
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 16 May 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.844832
Eczema, one of the most prevalent inflammatory skin diseases among children, is potentially influenced by genetic, environmental and social factors. However, few studies have investigated the effect of residential environment and lifestyle on childhood eczema. Therefore, this study conducted a cross-sectional study based on 2,781 preschool children in Shenzhen, China, during 2015–2016. Logistic regression models were employed to analyze the associations between residential/household environment, lifestyle, dietary habits and eczema in children. The prevalence of eczema among children in Shenzhen was 24.6%. Significant associations (increased odds >50%, P < 0.05) were found between childhood eczema and the factors of using composite wood floors (adjusted OR = 1.777 for doctor-diagnosed eczema, 1.911 for eczema-like symptoms), living in a villa/townhouse (aOR = 3.102, 2.156), the presence of mold or damp stains in the child's room (aOR = 1.807, 2.279), and rarely cleaning the child's room (aOR = 1.513, 1.540). In addition, watching TV/playing computer games for more than one hour per day was significantly associated with eczema (aOR = 1.172, 1.174). Notably, we found that eating rice/pasta one to three times per week may elevate the risk of eczema-like symptoms (aOR = 1.343), which warrants further investigation. In addition, ambient air pollution, in the covariates, may also affect childhood eczema. Therefore, avoiding these adverse factors and creating a low-risk environment are crucial to prevent childhood eczema.
Eczema, also known as allergic dermatitis, is one of the most prevalent inflammatory skin diseases among children. It usually occurs as pruritus at the back of the knees and the front of the elbow. About 15–30% of children all over the world suffer from eczema (1, 2). Although eczema is not life-threatening, it can lead to skin damage and cause a heavy burden on the quality of life of patients and their families, as well as consuming medical resources (3, 4). Moreover, eczema is a precursor to asthma and allergic rhinitis, and preventive measures for eczema are also aimed at preventing these more severe conditions later in life. Therefore, it is necessary to explore the key pathogenic factors in order to establish more effective preventive and therapeutic strategies.
The incidence of eczema may be associated with genetic factors, ambient air exposure, and social and economic status (5–8). However, the rapid urbanization and industrialization in China have changed people's consumption patterns, lifestyles and living environments (9–11). Meanwhile, the prevalence of eczema in children has also increased rapidly (12). Studies have reported that eczema in children from specific regions may be associated with the residential (13–16) and household environment (17–19). However, studies related to building materials and house types are rather limited by regions. Besides, dietary habits such as vegetable and fruit intake (20–23) and lifestyle factors e.g., parental smoking (14, 24) may also increase odds of eczema. But current findings have partially been conflicting, which may be because there are many confounders in dietary and lifestyle factors. However, no studies have incorporated all of these potential factors into investigation, making it difficult to explore the key influencing factors.
Hence, this study systemically investigated the associations of dietary habits, residential/household environment, and lifestyle and childhood eczema in Shenzhen, China. To the best of our knowledge, we provided the first comprehensive data on these potential influencing factors of childhood eczema in a typically urbanizing and industrializing region.
This study was based on a follow-up to the nationwide “China-Children-Homes-Health (CCHH)” study performed in 2010–2012 in multiple cities (12, 25). A total of 4,700 questionnaires were distributed to 30 kindergartens to investigate allergies and infections among children during 2015–2016 in Shenzhen, China (Figure 1). Shenzhen, which neighbors Hong Kong, is one of the most developed and urbanized cities in China, with a population of more than 13 million. Shenzhen features a subtropical maritime climate with a high annual temperature (24°C) and relative humidity of about 70%. Notably, Shenzhen has the largest number of kindergarten children (>500,000) in China.
Children in kindergartens were randomly sampled to represent the general population of preschool children in Shenzhen. Our questionnaire was based on the International Study of Asthma and Allergies in Childhood (ISAAC) (26) and a Swedish questionnaire regarding dampness in buildings and health (DBH) (27), with small changes to suit the conditions in the region. We collected information on eczema in childhood, residential/household environment, lifestyle and dietary habits of all family members. We entrusted the kindergartens to provide the questionnaires to the children's parents. To improve reliability, questionnaires were recommended to be filled out by the children's parents and returned to the kindergartens within 1 week.
We retrieved 4,614 filled questionnaires in total, with a very high response rate of 98.2%. First, 136 invalid samples with a large number of missing data were excluded. We then excluded 1,212 children aged younger than 3 years or older than 6 years. In addition, 485 questionnaires were invalid because of incomplete information about sex, age and eczema outcomes. Finally, a total of 2,781 samples with paired questionnaires were included in this study.
The residential/household environment represented the outdoor and indoor living environment. The lifestyles included living and dietary habits in the last 12 months before the survey. Relatively long exposure period was set to reflect the actual scenario of sensitization, because (1) eczema is a long-term disease and children are prone to recurrent attacks once eczema is triggered, and (2) the potential influencing factors such as dietary intake and lifestyles are generally stable within a long period.
Meats, seafood, fruits, vegetables, beans/grains, rice/pasta, eggs, milk, and fast food are considered common dietary components in China and were classified according to the frequency of their intake. Zero points represented never or occasional intake, one point was less than four times per week, and two points was four times or more per week (28).
The residential environment included the location (residential area and located near a highway or not), size, age, and the type of dwelling. The household environment, being the indoor environment formed by individual habits, encompassed mold, damp stains, water damage, window condensation, and house decoration status (floor materials and repainting the child's room or not). Lifestyles were defined as the daily routine and living habits of children and their families, including the frequency of cleaning and ventilating and airing bedclothes, the time spent watching TV/playing with a computer, keeping pets at home, and smoking in the child's room. Children were defined as being “exposed” when their questionnaires answered “Yes” to the corresponding questions.
“DDE” was defined by the following question: “Has your child ever been diagnosed with eczema by doctor(s)?”
“ELS” was defined by reviewing the children's eczema-like symptoms in the past 12 months. The symptoms were based on the diagnostic criteria, including redness, itching, rash, dryness, desquamation or blisters, and seborrhea.
Children were defined as having “DDE” or “ELS” when their questionnaires answered “Yes” to the corresponding questions.
According to previous studies (16, 21, 29–31), parental atopy, breast feeding and a child's age, sex, and birth season are the most general potential confounders for the associations of dietary habits, residential/household environment, and lifestyle with childhood eczema (Table 1). The information on confounding covariates was selected from the questionnaire. Birth season was classified according to the international standard season dates, and we defined parental atopy as at least one of the child's family members (siblings, parents, and/or grandparents) having had at least one of the following diseases: asthma, eczema, or rhinitis (8). These covariates were adjusted for in Model 2 and Model 3.
Ambient air pollution has been reported to be associated with increased odds of childhood eczema (8). Three main ambient air pollutants (PM10, SO2, and NO2) were selected to be adjusted for in Model 3. The daily mean concentrations of each air pollutant during 2008–2016 for each participant were obtained from 12 municipal monitoring stations for ambient air pollutants. Personal exposure to outdoor PM10, SO2, and NO2 was calculated by the inverse distance weighted (IDW) method (25).
We used binary logistic regression models to evaluate the associations of childhood eczema with dietary habits, residential/household environment, and lifestyle by adjusting for potential confounding covariates. Pearson's chi-square test was used to compare the differences in childhood eczema prevalence. Associations in the regression analysis were calculated as the odds ratio (OR) with a 95% confidence interval (95% CI). A P < 0.05 was considered statistically significant. First, a single-variable model was adopted to evaluate the crude ORs of residential/household environment and lifestyle for childhood eczema (Model 1). Second, parental atopy, breast feeding and the child's age, sex and birth season were adjusted in Model 2. Third, the effects of ambient air pollutants were further adjusted (Model 3). All statistical analyses were performed using SPSS software (version 18.0, SPSS Inc, Chicago, IL, USA).
This cross-sectional study is the first to systematically investigate the effects of living environment and lifestyle habits on childhood eczema in southern China. The effect of ambient air pollution was adjusted in the regression models. The results showed that diagnosed eczema among children was significantly associated with the residential/household environment, and lifestyles of their family members (Figure 2). However, we did not observe correlations between dietary factors and childhood DDE (P > 0.05), while fast food intake was found correlated with ELS (P < 0.05).
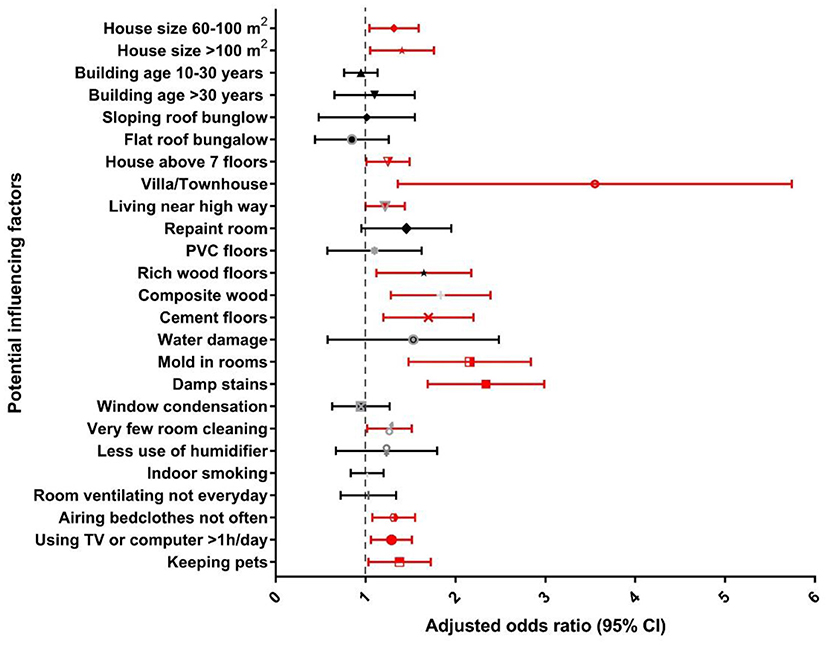
Figure 2. Associations between residential/household and lifestyle factors and diagnosed eczema among children in southern China.
The prevalence of childhood eczema according to the covariates is shown in Table 1. Among the 2,781 respondents, 685 (24.6%) had doctor-diagnosed eczema, and 859 (30.9%) had experienced ELS in the past 12 months. Children with parental atopy (P < 0.001) had the highest prevalence of childhood eczema (40.8% for diagnosed eczema, 46.1% for ELS). An age difference was observed in DDE prevalence among children, with the highest prevalence among children aged 3 years (29.0%). Notably, we did not find an association between childhood eczema and sex or breast feeding. In this study, the prevalence of eczema in children was comparable to those in other Chinese cities including Wuhan (23%), Shanghai (21.1%), Changsha (28.6%), and Beijing (29.7%) (8, 16, 19), and to those in developed countries, such as Spain (21.9%), Sweden (23.0%), and the United States (20.0%) (32–35), suggesting that atopic eczema is a widely distributed problem of public health.
The associations of eczema prevalence in children and residential/household environment and lifestyle habits obtained by the chi-square test are shown in Table 2. The prevalence of DDE and ELS was relatively high with the use of rich wood, composite wood, or cement as floor materials, the behavior of rarely cleaning the child's room, and the presence of mold or damp stains in the child's room (P ≤ 0.001). Repainting the child's room, house size, building age, house type, airing bedclothes, time spent watching TV/playing with a computer, and keeping pets at home also had a significant impact on the prevalence of childhood eczema (P ≤ 0.01), especially living in a villa/townhouse (47.4%).
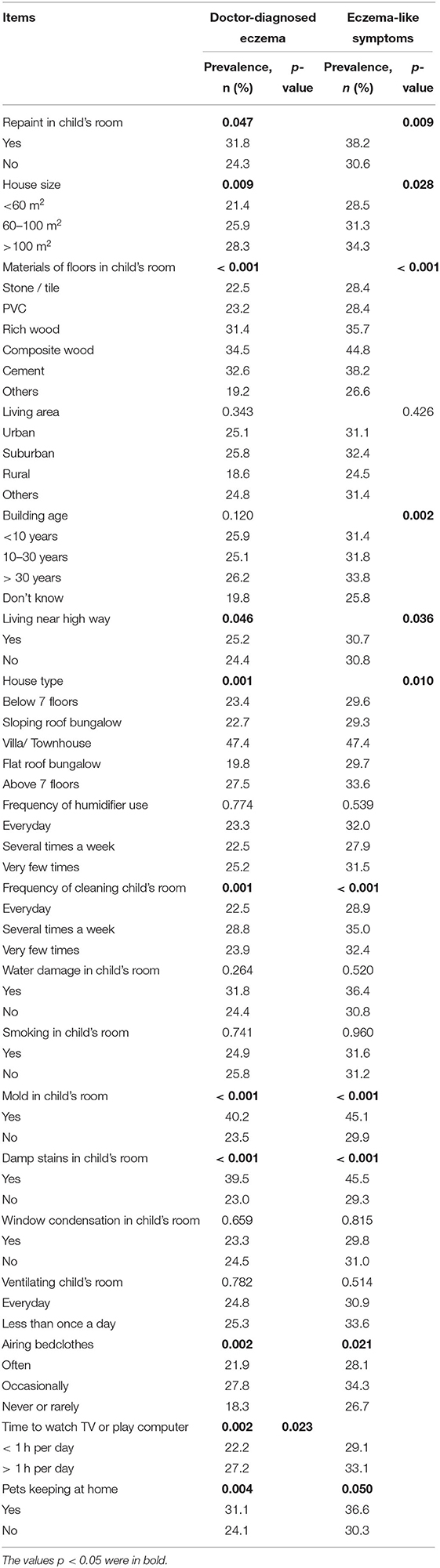
Table 2. Prevalence (%) of eczema or related symptoms stratified by residential/household environment and lifestyles (n = 2,781).
Table 3 showed the associations between current dietary habits and eczema prevalence in children. Children with higher frequencies of eating rice/pasta every week had a significantly increased prevalence of DDE and ELS (P < 0.05). In addition, a relatively high prevalence of both DDE and ELS was found among children who never eat fruits or vegetables, have a moderate intake of rice/pasta, and have a high intake of fast food. The prevalence of DDE was lower among children with a moderate intake of fruits (23.1%) or vegetables (22.1%). In addition, a moderate intake of vegetables had a significantly protective effect on DDE, which is consistent with previous studies (20, 21). A significant association was also found between a moderate intake of rice/pasta and an increased risk of ELS (adjusted OR, 95% CI = 1.34, 1.01–1.78), which agrees with a previous study (21). However, Cai (36) reported that fast food intake had a significantly protective effect on childhood eczema, as parents deliberately changed the original dietary habits of DDE-diagnosed children to avoid adverse risk factors for their children.
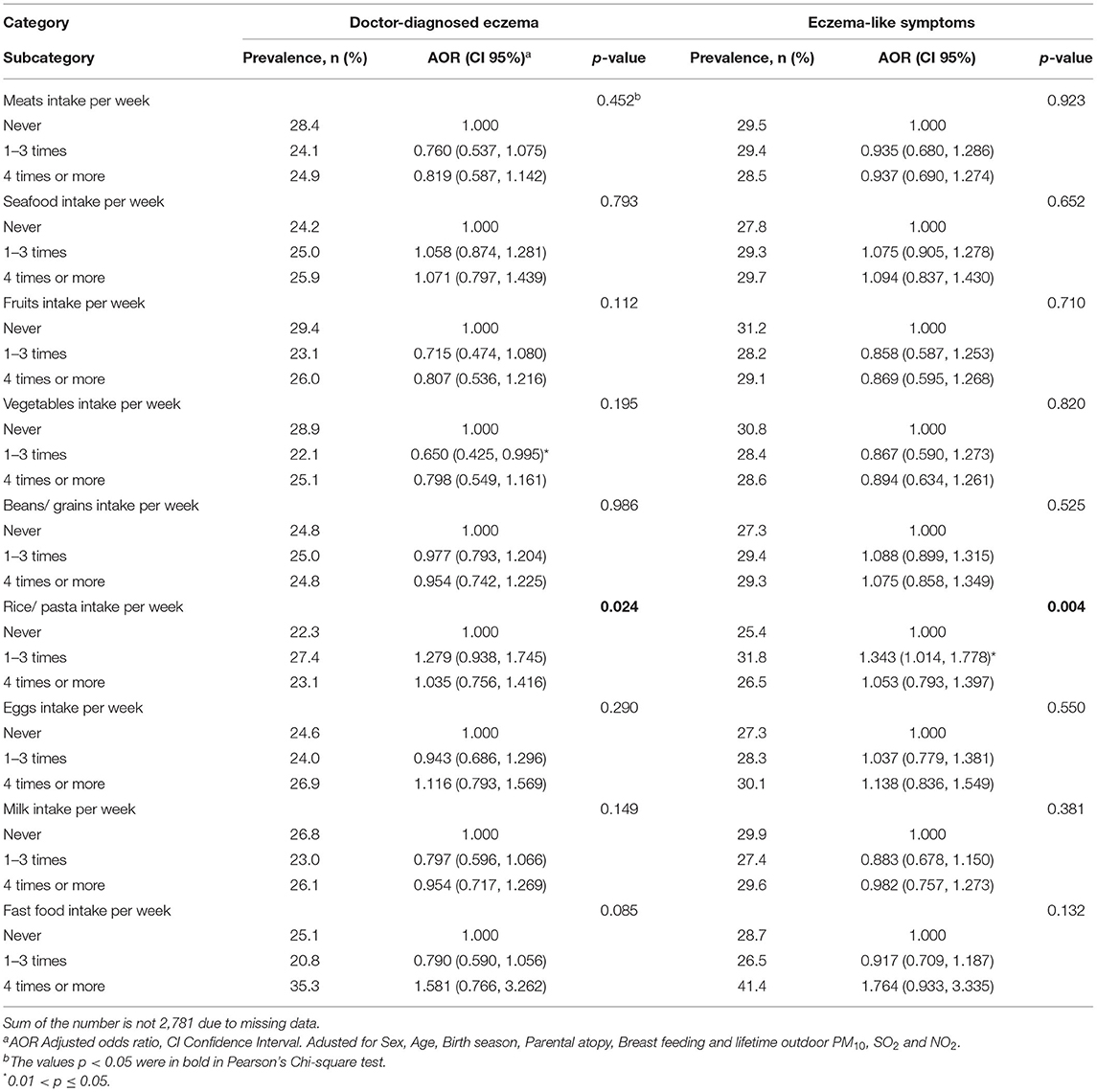
Table 3. Associations between dietary habits and eczema in children from southern China (n = 2,781).
Figures 2, 3 presents the adjusted odds ratio for DDE and ELS associated with residential/household and lifestyle factors, respectively. Specifically, for residential factors, living in a villa/townhouse (3.10, 1.62–5.95 for DDE; 2.16, 1.16–4.00 for ELS) or in a multistory building (1.23, 1.02–1.50 for DDE, 1.24, 1.04–1.47 for ELS) with more than seven floors was significantly associated with increased risk of childhood eczema. Living near a highway was also a risk factor for childhood eczema (1.20, 1.00–1.44 for DDE; 1.18, 1.00–1.39 for ELS). Moreover, living in a larger house (>100 m2) had a significant positive association with increased odds of childhood eczema (1.37, 1.07–1.77 for DDE; 1.29, 1.02–1.62 for ELS).
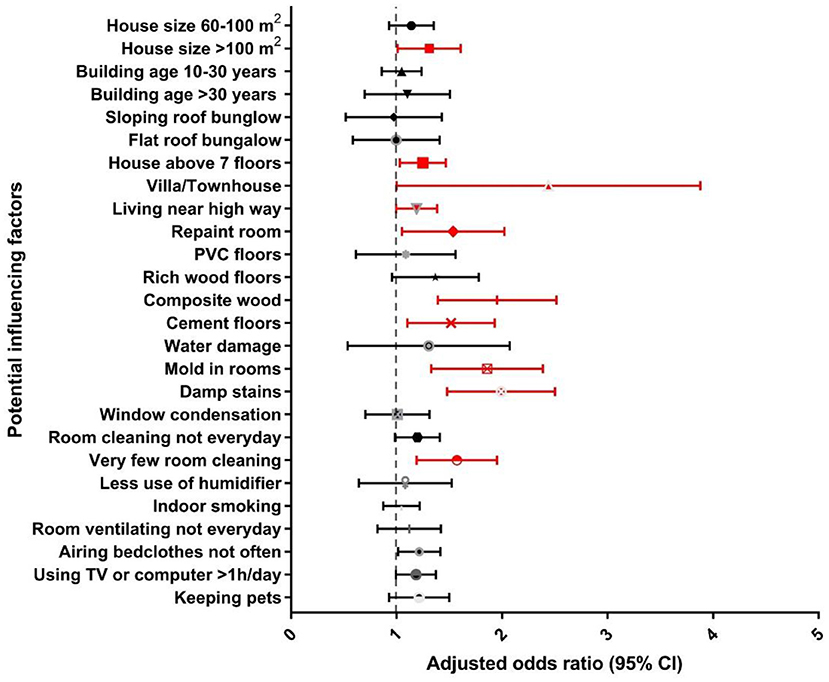
Figure 3. Associations between residential/household and lifestyle factors and eczema-like symptoms among children in southern China.
Residential characteristics may reflect the socio-economic status (SES) of a family indirectly and determine the type and degree of outdoor pollutants, which are closely related to childhood diseases (14, 37, 38). We found childhood eczema to have significant associations with residential characteristics, including size and type of house. After lifetime outdoor PM10 and SO2 were added to the confounders, living near a highway was found to be a risk factor for childhood eczema, and the larger the house, the higher the risk of DDE in children. Living in a multistory building of more than seven floors or in a villa/townhouse was significantly associated with an increased risk of childhood eczema, which is consistent with previous studies (16, 36, 39). Our report also suggested that living near a highway is a risk factor for childhood eczema after adjusting for all of the covariates, except for NO2, which is consistent with previous reports (15, 39). However, several studies in Taiyuan and Shanghai, China did not find significant associations between childhood eczema and living near a highway (40, 41). Further studies on these factors are needed.
In terms of household factors, compared with stone/tile, use of composite wood and cement as floor materials was significantly associated with increasing odds of childhood eczema (Figures 2, 3). Repainting the child's room was a risk factor for ELS (1.49, 1.08–2.04). Moreover, mold or damp stains in the child's room were very significantly associated with a higher prevalence of childhood eczema.
The household environment can also produce indoor pollution, which can affect childhood diseases (14). Our report suggested that repainting the child's room was significantly associated with an increased risk of ELS, which is consistent with a Russian study (42). In particular, the risk of childhood eczema was doubled with the presence of mold or damp stains in the child's room in all models, which is consistent with previous reports (43–46). Our study also found that using composite wood, rich wood, or cement as flooring material in the child's room was significantly associated with an increased risk of childhood eczema. The same results were obtained in Shanghai, China (36). These results may have occurred because composite wood, rich wood and cement materials have greater hygroscopicity (39), which will cause invisible micro-mildew, especially in the hot and humid city of Shenzhen. Fungi in the mildew could become allergens, stimulating the body to produce specific immunoglobulin E (IgE), and eventually causing allergic dermatitis such as eczema (47).
Lifestyle factors were also found to associated with DDE and ELS (Figures 2, 3). Rare cleaning of the child's room had a significant association with an increased risk of childhood eczema in all models (Model 3: 1.51, 1.16–1.98 for DDE and 1.18, 0.99–1.42 for ELS). The frequency of airing bedclothes and keeping pets at home were also risk factors for childhood eczema. Notably, we also found that too much time watching TV/playing with a computer (> 1 h per day) was significantly related to an increased risk of childhood eczema (1.27, 1.07–1.52 for DDE and 1.17, 1.00–1.38 for ELS).
We found that childhood eczema has significant associations with lifestyle, including frequency of cleaning the child's room and airing bedclothes, keeping pets at home, and the child's time spent watching TV/playing with a computer. These results are consistent with those reported from Shanghai and Japan; not cleaning children's rooms or airing bedclothes frequently increased the risk of eczema in children (36, 48). However, we also found that there was no significant association between childhood eczema and rarely airing bedclothes. This may be because parents may change their cleaning habits when their children develop symptoms of eczema, inadvertently engaging in the protective factors that are beneficial to children's health. Another study, in Baotou city, showed that use of a humidifier increased the prevalence of childhood eczema (49). However, our results are consistent with those reported from Shanghai, with no association found between humidifiers and eczema (36). This result is probably because the climate in southern cities is always humid. Keeping pets at home was also significantly associated with an increased risk of childhood eczema, which coincided with a previous report (22). Notably, we also found another interesting result that spending too much time watching TV/playing with a computer was significantly associated with an increased risk of DDE. Despite the lack of a firm explanation for this observation, exposure time to electronic products might be inversely linked to time engaged in exercise.
The environmental pathogenic mechanisms of eczema in children may be multifaceted and have not been fully understood, which may be related to the dysregulation of cytokines and inflammatory mediators directly or indirectly induced by chronic exposure to xenobiotics (50–52). Besides, evidence have proved that indoor exposure to exogenous microbiota may alter intestinal microbiota in children, and thus regulate the immunological functions (53–55). In addition, indoor wood materials and coating on the walls may release organic pollutants such as organophosphates or brominated flame retardants, which may also exert hazardous effects on gut microbiota and potentially impair immune systems (56, 57). Nevertheless, complete skin barriers are crucial to prevent the occurrence of eczema (58), while the use of humidifiers and keeping pets at home may bring a risk to weaken the stratum corneum. We also found that eating fast food may be an influencing factor, which may be due to altered intestinal microbiota, or the intake of fatty acid and concomitant inflammation (59, 60).
The present study had some strengths. Above all, this study had a relatively large sample size, representing children in the general population. In addition, the response rate of the questionnaires was high (98%), which ensured the reliability and consistency of the results. Furthermore, the questions on atopic eczema in our study were taken from the ISAAC study (61), which was validated in previous worldwide studies (62). Nevertheless, several limitations also existed in this study. First, limited by the cross-sectional design, a cause-effect relationship could not be established. Second, information on ELS mainly came from the observations of parents, and the definition of ELS was more general in the questionnaire than in a clinical setting. Therefore, the prevalence of eczema may be overestimated. Third, the significant associations presented in this study could still be confounded by other factors. For example, some of these significant associations may disappear if the SES of the parents were included in the models. Another limitation in study design is the sensitization status of the study subjects is not considered. Besides, eczema is a strongly genetic disease with environment acting as the precipitating factor, while gene-environment interaction was not included in this study, which warrants further investigation.
Our study indicated significant associations between childhood eczema and both living environment and lifestyle habits after adjusting for covariates including the child's sex, age, and birth season, parental atopy, breast feeding, and ambient air pollution, with lifetime outdoor PM10/SO2/NO2 values. Floor materials, repainting, house size and type, living near a highway, the frequency of cleaning the child's room and airing bedclothes, mold or damp stains in the child's room, pet-keeping at home, time spent watching TV/playing with a computer, and a moderate intake of rice/pasta were found to be risk factors for childhood eczema. A moderate intake of vegetables and fruits could decrease the risk of childhood eczema. Parents and kindergarten staff should make an attempt to avoid giving their children too many electronics-based tasks and create a low risk living environment for children during their growth stage.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Shenzhen Institute of Information Technology. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
YL: investigation, data analysis, and writing. SS: investigation and writing—reviewing and editing. DZ: writing—reviewing and editing. WL: data analysis. ZD and SL: supervision. All authors contributed to the article and approved the submitted version.
This work was supported by the Shenzhen Science and Technology Project (JCYJ20180307160045548 and JSGG20180504165551779), Research platform and projects of the education department of Guangdong province (2018GKTSCX063), and with the subject of Shenzhen Institute of Information Technology (HX-227 and SZIIT2020KJ004).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We gratefully acknowledge all the participating children and their parents, as well as the co-operation and contribution of each kindergarten. We also highly appreciate all the teachers and students for their great effort and hard work in this research.
1. Leung DY, Bieber T. Atopic dermatitis. Lancet. (2003) 361:151–60. doi: 10.1016/S0140-6736(03)12193-9
2. Williams H, Stewart A, von Mutiu E, Cookson W, Anderson HR. Is eczema really on the increase worldwide? J Allergy Clin Immunol. (2008) 121:947–54. doi: 10.1016/j.jaci.2007.11.004
3. Fishbein AB, Mueller K, Kruse L, Boor P, Sheldon S, Zee P, et al. Sleep disturbance in children with moderate/severe atopic dermatitis: a case-control study. J Am Acad Dermatol. (2018) 78:336–41. doi: 10.1016/j.jaad.2017.08.043
4. Flohr C. Recent perspectives on the global epidemiology of childhood eczema. Allergol Immunopathol. (2011) 39:174–82. doi: 10.1016/j.aller.2011.02.004
5. Anderson HR, Ruggles R, Pandey KD, Kapetanakis V, Brunekreef B, Lai CK, et al. Ambient particulate pollution and the world-wide prevalence of asthma, rhino-conjunctivitis and eczema in children: Phase One of the International Study of Asthma and Allergies in Childhood (ISAAC). Occup Environ Med. (2010) 67:293–300. doi: 10.1136/oem.2009.048785
6. Chung KA, Zhang JF, Zhong NS. Outdoor air pollution and respiratory health in Asia. Respirol. (2011) 16:1023–6. doi: 10.1111/j.1440-1843.2011.02034.x
7. Stewart AW, Mitchell EA, Pearce N, Strachan DP, Weiland SK. The relationship of per capita gross national product to the prevalence of symptoms of asthma and other atopic diseases in children (ISAAC). Int J Epidemiol. (2001) 30:173–9. doi: 10.1093/ije/30.1.173
8. Lu C, Deng L, Ou C, Yuan H, Chen X, Deng. Preconceptional and perinatal exposure to traffic-related air pollution and eczema in preschool children. J Dermatol Sci. (2016) 85:85–95. doi: 10.1016/j.jdermsci.2016.11.004
9. Weschler CJ. Changes in indoor pollutants since the 1950s. Atmos Environ. (2009) 43:153–69. doi: 10.1016/j.atmosenv.2008.09.044
10. Williams H, Flohr C. How epidemiology has challenged 3 prevailing concepts about atopic dermatitis. J Allergy Clin Immunol. (2006) 118:209–13. doi: 10.1016/j.jaci.2006.04.043
11. Xu F, Yan S, Li F, Cai M, Chai W, Wu M, et al. Prevalence of childhood atopic dermatitis: an urban and rural community-based study in Shanghai, China. PLoS ONE. (2012) 7:e36174. doi: 10.1371/journal.pone.0036174
12. Zhang Y, Li B, Huang C, Yang X, Qian H, Deng Q, et al. Ten cities cross-sectional questionnaire survey of children asthma and other allergies in china. Chin Sci Bull. (2013) 58, 4182–4189. doi: 10.1007/s11434-013-5914-z
13. Herbarth O, Fritz GJ, Rehwagen M, Richter M, Röder S, Schlink U. Association between indoor renovation activities and eczema in early childhood. Int J Hyg Environ Health. (2006) 209:241–7. doi: 10.1016/j.ijheh.2006.01.003
14. Liu W, Huang C, Hu Y, Zou Z, Shen L, Sundell J. Associations of building characteristics and lifestyles with home dampness-related exposures in Shanghai dwellings. Build Environ. (2015) 88:106–15. doi: 10.1016/j.buildenv.2014.10.028
15. Robinson CL, Baumann LM, Romero K, Combe JM, Gomez A, Gilman RH, et al. Effect of urbanisation on asthma, allergy and airways inflammation in a developing country setting. Thorax. (2011) 66:1051–7. doi: 10.1136/thx.2011.158956
16. Zhang M, Wu Y, Yuan Y, Zhou E, Sundell J, Sun Y, et al. Effects of home environment and lifestyles on prevalence of atopic eczema among children in Wuhan area of China. Chinese Sci Bull. (2013) 58:4217–22. doi: 10.1007/s11434-013-5685-6
17. Choi J, Chun C, Sun Y, Choi Y, Kwon S, Bornehag C, et al. Associations between building characteristics and children's allergic symptoms—A cross-sectional study on child's health and home in Seoul, South Korea. Build Environ. (2014) 75:176–81. doi: 10.1016/j.buildenv.2014.01.019
18. Sun Y, Hou J, Kong X, Zhang Q, Wang P, Weschler LB, et al. “Dampness” and “Dryness”: What is important for children's allergies? A cross-sectional study of 7366 children in northeast Chinese homes. Build Environ. (2018) 139:38–45. doi: 10.1016/j.buildenv.2018.05.013
19. Norbäck D, Lu C, Zhang Y, Li B, Zhao Z, Huang C, et al. Sources of indoor particulate matter (PM) and outdoor air pollution in China in relation to asthma, wheeze, rhinitis and eczema among pre-school children: Synergistic effects between antibiotics use and PM[[sb]]10[[/s]] and second hand smoke. Environ Int. (2019) 125:252–60. doi: 10.1016/j.envint.2019.01.036
20. Andrusaityte S, Grazuleviciene R, Petraviciene I. Effect of diet and maternal education on allergies among preschool children: a case-control study. Environ Res. (2017) 159:374–80. doi: 10.1016/j.envres.2017.08.020
21. Cai J, Liu W, Hu Y, Zou Z, Shen L, Huang C. Household environment, lifestyles, and dietary habits in relation to childhood atopic eczema in Shanghai, China. Int Arch Occup Environ Health. (2016) 90:141–59. doi: 10.1007/s00420-016-1177-8
22. Clayton T, Asher MI, Crane J, Ellwood P, Mackay R, Mitchell EA, et al. Time trends, ethnicity and risk factors for eczema in New Zealand children: ISAAC Phase Three. Asia Pac Allergy. (2013) 3:161–78. doi: 10.5415/apallergy.2013.3.3.161
23. Galazzo G, van Best N, Bervoets L, Dapaah IO, Savelkoul PH, Hornef MW, et al. Development of the microbiota and associations with birth mode, diet, and atopic disorders in a longitudinal analysis of stool samples, collected from infancy through early childhood. Gastroenterol. (2020) 158:1584–96. doi: 10.1053/j.gastro.2020.01.024
24. Ehlayel MS, Bener A. Duration of breast-feeding and the risk of childhood allergic diseases in a developing country. Allergy Asthma Proc. (2008) 29:386–91. doi: 10.2500/aap.2008.29.31387
25. Deng Q, Lu C, Norbäck D, Bornehag C, Zhang Y, Liu W, et al. Early life exposure to ambient air pollution and childhood asthma in China. Environ Res. (2015) 143:83–92. doi: 10.1016/j.envres.2015.09.032
26. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. (2006) 368:733–43. doi: 10.1016/S0140-6736(06)69283-0
27. Bornehag C, Sundell J, Sigsgaard T. Dampness in buildings and health (DBH): Report from an ongoing epidemiological investigation on the association between indoor environmental factors and health effects among children in Sweden. Indoor Air. (2004) 14:59–66. doi: 10.1111/j.1600-0668.2004.00274.x
28. Alvarez Zalloa N, Aguinaga-Ontoso I, Alvarez-Alvarez I, Marin-Fernandez B, Guillén-Grima F, Azcona-San Julián C. Influence of the Mediterranean diet during pregnancy in the development of wheezing and eczema in infants in Pamplona, Spain. Allergol Immunopathol. (2017) 46:9–14. doi: 10.1016/j.aller.2017.02.009
29. Blattner CM, Murase JE. A practice gap in pediatric dermatology: Does breast-feeding prevent the development of infantile atopic dermatitis? J Am Acad Dermatol. (2014) 71:405–6. doi: 10.1016/j.jaad.2014.01.868
30. Nurmatov U, Nwaru BI, Devereux G, Sheikh A. Confounding and effect modification in studies of diet and childhood asthma and allergies. Allergy. (2012) 67:1041–59. doi: 10.1111/j.1398-9995.2012.02858.x
31. Qu F, Weschler LB, Sundell J, Zhang Y. Increasing prevalence of asthma and allergy in Beijing pre-school children: Is exclusive breastfeeding for more than 6 months protective? Chin Sci Bull. (2013) 58:4190–202. doi: 10.1007/s11434-013-5790-6
32. Aguilera I, Pedersen M, Garcia-Esteban R, Ballester F, Basterrechea M, Esplugues A, et al. Early-life exposure to outdoor air pollution and respiratory health, ear infections, and eczema in infants from the INMA study. Environ Health Perspect. (2012) 121:387–92. doi: 10.1289/ehp.1205281
33. Bolat E, Arikoglu T, Sungur MA, Batmaz SB, Kuyucu S. Prevalence and risk factors for wheezing and allergic diseases in preschool children: a perspective from the Mediterranean coast of Turkey. Allergol Immunopathol. (2017) 45:362–8. doi: 10.1016/j.aller.2017.01.002
34. Bornehag C, Sundell J, Hagerhed-Engman L, Sigsggard T, Janson S, Aberg N. ‘Dampness’ at home and its association with airway, nose, and skin symptoms among 10,851 preschool children in Sweden: a cross-sectional study. Indoor Air. (2005) 15:48–55. doi: 10.1111/j.1600-0668.2005.00306.x
35. Sun Y, Sundell J. Life style and home environment are associated with racial disparities of asthma and allergy in Northeast Texas children. Sci Total Environ. (2011) 409:4229–34. doi: 10.1016/j.scitotenv.2011.07.011
36. Cai J. The Associations of Home Dampness-related Indicators and Bed Dust Mites with Childhood Eczema. Shanghai, China: University of Shanghai for Science & Technology. (2017).
37. Hägerhed-Engman L, Bornehag C, Sundell J. Building characteristics associated with moisture related problems in 8,918 Swedish dwellings. Int J Environ Health Res. (2009) 19:251–65. doi: 10.1080/09603120802527653
38. Keet CA, McCormack MC, Pollack CE, Peng RD, McGowan E, Matsui EC. Neighborhood poverty, urban residence, race/ethnicity, and asthma: rethinking the inner-city asthma epidemic. J Allergy Clin Immunol. (2015) 135:655–62. doi: 10.1016/j.jaci.2014.11.022
39. Liu W. Effects of household environment and indoor ventilation on childhood airway and allergic diseases. Shanghai, China: University of Shanghai for Science & Technology. (2017).
40. Chang J, Liu W, Hu Y, Zou Z, Shen L, Wang X, et al. Associations between heavy traffic near residence and childhood health outcomes as modified by bedroom floor level and bedroom ventilation. Build Environ. (2017) 114:56–67. doi: 10.1016/j.buildenv.2016.12.014
41. Li CH. The association between indoor environmental exposure and allergic symptoms such as asthma among preschool children. Taiyuan, China: Shanxi University. (2019).
42. Jaakkola JJ, Parise H, Kislitsin V, Lebedeva NI, Spengler JD. Asthma, wheezing, and allergies in russian schoolchildren in relation to new surface materials in the home. Am J Public Health. (2004) 94:560–2. doi: 10.2105/AJPH.94.4.560
43. Cai J, Liu W, Hu Y, Zou Z, Shen L, Huang C. Associations between home dampness-related exposures and childhood eczema among 13,335 preschool children in Shanghai, China: a cross-sectional study. Environ Res. (2016) 146:18–26. doi: 10.1016/j.envres.2015.12.009
44. Taylor-Robinson DC, Williams H, Pearce A, Law C, Hope S. Do early-life exposures explain why more advantaged children get eczema? Findings from the U.K. Millennium Cohort Study Br J Dermatol. (2016) 174:569–78. doi: 10.1111/bjd.14310
45. Wang J, Zhao Z, Zhang Y, Li B, Huang C, Zhang X, et al. Asthma, allergic rhinitis and eczema among parents of preschool children in relation to climate, and dampness and mold in dwellings in China. Environ Int. (2019) 130:104910. doi: 10.1016/j.envint.2019.104910
46. Zhao Z, Zhang X, Liu R, Norback D, Wieslander G, Chen J, et al. Prenatal and early life home environment exposure in relation to preschool children's asthma, allergic rhinitis and eczema in Taiyuan, China. Chin Sci Bull. (2013) 58:4245–51. doi: 10.1007/s11434-013-5705-6
47. Gaitanis G, Magiatis P, Hantschke M, Bassukas ID, Velegraki A. The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev. (2012) 25:106–41. doi: 10.1128/CMR.00021-11
48. Miyake Y, Ohya Y, Tanaka K, Yokoyama T, Sasaki S, Fukushima W, et al. Home environment and suspected atopic eczema in Japanese infants: the Osaka Maternal and Child Health Study. Pediatr Allergy Immunol. (2007) 18:425–32. doi: 10.1111/j.1399-3038.2007.00545.x
49. Wang LF, Huang XY, Sundell J, He LJ, Jin G, Zhang YP. Impact of home humidifier on children's eczema (in Chinese). Chin Sci Bull. (2016) 61:1721–7. doi: 10.1360/N972015-01335
50. Datsi A, Steinhoff M, Ahmad F, Alam M, Buddenkotte J. Interleukin-31: The “itchy” cytokine in inflammation and therapy. Allergy. (2021) 76:2982–97. doi: 10.1111/all.14791
51. Han X, Krempski JW, Nadeau K. Advances and novel developments in mechanisms of allergic inflammation. Allergy. (2020) 75:3100–11. doi: 10.1111/all.14632
52. Rojahn TB, Vorstandlechner V, Krausgruber T, Bauer WM, Alkon N, Bangert C, et al. Single-cell transcriptomics combined with interstitial fluid proteomics defines cell type-specific immune regulation in atopic dermatitis. J Allergy Clin Immunol. (2020) 146:1056–69. doi: 10.1016/j.jaci.2020.03.041
53. Fujimura KE, Demoor T, Rauch M, Faruqi AA, Jang S, Johnson CC, et al. House dust exposure mediates gut microbiome Lactobacillus; enrichment and airway immune defense against allergens and virus infection. Proc Natl Acad Sci U S A. (2014) 111:805. doi: 10.1073/pnas.1310750111
54. Konya T, Koster B, Maughan H, Escobar M, Azad MB, Guttman DS, et al. Associations between bacterial communities of house dust and infant gut. Environ Res. (2014) 131:25–30. doi: 10.1016/j.envres.2014.02.005
55. Ta L, Tay C, Lay C, de Sessions PF, Tan C, Tay M, et al. Household environmental microbiota influences early-life eczema development. Environ Microbiol. (2021) 23:7710–22. doi: 10.1111/1462-2920.15684
56. Roman P, Cardona D, Sempere L, Carvajal F. Microbiota and organophosphates. Neurotoxicology. (2019) 75:200–8. doi: 10.1016/j.neuro.2019.09.013
57. Yasmin S, Whalen M. Flame retardants, hexabromocyclododecane (HCBD) and tetrabromobisphenol a (TBBPA), alter secretion of tumor necrosis factor alpha (TNFα) from human immune cells. Arch Toxicol. (2018) 92:1483–94. doi: 10.1007/s00204-018-2156-5
58. Kelleher MM, Cro S, Cornelius V, Lodrup Carlsen KC, Skjerven HO, Rehbinder EM, et al. Skin care interventions in infants for preventing eczema and food allergy. Cochrane Database Syst. Rev. (2021) 2:CD013534. doi: 10.1002/14651858.CD013534.pub2
59. Neerven R, Savelkoul H. Nutrition and allergic diseases. Nutrients. (2017) 9:762. doi: 10.3390/nu9070762
60. Rutter CE, Silverwood RJ, Williams HC, Ellwood P, Asher I, Garcia-Marcos L, et al. Are environmental factors for atopic eczema in ISAAC phase three due to reverse causation?. J. Invest. Dermatol. (2019) 139:1023–1036. doi: 10.1016/j.jid.2018.08.035
61. Weiland SK, Bjorksten B, Brunekreef B, Cooksonz W, von Mutius E, Strachan DP. Phase II of the International Study of Asthma and Allergies in Childhood (ISAAC II): rationale and methods. Eur Respir J. (2004) 24:406–12. doi: 10.1183/09031936.04.00090303
Keywords: atopic eczema, children, dietary habits, residential/household environment, lifestyle
Citation: Liu Y, Sun S, Zhang D, Li W, Duan Z and Lu S (2022) Effects of Residential Environment and Lifestyle on Atopic Eczema Among Preschool Children in Shenzhen, China. Front. Public Health 10:844832. doi: 10.3389/fpubh.2022.844832
Received: 28 December 2021; Accepted: 27 April 2022;
Published: 16 May 2022.
Edited by:
Atin Adhikari, Georgia Southern University, United StatesReviewed by:
Wei Yu, Chongqing University, ChinaCopyright © 2022 Liu, Sun, Zhang, Li, Duan and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenya Duan, enlkdWFuQDE2My5jb20=; Shaoyou Lu, bHVzaHkyM0BtYWlsLnN5c3UuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.