- 1Department of Medical Social Sciences, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States
- 2Institute for Innovations in Developmental Sciences, Northwestern University, Chicago, IL, United States
- 3Early Neurodevelopment and Mental Health Team, Telethon Kids Institute, Nedlands, WA, Australia
- 4School of Population Health, Curtin University, Bentley, WA, Australia
- 5Department of Psychiatry and Behavioral Sciences, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States
- 6Department of Preventive Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States
- 7Department of Pediatrics, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States
- 8Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
- 9College of Health Solutions, Arizona State University, Tempe, AZ, United States
- 10Department of Population Health Sciences, Spencer Fox Eccles School of Medicine at the University of Utah, Salt Lake City, UT, United States
Translation of developmental science discoveries is impeded by numerous barriers at different stages of the research-to-practice pipeline. Actualization of the vast potential of the developmental sciences to improve children's health and development in the real world is imperative but has not yet been fully realized. In this commentary, we argue that an integrated developmental-implementation sciences framework will result in a translational mindset essential for accelerating real world impact. We delineate key principles and methods of implementation science of salience to the developmental science audience, lay out a potential synthesis between implementation and developmental sciences, provide an illustration of the Mental Health, Earlier Partnership (MHE-P), and set actionable steps for realization. Blending these approaches along with wide-spread adoption of the translational mindset has transformative potential for population-level impact of developmental science discovery.
Introduction
A major obstacle to improving children's health and social-emotional wellbeing is the nature of development itself, including pace, self-righting tendencies, and the formative role of environmental influences (1). This dynamic nature of development undermines decisional certainty in risk determination regarding when to act, with whom, and how. Further, entrenched conceptual and methodologic obstacles fuel a substantial gap between research evidence and application with the intended populations in “real-world” systems (2, 3). Traditional siloing of discovery-oriented and applied developmental sciences and the outdated notion of a sequential translational pipeline are also impediments (4). Contemporary implementation models emphasize a rapid, dynamic and iterative process including continuous evaluation of when evidence is “good enough” to implement (5, 6).
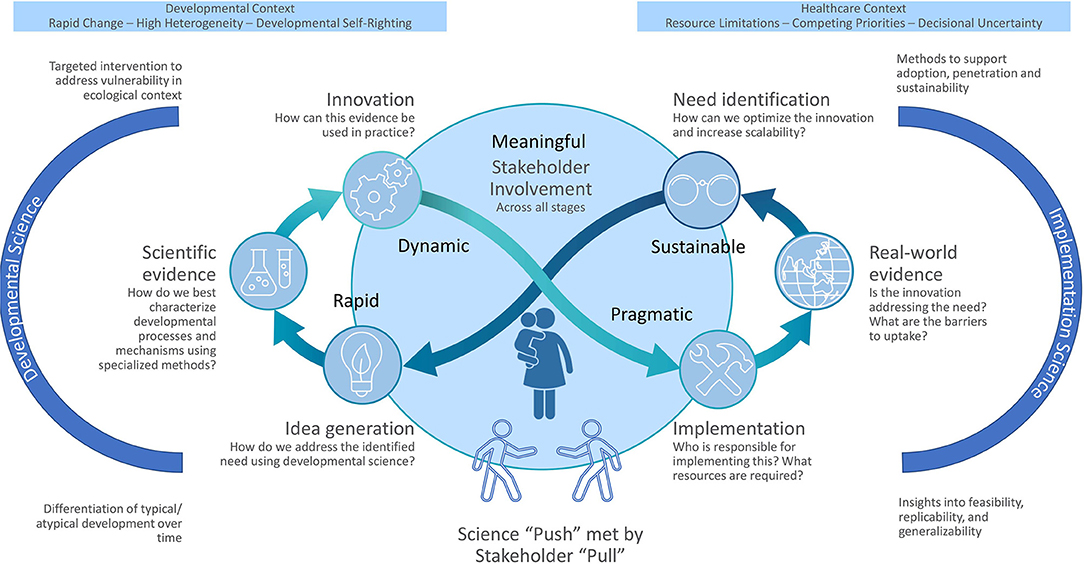
To advance this “science-to-impact quest” (5), we propose an actionable framework integrating developmental and implementation sciences, toward greater integration of translational thinking into the developmental sciences. Developmental science typically focuses on the individual or family, emphasizing in-depth assessments. In contrast, implementation science employs methods to promote systematic uptake, integration, and sustainment of research into real-world delivery systems implementing a policy, practice, tool, or intervention (2, 7). Although implementation science has typically focused on healthcare, it is relevant across multi-sectorial developmental contexts (e.g., childcare, and educational settings) (8, 9). Heuristically, insights from developmental science drive innovations based on characterizing developmental process in context, while implementation science guides real-world uptake of these innovations. However, this process ought not to be sequential or each aim pursued by separate teams (10). Consistent with recursive models (11), Figure 1 highlights this blended developmental-implementation framework. It is bidirectional and continuous, with innovators developing, testing, and “pushing out" discoveries and stakeholders creating “pull” for innovations aligned with needs and preferences as evidence evolves (6). We explicate core implementation science principles, illustrate with a developing initiative, the Mental Health, Earlier Partnership (MHE-P), and lay out future directions.
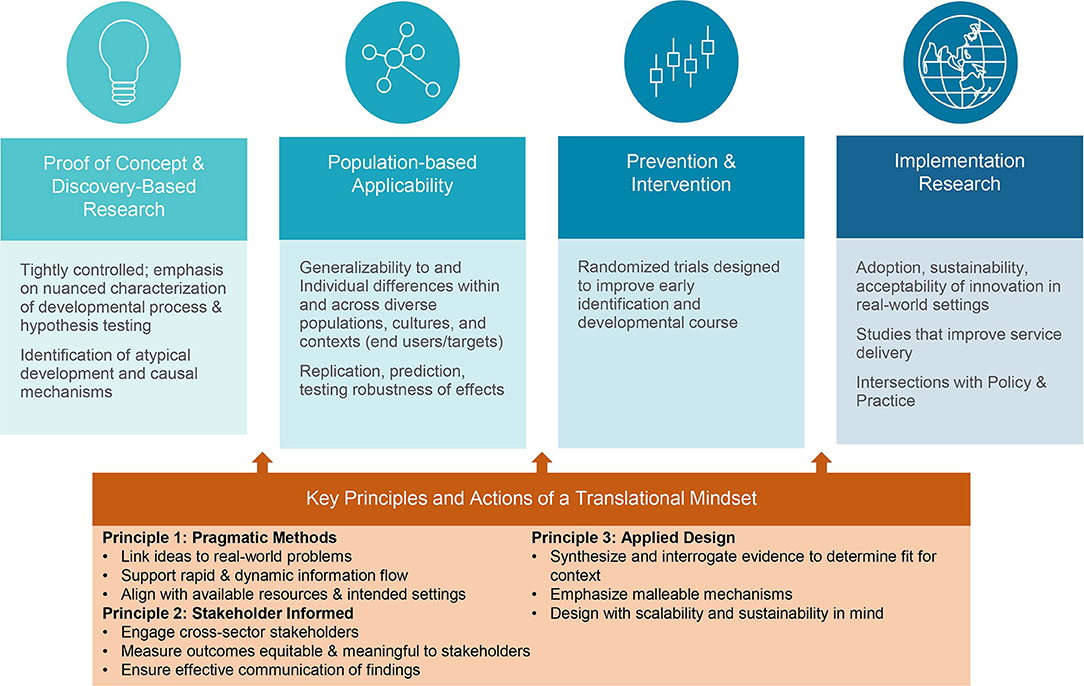
This blended developmental-implementation sciences framework will result in a translational mindset that accelerates research-to-practice application. Translation moves discovery into programs and policies that mitigate problems in human development, health, and functioning (4). Our concept of “translational mindset” is a multi-faceted heuristic concerning how researchers prioritize, formulate, design, enact, and disseminate research. We emphasize mindset rather than action per se because its essence is incorporating these considerations into scientific thinking and innovation (rather than suggesting that all scientists must directly engage in applied implementation endeavors). There are a number of exemplary developmental translational efforts, largely in prevention science [e.g., (5, 12–16)]. However, these are the exception. The translational mindset underscores that for significant impact, research must be formulated with real-world problems in mind. Figure 2 highlights its salience across the developmental science translational sequence (4).
Below are core implementation science principles and their salience to developmental research:
Principle 1: Pragmatic Methods
Pragmatic methods should be generalizable to diverse populations, feasible in real world settings, sensitive to change, publicly available, and developed and tested with efforts to eliminate or reduce potential bias (17). Pragmatic considerations occur from conception through to dissemination (10). A translational mindset requires viewing priorities, pragmatics, and feasibility outside a rarified research context (e.g., minimizing burden on respondents and systems and producing interpretable metrics). Implementation typically relies on brief or automated assessment methods because it requires ongoing data collection in resource-limited settings without specialized supports (2, 18–20). This contrasts with the typical specialized developmental science methods requiring intensive training and in-person assessment. We propose raising pragmatic concerns to an equal position with developmental considerations at the measurement selection table (21, 22). This includes considering what is “good enough” to address specific questions of interest (e.g., when is direct developmental assessment needed vs. a developmental screening questionnaire will suffice), employing modern psychometrics to improve measurement efficiency and weighting intensity of measurement burden in selection (23).
Second, pragmatics involves supporting a dynamic and actionable information flow between researchers and implementation systems (24). The historical separation of evidence-generators from evidence-users creates confusion regarding diffusion of responsibility. Real-world considerations are introduced from the inception including, “who may benefit?,” “how will this be used?,” and “what are uptake barriers?” Achieving a simultaneous push-pull requires iterative exchange between innovators and systems toward bi-directional “fit” (25).
Principle 2. Stakeholder Engagement
Stakeholder engagement at every research stage ensures that aims, methods, and outputs are relevant, equitable, meaningful, and feasible for people and systems for which they are designed. The most groundbreaking discovery will not realize its potential for real-world impact if not framed in a way that matters to stakeholders. While stakeholder engagement diverges from the traditional investigator-driven, lab-based approach of developmental sciences, this reorientation is intended to catalyze the salience and impact of developmental research [for skills relevant to this reorienting see (26)]. The first key action is to identify and engage diverse, cross-sector stakeholders, such as program developers, community members (e.g., caregivers of young children), implementing agents/organizations (e.g., pediatricians, educators, and early interventionists), and systems-level influencers (e.g., policymakers, financers of services). Representation of diverse voices is essential to ensure equitable and meaningful approaches across contexts and groups (27). Varied stakeholder voices contribute a necessary, unique perspective in the complex processes involved in wide-scale implementation and ensuring translatability and acceptability to systems and people who engage with them.
Ongoing engagement of stakeholders with diverse lived and/or professional experiences, and from different sectors, ensures a bi-directional meaning-making process that supports uptake of research evidence. Early in the research process, engagement ensures that research findings are relevant and actionable by measuring outcomes that are meaningful to stakeholders. Stakeholder involvement in interpretation of these outcomes helps ensure equitable research narratives aligned with stakeholder needs and values (28). Finally, ensuring effective communication of findings is key to promoting adoption among diverse stakeholders and supporting engagement in the research translation process (26). This requires going beyond traditional academic outputs to accessible public communication with policy and practice reach.
Principle 3: Applied Design
Central to the translational mindset is a systems perspective that continuously considers whether innovations are scalable and sustainable with equity across diverse real-world contexts. Thus, applied design first involves synthesizing and interrogating evidence to determine fit for context. Our integrated framework leverages developmental science emphasis on individual differences and contextual influences to provide a more nuanced, context-specific approach to implementation of new research evidence (5, 29, 30). Second, researchers are encouraged to emphasize malleable risk and resilience markers and mechanisms, preferably those with corollary evidence-based interventions, to drive impact-focused outcomes [see (12) for accounting of this translational journey]. Finally, researchers must design with scalability and sustainability in mind. For example, when designing a lab-based study to characterize infant cognitive development considering how tasks could ultimately be scaled up for use at a population level (e.g., remote delivery, real time coding, short forms). Implementation must be aligned with routine procedures of real-world systems, without specialized resources (31). This necessitates testing optimal implementation strategies to achieve this (2); [For research designs for testing implementation strategies see (32, 33)].
Mental Health, Earlier Partnership
To illustrate the application of the translational mindset, we present the MHE-P, an evolving developmental science based-implementation initiative advancing our “healthier, earlier” mission (1, 34); [For exemplars of the later stages of this process see (35, 36)]. We share an early-stage project to make this translational mindset come alive, including touching on myriad anticipated challenges [for fuller explication of meeting the challenges to implementation of new innovations in pediatric healthcare, see (8, 31, 37)]. MHE-P is designed to achieve scalable and sustainable implementation of mental health risk identification and health promotion by establishing acceptability to clinicians and caregivers, and generalizability, adaptability, and implementation with fidelity in pediatrics (38). Implementation is to be guided by Figure 1's recursive process to identify needs, priorities, barriers, and facilitators from stakeholders in the design of the MHE-P implementation strategy. Because a key aspect of implementation is distributed leadership (moving from researcher to system-level leader driven) (39), MHE-P leadership includes community health system leaders to ensure a sustainable approach. Active sustainment planning will be key from the outset to engage external stakeholders and align with value-based incentives (38). MHE-P is described illustratively in the steps outlined below by applying a translational mindset to a developmental program of research (“the science of when to worry and when to act”). MHE-P activities are linked to the principles described above and the processes depicted in the center of Figure 1 and noted in italics as appropriate.
Addressing the Need
MHE-P aims to address the challenges inherent to identification and modification of early social-emotional vulnerability presaging mental health risk within pediatric primary care. We determined pediatric primary care to be the optimal translational context to achieve shared goals because: (1) It is a nearly universal, non-stigmatized setting, increasing likelihood of population impact, and (2) monitoring and support of socioemotional development is central to routine well-child visits (40). For the MHE-P, we first engaged with community-based pediatric clinicians (e.g., pediatricians, family medicine physicians, pediatric nurse practitioners) who could help position our goals with issues of high salience to routine pediatric care (Stakeholder Engagement). Challenges include mental health equity considerations, as children from racial-ethnic minorities are less likely to have access to early identification or evidence-based intervention, and more likely to suffer adverse consequences of bias or stigma (41–43). In instances with disparities in prevalence and outcomes, implementation strategies that account for factors, such as history of racial discrimination and access to health care, are essential (27). In MHE-P, we aim to increase equity in early identification of risk and referrals for evidence-based services—a documented disparity among pediatric racial/ethnic minorities (41).
Science “Push” Met by Stakeholder “Pull” (Stakeholder Engagement; Pragmatic Methods)
The beginning of the MHE-P initiative was focused on the process of linking scientific innovations (“Push”) to real world problems in need of solutions (“Pull”). Problem specification within MHE-P started with the research team and our pediatric partners agreeing that presenting concerns about young children's social-emotional wellbeing are common (40) and systems for identification and prevention were deficient (44, 45). The absence of empirical parameters for differentiation of transient and normative behaviors from concerning behaviors impeding risk determination (1). Another barrier to uptake of screening tools for early identification is reluctance to screen because of uncertainty about action/resources upon problem detection (46). This quickly confirmed our hypothesis that a major barrier to effective early identification and prevention was decisional uncertainty (1). Although a number of screening instruments existed, they were lengthy, downward extensions of mental health concepts for older children (e.g., DSM syndromes) that pediatricians did not find particularly useful in the care of young children. Additionally, both parents and providers expressed concern about stigma associated with early identification of mental health risk (30). This pointed us to the need to engage stakeholders in framing communications regarding probabilistic risk that would be developmentally promotive and non-stigmatizing, and conveyed in a developmentally and socio-culturally valid manner (47, 48). As a result, a key goal of MHE-P is developing decision supports and a common, non-stigmatizing language.
Our recent survey of pediatric providers underscores the importance providers place on early identification coupled with significant uncertainty about determining mental health risk and corollary action in children 5 years of age and under (44) (“pull”). The absence of actionable “identify and act” guidance to address socioemotional concerns in young children (49) leads to missed opportunity for mitigating the enduring public, social, and economic impacts linked to neurodevelopmental vulnerability [e.g., (50)]. The real-world problem is the absence of practical tools for decision-making and a clear sightline to action impeding early identification and widespread promotion of young children's social-emotional wellbeing (addressing needs).
Innovation and Need Identification (Stakeholder Engagement; Applied Design)
Fortunately, the “science of when to worry and when to act” is aligned with to the real-world problem of accurately interpreting indicators of risk in early childhood and acting in accordance (1). Thus, developmental measurement tools (51, 52) “embrace” development via operationalizing features that differentiate typical:atypical patterns of emotional dysregulation. As a broad indicator of socio-emotional risk, these measures assess irritability evident in early life that has cross-cutting predictive utility for common internalizing, externalizing, and related adaptational problems (53) (utility of research evidence in practice). However, we soon realized validation of these psychometrically robust tools had no impact on real world practice. Via extensive discussion with pediatric population health and implementation experts, it became clear that this science-to-impact quest would require adoption of a translational mindset, cross-sector collaboration, and a team science approach.
Fit With the Context and Workflow (Stakeholder Engagement; Applied Design)
Alignment with the intended setting and resources was key. Although we had broadly aligned our scientific objectives with the expressed needs of the primary care setting, significant feasibility challenges remained, including: (a) Our irritability survey being too long for routine screening indicating a need to optimize the innovation; (b) the absence of decision supports (e.g., what score signifies that intervention is warranted; also optimize the innovation); (c) complexities of workflow integration and ensuring provider uptake as part of routine care (implementation) and; (d) the disconnect between the science of irritability vs. providers' and caregivers' ideas about social-emotional wellbeing in young children [e.g., the notion of using irritability to determine “probabilistic risk” at the vulnerability phase is a shift from a traditional medical mindset of the presence or absence of disorder (47); “science push-stakeholder pull”]; and (e) the dearth of routinely accessible prevention services for identified children and families (need identification). Thus, these irritability tools needed adaptation (e.g., psychometric reduction; pragmatic), expansion, reframing, and workflow integration based on leveraging contextual resources and pediatric stakeholder input.
The use of health information technologies for integration into the EHR and clinical workflow facilitates sustainment (54, 55) (leveraging contextual resources). EHR-based algorithms are important for improving equitable implementation (27) because quantification reduces reliance on social stereotyping (56). For example, the use of computer adaptive testing for precise, brief irritability screening and generation of a predictive algorithm to guide decision-making would enhance provider motivation and reduce cognitive burden (57). The goal of the algorithm is to ensure reliable and equitable personalized risk estimation through increased precision (particularly reduction of false positives in light of the rapid pace of development in early childhood). The likelihood that neurodevelopmental vulnerability—indicated by elevated irritability—will result in heightened mental health risk, is shaped by the child's unique developmental context. To account for risk amplifying and resilience promoting contextual influences, weighted risk algorithms leveraging routine information available within the EHR can then generate an individual child's risk based on consideration of developmental (e.g., language skills) and social-ecological context (e.g., ACES exposure, responsive family environment) in which behavior is embedded (23).
In this early stage, MHE-P has largely focused on barriers and strategies at the provider level [for other levels -such as, patients/families, insurers and health care providing organizations, see (58, 59)]. A significant and common implementation barrier is the gap between innovation characteristics and the realities of routine clinical care. For example, pediatricians already screen for myriad developmental and social factors. Multiple stakeholder discussions have probed whether the proposed irritability screening and predictive algorithm would link to and/or overlap with that information, adding system burden. This required a clear explication of (a) how computer adaptive irritability screening would occur automatically, (b) be integrated with the EHR, and (c) how the algorithm could reduce burden by integrating other information already collected into a single social-emotional risk score. To ensure tailoring to context, we are in the process of mapping constructs empirically demonstrated to predict mental health risk [e.g., irritability, ACES exposure (60)] to parallel or proxy data collected as part of routine care [e.g., (55)]. Framing risk estimation within non-stigmatizing, strengths-based “health” language necessitates significant input from providers and caregivers.
Linkage to Preventive Intervention (Stakeholder Engagement; Applied Design)
While this addresses the identification challenge (i.e., when to worry), pediatric systems will require similarly scalable and sustainable evidence-based interventions (when/how to act). Further, providers are more likely to feel confident in risk identification if they have an accessible evidence-based solution to refer to. MHE-P proposes coupling early risk identification and decision support with a virtually delivered parenting intervention, the Family Check-Up 4 Health [FCU4Health; (31)]. This program has been implemented in primary care but, consistent with Figure 1, requires adaptation of the implementation strategy for sustainability (61). Thus, the FCU4Health aspect of the proposed prevention system moves from the Implementation Research domain of Figure 2 to the Prevention and Intervention domain, and back. MHE-P will develop a clinical dashboard that informs pediatric providers of families' intervention-related progress aligning with the needs of the primary care system for ongoing provision of clinically useful information. Implementation strategies will be especially geared to identifying barriers to virtual engagement for under-resourced populations (addressing community need) (19).
Conclusions and Future Directions
We propose an actionable translational framework to actualize the potential of developmental sciences to generate population impact in children's health and development. We discuss how principles of implementation science can guide key actions to support developmental scientists adopting a translational mindset, with potential to heighten meaningfulness to stakeholders in child-serving systems and incorporating considerations of systems-oriented socioecological context (62). There is a key role for delivery systems and users to play in enabling, reinforcing and reimbursing evidence-driven preventive care in the developmental vulnerability phase. Meaningful framing and alignment with priorities of primary care stakeholders (caregivers of young children, pediatricians, clinic staff, insurers, health information technology experts, advocacy and policy organizations) was essential to moving the MHE-P initiative forward. Funding systems can also drive this shift to increase public health impact via creative reimagining to support the expanded duration requisite to this translational scope (63). The blending of currently disparate developmental and implementation sciences fields moves the dial toward the realization of healthier, earlier outlooks.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
LW and JS conceived of the study framework. AF-J, LM, AK, CHB, MD, PF, CB, and SK-J participated in different phases of the manuscript conceptualization and refinement process. LW, JS, and AF-J collaborated in the drafting of the manuscript and its finalization. All authors have contributed to, read and approved the manuscript.
Funding
This work was supported in part by grants MH121877 and MH107652 (PI LW), USDA 2018-68001-27550 (PIs CB and JS), DA027828 (PI CHB), and support from Northwestern University Institute for Innovations in Developmental Sciences and Telethon Kids Institute.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer CW declared a past co-authorship with one of the authors JS to the handling editor.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We gratefully acknowledge the contributions of our many MHE-P collaborators.
References
1. Wakschlag LS, Roberts MY, Flynn RM, Smith JD, Krogh-Jespersen S, Kaat AJ, et al. Future directions for early childhood prevention of mental disorders: a road map to mental health, earlier. J Clin Child Adolesc Psychol. (2019) 48:539–54. doi: 10.1080/15374416.2018.1561296
2. Bauer MS, Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. (2020) 283:112376. doi: 10.1016/j.psychres.2019.04.025
3. Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. (2011) 104:510–20. doi: 10.1258/jrsm.2011.110180
4. Gunnar MR, Cicchetti D. Meeting the challenge of translational research in child development: opportunities and roadblocks. In: Minnesota Symposia on Child Psychology. 35. Hoboken, NJ: Wiley Online Library (2009). p. 1–27. doi: 10.1002/9781119466864.ch1
5. Dodge KA. Toward population impact from early childhood psychological interventions. Am Psychol. (2018) 73:1117–29. doi: 10.1037/amp0000393
6. Ramsey AT, Proctor EK, Chambers DA, Garbutt JM, Malone S, Powderly WG, et al. Designing for accelerated translation (dart) of emerging innovations in health. J Clin Transl Sci. (2019) 3:53–8. doi: 10.1017/cts.2019.386
7. Stevens KR, Tobin JN. Introduction to the jcts special issue on dissemination and implementation sciences. J Clin Transl Sci. (2020) 4:149–51. doi: 10.1017/cts.2020.488
8. Hoagwood KE, Purtle J, Spandorfer J, Peth-Pierce R, Horwitz SM. Aligning dissemination and implementation science with health policies to improve children's mental health. Am Psychol. (2020) 75:1130–45. doi: 10.1037/amp0000706
9. Lyon AR, Brewer SK, Areán PA. Leveraging human-centered design to implement modern psychological science: return on an early investment. Am Psychol. (2020) 75:1067–79. doi: 10.1037/amp0000652
10. Kwan BM, Brownson RC, Glasgow RE, Morrato EH, Luke DA. Designing for dissemination and sustainability to promote equitable impacts on health. Annu Rev Public Health. (2022) 43. doi: 10.1146/annurev-publhealth-052220-112457
11. Davis M, Sandberg E, Miranda M (editors). Out-reach, in-reach, in-translation, out-translation (oiio) model: a novel framework for community engaged research. In: American Public Health Association Annual Meeting. Chicago, IL (2015).
12. Shaw DS. Translational issues in the development and prevention of children's early conduct problems. In: Minnesota Symposia on Child Psychology. Hoboken, NJ: Wiley Online Library (2009). 273 p.
13. Blair C, Diamond A. Biological processes in prevention and intervention: the promotion of self-regulation as a means of preventing school failure. Dev Psychopathol. (2008) 20:899–911. doi: 10.1017/S0954579408000436
14. Nelson III CA, Zeanah CH, Fox NA. How early experience shapes human development: the case of psychosocial deprivation. Neural Plast. (2019) 2019:1676285. doi: 10.1155/2019/1676285
15. Rapee RM, Coplan RJ. Conceptual relations between anxiety disorder and fearful temperament. New Dir Child Adolesc Dev. (2010) 2010:17–31. doi: 10.1002/cd.260
16. Pérez-Edgar K, Fox NA. Behavioral Inhibition: Integrating Theory, Research, and Clinical Perspectives. Cham: Springer (2018).
17. Glasgow RE, Riley WT. Pragmatic measures: what they are and why we need them. Am J Prev Med. (2013) 45:237–43. doi: 10.1016/j.amepre.2013.03.010
18. Berkel C, Gallo CG, Sandler IN, Mauricio AM, Smith JD, Brown CH. Redesigning implementation measurement for monitoring and quality improvement in community delivery settings. J Prim Prev. (2019) 40:111–27. doi: 10.1007/s10935-018-00534-z
19. Smith JD, Rafferty MR, Heinemann AW, Meachum MK, Villamar J, Lieber RL, et al. Pragmatic adaptation of implementation research measures for a novel context and multiple professional roles: a factor analysis study. BMC Health Serv Res. (2020) 20:257. doi: 10.1186/s12913-020-05118-4
20. Powell BJ, Stanick CF, Halko HM, Dorsey CN, Weiner BJ, Barwick MA, et al. Toward criteria for pragmatic measurement in implementation research and practice: a stakeholder-driven approach using concept mapping. Implement Sci. (2017) 12:118. doi: 10.1186/s13012-017-0649-x
21. Krogh-Jespersen S, MacNeill LA, Anderson EL, Stroup HE, Harriott EM, Gut E, et al. Disruption leads to methodological and analytic innovation in developmental sciences: recommendations for remote administration and dealing with messy data. Front Psychol. (2022) 12:732312. doi: 10.3389/fpsyg.2021.732312
22. Morris A, Wakschlag L, Krogh-Jespersen S, Fox N, Planalp B, Perlman S, et al. Principles for guiding the selection of early childhood neurodevelopmental risk and resilience measures: healthy brain and child development study as an exemplar. Advers Resil Sci. (2020) 1:247–67. doi: 10.1007/s42844-020-00025-3
23. MacNeill L, Allen N, Poleon R, Vargas T, Osborne K, Damme K, et al. Translating RDoC to real-world impact in developmental psychopathology: A neurodevelopmental framework for application of mental health risk calculators. Develop Psychopathol. (2021) 33:1665–84. doi: 10.1017/S0954579421000651
24. Gallo CG, Berkel C, Mauricio A, Sandler I, Wolchik S, Villamar JA, et al. Implementation methodology from a social systems informatics and engineering perspective applied to a parenting training program. Fam Syst Health. (2021) 39:7–18. doi: 10.1037/fsh0000590
25. Chambers DA, Pintello D, Juliano-Bult D. Capacity-building and training opportunities for implementation science in mental health. Psychiatry Res. (2020) 283:112511. doi: 10.1016/j.psychres.2019.112511
26. Tabak RG, Padek MM, Kerner JF, Stange KC, Proctor EK, Dobbins MJ, et al. Dissemination and implementation science training needs: insights from practitioners and researchers. Am J Prev Med. (2017) 52:S322–9. doi: 10.1016/j.amepre.2016.10.005
27. Smith JD, Davis P, Kho AN. Community-driven health solutions on chicago's south side. Stanford Soc Innovat Rev. (2021) 19:27−9. doi: 10.48558/85p7-3113
28. McNulty M, Smith J, Villamar J, Burnett-Zeigler I, Vermeer W, Benbow N, et al. Implementation research methodologies for achieving scientific equity and health equity. Ethn Dis. (2019) 29(Suppl. 1):83. doi: 10.18865/ed.29.S1.83
29. Finlay-Jones A, Ang JE, Bennett E, Downs J, Kendall S, Kottampally K, et al. Caregiver-mediated interventions to support self-regulation among infants and young children (0-5 years): a protocol for a realist review. BMJ Open. (2021) 11:e046078. doi: 10.1136/bmjopen-2020-046078
30. Shonkoff JP. Making developmental science accessible, usable, and a catalyst for innovation. Appl Dev Sci. (2020) 24:37–42. doi: 10.1080/10888691.2017.1421430
31. Smith JD, Berkel C, Rudo-Stern J, Montaño Z, St George SM, Prado G, et al. The family check-up 4 health (fcu4health): applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care. Front Public Health. (2018) 6:293. doi: 10.3389/fpubh.2018.00293
32. Brown CH, Curran G, Palinkas LA, Aarons GA, Wells KB, Jones L, et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. (2017) 38:1–22. doi: 10.1146/annurev-publhealth-031816-044215
33. Hwang S, Birken SA, Melvin CL, Rohweder CL, Smith JD. Designs and methods for implementation research: advancing the mission of the Ctsa Program. J Clin Transl Sci. (2020) 4:159–67. doi: 10.1017/cts.2020.16
34. Wakschlag L, Smith J, Members Members of the Mental Health Earlier Partnership. What Are We Waiting For? An Action Plan for Real-World Translation of Early Childhood Neurodevelopmentally-Based Identification and Prevention of Mental Health Problems. Newslett Am Psychol Assoc Div 53 Clin Child Psychol. (2021) 37:4–7. https://sccap53.org
35. Palinkas LA, He AS, Choy-Brown M, Hertel AL. Operationalizing social work science through research–practice partnerships:lessons from implementation science. Res Soc Work Pract. (2017) 27:181–8. doi: 10.1177/1049731516666329
36. Ramanadhan S, Davis MM, Armstrong R, Baquero B, Ko LK, Leng JC, et al. Participatory implementation science to increase the impact of evidence-based cancer prevention and control. Cancer Causes Control. (2018) 29:363–9. doi: 10.1007/s10552-018-1008-1
37. Smith JD, Cruden GH, Rojas LM, Van Ryzin M, Fu E, Davis MM, et al. Parenting interventions in pediatric primary care: a systematic review. Pediatrics. (2020) 146:e20193548. doi: 10.1542/peds.2019-3548
38. Fournier AK, Wasserman MR, Jones CF, Beam EL, Gardner EE, Nourjah P, et al. Developing Ahrq's feasibility assessment criteria for wide-scale implementation of patient-centered outcomes research findings. J Gen Intern Med. (2020) 36:1–9. doi: 10.1007/s11606-020-06247-6
39. Brach C, Lenfestey N, Roussel A, Amoozegar J, Sorensen A. Will It Work Here? A Decisionmaker's Guide to Adopting Innovations. Washington DC: Agency for Healthcare Research and Quality US Department of Health and Human Services (2008).
40. Boat TF, Kelleher KJ. Fostering healthy mental, emotional, and behavioral development in child health care. JAMA Pediatr. (2020) 174:745–6. doi: 10.1001/jamapediatrics.2020.1485
41. Alegria M, Vallas M, Pumariega A. Racial and ethnic disparities in pediatric mental health. Child Adolesc Psychiatr Clin N Am. (2010) 19:759–74. doi: 10.1016/j.chc.2010.07.001
42. Davis AE, Perry DF, Rabinovitz L. Expulsion prevention: framework for the role of infant and early childhood mental health consultation in addressing implicit biases. Infant Ment Health J. (2020) 41:327–39. doi: 10.1002/imhj.21847
43. Sabol T, Kessler C, Rogers O, Silver J, A P, Briggs-Gowan M, et al. A window into racial disparities in preschool disciplinary action using developmental methodology. Ann N Y Acad Sci. (2021). doi: 10.1111/nyas.14687
44. Merle J, Carroll AJ, Mohanty N, Berkel C, Scherr C, Davis MM, et al. Pediatric clinicians' perspectives on identification and intervention for young children's social-emotional wellbeing in primary care.
45. Carroll AJ, Knapp AA, Villamar JA, Mohanty N, Burton ND, Coldren E, et al. Engaging primary care clinicians in the selection of implementation strategies for toddler social-emotional health promotion in community health centers.
46. Pinto-Martin JA, Dunkle M, Earls M, Fliedner D, Landes C. Developmental stages of developmental screening: steps to implementation of a successful program. Am J Public Health. (2005) 95:1928–32. doi: 10.2105/AJPH.2004.052167
47. MacDuffie KE, Estes AM, Peay HL, Pruett JR, Wilfond BS. The ethics of predicting autism spectrum disorder in infancy. J Am Acad Child Adolesc Psychiatry. (2021) 1508:123–36. doi: 10.1016/j.jaac.2021.01.006
48. Alegria M, Atkins M, Farmer E, Slaton E, Stelk W. One size does not fit all: taking diversity, culture and context seriously. Adm Policy Ment Health. (2010) 37:48–60. doi: 10.1007/s10488-010-0283-2
49. Finlay-Jones A, Krogh-Jespersen S, Smith J, Wakschlag LS. From “watch and wait” to “identify and act”: a global public health imperative. (2021).
50. Conti G, Heckman JJ. The developmental approach to child and adult health. Pediatrics. (2013) 131(Suppl. 2):S133–41. doi: 10.1542/peds.2013-0252d
51. Wakschlag L, Briggs-Gowan M, Choi S, Nichols S, Kestler J, et al. Advancing a multidimensional, developmental spectrum approach to preschool disruptive behavior. J Am Acad Child Adolesc Psychiatry. (2014) 53:82–96. doi: 10.1016/j.jaac.2013.10.011
52. Krogh-Jespersen S, Kaat AJ, Petitclerc A, Perlman SB, Briggs-Gowen MJ, Burns JL, et al. Calibrating temper loss severity in the transition to toddlerhood: Implications for developmental science. App Develop Sci. (2021). doi: 10.1080/10888691.2021.1995386
53. Wakschlag L, Perlman S, Blair R, Leibenluft E, Briggs-Gowan M, Pine D. The neurodevelopmental basis of early childhood disruptive behavior: irritable and callous phenotypes as exemplars. Am J Psychiatry. (2018) 175:114–30. doi: 10.1176/appi.ajp.2017.17010045
54. Bass M, Rosen KD, Gerend MA, Wakschlag LS, Madkins K, Crosby ST, et al. Development and feasibility of a configurable assessment messaging platform for interventions (CAMPI). Famil Syst Health. (2021) 39:19–28. doi: 10.1037/fsh0000592
55. Oliver D, Spada G, Colling C, Broadbent M, Baldwin H, Patel R, et al. Real-world implementation of precision psychiatry: transdiagnostic risk calculator for the automatic detection of individuals at-risk of psychosis. Schizophr Res. (2021) 227:52–60. doi: 10.1016/j.schres.2020.05.007
56. Lau BD, Haider AH, Streiff MB, Lehmann CU, Kraus PS, Hobson DB, et al. Eliminating healthcare disparities via mandatory clinical decision support: the venous thromboembolism (Vte) example. Med Care. (2015) 53:18. doi: 10.1097/MLR.0000000000000251
57. Van Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. (2003) 93:248–55. doi: 10.2105/AJPH.93.2.248
58. Leslie LK, Mehus CJ, Hawkins JD, Boat T, McCabe MA, Barkin S, et al. Primary health care: potential home for family-focused preventive interventions. Am J Prev Med. (2016) 51(4 Suppl. 2):S106–18. doi: 10.1016/j.amepre.2016.05.014
59. Breitenstein SM, Laurent S, Pabalan L, Risser HJ, Roper P, Saba MT, et al. Implementation findings from an effectiveness-implementation trial of tablet-based parent training in pediatric primary care. Fam Syst Health. (2019) 37:282–90. doi: 10.1037/fsh0000447
60. Wakschlag L, Pool L, MacNeill L, Krogh-Jespersen S, Adam H, Barch D, et al. Predictive utility of irritability” in context”: proof-of-principle for an early childhood mental health risk calculator. (2021).
61. Berkel C, Rudo-Stern J, Abraczinskas M, Wilson C, Lokey F, Flanigan E, et al. Translating evidence-based parenting programs for primary care: stakeholder recommendations for sustainable implementation. J Community Psychol. (2020) 48:1178–93. doi: 10.1002/jcop.22317
62. Briggs RD. Integrated Early Childhood Behavioral Health in Primary Care: A Guide to Implementation and Evaluation. New York, NY: Springer (2016).
Keywords: developmental science, implementation science, translation, impact, research pipeline, team science
Citation: Wakschlag LS, Finlay-Jones AL, MacNeill LA, Kaat AJ, Brown CH, Davis MM, Franklin P, Berkel C, Krogh-Jespersen S and Smith JD (2022) Don't Get Lost in Translation: Integrating Developmental and Implementation Sciences to Accelerate Real-World Impact on Children's Development, Health, and Wellbeing. Front. Public Health 10:827412. doi: 10.3389/fpubh.2022.827412
Received: 23 December 2021; Accepted: 24 March 2022;
Published: 14 April 2022.
Edited by:
Harshad Thakur, Tata Institute of Social Sciences, IndiaReviewed by:
Guillermo Palma, Simón Bolívar University, VenezuelaCourtney Wolk, University of Pennsylvania, United States
Copyright © 2022 Wakschlag, Finlay-Jones, MacNeill, Kaat, Brown, Davis, Franklin, Berkel, Krogh-Jespersen and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lauren S. Wakschlag, bGF1cmlld0Bub3J0aHdlc3Rlcm4uZWR1
 Lauren S. Wakschlag
Lauren S. Wakschlag Amy L. Finlay-Jones
Amy L. Finlay-Jones Leigha A. MacNeill
Leigha A. MacNeill Aaron J. Kaat1,2
Aaron J. Kaat1,2 C. Hendricks Brown
C. Hendricks Brown Matthew M. Davis
Matthew M. Davis Cady Berkel
Cady Berkel Sheila Krogh-Jespersen
Sheila Krogh-Jespersen Justin D. Smith
Justin D. Smith