- 1Department of Health Promotion and Health Education, National Taiwan Normal University, Taipei, Taiwan
- 2Graduate Institute of Sport, Leisure and Hospitality Management, National Taiwan Normal University, Taipei, Taiwan
- 3Master's Program of Transition and Leisure Education for Individuals With Disabilities, University of Taipei, Taipei, Taiwan
- 4School of Gerontology Health Management, College of Nursing, Taipei Medical University, Taipei, Taiwan
- 5Health Convergence Medicine Laboratory, Biomedical Research Institute, Pusan National University Hospital, Busan, South Korea
- 6Department of Rehabilitation Medicine, School of Medicine, Pusan National University, Busan, South Korea
Introduction: Several studies have suggested that physical activity and sedentary behavior are strongly and independently associated with body composition and obesity. However, few studies have investigated whether substituting sedentary time with moderate-to-vigorous physical activity is associated with body composition in older adults, especially among those older than 75 years.
Methods: This study examined the associations between replacing sedentary time with physical activity and obesity indices in a sample of 199 community-dwelling older Taiwanese adults (52.3% women; 80.6 ± 7.0 years). Physical activity and sedentary behavior were measured using the triaxial accelerometer (GT3X+, ActiGraph). Body composition indices were computed through a bioelectrical impedance analysis of body fat percentage and appendicular skeletal muscle mass index. Waist circumference and body mass index were measured by trained personnel. Isotemporal substitution analyses estimated these associations after adjusting for sociodemographic characteristics and nutritional status.
Results: The study showed that substituting 30 min of sedentary behavior per day with moderate-to-vigorous physical activity was associated with lower body fat percentage (B = −1.408, 95% CI = −2.55, −0.264), body mass index (B = −0.681, 95% CI = −1.300, −0.061), and waist circumference (B = −2.301, 95% CI = −4.062, −0.539) after adjusting for covariates. Substituting 30 min of light physical activity per day with moderate-to-vigorous physical activity was associated with lower waist circumference (B = −2.230, 95% CI = −4.173, −0.287) after adjusting for covariates. Stratified analyses indicated that associations were stronger in youngest-old older adults, and in older adults with a normal nutritional status (vs. underweight status).
Discussion: These findings confirm the importance of reducing sedentary behavior and increasing moderate-to-vigorous physical activity among older adults to improve their physical health, as well as highlighting the importance of taking into account nutritional status and age group.
Introduction
As the aging population trends are higher globally, the number of older people is estimated to increase from 1 billion in 2020 to 2.1 billion by 2050 (1). Chronic ailments such as cardiovascular diseases and type two diabetes are increasingly prevalent in older individuals worldwide (2, 3). Studies have indicated that maintaining a healthy body weight in old age plays a vital role in preventing chronic diseases (4, 5) and that the prevalence of obesity has increased in high-income (6) as well as low to middle-income countries (7). Moreover, a longitudinal study indicated that long-term exposure to obesity is associated with poor performance of physical function in later life (8). Given that several studies have suggested that physical activity and sedentary behavior (SB) are strongly and independently associated with cardiac biomarkers and body composition (9–11), it is important to develop effective strategies for older populations.
Good nutritional status, physical activity, and SB play crucial roles in preventing metabolic syndrome and sarcopenia in older adults (12). Even in older adults aged 75 years and above, physical activity seems to delay age-related physiological decline, via its influence on several pathways, including improved cardiovascular fitness, decelerated sarcopenia, reduced adiposity, and improved immunity (13). Previous studies on obesity risk factors in older adults often highlighted the direct health benefits of light physical activity (LPA) and moderate-to-vigorous physical activity (MVPA) (14–16). According to the latest WHO guidelines on physical activity and SB, older adults should limit the amount of time spent being sedentary; replacing sedentary time with physical activity of any intensity provides health benefits (17).
Isotemporal substitution models have frequently been used in statistical analysis to explore the association between reallocating the time spent in SB and other health outcomes such as mortality, mental health, adiposity, fitness, and cardiometabolic biomarkers (18). These models assume that available time for physical activity and SB is limited—increasing the time spent on one activity, such as sedentary time, means less time for another activity, such as MVPA (19). This indicates that these activities are co-dependent. Previous studies have implied that substituting sedentary time for MVPA time had a beneficial effect on body mass index (BMI) (20), waist circumference (WC) (16, 21), and body fat percentage (15, 20). However, few studies have examined the associations between substituting SB with MVPA and body composition (including appendicular skeletal muscle) in older adults (18, 22). Moreover, previous systematic reviews revealed that most studies were with youngest-old adults (aged 65–74 years), and none were with middle (75–84 years) (21) or oldest-old adults (85 years and above) (23). Therefore, the present study aims to examine the association between body composition and replacing sedentary time with physical activity in youngest-old to oldest-old community-dwelling older adults. The outcomes were body composition [appendicular skeletal muscle mass index (ASMI), body fat percentage, etc.], BMI, and WC. Compared to the muscle mass, the ASMI is calculated as appendicular skeletal mass index (ASM)/height2 (ASM/m2) which correlates with nutrition and physical status and may be a more effective indicator than the muscle mass in preventing the sarcopenia (24). The hypothesis of this study is that replacing SB with physical activity of any intensity is associated with lower body fat percentage BMI, WC, and greater ASMI in all older adults.
Materials and methods
This study uses a cross-sectional design and it was approved by the Research Ethics Committee of the National Taiwan University Hospital (REC Number: 202008046RINC).
Participants
The study recruited 199 community-dwelling individuals. Inclusion criteria were individuals aged from 65 to 98 years (the proportion: youngest-old adults: 24.1%; middle-old adults: 44.7%; oldest-old adults: 31.2%), living in Taipei City—Taiwan, the ability to walk independently, no severe hearing or visual impairments, and consistently wearing a triaxial accelerometer for 7 days. The participants were recruited through two channels. The first was patients who had consulted a doctor at the National Taiwan University Hospital for medical issues. The other channel was patients who saw a doctor in the outpatient clinic of the same hospital. Participants were recruited through phone calls for verbal agreement. The sampling was carried out from August 2020 to March 2021. Participants from both channels provided informed consent.
Obesity indices
Body mass index and waist circumference
BMI is calculated by dividing an individual's body weight in kilograms by the square of the person's height in meters. WC is measured at the middle point between the vertebral rib and the top of the ilium, roughly in line with the umbilicus (25).
Appendicular skeletal muscle mass index and body fat percentage
Body fat percentage (%) and ASMI (muscle mass/m2) were calculated using bioelectrical impedance analysis (“Babybot” — Netown, Taiwan) (26). ASMI is the sum of the muscle mass of a person's four limbs divided by the square of their height in meters (27). ASMI is used as an indicator of sarcopenia (defined as age-related loss of muscle mass and function) (28, 29). These anthropometric indices were measured by trained personnel.
Objectively monitored physical activity and sedentary behavior
Participants were requested to wear a hip-mounted triaxial accelerometer (ActiGraph GT3X+, Pensacola, FL, USA) continuously for 7 days (30) to estimate the time spent in SB (≤ 99 counts/min), LPA (100–2019 counts/min), and MVPA (≥2020 counts/min). Instructions on how to wear and remove the accelerometer before and after taking a shower or performing water-based activities were given to participants by trained personnel. Sleep time was excluded using the sleep log. The vertical axis data from the accelerometers were then downloaded using the ActiLife software (version 6.0, Pensacola, FL, USA). Standard protocols for data collection and processing criteria of the triaxial accelerometer from ActiGraph were followed, as suggested by a systematic review (31). A valid day was 600 min or more of wear time; a zero-count was considered non-wear time, defined as no SB or physical activity for 60 consecutive minutes. Furthermore, data from at least four valid days (three weekdays and one weekend day) were classified as valid and included in the analysis.
Covariates
Sociodemographic characteristics such as age, gender, educational level, and living status were self-reported. Participants were also asked to report their cigarette and alcohol use habits. They were also asked to report whether they were ever diagnosed with hypertension or diabetes. Because previous study inplies that with mini nutritional assessment score is low in elderly subjects with sarcopenia (32) and negatively associated with central obesity (33), nutritional status was assessed through mini nutritional assessment short-form questions (34). The participants were then categorized as either “normal nutrition” (12–14 points) or “at risk of malnutrition” (≤ 11 points) status.
Statistical analyses
Descriptive analyses were conducted using the IBM SPSS 23.0 software (SPSS Inc., IBM, Chicago, IL, USA). Outcomes can be either continuous or dichotomous for isotemporal substitution modeling (19). Multiple linear regression models were used to analyze the theoretical effect of replacing 30 min of sedentary time with LPA and MVPA (35). The models considered all the LPA and MVPA activity variables simultaneously, with the exception of sedentary time. The total wear time variables and covariates were kept constant. Including the total wear-time variable made time isotemporal. The regression estimate for each activity variable in the model—unstandardized coefficients (B) with 95% confidence interval (CI)—demonstrated the effect of substituting 30 min of sedentary time with an equivalent LPA and MVPA time. All analyses were conducted using the SPSS 23.0 software for Windows (SPSS Inc., IBM, Chicago, IL, USA). Stratified analyses for nutritional status (normal vs. at risk of malnutrition) and age group (65–74 vs. 75 years old and above) were performed and are reported in the Appendix.
Results
Participant characteristics
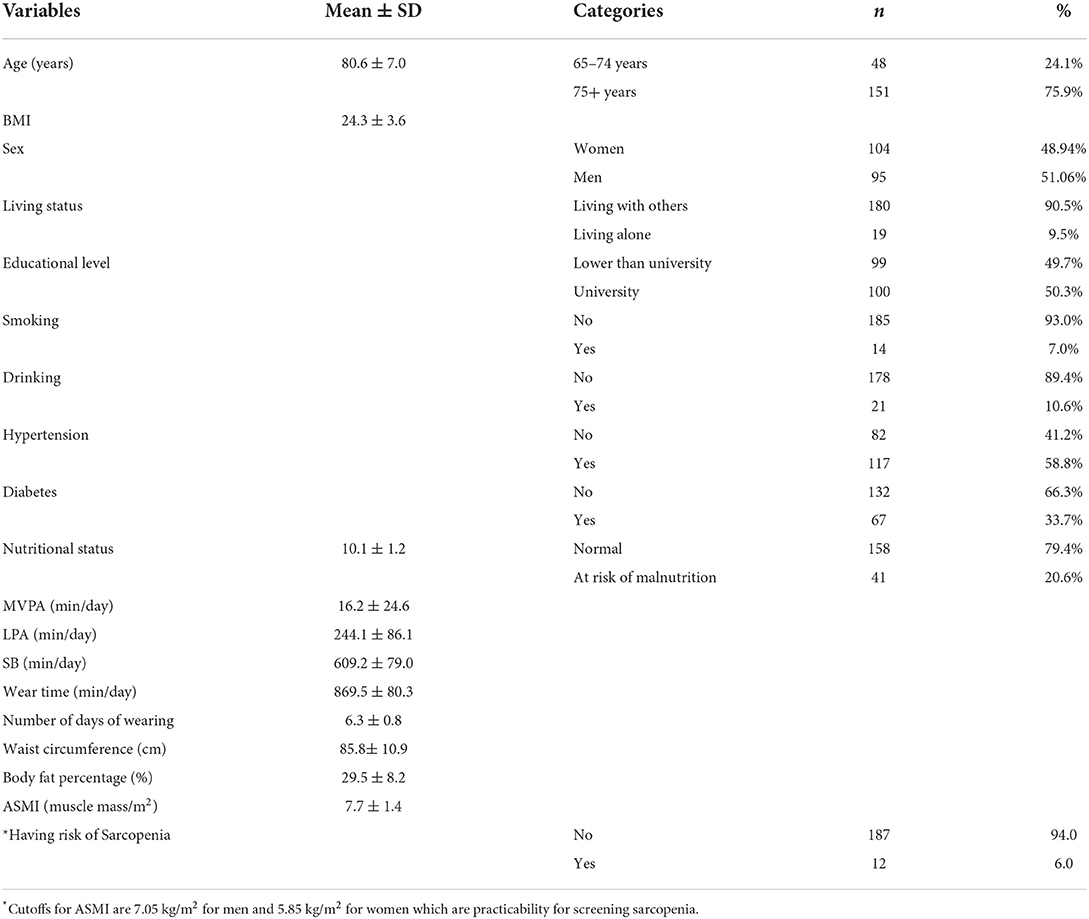
All 199 individuals (52.3% women; 80.6 ± 7.0 years) aged 65 years and older (more than three quarters of them were older than or equal to 75 years old) were included in the analyses (Table 1). Most of the participants lived with others (90.5%) and had tertiary education (50.3%). The majority of them did not smoke cigarettes (93.0%) or drink alcohol (89.4%), were diagnosed with hypertension (58.8%), and did not have diabetes (66.3%). The participants' average BMI (24.3 ± 3.6 kg/m2) was on the cusp of obesity. The average duration for LPA, MVPA, SB, and wear time were 244.1 ± 86.2, 16.2 ± 24.6, 609.2 ± 79.0, and 869.5 ± 80.3 min/day (average days worn: 6.3 ± 0.8), respectively. In terms of obesity indices, participants' average WC (cm), body fat percentage (%), and ASMI (muscle mass/m2) were 85.8 ± 10.9, 29.5 ± 8.2, 7.7 ± 1.4, respectively.
Isotemporal substitution model
The results of replacing 30 min of SB with LPA and MVPA on the risk factors of obesity using unadjusted and adjusted isotemporal substitution models are shown in Tables 2, 3. In the unadjusted model, the test results indicated that reallocating 30 min of SB per day with MVPA (increasing MVPA at the expense of SB) was associated with lower body fat percentage (B = −2.216, 95% CI = −3.695, −0.736). Replacing 30 min of LPA per day with MVPA was also associated with lower body fat percentage (B = −2.024, 95% = −3.669, −0.379). In the adjusted model, the test results indicated that reallocating 30 min of SB per day with MVPA (increasing MVPA at the expense of SB) was associated with lower body fat percentage (B = −1.408, 95% CI = −2.552, −0.264), BMI (B = −0.681, 95% CI = −1.300, −0.061), and WC (B = −2.301, 95% CI = −4.062, −0.539). Furthermore, reallocating 30 min of LPA per day with MVPA was also associated with lower WC (B = −2.230, 95% CI = −4.173, −0.287). There was no significant relationship between ASMI and reallocating any type of physical activity with SB. In stratified analysis of the adjusted model, the results indicated that reallocating 30 min of SB per day with MVPA was also associated with lower body fat percentage (B = −1.960, 95% CI = −3.387, −0.532), BMI (B = −0.766, 95% CI = −1.495, −0.036), and WC (B = −2.322, 95% CI = −4.150, −0.493) in the normal nutritional status group. Moreover, replacing 30 min of LPA per day with MVPA was associated with lower WC in this group. There were no significant associations between any indicators of body composition and reallocating any type of physical activity with SB in having risk of malnutrition group. In terms of stratified analysis of the adjusted model for age agroup, the results showed that replacing 30 min of SB per day with MVPA was associated with lower body fat percentage (B = −2.105, 95% CI = −4.177, −0.033) in the age group of 65–74 years. There were no significant associations between any indicators of body composition and replacing any type of physical activity with SB in the age group of 75 years old and above, middle-old (75–84 years), and oldest-old (85 years and above). Addiitonally, the null associations were also apparent when further excluding those who were with underweight nutritional status in two age group.
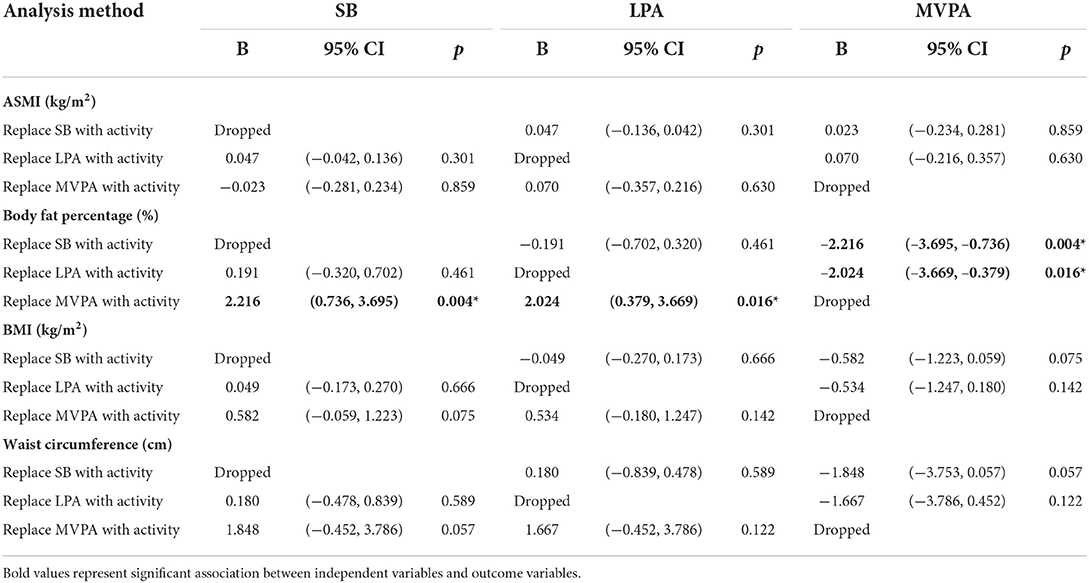
Table 2. Unadjusted isotemporal substitution models examining the associations of replacing 30 min sedentary behavior, LPA, and MVPA on body composition (n = 199).
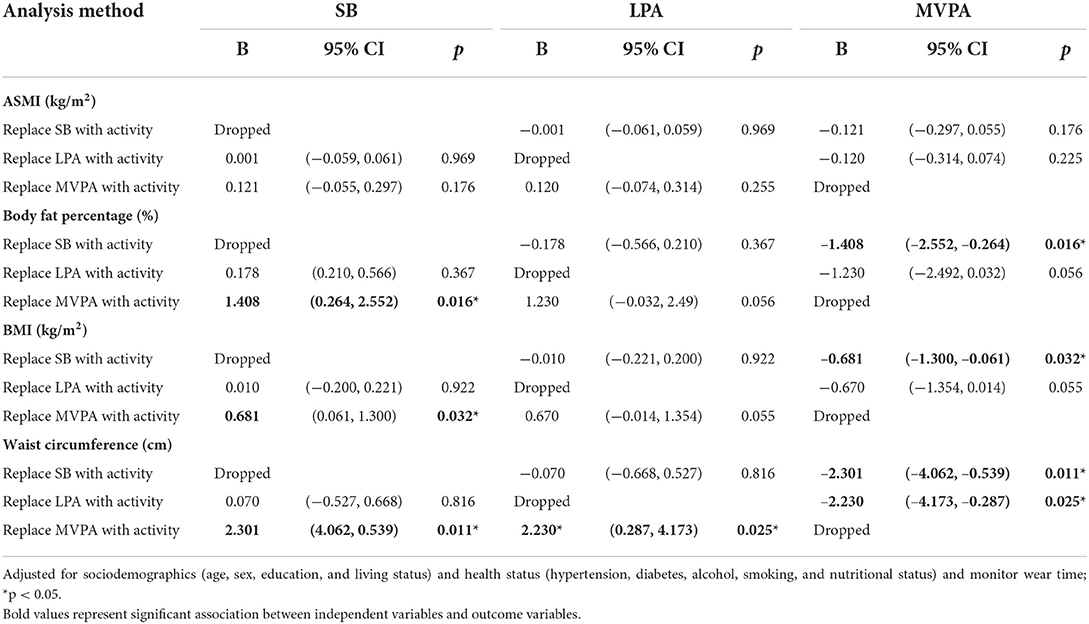
Table 3. Adjusted substitution models examining the associations of replacing 30 min sedentary behavior, LPA and MVPA on body composition (n = 199).
Discussion
Among factors related to obesity, physical activity has been recognized as a critical lifestyle factor to prevent or delay muscle loss and cardiovascular diseases with aging. Higher physical intensity helps maintain the skeletal muscle's aerobic capacity in older adults (36), reduces insulin resistance, and has an anti-inflammatory effect on the immune system (24). This study further presents a novel opportunity to investigate the effect of replacing SB with physical activity on the risks of obesity in community-dwelling older adults. The present study found that replacing 30 min of SB with the same amount of MVPA time is associated with better body fat percentage, BMI, and WC in a sample of community-dwelling older adults ranging in age from 65 to 98 years. Associations held when taking age, sex, sociodemographic characteristics, health status, and nutritional status into account. Moreover, a significant relationship was found between WC and replacing a period of LPA with MVPA. Therefore, MVPA is an essential daily activity associated with the risks of obesity. A 30-min reallocation of SB time to MVPA time was associated with ~1.41% lower body fat percentage, 0.68 kg/m2 lower BMI, and 2.30 cm lower WC. A 30-min reallocation of LPA time to MVPA time was associated with ~2.23 cm lower WC.
Previous studies on adults aged 65–80 have highlighted the benefits of replacing sedentary time with MVPA time on improved BMI, WC (15, 21), type two diabetes, body fat percentage (15), and muscle mass (23). Similarly, this study further finds that substituting 30 min of SB time for MVPA time is significantly associated with improved body fat percentage, BMI, and WC in a sample of youngest-old to oldest older adults. However, it is important to note that the results did not reach statistical significance in the adjusted model when examining associations in the age group 75 years and above (n = 151), suggesting that effects were stronger in the younger age group (65–74 years, n = 48). The null associations were also apparent when splitting the 75+ age group into middle-old (75–84 years) and oldest-old (85 years and above) and further excluding those who were with underweight nutritional status in two age group. Given that a previous prospective study also indicated that the associations between diet and physical activity and body composition may be weaker in mid to old-older adults because body weight, body fat, and muscle mass are generally lower in aging process (37), these findings warrant further investigation in a larger sample and with a more comprehensive assessment of health lifestyle.
Our results revealed that there were no statistical significance in replacing LPA with SB on obesity indices, while previous studies show that reallocating 30 min from sedentary time to LPA was associated with significant decreases in BMI (15, 21, 38), WC (15, 21), and body fat (38) in older adults. A potential explanation for this finding may be that the average BMI (mean: 24.3 kg/m2) and WC (mean: 85.8 cm) of our sample were lower than those studies (mean BMI: 28.1 kg/m2 and above; mean WC: 107 cm and above). A previous study also indicated that the magnitude of associations between PA and body composition is greater for higher intensity activities (33). As the sample size of this study was relatively small, it is possible that it wasn't sufficiently powered to detect effects of LPA. Our finding showed no effect on the muscle mass. Previous researches have investigated the above effect on the muscle mass. One cross-sectional study indicated that reallocating 1 h of MVPA time per day instead of SB time was associated with increased muscle mass (23). Another two studies showed that reallocating SB time to LPA time does not affect muscle mass (i.e., fat-free mass index) (38, 39). A possible reason could also be that the average age of our participants is older [80.1 vs. 64.6 (38) and 69.3 years (39)]. Nutrition such as dietary protein (40) and physical activity should be simultaneously considered (41) when maintaining or improving muscle mass. In terms of stratified analysis, the results indicated that the benefits of substituting SB with MVPA were apparent for normal nutritional status older adults. Although there is no study has investigated the association between replacing SB with PA on body composition in older adults at risk of malnutrition, one study implied that protein supplementation plus exercise training is effective in improving lean mass and muscle strength in frail older individuals which emphasized that nutrient intake and physical activity are both important to low weight older adults (32).
The study shows that MVPA is often the primary factor driving the relationship between daily activities and adiposity or obesity. However, reallocating SB time with LPA time is not associated with obesity risks because LPA intensity is not significant enough to reduce body fat or increase muscle mass. This finding is consistent with that of a previous study (23). This study suggests that replacing 30 min of SB with MVPA may be key to preventing obesity in older adults. This study can assist health professionals in designing appropriate strategies to delay age-related physiological decline and reduce the negative influences of an inactive lifestyle on the aging process.
Strengths and limitations
To our knowledge, this is the first study to examine the effect of replacing SB time with LPA or MVPA time on appendicular skeletal muscle mass index by using isotemporal substitution analysis in youngest-old to oldest-old older adults. Moreover, we also measured the nutritional status of older adults as a covariate in the statistical model with the mini nutritional assessment. Because previous literature also indicated that with mini nutritional assessment score is low in elderly subjects with sarcopenia (42) and negatively associated with central obesity (32). Nevertheless, this study has certain limitations. First, the study's cross-sectional design requires interpreting the interchanging results as emphasizing the differences between groups with different activity patterns. Second, the study's sample size is relatively small and uses convenience sampling, and therefore, it cannot represent the Taiwanese population as a whole. Future studies should use a long-term study design and representative sample of older adults in the area. Third, the objective physical activity measurement (triaxial accelerometers, Actigraph GT3X+) cannot detect whether older adults are swimming, sitting, standing, lying down, or taking an afternoon nap. Thus, the time spent in SB, LPA, or MVPA can be over or underestimated. Finally, energy intake was not included in the study. For more comprehensive interventions in older adults' health, other indicators of health status (e.g., well-being and quality of life) is suggested to be included in future studies.
Conclusion
In conclusion, this study has shown that replacing 30 min of SB with MVPA can reduce body fat percentage, BMI, and WC of community-dwelling older adults. The findings also highlight the importance of taking into account different stages of older adulthood as well as nutritional factors when intervening to reduce SB and increase physical activity.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Research Ethics Committee of National Taiwan University Hospital (REC Number: 202008046RINC). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
T-FL: formal analysis and writing—original draft. YL: conceptualization, data curation, and writing—review and editing. M-CH: data curation and writing—review and editing. H-YY, J-HP, and JC: writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Institute of Information and Communications Technology Planning and Evaluation (IITP) grant funded by the Korea Government (MSIT) (No. 2022-0-00501, Development of Wearable Device Assessment Technology).
Acknowledgments
We would like to thank all the corresponding authors and co-author teams of the studies included in this study for providing the data that enabled us to conduct our analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.837213/full#supplementary-material
Abbreviations
SB, sedentary behavior; MVPA, moderate-to-vigorous physical activity; LPA, light physical activity; ASMI, appendicular skeletal mass; WC, waist circumference.
References
1. Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States, Current Population Reports, P25-1140. Washington, DC: U.S. Census Bureau (2014).
2. Ashton HA, Buxton MJ, Day NE, Kim LG, Marteau TM, Scott RA, et al. The multicentre aneurysm screening study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet. (2002) 360:1531–9. doi: 10.1016/S0140-6736(02)11522-4
3. Ida S, Kaneko R, Imataka K, Murata KJC. Relationship between frailty and mortality, hospitalization, and cardiovascular diseases in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. (2019) 18:1–13. doi: 10.1186/s12933-019-0885-2
4. Khanam F, Hossain MB, Mistry SK, Afsana K, Rahman M. Prevalence and risk factors of cardiovascular diseases among Bangladeshi adults: findings from a cross-sectional study. J Epidemiol Global Health. (2019) 9:176. doi: 10.2991/jegh.k.190531.001
5. Piché M-E, Tchernof A, Després J-P. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. (2020) 126:1477–500. doi: 10.1161/CIRCRESAHA.120.316101
6. Peralta M, Ramos M, Lipert A, Martins J, Marques A. Prevalence and trends of overweight and obesity in older adults from 10 European countries from 2005 to 2013. Scand J Public Health. (2018) 46:522–9. doi: 10.1177/1403494818764810
7. Romano E, Ma R, Vancampfort D, Firth J, Felez-Nobrega M, Haro JM, et al. Multimorbidity and obesity in older adults from six low- and middle-income countries. Prev Med. (2021) 153:106816. doi: 10.1016/j.ypmed.2021.106816
8. Stenholm S, Sallinen J, Koster A, Rantanen T, Sainio P, Heliövaara M, et al. Association between obesity history and hand grip strength in older adults—exploring the roles of inflammation and insulin resistance as mediating factors. J Gerontol Ser A. (2011) 66A:341–8. doi: 10.1093/gerona/glq226
9. Vasankari V, Husu P, Vähä-Ypyä H, Suni J, Tokola K, Halonen J, et al. Association of objectively measured sedentary behaviour and physical activity with cardiovascular disease risk. Eur J Prev Cardiol. (2017) 24:1311–8. doi: 10.1177/2047487317711048
10. Katzmarzyk PT, Ross R, Blair SN, Després J-P. Should we target increased physical activity or less sedentary behavior in the battle against cardiovascular disease risk development? Atherosclerosis. (2020) 311:107–15. doi: 10.1016/j.atherosclerosis.2020.07.010
11. Christofoletti M, Sandreschi PF, Manta SW, Confortin SC, Delevatti RS, D'Orsi E, et al. Clustering of physical activity and sedentary behavior associated with body composition in Brazilian older adults. J Aging Phys Act. (2021) 1:1–7. doi: 10.1123/japa.2020-0157
12. Kudo N, Nishide R, Mizutani M, Ogawa S, Tanimura S. Association between the type of physical activity and metabolic syndrome in middle-aged and older adult residents of a semi-mountainous area in Japan. Environ Health Prev Med. (2021) 26:46. doi: 10.1186/s12199-021-00949-x
13. Stessman J, Hammerman-Rozenberg R, Cohen A, Ein-Mor E, Jacobs JM. Physical activity, function, and longevity among the very old. Arch Internal Med. (2009) 169:1476–83. doi: 10.1001/archinternmed.2009.248
14. Jefferis BJ, Parsons TJ, Sartini C, Ash S, Lennon LT, Wannamethee SG, et al. Does duration of physical activity bouts matter for adiposity and metabolic syndrome? A cross-sectional study of older British men. Int J Behav Nutr Phys Act. (2016) 13:1–11. doi: 10.1186/s12966-016-0361-2
15. Galmes-Panades AM, Varela-Mato V, Konieczna J, Wärnberg J, Martínez-González MÁ, Salas-Salvadó J, et al. Isotemporal substitution of inactive time with physical activity and time in bed: cross-sectional associations with cardiometabolic health in the PREDIMED-Plus study. Int J Behav Nutr Phys Act. (2019) 16:137. doi: 10.1186/s12966-019-0892-4
16. McGregor DE, Carson V, Palarea-Albaladejo J, Dall PM, Tremblay MS, Chastin SFM. Compositional analysis of the associations between 24-h movement behaviours and health indicators among adults and older adults from the Canadian health measure survey. Int J Environ Res Public Health. (2018) 15:1779. doi: 10.3390/ijerph15081779
17. World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance. Geneva: World Health Organization (2020).
18. Grgic J, Dumuid D, Bengoechea EG, Shrestha N, Bauman A, Olds T, et al. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: a systematic scoping review of isotemporal substitution studies. Int J Behav Nutr Phys Act. (2018) 15:69. doi: 10.1186/s12966-018-0691-3
19. Mekary RA, Ding EL. Isotemporal substitution as the gold standard model for physical activity epidemiology: why it is the most appropriate for activity time research. Int J Environ Res Public Health. (2019) 16:797. doi: 10.3390/ijerph16050797
20. Pelclová J, Štefelová N, Dumuid D, Pedišić Ž, Hron K, Gába A, et al. Are longitudinal reallocations of time between movement behaviours associated with adiposity among elderly women? A compositional isotemporal substitution analysis. Int J Obes. (2020) 44:857–64. doi: 10.1038/s41366-019-0514-x
21. Colley RC, Michaud I, Garriguet D. Reallocating time between sleep, sedentary and active behaviours: associations with obesity and health in Canadian adults. Health Rep. (2018) 29:3–13. doi: 10.3966/168232812016092603001
22. Rollo S, Antsygina O, Tremblay MS. The whole day matters: understanding 24-h movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. (2020) 9:493–510. doi: 10.1016/j.jshs.2020.07.004
23. Sánchez-Sánchez JL, Mañas A, García-García FJ, Ara I, Carnicero JA, Walter S, et al. Sedentary behaviour, physical activity, and sarcopenia among older adults in the TSHA: isotemporal substitution model. J Cachexia Sarcopenia Muscle. (2019) 10:188–98. doi: 10.1002/jcsm.12369
24. Bilski J, Pierzchalski P, Szczepanik M, Bonior J, Zoladz JA. Multifactorial mechanism of sarcopenia and sarcopenic obesity. Role Phys Exerc Microb Myokines. (2022) 11:160. doi: 10.3390/cells11010160
25. Bosy-Westphal A, Geisler C, Onur S, Korth O, Selberg O, Schrezenmeir J, et al. Value of body fat mass vs. anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes. (2006) 30:475–83. doi: 10.1038/sj.ijo.0803144
26. Huang S-Y, Lee K-T, Chang C-S, Shih Y-C, Chen S-H, Lu X-J, et al. Using deuterium oxide dilution method to validate percent body fat measured by bioelectrical impedance analysis in Taiwanese. Taiwan J Fam Med. (2016) 26:123–34.
27. Walowski CO, Braun W, Maisch MJ, Jensen B, Peine S, Norman K, et al. Reference values for skeletal muscle mass: current concepts and methodological considerations. Nutrients. (2020) 12:755. doi: 10.3390/nu12030755
28. Poggiogalle E, Lubrano C, Sergi G, Coin A, Gnessi L, Mariani S, et al. Sarcopenic obesity and metabolic syndrome in adult Caucasian subjects. J Nutr Health Aging. (2016) 20:958–63. doi: 10.1007/s12603-015-0638-1
29. Ge S, Du Q, Feng X, Liu Y, Wang H, Hai S, et al. Optimal cutoffs for the diagnosis of sarcopenia in older Chinese adults. Front Nutr. (2022) 9:853323. doi: 10.3389/fnut.2022.853323
30. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. (2008) 40:181–8. doi: 10.1249/mss.0b013e31815a51b3
31. Migueles JH, Cadenas-Sanchez C, Ekelund U, Delisle Nyström C, Mora-Gonzalez J, Löf M, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Medi. (2017) 47:1821–45. doi: 10.1007/s40279-017-0716-0
32. Chang CS, Chang Y-F, Liu P-Y, Wu S-J, Chiu C-J, Chen C-Y, et al. Interaction of central obesity and sarcopenia on nutritional status in the community-dwelling older people. Arch Gerontol Geriatr. (2020) 87:104003. doi: 10.1016/j.archger.2019.104003
33. Vaara JP, Vasankari T, Wyss T, Pihlainen K, Ojanen T, Raitanen J, et al. Device-based measures of sedentary time and physical activity are associated with physical fitness and body fat content. Front Sports Act Living. (2020) 2:587789. doi: 10.3389/fspor.2020.587789
34. Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: the mini nutritional assessment as part of the geriatric evaluation. Nutr Rev. (1996) 54(1 Pt 2):S59–65.
35. Kim K-B, Kim K, Kim C, Kang S-J, Kim HJ, Yoon S, et al. Effects of exercise on the body composition and lipid profile of individuals with obesity: a systematic review and meta-analysis. J Obes Metab Syndr. (2019) 28:278–94. doi: 10.7570/jomes.2019.28.4.278
36. Forbes SC, Little JP, Candow DG. Exercise and nutritional interventions for improving aging muscle health. Endocrine. (2012) 42:29–38. doi: 10.1007/s12020-012-9676-1
37. Jungert A, Eichner G, Neuhäuser-Berthold M. Trajectories of body composition during advanced aging in consideration of diet and physical activity: a 20-year longitudinal study. Nutrients. (2020) 12:3626. doi: 10.3390/nu12123626
38. Powell C, Browne LD, Carson BP, Dowd KP, Perry IJ, Kearney PM, et al. Use of compositional data analysis to show estimated changes in cardiometabolic health by reallocating time to light-intensity physical activity in older adults. Sports Med. (2020) 50:205–17. doi: 10.1007/s40279-019-01153-2
39. Gába A, Pelclová J, Štefelová N, Pridalová M, Zajac-Gawlak I, Tlučáková L, et al. Prospective study on sedentary behaviour patterns and changes in body composition parameters in older women: a compositional and isotemporal substitution analysis. Clin Nutr. (2021) 40:2301–7. doi: 10.1016/j.clnu.2020.10.020
40. Putra C, Konow N, Gage M, York CG, Mangano KM. Protein source and muscle health in older adults: a literature review. Nutrients. (2021) 13:743. doi: 10.3390/nu13030743
41. Lai TF, Lin CY, Chou CC, Huang WC, Hsueh MC, Park JH, et al. Independent and joint associations of physical activity and dietary behavior with older adults' lower limb strength. Nutrients. (2020) 12:443. doi: 10.3390/nu12020443
Keywords: adiposity, elderly, accelerometry, body composition, inactivity
Citation: Lai T-F, Liao Y, Hsueh M-C, Yen H-Y, Park J-H and Chang JH (2022) Substituting sedentary time with physical activity in youngest-old to oldest-old community-dwelling older adults: Associations with body composition. Front. Public Health 10:837213. doi: 10.3389/fpubh.2022.837213
Received: 16 December 2021; Accepted: 07 November 2022;
Published: 29 November 2022.
Edited by:
Stephanie Schrempft, Hôpitaux universitaires de Genève (HUG), SwitzerlandReviewed by:
Ann Swartz, University of Wisconsin–Milwaukee, United StatesDiego Christofaro, São Paulo State University, Brazil
Copyright © 2022 Lai, Liao, Hsueh, Yen, Park and Chang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jong-Hwan Park, amhwYXJrMTQ4NUBnbWFpbC5jb20=; Jae Hyeok Chang, a3VsdTczQGdtYWlsLmNvbQ==
 Ting-Fu Lai
Ting-Fu Lai Yung Liao
Yung Liao Ming-Chun Hsueh
Ming-Chun Hsueh Hsin-Yen Yen
Hsin-Yen Yen Jong-Hwan Park
Jong-Hwan Park Jae Hyeok Chang
Jae Hyeok Chang