
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 21 February 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.825585
Background: Health interventions may differently impact adolescents from diverse backgrounds. This study examined whether a smoking preventive intervention was equally effective in preventing cigarette smoking and use of alternative tobacco products (ATPs, i.e., snus, e-cigarettes, and waterpipe) among students from different socioeconomic backgrounds, i.e., occupational social classes (OSC).
Methods: Data was from the school-based intervention X:IT II targeting 13- to 15-year-olds Danes. The intervention focused on three main components: smoke-free school time, smoke-free curriculum, and parental involvement. In total, 46 schools were included at baseline (N = 2,307, response rate = 86.3%). Using a difference-in-differences approach, changes in current smoking and ever use of ATPs were estimated among students in high versus low OSC at second follow-up. Analyses were based on available cases (N = 826) and multiple imputations of missing data at the second follow-up (N = 1,965).
Results: At baseline (age 13), 1.0% of students from high OSC and 4.8% from low OSC currently smoked cigarettes, while this was the case among 24.5 and 25.6%, respectively, at the second follow-up (age 15). Estimates indicated that social inequalities in current smoking diminished over time (p < 0.001). Regarding ATPs, 10.0% of high OSC students and 13.9% of low OSC students had ever used ATPs at baseline, while at second follow-up, 46.8 and 60.8%, respectively, had ever used ATPs. Estimates indicated that social inequalities in ever use of ATPs widened over time (p < 0.001).
Conclusions: The X:IT II intervention seemed to diminish socioeconomic disparities in smoking over the study period. Meanwhile, social inequalities in ever use of ATPs increased. Therefore, besides focusing on narrowing the social disparities in cigarette smoking, future efforts may, to a larger extent, focus on adolescents' use of ATPs.
Smoking remains one of the leading causes of years of life lost and increased morbidity in Denmark and worldwide (1, 2). Globally, a critical political and public health issue is protecting children and adolescents from the health hazards of using tobacco products (3). Individuals initiating a tobacco use in their teenage years are more likely to continue smoking in adulthood, be addicted to nicotine, have issues with smoking cessation, and have higher risks of health adversities in later life (4–6). One significant concern is adolescents' being exposed to smoking in their environment, i.e., among parents, siblings, teachers, or peers (7–9). Specifically, when adolescents see others smoke in their near environment, they are more prone to perceive smoking as socially acceptable and susceptible to smoke themselves. Moreover, second-hand exposure to smoke is considered a health risk in itself (1). Therefore, preventing smoking uptake in adolescence and limiting the exposure of smoking in adolescents' everyday lives may have crucial public health benefits. In Denmark, a continuous goal by stakeholders has been to create a smoke-free future for Danish children (10). For several decades, overall smoking prevalences have decreased, e.g., among Danish schoolchildren, daily smoking had decreased from 18.6% in 1991 to 4.5% in 2014 (11). However, more recent reports indicate changing smoking patterns among the youth population; some numbers show a stagnation in smoking uptake among some parts of the Danish youth (12), while others show decreasing trends in daily but not in occasional smoking (13). In Denmark and internationally, there seems to be a stagnation or even an increase in smoking prevalence among youths from lower socioeconomic backgrounds (11, 14). Additionally, social disparities in smoking have not diminished, quite conversely, research indicates increasing socioeconomic differences in smoking during the last decades (11, 15). Consequently, targeting the socioeconomic differences in smoking is essential in smoking preventive efforts. The social inequalities in tobacco-related harms have also been well-documented internationally (16).
Another increasing public health concern is the use of other tobacco products than conventional cigarettes, including e-cigarettes, smokeless tobacco (e.g., snus), and waterpipe (i.e., alternative tobacco products; ATPs). These products have gained growing interest in a Danish and global context—especially among the youth (17, 18). In fact, there has internationally been an increasing trend in youth use of e-cigarettes, snus, and waterpipe in recent years (18–21). In e.g., USA and Norway, the use of some ATPs has even exceeded the use of conventional cigarettes (22–24). However, the research on socioeconomic differences in the use of ATPs is somewhat inconsistent and limited, with some research indicating a social gradient in the uptake of ATPs among students from different socioeconomic groups (18, 25), while other studies found no socioeconomic differences in the use of ATPs (26–28). Several concerns are linked to the increasing use of ATPs, including health risks and the risk of becoming addicted to nicotine (29, 30). Moreover, adolescents may learn rituals associated with cigarette smoking by using, e.g., e-cigarettes, including the body language, taking smoking breaks, and how to handle a tobacco product (31). Another concern is the concurrent use of multiple tobacco and nicotine products—or that using one tobacco product use may impact decisions to use or try other products. For example, a Norwegian study found that using smokeless tobacco in youth increased the risk of smoking conventional cigarettes in adulthood (32). In this connection, there are concerns that ATPs may be a gateway to conventional cigarette smoking (31, 33), while other studies discuss the common liability hypothesis as a possible explanation for using multiple tobacco products and shifting from one tobacco product to another (34). Given these concerns, tobacco control policies aiming at preventing smoking should focus not only on conventional cigarettes but also on the use of ATPs.
Internationally, a host of interventions have been implemented to reduce smoking uptake among adolescents—many in the school setting—with mixed evidence of their effect (35). One study analyzed data from 49 randomized controlled trials on the effect of smoking preventive interventions (including data from approximately 140,000 schoolchildren) and found a 12% reduction in smoking initiation among children in the intervention groups compared with children in the control groups at more than 1 year follow-up from baseline (35). However, they found no effect at 1 year or less. In a Danish context, one of the first smoking preventive interventions which were found to decrease smoking uptake among adolescents was the X:IT study (36). An evaluation of X:IT indicated that if all intervention components were implemented as intended, X:IT could reduce the proportion of adolescents who smokes up to 25% at 1 year follow up (37). Studies evaluating the effect of preventive interventions on other tobacco products than cigarettes are still very sparse, and research with this aim has been called for in recent years (38).
The effect of school-based smoking and health interventions have been found to differ according to adolescents' socioeconomic backgrounds, although the directions are not unidimensional; some research indicated better intervention effects among students from higher socioeconomic backgrounds (39), while other research found that adolescents from lower socioeconomic backgrounds received the highest benefits of health interventions (40). Consequently, health interventions may both widen or narrow social inequalities in health. In the Danish X:IT study, the process evaluation of the intervention indicated that some aspects of the intervention were more easily adopted by students and parents from higher socioeconomic backgrounds (41). These findings may have important implications for the overall effects of the intervention. To our knowledge, no studies have evaluated socioeconomic differences in the trajectories of ATP use before and after implementing a tobacco preventive intervention.
Considering the limited research evaluating socioeconomic differences in tobacco use after the implementation of a smoking preventive intervention, the current study sought to examine trajectories of cigarette smoking among adolescents participating in a school-based smoking preventive intervention: The X:IT II intervention. Further, as a secondary aim, this study examined trajectories in ATP use across socioeconomic groups during the period. Adolescents were followed over the course of 2 years—from baseline (beginning of grade 7; ~13 years) to second follow-up (end of grade 8; ~15 years).
X:IT II is a school-based intervention with the aim of preventing smoking uptake among students from 7th to 9th grade (13- to 15-year-olds). The intervention consists of multiple initiatives to reduce youth smoking and is inspired by previous successful smoking preventive interventions from Norway and Sweden (42, 43). X:IT II is a modified version of the first X:IT intervention developed in 2010 by the Danish Cancer Society and was evaluated in a cluster-randomized controlled trial (RCT) as well as with a qualitative process evaluation (18). Findings from the RCT showed that students at intervention schools had significantly lower odds of smoking cigarettes compared to students at control schools (OR: 0.61, 95% CI: 0.45–0.82) 1 year after implementation of the intervention (19); thus, the evaluation showed overall positive effects in reducing smoking among students. However, the process evaluation indicated that some of the intervention components (i.e., wording and pictures used) were more easily adopted by students and parents from higher socioeconomic backgrounds (22). Therefore, to address these social inequalities in the adoption of the X:IT intervention, a modified version of the intervention was developed—the X:IT II intervention. The three main intervention components of the X:IT II intervention were (44):
• Smoke-free school time. At the time of the study, Denmark had a much more lenient smoking policy compared with other Scandinavian countries. In 2007, the first law restricting smoking in public places was employed, and in 2012, smoking at school grounds was fully banned for students, employees, and visitors (45). Smoking rules at X:IT II intervention schools are even stricter than national legislations. Hence, schools included in the intervention are encouraged to ensure that neither students, teachers, other employees, nor visitors smoke during school hours—neither at school grounds nor at other places during school hours, e.g., just outside of the school area, at parks, shops, etc. This is also known as “smoke-free school time.”
• Parental involvement. This component consists of two dimensions: 1) smoke-free agreements, which involve that the parent and the child both sign an agreement committing the child not to smoke in the following school year, and 2) smoke-free dialogues between the parent and the child. Here, parents commit to have continuous dialogues with their children about smoking and tobacco use. Parents could receive help for these chats using the website (www.snakomtobak.dk, in English: Chat about Tobacco) developed for the purpose. The website targets several groups of parents, including smoking and non-smoking parents as well as parents with and without children who smoke. At parent–teacher meetings at the beginning of the school year, teachers introduced the website and the X:IT intervention to parents.
• Smoke-free curriculum. The educational material “Up in Smoke” (www.opiroeg.dk) was specifically developed to teach students in 7th to 9th grade about smoking, health risks, the pressure of smoking, etc. The material was based on self-efficacy training and appraisal of outcome expectations and included eight lessons a year over the course of 3 years. It was intended to be cross-curricular and, thus, could fit in with ordinary school activities to prevent excess workload on the teachers. In the revised X:IT II intervention, the general readability of the material was improved, and the automated readability index was lowered, e.g., a glossary appears when clicking on academic words such as “cancer” or “oxygen.”
The participating schools had each assigned a school coordinator, most often a teacher, who coordinated intervention activities at the schools and informed colleagues about the intervention.
This study evaluates the X:IT II intervention after the second year of implementation. The intervention was evaluated over the course of 3 years, from 2017 until 2020. Overall, 300 schools were randomly selected and invited to participate in the evaluation of which 57 schools accepted the invitation. However, prior to the baseline data collection, 11 schools withdrew their participation: two schools had hired new school leaders who chose not to prioritize the intervention; two schools had to prioritize other projects because they were involved in more projects at once; and seven schools responded that they did not have time to participate. In total, the baseline measurement consisted of 46 schools across Denmark (Figure 1). Data collection consisted of online self-reported surveys to students and school coordinators at the beginning of 7th grade (baseline) until the end of 9th grade (third follow-up measurement). The school coordinator handled the data collection among students.
This study utilized data from baseline and the second follow-up measurement (at the end of 8th grade in 2019). All students at the 46 enrolled schools were encouraged to participate in the study (N = 2,307). Out of all eligible students, 1,989 students (response rate = 86.3%) answered the baseline questionnaire. At second follow-up, 1,148 students responded to the questionnaire out of 1,625 eligible students (response rate = 70.6%). In total, information on both baseline and second follow-up were obtained from 826 students, and 1,965 students had available information in the imputed data set. The current study evaluates the effect of the X:IT II intervention as pre-specified in Current Controlled Trials (ISRCTN31292019).
The outcome measure of current smoking was assessed by dichotomizing students' responses to the question “How often do you smoke?” into currently smoking (daily, weekly, monthly, or more seldom) vs. do not smoke.
The outcome measure of ATP use was assessed by three questions; hence, students were asked if they had ever used one of the following products: snus, e-cigarettes, and waterpipe, respectively. Response categories ranged from a single time and up to more than 40 times. We dichotomized the variable into 1 = had ever used ATPs (i.e., either snus, e-cigarettes, or waterpipe) and 0 = had never used ATPs.
Socioeconomic position was assessed by two questions about the occupation of students' father and mother (OSC). OSC was coded in accordance with the Danish Occupational Social Class Measurement (46) and was categorized from I = high to V = low social class as well as VI = parents receiving social benefits. The highest-ranking parent determined the OSC. OSC was categorized into three groups: high (I to II), medium (III to IV), and low (V to VI). Previous research has found students to be generally able to answer questions about their parents' occupation status with fair validity (47).
Due to well-established gender differences in smoking uptake and use (48), analyses were adjusted for gender. Gender was assessed with the question “are you a boy or a girl?” with response options 1 = boy, 2 = girl, and 3 = students who felt they did not fit into neither of the two first categories. Students in the last category (1.3% of students) were excluded for further analyses.
A difference-in-differences design was used to evaluate the effect of X:IT II on current smoking and ever use of ATPs according to students' OSC. The difference-in-difference method is considered a useful approach for assessing the impact of interventions by estimating the trajectories of change between two groups before and after receiving a treatment. This method is particularly useful in non-randomized study designs with no obvious control groups (49). Hence, using this approach, trajectories of change in current smoking and ever use of ATPs were estimated before and after the implementation of X:IT II among students in two groups; students from high and low OSC, respectively. High OSC served as the comparison group (group C), while low OSC was considered the exposed group (group E), as the X:IT II intervention was modified to specifically target students from low OSC. Changes in outcomes were estimated as (Cafter–Cbefore)–(Eafter–Ebefore). When difference-in-differences estimates are close to zero, the intervention is expected to be equally effective among students across their OSC. Analyses were based on available cases (N = 690), which comprised the proportion of students participating in both the baseline and the second follow-up measurement, and who had responded to the OSC measure as well as measures about tobacco product use at baseline and second follow-up. All analyses were carried out using SAS v. 9.4.
The analyses were based on multiple imputations of missing data at the second follow-up measurement (N = 78.600). Imputations of missing data were based on several variables in the baseline dataset commonly associated with smoking (i.e., gender, smoking frequency, ethnicity, OSC, intention to smoke, exposure to smoking at home and school, and parents' attitudes about smoking). First, baseline variables were imputed to ensure a monotone pattern of missing observations in the baseline dataset. Secondly, smoking frequency at second follow-up was imputed using multistage imputation. Because of intraclass correlations between schools and classes, two times 20 rounds of imputations were carried out. First, the school and class effects were overestimated on the standard errors by including the school and class variables as fixed effects in the imputation model. Thereafter, school and class effects were underestimated on the standard errors by not including school and class variables as effects in the imputation model. In total, 40 imputed data sets were created, and as suggested by Graham (50), analyses of these data sets should provide a pragmatic evaluation of the standard error. The PROC MI procedure in SAS was used with a repeated statement for unadjusted analyses and analyses adjusted for gender. The 40 imputed data sets were analyzed with a random-effect logistic regression model including the same variables as used in the analysis of available cases. The results were collected with the PROC MIANALYZE procedure. The same procedure undertaken for the analyses concerning current smoking was used for ever use of ATPs.
Power calculations were conducted in accordance with Donner and Klar (51) based on the following assumptions: each school cluster comprised 50 students; the intraclass correlation coefficient for current smoking among 15-year-olds was 0.053; the smoking prevalence in 9th grade was 17.9%; and the expected reduction in smoking was 25% (i.e., from 17.9% to 13.4%) with a power of 80%. These calculations showed a need for 48 schools comprising around 2,400 students.
As presented in Table 1A, 826 participants were eligible for analyses who both answered the baseline measurement as well as the second follow-up measurement. In total, 1,139 (58.0%) were considered non-participants, i.e., they did not respond to the second follow-up measurement. More students from a low and medium OSC, who currently smoke, and who have ever used ATPs did not respond to the second follow-up.
Table 1B outlines a more comprehensive overview of the participants and non-participants in relation to the use of various ATPs; overall, results show that more students who had ever used waterpipe, snus, and e-cigarettes missed responding at second follow-up.
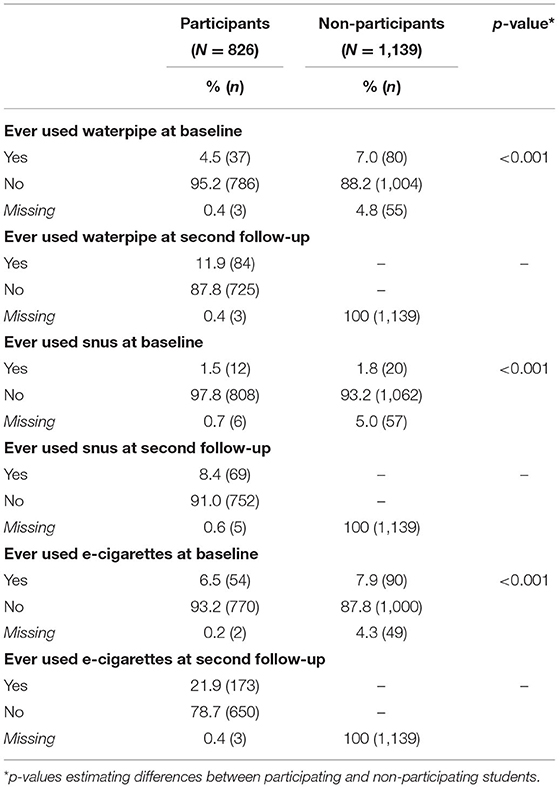
Table 1B. Characteristics of participants and non-participants in the second follow-up, ever use of ATPs (N = 1,965).
Table 2 displays descriptive information of baseline cases and imputed cases. Overall, no marked differences are seen between baseline cases and imputed cases in relation to gender as well as current smoking and ever use of ATPs at baseline; however, more students currently smoke (23.8 vs. 8.4%) and have ever used ATPs (49.7 vs. 25.4%) at second follow-up in the imputed cases compared with the baseline cases.
Table 3 shows the results of the difference-in-differences analyses of current smoking between socioeconomic groups. Adjusted for gender, the analyses of available cases showed that 0.3% of students from a high OSC currently smoked at baseline, while this was the case for 3.0% of students from a low OSC. At second follow-up, 8.3% of students from a high OSC and 10.9% of students from a low OSC currently smoked cigarettes. The adjusted difference-in-differences analysis of available cases showed an estimate close to zero, and the interaction term between OSC and time was insignificant. This indicates that there were no socioeconomic differences in smoking trajectories between OSC groups. However, the unadjusted and adjusted difference-in-differences analysis of imputed cases showed a somewhat different pattern. Adjusted for gender, 1% of the high OSC students were currently smoking at baseline, while this applied to 4.8% among students from a low OSC. At follow-up, 24.5% of the students from a high OSC and 25.6% from a low OSC were currently smoking.
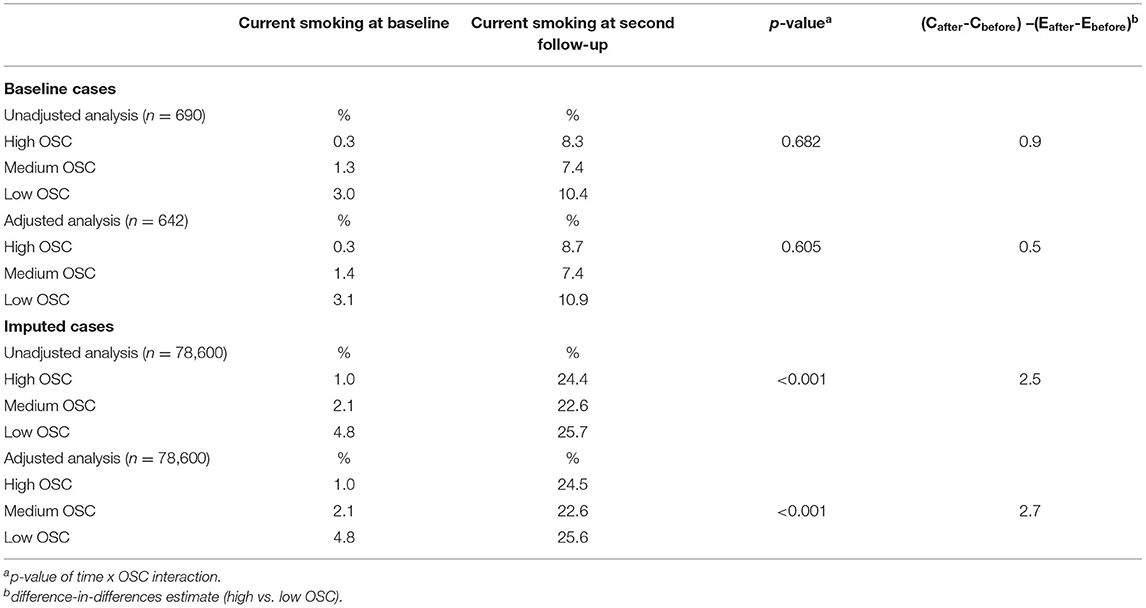
Table 3. Difference-in-differences analyses of current smoking by occupational social class (OSC): analyses of available cases and imputed cases, unadjusted and adjusted for gender.
Results showed that relative more students from a high OSC were currently smoking at second follow up relative to baseline compared with students from a low OSC (see also Figure 2); hence, indicating differential trajectories from baseline to second follow-up in current smoking among students from low and high OSC (p < 0.001).
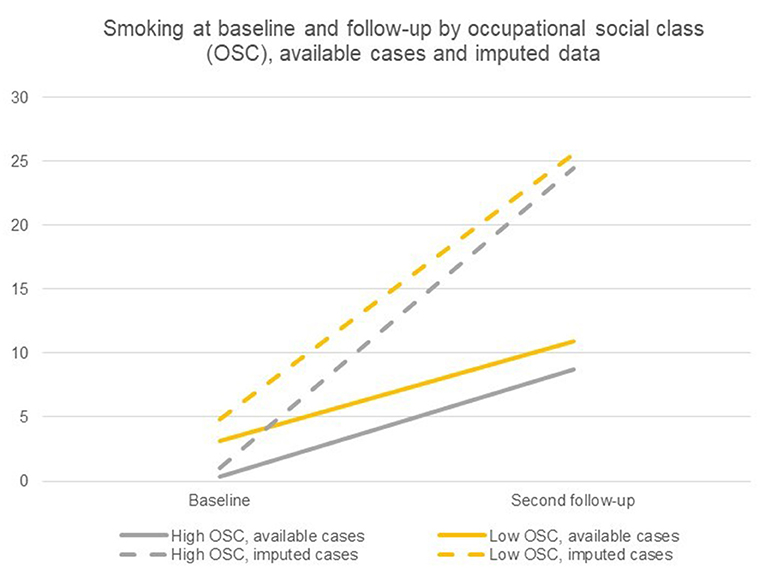
Figure 2. Current smoking at baseline and second follow-up by occupational social class (OSC), available cases and imputed cases.
Table 4 displays the difference-in-differences analyses of ever use of ATPs stratified by OSC of students. In adjusted analyses for gender of available cases, results showed that 7.6% of students from a high OSC and 11.6% from a low OSC had ever used ATPs at baseline. At second follow-up, 8.3% of students from a high OSC and 10.9% from a low OSC had ever used ATPs. The adjusted difference-in-differences analysis of imputed cases showed a similar pattern, although differences between OSC groups were more pronounced; adjusted for gender, 10.0% of students from a high OSC and 13.9% of students from a low OSC had ever used ATPs at baseline. At second follow-up, 46.8% of students from a high OSC and 60.8% of students from a low OSC had ever used ATPs.
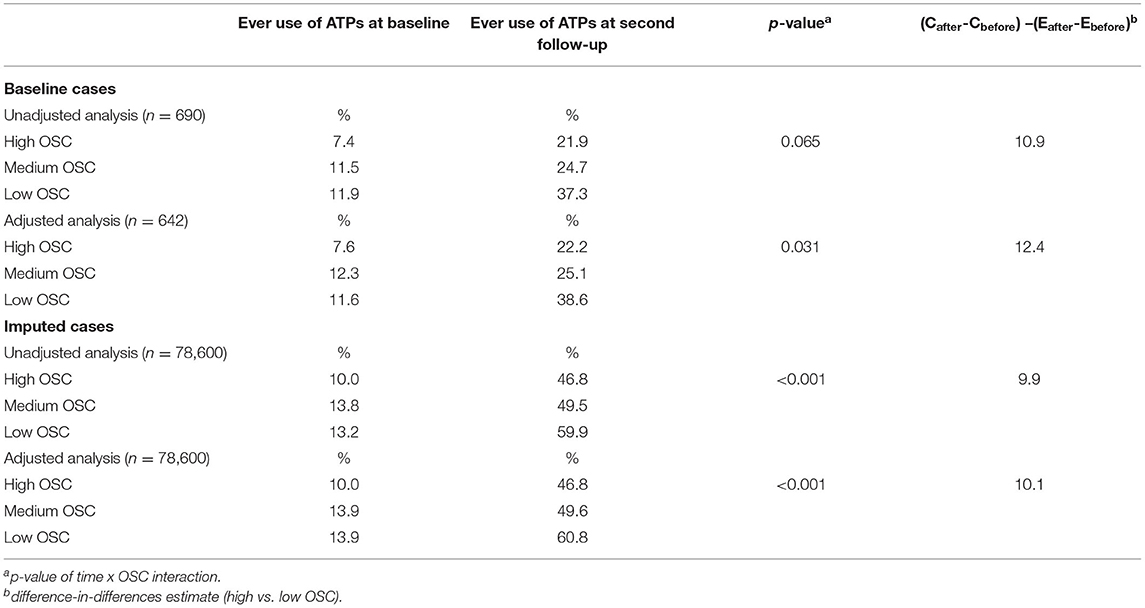
Table 4. Difference-in-differences analyses of ever use of alternative tobacco products (ATPs) by occupational social class (OSC): analyses of available cases and imputed cases, unadjusted and adjusted for gender.
The difference-in-differences estimates for the adjusted difference-in-differences analysis of available cases and imputed data indicated substantial differences in trajectories of ever use of ATPs between OSC groups (p < 0.001). Hence, relative more students from a low OSC had ever used ATPs at second follow up relative to baseline compared with students from a high OSC (see also Figure 3).
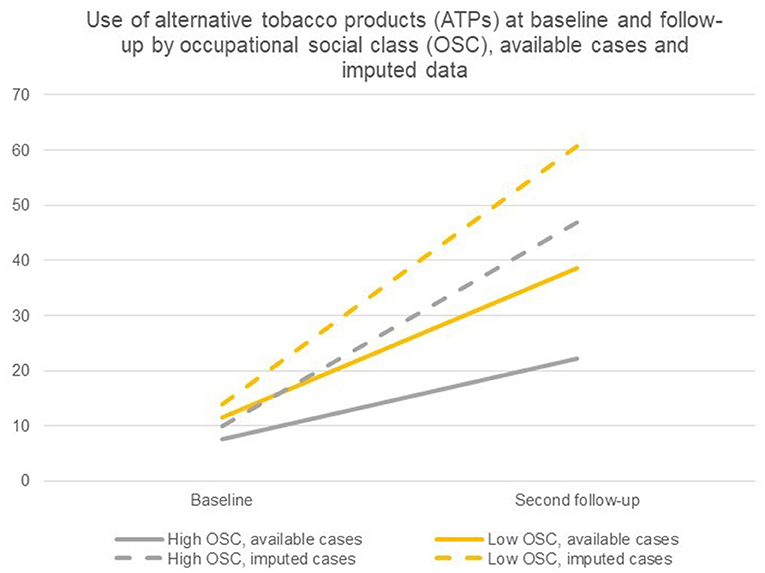
Figure 3. Ever use of ATPs at baseline and second follow-up by occupational social class (OSC), available cases and imputed cases.
This study is among the first to examine differential trajectories of smoking and ATP use between socioeconomic groups before and after implementation of a smoking preventive intervention. Findings provide crucial knowledge for current and future actions against youth tobacco use, as initiatives should focus on benefiting all groups equally—or benefit the groups most in need of prevention efforts.
First, in line with most research (11), this study found that more students from low OSC were currently smoking cigarettes compared with adolescents from high OSC at baseline. However, from baseline to second follow-up, smoking developed somewhat differently among students from diverse socioeconomic backgrounds. Importantly, the gap in current smoking between students from low and high OSC narrowed over time from a difference of almost four percentage points at baseline to about one percentage point at second follow-up. In a recent study, we investigated trajectories of current smoking between OSC groups from baseline to first follow-up, i.e., at the end of grade 7 (52). The study indicated that X:IT II did not create differential trajectories in current smoking among adolescents from diverging socioeconomic backgrounds over the course of one school year. In the present study, students are followed until the end of grade 8 and thus, findings from the current study indicate that tobacco patterns have developed differently at this point in the intervention compared with the first follow-up measurement. Nevertheless, these findings should be viewed positively in the sense that the X:IT II intervention seems to be more beneficial for some groups of adolescents at higher risk of smoking cigarettes, i.e., from a low OSC. Thus, the intervention did not widen the social inequalities in smoking. Considering these findings, the X:IT II seems to be successful in targeting students from lower socioeconomic backgrounds. Similarly, a review by Tinner et al. (40) suggested that adolescents with lower socioeconomic positions benefited most from smoking preventive initiatives. However, there is generally a dearth of literature examining socioeconomic differences in the effect of smoking preventive interventions. The X:IT II intervention builds on a multilevel approach in which several components on individual and environmental levels are initiated to reduce adolescent smoking. This approach is considered ideal for limiting the social inequalities in intervention effects, while interventions solely aiming at the individual level may increase social inequalities (53).
From this study, we do not have knowledge about the development in smoking among adolescents unexposed to the intervention, although knowledge builds on previous findings from the first X:IT intervention with both an exposed and unexposed group. Some of the socioeconomic effects in smoking may have been impacted by an overall societal focus on decreasing smoking among youth, with increasing political actions against smoking (45). In this connection, one Danish study showed that the absolute socioeconomic differences in smoking decreased during the past decade; however, the relative socioeconomic differences in smoking increased during the same period, and smoking remained highest among students in the lowest socioeconomic group during the entire study period from 1991 to 2014 (11). Findings from other westernized countries also suggest rather stable or increasing socioeconomic differences in smoking over time (15, 54). As most political actions were in effect after implementation of this study (45), these initiatives were not expected to impact the study results. Future research may further investigate whether socioeconomic differences in smoking are influenced by the recent increased political and societal attention to smoking–these studies would also be fruitful for investigating whether trajectories in smoking varies over time for adolescents unexposed to intervention components.
Secondly, this study examined trajectories in ever use of ATPs between OSC groups. At baseline, more students from low OSC compared to high OSC had ever used ATPs. However, conversely to the development in current smoking during the study period, the socioeconomic differences in ever use of ATPs widened over time. There may be several mechanisms to explain these findings. First and foremost, the intervention was designed to prevent cigarette smoking uptake among students (44) and, thus, it was not a primary aim of the intervention to prevent the uptake of other tobacco products. Nonetheless, it has previously been discussed whether smoking preventive interventions may be effective in also reducing the use of ATPs as several characteristics associated with cigarette smoking are associated with ATP use (55). Consequently, many of the same mechanisms or pathways to cigarette smoking may apply to ATP use. However, a main focus on reducing cigarette smoking among adolescents may have some unfortunate side effects, e.g., pushing some groups of youths toward using other substances which may not be seen as just as harmful or damaging to health compared with conventional cigarettes. Our study may reflect this tendency. This may be due to the X:IT II intervention itself, which focused on cigarette smoking, combined with the current societal tendencies where laws on conventional cigarettes have been tightened substantially in recent years (45). The most recent adopted Danish law comprises several initiatives to prevent especially youth smoking and use of other tobacco and nicotine products, e.g., e-cigarettes, although these were not initiated at the time of the study. Moreover, in a recent study among students enrolled in the X:IT II intervention, students reported that knowing smoking is dangerous and not wanting to be addicted to smoking were the top reasons for not smoking cigarettes. These findings indicate a high awareness of the health-damaging effects of cigarette smoking (56). However, we do not have knowledge about students' reasoning toward using or not using ATPs.
The few studies that have evaluated the influence of tobacco prevention interventions on students' use of other tobacco products than conventional cigarettes have shown mixed results (57, 58). For example, an evaluation of an outdoor smoking ban found no impact on students' use of e-cigarettes and waterpipe at follow-up (57). In contrast Hedman et al. (58) found a lower prevalence of snus use among students in the intervention group compared with the control group. Here, the intervention comprised tobacco-free contracts and education in tobacco-related health issues. These findings indicate that interventions with multiple initiatives aiming at ATPs may potentially impact students' decisions about ATP use. The intervention components of X:IT II comprise parental involvement, including smoke-free agreements, as well as smoke-free school time, and smoke-free educational material. Thus, extending current intervention components to increase awareness and knowledge about ATPs may produce positive outcomes. However, none of the identified studies evaluated subgroup effects of the interventions in terms of students' socioeconomic backgrounds. As the use of ATPs is increasingly prevalent among adolescents, there is an urgent need for future research to examine the effect of prevention efforts on ATPs and whether the effect differs between socioeconomic groups.
The X:IT II intervention was based on a previously shown effective intervention in reducing smoking uptake evaluated in a large cluster-randomized controlled trial (36, 37). In this study, all schools were included as intervention schools, and the differential effects of the intervention between socioeconomic groups were evaluated utilizing a difference-in-differences design (44). Power calculations estimated a need for 48 schools which was fulfilled in the recruitment process where 57 schools agreed to participate. However, 11 schools withdrew from the study, leaving 46 schools enrolled in the baseline data collection. We were, nonetheless, very close to the calculated number of schools required for evaluating the X:IT II intervention. Further, schools enrolled in the X:IT II study are representative to Danish schools of schools nationwide in regard to organizational resources, enrolled number of students at schools, average grades, and students with foreign origin, although more public schools participated in the X:IT II study (59). To account for possible bias due to drop-out over time, we applied multiple imputation of data at second follow-up. In the imputation phase, 40 datasets were created with over- and underestimation of the school and class effects to account for intraclass correlations between school and classes. The social environment across schools as well as the intensity of the intervention may also vary between schools. However, as the aim of this study was to examine differential effects between students from high vs. low OSC, the differences between schools may not be that important in this specific study. We know that implementation most likely varies across schools—as was the case in the evaluation of the first X:IT intervention (60)—however, we do not expect implementation at the school level to be influenced by the individual level of OSC.
The two key assumptions behind the difference-in-differences approach are 1) parallel trends and 2) common shocks. It is thus assumed that parallel trends will occur between the exposed group and the comparison group before intervention and after the implementation of the intervention. As smoking is more common among students from low OSC compared with high OSC, this assumption was not fulfilled. Nonetheless, very few students smoke at the beginning of grade 7, and therefore, estimates for calculation of trends will be low and—at least to some extent—unreliable. The assumption of common shocks is that any event during or after the intervention will equally affect the exposure and comparison groups. This assumption is expected to be fulfilled as there is no reason to assume differences between the groups.
We used students' self-reporting of OSC which is a commonly used measure of students' socioeconomic backgrounds, i.e., it has been used in the Danish contribution to the WHO collaborative study “Health Behavior in School-aged Children study” for more than 20 years (11). The coding of OSC in Danish studies is adapted to the Danish labor market and is comparable to other measures utilized, e.g., the British Registrar General's social classification and the European socioeconomic classification (46, 61). The measure of OSC used in this study assesses both occupational skills and competencies necessary for the job as well as the power and control associated with the job position. Previous research has found that self-reports of parental occupation is a more valid measure of socioeconomic position than parental education (44). The measures used in this study to assess tobacco use among adolescents, i.e., current cigarette smoking and ever use of ATPs, respectively, were not directly comparable. Unfortunately, we did not have information about current use of ATPs. It could be that the intervention components were better suited for preventing current use more so than ever use, as the main outcome for the evaluation was current smoking. Thus, future research may further examine the impact of interventions on adolescents' current use of ATPs.
Findings from the current study have several important implications. Specifically, findings suggest that the X:IT II intervention decreased socioeconomic inequalities in smoking over time. This is an important finding as adolescents from lower socioeconomic backgrounds are more at risk of using tobacco products (11). X:IT II was implemented in Danish lower secondary schools. The embeddedness in the school arena provides an ideal setting for reaching all children and adolescents regardless of their individual backgrounds. Therefore, the X:IT II intervention may be considered ideal for preventing smoking uptake among schoolchildren and adolescents. Nonetheless, this study also indicated that social inequalities in ever use of ATPs widened over time, with students from lower socioeconomic backgrounds being substantially more prone to have ever used these products. This may call for special attention in the design of preventive initiatives to account for the increasing use of and interest in ATPs among youth. As the current research on differential socioeconomic effects in tobacco preventive interventions is sparse, future research should be designed to address this lacking knowledge in subgroup effects of interventions. Moreover, a future area of research could be to examine the mechanisms in which socioeconomic differences in tobacco product use occur after the implementation of a tobacco preventive intervention.
This study found that socioeconomic disparities in cigarette smoking narrowed over a 2 year-period in which a smoking preventive intervention (X:IT II) was implemented. X:IT II was designed to appeal equally to students from lower and higher socioeconomic backgrounds. Hence, this study indicates promising findings in impacting decisions about smoking among students from lower socioeconomic backgrounds. However, the current study found that social disparities in ever use of ATPs widened over the study period. As this study is among the first to examine differential trajectories of smoking and ATP use between socioeconomic groups before and after the implementation of a smoking preventive intervention, more research in this area is needed.
Data that support the findings of this available from the University of Southern Denmark (SDU). Restrictions to the availability of data that were used under license and are therefore publicly available. However, data are available from the corresponding upon reasonable request and with permission of SDU. Requests to access datasets should be directed to Simone Gad Kjeld, simk@sdu.dk.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements. However, parents of students received written information sent out by the schools and were verbally informed at a parents-teacher meeting about the purposes of this study and that participation of their child was voluntary. Further, students were verbally informed by the teachers before answering the questionnaires, and written information about the study was provided in the beginning of the questionnaire, including that students' participation was voluntary, and that their answers would be treated with confidence.
SK, LL, SA, and LB conceptualized and designed this study. LL carried out the main analyses. SK drafted the initial manuscript. LL, SA, and LB critically reviewed and revised the manuscript. All authors read and approved the final manuscript.
This study was funded by the Danish Cancer Society. The Danish Cancer Society developed the intervention. The funding body was not involved in the design of the study, collection, analyses, interpretation of data, nor in the writing of the manuscript, and in the decision to submit the manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The X:IT II project group would like to thank all participating schools, students, parents, teachers, and principals.
OSC, Family occupational social class; ATPs, Alternative tobacco products.
1. US Department of Health Human Services. The Health Consequences of Smoking−50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health (2014).
2. Eriksen L, Davidsen M, Jensen HAR, Ryd JT, Strøbæk L, White ED, et al. Sygdomsbyrden i Danmark: Risikofaktorer [The Disease Burden in Denmark: Risk Factors]. The Danish Health Authority (2016).
3. Clark H, Coll-Seck AM, Banerjee A, Peterson S, Dalglish SL, Ameratunga S, et al. A future for the world's children? A WHO–UNICEF–Lancet Commission. Lancet. (2020) 395:605–58. doi: 10.1016/S0140-6736(19)32540-1
4. Leslie FM. Unique, long-term effects of nicotine on adolescent brain. Pharmacol Biochem Behav. (2020) 197:173010. doi: 10.1016/j.pbb.2020.173010
5. Chassin L, Presson CC, Sherman SJ, Edwards DA. The natural history of cigarette smoking: predicting young-adult smoking outcomes from adolescent smoking patterns. Health Psychol. (1990) 9:701. doi: 10.1037/0278-6133.9.6.701
6. Pisinger C, Vestbo J, Borch-Johnsen K, Jørgensen T. Smoking cessation intervention in a large randomised population-based study. The Inter99 study. Prev Med. (2005) 40:285–92. doi: 10.1016/j.ypmed.2004.06.001
7. Poulsen L, Osler M, Roberts C, Due P, Damsgaard M, Holstein B. Exposure to teachers smoking and adolescent smoking behaviour: analysis of cross sectional data from Denmark. Tob Control. (2002) 11:246–51. doi: 10.1136/tc.11.3.246
8. Mays D, Gilman SE, Rende R, Luta G, Tercyak KP, Niaura RS. Parental smoking exposure and adolescent smoking trajectories. Pediatrics. (2014) 133:983–91. doi: 10.1542/peds.2013-3003
9. Kristjansson AL, Sigfusdottir ID, James JE, Allegrante JP, Helgason AR. Perceived parental reactions and peer respect as predictors of adolescent cigarette smoking and alcohol use. Addict Behav. (2010) 35:256–9. doi: 10.1016/j.addbeh.2009.10.002
11. Holstein BE, Andersen A, Damsgaard MT, Due P, Bast LS, Rasmussen M. Trends in socioeconomic differences in daily smoking among 15-year-old Danes 1991–2014. Scand J Public Health. (2019) 48:667–73. doi: 10.1177/1403494819848284
12. Hoffmann SH, Schramm S, Jarlstrup NS, Christensen AI. Danskernes Rygevaner: Udvikling fra 1994 til 2017. [Smoking Habits Among Danish Citisens. The Development From 1994 to 2017]. Copenhagen: National Institute of Public Health (2018).
13. Brink A-L, Stage M. Røgfri Fremtids Ungeundersøgelse 2017–2020. [The Youth Study of Smokefree Future 2017-2020]. Danish Cancer Society and the TrygFoundation (2021).
14. Knaappila N, Marttunen M, Fröjd S, Lindberg N, Kaltiala-Heino R. Socioeconomic trends in adolescent smoking in Finland from 2000 to 2015. J Adolesc Health. (2019) 64:776–82. doi: 10.1016/j.jadohealth.2018.11.017
15. de Looze M, ter Bogt T, Hublet A, Kuntsche E, Richter M, Zsiros E, et al. Trends in educational differences in adolescent daily smoking across Europe, 2002–10. Eur J Public Health. (2013) 23:846–52. doi: 10.1093/eurpub/ckt022
16. Loring B. Tobacco and Inequities: Guidance for Addressing Inequities in Tobacco-Related Harm: World Health Organization. Regional Office for Europe (2014).
17. Goniewicz ML, Gawron M, Nadolska J, Balwicki L, Sobczak A. Rise in electronic cigarette use among adolescents in Poland. J Adolesc Health. (2014) 55:713–5. doi: 10.1016/j.jadohealth.2014.07.015
18. Kinnunen JM, Ollila H, Lindfors PL, Rimpelä AH. Changes in electronic cigarette use from 2013 to 2015 and reasons for use among Finnish adolescents. Int J Environ Res Public Health. (2016) 13:1114. doi: 10.3390/ijerph13111114
19. Rasmussen M, Kierkegaard L, Rosenwein SV, Holstein BE, Damsgaard MT, Due P. Skolebørnsundersøgelsen 2018: Helbred, Trivsel og Sundhedsadfærd Blandt 11-, 13- og 15-Årige Skoleelever i Danmark. [Health Behavior in School-Aged Children - a WHO Collaborative Cross-National Survey 2018: Health, Well-Being and Health Behaviors Among 11, 13, and 15-Year-Old School Children in Denmark]. Copenhagen: National Institute of Public Health (2018).
20. Geidne S, Beckman L, Edvardsson I, Hulldin J. Prevalence and risk factors of electronic cigarette use among adolescents: data from four Swedish municipalities. Nord Stud Alcohol Drugs. (2016) 33:225–40. doi: 10.1515/nsad-2016-0017
21. Jawad M, Charide R, Waziry R, Darzi A, Ballout RA, Akl EA. The prevalence and trends of waterpipe tobacco smoking: a systematic review. PloS ONE. (2018) 13:e0192191. doi: 10.1371/journal.pone.0192191
22. Lundberg CS, Kvaavik E, Tokle R. Nye bruksmønstre i et tobakksmarked i endring–kombinert bruk av sigaretter, snus og e-sigaretter blant ungdom [New patterns of use in a changing tobacco market–combined use of cigarettes, snus, and e-cigarettes among youth]. Nord Stud Alcohol Drugs. (2019) 36:6–20. doi: 10.1177/1455072518797823
23. Zhu S-H, Gamst A, Lee M, Cummins S, Yin L, Zoref L. The use and perception of electronic cigarettes and snus among the US population. PloS ONE. (2013) 8:e79332. doi: 10.1371/journal.pone.0079332
24. Ruokolainen O, Ollila H, Lahti J, Rahkonen O. Intergenerational social mobility, smoking and smokeless tobacco (snus) use among adolescents during 2008–2017. Addict Behav. (2019) 98:106022. doi: 10.1016/j.addbeh.2019.06.011
25. Kinnunen JM, Rimpelä AH, Lindfors PL, Clancy L, Alves J, Hoffmann L, et al. Electronic cigarette use among 14-to 17-year-olds in Europe. Eur J Public Health. (2021) 31:402–8. doi: 10.1093/eurpub/ckaa145
26. Friedman AS, Horn SJ. Socioeconomic disparities in electronic cigarette use and transitions from smoking. Nicotine Tob Res. (2019) 21:1363–70. doi: 10.1093/ntr/nty120
27. Hanewinkel R, Isensee B. Risk factors for e-cigarette, conventional cigarette, and dual use in German adolescents: a cohort study. Prev Med. (2015) 74:59–62. doi: 10.1016/j.ypmed.2015.03.006
28. Øverland S, Tjora T, Hetland J, Aarø LE. Associations between adolescent socioeducational status and use of snus and smoking. Tob Control. (2010) 19:291–6. doi: 10.1136/tc.2009.034512
29. Glantz SA, Bareham DW. E-cigarettes: use, effects on smoking, risks, and policy implications. Annu Rev Public Health. (2018) 39:215–35. doi: 10.1146/annurev-publhealth-040617-013757
30. Byhamre ML, Araghi M, Alfredsson L, Bellocco R, Engström G, Eriksson M, et al. Magnusson C. Swedish snus use is associated with mortality: a pooled analysis of eight prospective studies. Int J Epidemiol. (2020) 49:2041–50. doi: 10.1093/ije/dyaa197
31. Chapman S, Bareham D, Maziak W. The gateway effect of e-cigarettes: reflections on main criticisms. Nicotine Tob Res. (2019) 21:695–8. doi: 10.1093/ntr/nty067
32. Grøtvedt L, Forsén L, Ariansen I, Graff-Iversen S, Holmen TL. Impact of snus use in teenage boys on tobacco use in young adulthood; a cohort from the HUNT Study Norway. BMC Public Health. (2019) 19:1–10. doi: 10.1186/s12889-019-7584-5
33. Owotomo O, Stritzel H, McCabe SE, Boyd CJ, Maslowsky J. Smoking intention and progression from e-cigarette use to cigarette smoking. Pediatrics. (2020) 146:e2020002881. doi: 10.1542/peds.2020-002881
34. Vanyukov MM, Tarter RE, Kirillova GP, Kirisci L, Reynolds MD, Kreek MJ, et al. Ridenour TA. Common liability to addiction and “gateway hypothesis”: theoretical, empirical and evolutionary perspective. Drug Alcohol Depend. (2012) 123:3–17. doi: 10.1016/j.drugalcdep.2011.12.018
35. Thomas RE, McLellan J, Perera R. School-based programmes for preventing smoking. Evid Based Child Health. (2013) 8:1616–2040. doi: 10.1002/ebch.1937
36. Andersen A, Bast LS, Ringgaard LW, Wohllebe L, Jensen PD, Svendsen M, et al. Design of a school-based randomized trial to reduce smoking among 13 to 15-year olds, the X: IT study. BMC Public Health. (2014) 14:518. doi: 10.1186/1471-2458-14-518
37. Andersen A, Krølner R, Bast LS, Thygesen LC, Due P. Effects of the X: IT smoking intervention: a school-based cluster randomized trial. Int J Epidemiol. (2015) 44:1900–8. doi: 10.1093/ije/dyv145
38. Nagelhout GE, Popova L, Kuipers MA. Why are new tobacco control interventions needed? Int J Environ Res Public Health. (2018) 15:658. doi: 10.3390/ijerph15040658
39. Mercken L, Moore L, Crone M, De Vries H, De Bourdeaudhuij I, Lien N, et al. The effectiveness of school-based smoking prevention interventions among low-and high-SES European teenagers. Health Educ Res. (2012) 27:459–69. doi: 10.1093/her/cys017
40. Tinner L, Caldwell D, Hickman M, MacArthur GJ, Gottfredson D, Perez AL, et al. Examining subgroup effects by socioeconomic status of public health interventions targeting multiple risk behaviour in adolescence. BMC Public Health. (2018) 18:1180. doi: 10.1186/s12889-018-6042-0
41. Christiansen TB, Nissen M. Procesevaluering af Projekt X:IT: Projektets Implementering på Skolerne [Process Evaluation of the X:IT Project: the Implementation of the Project on Schools]. The Danish Cancer Society (2012).
42. Jøsendal O, Aarø LE, Torsheim T, Rasbash J. Evaluation of the school-based smoking-prevention program “BE smokeFREE”. Scand J Psychol. (2005) 46:189–99. doi: 10.1111/j.1467-9450.2005.00448.x
43. Nilsson M, Stenlund H, Bergström E, Weinehall L, Janlert U. It takes two: reducing adolescent smoking uptake through sustainable adolescent–adult partnership. J Adolesc Health. (2006) 39:880–6. doi: 10.1016/j.jadohealth.2006.07.004
44. Bast LS, Due P, Lauemøller SG, Kjær NT, Christiansen T, Andersen A. Study protocol of the X: IT II-a school-based smoking preventive intervention. BMC Public Health. (2019) 19:497. doi: 10.1186/s12889-019-6805-2
45. The Danish Ministry of Health. Initiativer på Tobaksområdet og Prisudvikling Siden år 2000 [Initiatives on the Tobacco Area and Price Development Since 2000]. The Danish Ministry of Health (2020).
46. Christensen U, Krølner R, Nilsson CJ, Lyngbye PW, Hougaard CØ, Nygaard E, et al. Addressing social inequality in aging by the Danish occupational social class measurement. J Aging Health. (2014) 26:106–27. doi: 10.1177/0898264314522894
47. Lien N, Friestad C, Klepp KI. Adolescents' proxy reports of parents' socioeconomic status: how valid are they? J Epidemiol Community Health. (2001) 55:731–7. doi: 10.1136/jech.55.10.731
48. White HR, Pandina RJ, Chen P-H. Developmental trajectories of cigarette use from early adolescence into young adulthood. Drug Alcohol Depend. (2002) 65:167–78. doi: 10.1016/S0376-8716(01)00159-4
49. Fredriksson A, Oliveira GMD. Impact evaluation using Difference-in-Differences. RAUSP Manag J. (2019) 54:519–32. doi: 10.1108/RAUSP-05-2019-0112
50. Graham JW. Multiple imputation and analysis with multilevel (cluster) data. In: Missing Data. New York: Springer (2012). p. 133–50.
51. Donner A, Klar N. Statistical considerations in the design and analysis of community intervention trials. J Clin Epidemiol. (1996) 49:435–9. doi: 10.1016/0895-4356(95)00511-0
52. Bast LS, Lund L, Lauemøller SG, Kjeld SG, Due P, Andersen A. Socio-economic differences in smoking among adolescents in a school-based smoking intervention: the X: IT II study. Scand J Public Health. (2021) 49:961–9. doi: 10.1177/14034948211007683
53. McLaren L, McIntyre L, Kirkpatrick S. Rose's population strategy of prevention need not increase social inequalities in health. Int J Epidemiol. (2010) 39:372–7. doi: 10.1093/ije/dyp315
54. Hublet A, De Bacquer D, Valimaa R, Godeau E, Schmid H, Rahav G, et al. Smoking trends among adolescents from 1990 to 2002 in ten European countries and Canada. BMC Public Health. (2006) 6:1–7. doi: 10.1186/1471-2458-6-280
55. Kjeld SG, Andersen S, Andersen A, Glenstrup S, Lund L, Danielsen D, et al. Who are the young users of tobacco products? Prevalence and characteristics of Danish adolescents who have either smoked cigarettes, used alternative tobacco products, or used both. Nord Stud Alcohol Drugs. (2021) 38:555–72. doi: 10.1177/14550725211027687
56. Kjeld SG, Glenstrup S, Bast LS. Gender and socioeconomic disparities in reasons for not smoking cigarettes among Danish adolescents. BMC Res Notes. (2021) 14:1–5. doi: 10.1186/s13104-021-05454-6
57. Rozema A, Mathijssen J, Jansen M, Van Oers J. Schools as smoke-free zones? Barriers and facilitators to the adoption of outdoor school ground smoking bans at secondary schools. Tob Induc Dis. (2016) 14:1–9. doi: 10.1186/s12971-016-0076-9
58. Hedman L, Andersson M, Stridsman C, Rönmark E. Evaluation of a tobacco prevention programme among teenagers in Sweden. BMJ Open. (2015) 5:e007673. doi: 10.1136/bmjopen-2015-007673
59. Kjeld SG, Lauemøller SG, Lund L, Andersen A, Bast LS. School characteristics and participation in a smoking prevention intervention. Health Behav Policy Rev. (2020) 7:170–8. doi: 10.14485/HBPR.7.3.1
60. Bast LS, Andersen A, Ersbøll AK, Due P. Implementation fidelity and adolescent smoking: the X: IT study—a school randomized smoking prevention trial. Eval Prog Plann. (2019) 72:24–32. doi: 10.1016/j.evalprogplan.2018.09.004
Keywords: smoking, tobacco, snus, e-cigarette, waterpipe, alternative tobacco products, school-based intervention, prevention
Citation: Kjeld SG, Lund L, Andersen S and Bast LS (2022) Socioeconomic Differences in Cigarette Smoking and Alternative Tobacco Product Use Among Adolescents in a School-Based Smoking Preventive Intervention: Findings From the Second Year of the X:IT II Study. Front. Public Health 10:825585. doi: 10.3389/fpubh.2022.825585
Received: 30 November 2021; Accepted: 14 January 2022;
Published: 21 February 2022.
Edited by:
Christiane Stock, Charité Medical University of Berlin, GermanyReviewed by:
Birute Strukcinskiene, Klaipėda University, LithuaniaCopyright © 2022 Kjeld, Lund, Andersen and Bast. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Simone Gad Kjeld, simk@sdu.dk
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.