
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 27 April 2022
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.806600
This article is part of the Research TopicImmune Responses to HIV Infection: Basic, Clinical and Translational Research in East and Southeast AsiaView all 43 articles
 Yuanyuan Xu1†
Yuanyuan Xu1† Sushu Wu1†
Sushu Wu1† Xuezhen Fu2
Xuezhen Fu2 Jie Ding3
Jie Ding3 Wenjiong Xu4
Wenjiong Xu4 Xin Li1
Xin Li1 Hongjie Shi1
Hongjie Shi1 Mengkai Qiao4
Mengkai Qiao4 Zhengping Zhu1*
Zhengping Zhu1*Background: The growing HIV epidemic among student men who have sex with men (MSM) necessitates immediate attention from public health. In China, male students who have sex with men (SMSM) were also at an increasing risk of HIV transmission. The aim of this study was to investigate the trends in HIV prevalence, HIV-related risk behaviors, and HIV testing, as well as analyze the factors associated with HIV infection among SMSM in Nanjing.
Methods: Data were collected through face-to-face questionnaire interviews and laboratory testing in Nanjing. The participants were recruited among SMSM by snowball sampling and internet-recruited convenience sampling annually from 2016 to 2020. The self-report data primarily included demographics, HIV knowledge, HIV-related behaviors, and HIV testing, while the laboratory test results of HIV and syphilis were collected. Linear-by-linear chi-square test was used to analyze the trends of HIV/syphilis prevalence and its risk behaviors. The binary logistic regression model was used to explore the factors associated with HIV infection.
Results: During the 5 years from 2016 to 2020, a total of 775 SMSM were recruited in our survey (220, 112, 171, 142, and 120, respectively). The HIV prevalence was 5.2, 6.3, 5.3, 7.0, and 8.3%, without a significant increasing trend (P = 0.277). Syphilis prevalence fluctuated from 5.7% in 2016 to 4.2% in 2020, without a significant decreasing trend (P = 0.318). The proportion of consistent condom use in anal intercourse (48.5 to 56.2%, P < 0.05), and HIV testing in the past 12 months (51.0 to 59.2%, P < 0.05) were increasing. A remarkable growing trend has been reported in the percentage of MSM with more than one male sex partner (46.2 to 59.2%, P < 0.05). Multivariate analysis showed that HIV testing in the past 12 months was a protective factor against HIV infection. MSM who had unprotected anal intercourse (UAI) in the past 6 months, recreational drug use, and currently syphilis infection were risk factors for HIV infection.
Conclusions: We observed stable HIV/ syphilis prevalence, increasing consistent condom use, increasing HIV testing rate, and increasing multiple male sex partners dramatically among SMSM in China. The original comprehensive intervention measures should be continuously strengthened for the subgroup. To satisfy the current HIV prevention requirements, new biological interventions should be introduced and carried out as major components of combination prevention programs.
Human immunodeficiency virus (HIV) epidemic among MSM has aroused nationwide substantial concern. The overall HIV prevalence among MSM in China expanded steadily from 5.5% in 2009 (1) to 8.0% in 2015 (2). A meta-analysis extracted from 355 cross-sectional studies and covering 59 cities of China also displayed a climbing tendency in the HIV prevalence among MSM from 2001 to 2018 (3). SMSM (also male students who have oral or anal sex with men) is a unique subgroup of the MSM community, regardless of their sexual orientation or sexual identity, facing an enlarging risk of HIV transmission in China. The newly diagnosed student HIV cases increased from 794 cases in 2010 to 3422 cases in 2019 in China. The 10 years' surveillance (2010–2019) described a total of 23,307 newly-diagnosed student HIV cases, 80.0% of which were infected via homosexual transmission (4). A multicenter cross-sectional study in seven major Chinese cities showed that the HIV incidence rate were 10.0/100 person-year among college student MSM during 2012–2013 (5). Recent meta-analyses also showed that the prevalence of HIV infection among SMSM in China increased from 3.0% between 2003 and 2006 (6) to 5.2% between 2012 and 2016 (7). This rising HIV prevalence among SMSM identifies a distinct risk population that could have an influence on HIV transmission in the school.
Previous studies indicated that HIV prevalence among MSM in Nanjing remained steady at a high level from 2013 to 2017 (8). Among the 183 newly diagnosed student HIV cases reported from 2002 to 2014, 90.2% were infected via male homosexual transmission (9). The newly diagnosed student HIV cases from 2011 to 2016 were 20, 36, 42, 80, and 86, respectively and the proportion of homosexual transmission reached to 93.4% (10). In a previous study in Nanjing, only 10.9% of HIV-positive student MSM insisted on using condoms when having intercourse with male regular sexual partners and 11.9% when having intercourse with those casual partners (11). Moreover, a previous study showed that HIV prevalence among young MSM in Nanjing were 6.76, 9.91, 10.40, 9.14, and 6.82% from 2013 to 2017, respectively (12). The alarming HIV epidemic among student MSM in Nanjing needs to be handled seriously by public health, as evidenced by the annual growth in the number of newly reported cases and the overwhelming dominance of homosexual transmission.
Nanjing implemented comprehensive prevention strategies to mitigate the HIV epidemic among young students especially SMSM, including acquired immunodeficiency syndrome (AIDS) prevention publicity and education, peer education, condom promotion, voluntary HIV testing and counseling (VCT), immediate antiretroviral therapy (ART), and referrals for standard sexually transmitted diseases (STD) treatment from 2015. The China Action Plan for the Thirteenth 5-Year Plan for Combating and Prevention of AIDS were announced by the State Council of China, which outlines the holistic requirements, measures of prevention and treatment, and safeguard measures. The AIDS Prevention and Control Commission of The State Council had launched the third round of national comprehensive demonstration zones for AIDS prevention and control since 2015. Following those requirements, Nanjing city actively explores innovations of HIV prevention for young students in colleges and universities to promote HIV/AIDS prevention and control work, such as strengthening organization management, the regular epidemic notification, multi-department cooperation mechanisms, and expanding the coverage of AIDS education through distinct activities.
However, it is unknown about the effectiveness of these comprehensive strategies among SMSM. Therefore, we conducted a special cross-sectional survey annually. Now, we analyzed the five consecutive surveys from 2016 to 2020 to assess the trends of HIV prevalence, risk behaviors, and HIV testing as well as clarify the factors associated with HIV infection among SMSM.
The study was carried out in Nanjing, the capital city of Jiangsu Province in eastern China, which has a population of 8.6 million people. There are 44 colleges and universities and 21 vocational schools in Nanjing, resulting in a large number of college students, thus including a sizeable number of SMSM.
Male students who had anal or oral intercourse with men in the previous 12 months, were at least 16 years old and were willing to offer written informed consent were included in our questionnaires.
Since the total scale and specific distribution of the SMSM population in Nanjing could not be grasped, the participants were recruited annually from April to July between 2016 and 2020 using snowball sampling and convenience sampling. For the former sampling, volunteers and student volunteers of two MSM Community Based Organizations (CBOs) were mobilized to introduce MSM students who they know to participate in the study. For the latter sampling, we issued recruitment notices through the QQ or WeChat, groups of the MSM CBOs and the Nanjing CDC official website, recruiting SMSMs who are willing to participate.
The surveys were conducted at the VCT clinics of Nanjing CDC or Qinhuai district CDC, whose staff members were annually well-trained interviewers and supervisors. Repeated participants during the same survey year were screened and excluded by duplicate reported telephone numbers. After the qualification screening and written informed consent from each of the eligible participants, face-to-face questionnaires were conducted anonymously in a private room by trained CDC staff. Supervisors are in charge of checking over the questionnaires and conducting supplementary surveys. After pre-test counseling and stringent aseptic procedures, skilled nurses drew 5 mL of venous blood from them. Throughout the 5 years of surveys, the venues, key interviewers, and recruitment strategies remained unchanged.
Data extracted in the questionnaire include demographic information, HIV knowledge, sexual behaviors in the past 6 months (P6M), recreational drug use, diagnosis of sexually transmitted diseases (STD), access to HIV prevention services, and HIV testing in the past 12 months (P12M). We provided rik-reduction counseling for each participant after the test. There was no collection of names or identifiers, however, cell phone numbers were recorded to inform laboratory test results and give referral services as needed. Confirmed HIV cases were subsequently referred to the ART clinic for treatment while current syphilis cases were referred to STD clinics for standard treatment. The receiving clinics will inform the CDC staff whether the case received the necessary treatment promptly.
All the blood samples were tested for HIV and syphilis. Laboratory testing was performed under the National Guideline for Detection of HIV/AIDS (13) and Diagnosis for syphilis (14). We used a rapid test (Determine HIV-1/2, Alere Medical, Chiba Prefecture, Japan) for preliminary HIV-1 antibody screening and an enzyme-linked immunoassay (HIV Ag/Ab ELISA KIT 96T, Zhuhai Livzon Diagnostics, China) for HIV retesting and a western blot assay (HIV BLOT 2.2, MP, Singapore) for HIV confirmation. We used both a treponema pallidum particle assay (TPPA) (Alere Medical) and a rapid plasma reagin test (Diagnosis; Shanghai, Kehua, China) to detect syphilis. Positive results on both tests were considered a confirmed current syphilis infection.
In this study, UAI was defined as failure to consistently use a condom during anal sex in the P6M. UAI was categorized as ‘No' if having no anal sex or always using condom every time and ‘Yes' if condoms were not used all the time. ‘Received any intervention' was defined as receiving any service including AIDS/STI educational materials distribution, condom distribution, lubricant distribution, peer education, HIV counseling, or HIV testing in the past 12 months. ‘Multiple sexual partners' was defined as having two or more male sexual partners in the P6M. Recreational drugs included poppers (alkyl nitrites), ecstasy, ice (methamphetamine), amphetamine, tramadol, and ketamine (8, 15).
Data were double entered using Epi Data (version 3.1, Denmark) and analyzed using SPSS (version 18.0, LEAD Technologies Inc.). Descriptive statistics were used to describe participants' demographic characteristics and prevalence rates. Linear-by-linear chi-square tests were performed to analyze trends in socio-demographic characteristics, HIV prevalence, risk behaviors, and HIV testing from 2016 to 2020. The univariate and multivariate logistic regression analyses were performed to analyze the factors associated with HIV infection. The variables with a P-value <0.1 in univariate analyses were included in the multivariate regression analysis. A stepwise multivariate logistic regression model was conducted to determine variables associated with HIV infection. All statistical significance test results were reported as p-values, which <0.05 (two-tailed) was considered statistically significant.
A total of 775 SMSM were recruited in our survey (220, 112, 171, 142, and 120, respectively) during the 5 years from 2016 to 2020. The socio-demographic characteristics of the participants were shown in Table 1. The average age of all the participants was (22.2±2.7). From 2016 to 2020, the average age was (22.2 ± 2.4), (22.5 ± 2.3), (21.5 ± 2.6), (22.9 ± 3.4), and (22.4 ± 2.6), respectively. The majority of them were Jiangsu residents, highly educated and homosexual. Among the 775 SMSM, 65.5% of them had lived in Nanjing city for more than 2 years and 83.7% of them had sought partners using internet or social networking applications. The composition of the participants and their corresponding characteristics were comparable in the five surveys except for venues of seeking partner (Table 1).
The HIV prevalence among SMSM was 5.2, 6.3, 5.3, 7.0, and 8.3%, respectively. Although there seemed to be an increasing trend, the differences weren't statistically significant according to the linear-by-linear chi-square test (χ2 = 1.184, P = 0.277). Syphilis prevalence was 5.7, 1.8, 2.3, 2.1, and 4.2%, respectively. Despite the figures fell from 5.7percent in 2016 to 2.1percent in 2019 and rebounded to 4.2 percent in 2020, the differences were not statistically significant (χ2 = 0.999, P = 0.318). The trend of the prevalence of HIV/Syphilis was presented in Figure 1. As shown in Table 2, the proportion of consistently using condoms during anal intercourse (AI) increased significantly from 48.5 to 56.2%, whereas the proportion of having multiple male sex partners rose significantly from 46.2% in 2016 to 59.2% in 2020. The proportions of participants who had AI with a regular male partner demonstrated an increasing trend across the years (P < 0.05). In the meantime, the proportion of participants who tested for HIV in the P12M increased statistically (P < 0.05). The mean age at first AI with males was (19.4 ± 2.2) years old. The variables including AIDS awareness, age at first AI with males lower than 18, had AI, had AI with a casual male partner, had commercial anal sex, had vaginal sex, ever used recreational drugs, diagnosed with STD, and received any intervention showed no significant change over the 5 years.
Factors associated with HIV infection among SMSM from the univariate analyses were presented in Table 3. Factors with p-values < 0.10 in univariate analyses were selected for the multivariate analysis. Factors associated with HIV infection from the multivariable logistic regression were reported in Table 4. Those who had UAI in the P6M (OR = 2.2, 95% CI: 1.1–4.0), ever used recreational drugs (OR = 2.3, 95%CI: 1.2–4.2) and currently syphilis infected (OR = 4.6, 95% CI: 1.7–12.9) were associated with higher risk for HIV infection. The participants who tested for HIV in the P12M (OR = 0.4, 95% CI: 0.2–0.8) were less likely to be infected with HIV compared with those not tested.
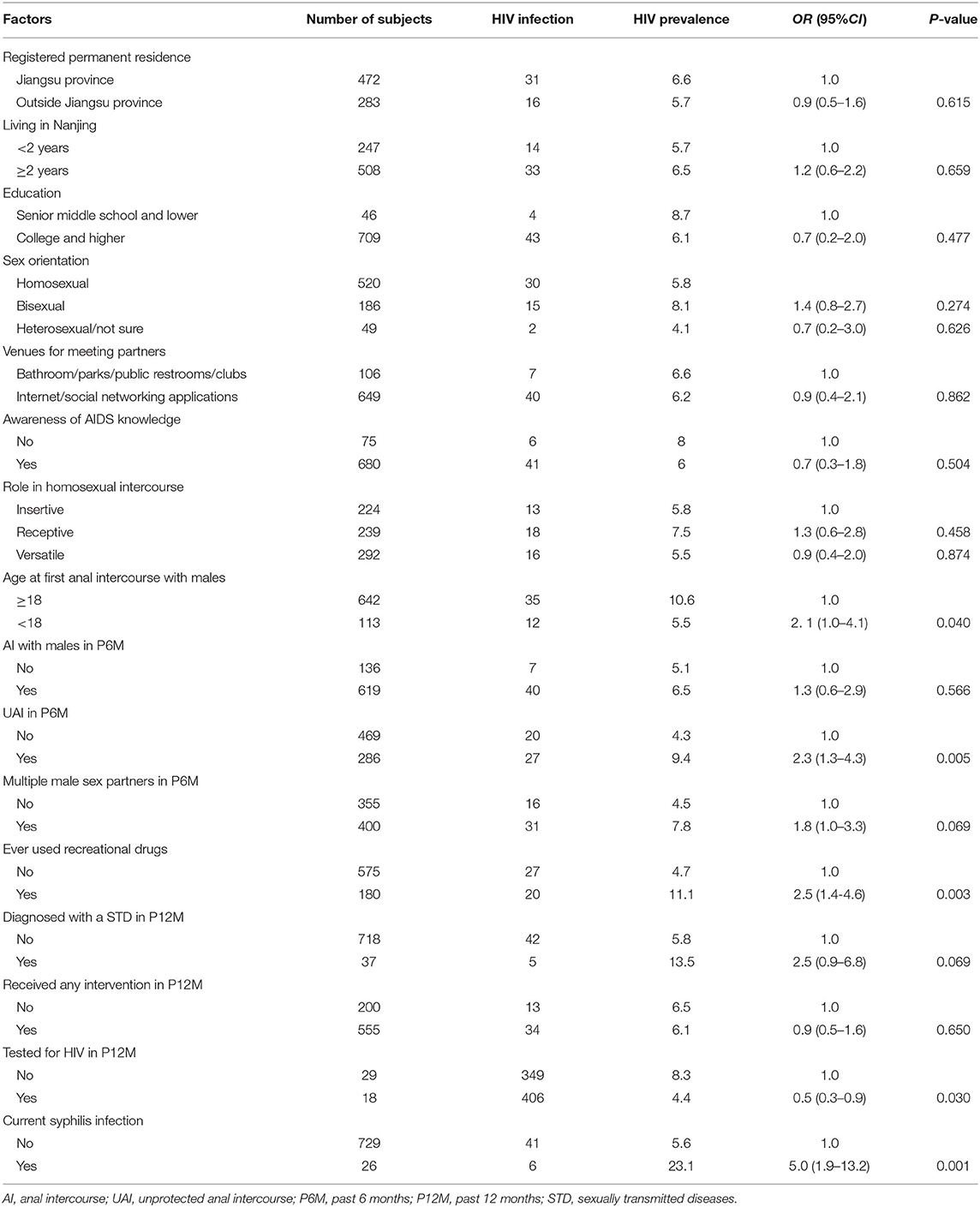
Table 3. Factors associated with HIV infection by univariate logistic regression analyses among SMSM in Nanjing, China.
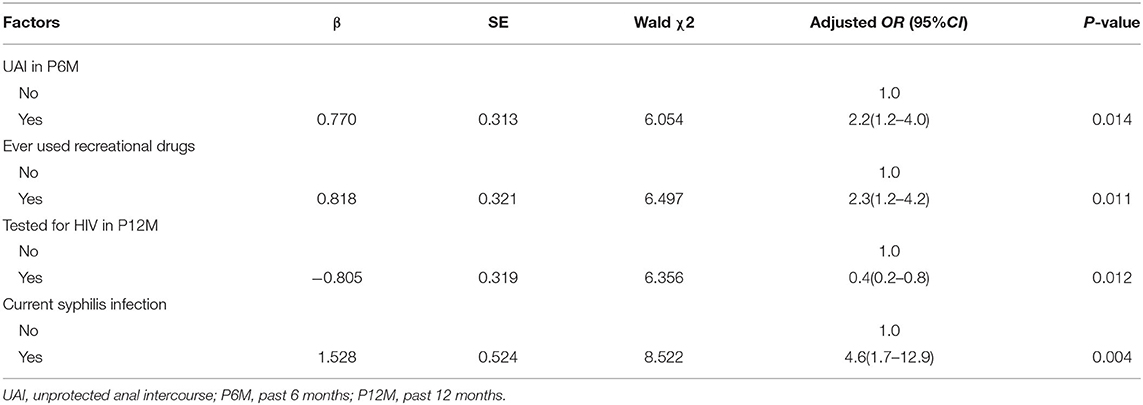
Table 4. Factors associated with HIV infection by multivariate logistic regression analysis among SMSM in Nanjing, China.
Our study found that HIV prevalence among SMSM in Nanjing remained steady from 2016 to 2020, coinciding with the stable HIV prevalence among general MSM during 2013−2017 (8). Although the syphilis prevalence fell from 2016 to 2019 and then rose somewhat in 2020, there is no discernible downward trend overall. The HIV prevalence among SMSM was still much lower than the general MSM population in Nanjing. Compared with other cities, HIV prevalence among SMSM in Nanjing was lower than the reports from seven cities of China (16) (6.5% between 2012 and 2013), Chongqing (17) (10.2% between 2013 and 2014), and Beijing (18) (7.5% between 2013 and 2014). It was also lower than HIV prevalence among young MSM in other countries [e.g., 7.8% in Chicago (19), 10.0% in in 21 US cities in 2008 (20), 24.0% in Thailand (21)]. However, we observed higher HIV prevalence than that in Changsha (22) (5.5% in 2018) and Tianjin (23) (3.15% in 2014 and 4.03% in 2016), which indicated that it was still a serious public health problem among SMSM in Nanjing.
We found an increasing trend in the proportion of consistent condom use during anal intercourse, addressing the concern as to the protective effect of condom use. Simultaneously, we also found an increasing trend in the proportion of HIV testing in P12M, which could attribute to the comprehensive prevention implementation among colleges in Nanjing. Since 2015, Nanjing was designated one of the demonstration zones and launched the “One Region, Different Strategies,” implementing a series of interventions such as HIV epidemic notification, trainers training action, peer education, promotion of condom use, and HIV testing in 51 colleges or vocational schools in Nanjing. The infection rate of HIV did not decrease due to the increase of condom use and detection frequency, indicating further combination prevention programs will be needed containing more evidence-based biomedical interventions besides behavioral and structural interventions to meet the current HIV prevention needs. WHO recommended Post-exposure prophylaxis (PEP) for preventing the acquisition of HIV in 2014 (24) and Pre-exposure prophylaxis (PrEP) in 2015 (25) as an additional prevention choice for people at substantial risk of HIV infection. Hence, we should add in-depth knowledge of PEP and PrEP in our propaganda and promote the critical vulnerable groups of students to obtain corresponding services to greatly impact on reducing the newly-infected cases as possible. Although slightly half of the participants had multiple sexual partners, lower than that reported in three cities of China (65.2%), alarming that the percentage of multiple sexual partners constantly rose from 46.2% in 2016 to 59.2% in 2020. Two factors may explain this result: First, smartphones and network apps can break through the time and place limits and facilitate real-time location to seek sexual partners conveniently using geospatial information technology (e.g. Blued, Aloha, Jack'd, and Zank). App-using MSM were more likely to have multiple sexual partners (26, 27); Second, the proportion of seeking partners via internet/social network apps showed a growing trend during the 5 years. In light of the severe HIV epidemic situation among SMSM in Nanjing, multiple sexual partners could increase the odds of HIV infection and transmission (5, 28). The new generation is not interested in stereotyped propaganda and traditional ideas, so the government must innovate targeted health education and intervention to prevent high-risk sexual behavior based on new media among the subgroup.
Our study showed that UAI in P6M, recreational drug use, HIV testing in P12M and current syphilis infection were associated with HIV infection among SMSM. Similar to other studies, UAI, recreational drug use, and current syphilis infection were the pushers of HIV infection in among SMSM (5, 23). Although closed to 90 percent of participants had sufficient HIV prevention knowledge, only less than half of them used condom consistently. It showed that SMSM had high-risk sexual behaviors and a separation between knowledge and behavior. Syphilis can facilitate HIV transmission because syphilis lesions increase the sexual transmission efficiency of HIV (29). Our study found the total prevalence was 3.2%, slightly lower than that reported among SMSM in Beijing (30) (3.6%) and seven major Chinese cities (5) (4.1%). However, nearly 5% of SMSM reported that they had been diagnosed with STD in the last year, indicating that syphilis and other STDs in SMSM should not be ignored. Therefore, it is imperative to strengthen sexual health and sexual morality education among youth and adolescents. Meanwhile, standard STD treatment and expanding HIV testing for STD outpatient patients need to be further implemented.
In recent years, new drug abuse has become a public health and social problem of global concern. Our study showed that almost a quarter of participants ever used recreational drugs. Although the proportion was lower than that reported among MSM in Beijing (26.8%) (31), two cities of China (32) (29.8%), Ireland (33) (36.0%), New Zealand (34) (36.7%), and the United Kingdom (35) (28.0%), we hadn't observed a declining trend during our study period. Rush popper, as a most common recreational drug, was widely used among MSM to help enhance sexual pleasure by dilating capillaries and relaxing anal sphincters, thus, reducing pain associated with anal sex (31). It is not legally restricted in China and can be purchased easily and cheaply through the internet with advanced internet. Two studies found a higher proportion of recreational drug use among people younger than 25 years old and high educated (36, 37), suggesting that warning education about recreational drugs and interventions addressing reducing recreational drug use also should be focused on SMSM. Furthermore, effective laws and special campaigns to crack down on recreational drug use should be developed, implemented and enforced.
HIV testing is an essential component of HIV prevention. Our study confirmed that HIV testing was a protective factor associated with HIV infection. The counseling that accompanies HIV testing could convey more knowledge or inspire motivation for HIV prevention and enhance HIV awareness, thus HIV testers might be more attentive to taking precautions by reducing high-risk behaviors to lower their HIV risk (18). Our study also showed that the HIV testing rate was over a half among SMSM, lower than that reported in 3 cities of China (70.6%) (38) and USA (78%) (39). HIV testing is central to the UNAIDS 90-90-90 Targets by 2020. However, there was still a large gap between HIV testing rate among SMSM in Nanjing and ‘UNAIDS 90% HIV detection target'. Compared with general MSM, there are additional barriers to HIV testing among students, including low-risk perception, fear of positive diagnosis, concern of disclosure of sexuality, and limited access to testing resources (40, 41). Previous studies suggested HIV self-testing can promote active detection, eliminate the concern of privacy disclosure, and improve the accessibility and pertinence of HIV testing among MSM in China (42, 43). Therefore, we should further expand HIV testing, especially HIV self-testing, promote the habit of regular detection and improve online post-test services in college students to ensure early detection and treatment of student HIV case, thus curbing the rapidly rising HIV epidemic in colleges and universities.
This study had several limitations. First, five cross-sectional studies were inherently descriptive and did not illustrate the causal relationship. Second, the participants were recruited from MSM venues, some MSM social platforms, and a government internet site and they may not be representative of MSM who do not go to these venues or visit the website, which may result in lack of information from hidden SMSM. Third, the questionnaire was answered based on subjective reports and MSM and HIV/AIDS are sensitive issues, leading to a possible information bias. Fourth, because the objects were MSM students in colleges or universities who were very difficult to contact, our study required participants to come to our VCT clinics for HIV testing and questionnaire, which formed a slightly smaller sample size per year.
We observed stable HIV prevalence, increasing consistent condom use and increasing HIV testing rate among SMSM. However, an increase of multiple male partners and steady recreational drug use were observed. In response to the high HIV burden among SMSM in Nanjing, original comprehensive intervention measures, especially promoting condom use, expanding HIV testing and timely treatment, reducing recreational drug use, expanding STD screening and standard treatment should be continuously strengthened. To satisfy the current HIV prevention requirements among SMSM, new biological interventions like PEP and PrEP should be introduced and carried out as major components of combination prevention programs.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Nanjing National Center for AIDS and STD Control. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
SW, XL, and HS were contributed to data collection. WX and MQ contributed to laboratory testing, JD contributed to quality control, YX and XF were responsible for data analysis and manuscript writing, ZZ contributed to the study design and manuscript revision. All authors read and approved the final manuscript.
This study was supported by Nanjing Municipal Key Medical Science and Technology Development Project (Grant no. ZKX19050) and Nanjing Key Medical Specialty Project of Infectious Diseases. The funding had no role in study design, data collection, but had a role in data analysis and preparation for manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors are grateful to all the participants. The authors especially express their thanks to MSM CBOs including: Nanjing Xingyou Community Based Organization, Nanjing Bibochi Bathroom Community Based Organization and Nanjing Compass work studio.
1. Qin Q, Tang W, Ge L, Li D, Mahapatra T, Wang L, et al. Changing trend of HIV, Syphilis and Hepatitis C among men who have sex with men in China. Sci Rep. (2016) 6:31081. doi: 10.1038/srep31081
2. Ge L, Li D, Li P, Guo W, Cui Y. Population specific sentinel surveillance for HIV infection, syphilis and HCV infection in China, during 2010–2015. Dis Surveill. (2017) 32:111eillLi P, Gu3784/j.issn.1003-9961.2017.02.008
3. Dong MJ, Peng B, Liu ZF, Ye QN, Liu H, Lu XL, et al. The prevalence of HIV among MSM in China: a large-scale systematic analysis. BMC Infect Dis. (2019) 19:1000. doi: 10.1186/s12879-019-4559-1
4. Cai C, Tang H, Chen F, Li D, Lv F, et al. Characteristics and trends of newly reported HIV infection in young students in China, 2010–2019. Chin J Epidemiol. (2020) 41:1455–455:0 Epidem3760/cma.j.cn112338-20200417-00592
5. Zhang J, Xu JJ, Chu ZX, Hu QH, Han XX, Zhao B, et al. Disparity of human immunodeficiency virus incidence and drug resistance in college student, non-student youth and older men who have sex with men: a cross-sectional study from seven major cities of China. Chin Med J (Engl). (2020) 133:2778–7783:ed J (E1097/cm9.0000000000001161)
6. Li Y, Xu J, Reilly KH, Zhang J, Wei H, Jiang Y, et al. Prevalence of HIV and syphilis infection among high school and college student MSM in China: a systematic review and meta-analysis. PLoS ONE. (2013) 8:e69137. doi: 10.1371/journal.pone.0069137
7. Shi A, Zhang Z, Wang J, Zhao Y, Wang W, Zhang H, et al. Meta analysis of the high risky behaviors and detection rate of HIV infection among MSM students in Mainland China. Chin J Sch Health. (2018) 39:702–5. doi: 10.16835/j.cnki.1000-9817.2018.05.018
8. Zhu Z, Yan H, Wu S, Xu Y, Xu W, Liu L, et al. Trends in HIV prevalence and risk behaviours among men who have sex with men from 2013 to 2017 in Nanjing, China: a consecutive cross-sectional survey. BMJ Open. (2019) 9:e021955. doi: 10.1136/bmjopen-2018-021955
9. Xu Y, Zhu Z, Wu S et al. HIV/AIDS epidemic status among young students in Nanjing City during 2002–2014. Chin J AIDS STD. (2015) 24:893–4. doi: 10.13419/j.cnki.aids.2015.10.19
10. Xu Y, Li X, Wu S, Liu L, Guo L, Li X, et al. Epidemiological characteristics of HIV infection among population aged 15–24 years from 2011 to 2016 in Nanjing. Chin J Sch Health. (2018) 39:1202–202:8 Sch H16835/j.cnki.1000-9817.2018.08.025
11. Li X. The Epodemiological Characteristics of HIV/AIDS and the Transmission Networks of HIV-1 Among Young Students. Nanjing: Southeast University (2017).
12. Zhu Z, Xu Y, Wu S, Liu L, Li X, Xu W, et al. The epedemiological survey of HIV and syphilis infection among young men who have sex with men. Chin J Dis Control Prev. (2018) 22:1265–265:8 Dis C16462/j.cnki.zhjbkz.2018.12.015
13. Chinese Center for Disease Control and Prevention. National Guideline for Detection of HIV/AIDS (revision in 2015). Beijing: Chinese Center for Disease Control and Prevention (2015).
14. National Health Commission of the People's Republic of China. Diagnosis for Syphilis. Beijing (2018).
15. Dai Y, Musumari PM, Chen H, Huang Y, Techasrivichien T, Suguimoto SP, et al. Recreational drug use, polydrug use and sexual behaviors among men who have sex with men in Southwestern China: a cross-sectional study. Behav Med. (2019) 45:314–22. doi: 10.1080/08964289.2018.1538099
16. Xu JJ, Tang WM, Zou HC, Mahapatra T, Hu QH, Fu GF, et al. High HIV incidence epidemic among men who have sex with men in china: results from a multi-site cross-sectional study. Infect Dis Poverty. (2016) 5:82. doi: 10.1186/s40249-016-0178-x
17. Zeng X, Zhong X, Peng B, Zhang Y, Kong C, Liu X, et al. Prevalence and associated risk characteristics of HIV infection based on anal sexual role among men who have sex with men: a multi-city cross-sectional study in Western China. Int J Infect Dis. (2016) 49:111fect Disern 1016/j.ijid.2016.06.009
18. Liu Y, Qian HZ, Ruan Y, Wu P, Osborn CY, Jia Y, et al. Frequent HIV testing: impact on HIV risk among chinese men who have sex with men. J Acquir Immune Defic Syndr. (2016) 72:452 Immune Defic1097/qai.0000000000001001
19. Garofalo R, Hotton AL, Kuhns LM, Gratzer B, Mustanski B. Incidence of HIV infection and sexually transmitted infections and related risk factors among very young men who have sex with men. J Acquir Immune Defic Syndr. (2016) 72:79r Immune Defi1097/qai.0000000000000933
20. Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM. High HIV incidence and prevalence and associated factors among young MSM, 2008. Aids. (2013) 27:269B, Bowles KE,1097/QAD.0b013e32835ad489
21. Khawcharoenporn T, Mongkolkaewsub S, Naijitra C, Khonphiern W, Apisarnthanarak A, Phanuphak N, et al. Risk, risk perception and uptake of HIV testing and counseling among youth men who have sex with men attending a gay sauna. AIDS Res Ther. (2019) 16:13. doi: 10.1186/s12981-019-0229-z
22. Chen J, Chen J, Xie Z, Shen L, Yang R, Zhang X, et al. Characteristics of high risk behavior of AIDS among male students who have sex with men in Changsha. Chin J AIDS STD. (2019) 25:1161–161:9 AIDS S13419/j.cnki.aids.2019.11.17
23. Bai J, Liu Y, Liu Z, Guo Y, Zhou N. Behavior characteristics and HIV/syphilis infection status among MSM students in Tianjin from 2012 to 2016. Chin J AIDS STD. (2018) 24:58AIDS STDiu10.13419/j.cnki.aids.2018.01.16
24. WHO. Guidelines on post-exposure prophylaxis for HIV and the use of co-trimoxazole prophylaxis for HIV-related infections among adults, adolescents and children[EB/OL]. (2014-12-1) [2021-3-12] Available online at: http://www.who.int/publications/i/item/9789241506830
25. WHO. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. [EB/OL]. (2015-11-9) [2021-3-12] Available online at: http://apps.who.int/iris/bitstream/handle/10665/189977/WHO_HIV_2015.36_eng.pdf;jsessionid=76D67CDD17D75CD87ED960232E0C131B?sequence=1
26. Wei L, Chen L, Zhang H, Yang Z, Zou H. Use of gay app and the associated HIV/syphilis risk among non-commercial men who have sex with men in Shenzhen, China: a serial cross-sectional study. Sex Transm Infect. (2019) 95:496sm Infectho ha1136/sextrans-2018-053902
27. Hong H, Xu J, McGoogan J, Dong H, Xu G, Wu Z. Relationship between the use of gay mobile phone applications and HIV infection among men who have sex with men in Ningbo, China: a cross-sectional study. Int J STD AIDS. (2018) 29:491D AIDSMcGoog1177/0956462417738468
28. You X, Gilmour S, Cao W, Lau JT, Hao C, Gu J, et al. HIV incidence and sexual behavioral correlates among 4,578 men who have sex with men (MSM) in Chengdu, China: a retrospective cohort study. BMC Public Health. (2021) 21:802. doi: 10.1186/s12889-021-10835-4
29. Wu MY, Gong HZ, Hu KR, Zheng HY, Wan X, Li J. Effect of syphilis infection on HIV acquisition: a systematic review and meta-analysis. Sex Transm Infect. (2020) 97:525–33. doi: 10.1136/sextrans-2020-05470
30. Zhao D, Li D. Prevalence of HIV and syphilis among male students who have sex with men (MSM) in Beijing. Chin J AIDS STD. (2019) 25:1276–276:9 AI10.13419/j.cnki.aids.2019.12.20
31. Zhang H, Teng T, Lu H, Zhao Y, Liu H. Yin L, et al. Poppers use and risky sexual behaviors among men who have sex with men in Beijing, China. Drug Alcohol Depend. (2016) 160:42cohol Depend1016/j.drugalcdep.2015.11.037
32. Wang X, Li Y, Wu Z, Tang Z, Reilly KH, Nong Q. Nitrite inhalant use and HIV infection among chinese men who have sex with men in 2 large cities in China. J Addict Med. (2017) 11:468 Medong chine1097/adm.0000000000000347
33. Barrett P, O'Donnell K, Fitzgerald M, Schmidt AJ, Hickson F, Quinlan M, et al. Drug use among men who have sex with men in Ireland: prevalence and associated factors from a national online survey. Int J Drug Policy. (2019) 64:5–12. doi: 10.1016/j.drugpo.2018.11.011
34. Saxton P, Newcombe D, Ahmed A, Dickson N, Hughes A. Illicit drug use among New Zealand gay and bisexual men: prevalence and association with sexual health behaviours. Drug Alcohol Rev. (2018) 37:180ohol Revwith1111/dar.12536
35. Thurtle N, Dargan PI, Hunter LJ, Lovett C, White JA, Wood DM, et al. comparison of recreational drug use amongst sexual health clinic users in London with existing prevalence data. Int J STD AIDS. (2016) 27:1309–309:6STD AID1177/0956462415616056
36. Chen J, Huang YL, Chen HL, Xia J. Nitrite inhalants use, sexual behaviors and HIV/syphilis infection among men who have sex with men in Chongqing, China. Infect Dis Poverty. (2020) 9:127. doi: 10.1186/s40249-020-00748-6
37. Xu Y, Zhu Z, Wu S, Liu L, Guo L, Li X. Status and associated factors of recreational drug use among man who have sex with man in Nanjing. Chin J Dis Control Prev. (2019) 23:1476–476:9 Dis Co16462 /j.cnki.zhjbkz.2019.12.009
38. Han J, Li J, Wang K, Jiang T, Song B, Wang H, et al. Status and influencing factors of knowledge awareness and service acceptance of HIV non-occupational post-exposure prophylaxis of men who have sex with men among college students among three cities of China, 2019. Chin J Prev Med. (2020) 54:1220–220:0 Prev 3760/cma.j.cn112150-20200310-00302
39. Ye R, Liu C, Tan S, Li J, Simoni JM, Turner D. Factors associated with past HIV testing among men who have sex with men attending university in China: a cross-sectional study. Sex Health. (2021) 18:58lthC, Tan S, 1071/sh20088
40. Sumartojo E, Lyles C, Choi K, Clark L, Collins C, Grey CG, et al. Prevalence and correlates of HIV testing in a multi-site sample of young men who have sex with men. AIDS Care. (2008) 20:1arence and co1080/09540120701450425
41. Levy ME, Wilton L, Phillips G, Glick SN, Kuo I, Brewer RA, et al. Understanding structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS Behav. (2014) 18:972–96. doi: 10.1007/s10461-014-0719-x
42. Zhang C, Koniak-Griffin D, Qian HZ, Goldsamt LA, Wang H. Impact of providing free HIV self-testing kits on frequency of testing among men who have sex with men and their sexual partners in China: a randomized controlled trial. PLoS Med. (2020) 17:e1003365. doi: 10.1371/journal.pmed.10033
Keywords: HIV/AIDS, men who have sex with men, prevalence, risk behaviors, students
Citation: Xu Y, Wu S, Fu X, Ding J, Xu W, Li X, Shi H, Qiao M and Zhu Z (2022) Trends in HIV Prevalence and HIV-Related Risk Behaviors Among Male Students Who Have Sex With Men From 2016 to 2020 in Nanjing, China: Consecutive Cross-Sectional Surveys. Front. Public Health 10:806600. doi: 10.3389/fpubh.2022.806600
Received: 01 November 2021; Accepted: 24 March 2022;
Published: 27 April 2022.
Edited by:
Weiming Tang, University of North Carolina at Chapel Hill, United StatesReviewed by:
Tolulope Olumide Afolaranmi, University of Jos, NigeriaCopyright © 2022 Xu, Wu, Fu, Ding, Xu, Li, Shi, Qiao and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhengping Zhu, enpwQG5qY2RjLmNu
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.