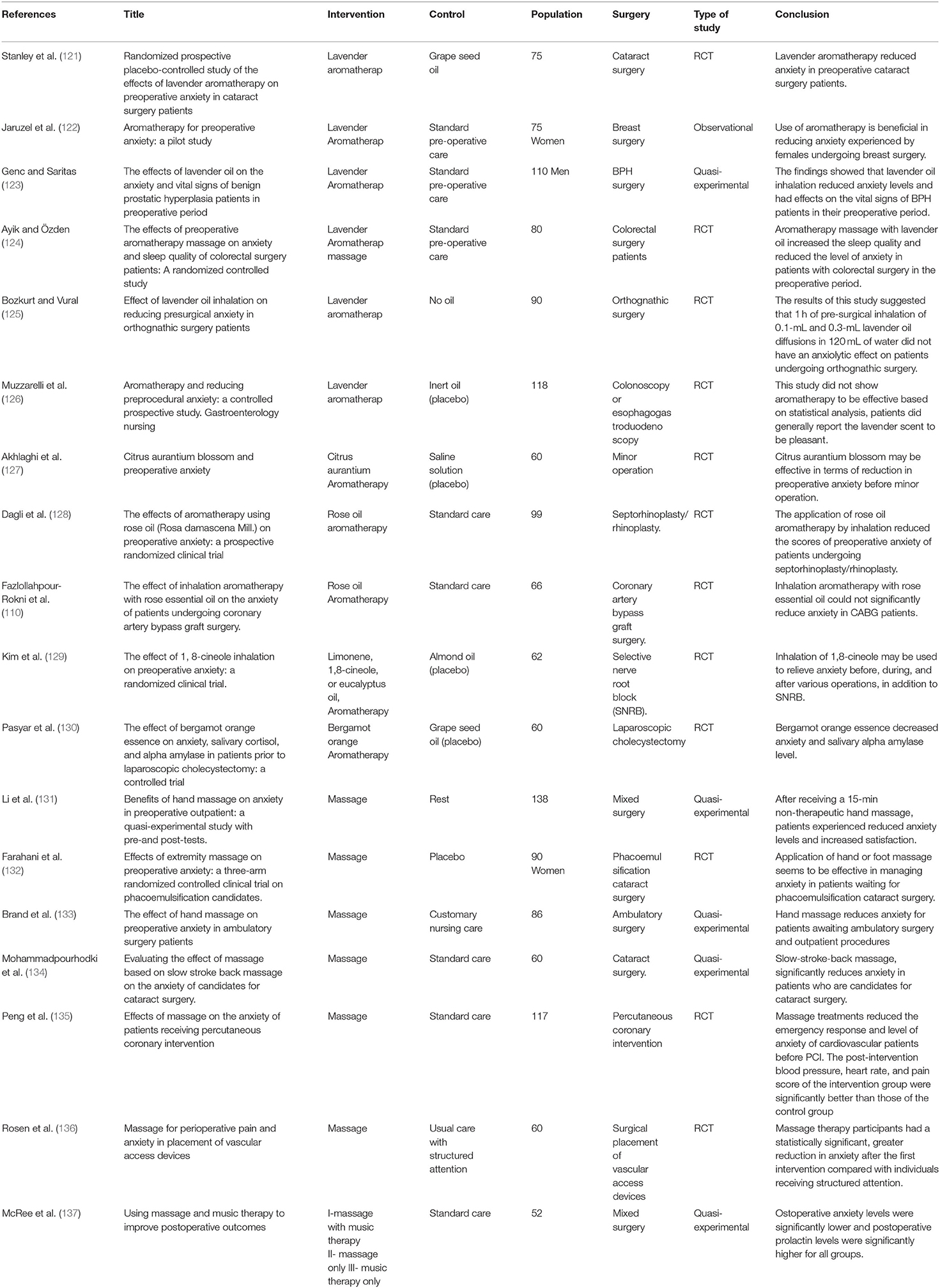
Music Therapy
Music listening triggers the parasympathetic nervous system and reduces sympathetic nervous activity (82). These changes reduce anxiety and help patients to become more relaxed emotionally and physically (82). Moreover, music can distract patients from pain and anxiety (83). Headphones also mask the environmental annoying noises. Heart rate, blood pressure, and respiratory rate may be regulated by listening to music (41, 84). Music is a cheap, safe, non-invasive, and effective non-pharmacological intervention (85). Also, music can reduce the doses of required anesthesia as two clinical trials showed that in patients who listened to favorite music lower doses of propofol (for sedation) and alfentanil were used compared to the control group (86). Music exposure in the preoperative period reduced self-reported anxiety before, during, and after cataract surgery (87). In addition, systolic blood pressure after surgery was significantly lower in patients who had music exposure before cataract surgery than patients of the control group (87). Listening to the favorite music preoperatively before elective inguinal hernia surgery reduced postoperative State-Trait Anxiety Inventory form 1 (STAI-1) score and improved postoperative patient satisfaction in the music group compared to the control group. Although preoperative STAI-1, STAI-2 scores and numeric rating scale (NRS) were similar between the groups (88). The median of the Hospital Anxiety and Depression Scale (HADS) reduced significantly from 7 to 2 after using the music in women who were undergoing elective minor gynecological surgeries (89).
A clinical trial study compared the efficacy of three genres of music on dental surgery anxiety and concluded that classical Western music significantly was effective compared to Turkish music and soft rock music (90) (Table 2). In a randomized clinical trial, outpatient surgery children were randomized into three groups; music, midazolam, and control. Music therapy didn't relieve anxiety during anesthesia induction (91).
A prospective randomized study showed no efficacy of music used in reducing the preoperative anxiety of children based on heart rate changes (92). Although preselected music caused a reduction of anxiety before cesarean delivery and postoperative pain, the patient-selected one did not. Total satisfaction scores of patients and postoperative anxiety were not different among the music and control groups (93). Among young infants, preoperative and intraoperative music interventions were not effective on preoperative anxiety based on the COMFORT-Behavior scale and physiological measurements such as blood pressure and heart rate (94).
Pre-Operation Preparation Video
Audiovisual (AV) programs can reduce anxiety and improve coping skills and patients' knowledge (106). Besides, they are used as active (e.g., Interactive games) and passive (e.g., preoperative preparation videos) distraction tools (107). Computers and other technologies (such as video glasses and smartphone applications) are used in this intervention (108, 109). The mechanism of this intervention is based on the interaction between situational anxiety, information retention, and memory (100). The most common type of AV interventions is preoperative (pre-op) preparation videos (99).
Compared with the control group, preoperative anxiety was lower among children who watched peer-modeling pre-op preparation videotape 1 hbefore admission (95) (Table 2). Using 12-min pre-op Video Compact Disc training 48 h before surgery was more effective than pre-op booklet training in children who planned to undergo inguinal hernia surgery (96). Among patients of bariatric surgery, adding audiovisual (film) preoperative information to traditional instructions reduced preoperative anxiety (97).
Watching favorite animated cartoons before anesthesia induction had the lowest modified Yale Preoperative Anxiety Scale (mYPAS) compared with playing with toy and control group in children (98). In contrast, a study showed no significant difference in behaviors related to anxiety between peer-modeling of a pre-op preparation video watching and preoperative teaching (99). Among patients of colonoscopy control and intervention groups were randomly selected. Watching informative videos before colonoscopy significantly reduced anxiety based on Spielberger state anxiety inventory (STAI) in the intervention group before the colonoscopy (100). A clinical trial study among knee osteoarthritis patients reported that patients who watched video information before joint lavage had a lower level of preoperative anxiety and more tolerability (101). In a study, 110 patients of upper and lower limb surgery by regional anesthesia were randomized into study and control groups. Patients in the study group received preoperative multimedia information and they were less anxious than the control group (102). A randomized controlled trial among women who were a candidate for elective cesarean delivery reported that virtual reality information Video did not reduce preoperative anxiety compared to standard preoperative information techniques (103).
Moreover, the efficacy of the combination of video watching with other interventions is evaluated. Using peer-modeling pre-op preparation video combined with an information booklet (104) and watching a generic film (105) was significantly more effective than using video alone.
Aromatherapy
Some essential oils which are concentrated essences extracted from aromatic plants may have a physiological or pharmacological effect. They can be used via different modes like massage, inhalation, skin absorption, ingestion, and bath (110, 111). Pain control is among the most common indication of essential oils (112). The therapeutic use of these oils is called aromatherapy which is known as a modality of complementary and alternate therapy (113–115). Aromatherapy has been used for thousands of years ago in Egypt and India (111).
Till now, more than 40 types of plant extracts are used for aromatherapy. Lavender oil, rose oil, and citrus species oils are the most commonly used (116–118). Around the world, Aromatherapy is used broadly by nurses as complementary and alternative medicines because it is applied easily and does not need any licensed experts, equipment, and patient involvement (119). Aromatherapy is used for symptom therapy of preoperative anxiety, nausea, vomiting, critical care, wellbeing, anxiety, depression, stress, insomnia, pain, dementia, and oncology in inpatient and outpatient settings (120).
A single-center prospective randomized placebo-controlled trial reported that lavender reduced preoperative anxiety among cataract surgery patients (121) (Table 3). In a study of 30 women undergoing breast surgery a significant reduction of preoperative anxiety was recorded after using a sustained-release lavender oil aromatherapy skin patch (122). Using the inhaled lavender oil in elderly men scheduled for benign prostate hyperplasia (BPH) surgery showed a significant decrease in anxiety and respiration and an increase of oxygen saturation compared to the control group (123). Massage with 5% lavender oil quality in patients with colorectal surgery reduced the anxiety level and increased sleep quality in the preoperative period (124). On the other hand, preoperative inhalation of lavender oil (0.1-mL and 0.3-mL diffused in 120 mL of water) did not have an anxiolytic effect among orthognathic surgery (bilateral sagittal split, Le Fort I, and bimaxillary osteotomies) candidate (125). Moreover, another controlled prospective study in patients who were scheduled for colonoscopy or esophagogastroduodenoscopy showed no beneficial effect of lavender use on preoperative anxiety although that was pleasant to patients (126). Oral use of Citrus aurantium blossom reduced preoperative anxiety in minor operation candidates compared to the control group (127).
Inhalation of rose oil before septorhinoplasty/rhinoplasty surgeries was effective in decreasing preoperative anxiety in a prospective randomized clinical trial (128). In contrast, a single-blind randomized clinical trial showed that inhalation of three drops of 4% rose essential oil for 10 min in one night and 1 h before coronary artery bypass graft (CABG) was not significantly effective in reducing preoperative anxiety (110). Inhalation of 1,8-Cineole (the major component of eucalyptus) in a randomized controlled trial Performed in 62 patients before selective nerve root block (SNRB) showed the efficacy of this type of aromatherapy in anxiety reduction (129). A pre-post-designed clinical study performed on candidates for cholecystectomy showed that bergamot orange essence can help in decreasing anxiety (130).
Massage
Touching and manipulation of soft tissue for therapeutic goals are named massage (138). It has been used as a therapeutic intervention since thousands of years ago especially in china (139). Hand massage as a non-pharmacological, simple, cheap, and non-invasive nursing intervention can significantly reduce preoperative pain, anxiety, and stress. In addition, it can improve positive feelings like relaxation, calmness, and satisfaction (133, 140–142). No side effects are reported about massage (143). Various mechanisms for the therapeutic effect of massage are explained theoretically. Massage reduces pain by muscle relaxation and enkephalins release (139, 144). The powerful stimulus of massage is conducted faster than pain along nerve pathways to the brain so massage can block pain conduction at the peripheral points (gaits of pain) and relieve pain (139, 145). Another mechanism explains that massage can increase the circulation of soft tissue so irritant substances including lactic acid and inflammatory substances are removed from the tissue. Besides, massage reduces pain sensation by inducing a sense of wellbeing (146).
A pre-and post-test quasi-experimental study (without a control group) reported that one session of 15-min hand massage help in reducing preoperative anxiety levels and increasing satisfaction (Table 3) (131). The massage was provided by Caring Hands massage volunteers from the 7 days Mayo Clinic Volunteer Program (131). A three-arm randomized study compared the efficacy of hand and foot massage with placebo and reported that a one session 5-min massage before cataract surgery significantly reduced anxiety and no significant differences were seen between hand and foot massage based on visual analog scale and physiological indicators (132). The massage was provided by a qualified nursing assistant, who had successfullycompleteda 12-h a workshop on therapeutic applications of classic massage 10 min before the surgery (132). Hand massage also reduced anxiety among patients in the ambulatory surgery setting (133). Slow stroke back massage for 15 min 30 min before surgery significantly reduced anxiety in cataract surgery candidates (134). Massage intervention for 20 min in one session for cardiovascular patients before percutaneous coronary intervention (PCI) reduced anxiety level and emergency response. Moreover, blood pressure, pain score, and heart rate after the operation were lower in comparison to the control group (135). A randomized, controlled trial (RCT) compared massage therapy with usual cares by using the State-Trait Anxiety Inventory (STAI) and 11-point numerical rating scale (0 = no pain to 10 = worst possible pain) among patients with cancer who were scheduled for surgical insertion of the vascular access device and concluded that a 20-min massage therapy before and after operation significantly reduced anxiety (136). A study evaluated the effect of music and massage among three intervention groups and one control group. In one group, patients had one session of 30 min of massage therapy and 30 min of music listening before the operation. In the second group, patients had 30 min of music listening and patients of the third group had 30 min of massage before the operation. Standard care was done for patients in the control group. Then the hemodynamic status (blood pressure and pulse rate), level of serum cortisol, and prolactin and anxiety level (by using STAI-6) were measured. This study showed that preoperative anxiety scores, preoperative and post-operative cortisol levels, and blood pressure were not significantly different among the 4 groups but postoperative anxiety scores were lower in intervention groups compared with the control group. Moreover, the combination of music and massage more effective than using massage or music alone in reducing postoperative anxiety (137).
Massage for pre-operative anxiety needs some equipment like a specific bed and trained personnel. Patients with pain and tenderness in massage site, severely immunocompromised state, pregnancy, bleeding disorder, dermatologic problems, allergy/sensitivity to gloves or massage oil, acute coronary syndrome, neuropathy, or delirium are not suitable candidates for this technique and are excluded in many studies. Another important point about the studies on this technique is that blinding the participant is not possible due to the nature of the intervention.
Meditation and Guided Imagery Relaxation Therapy
Guided imagery relaxation therapy is a relaxing technique based on the interaction between the brain, mind, body, and behavior. Relaxation means being free from physiological and psychological tension. In this technique, the patient changes negative or stressful feelings by focusing on pleasing images (147). Images can be visual, auditory, tactile, and motor forms (148).
A randomized, triple-blind clinical trial which was done to evaluate the effect of Guided imagery relaxation therapy on preoperative anxiety reported that this intervention significantly reduced anxiety among video-laparoscopic bariatric surgery candidates (50). A randomized study investigated the effect of Guided imagery relaxation therapy in reducing preoperative anxiety and postoperative pain among children and reported that Guided imagery relaxation therapy (Table 1).
Significantly reduced postoperative pain and preoperative anxiety in children (51). Among patients of cardiac surgery, guided imagery relaxation therapy reduced the pain, length of hospital stay, and anxiety (52). A study was conducted among patients of spinal fusion surgery and compared intervention (using a DVD with information and guided imagery/relaxation practices) with the control group. Lower post-operative pain intensity was reported among the intervention group but coping strategies (eating, sleeping, and walking) and State-trait anxiety were not significantly different (53). A randomized controlled clinical trial study concluded that a combination of preoperative information with techniques of anxiety management and positive suggestions reduced perioperative anxiety in cataract surgery patients (54). A study compared 26 imagery patients with 25 controls and reported that by using imagery relaxing therapy, cortisol level was reduced but noradrenaline levels were higher than controls, and the level of State-anxiety was similar in both groups (55). Another report on 100 patients undergoing cataract surgery receiving mediation showed reduced preoperative anxiety measured by the Amsterdam Preoperative Anxiety and Information Scale compared to the control group (149).
Hypnosis
Since many years ago, hypnosis has been used in surgical processes to reduce the amount of administered analgesics (150). Hypnosis is a modified state of consciousness that is different from normal consciousness and sleep stages.
In hypnosis patients are put in induction of a trance state so acceptable suggestions are delivered to patients. Hypnosis helps patients to improve their performance, perceptual, sensory, and memory abilities (151). The therapeutic effect of hypnosis is based on perception and attention alterations. Hypnotherapists achieve clinical goals such as anxiety, pain, and nausea reduction by distracting attention and modifying perception in patients (152–154). Hypnosis consists of three phases, first phase is induction that helps the patients to be relaxed. In the second phase suggestions (symptom therapies) are delivered to patients. In the third phase, the patient is backed to a normal consciousness state (155). Hypnosis is considered as an adjunctive or primary intervention and is used for managing anxiety, acute or chronic pain especially in children (156–158).
In a trial study consisting of 3 groups, the control, hypnosis, and attention control groups were compared and it was reported that post-intervention anxiety was significantly lower in the hypnosis group (57) (Table 1). A clinical trial was conducted among 150 women who underwent minor breast surgery and reported that hypnosis reduced postoperative anxiety and fatigue score compared to the control group but the level of post-operative breast pain was not significantly different among them (56). A randomized trial in 120 children showed that a short hypnosis session before the operation had no beneficial effect on postoperative pain and anxiety in comparison to the control group (58). Using hypnosis in patients of dental surgery significantly reduced intraoperative anxiety compared to the control group (using only local anesthesia as standard care) (59). A clinical randomized study compared the efficacy of midazolam and hypnosis among children. They assessed anxiety level by using the mYPAS score in four phases (the first phase entering the department, second entering the operation room, third fixing the face mask) and postoperative behavioral changes by using the Post-hospitalization Behavioral Questionnaire (PHBQ) and concluded that the effect of hypnosis was similar to midazolam in reducing preoperative anxiety (60). Among children who had hypnosis therapy at the time of anesthesia, anxiety (anxiety level was assessed by the modified Yale preoperative anxiety scale) was significantly lower compared to the control group (61). In a study, patients who had self-hypnosis experienced more postoperative relaxation and had lesser use of pain medications unlike the control group (62). A 15-min hypnosis therapy before incisional breast biopsy reduced distress before surgery [based on visual analog scales (VAS)] compared to the control group (63).
Acupuncture
Acupuncture is a traditional treatment that originated from China and spread through the world that uses needling specific points through the patient's skin for therapeutic purposes (159). Acupuncture is increasingly used and investigated for its potential in treating preoperative anxiety (160). A meta-analysis of the 13 published clinical trials, including 439 patients and 595 control participants, evaluating the effect of acupuncture techniques on preoperative anxiety showed the statistically significant superiority of acupuncture compared to placebo or no-treatment groups (160). Studies offered acupuncture sessions lasting between 10 and 30 min; sessions were conducted in operating waiting rooms on the day of surgery using acupuncture needles, balls, and beads in body and/or auricular acupoints (160).
Discussion
The review of literature on the non-pharmacologic interventions for preoperative anxiety showed a wide range of options evaluated for this indication with promising results. However, there are some concerns about the availability, cost, and required educated personnel to bring these methods into clinical practice. For example CBT, due to the limited number of practitioners, even in developed countries, can be difficult to find. Similar limitations may be present in practicing meditation and guided imagery relaxation therapies. On the other hand applying techniques such as aromatherapy and music is easy without the need for a specially trained therapist and can be more widely recommended and practiced.
Regarding the person who delivers the non-pharmacologic method to the patient, there is not unique practice in different methods and even in the same method among different studies. Interview and communication strategies have mostly been practiced by the surgeon or anesthesiologist of the patient. Cognitive-behavioral therapy is mostly delivered by trained psychologists. The limitations in the access to trained psychologists for practicing CBT led to attempts to turn the technique into a simplified therapy administered by nurses using treatment manuals. However, manualized therapies have limitations, especially facing more complicated patients and the efficacy is more limited compared to the trained psychologists who delivered CBT (161). Hypnosis also suffers similar limitations. Meditation and guided imagery relaxation therapy, massage, and acupuncture of specific points are among the easier techniques which can be more simplified and manualized. These techniques are routinely practiced by different members of the perioperative care team, mostly nurses, passing the short training courses. At the end of the spectrum aromatherapy, preparative video training, and music therapy can be even self-practice by the patients following simple instructions without the need for a specific training course for the delivery of these methods.
Regarding the timing of delivery of non-pharmacologic methods for preoperative anxiety, most studies evaluated the efficacy of these methods the day before or the same day of surgical procedure. However, this time seems to be late because many patients may suffer anxiety from the time scheduled for the surgery which is mostly long before the surgical procedure. It is reported that assessment of patients about the level of preoperative anxiety 1–2 weeks prior to the surgical procedure was more effective in alleviating the anxiety compared to the preoperative visit on the night before surgery (7). So earlier assessment of anxiety is recommended which provides us the opportunity of earlier intervention and referral of patients with a higher level of anxiety for a psychological consultation (7).
This study has some limitations. First of all, this study is just a narrative review of some clinical trials which were conducted to evaluate the efficacy of some of the non-pharmacological interventions for reducing preoperative anxiety. Second, we didn't evaluate the quality of the trials by a specific objective instrument. Beside these limitations the study has important strength which is the first study that gathers the current clinical evidence on non-pharmacologic treatments for anxiety, altogether.
Implications of the Results for Practice, Policy, and Future Research
As described above, due to the side effects of pharmacological interventions of preoperative anxiety, non-pharmacological interventions are becoming an alternative suggested item. Overall, few side effects are reported about non-pharmacological interventions so they can be used in patients of different ages and types of disease and surgery. As there are some controversies about the efficacy of these interventions in preoperative anxiety, more randomized clinical trials with a larger sample size are needed to evaluate the efficacy of these interventions.
Author Contributions
XH and YW designed the work, reviewed the literature, and drafted the first version of the manuscript. RW and MA researched the literature, added some parts, and critically revised the article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank Dr. Leyla Abbasi at the Research Consultation Center for her invaluable assistance in editing this manuscript.
References
1. Buehrer TW, Rosenthal R, Stierli P, Gurke L. Patients' views on regional anesthesia for elective unilateral carotid endarterectomy—a prospective cohort study. Ann Vasc Surg. (2015) 29:1392–9. doi: 10.1016/j.avsg.2015.04.085
2. Munafò MR, Stevenson J. Anxiety and surgical recovery: reinterpreting the literature. J Psychosom Res. (2001) 51:589–96. doi: 10.1016/S0022-3999(01)00258-6
3. Kain ZN, Maranets I. Preoperative anxiety and intraoperative anesthetic requirements. Anesth Analg. (2000) 91:250. doi: 10.1213/00000539-200007000-00063
4. Caumo W, Schmidt AP, Schneider CN, Bergmann J, Iwamoto C, Bandeira D, et al. Risk factors for preoperative anxiety in adults. Acta Anaesthesiol Scand. (2001) 45:298–307. doi: 10.1034/j.1399-6576.2001.045003298.x
5. Corman HH, Hornick EJ, Kritchman M, Terestman N. Emotional reactions of surgical patients to hospitalization, anesthesia and surgery. Am J Surg. (1958) 96:646–53. doi: 10.1016/0002-9610(58)90466-5
6. Vernon D, Foley J, Sipowicz R, Schulman J. The psychological responses of children to hospitalization and illness. Kango kenkyu Jpn J Nurs Sci. (1971) 4:45.
7. Stamenkovic DM, Rancic NK, Latas MB, Neskovic V, Rondovic GM, Wu JD, et al. Preoperative anxiety and implications on postoperative recovery: what can we do to change our history. Minerva Anestesiol. (2018) 84:1307–17. doi: 10.23736/S0375-9393.18.12520-X
8. Khalili N, Karvandian K, Ardebili HE, Eftekhar N, Nabavian O. Predictive factors of preoperative anxiety in the anesthesia clinic: a survey of 231 surgical candidates. Arch Anesth Crit Care. (2019) 5:122–7. doi: 10.18502/aacc.v5i4.1452
9. Kulik JA, Mahler HI. Social support and recovery from surgery. Health Psychol. (1989) 8:221. doi: 10.1037/0278-6133.8.2.221
10. Akkaş Gürsoy A. To determine the anxiety levels and the factors which may cause anxiety in preoperative surgical patients. J Nursing Res Dev. (2001) 1:23–9.
11. Clark DA, Cook A, Snow D. Depressive symptom differences in hospitalized, medically ill, depressed psychiatric inpatients and nonmedical controls. J Abnorm Psychol. (1998) 107:38. doi: 10.1037/0021-843X.107.1.38
12. Jørgensen P, Aagaard J, Jespersen JH, Mortensen L. Nonspecific psychological distress, psychosocial stressors and delusional psychosis: a comparison with psychiatrically symptom free surgical controls. Acta Psychiatr Scand. (1987) 75:190–4. doi: 10.1111/j.1600-0447.1987.tb02773.x
13. Perks A, Chakravarti S, Manninen P. Preoperative anxiety in neurosurgical patients. J Neurosurg Anesthesiol. (2009) 21:127–30. doi: 10.1097/ANA.0b013e31819a6ca3
14. Boeke S, Stronks D, Verhage F, Zwaveling A. Psychological variables as predictors of the length of post-operative hospitalization. J Psychosom Res. (1991) 35:281–8. doi: 10.1016/0022-3999(91)90082-Y
15. Vernon DT, Schulman JL, Foley JM. Changes in children's behavior after hospitalization: some dimensions of response and their correlates. Am J Dis Child. (1966) 111:581–93. doi: 10.1001/archpedi.1966.02090090053003
16. Kain ZN, Caldwell-Andrews AA, Maranets I, McClain B, Gaal D, Mayes LC, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg. (2004) 99:1648–54. doi: 10.1213/01.ANE.0000136471.36680.97
17. Badner NH, Nielson WR, Munk S, Kwiatkowska C, Gelb AW. Preoperative anxiety: detection and contributing factors. Can J Anaesth. (1990) 37:444. doi: 10.1007/BF03005624
18. Boeke S, Duivenvoorden HJ, Verhage F, Zwaveling A. Prediction of postoperative pain and duration of hospitalization using two anxiety measures. Pain. (1991) 45:293–7. doi: 10.1016/0304-3959(91)90053-Z
19. Williams JG, Jones JR. Psychophysiological responses to anesthesia and operation. JAMA. (1968) 203:415–7. doi: 10.1001/jama.1968.03140060039010
20. Vileikyte L. Stress and wound healing. Clin Dermatol. (2007) 25:49–55. doi: 10.1016/j.clindermatol.2006.09.005
21. Linn BS, Linn MW, Klimas NG. Effects of psychophysical stress on surgical outcome. Psychosom Med. (1988). doi: 10.1097/00006842-198805000-00002
22. Boeke S, Jelicic M, Bonke B. Pre-operative anxiety variables as possible predictors of post-operative stay in hospital. Br J Clin Psychol. (1992) 31:366–8. doi: 10.1111/j.2044-8260.1992.tb01008.x
23. Aitkenhead AR, Smith G, Rowbotham DJ. Textbook of Anaesthesia. Amsterdam: Elsevier Health Sciences (2007).
24. Weissman C. The metabolic response to stressan overview and update. Anesthesiology. (1990) 73:308–27. doi: 10.1097/00000542-199008000-00020
25. John M. Managing anxiety in the elective surgical patient. Br J Nurs. (2009) 18:416–9. doi: 10.12968/bjon.2009.18.7.41655
26. Kiecolt-Glaser JK, Page GG, Marucha PT, MacCallum RC, Glaser R. Psychological influences on surgical recovery: perspectives from psychoneuroimmunology. Am Psychol. (1998) 53:1209. doi: 10.1037/0003-066X.53.11.1209
27. Woldegerima Y, Fitwi G, Yimer H, Hailekiros A. Prevalence and factors associated with preoperative anxiety among elective surgical patients at University of Gondar Hospital. Gondar, Northwest Ethiopia, 2017. A cross-sectional study. Int J Surg Open. (2018) 10:21–9. doi: 10.1016/j.ijso.2017.11.001
28. Kain ZN, Mayes LC, Bell C, Weisman S, Hofstadter MB, Rimar S. Premedication in the United States: a status report. Anesth Analg. (1997) 84:427–32. doi: 10.1213/00000539-199702000-00035
29. Kang HE, Jung SM, Park S. Pharmacological and non-pharmacological interventions to alleviate anxiety before pediatric anesthesia: a survey of current practice in Korea. Anesth Pain Med. (2016) 11:55–63. doi: 10.17085/apm.2016.11.1.55
30. Jlala HA, Bedforth NM, Hardman JG. Anesthesiologists' perception of patients' anxiety under regional anesthesia. Local Reg Anesth. (2010) 3:65. doi: 10.2147/LRA.S11271
31. Bondy LR, Sims N, Schroeder DR, Offord KP, Narr BJ. The effect of anesthetic patient education on preoperative patient anxiety. Reg Anesth Pain Med. (1999) 24:158–64. doi: 10.1097/00115550-199924020-00011
32. Giraudet-Le Quintrec J-S, Coste J, Vastel L, Pacault V, Jeanne L, Lamas J-P, et al. Positive effect of patient education for hip surgery: a randomized trial. Clin Orthop Relat Res. (2003) 414:112–20. doi: 10.1097/01.blo.0000079268.91782.bc
33. Vuorma S, Rissanen P, Aalto AM, Hurskainen R, Kujansuu E, Teperi J. Impact of patient information booklet on treatment decision–a randomized trial among women with heavy menstruation. Health Expect. (2003) 6:290–7. doi: 10.1046/j.1369-7625.2003.00225.x
35. Blumenthal JA, Babyak MA, Carney RM, Keefe FJ, Davis RD, LaCaille RA, et al. Telephone-based coping skills training for patients awaiting lung transplantation. J Consult Clin Psychol. (2006) 74:535. doi: 10.1037/0022-006X.74.3.535
36. Kalkhoran MA, Karimollahi M. Religiousness and preoperative anxiety: a correlational study. Ann Gen Psychiatry. (2007) 6:1–5. doi: 10.1186/1744-859X-6-17
37. Agarwal A, Ranjan R, Dhiraaj S, Lakra A, Kumar M, Singh U. Acupressure for prevention of pre-operative anxiety: a prospective, randomised, placebo controlled study. Anaesthesia. (2005) 60:978–81. doi: 10.1111/j.1365-2044.2005.04332.x
38. Cooke M, Chaboyer W, Schluter P, Hiratos M. The effect of music on preoperative anxiety in day surgery. J Adv Nurs. (2005) 52:47–55. doi: 10.1111/j.1365-2648.2005.03563.x
39. Twiss E, Seaver J, McCaffrey R. The effect of music listening on older adults undergoing cardiovascular surgery. Nurs Crit Care. (2006) 11:224–31. doi: 10.1111/j.1478-5153.2006.00174.x
40. Yardakçi R, Akyolcu N. The effect of the visits made preoperative period on the patients' anxiety level. J Nurs Res Deve. (2004) 6:7–14.
41. McClurkin SL, Smith CD. The duration of self-selected music needed to reduce preoperative anxiety. J Perianesth Nurs. (2016) 31:196–208. doi: 10.1016/j.jopan.2014.05.017
42. Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database Syst Rev. (2013) 6:CD006908. doi: 10.1002/14651858.CD006908.pub2
43. O'regan P, Wills T. The growth of complementary therapies: and their benefits in the perioperative setting. J Perioper Pract. (2009) 19:382–6. doi: 10.1177/175045890901901102
44. Wright KD, Stewart SH, Finley GA, Buffett-Jerrott SE. Prevention and intervention strategies to alleviate preoperative anxiety in children: a critical review. Behav Modif. (2007) 31:52–79. doi: 10.1177/0145445506295055
45. Dao TK, Youssef NA, Armsworth M, Wear E, Papathopoulos KN, Gopaldas R. Randomized controlled trial of brief cognitive behavioral intervention for depression and anxiety symptoms preoperatively in patients undergoing coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. (2011) 142:e109–15. doi: 10.1016/j.jtcvs.2011.02.046
46. Gade H, Friborg O, Rosenvinge JH, Småstuen MC, Hjelmesæth J. The impact of a preoperative cognitive behavioural therapy (CBT) on dysfunctional eating behaviours, affective symptoms and body weight 1 year after bariatric surgery: a randomised controlled trial. Obes Surg. (2015) 25:2112–9. doi: 10.1007/s11695-015-1673-z
47. Cassin SE, Sockalingam S, Du C, Wnuk S, Hawa R, Parikh SV, et al. Pilot randomized controlled trial of telephone-based cognitive behavioural therapy for preoperative bariatric surgery patients. Behav Res Ther. (2016) 80:17–22. doi: 10.1016/j.brat.2016.03.001
48. Rajeswari SR, Rayala Chandrasekhar CV, Uloopi K, RojaRamya KS, Ramesh MV. Effectiveness of cognitive behavioral play therapy and audiovisual distraction for management of preoperative anxiety in children. Int J Clin Pediatr Dent. (2019) 12:419. doi: 10.5005/jp-journals-10005-1661
49. Birch S, Stilling M, Mechlenburg I, Hansen TB. No effect of cognitive behavioral patient education for patients with pain catastrophizing before total knee arthroplasty: a randomized controlled trial. Acta Orthop. (2020) 91:98–103. doi: 10.1080/17453674.2019.1694312
50. Felix MMdS, Ferreira MBG, Oliveira LFd, Barichello E, Pires PdS, Barbosa MH. Guided imagery relaxation therapy on preoperative anxiety: a randomized clinical trial. Rev Lat Am Enfermagem. (2018) 26:e3101. doi: 10.1590/1518-8345.2850.3101
51. Vagnoli L, Bettini A, Amore E, De Masi S, Messeri A. Relaxation-guided imagery reduces perioperative anxiety and pain in children: a randomized study. Eur J Pediatr. (2019) 178:913–21. doi: 10.1007/s00431-019-03376-x
52. Haipin L, Speir AM, CapoBianco P, Barnett SD. Guided imagery in cardiac surgery. Outcomes Manag. (2002) 6:132–7.
53. Charette S, Fiola JL, Charest M-C, Villeneuve E, Théroux J, Joncas J, et al. Guided imagery for adolescent post-spinal fusion pain management: a pilot study. Pain Manag Nurs. (2015) 16:211–20. doi: 10.1016/j.pmn.2014.06.004
54. Kekecs Z, Jakubovits E, Varga K, Gombos K. Effects of patient education and therapeutic suggestions on cataract surgery patients: a randomized controlled clinical trial. Patient Educ Couns. (2014) 94:116–22. doi: 10.1016/j.pec.2013.09.019
55. Manyande A, Berg S, Gettins D, Stanford SC, Mazhero S, Marks DF, et al. Preoperative rehearsal of active coping imagery influences subjective and hormonal responses to abdominal surgery. Psychosom Med. (1995) 57:177–82. doi: 10.1097/00006842-199503000-00010
56. Amraoui J, Pouliquen C, Fraisse J, Dubourdieu J, Guzer SRD, Leclerc G, et al. Effects of a hypnosis session before general anesthesia on postoperative outcomes in patients who underwent minor breast cancer surgery: the HYPNOSEIN randomized clinical trial. JAMA Network Open. (2018) 1:e181164 doi: 10.1001/jamanetworkopen.2018.1164
57. Saadat H, Drummond-Lewis J, Maranets I, Kaplan D, Saadat A, Wang S-M, et al. Hypnosis reduces preoperative anxiety in adult patients. Anesth Analg. (2006) 102:1394–6. doi: 10.1213/01.ane.0000204355.36015.54
58. Duparc-Alegria N, Tiberghien K, Abdoul H, Dahmani S, Alberti C, Thiollier AF. Assessment of a short hypnosis in a paediatric operating room in reducing postoperative pain and anxiety: a randomised study. J Clin Nurs. (2018) 27:86–91. doi: 10.1111/jocn.13848
59. Hermes D, Gerdes V, Trübger D, Hakim S, Sieg P. Evaluation of intraoperative standardized hypnosis with the state-trait anxiety inventory. Mund Kiefer Gesichtschir. (2004) 8:111–7. doi: 10.1007/s10006-004-0533-0
60. Calipel S, Lucas-Polomeni MM, Wodey E, Ecoffey C. Premedication in children: hypnosis versus midazolam. Paediatr Anaesth. (2005) 15:275–81. doi: 10.1111/j.1460-9592.2004.01514.x
61. Huet A, Lucas-Polomeni M-M, Robert J-C, Sixou J-L, Wodey E. Hypnosis and dental anesthesia in children: a prospective controlled study. Int J Clin Exp Hypn. (2011) 59:424–40. doi: 10.1080/00207144.2011.594740
62. Ashton C Jr, Whitworth G, Seldomridge J, Shapiro P, Weinberg A, Michler R, et al. Self-hypnosis reduces anxiety following coronary artery bypass surgery. A prospective, randomized trial. J Card Surg. (1997) 38:69–75.
63. Schnur JB, Bovbjerg DH, David D, Tatrow K, Goldfarb AB, Silverstein JH, et al. Hypnosis decreases presurgical distress in excisional breast biopsy patients. Anesth Analg. (2008) 106:440–4. doi: 10.1213/ane.0b013e31815edb13
64. Lim L, Chow P, Wong C-Y, Chung A, Chan Y-H, Wong W-K, et al. Doctor–patient communication, knowledge, and question prompt lists in reducing preoperative anxiety–a randomized control study. Asian J Surg. (2011) 34:175–80. doi: 10.1016/j.asjsur.2011.11.002
65. Jadin SMMF. Effect of structured pre-anesthetic communication on preoperative patient anxiety. Medizinische Fakultät der Universität Basel. (2018) 8:1–5. doi: 10.4172/2155-6148.1000767
66. Nikumb VB, Banerjee A, Kaur G, Chaudhury S. Impact of doctor-patient communication on preoperative anxiety: study at industrial township, Pimpri, Pune. Ind Psychiatry J. (2009) 18:19. doi: 10.4103/0972-6748.57852
67. Abbasi S, Akbari L. The effect of personnel primary communication on the pre-operative anxiety of patients admitted to operating room. Nurs Pract Today. (2015) 2:164–70.
68. Olatunji BO, Cisler JM, Deacon BJ. Efficacy of cognitive behavioral therapy for anxiety disorders: a review of meta-analytic findings. Psychiatric Clinics. (2010) 33:557–77. doi: 10.1016/j.psc.2010.04.002
69. Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. (2006) 26:17–31. doi: 10.1016/j.cpr.2005.07.003
70. Arch JJ, Craske MG. First-line treatment: a critical appraisal of cognitive behavioral therapy developments and alternatives. Psychiatric Clinics. (2009) 32:525–47. doi: 10.1016/j.psc.2009.05.001
71. Klein DF. Flawed meta-analyses comparing psychotherapy with pharmacotherapy. Am J Psychiatry. (2000) 157:1204–11. doi: 10.1176/appi.ajp.157.8.1204
72. Kaczkurkin AN, Foa EB. Cognitive-behavioral therapy for anxiety disorders: an update on the empirical evidence. Dialogues Clin Neurosci. (2015) 17:337. doi: 10.31887/DCNS.2015.17.3/akaczkurkin
73. Papaioannou M, Skapinakis P, Damigos D, Mavreas V, Broumas G, Palgimesi A. The role of catastrophizing in the prediction of postoperative pain. Pain Med. (2009) 10:1452–9. doi: 10.1111/j.1526-4637.2009.00730.x
74. Rajput SK, Tiwari T, Chaudhary AK. Effect of preoperative multimedia based video information on perioperative anxiety and hemodynamic stability in patients undergoing surgery under spinal anesthesia. J Family Med Prim Care. (2021) 10:237–42. doi: 10.4103/jfmpc.jfmpc_1544_20
75. Eijlers R, Staals LM, Legerstee J, Berghmans J, Strabbing EM, van der Schroeff M, et al. Predicting intense levels of child anxiety during anesthesia induction at hospital arrival. J Clin Psychol Med Settings. (2020) 28:313–22. doi: 10.1007/s10880-020-09716-6
76. Hadlandsmyth K, Conrad M, Steffensmeier KS, Van Tiem J, Obrecht A, Cullen JJ, et al. Enhancing the biopsychosocial approach to perioperative care: a pilot randomized trial of the perioperative pain self-management (PePS) intervention. Ann Surg. (2020) 275:e8–14. doi: 10.1097/SLA.0000000000004671
77. Rosmarin DH, Pargament KI, Mahoney A. The role of religiousness in anxiety, depression, and happiness in a Jewish community sample: a preliminary investigation. Ment Health Relig Cult. (2009) 12:97–113. doi: 10.1080/13674670802321933
78. Henrie J, Patrick JH. Religiousness, religious doubt, and death anxiety. Int J Aging Hum Dev. (2014) 78:203–27. doi: 10.2190/AG.78.3.a
79. Wink P. Who is afraid of death? Religiousness, spirituality, and death anxiety in late adulthood. J Relig Spiritual Aging. (2006) 18:93–110. doi: 10.1300/J496v18n02_08
80. Barati Z, Mohammadian M, Jaafari GH, Karami Jooshan M, Mohebi S. The relationship between preoperative anxiety and religious beliefs. Islam Health J. (2015) 2:42–7.
81. Hosseini M, Salehi A, Fallahi Khoshknab M, Rokofian A, Davidson PM. The effect of a preoperative spiritual/religious intervention on anxiety in Shia Muslim patients undergoing coronary artery bypass graft surgery: a randomized controlled trial. J Holist Nurs. (2013) 31:164–72. doi: 10.1177/0898010113488242
82. Jia T, Ogawa Y, Miura M, Ito O, Kohzuki M. Music attenuated a decrease in parasympathetic nervous system activity after exercise. PLoS ONE. (2016) 11:e0148648. doi: 10.1371/journal.pone.0148648
83. Aitken JC, Wilson S, Coury D, Moursi AM. The effect of music distraction on pain, anxiety and behavior in pediatric dental patients. Pediatr Dent. (2002) 24:114–8.
84. Palmer JB, Lane D, Mayo D, Schluchter M, Leeming R. Effects of music therapy on anesthesia requirements and anxiety in women undergoing ambulatory breast surgery for cancer diagnosis and treatment: a randomized controlled trial. J Clin Oncol. (2015) 33:3162. doi: 10.1200/JCO.2014.59.6049
85. Cunningham MF, Monson B, Bookbinder M. Introducing a music program in the perioperative area. AORN J. (1997) 66:674–82. doi: 10.1016/S0001-2092(06)62920-7
86. Koch ME, Kain ZN, Ayoub C, Rosenbaum SH. The sedative and analgesic sparing effect of music. Anesthesiology. (1998) 89:300–6. doi: 10.1097/00000542-199808000-00005
87. Muddana SK, Hess OM, Sundar S, Venkatesh R. Preoperative and perioperative music to reduce anxiety during first-time phacoemulsification cataract surgery in the high-volume setting: randomized controlled trial. J Cataract Refract Surg. (2020). doi: 10.1097/j.jcrs.0000000000000485
88. Akelma FK, Altinsoy S, Arslan M, Ergil J. Effect of favorite music on postoperative anxiety and pain. Anaesthesist. (2020) 69:198–204. doi: 10.1007/s00101-020-00731-8
89. Tan DJA, Polascik BA, Kee HM, Hui Lee AC, Sultana R, Kwan M, et al. The Effect of perioperative music listening on patient satisfaction, anxiety, and depression: a quasiexperimental study. Anesthesiol Res Prac. (2020) 2020:3761398. doi: 10.1155/2020/3761398
90. Kupeli I, Gülnahar Y. Comparing different music genres in decreasing dental anxiety in young adults who underwent third molar surgery in turkey: randomized controlled trial. J Oral Maxillofac Surg. (2020) 78:546.e1–7. doi: 10.1016/j.joms.2019.11.029
91. Kain ZN, Caldwell-Andrews AA, Krivutza DM, Weinberg ME, Gaal D, Wang S-M, et al. Interactive music therapy as a treatment for preoperative anxiety in children: a randomized controlled trial. Anesth Analg. (2004) 98:1260–6. doi: 10.1213/01.ANE.0000111205.82346.C1
92. Nguyen CV, Alvin M, Lee C, George D, Gilmore A, Tripi PA, et al. A prospective randomised study on efficacy of music for decreasing preoperative anxiety in children. J Perioper Pract. (2021) 31:268–73. doi: 10.1177/1750458920939780
93. Drzymalski DM, Lumbreras-Marquez MI, Tsen LC, Camann WR, Farber MK. The effect of patient-selected or preselected music on anxiety during cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. (2020) 33:4062–8. doi: 10.1080/14767058.2019.1594766
94. Kühlmann AYR, van Rosmalen J, Staals LM, Keyzer-Dekker CMG, Dogger J, de Leeuw TG, et al. Music interventions in pediatric surgery (The Music Under Surgery In Children Study): a randomized clinical trial. Anesth Analg. (2020) 130:991–1001. doi: 10.1213/ANE.0000000000003983
95. Pinto RP, Hollandsworth JG. Using videotape modeling to prepare children psychologically for surgery: influence of parents and costs versus benefits of providing preparation services. Health Psychol. (1989) 8:79. doi: 10.1037/0278-6133.8.1.79
96. Karabulut N, Arikan D. The effect of different training programs applied prior to surgical operation on anxiety levels. Yeni Symposium (2009).
97. Helms LJ. Video education to improve preoperative anxiety in the bariatric surgical patient: a quality improvement project. J Perianesth Nurs. (2020) 35:467–71. doi: 10.1016/j.jopan.2020.01.012
98. Lee J, Lee J, Lim H, Son J-S, Lee J-R, Kim D-C, et al. Cartoon distraction alleviates anxiety in children during induction of anesthesia. Anesth Analg. (2012) 115:1168–73. doi: 10.1213/ANE.0b013e31824fb469
99. Durst LM. Preoperative teaching videotape: the effect on children's behavior. AORN J. (1990) 52:576–84. doi: 10.1016/S0001-2092(07)69884-6
100. Luck A, Pearson S, Maddem G, Hewett P. Effects of video information on precolonoscopy anxiety and knowledge: a randomised trial. Lancet. (1999) 354:2032–5. doi: 10.1016/S0140-6736(98)10495-6
101. Ayral X, Gicquere C, Duhalde A, Boucheny D, Dougados M. Effects of video information on preoperative anxiety level and tolerability of joint lavage in knee osteoarthritis. Arthritis Care Res. (2002) 47:380–2. doi: 10.1002/art.10559
102. Jlala H, French J, Foxall G, Hardman J, Bedforth N. Effect of preoperative multimedia information on perioperative anxiety in patients undergoing procedures under regional anaesthesia. Br J Anaesth. (2010) 104:369–74. doi: 10.1093/bja/aeq002
103. Noben L, Goossens SMTA, Truijens SEM, Van Berckel MMG, Perquin CW, Slooter GD, et al. A virtual reality video to improve information provision and reduce anxiety before cesarean delivery: randomized controlled trial. JMIR Ment Health. (2019) 6:e15872. doi: 10.2196/15872
104. Wakimizu R, Kamagata S, Kuwabara T, Kamibeppu K. A randomized controlled trial of an at-home preparation programme for Japanese preschool children: effects on children's and caregivers' anxiety associated with surgery. J Eval Clin Pract. (2009) 15:393–401. doi: 10.1111/j.1365-2753.2008.01082.x
105. Melamed BG, Siegel LJ. Reduction of anxiety in children facing hospitalization and surgery by use of filmed modeling. J Consult Clin Psychol. (1975) 43:511. doi: 10.1037/h0076896
106. O'Conner-Von S. Preparation of adolescents for outpatient surgery: using an Internet program. AORN J. (2008) 87:374–98. doi: 10.1016/j.aorn.2007.07.024
107. Chow CH, Van Lieshout RJ, Schmidt LA, Dobson KG, Buckley N. Systematic review: audiovisual interventions for reducing preoperative anxiety in children undergoing elective surgery. J Pediatr Psychol. (2016) 41:182–203. doi: 10.1093/jpepsy/jsv094
108. Kerimoglu B, Neuman A, Paul J, Stefanov DG, Twersky R. Anesthesia induction using video glasses as a distraction tool for the management of preoperative anxiety in children. Anesth Analg. (2013) 117:1373–9. doi: 10.1213/ANE.0b013e3182a8c18f
109. Klassen JA, Liang Y, Tjosvold L, Klassen TP, Hartling L. Music for pain and anxiety in children undergoing medical procedures: a systematic review of randomized controlled trials. Ambul Pediatr. (2008) 8:117–28. doi: 10.1016/j.ambp.2007.12.005
110. Fazlollahpour-Rokni F, Shorofi SA, Mousavinasab N, Ghafari R, Esmaeili R. The effect of inhalation aromatherapy with rose essential oil on the anxiety of patients undergoing coronary artery bypass graft surgery. Complement Ther Clin Pract. (2019) 34:201–7. doi: 10.1016/j.ctcp.2018.11.014
112. Heydari M, Homayouni K, Hashempur M, Shams M. Topical citrullus colocynthis in painful diabetic neuropathy: a double-blind randomized placebo-controlled clinical trial. J Diabetes. (2015) 8:246–52. doi: 10.1111/1753-0407.12287
113. Schnaubelt K. Advanced Aromatherapy: The Science of Essential Oil Therapy. Rochester, VT; Healing Arts Press (1998).
115. Mosavat SH, Ghahramani L, Sobhani Z, Haghighi ER, Chaijan MR, Heydari M. The effect of leek (Allium iranicum (Wendelbo)) leaves extract cream on hemorrhoid patients: A double blind randomized controlled clinical trial. Eur J Integr Med. (2015) 7:669–73. doi: 10.1016/j.eujim.2015.08.008
116. Ali B, Al-Wabel NA, Shams S, Ahamad A, Khan SA, Anwar F. Essential oils used in aromatherapy: a systemic review. Asian Pac J Trop Biomed. (2015) 5:601–11. doi: 10.1016/j.apjtb.2015.05.007
117. Niazi M, Hashempur MH, Taghizadeh M, Heydari M, Shariat A. Efficacy of topical Rose (Rosa damascena Mill.) oil for migraine headache: a randomized double-blinded placebo-controlled cross-over trial. Complement Ther Med. (2017) 34:35–41. doi: 10.1016/j.ctim.2017.07.009
118. Jafarpour M, Yousefi G, Hamedi A, Shariat A, Salehi A, Heydari M. Effect of a traditional syrup from Citrus medica L. fruit juice on migraine headache: a randomized double blind placebo controlled clinical trial. J Ethnopharmacol. (2016) 179:170–6. doi: 10.1016/j.jep.2015.12.040
119. Fayazi S, Babashahi M, Rezaei M. The effect of inhalation aromatherapy on anxiety level of the patients in preoperative period. Iran J Nurs Midwifery Res. (2011) 16:278.
120. Farrar AJ, Farrar FC. Clinical aromatherapy. Nurs Clin North Am. (2020) 55:489–504. doi: 10.1016/j.cnur.2020.06.015
121. Stanley PF, Wan LF, Karim RA. A randomized prospective placebo-controlled study of the effects of lavender aromatherapy on preoperative anxiety in cataract surgery patients. J Perianesth Nurs. (2020) 35:403–6. doi: 10.1016/j.jopan.2019.12.004
122. Jaruzel CB, Gregoski M, Mueller M, Faircloth A, Kelechi T. Aromatherapy for preoperative anxiety: a pilot study. J Perianesth Nurs. (2019) 34:259–64. doi: 10.1016/j.jopan.2018.05.007
123. Genc H, Saritas S. The effects of lavender oil on the anxiety and vital signs of benign prostatic hyperplasia patients in preoperative period. Explore. (2020) 16:116–22. doi: 10.1016/j.explore.2019.07.008
124. Ayik C, Özden D. The effects of preoperative aromatherapy massage on anxiety and sleep quality of colorectal surgery patients: a randomized controlled study. Complement Ther Med. (2018) 36:93–9. doi: 10.1016/j.ctim.2017.12.002
125. Bozkurt P, Vural Ç. Effect of lavender oil inhalation on reducing presurgical anxiety in orthognathic surgery patients. J Oral Maxillofac Surg. (2019) 77:2466. e1–7. doi: 10.1016/j.joms.2019.08.022
126. Muzzarelli L, Force M, Sebold M. Aromatherapy and reducing preprocedural anxiety: a controlled prospective study. Gastroenterol Nurs. (2006) 29:466–71. doi: 10.1097/00001610-200611000-00005
127. Akhlaghi M, Shabanian G, Rafieian-Kopaei M, Parvin N, Saadat M, Akhlaghi M. Citrus aurantium blossom and preoperative anxiety. Revista Brasileira de Anestesiologia. (2011) 61:702–12. doi: 10.1590/S0034-70942011000600002
128. Dagli R, Avcu M, Metin M, Kiymaz S, Ciftci H. The effects of aromatherapy using rose oil (Rosa damascena Mill.) on preoperative anxiety: a prospective randomized clinical trial. Eur J Integr Med. (2019) 26:37–42. doi: 10.1016/j.eujim.2019.01.006
129. Kim KY, Seo HJ, Min SS, Park M, Seol GH. The effect of 1, 8-cineole inhalation on preoperative anxiety: a randomized clinical trial. Evid Based Complement Alternat Med. (2014) 2014:820126. doi: 10.1155/2014/820126
130. Pasyar N, Rambod M, Araghi F. The effect of bergamot orange essence on anxiety, salivary cortisol, and alpha amylase in patients prior to laparoscopic cholecystectomy: a controlled trial. Complement Ther Clin Pract. (2020) 39:101153. doi: 10.1016/j.ctcp.2020.101153
131. Li Z, Bauer B, Aaberg M, Pool S, Van Rooy K, Schroeder D, et al. Benefits of hand massage on anxiety in preoperative outpatient: a quasi-experimental study with pre-and post-tests. Explore. (2021) 17:410–6. doi: 10.1016/j.explore.2020.08.016
132. Farahani MF, Zamenjani MN, Nasiri M, Shamsikhani S, Purfarzad Z, Harorani M. Effects of extremity massage on preoperative anxiety: a three-arm randomized controlled clinical trial on phacoemulsification candidates. J Perianesth Nurs. (2020) 35:277–82. doi: 10.1016/j.jopan.2019.10.010
133. Brand LR, Munroe DJ, Gavin J. The effect of hand massage on preoperative anxiety in ambulatory surgery patients. AORN J. (2013) 97:708–17. doi: 10.1016/j.aorn.2013.04.003
134. Mohammadpourhodki R, Sargolzaei MS, Basirinezhad MH. Evaluating the effect of massage based on slow stroke back massage on the anxiety of candidates for cataract surgery. Rom J Ophthalmol. (2019) 63:146. doi: 10.22336/rjo.2019.22
135. Peng S, Ying B, Chen Y, Sun X. Effects of massage on the anxiety of patients receiving percutaneous coronary intervention. Psychiatr Danub. (2015) 27:44–9.
136. Rosen J, Lawrence R, Bouchard M, Doros G, Gardiner P, Saper R. Massage for perioperative pain and anxiety in placement of vascular access devices. Adv Mind Body Med. (2013) 27:12–23. doi: 10.1089/thy.2012.0495
137. McRee LD, Noble S, Pasvogel A. Using massage and music therapy to improve postoperative outcomes. AORN J. (2003) 78:433–47. doi: 10.1016/S0001-2092(06)60754-0
139. Watson S. The effects of massage: an holistic approach to care. Nurs Standard. (1997) 11:45–7. doi: 10.7748/ns.11.47.45.s47
140. Boitor M, Martorella G, Maheu C, Laizner AM, Gélinas C. Effects of massage in reducing the pain and anxiety of the cardiac surgery critically ill—a randomized controlled trial. Pain Medicine. (2018) 19:2556–69. doi: 10.1093/pm/pny055
141. Cutshall SM, Mahapatra S, Hynes RS, Van Rooy KM, Looker SA, Ghosh A, et al. Hand massage for cancer patients undergoing chemotherapy as outpatients: a pilot study. Explore. (2017) 13:393–9. doi: 10.1016/j.explore.2017.06.007
142. Petry JJ. Surgery and complementary therapies: a review. Altern Ther Health Med. (2000) 6:64. doi: 10.1089/10762800050115239
143. Mei L, Miao X, Chen H, Huang X, Zheng G. Effectiveness of Chinese hand massage on anxiety among patients awaiting coronary angiography: a randomized controlled trial. J Cardiovasc Nurs. (2017) 32:196–203. doi: 10.1097/JCN.0000000000000309
144. Kaada B, Torsteinbø O. Increase of plasma beta-endorphins in connective tissue massage. Gen Pharmacol. (1989) 20:487. doi: 10.1016/0306-3623(89)90200-0
145. Piotrowski MM, Paterson C, Mitchinson A, Kim HM, Kirsh M, Hinshaw DB. Massage as adjuvant therapy in the management of acute postoperative pain: a preliminary study in men. J Am Coll Surg. (2003) 197:1037–46. doi: 10.1016/j.jamcollsurg.2003.07.020
146. Nixon M, Teschendorff J, Finney J, Karnilowicz W. Expanding the nursing repertoire: the effect of massage on post-operative pain. Aust J Adv Nurs. (1997) 14:21–6.
147. Claire BJ. Complementary and alternative therapies in nursing edited by ruth lindquist, mariah snyder, and mary fran tracy. J Hospital Librarianship. (2014) 14:331–2. doi: 10.1080/15323269.2014.923975
148. Achterberg J. Mind and medicine: the role of imagery in healing. J Am Soc Phys Res. (1989) 83:93–100.
149. Gupta S, Pradhan S. Effect of psychoneurobics (meditation technique) on status of anxiety in patients undergoing cataract surgery: a randomized controlled trial. Int J Prev Curative Commun Med. (2018) 4:36–42. doi: 10.24321/2454.325X.201822
150. Frenay M-C, Faymonville M-E, Devlieger S, Albert A, Vanderkelen A. Psychological approaches during dressing changes of burned patients: a prospective randomised study comparing hypnosis against stress reducing strategy. Burns. (2001) 27:793–9. doi: 10.1016/S0305-4179(01)00035-3
152. Raz A, Fan J, Posner MI. Hypnotic suggestion reduces conflict in the human brain. Proc Nat Acad Sci. (2005) 102:9978–83. doi: 10.1073/pnas.0503064102
153. Wobst AH. Hypnosis and surgery: past, present, and future. Anesth Analg. (2007) 104:1199–208. doi: 10.1213/01.ane.0000260616.49050.6d
154. Zahourek RP. Trance and suggestion: timeless interventions and implication for nurses in the new millennium. Holist Nurs Pract. (2001) 15:73–82. doi: 10.1097/00004650-200104000-00012
155. Kravits K. Hypnosis: adjunct therapy for cancer pain management. J Adv Pract Oncol. (2013) 4:83. doi: 10.6004/jadpro.2013.4.2.2
156. Butler LD, Symons BK, Henderson SL, Shortliffe LD, Spiegel D. Hypnosis reduces distress and duration of an invasive medical procedure for children. Pediatrics. (2005) 115:e77–85. doi: 10.1542/peds.2004-0818
157. Liossi C, Hatira P. Clinical hypnosis in the alleviation of procedure-related pain in pediatric oncology patients. Int J Clin Exp Hypn. (2003) 51:4–28. doi: 10.1076/iceh.51.1.4.14064
158. Iserson KV. Hypnosis for pediatric fracture reduction. J Emerg Med. (1999) 17:53–6. doi: 10.1016/S0736-4679(98)00114-0
159. Kovich F A. new definition of an acupuncture meridian. J Acupunct Meridian Stud. (2019) 12:37–41. doi: 10.1016/j.jams.2018.05.001
160. Bae H, Bae H, Min B-I, Cho S. Efficacy of acupuncture in reducing preoperative anxiety: a meta-analysis. Evid Based Complement Alternat Med. (2014) 2014: 850367. doi: 10.1155/2014/850367
Keywords: preoperative anxiety, non-pharmacological, cognitive-behavioral therapy, aromatherapy, relaxation
Citation: Wang R, Huang X, Wang Y and Akbari M (2022) Non-pharmacologic Approaches in Preoperative Anxiety, a Comprehensive Review. Front. Public Health 10:854673. doi: 10.3389/fpubh.2022.854673
Received: 14 January 2022; Accepted: 14 March 2022;
Published: 11 April 2022.
Edited by:
Mojtaba Heydari, Shiraz University of Medical Sciences, IranReviewed by:
Reza Ghanei Gheshlagh, Kurdistan University of Medical Sciences, IranSeyed Hamdollah Mosavat, Shiraz University of Medical Sciences, Iran
Copyright © 2022 Wang, Huang, Wang and Akbari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuan Wang, sandyyuan198842@gmail.com
 Rulin Wang1
Rulin Wang1