
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 25 January 2022
Sec. Digital Public Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.823692
This article is part of the Research Topic mHealth Tools for Patient Empowerment and Chronic Disease Management View all 20 articles
With the development of telemedicine and e-health, usage of online health communities has grown, with such communities now representing convenient sources of information for patients who have geographical and temporal constraints regarding visiting physical health-care institutions. Many previous studies have examined patient–provider communication and health-care service delivery in online health communities; however, there is a dearth of research exploring the relationship between patients' level of self-disclosure and the establishment of patients' trust in physicians. Consequently, this study aims to explore how patients' self-disclosure affects the establishment of patients' trust in physicians. “Good Doctor,” which is a China-based online health community, was used as a data source, and a computer program was developed to download data for patient–physician communication on this community. Then, data for communications between 1,537 physicians and 63,141 patients were obtained. Ultimately, an empirical model was built to test our hypotheses. The results showed that patients' self-disclosure positively influences their establishment of trust in physicians. Further, physicians' provision of social support to patients showed a complete mediating effect on the relationship between patients' self-disclosure and patients' establishment of trust in physicians. Finally, evidence of “hope-for-help” motivation in patients' messages weakened the effect of patients' self-disclosure when physicians' social support was text-based, but strengthened it when physicians' social support was voice-based.
With the continuing development of health information technology (1) and telemedicine, online health communities (OHCs), such as Good Doctor (haodf.com) and Chunyu Doctor (chunyuyisheng.com), are becoming increasingly popular online platforms through which patients and physicians can communicate and exchange information (2–6). OHCs provide patients with an online health consultation service, which allows them to communicate with physicians in order to obtain medical information and services; meanwhile, OHCs can provide physicians with economic and social returns (e.g., such as reputation, if the physicians service the patients on OHCs, the physicians can obtain external reputation which is distinct from offline service, such as the electronic votes, gifts, thanks letters from patients) (7). OHCs are extremely convenient for patients who have geographical and temporal constraints regarding physically contacting health-care professionals (8). Overall, the widespread use of OHC facilitates physician–patient communication and improves the accessibility of health-care services.
When compared with offline, face-to-face communication, OHCs represent extremely convenient resources through which patients can investigate diseases and symptoms. However, as OHCs are internet-based, all contact is virtual; thus, OHCs do not afford tangible diagnoses, such as inspections involving physical appraisals (e.g., palpation) or examinations of symptoms that can only be heard or smelled. Therefore, on OHCs, patients' level of self-disclosure is essential for helping the physicians make appropriate medical decisions. However, dialogue on OHCs occurs through computer-mediated communication (CMC), and combining CMC with non-tangible (i.e., non-face-to-face) diagnoses may lead to patients having less trust in physicians when compared to face-to-face communication and offline diagnoses. Thereby, on OHCs, how to improve the patient-physician trust based on the patients' self-disclosure is important to the patients and the physicians.
Self-disclosure refers to information one person communicates to another and, in the social-psychology context, is considered a kind of social behaviour (9). Previous studies have found that, when compared with face-to-face communication, users of CMC tend to disclose more personal information, mainly as a result of the anonymity such services afford (10–12). Thus, along with being distinct from face-to-face communication and representing a novel and unique method of performing self-disclosure, CMC can, in certain contexts, increase the degree self-disclosure, which could contribute to building trust (13). Therefore, it is essential to explore the relationship between self-disclosure and trust in patient–physician CMC in the OHC context. As to patient–physician trust, Gabay (14) found that perceived participative communication (PPC) can improve patient-physician trust, and the patients' perceived control over health positively moderates the relationship between PPC and patient-provider trust. Meanwhile, the physicians' good listening abilities and impartial concern for patients' well being are important factors that can increase the patients' trust in physician (15). Furthermore, Gabay (16) also discussed the communication barriers to trust (e.g., underrating patient's autonomy and lack of attentive listening) and proposed a way of patient-centred communication to improve patient's self-worth and trust. These studies provide well enlightenment for us to understand patient-physician trust. In real life, when a patient consults a physician through an OHC, the patient's trust in the physician develops gradually during the subsequent slow communication process (17). Notably, a previous study has shown that longer information exchange through CMC is more likely to foster trust (18). Therefore, after multiple rounds of CMC-mediated interaction, the physician and patient should develop an understanding of each other and a trusting relationship. From the patient perspective, trust in the physician is influenced by how much information they disclose to the physician (19, 20). Therefore, high patient self-disclosure is important for the establishment of physician–patient trust. Moreover, social support, which refers to interpersonal relations and, in this context, usually concerns emotional and informational support, is another important element in the OHC context, and can affect cooperation and relationships between physicians and patients. Receiving social support from physicians not only benefits patients' mental health (21), but can also, the field of e-health, play a significant role in patients' self-disclosure and trust (22).
Multiple studies across several fields have directly explored self-disclosure, social support, and trust (23–25); however, there is a dearth of research exploring the mechanisms that influence self-disclosure, social support, and trust. Moreover, little research has explored the mediating role of social support from physicians in the relationship between patients' self-disclosure and their building of trust in physicians. In the present research, we explore the effect of patients' self-disclosure on their trust in physicians, as well as the mediating role of social support from physicians in this relationship. Additionally, showing hope of receiving help when asking questions of physicians can not only indicate to physicians the type of information the patients desire, but may also help patients have good CMC experiences (26). For example, questions such as Do I need an operation? and How should I take the medicine?, which indicate a hope for help, may help physicians accurately and quickly understand the patients' requests, and also help the physicians provide better social support to the patients. However, existing research on the role of patients' “hope-for-help” motivation in patient–provider communication is sparse. Therefore, this study also investigates the moderating role of patients' hope-for-help motivation on the relationship between patients' self-disclosure and physicians' social support in patient–provider communication.
To explore how to build, and the factors that affect, patients' trust in physicians during online patient–provider communication, this research explores the following three questions:
RQ1: How does patients' self-disclosure affect the establishment of patients' trust in physicians?
RQ2: What is the role of social support from physicians in the relationship between patients' self-disclosure and the establishment of patients' trust in physicians?
RQ3: What is the role of patients' hope-for-help motivation in the relationship between patients' self-disclosure and physicians' provision of social support?
To answer the above questions, this study constructed a moderated mediation model to verify the relationship between patients' self-disclosure and the establishment of patients' trust in physicians. To the best of our knowledge, this is the first study to explore patients' self-disclosure and trust during CMC on OHCs. The research findings may provide some insights into physician–patient trust and patient–provider communication in telemedicine and e-health.
CMC originated from the “computer supported cooperation” in the 1980s. With the progress of electronic communication technology and the increase of the human being's cooperation, to communicate conveniently, more and more people begin to use the emerging communication tools to communicate and carry out cooperation based on computers. Later, this communication is called computer-mediated communication, which is abbreviated as CMC. At present, CMC is widely regarded as a new communication mode for people to search, transmit, process and communicate with each other under the help of the Internet. There are three basic communication elements in CMC: the disseminator, the media, the receiver of information. Consequently, CMC is essentially a way of information transmission to some extent. Now, CMC has been applied to many fields, such as electronic commerce, online healthcare, distance learning, online communication, and online cooperation. In online healthcare, with the development of telemedicine and e-health, CMC through OHCs has become an important medium of patient–provider communication. CMC can negate geographical and temporal constraints, representing a convenient method by which physicians and patients can communicate.
Previous studies have explored physician–patient CMC from multiple perspectives, such as interaction frequency (3), interactional unfairness (27), communication competences (28), and interaction engagement (29). However, few studies have investigated the relationship between patients' self-disclosure and the establishment of patients' trust in physicians in the context of OHCs. Further, little research has sought to answer the following questions: what role does social support from physicians play in the relationship between patients' self-disclosure and the establishment of patients' trust in physicians? Does it act as a mediating variable affecting the relationship between physicians and patients? Additionally, few studies have explored the moderating effect of patients' hope-for-help motivation on the relationship between patients' self-disclosure and physicians' provision of social support.
Self-disclosure is defined as the communication and presentation of personal information to another person (30–32), and plays an important role in the establishment of trust in others. Specifically, when individuals disclose personal information to one another, they improve understanding of each other and create trust (33). Social penetration theory (34) suggests that self-disclosure is a basic form of social exchange; as relationships develop, this exchange deepens and becomes more extensive. Meanwhile, Knapp's staircase model of relationships (35) also emphasised that self-disclosure can promote the intimacy of relationships and the formation of trust. The relationship between self-disclosure and trust is applicable to the physician–patient relationship. When a patient consults a physician, more self-disclosure on the part of the patient can promote interaction with the physician (36) and significantly improve the patient's experience, which leads to higher patient satisfaction (37). Additionally, when patients disclose more information to physicians, the physician–patient dialogue and contact increase, and the patients become more willing to trust the physicians (19, 20) and consult further with the physicians regarding their disease. Based on these findings, hypothesis H1 was proposed for the present study:
H1: Patients' self-disclosure positively influences the establishment of patients' trust in physicians.
Generally speaking, social support can be divided into information support (38) and emotional support (39, 40). Information support involves providing actionable and objective information to a recipient. Meanwhile, emotional support, as a form of social support, involves empathising and providing emotional validation and encouragement (41). Regarding the relationship between self-disclosure and social support, Lee et al. (42) showed that individuals who disclose more information are more likely to receive social support. Meanwhile, Kim and Lee (43) suggested that honest self-disclosure positively affects the likelihood of receiving social support. Similarly, in the context of e-health, studies have found that the greater patients' self-disclosure through CMC, the more likely they are to receive physician feedback and social support (44). When patients communicate with physicians, disclosing more information indicates that they want the physicians to understand more about their symptoms and feelings. Furthermore, through high self-disclosure patients can obtain more information support (e.g., in regard to medication instructions and treatment plans) and emotional support (caring comments and tips) from physicians. Physicians can employ textual media to provide text-based social support to patients. However, they can also use richer media; for example, using voice media to provide voice-based social support to patients. Compared with text-based social support, voice-based social support can, through its greater richness, transmit more information (45, 46). Based on the above findings, we formulated hypotheses H2 and H3:
H2: Patients' self-disclosure positively influences physicians' text-based social support.
H3: Patients' self-disclosure positively influences physicians' voice-based social support.
More social support can increase patients' satisfaction with physicians' services (8), which can make them more willing to carry out further consultations with the physicians regarding their disease. Furthermore, higher level of social support also can often give rise to satisfactory social interaction and increase good psychological perception in physicians (47). Meanwhile, satisfactory social interaction can make patients perceive physicians as holding good intent towards themselves, and impel patients to consider that the information provided by physicians is more trustworthy (48). Besides, the social support can also increase people's health and well-being based on the social relationships, and it can transmit information, emotion, esteem among individuals (49). This can help patients improve the trust and reap more positive health outcomes (50, 51). Based on the above analysis, it can be seen that, not only does patients' self-disclosure have a direct effect on the establishment of trust in physicians, but it also has an indirect effect, through social support. Therefore, hypotheses H4 and H5 were formulated:
H4: Text-based social support from physicians mediates the relationship between patients' self-disclosure and the establishment of patients' trust in physicians.
H5: Voice-based social support from physicians mediates the relationship between patients' self-disclosure and the establishment of patients' trust in physicians.
Motivation represents an individual's psychological needs. Previous studies have shown that individuals' psychological needs have an important influence on the reception of social support during online disclosure (42, 52). Li et al. (53) suggested that individual psychological needs can impact the relationship between self-disclosure and social support. In other words, people with strong needs are more likely to disclose more information in order to receive more social support (53). On OHCs, when patients show hope-for-help motivation, this indicates that they are seeking social support. When patients express such motivation (e.g., through questions such as Is my illness serious? Do I need surgery? How is it treated?), physicians will find it easier to understand the patients' information demands. In such occasions, physicians will send more information to patients (26). According to the media-richness theory (45, 46), rich media can transmit more information than lean media, and rich media can also deliver multiple additional cues, such as voice tones, intonation, and emotions. During the online consultation process, if the patients present greater hope-for-help motivation, physicians will find it easier to understand the patients' information requests, and will consequently provide more social support. To enhance the effectiveness of their communication, physicians, upon noting hope-for-help motivation, may be more likely to use richer media (e.g., voice) to provide social support than leaner media (e.g., text). Besides, the rich media have faster and real-time feedback ability compared with the lean media. When the patients present hope-for-help motivation, sometimes there are urgent information in the motivation provided by the patients (e.g., through questions such as Can I go to your hospital? What else needs to be checked? Do I need an operation as soon as possible? I am very anxious and fear for delaying my illness. I hope you can give me a suggestion). At this time, to feed back information quickly, the physicians may choose a rich media (e.g., voice) to provide social support, other than a lean media (e.g., text). Therefore, hypotheses H6a and H6b were formulated.
H6a: Patient motivation weakens the effect of patients' self-disclosure on physicians' provision of text-based social support.
H6b: Patient motivation strengthens the effect of patients' self-disclosure on physicians' provision of voice-based social support.
The research model for the present study is shown in Figure 1.
With the development of telemedicine and e-health, OHCs have become popular online medical consultation platforms. Good Doctor (haodf.com) is a China-based OHC that allows people to seek medical services for a fee. Good Doctor, which was created in 2006, is currently the largest e-health platform; at present, it features over 300 departments, covering over 3,000 diseases. The present research data are sourced from Good Doctor. We chose Good Doctor as the data source for two reasons. First, Good Doctor contains a great deal of data on many diseases, such as chronic diseases, serious diseases, and diseases that patients can be reluctant to disclose in public (high-privacy diseases). Second, Good Doctor contains data regarding physicians' attributes and patient–provider communication; such data greatly facilitated our research.
We collected from Good Doctor patient–provider communication data and data on physicians' attributes for November 2020. We used crawler software to download the data from the Good Doctor website. Thirty diseases were represented in our data, 10 high-privacy diseases and 20 common diseases. After downloading the data, we processed the data through the following steps: (1) deleted data that could not be recognised by a computer, (2) removed “space” characters, and (3) deleted data unrelated to our research (e.g., physicians' notes, tips). After applying these steps, the final dataset featured communication data from 1,537 physicians and 63,141 patients. The patient data contained 196,291 textual items, while the physician data contained 167,702 textual items and 41,538 voice items. The physicians' attribute data contained included physicians' clinical titles, educational titles, number of patients served, and total number of consultations. Thus, our final dataset featured physicians' attribute data and communication data. An example of doctor–patient communication on Good Doctor is shown in Figure 2.
The dependent variable was the establishment of patients' trust in the physicians. In e-business, sales of a product/service is an intuitive expression of consumers' trust in a business (54); similarly, in e-health, If the patients trust the physicians, the patients are likely to choose the physicians to consult the disease (20, 55, 56). For example, Gong (55) found that physicians' good service quality and reputation can enable patients to establish a trust relationship with them, and select these physicians in OHCs. Yoo et al. (56) considered that the trust propensity, platform reputation, and perceived physician credibility are important factors that can trigger patients' trust in physicians, and urge these patients to choose the physicians.Therefore, to some extent, the increment of patients who served by physicians can directly reflect the trust of patients to physicians. In our research, we used the increment of patients in the next month as a proxy variable to indicate the establishment of patients' trust in physicians. In this research, for each physician the increment in patients was obtained by subtracting the physician's number of patients in November 2020 from the number of patients in December 2020.
The independent variable was patients' self-disclosure; specifically, if the patients are willing to disclose more information, they will use more words to state their conditions. Contrarily, if they don't want to disclose information, they will employ less words or speak nothing to express their opinions and attitudes (57, 58). Therefore, the amount of disclosure is significantly correlated with the disclosure degree (58, 59). To effectively represent the amount and degree of patient disclosure, for each patient we used the average length (in characters) of their textual messages (PTL) to indicate the patient's level of self-disclosure. Physicians' social support was regarded as a mediating variable. Similarly, we used the average length (in characters) of the textual information (TL) and the duration (in seconds) of the voice information (VL) to quantify text-based and voice-based social support (57), respectively. Meanwhile, this study regards patients' hope-for-help motivation as a moderator variable, and this was quantified using the average length (in characters) of patients' hope for help messages. In addition, the number of textual messages patients send to physicians (PTN) may influence physician's provision of social support; concurrently, physicians who have a high clinical title (ClinicT), good reputation, and rich experience in medical diagnosis and treatment may provide more support to patients. Therefore, we controlled the influence of PTN, physicians' ClinicT, the time physicians spent online (OnlineT), the number of people who visited physicians' pages (VisitNum), the number of votes physicians received from patients (Votes, it is a kind of reputation which is the same as the gifts and thanks letter), and the price of consultation. The specific variable definitions are shown in Table 1.
The calculation formulas for TL, VL, PTL, and PTN described in Table 1 are presented below in formulae 1–4, respectively.
In the above formulae, TL represents the average length (in characters) of the textual information physicians sent to patients, and VL represents the average length (in seconds) of the voice information physicians sent to patients. PTL represents the average length (in characters) of the textual information patients sent to physicians, and PTN represents the average number of textual messages patients sent to physicians. m indicates the number of patients the physician served during November 2020, n1and n2represent the number of text dialogues and voice dialogues, respectively, a physician had with a patient. n3 represents the number of text dialogues each patient had with each physician.
To test the above hypotheses, we applied a moderated mediation model approach, creating four models. To reduce the fluctuation of the data, we created a natural logarithm transformation for all variables; for convenience, the original variable name was used to express the processed variables. We used Model 1 to test the effect of patients' self-disclosure on the establishment of patients' trust in physicians.
Model 1
Model 2 tests the effect of patients' self-disclosure on text-based and voice-based social support from physicians.
Model 2
Model 3 tests the mediating effect of physicians' provision of social support on the relationship between patients' self-disclosure and the establishment of patients' trust in physicians.
Model 3
Model 4 tests the moderating effect of patient motivation on the relationship between patients' self-disclosure and social support from physicians.
Model 4
In the above models, the specific meaning of parameters is shown in Table 2.
The descriptive statistics of the variables are shown in Table 3, and the variable correlations are shown in Table 4. The mean variance inflation factor (VIF) was 2.71, and in all models the VIFs were <5. Therefore, there were no multicollinearity problems in our study. In this study, we use a moderation-mediation model to verify above hypotheses in our research. The moderation-mediation model can be divided into two parts: mediation model and moderation model. The mediation model contains model 1, model 2 and model 3. First of all, model 1 verifies the main effect between independent variable (PTL) and dependent variable (PT). If the coefficient β1 is significant, the main effect is effective. Secondly, the coefficient β2 and β3 must be significant in model 2. Finally, in model 3, the coefficient (γ4, δ4) of mediating variable (TL,VL) must be significant and the coefficient (β4) of independent variable (PTL) must be not significant. When above conditions are met, the mediating effect is effective. The model 4 is a moderation model and it can verify the moderation effect. In model 4, if the coefficient (β5, γ5, θ5 or β6, γ6, θ6) of independent variable (PTL), moderator variable (HFH) and the interactive item ( HFH*PTL) is significant, the moderating effect is effective. Table 5 presents the estimation results. Column (1) shows the estimation result for the control variables only. H1 predicted that patients' self-disclosure positively influences the establishment of patients' trust in physicians. Based on the regression result shown in column (2), β1 (β1 = 0.132, t= 3.19, ρ < 0.01) was positive and significant; thus, H1 was supported, and the main effect was verified.
H2 and H3 predicted that patients' self-disclosure positively influences physicians' provision of text-based and voice-based, respectively, social support. Columns (3,4) indicate that β2 (β2 = 0.439, t= 8.52, ρ < 0.01) and β3 (β3 = 0.347, t= 7.58, ρ < 0.01) are positive and significant; thus, H2 and H3 are supported. This indicates that, during the process of patient–provider communication, an increasing amount of information is disclosed by patients, and physicians consequently obtain better understanding of patients' medical conditions and provide more effective treatment and social support to patients.
Column (5) tests the mediating effect of physicians' text-based and voice-based social support. In column (5), β4 (β4 = 0.050, t=1.11, ρ>0.1) is not significant, whereas γ4 (γ4 = 0.095, t= 3.21, ρ < 0.01) and δ4 (δ4 = 0.092, t= 5.07, ρ < 0.01) are positive and significant; this indicates that H4 and H5 were supported. These findings suggest that, in OHCs, if patients obtain more information and support from physicians, they can develop a more favourable perception of their medical experience and become more willing to build a trust relationship with the physicians. Thus, social support from physicians plays a complete mediating role in the relationship between patients' self-disclosure and the establishment of patients' trust in physicians.
Columns (6,7) test the moderating effect of patients' hope-for-help motivation on the relationship between patients' self-disclosure and physicians' social support. In columns (6,7), θ5 (θ5 = −0.080, t = −3.27, ρ < 0.01) is negative and significant, whereas θ6 (θ6 = 0.052, t = 2.65, ρ <0.01) is positive and significant; thus, H6a and H6b are supported. The specific moderating effect of hope-for-help motivation is shown in Figures 3, 4. This shows that patients' hope-for-help motivation weakens the effect of patients' self-disclosure on physicians' provision of text-based support, and strengthens the effect of patients' self-disclosure on physicians' provision of voice-based support.
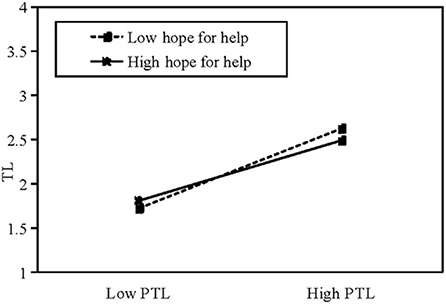
Figure 3. The mediating effect of hope-for-help motivation on TL. PTL: length of patient's textual messages.
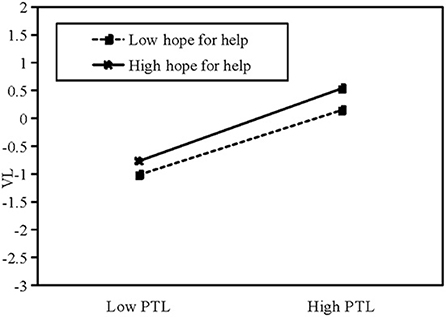
Figure 4. The mediating effect of hope-for-help motivation on VL. PTL: length of patient's textual messages.
To test the robustness of our results, we used data from December 2020 (communication data) and January 2021 (number of patients who consulted each physician) to verify our results. Table 6 shows that most of our results are robust and credible.
Based on the Good Doctor medical platform, which is a big online health community in China, this study used a moderation-mediation model to explore the relationship among patients' self-disclosure, physicians' social support and the patients' establishment of trust in physicians. Additionally, it also tested the moderating effect of patients' motivation for “hope for help” on the physicians' social support. The results show that the patients' self-disclosure positively affect the patients' establishment of trust in physicians. The physicians' social support plays a complete mediating effect between the patients' self-disclosure positively and the patients' establishment of trust in physicians. Moreover, the patients' motivation for “hope for help” weakens the effect of patients' self-disclosure on physicians' provision of text-based social support and strengthens the effect of patients' self-disclosure on physicians' provision of voice-based social support. This research has some theoretical and practical contributions. First of all, this study is helpful to understand the patient-physician communication and patient-physician trust. It first establishes the contact between the patients' self-disclosure and the patients' establishment of trust in physicians from the patients. Secondly, this study extends the healthcare theory in OHCs and make the service and trust mechanism clear during the process of CMC. Thirdly, it provides the beneficial and essential practical implications for patients, physicians and the online health platforms. Overall, our research investigated the relationship between patients' self-disclosure, the physicians' social support and the establishment of patients' trust in physicians. It expands the health-care service delivery theory in e-health and has strong practical significance for patients, physicians, online medical platform, and the digital public health of human beings.
This study provides insights for practise. First, our research provides a new approach for investigating the deep influencing mechanisms for the relationship between patients' self-disclosure and the establishment of patients' trust in physicians. Our research reveals a credible path by which patients can build trust in physicians during CMC. We found that patients' self-disclosure is helpful for building a harmonious and credible trust relationship between physicians and patients. Thus, when patients consult physicians, they should disclose as much information as possible.
Second, social support from physicians is significant for patients. Trust between physicians and patients is an essential element of physician–patient communication. If patients disclose more information to physicians, the physicians will provide more social support to the patients, and the patients will consequently become more willing to trust the physicians. The physicians should pay attention to the patients' self-disclosure, if there are more self-disclosure from patients, it means that the patients want to explain their symptoms and conditions clearly, the physicians should feed back the information as more as possible through text and voice media. At this time, the patients will consider that the physicians' service is worthy and they will trust physicians more. Meanwhile, if patients seek to obtain more social support from physicians, the patients could show more “hope-for-help” motivation to the physicians. Moreover, as a result of its richness as a medium, physicians should use voice media as much as possible when communicating with patients, as such media is helpful for providing increased social support and building a strong physician–patient relationship.
Third, CMC platforms could provide some modular options that help patients indicate their information needs. Such options could relate to medication, operations, diseases, and appointments. With such functionality, patients could disclose information more accurately and conveniently, and physicians could more easily understand patients' desires and, consequently, provide more social support.
There are some limitations to our study. First, the data in our research are sourced only from the Good Doctor website, which is a large online e-health community in China; future studies should use data from multiple online platforms to verify our hypotheses. Second, our research data are cross-sectional; future research should use panel data to obtain more robust results. Third, this paper focussed solely on information quantities to determine patients' levels of self-disclosure and physicians' levels of social support; future research should more closely consider the influence of communication content.
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
All authors made substantial contributions to the research and agree with the content of the final manuscript.
This work was supported by the National Natural Science Foundation Project (Grant No. 71871144), the Science and Technology Development Program of University of Shanghai for Science and Technology (Grant No. 2020KJFZ046), the Major Program of the National Fund of Philosophy and Social Science of China (Grant No. 18ZDA088), the Shanghai University of Finance and Economics Graduate Innovation Fund (Grant No. CXJJ-2019-400), and the Fund of Shanghai University of Sport (Grant No. A1-0303-21-0001-5).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ClinicT, Clinical title; CMC, Computer-mediated communication; HFH, Hope for help messages; OHC, Online health community; OnlineT, Time online; PT, Patients’ trust in physicians, ; PTL, Length of patient's textual messages; PTN, Patient's number of textual messages; TL, Text-message length; VisitNum, Number of people who have visited a physician's page; VL, Voice-message length.
1. Abbott PA, Foster J, de Marin Hde F, Dykes PC. Complexity and the science of implementation in health IT—Knowledge gaps and future visions. Int J Med Inform. (2014) 83:e12–22. doi: 10.1016/j.ijmedinf.2013.10.009
2. Liu F, Li Y, Ju X. Exploring patients' consultation behaviors in the online Health Community: The role of disease risk. Telemed J E Health. (2019) 25:213–20. doi: 10.1089/tmj.2018.0033
3. Yang H, Guo X, Wu T. Exploring the influence of the online physician service delivery process on patient satisfaction. Decis Support Syst. (2015) 78:113–21. doi: 10.1016/j.dss.2015.05.006
4. Jiang J, Yang M, Kiang M, Cameron A. Exploring the freemium business model for online medical consultation services in China. Inf Process Manag. (2021) 58:102515. doi: 10.1016/j.ipm.2021.102515
5. Wu H, Lu N. Online written consultation, telephone consultation and offline appointment: an examination of the channel effect in online health communities. Int J Med Inform. (2017) 107:107–19. doi: 10.1016/j.ijmedinf.2017.08.009
6. Wang P, Zhou L, Mu D, Zhang D, Shao Q. What makes clinical documents helpful and engaging? An empirical investigation of experience sharing in an online medical community. Int J Med Inform. (2020) 143:104273. doi: 10.1016/j.ijmedinf.2020.104273
7. Guo S, Guo X, Fang Y, Vogel D. How doctors gain social and economic returns in online health-care communities: a professional capital perspective. J Manag Inf Syst. (2017) 34:487–519. doi: 10.1080/07421222.2017.1334480
8. Chen S, Guo X, Wu T, Ju X. Exploring the online doctor–patient interaction on patient satisfaction based on text mining and empirical analysis. Inf Process Manag. (2020) 57:102253. doi: 10.1016/j.ipm.2020.102253
9. Trepte S, Reinecke L. The reciprocal effects of social network site use and the disposition for self-disclosure: a longitudinal study. Comput Hum Behav. (2013) 29:1102–12. doi: 10.1016/j.chb.2012.10.002
10. Joinson AN. Self-disclosure in computer-mediated communication: the role of self-awareness and visual anonymity. Eur J Soc Psychol. (2001) 31:177–92. doi: 10.1002/ejsp.36
11. Tidwell LC, Walther JB. Computer-mediated communication effects on disclosure, impressions, and interpersonal evaluations: getting to know one another a bit at a time. Hum Commun Res. (2002) 28:317–48. doi: 10.1111/j.1468-2958.2002.tb00811.x
12. Jiang LC, Bazarova NN, Hancock JT. The disclosure–intimacy link in computer-mediated communication: an attributional extension of the hyperpersonal model. Hum Commun Res. (2011) 37:58–77. doi: 10.1111/j.1468-2958.2010.01393.x
13. Miller MK, Mandryk RL. Meeting with Media: Comparing Synchronous Media Sharing and Icebreaker Questions in Initial Interactions via Video Chat. Proc ACM Hum Comput Interact. (2021) 5:1–26. doi: 10.1145/3479518
14. Gabay G. Perceived control over health, communication and patient–physician trust. Patient Educ Couns. (2015) 98:1550–7. doi: 10.1016/j.pec.2015.06.019
15. Fiscella K, Meldrum S, Franks P, Shields CG, Duberstein P, McDaniel SH, et al. Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care. (2004) 42:1049–55. doi: 10.1097/00005650-200411000-00003
16. Gabay G. Patient self-worth and communication barriers to Trust of Israeli Patients in acute-care physicians at public general hospitals. Qual Health Res. (2019) 29:1954–66. doi: 10.1177/1049732319844999
17. Ward PR. Improving access to, use of, and outcomes from public health programs: the importance of building and maintaining trust with patients/clients. Front Public Health. (2017) 5:22. doi: 10.3389/fpubh.2017.00022
18. Walther JB. Computer-mediated communication impersonal, interpersonal, and hyperpersonal interaction. Commun Res. (1996) 23:3–43. doi: 10.1177/009365096023001001
19. Coleman JS. Social capital in the creation of human capital. Am J Sociol. (1988) 94:S95–S120. doi: 10.1086/228943
20. Hou J, Shim M. The role of provider–patient communication and trust in online sources in Internet use for health-related activities. J Health Commun. (2010) 15 Supplement 3:186–199. doi: 10.1080/10810730.2010.522691
21. Yan L, Tan Y. Feeling blue? Go online: an empirical study of social support among patients. Inf Syst Res. (2014) 25:690–709. doi: 10.1287/isre.2014.0538
22. Yan Z, Wang T, Chen Y, Zhang H. Knowledge sharing in online health communities: a social exchange theory perspective. Inf Manag. (2016) 53:643–53. doi: 10.1016/j.im.2016.02.001
23. Guo Y, Goh DHL. ‘I Have AIDS': content analysis of postings in HIV/AIDS support group on a Chinese microblog. Comput Hum Behav. (2014) 34:219–26. doi: 10.1016/j.chb.2014.02.003
24. Huang HY. Examining the beneficial effects of individual's self-disclosure on the social network site. Comput Hum Behav. (2016) 57:122–32. doi: 10.1016/j.chb.2015.12.030
25. Zhang R. The stress-buffering effect of self-disclosure on Facebook: an examination of stressful life events, social support, and mental health among college students. Comput Hum Behav. (2017) 75:527–37. doi: 10.1016/j.chb.2017.05.043
26. Oh H J, Lee B. The effect of computer-mediated social support in online communities on patient empowerment and doctor–patient communication. Health Commun. (2012) 27:30–41. doi: 10.1080/10410236.2011.567449
27. Zhang X, Guo X, Lai K, Yi W. How does online interactional unfairness matter for patient–doctor relationship quality in online health consultation? The contingencies of professional seniority and disease severity. Eur J Inf Syst. (2019) 28:336–54. doi: 10.1080/0960085X.2018.1547354
28. De Almeida CV, Belim C. Health professionals' communication competences as a light on the patient pathway: the assertiveness, clarity, and positivity (ACP) model. Int J Appl Res Public Health Manag. (2021) 6:14–29. doi: 10.4018/IJARPHM.2021010102
29. Zhao Y, Da J, Yan J. Detecting health misinformation in online health communities: Incorporating behavioral features into machine learning based approaches. Inf Process Manag. (2021) 58:102390. doi: 10.1016/j.ipm.2020.102390
30. Manne S, Ostroff J, Rini C, Fox K, Goldstein L, Grana G. The interpersonal process model of intimacy: the role of self-disclosure, partner disclosure, and partner responsiveness in interactions between breast cancer patients and their partners. J Fam Psychol. (2004) 18:589–99. doi: 10.1037/0893-3200.18.4.589
31. Redlinger-Grosse K, Veach PMC, MacFarlane IM. What would you say? Genetic counseling graduate students' and counselors' hypothetical responses to patient requested self-disclosure. J Genet Couns. (2013) 22:455–68. doi: 10.1007/s10897-012-9568-9
32. Balcom JR, Veach PMC, Bemmels H, Redlinger-Grosse K, LeRoy BS. When the topic is you: Genetic counselor responses to prenatal patients'requests for self-disclosure. J Genet Couns. (2013) 22:358–73. doi: 10.1007/s10897-012-9554-2
33. Weber LR, Carter A. On constructing trust: temporality, self-disclosure, and perspective-taking. Int J Sociol Soc Policy. (1998) 18:7–26. doi: 10.1108/01443339810788290
34. Altman I, Taylor DA. Social Penetration: The Development of Interpersonal Relationships. Holt: Rinehart and Winston (1973).
36. Park S, Chung N. Mediating roles of self-presentation desire in online game community commitment and trust behavior of massive multiplayer online role-playing games. Comput Hum Behav. (2011) 27:2372–9. doi: 10.1016/j.chb.2011.07.016
37. Zink KL, Perry M, London K, Floto O, Bassin B, Burkhardt J, et al. “Let Me Tell You About My…” Provider Self-Disclosure in the Emergency Department Builds Patient Rapport'. West J Emerg Med. (2017) 18:43–9. doi: 10.5811/westjem.2016.10.31014
38. Frost JH, Massagli MP. Social uses of personal health information within Patients Like Me, an online patient community: what can happen when patients have access to one another's data. J Med Internet Res. (2008) 10:e15. doi: 10.2196/jmir.1053
39. Yoo W, Namkoong K, Choi M, Shah DV, Tsang S, Hong Y, et al. Giving and receiving emotional support online: communication competence as a moderator of psychosocial benefits for women with breast cancer. Comput Human Behav. (2014) 30:13–22. doi: 10.1016/j.chb.2013.07.024
40. Rubenstein EL. ‘They are always there for me': The convergence of social support and information in an online breast cancer community. J Assoc Inf Sci Technol. (2015) 66:1418–30. doi: 10.1002/asi.23263
41. Meng J, Dai Y. Emotional support from AI chatbots: should a supportive partner self-disclose or not? J Comput Mediat Commun. (2021) 26:207–22. doi: 10.1093/jcmc/zmab005
42. Lee KT, Noh MJ, Koo DM. Lonely people are no longer lonely on social networking sites: The mediating role of self-disclosure and social support. Cyberpsychol Behav Soc Netw. (2013) 16:413–8. doi: 10.1089/cyber.2012.0553
43. Kim J, Lee JER. The facebook paths to happiness: effects of the number of facebook friends and self-presentation on subjective well-being. Cyberpsychol Behav Soc Netw. (2011) 14:359–64. doi: 10.1089/cyber.2010.0374
44. Chuang KY, Yang CC. Helping you to help me: exploring supportive interaction in online health community. Proc Am Socie Inf Sci Technol. (2010) 47:1–10. doi: 10.1002/meet.14504701140
45. Daft RL, Lengel RH. Organizational information requirements, media richness and structural design. Manag Sci. (1986) 32:554–71. doi: 10.1287/mnsc.32.5.554
46. Daft RL, Lengel RH, Trevino LK. Message equivocality, media selection, and manager performance: Implications for information systems. MIS Q. (1987) 11:355–66. doi: 10.2307/248682
47. Lin C Y, Namdar P, Griffiths M D, Pakpour AH. Mediated roles of generalized trust and perceived social support in the effects of problematic social media use on mental health: a cross-sectional study. Health Expect. (2021) 24:165–73. doi: 10.1111/hex.13169
48. Yang Q, Chen Y, Wendorf Muhamad J. Social support, trust in health information, and health information-seeking behaviors (HISBs): a study using the 2012 annenberg national health communication survey (ANHCS). Health Commun. (2017) 32:1142–50. doi: 10.1080/10410236.2016.1214220
49. Coulson NS. Receiving social support online: an analysis of a computer-mediated support group for individuals living with irritable bowel syndrome. Cyberpsychol Behav. (2005) 8:580–4. doi: 10.1089/cpb.2005.8.580
50. Hether HJ, Murphy ST, Valente TW. It's better to give than to receive: the role of social support, trust, and participation on health-related social networking sites. J Health Commun. (2014) 19:1424–39. doi: 10.1080/10810730.2014.894596
51. Li Y, Wang X. Seeking health information on social media: a perspective of trust, self-determination, and social support. J Organ End User Comput. (2018) 30:1–22. doi: 10.4018/JOEUC.2018010101
52. Han X, Li B, Qu J, Zhu Q. Weibo friends with benefits for people live with HIV/AIDS? The implications of Weibo use for enacted social support, perceived social support and health outcomes. Soc Sci Med. (2018) 211:157–63. doi: 10.1016/j.socscimed.2018.06.016
53. Li Y, Guo Y, Chen L. Predicting social support exchanging among male homosexuals who are HIV-positive in social media context: the role of online self-disclosure. J Homosex. (2021) 1–17. doi: 10.1080/00918369.2021.1935623
54. Kim S, Park H. Effects of various characteristics of social commerce (s-commerce) on consumers' trust and trust performance. Int J Inf Manag. (2012) 33:318–32. doi: 10.1016/j.ijinfomgt.2012.11.006
55. Gong Y, Wang H, Xia Q, Zheng L, Shi Y. Factors that determine a Patient's willingness to physician selection in online healthcare communities: a trust theory perspective. Technol Soc. (2021) 64:101510. doi: 10.1016/j.techsoc.2020.101510
56. Yoo S, Li H, Xu Z. Can I talk to an online doctor? understanding the mediating effect of trust on patients' online health consultation. J Organ Comput Electron. (2021) 31:59–77. doi: 10.1080/10919392.2020.1834810
57. Nazione S, Perrault EK, Keating DM. Finding common ground: Can provider-patient race concordance and self-disclosure bolster patient trust, perceptions, and intentions? J Racial Ethn Health Disparities. (2019) 6:962–72. doi: 10.1007/s40615-019-00597-6
58. Wheeless LR, Grotz J. The measurement of trust and its relationship to self-disclosure. Human Commun Res. (1977) 3:250–257. doi: 10.1111/j.1468-2958.1977.tb00523.x
Keywords: e-health, self-disclosure, social support, physician-patient trust, media richness, computer-mediated communication
Citation: Liu J, He J, He S, Li C, Yu C and Li Q (2022) Patients' Self-Disclosure Positively Influences the Establishment of Patients' Trust in Physicians: An Empirical Study of Computer-Mediated Communication in an Online Health Community. Front. Public Health 10:823692. doi: 10.3389/fpubh.2022.823692
Received: 28 November 2021; Accepted: 03 January 2022;
Published: 25 January 2022.
Edited by:
Pedro Sousa, Coimbra Nursing School, PortugalReviewed by:
Gillie Gabay, Achva Academic College, IsraelCopyright © 2022 Liu, He, He, Li, Yu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianjia He, aGVqaWFuamlhQHVzc3QuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.