- 1The Centre for Modern Chinese City Studies, Research Center for China Administrative Division, Future City Lab, East China Normal University, Shanghai, China
- 2Faculty of Environmental Science and Engineering, Kunming University of Science and Technology, Kunming, China
- 3Department of Urban Development and Mobility, Luxembourg Institute of Socio-Economic Research (LISER), Esch-sur-Alzette, Luxembourg
- 4Faculty of Land Resource Engineering, Kunming University of Science and Technology, Kunming, China
Aim: Evidence on the association between natural-built environments and depression is largely derived from the general population and prone to residential self-selection bias because of the nature of cross-sectional research design. Despite emerging adulthood, which includes the university years, is a critical stage for forming life-long health habits, studies on this topic focusing on undergraduate students are limited. The current study aims to illustrate the underlying mechanisms for how the campus-based environments affect depression in undergraduate students.
Methods: Based on a nationwide representative analytical sample of 22,009 Chinese undergraduates in 2018, we examined participants' reports of depression and campus-centered natural/built environments within multiple buffer sizes including 0.5, 1.0, and 2.5 km. After disentangling residential self-selection, we explored the moderating role of the socioeconomic attributes of undergraduates. The depression outcome was measured by the nine-item Patient Health Questionnaire (PHQ9). Indicators of exposure to green and blue space, transportation infrastructure, and food environments were objectively assessed using different circular buffers around each campus address.
Results: Modeling results indicated that campus neighborhoods with more scattered trees (0.5 km), water (0.5, 1.0, and 2.5 km), and street intersections (1.0 and 2.5 km) were protective against depression. In contrast, those living near denser distributions of outlets serving take-away sweets and fast food (0.5, 1.0, and 2.5 km) were susceptible to depression. These associations were modified by undergraduates' socioeconomic attributes (e.g., grade, Hukou status, and ethnicity) and varied according to geographical scales and exposure metrics.
Conclusion: To deliver effective environmental interventions to curb the prevalence of depression among undergraduate students, further planning policies should focus on the careful conception of the campus-based environment, especially regarding different spatial scales.
Background
The university period is a critical stage of emerging adulthood (1) during which time individuals are often faced with increasing expectations from their families and society. When there is a perceived failure to meet these expectations, the onset of common mental disorders, such as depression, and risky behaviors, such as suicide, may arise (2, 3). Depression is prevalent among university students in many regions of the world (2, 4, 5) and affects the quality of life, relationships, academic attachment, and work opportunities of many students (6). Many studies reported over 30% of university students suffer from depression (2, 5), which is much higher than global and national levels in China (6, 7). The latest report on national mental health development in China (2019–2020) reported that roughly 18.5% university students were depressed with depressive scores (assessed by the Center for Epidemiological Studies Depression Scale, CES-D) ranging from 10 to 17, and 4.2% of other university students are at high risk of depression with CES-D scores over 17 (8). To respond to the high prevalence and well-documented negative effects of depression in university students, depression screening and prevention have attracted the attention of policy-makers.
The high prevalence rate of depression could be attributed to biological characteristics and external environmental factors, including social, natural, and built components of the environment (2, 9). Unlike adolescents, biologically, most university students are at a point in emerging adulthood where they “have reached physical and sexual maturity, and are highly diverse in their educational and occupational combinations and trajectories, p. 569” (1). In contrast with adults, the majority of university students are not yet in stable long-term romantic or career commitments (1). Consequently, most university students often experience stress, anxiety, and depression (2, 5, 10–12). In addition, most undergraduates in China live and learn on campuses with unique environments and corresponding management modes (12). To mitigate students' living expenditures and facilitate student management, universities typically offer or compel students to live in the low-cost dormitories within or near the campus (13). As a result, undergraduates have hardly any freedom to choose their residences (14). In addition, students perform most of their daily routines (e.g., learning, living, eating, etc.) within or surrounding these campuses (12). Given these factors, there are grounds to explore the implications of campus environment on the mental status of students.
Numerous studies have associated geriatric, adolescent, and pre-natal depression with exposure to natural and built environments (NBEs), especially in regards to the residential and working neighborhoods that are central to people's daily activities (15–20). However, little is known regarding depression in undergraduates in this context. The theoretical and empirical evidence points to the potential of NBEs to reshape depression-related behaviors, including physical activities, social contacts, etc., but their effects on depression itself remains mixed when it comes to different environmental variables and populations (21). Natural spaces, especially green spaces show potential to reduce depressive moods (19, 22–24) and improve mental health (25, 26) through stress relief (11), physical activity (PA) (27, 28), and social cohesion (24, 29). Most existing findings relevant for human benefits in relation to depression have been associated with generalized greenness (commonly captured by the normalized difference vegetation index [NDVI] or by overall greenery coverage) (19, 24, 26, 30), and very few studies have focused on specific types of green spaces (31–33). As reported, the associations between depression/depression-related behaviors and greens spaces differ depending on the type of green space concerned (34, 35). For instance, Giles-Corti et al. suggested the positive effects of flat grassy areas on facilitating social and physical recreation, but not walking, in older adults (34), whereas Holtan et al. associated social capital increase with the presence of tree canopies but not the presence of parks and grass (35). Built environments are broadly defined as human-made facilities and infrastructures for supporting human activities (25). Based on Ewing and Cervero's “5D” model (36), over 100 objective measures of built environments can be used to understand the relationship between built environment and mental health (37). Among these measures, food facilities and road/street environments are closely related to students' daily activities. Road/street environments are more likely to be related to physical activity (38), and food facilities are more likely to change dietary patterns (39), both of which could affect depression (40–42).
Although there is growing scientific recognition of the effect of NBEs on depression and depression-related behaviors (15, 19, 23, 38), there are still some limitations to investigating the relationships between campus environments and depression in undergraduates. First, there is limited relevant research regarding undergraduates who live in distinctive environments and take part in unique daily activities (12, 13). Second, few studies have been performed to examine how depression is correlated with different types of green spaces, which is meaningful to urban planning and decision-making (30, 31). In addition, residential self-selection bias (43–45) and the uncertain geographic context problem (46, 47) both affect research in this field. Residential self-selection implies that participants are likely to choose their neighborhood according to their lifestyle and personal preferences, so those who are healthy, or want to be healthy, may choose to live in a neighborhood with better environmental quality (e.g., places with greener spaces and better walkability) (44, 45). This kind of bias can affect the relationship between health outcomes and exposure to such environments (44, 45), but has rarely been addressed in previous studies (16, 24, 26). Investigating a subgroup population with little freedom to choose their residential location is recommended as an effective solution to mitigate this type of bias because of the high cost for longitudinal and (quasi) experimental research and the difficulties in distinguishing preferences and attitudes (14, 45). To relieve cost and ensure the safety of students, Chinese universities offer dormitories within or near the campus at which residence is compulsory (13), thereby constraining their choices of where to live and restricting most of their routine activities (i.e., learning, playing sports, eating, and living) within the campus environment (12). The uncertainty of geographic context is another undeniable problem relevant to environmental health (46, 47). The measures of exposure to NBEs varies with the definition of neighborhood (i.e., buffer sizes, buffer shapes, etc.), causing mixed findings regarding the relationship between NBEs and depression (38, 48). Empirically, multiple-scale environmental measures have been captured to solve this issue (38, 48).
Last but not least, individual socio-economic status (SES), such as gender, ethnicity, age, education status, and economic condition, have been reported to moderate the association between NBEs and depression (18, 19, 48), and the moderating roles are reported to differ in varying populations. For instance, green spaces are protective against depression among low-educated pregnant women, but this moderating role is not significant for their children's mental wellbeing (48, 49). Therefore, it is necessary to examine the moderating role of individual attributes on this association among undergraduates. Further, this is conducive to identifying subgroups for whom interventions to change the NBEs might be the most effective.
Given the above gaps in the literature (25, 30) and the daily routines of undergraduates in China (see Supplementary Figure 1), a conceptual framework (Figure 1) was proposed to illustrate the underlying mechanisms for how the campus-based environments affect depression. Subsequently, a nationwide representative sample of 22,009 undergraduates from 89 campuses across China was used to examine the associations between depression in undergraduates and campus-centered natural-built environments at multiple spatial scales (i.e., 0.5, 1, and 2.5 km)1. The moderating role of individual socioeconomic attributes was examined after RSS was disentangled. This study contributes to the literature in five aspects: First, it is the original attempt to relate the incidence of depression in undergraduates to NBEs within and surrounding campus environments where undergraduates' living and working conditions are combined (after controlling for RSS bias). Second, this study enhances our understanding of how different types of green spaces affect depression. Third, the uncertainty of geographic contexts is compared at multiple geographical scales (0.5, 1, and 2.5 km). Fourth, the association between NBEs and depression are not confounded by residential self-selection bias in this study. Finally, the individual-based moderating role of environment-depression associations among undergraduates is clarified through interaction analysis.
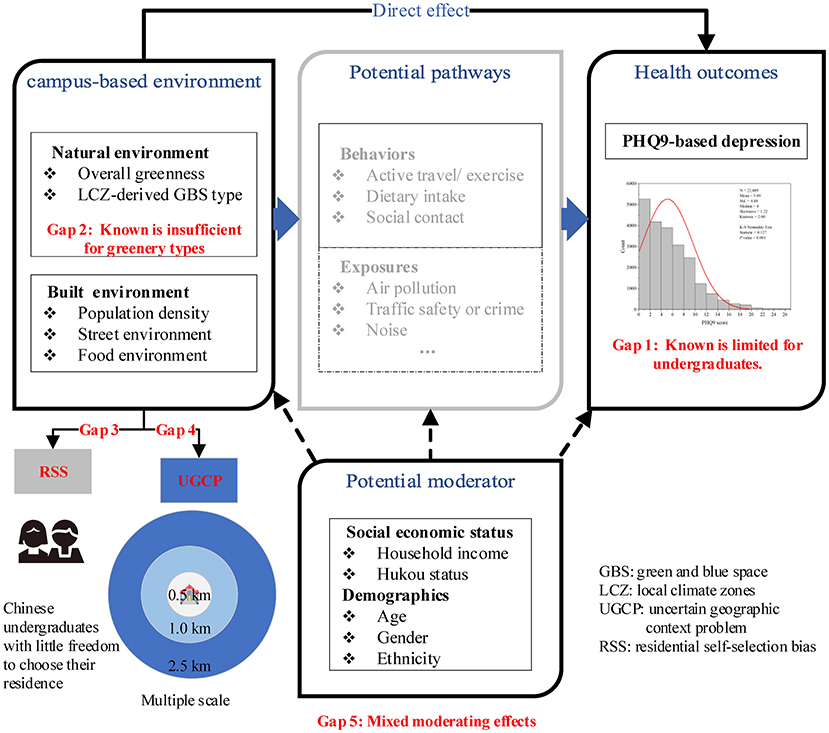
Figure 1. Conceptual framework illustrating how campus-based environmental factors affect depression.
Methods and Data
Data
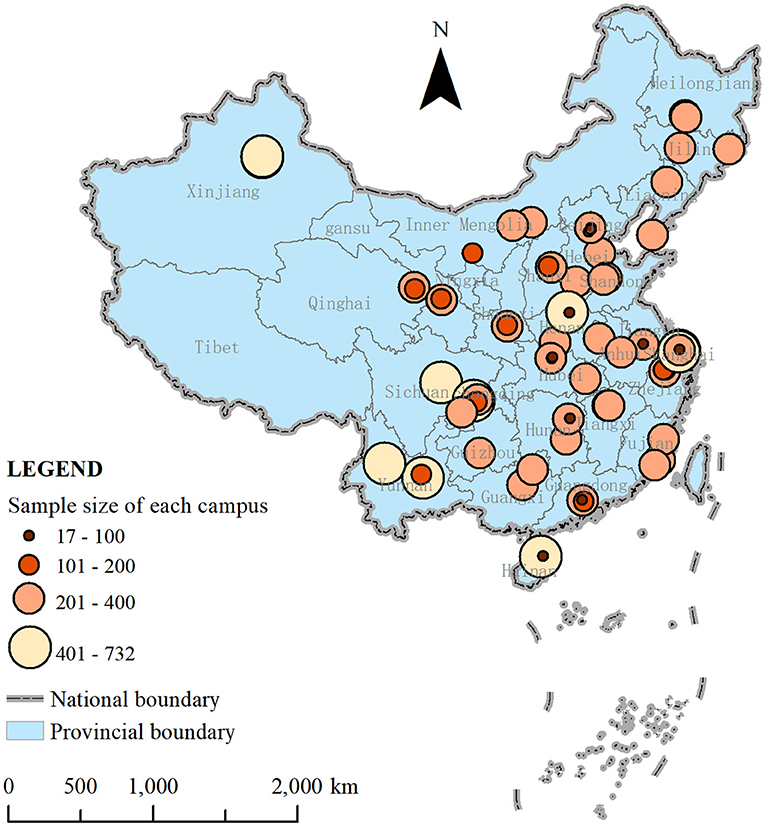
In this study, individual information was derived from a nationwide university-based survey on Chinese undergraduates conducted in 2018 (Ethics No. 2018-L-25). Using a stratified, multiple-stage cluster sample design, the research team generated a representative sample of 23,488 undergraduates from 90 campuses in 29 provincial units (Figure 2) after excluding 192 participants owing to missing data.
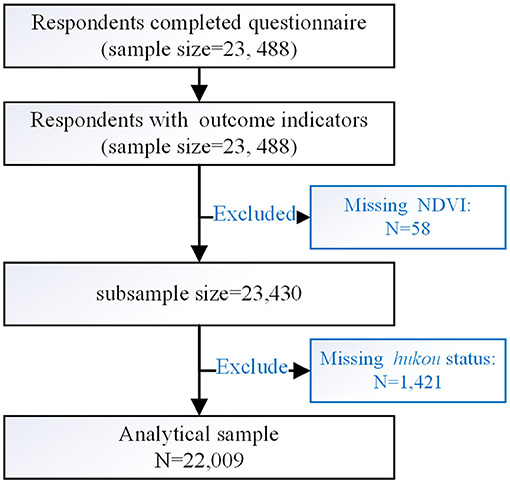
A structured questionnaire—designed by a multidisciplinary expert panel consisting of experienced epidemiologists and healthcare professionals—was used to collect data including socioeconomic characteristics, patterns of trips for routine activities, and health status. A set of natural and built environmental measurements was extracted by the GIS method according to the geocoded address of the campuses. According to prior studies (37, 50) and the transportation distances of participants (Supplementary Figure 1), functional neighborhoods were created for three distances of 0.5, 1, and 2.5 km. After excluding respondents with missing NDVI (n = 58) and Hukou status (n = 1,421), the final analytical sample comprised 22,009 respondents from 89 campuses (Figure 3).
Outcome
Depression severity was measured by the nine-item Patient Health Questionnaire (PHQ9, Supplementary Table 1) (51), one of the most widely used tools to measure depression severity for the previous 2 weeks in non-clinical populations (19, 52). This scale has been verified in the Chinese general population (53). Each item is scored from 0 to 3, and the sum scores could range from 0 to 27 (Supplementary Figure 2), with higher scores indicating more severe depression. The sum scores of PHQ9 < 5 is usually recognized as minimal or no depression (2, 51).
Environmental Exposure
Natural Environments
Empirical evidence on impact of NDVI on depression is conclusive (19, 20, 54); however, which type of green space has a greater effect on depression is not yet well-understood (30, 31). In this paper, we focus on the benefits of NDVI and five types of urban natural features (i.e., dense tree, scattered trees, bush/scrubs, low plants, and water) derived from local climate zone maps, for the reduction of depression. The NDVI index was calculated by the spectral reflectance measurements acquired in the near-infrared regions (760–900 nm) and visible red region (630–690 nm) retrieved from the Sentinal-2 satellite data with a high spatial resolution (10 × 10 m) in 2018 (55). The values of the unit-less index range from−1 to 1, with higher values indicating a higher level of green vegetation. The coverage ratio of each landscape type was derived from a 30 m Landsat 8 level 1 image of land cover according to the 2018 local climate zone map provided by the Hong Kong University through the mapping on the World Urban Database and Access Portal Tools (56). Local Climate Zones (LCZ) were developed as a classification system consisting of seven types of land cover, five of which can be described as green and blue spaces (GBS), including dense trees (LCZ_A), scattered trees (LCZ_B), bush, scrub (LCZ_C), low plants (LCZ_D), and water (LCZ_G) (57, 58).
Built Environments
The built environments were measured via three main categories depending on their influence on undergraduates' routine activities. As depression has been associated with urbanicity, population density was captured as a proxy of urbanicity, based on the assumption that urbanicity is correlated with population density (16). This was measured as the number of people per square kilometer, as reported by WorldPop in 2018, with a resolution of 100 × 100 m (14). Streets are an internal component of open spaces in cities and have attracted attention from scholars because of their close relation to transportation, especially modes of active travel (38, 59), which are protective against low levels of depression (60, 61). Three measures including street intersection density, road network density, and bus stop density were captured to characterize campus-based street environments. However, road network density and bus stop density were excluded because of collinearity. The number of street intersections (three-way or more), bus stops, and the lengths of road networks in the defined buffer were obtained from Open Street Map in 2018. The presence of diverse food outlets has previously been reported to be correlated with people's dietary patterns (39, 62). Unhealthy dietary patterns such as the consumption of sweets and high-fat food are associated with increased risk for depression (40, 41). Accordingly, food environments were measured based on the number of fast-food restaurants and take-away sweet shops (e.g., bakery shops, ice cream shops, and dessert house) per square kilometer. The count of each food outlet was retrieved from points of interest (POIs) data from the Gaode map (one of the largest map providers in China) in 2018.
SES Indicators and Other Covariates
Undergraduates who are older, female, and of lower socioeconomic status are more likely to report depression (2). The prevalence of depression also varies across rural and urban areas (7), and ethnic groups (48). Following prior studies in China (16, 24), the individual SES attributes of age, gender, ethnicity, Hukou status, and household income, were viewed as potential moderators of the association between environment and depression.
In addition, other individual and campus-based covariates were controlled including body mass index (BMI) and level of physical activity required for transportation (TPA) at the individual and urbanization level, and geographical variation and university type at the campus-based level. The BMI index was calculated by dividing weight in kilograms by the square of height in meters by in situ measurement, while TPA was defined as total time spent weekly on active travel (walking and cycling). TPA was generated according to respondents' answers to questions about the frequency (Fi), distance (Di), and average velocity of travel modes (Vi) for trips to seven categories of daily activities—learning, exercising, shopping, visiting friends, recreation, visiting the doctor, and working or doing internships. The Vi values were assumed to be 15, 5, and 0 km/h for cycling, walking, and other transport modes, respectively (63). The relative deviation of TPA was expressed as tertiles.
According to campus locality, the urbanization level was operationally defined as urban and suburban (14), and geographical variations were operationally defined as eastern, central, and western zones (64). School type was determined according to the Chinese university ranking system (high and general) as established by the National Ministry of Education. As reported, university students from higher level universities are expected to experience high levels of stress because of intense competition and pressure, which may in turn increase depression (11).
Statistical Analysis
Although the PHQ9 score was measured via arbitrary scales and not truly continuous (Supplementary Figure 2), the outcome was treated as continuous because there were more than five distinct values (0–27) for depression (65). Multivariate linear regressions were performed to explore influencing factors of depression at multiple scales (Model 1) for the low infra-class correlation (ICC = 0.03<0.06) in the null model and the robustness of linear regression modeling against moderate violations of the normal distribution assumption (65). Subsequently, multiplicative interaction terms were constructed to examine possible moderating roles of individual socioeconomic attributes on the associations between the frequency and severity of depression in undergraduates and exposure to natural and built environments within and surrounding campuses (Model 2). Variance inflation factor (VIF) values below 4 (Supplementary Table 2) were used to identify and control for multicollinearity among the independent variables (45), which excluded the road network and bus stop densities. To further avoid multicollinearities, the interaction term was generated by centered variables in interaction models. The Akaike Information Criterion (AIC) was introduced to compare the quality of these models; low AIC scores indicate a better model fit (16). The unstandardized coefficients (Coef.) and standardized error (SE) were reported for regression results. All statistical analyses were performed using IBM SPSS Statistics 26.0 and STATA 16.1.
Results
Descriptive Statistics of Samples
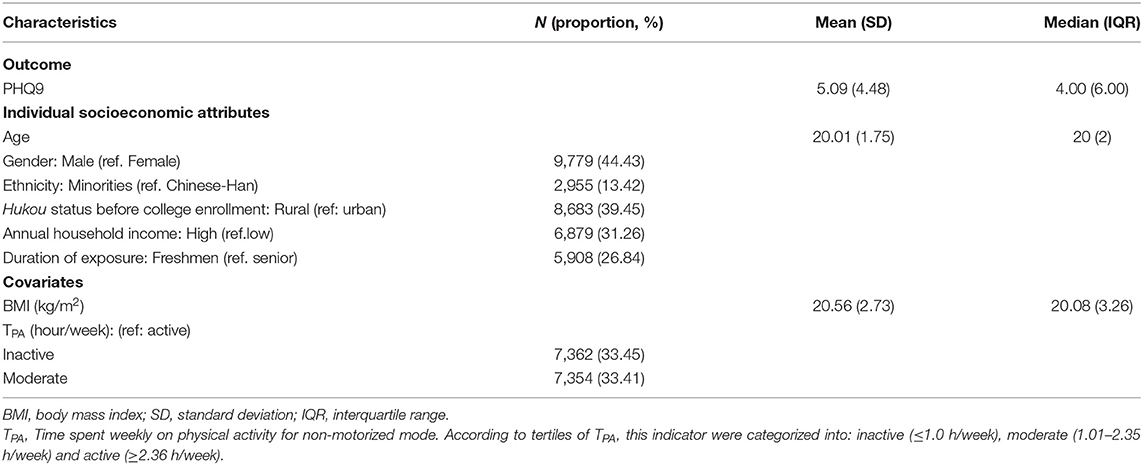
As seen in Table 1, the PHQ9 score ranged from 0 to 27 in undergraduates, with a median of 4, standard deviation of 4.48 (Table 1), and 47.7% were reported with depression (PHQ9 ≥ 5) of different degree (see Supplementary Figure 2). Although the average level of depressive score in undergraduates are reported with no depression (PHQ9 ≤ 4) (51), the relevant prevalence of depression is higher than previously reported rates. As reviewed, overall 30.6 and 24.4% of university students have experienced depressive symptoms worldwide (2) and in low-/middle- income countries (66). Additionally, the reported prevalence of depression was 14.9 and 24.3% among university students the United State and Malaysians (67, 68).
Of the 22,009 undergraduates, the majority were female, Chinese-Han, came from low-income families and urban places before enrolling in college, and had studied ≥ 1 year in the surveyed campus. The median TAP and BMI were 1.58 h/week and 20.08 kg/m2, respectively.
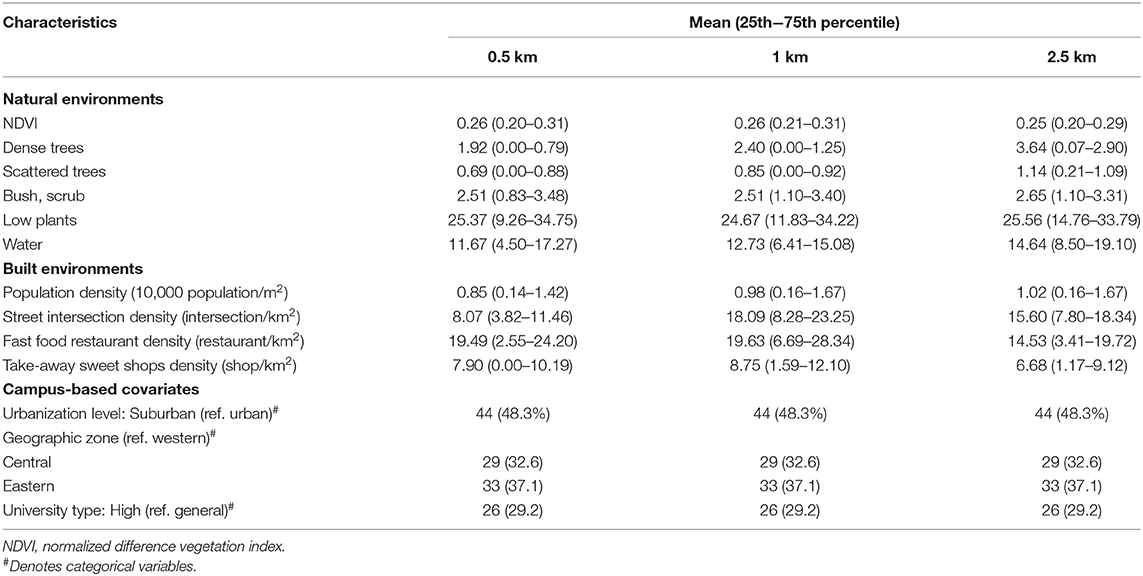
As illustrated in Table 2, the average coverage ratios of dense trees, scattered trees, bush and scrub, and water, and population density increased with the buffer radius as it extended from 0.5 to 2.5 km. Density variables for street intersections, fast-food restaurants, and take-away sweets shops were the greatest with a 1.0 km radius, followed by a 2.5 km radius, and 0.5 km radius.
Overall Associations Between Built Environment and Depression
Based on the unstandardized coefficients in Table 3, depression in undergraduates is significantly and negatively associated with scattered trees (0.5 km), water (0.5, 1.0, and 2.5 km), street intersection density (1.0 and 2.5 km), and population density (0.5 km). Inversely, undergraduates from campus with a higher density of outlets serving take-away sweets and fast foods (0.5, 1.0, and 2.5 km) are more likely to report higher depressive scores on the PHQ9. It is noteworthy that those impacts vary by different spatial scales.
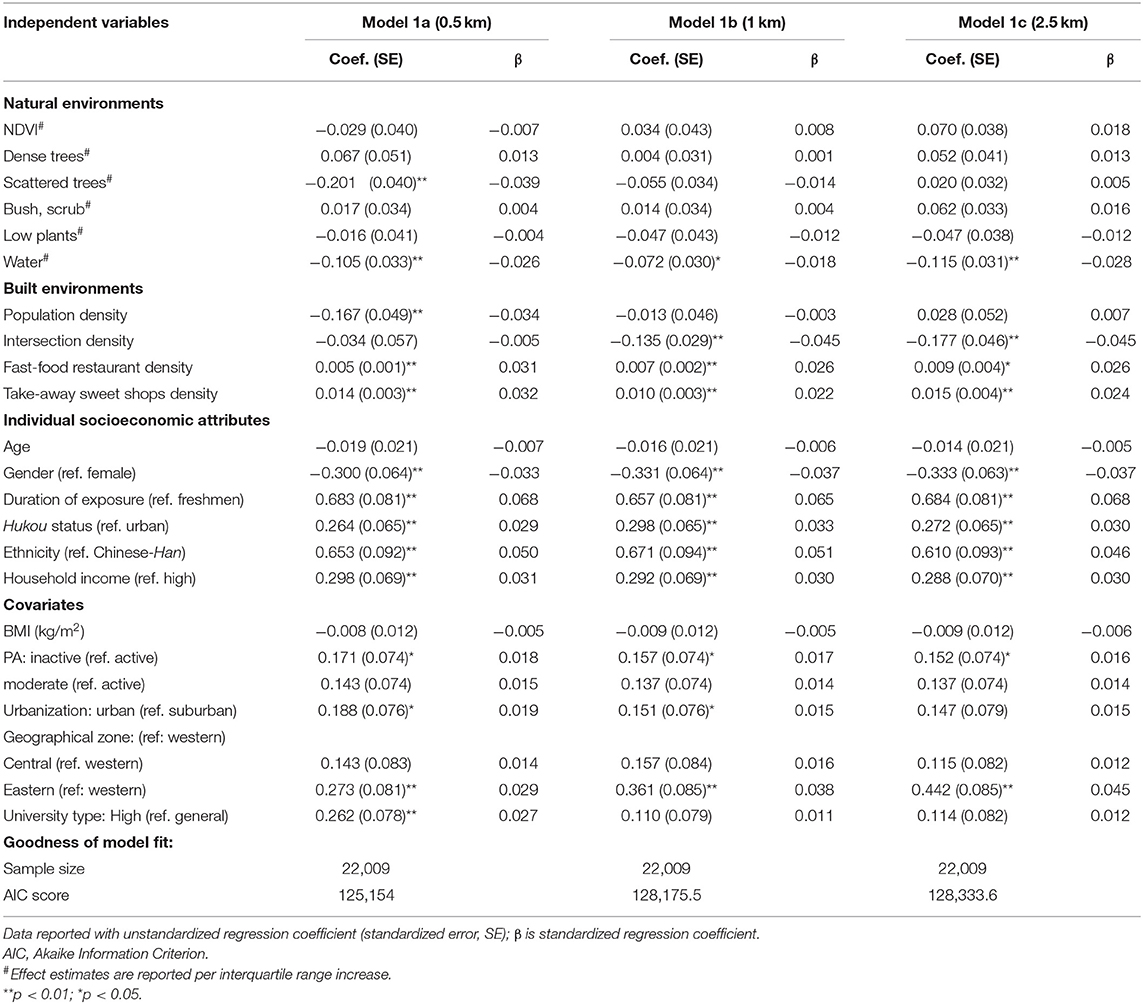
Table 3. Results of multivariate linear associations between PHQ9-based depression and exposure to natural and built environments at multiple scales.
The standardized coefficients (β) in Table 3 suggest that there are the highest negative associations between depression and scattered trees and population density. By contrast, the negative relations between depression and water decreased, with a buffer zone of 2.5 km showing the greatest association and a buffer zone of 1.0 km showing the weakest association. Additionally, the negative relationships between depression and street intersection density showed no difference across buffer distances. Unlike aforementioned negative associations, the positive correlation between depression and food outlets for take-away sweets and fast foods was greatest with a buffer zone of 0.5 km and weakest with a buffer zone of 1.0 km.
Other Determinants for Depression
In terms of individual covariates (Model 1 a – c), they played significant roles as expected. Specifically, female, senior, and ethnic minority undergraduates reported higher depressive scores. Urban hukou status before enrollment and high family income were positively and significantly related to higher depressive scores. Additionally, physical inactivity was positively correlated with depressive scores. Regarding campus-based covariates (Model 1 a – c), undergraduates from campuses located in eastern region (0.5, 1.0, and 2.5 km) and urban fields (0.5 km) were more likely to become depressed. In addition, undergraduates studying in high-level universities were more likely to suffer from severe depression (0.5 and 1.0 km).
Moderating Effects of Socioeconomic Factors
Table 4 and Supplementary Tables 3–5 reveal the moderating role of socioeconomic attributes on the association between environment and depression. The negative association between depression and water within a 0.5 km buffer zone is greater in undergraduates from urban cities than rural areas, but the association between depression and number of street intersections was higher in senior (1.0 and 2.5 km), ethnic (2.5 km), and urban-origin (1.0 and 2.5 km) undergraduates than their reference groups. The positive relationship between depression and take-away sweet shop density was stronger in Chinese-Han (0.5 km) and rural (2.5 km) undergraduates. There was no moderating role found for other associations.
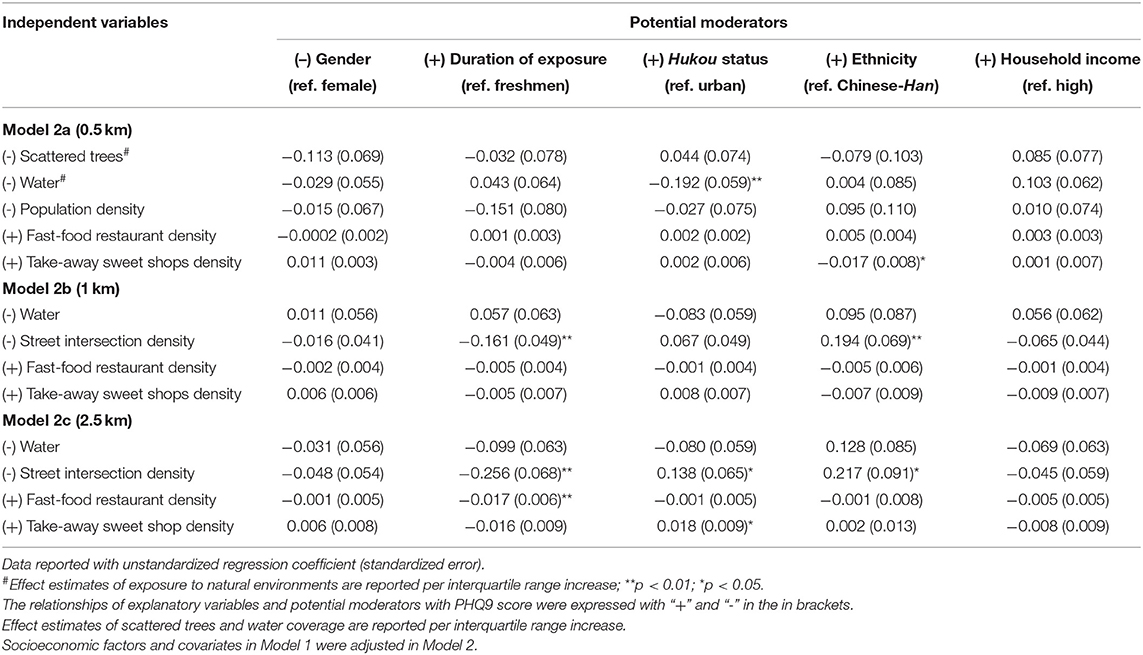
Table 4. Results of multivariate linear associations between depression in undergraduates and exposure to natural-built environments at multiple scales and with interaction effects of socioeconomic attributes.
Discussion
Specific Types of Natural Spaces, Not NDVI, Protect Against Depression
In contrast to the expectation that more NDVI mitigates depression (19, 48), the association failed to reach statistical significance in this study, which is consistent with some other previous findings (20, 54). Similar to prior studies (33, 69), however, more scattered trees within campuses helped to protect against depression. The spatial variation of protective effects of scattered trees on depression may be attributed to the fact that Chinese undergraduates conduct their daily activities within the campus. In contrast to some of the available evidence (20, 70), the prevention of depression was positively associated with an increase in coverage rate of water.
The Effect of the Built Environment on Depression Depends on Features and Spatial Scale
The built environment affects health through either modifying environmental exposure or reshaping behaviors (25). Some previous studies hold that population density mitigates depression as there are more opportunities to contact neighbors or friends (71) and to enjoy medical resources (72), thereby promoting health (16). However, this significant association was only observed within 0.5 km buffers (Table 3). One possible explanation is that the majority of Chinese undergraduates conduct their routine activities within and near campus, as they are required to complete most of their studying on campus and to live in dormitories within the campus or in the surrounding areas (12, 13). Another explanation for the inconclusive association is that most undergraduates can obtain good and affordable medical resources in school hospitals. Improvements to street connectivity create a more walkable neighborhood (73, 74) and encourage active travel such as walking and cycling (38), thereby preventing depression (75). Accordingly, more street intersections surrounding the campus can reduce depression by facilitating PA for transport and reducing the hazardous environmental exposure generated by vehicle transportation. Street intersection density is a commonly used measure of street connectivity that provides direct and safe pathways for active trips (38). Similar to a prior study (76), unhealthy food facilities serving fast foods and take-away sweets might shape a dietary pattern of sweets and high-fat foods (39), both of which are risk factors for depression (40–42).
Moderating Role of Socioeconomic Attributes
A better understanding of the moderating role that individual socioeconomic attributes have on the connections between NBEs and depression is conducive to identifying subgroups for whom interventions to improve NBEs might be the most effective. Increasingly, studies have focused on the moderating role of socioeconomic status, race/ethnicity, gender, age, and urbanicity on the relationships between depression and environment (18, 24, 48), but conclusions vary significantly in space, over time, and across population subgroups. Unlike previous studies on the moderating role of the health benefits of green spaces (48), we found no differences in the associations between scattered trees and depression based on household income and other potential moderators. In contrast, undergraduates from urban areas were generally more likely to benefit more from water (0.5 km), and subsequently experience lower levels of depression.
The presence of more street intersections appears to relate to depression more significantly in senior, urban, and ethnic minority students. This may be attributed to discrepancies in mobility and interaction among these students. Senior undergraduates generally have more opportunities to interact with this transportation infrastructure because of working or doing internships. Undergraduates originating from urban areas may visit destinations (e.g., shopping malls) far away from campus more frequently in their leisure time compared to those from rural areas (14). Additionally, a well-connected campus enables ethnic undergraduates more choices for non-motorized transportation (59). Consumption habits might be a possible explanation for the higher positive association between depression and take-way sweet facilities among rural undergraduates. Compared to students from urban areas who are used to more food choices, rural undergraduates' diet patterns could be more greatly affected by surrounding food facilities.
Implications for Public Health and Urban Planning
Depression is a leading cause for global disability and has been a cause of worldwide concern. Although there is huge variation across studies, the prevalence of depressive disorders in university students is considerably higher than rates reported in the general populations (2, 5–7). On average, 47.7% of Chinese undergraduates experienced depressive symptoms, which is much higher than the overall rates among university students in the globe (30.6%) and in the low-/middle- income countries (24.4%), as well as the 14.9% in the United State (2, 66, 67). Our findings regarding biological and environmental risk and protective factors for depression provide foundations for the prevention of not only depressive disorders, but also other complications, and in turn the reduction of disease and financial burdens.
In response to the high and increasing prevalence of depression in undergraduates, this study has significant implication for urban planning and public health promotion, for both China or other low- and middle-income countries. Our findings confirmed that scattered trees (but not overall greenery) and water within a 0.5 km buffer zone help alleviate depressive symptoms, as previously suggested in literature from other regions. First, campus designers and mangers should consider the effects of specific types of land-cover on depressed mood when seeking to improve or create new campuses. Second, urban designers and planners should include comprehensive plans for nearby areas, because undergraduates often are also exposed to the areas surrounding campuses. For example, better street connectivity and healthier food environments should be considered. Third, socioeconomic differences in the association between campuses and undergraduates show the importance of the dissemination of information regarding and promotion of health lifestyles by campus administrators.
Limitations
Despite our study's contributions to the literature, it also has several limitations. First, it follows a cross-sectional design, which precludes identifying causality between depression and exposure to NBEs. Second, static rather than dynamic or time-series exposure to NBEs was used to identify their effect on depression, although the duration of exposure was operationalized by the grade. Third, data sources on depression and individual covariates could be affected by recall bias, although face-to-face interviews could mitigate this bias to a certain extent. Fourth, since participants' medical and family histories of depression and other emotional disorders were inaccessible, the analyses could not be adjusted for these factors. Finally, measures of overall greenness and natural-land covers including dense trees, scattered trees, bush and scrubs, low plants, and water are operationally defined and characterized by different datasets under different resolutions, there thus might be some misclassification of exposure.
Conclusion
This study provides the first nationwide empirical evidence regarding the association between the severity of depression in Chinese undergraduates and the natural and built environmental characteristics within and surrounding their campus environments. After disentangling RSS, we found that natural landscapes and built environments can influence depression, but their effects varied by geographic spatial scales. Scattered trees and water had a protective effect but overall greenness or other landscape types had no association with depression. A well-connected campus buffers against depression. Conversely, more access to food outlets serving fast food and take-away sweets is related to higher levels of depression. Apart from gender and household income, the other individual socioeconomic attributes including ethnicity, Hukou status, and duration of exposure, were found to modify the associations between depression and campus environments, although the moderating roles varied across spatial scales and exposure metrics. The information from this nationwide study has implications that can be used to guide city planning for the improvement of campus environments by the management of natural and physical settings within and surrounding campuses. Further studies, not limited to depression, with prospective cohorts or quasi-experimental designs, are needed to clarify how natural and physical settings surrounding campuses affect the health of college students.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by First Affiliated Hospital of Kunming Medical University (Ethical number: 2018-L-25). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
HY and XC conceived the study. XC conducted the data analysis. HY prepared the draft of the manuscript. MD revised the manuscript. JC collected information on the campus-based environmental measurements. All authors provided critical feedback on all versions of the manuscript. All authors have read and approved the final manuscript.
Funding
This work was supported by the Strategic Priority Research Program (A) of the Chinese Academy of Sciences (Project No. XDA19040402) and the Shanghai Pujiang Program (2019PJC034).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Li He at the First Affiliated Hospital of Kunming Medical University for providing the data.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.844541/full#supplementary-material
Footnotes
1. ^A radius of 1.0 km was commonly used to define geographical buffer zone in prior studies. A radius of 0.5 km buffer zone was used to characterize the environments within campus and a radius of 2.5 km was used to characterize the environmental features (1.0–3.0 km) where considerable undergraduates were transported.
References
1. Arnett JJ, Žukauskiene R, Sugimura K. The new life stage of emerging adulthood at ages 18–29 years: implications for mental health. Lancet Psychiatr. (2014) 1:569–76. doi: 10.1016/S2215-0366(14)00080-7
2. Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. (2013) 47:391–400. doi: 10.1016/j.jpsychires.2012.11.015
3. Purborini N, Lee MB, Devi HM, Chang HJ. Associated factors of depression among young adults in Indonesia: a population- based longitudinal study. J Formosan Med Assoc. (2021) 120:1434–43. doi: 10.1016/j.jfma.2021.01.016
4. January J, Madhombiro M, Chipamaunga S, Ray S, Chingono A, Abas M. Prevalence of depression and anxiety among undergraduate university students in low- and middle-income countries: a systematic review protocol. Syst Rev. (2018) 7:57. doi: 10.1186/s13643-018-0723-8
5. Wang MY, Liu J, Wu X, Li L, Hao XD, Shen Q, et al. The prevalence of depression among students in Chinese universities over the past decade: a meta-analysis. J Hainan Med Univ. (2020) 26:286–699. doi: 10.13210/j.cnki.jhmu.20200218.001
6. WHO. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization (2017).
7. Huang YQ, Wang Y, Wang H, Liu ZR, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiat. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
8. Wang YX, Liu YN, Zhai JY, Cai JM, Chen ZY. Mental Health Status and Needs of College Students in 2020. Beijing: Social Science Literature Press (2021).
9. van den Bosch M, Meyer-Lindenberg A. Environmental exposures and depression: biological mechanisms and epidemiological evidence. Annu Rev Public Health. (2019) 40:239–59. doi: 10.1146/annurev-publhealth-040218-044106
10. Cheung DK, Tam DKY, Tsang MH, Zhang DLW, Lit DSW. Depression, anxiety and stress in different subgroups of first-year university students from 4-year cohort data. J Affect Disord. (2020) 274:305–14. doi: 10.1016/j.jad.2020.05.041
11. Yang T, Barnett R, Fan Y, Li L. The effect of urban green space on uncertainty stress and life stress: a nationwide study of university students in China. Health Place. (2019) 59:102199. doi: 10.1016/j.healthplace.2019.102199
12. Zhan G, Yan X, Zhu S, Wang Y. Using hierarchical tree-based regression model to examine university student travel frequency and mode choice patterns in China. Transport Policy. (2016) 45:55–65. doi: 10.1016/j.tranpol.2015.09.006
13. He SJ. Consuming urban living in “villages in the city”: studentification in Guangzhou, China. Urban Stud. (2015) 52:2849–73. doi: 10.1177/0042098014543703
14. Yang H, He D, Lu Y, Ren C, Huang X. Disentangling residential self-selection from the influence of built environment characteristics on adiposity outcomes among undergraduate students in China. Cities. (2021) 113:103165. doi: 10.1016/j.cities.2021.103165
15. James P, Hart JE, Banay RF, Laden F, Signorello LB. Built Environment and depression in low-income African Americans and Whites. Am J Prev Med. (2017) 52:74–84. doi: 10.1016/j.amepre.2016.08.022
16. Wang R, Liu Y, Xue D, Helbich M. Depressive symptoms among Chinese residents: how are the natural, built, and social environments correlated? BMC Public Health. (2019) 19:887. doi: 10.1186/s12889-019-7171-9
17. Yao W, Chen F, Wang S, Zhang X. Impact of exposure to natural and built environments on positive and negative affect: a systematic review and meta-analysis. Front Public Health. (2021) 9:758457. doi: 10.3389/fpubh.2021.758457
18. Barnett A, Zhang CJP, Johnston JM, Cerin E. Relationships between the neighborhood environment and depression in older adults: a systematic review and meta-analysis. Int Psychogeriatr. (2018) 30:1153–76. doi: 10.1017/S104161021700271X
19. Sarkar C, Webster C, Gallacher J. Residential greenness and prevalence of major depressive disorders: a cross-sectional, observational, associational study of 94 879 adult UK Biobank participants. Lancet Planetary Health. (2018) 2:e162–73. doi: 10.1016/S2542-5196(18)30051-2
20. Helbich M, Yao Y, Liu Y, Zhang J, Liu P, Wang R. Using deep learning to examine street view green and blue spaces and their associations with geriatric depression in Beijing, China. Environ Int. (2019) 126:107–17. doi: 10.1016/j.envint.2019.02.013
21. Yang H, Zhang Q, Helbich M, Lu Y, He D, Ettema D, et al. Examining non-linear associations between built environments around workplace and adults' walking behaviour in Shanghai, China. Transport Res A Policy Practice. (2022) 155:234–46. doi: 10.1016/j.tra.2021.11.017
22. Banay RF, James P, Hart JE, Kubzansky LD, Spiegelman D, Okereke OI, et al. Greenness and depression incidence among older women. Environ Health Perspect. (2019) 127:27001. doi: 10.1289/EHP1229
23. Bezold CP, Banay RF, Coull BA, Hart JE, James P, Kubzansky LD, et al. The association between natural environments and depressive symptoms in adolescents living in the United States. J Adolesc Health. (2018) 62:488–95. doi: 10.1016/j.jadohealth.2017.10.008
24. Liu Y, Wang R, Xiao Y, Huang B, Chen H, Li Z. Exploring the linkage between greenness exposure and depression among Chinese people: mediating roles of physical activity, stress and social cohesion and moderating role of urbanicity. Health Place. (2019) 58:102168. doi: 10.1016/j.healthplace.2019.102168
25. Frank LD, Iroz-Elardo N, MacLeod KE, Hong A. Pathways from built environment to health: a conceptual framework linking behavior and exposure-based impacts. J Transport Health. (2019) 12:319–35. doi: 10.1016/j.jth.2018.11.008
26. Collins RM, Spake R, Brown KA, Ogutu BO, Smith D, Eigenbrod F. A systematic map of research exploring the effect of greenspace on mental health. Landscape Urban Plan. (2020) 201:103823. doi: 10.1016/j.landurbplan.2020.103823
27. Picavet HSJ, Milder I, Kruize H, de Vries S, Hermans T, Wendel-Vos W. Greener living environment healthier people? exploring green space, physical activity and health in the Doetinchem Cohort Study. Prev Med. (2016) 89:7–14. doi: 10.1016/j.ypmed.2016.04.021
28. Lu Y. Using Google Street View to investigate the association between street greenery and physical activity. Landscape Urban Plan. (2019) 191:29. doi: 10.1016/j.landurbplan.2018.08.029
29. Wan C, Shen GQ, Choi S. Underlying relationships between public urban green spaces and social cohesion: a systematic literature review. City Cult Soc. (2021) 24:100383. doi: 10.1016/j.ccs.2021.100383
30. Markevych I, Schoierer J, Hartig T, Chudnovsky A, Hystad P, Dzhambov AM, et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res. (2017) 158:301–17. doi: 10.1016/j.envres.2017.06.028
31. Akpinar A, Barbosa-Leiker C, Brooks KR. Does green space matter? Exploring relationships between green space type and health indicators. Urban Forestry Urban Greening. (2016) 20:407–18. doi: 10.1016/j.ufug.2016.10.013
32. Jarvis I, Koehoorn M, Gergel SE, van den Bosch M. Different types of urban natural environments influence various dimensions of self-reported health. Environ Res. (2020) 186:109614. doi: 10.1016/j.envres.2020.109614
33. Nishigaki M, Hanazato M, Koga C, Kondo K. What types of greenspaces are associated with depression in urban and rural older adults? a multilevel cross-sectional study from JAGES. Int J Environ Res Public Health. (2020) 17:249276. doi: 10.3390/ijerph17249276
34. Giles-Corti B, Broomhall MH, Knuiman M, Ma K, Collins CKD. Increasing walking: how important is distance to, attractiveness, and size of public open space? Am J Prev Med. (2005) 28:69–176. doi: 10.1016/j.amepre.2004.10.018
35. Holtan MT, Dieterlen SL, Sullivan WC. Social life under cover: tree canopy and social capital in Baltimore, Maryland. Environ Behav. (2015) 47:502–25. doi: 10.1177/0013916513518064
36. Ewing R, Cervero R. Travel and the built environment. J Am Plan Assoc. (2010) 76:3. doi: 10.1080/01944361003766766
37. Nordbo ECA, Nordh H, Raanaas RK, Aamodt G. GIS-derived measures of the built environment determinants of mental health and activity participation in childhood and adolescence: a systematic review. Landsc Urban Plan. (2018) 177:19–37. doi: 10.1016/j.landurbplan.2018.04.009
38. Sallis JF, Cerin E, Conway TL, Adams MA, Frank LD, Pratt M, et al. Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study. Lancet. (2016) 387:2207–17. doi: 10.1016/S0140-6736(15)01284-2
39. Zhou P, Li R, Liu K. The neighborhood food environment and the onset of child-hood obesity: a retrospective time-trend study in a mid-sized city in China. Front Public Health. (2021) 9:688767. doi: 10.3389/fpubh.2021.688767
40. Li Y, Lv MR, Wei YJ, Sun L, Zhang JX, Zhang HG, et al. Dietary patterns and depression risk: a meta-analysis. Psychiatry Res. (2017) 253:373–82. doi: 10.1016/j.psychres.2017.04.020
41. Lassale C, Batty GD, Baghdadli A, Jacka F, Sanchez-Villegas A, Kivimaki M, et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatr. (2019) 24:1094. doi: 10.1038/s41380-018-0237-8
42. Reis DJ, Ilardi SS, Namekata MS, Wing EK, Fowler CH. The depressogenic potential of added dietary sugars. Med Hypotheses. (2020) 134:109421. doi: 10.1016/j.mehy.2019.109421
43. Boone-Heinonen J, Gordon-Larsen P, Guilkey DK, Jacobs DR Jr, Popkin BM. Environment and physical activity dynamics: the role of residential self-selection. Psychol Sport Exerc. (2011) 12:54–60. doi: 10.1016/j.psychsport.2009.09.003
44. Wu W, Yun Y, Zhai J, Sun Y, Zhang G, Wang R. Residential self-selection in the greenness-wellbeing connection: a family composition perspective. Urban Forest Urban Green. (2021) 59:127. doi: 10.1016/j.ufug.2021.127000
45. Zang P, Lu Y, Ma J, Xie B, Wang R, Liu Y. Disentangling residential self-selection from impacts of built environment characteristics on travel behaviors for older adults. Soc Sci Med. (2019) 238:112515. doi: 10.1016/j.socscimed.2019.112515
46. Zhao P, Kwan MP, Zhou S. The uncertain geographic context problem in the analysis of the relationships between obesity and the built environment in Guangzhou. Int J Environ Res Public Health. (2018) 15:20308. doi: 10.3390/ijerph15020308
47. Kwan MP. The uncertain geographic context problem. Ann Assoc Am Geogr. (2012) 102:958–68. doi: 10.1080/00045608.2012.687349
48. McEachan RR, Prady SL, Smith G, Fairley L, Cabieses B, Gidlow C, et al. The association between green space and depressive symptoms in pregnant women: moderating roles of socioeconomic status and physical activity. J Epidemiol Community Health. (2016) 70:253–9. doi: 10.1136/jech-2015-205954
49. McEachan RRC, Yang TC, Roberts H, Pickett KE, Arseneau-Powell D, Gidlow CJ, et al. Availability, use of, and satisfaction with green space, and children's mental wellbeing at age 4 years in a multicultural, deprived, urban area: results from the Born in Bradford cohort study. Lancet Planetar Health. (2018) 2:e244–54. doi: 10.1016/S2542-5196(18)30119-0
50. Loh VH, Veitch J, Salmon J, Cerin E, Mavoa S, Villanueva K, et al. Residential vs. school neighborhoods: associations with physical activity among adolescents. Health Place. (2020) 63:102328. doi: 10.1016/j.healthplace.2020.102328
51. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
52. Breedvelt JJF, Zamperoni V, South E, Uphoff EP, Gilbody S, Bockting CLH, et al. A systematic review of mental health measurement scales for evaluating the effects of mental health prevention interventions. Eur J Public Health. (2020) 30:539–45. doi: 10.1093/eurpub/ckz233
53. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
54. Noordzij JM, Beenackers MA, Oude Groeniger J, Timmermans E, Chaix B, Doiron D, et al. Green spaces, subjective health and depressed affect in middle-aged and older adults: a cross-country comparison of four European cohorts. J Epidemiol Community Health. (2021). doi: 10.1136/jech-2020-214257
55. Kaplan G, Avdan U. Object-based water body extraction model using Sentinel-2 satellite imagery. Eur J Remote Sens. (2017) 50:137–43. doi: 10.1080/22797254.2017.1297540
56. Shi Y, Ren C, Lau KK-L, Ng E. Investigating the influence of urban land use and landscape pattern on PM25 spatial variation using mobile monitoring and WUDAPT. Landscape Urban Plan. (2019) 189:15–26. doi: 10.1016/j.landurbplan.2019.04.004
57. Oke TR, Stewart ID. Local climate zones for urban temperature studies. Bull Am Meteorol Soc. (2012) 93:1879–900. doi: 10.1175/BAMS-D-11-00019.1
58. Ren C, Cai M, Li X, Zhang L, Wang R, Xu Y, et al. Assessment of local climate zone classification maps of cities in China and feasible refinements. Sci Rep. (2019) 9:18848. doi: 10.1038/s41598-019-55444-9
59. Zlatkovic M, Zlatkovic S, Sullivan T, Bjornstad J, Kiavash Fayyaz Shahandashti S. Assessment of effects of street connectivity on traffic performance and sustainability within communities and neighborhoods through traffic simulation. Sustain Cities Soc. (2019) 46:37. doi: 10.1016/j.scs.2018.12.037
60. Berke EM, Gottlieb LM, Moudon AV, Larson EB. Protective association between neighborhood walkability and depression in older men. J Am Geriatr Soc. (2007) 55:526–33. doi: 10.1111/j.1532-5415.2007.01108.x
61. Wang R, Lu Y, Zhang J, Liu P, Yao Y, Liu Y. The relationship between visual enclosure for neighbourhood street walkability and elders' mental health in China: using street view images. J Transport Health. (2019) 13:90–102. doi: 10.1016/j.jth.2019.02.009
62. Lamichhane AP, Mayer-Davis EJ, Puett R, Bottai M, Porter DE, Liese AD. Associations of built food environment with dietary intake among youth with diabetes. J Nutr Educ Behav. (2012) 44:217–24. doi: 10.1016/j.jneb.2011.08.003
63. Stefansdottir H, Næss P, Ihlebæk CM. Built environment, non-motorized travel and overall physical activity. Travel Behav Soc. (2019) 16:201–13. doi: 10.1016/j.tbs.2018.08.004
64. Zhong B, Giubilato E, Critto A, Wang L, Marcomini A, Zhang J. Probabilistic modeling of aggregate lead exposure in children of urban China using an adapted IEUBK model. Sci Total Environ. (2017) 584–5:259–67. doi: 10.1016/j.scitotenv.2016.11.164
65. Dzhambov AM, Hartig T, Tilov B, Atanasova V, Makakova DR, Dimitrova DD. Residential greenspace is associated with mental health via intertwined capacity-building and capacity-restoring pathways. Environ Res. (2019) 178:108708. doi: 10.1016/j.envres.2019.108708
66. Akhtar P, Ma L, Waqas A, Naveed S, Li Y, Rahman A, et al. Prevalence of depression among university students in low and middle income countries (LMICs): a systematic review and meta-analysis. J Affect Disord. (2020) 274:911–9. doi: 10.1016/j.jad.2020.03.183
67. American College Health A. American College Health Association-National College Health Assessment Spring 2008 Reference Group Data Report (abridged): the American College Health Association. J Am Coll Health. (2009) 57:477–88. doi: 10.3200/JACH.57.5.477-488
68. Abd Hamid NZ, Ibrahim S, Razali H. Prevalence of depression among university students: a cross-sectional study. Int J Educ Psychol Counsel. (2020) 5:204–10. doi: 10.35631/IJEPC.5360015
69. Dzhambov AM. Residential green and blue space associated with better mental health: a pilot follow-up study in university students. Arh Hig Rada Toksikol. (2018) 69:340–9. doi: 10.2478/aiht-2018-69-3166
70. Gascon M, Sanchez-Benavides G, Dadvand P, Martinez D, Gramunt N, Gotsens X, et al. Long-term exposure to residential green and blue spaces and anxiety and depression in adults: a cross-sectional study. Environ Res. (2018) 162:231–9. doi: 10.1016/j.envres.2018.01.012
71. Cramer V, Torgersen S, Kringlen E. Quality of life in a city: the effect of population density. Soc Indic Res. (2004) 69:103–16. doi: 10.1023/B:SOCI.0000032663.59079.0b
72. Vlahov D, Galea S. Urbanization, urbanicity, and health. J Urban Health. (2002) 79(4Suppl.1):S1–12. doi: 10.1093/jurban/79.suppl_1.S1
73. Gomez LF, Parra DC, Buchner D, Brownson RC, Sarmiento OL, Pinzon JD, et al. Built environment attributes and walking patterns among the elderly population in Bogota. Am J Prev Med. (2010) 38:592–9. doi: 10.1016/j.amepre.2010.02.005
74. Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. Am J Public Health. (2003) 93:1552–8. doi: 10.2105/AJPH.93.9.1552
75. Schuch FB, Werneck AO, Vancampfort D, Stubbs B, Teychene M, Lotufo PA, et al. Cross-sectional associations of leisure and transport related physical activity with depression and anxiety. J Psychiatr Res. (2021) 140:228–34. doi: 10.1016/j.jpsychires.2021.05.053
Keywords: natural environment, built environment, multiple scales, depressive symptoms, moderating effect, undergraduates, China
Citation: Yang H, Cui X, Dijst M, Tian S, Chen J and Huang J (2022) Association Between Natural/Built Campus Environment and Depression Among Chinese Undergraduates: Multiscale Evidence for the Moderating Role of Socioeconomic Factors After Controlling for Residential Self-Selection. Front. Public Health 10:844541. doi: 10.3389/fpubh.2022.844541
Received: 28 December 2021; Accepted: 02 February 2022;
Published: 07 April 2022.
Edited by:
Ruoyu Wang, University of Edinburgh, United KingdomReviewed by:
Dongsheng He, The University of Hong Kong, Hong Kong SAR, ChinaHongsheng Chen, Shenzhen University, China
Copyright © 2022 Yang, Cui, Dijst, Tian, Chen and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiangfen Cui, Y3VpMTk4N3JhaW5ueUAxNjMuY29t; Jie Chen, Y2hlbmppZUBrdXN0LmVkdS5jbg==
 Haoran Yang
Haoran Yang Xiangfen Cui
Xiangfen Cui Martin Dijst3
Martin Dijst3