- 1Department of Epidemiology and Health Statistics, School of Public Health, Wuhan University, Wuhan, China
- 2Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 3The Jockey Club School of Public Health and Primary Care, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 4Department of Epidemiology and Biostatistics, Institute of Basic Medical Sciences Chinese Academy of Medical Sciences, School of Basic Medicine of Peking Union Medical College, Beijing, China
- 5Center of Environmental and Health Sciences, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing, China
- 6Global Health Institute, Wuhan University, Wuhan, China
Background: Prior studies have reported the effects of particulate matter (PM) on respiratory disease (RD) hospitalizations, but few have quantified PM-related economic loss in the central region of China. This investigation aimed to assess the impacts of PM pollution on the risk burden and economic loss of patients admitted with RD.
Methods: Daily cases of RD admitted to the hospital from 1 January 2015 to 31 December 2020 were collected from two class-A tertiary hospitals in Wuhan, China. Time series analysis incorporated with a generalized additive model (GAM) was adopted to assess the impacts of fine particulate matter (PM2.5) and inhalable particulate matter (PM10) exposures on patients hospitalized with RD. Stratified analyses were performed to investigate underlying effect modification of RD risk by sex, age, and season. The cost of illness (COI) approach was applied to evaluate the related economic losses caused by PM.
Results: A total of 51,676 inpatients with a primary diagnosis of RD were included for the analysis. PM2.5 and PM10 exposures were associated with increased risks of hospitalizations for RD. Subgroup analysis demonstrated that men and children in the 0–14 years age group were more vulnerable to PM, and the adverse effects were promoted by low temperature in the cold season. A 152.4 million China Yuan (CNY) economic loss could be avoided if concentrations of PM2.5 and PM10 declined to 10 and 20 μg/m3, respectively.
Conclusions: PM2.5 and PM10 concentrations were positively associated with RD hospitalization. Men and children were more vulnerable to PM. Effective air pollution control measures can reduce hospitalizations significantly and save economic loss substantially.
Introduction
According to the Global Burden of Disease (GBD) Study 2019, particulate matter (PM) was one of the largest increased risk exposures worldwide between 2010 and 2019, the percentage of disability-adjusted life-years (DALYs) attributable to PM increased from 2.7% in 1990 to 4.7% in 2019 (1). PM pollution contributed to approximately global 2.49 million deaths and 83 million DALYs in 2017 (2). A province-level disease burden study in China reported that PM was one of the top four risk factors for a number of deaths and accounted for more than 5% of DALYs in 2017 (3).
PM can cause damage to the respiratory system by absorbing toxic metals, carcinogens, and pathogenic bacteria (4); on the other hand, PM deposited in the lung can lead to lung damage by mediating inflammatory response and oxidative stress (5, 6). Population-based epidemiological evidence suggests that PM was associated with respiratory disease (RD) morbidity and mortality (7, 8). Fine particulate matter (PM2.5) and inhalable particulate matter (PM10) were affirmed to be associated with increased emergency (9, 10) or hospital admissions (11, 12) for asthma (4, 11), pneumonia (13), chronic obstructive pulmonary disease (COPD) (11, 14), and bronchiectasis (11). Some studies also demonstrated the effect of PM on mortality in COPD (14), pneumonia (15), and lung cancer (15, 16). PM was the second-highest risk factor for respiratory tract cancer (tracheal, bronchus, and lung cancers) in 2019, contributing to 15.1% of deaths for these cancers (16). In the past few decades, China has experienced dramatic increases in industrialization and urbanization, accompanied by deterioration of air quality and population health. A study covering 338 Chinese cities revealed that PM2.5 caused 1.35 million all-cause premature mortalities, which were equivalent to 17.2% of reported deaths in China in 2017 (17).
Air pollution caused a heavy disease burden, at the same time the economic loss could not be ignored. Air pollution resulted in illness and in turn reduced productivity, decreased working hours and labor supply, and lost welfare (18, 19). An economic study forecasted that the global economic costs of outdoor air pollution gradually increased to 1% of global gross domestic product (GDP) by 2060, with the highest GDP losses in China (20), which mainly reaches to relatively high pollution-related health expenditures and aging population. In China, air pollutants caused economic loss attributable to hospital admission, and premature mortality was 2,065.54 billion China Yuan (CNY), accounting for 2.5% of the national GDP in 2017 (21). A lot of domestic studies analyzed medical costs or economic loss in the northern area like Shanxi (22) and Hebei (23) or economically developed regions like Beijing (24, 25) and the Pearl River Delta (26, 27). However, few studies focused on the central region. Wuhan is the only sub-provincial city in central China. The objective of this study is to provide the risk assessment for RD hospitalization followed by the economic loss evaluation of PM in Wuhan.
Methods
Description of the Study Area
Wuhan is the capital of Hubei province. In 2020, Wuhan had a 12.32 million permanent resident population (28). Wuhan is a nationally important industrial base and a comprehensive transportation hub. Vehicle sources and manufacturing emissions were the main air pollution sources in Wuhan (29). Meanwhile, Wuhan is located in the Jianghan Plain, which is one of the largest commercial grain production bases in China (30). Biomass burning also caused heavy pollution in Wuhan (31). The annual average concentration of PM2.5 and PM10 were 45 and 71 μg/m3, respectively in 2019, exceeding the national air quality secondary standard (PM2.5: 35 μg/m3; PM10: 70 μg/m3).
Data Collection
Records of Hospitalization
Hospitalization data were obtained from the hospital information system (HIS) of two class-A tertiary hospitals in Wuhan from 1 January 2015 to 31 December 2020. The data consisted of age, gender, principal disease diagnosis, admission date, discharge date, length of stay (LOS), and hospitalization expenses. The diagnosis of the disease was coded according to the International Classification of Disease Tenth Revision (ICD-10). Hospitalization due to all RDs (ICD-10: J00-J99), COPD (ICD-10: J40–J44), and pneumonia (ICD-10: J12-J18) was analyzed in this study. Hospitalization cost was adjusted according to the consumer price index (CPI) to eliminate the impact of price fluctuations.
Daily Air Pollutants and Meteorological Data
In recent years, the air pollutant concentrations obtained from ground monitoring networks have been used in many studies to evaluate the health effects associated with air pollution in China (21). Daily mean concentrations of PM2.5 and PM10 from 1 January 2015 to 31 December 2020 in Wuhan were collected from the Hubei Environmental Protection Bureau (https://sthjt.hubei.gov.cn/), and contemporary meteorological data, such as daily mean temperature and relative humidity, were obtained from China Meteorological Data Network (http://data.cma.cn/).
Statistical Analysis
A three-stage analysis was applied to assess the impact of PM2.5 and PM10 exposures on RD hospitalizations and related economic losses.
Time Series Decomposition
In the first stage, we decomposed the time-series data of all hospitalizations for RDs, pneumonia, and COPD to detect potential long-term trends and seasonality. The time series data were split into three components (32):
where Y is the number of RD hospitalizations, Tt is the long-term trend, and St is seasonality and Rt is residual.
Impact on Hospitalization
In the second stage, the Spearman rank correlation was applied to measure the association between air pollutants and meteorological data. A generalized additive model (GAM) with quasi-Poisson regression was used to fit the association between PM and RD hospitalization, adjusting for a set of covariates:
where Ei is the expected value of the hospitalization count for RD on day i; βi is the regression coefficient; Ci is mean concentrations of air pollutants on day i; Time is the days of calendar time on day i and DOW and Holiday are dummy variables that represent the day of the week and a public holiday, respectively (12); ns represents a natural spline smoothing function (12); Mt is the mean temperature; Rh is the relative humidity; and α is the intercept. The degree of freedom (df) of each variable was chosen referred to the previous study. We initialized the df as 4 df /year for Time, 3 df for Mt and Rh (33).
We calculated the percent change (PC) of hospitalization count for RD attributable per 10 μg/m3 addition of PM:
where βi refers to the regression coefficient of air pollutants derived from the GAM analysis.
Given that air pollutant exposure had a significant delayed effect on health, this study examined the effect with different lag structures of single-day lag (from lag0 to lag7), where lag0 corresponds to the current day. In addition, we estimated the association between PM and RD hospitalization count for subgroups stratified by gender (male and female), age (0–14, 15–64, and 65+ years), season (warm and cold season), and specific disease (pneumonia and COPD). The warm season was defined as the month of admission date between April and October, and the cold season was the month of admission date between November and March (34).
Economic Losses Analysis
In the third stage, we applied the cost-of-illness (COI) approach to estimate the economic loss due to hospital admissions for RD (21). Attributable number (AN) and attributable fraction (AF) are indicators of attributable risk. AN is the number of RD hospitalizations attributed to air pollution. AF represents the proportion of hospital admission contributed to air pollution in total hospitalization:
where β refers to the regression coefficient obtained from the GAM analysis; Ci is the mean concentration of PM on day i; C0 is the threshold concentration of PM, which was assumed to be 0 in this study (21).
where Popj represents the permanent population of Wuhan, which was 10.61, 10.77, 10.89, 11.08, 12.21, and 12.45 million in 2015, 2016, 2017, 2018, 2019 and 2020, respectively. Proj is the hospitalization rate of RD. We used the annual RD hospitalization rate of China in 2017 to replace it due to data unavailability, which was 810.22 per 105 population (21).
The economic loss attributable to RD hospitalization related to PM was estimated with the COI method:
where ECOloss is the average economic loss for RD hospitalization for each case; COSTmean is the average hospitalization cost for RD of each case; Daymean is the average LOS for inpatients of RD; PGDPday is the GDP per capita per day in Wuhan. TECOloss is the total economic loss for RD hospitalization attributable to PM.
Sensitivity Analysis
To test the robustness of the model, we performed a sensitivity analysis by: (1) changing df for Time (df = 3 or df = 5) and (2) establishing two-pollutants models (SO2, NO2, O3, CO).
All analyses were performed in R programming language (version 3.6.1, R Foundation for Statistical Computing, Vienna, Austria). The values of p < 0.05 were considered to be statistically significant.
Results
A total of 51,676 RD hospitalization cases were included in this study, of which 60.68% were men. Table 1 presents the descriptive statistics of daily hospitalization counts, air pollutant concentration, and meteorological factors. Daily mean hospitalization counts for all RDs were 23.57. More daily hospitalization counts were observed in men than women. In addition, daily hospitalization counts of the group aged 65+ were higher than that of the 0–14 and the 15–64 age groups.
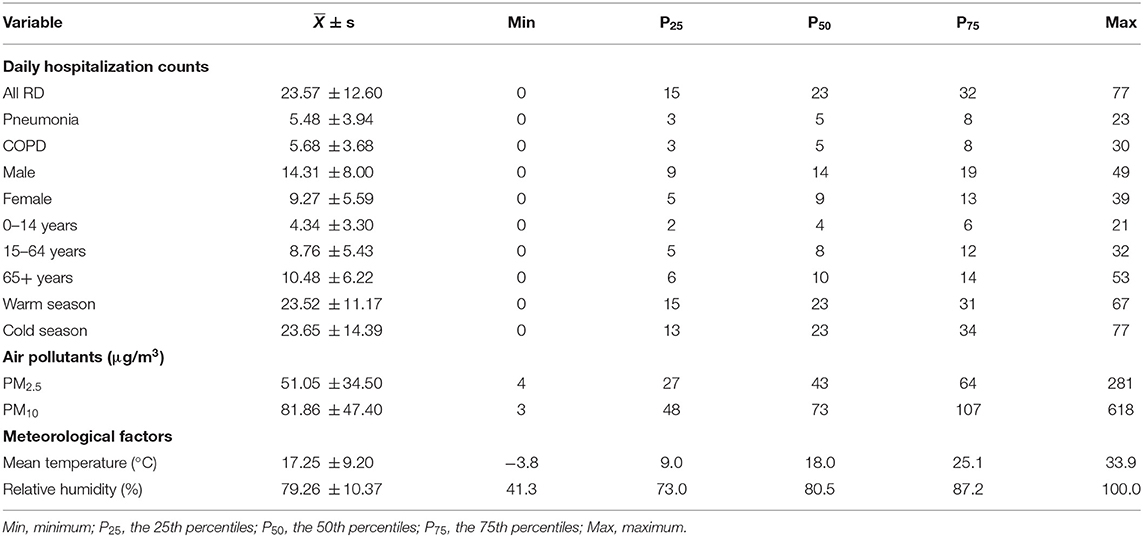
Table 1. Descriptive statistics of daily hospitalization counts of RD, air pollutant concentration, and meteorological factors in Wuhan, China, 2015–2020.
Figure 1 shows the result of the time series decomposition analysis of the hospitalization count of all RDs, pneumonia, and COPD from 2015 to 2020. The daily hospitalization counts showed an increasing trend between 2015 and 2019 but reduced notably in 2020. The obvious seasonal fluctuations existed in daily hospitalization counts, which were higher in spring and winter than that in summer and autumn.
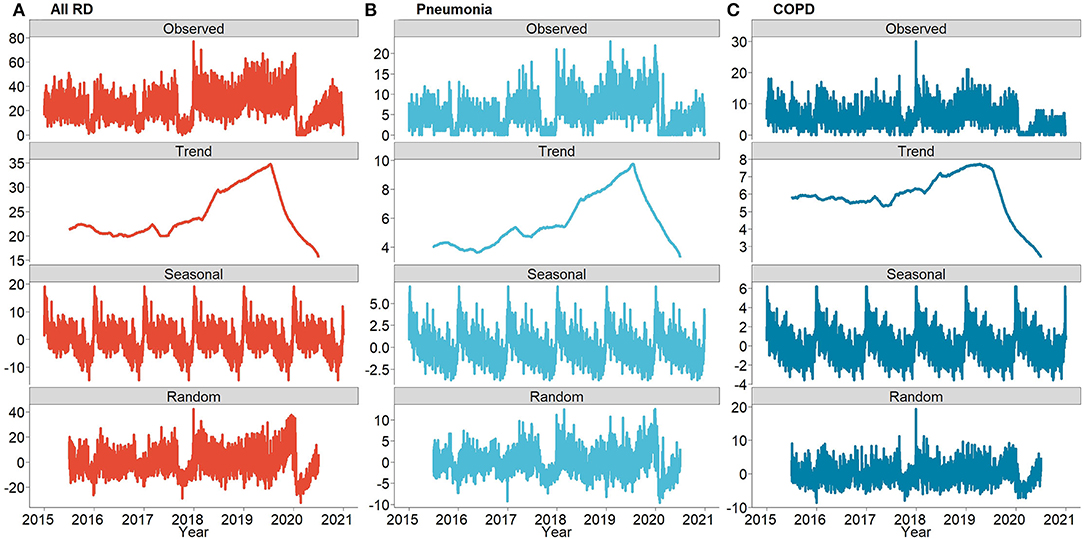
Figure 1. The decomposed distributions for the daily number of hospitalizations due to all RDs, Pneumonia and COPD in Wuhan, China from 2015 to 2020: (A) daily number of hospitalizations of all RDs, (B) daily number of hospitalizations of Pneumonia, and (C) daily number of hospitalizations of COPD.
The median of all RD hospitalization costs between 2015 and 2020 was 8,938.16 CNY, and the average LOS of all RDs was 9.33 days. More details are shown in Supplementary Tables S1, S2. Figure 2 illustrates the trend of average hospitalization costs and LOS by disease, gender, and age group from 2015 to 2020. The average hospitalization cost of patients with all RDs and COPD showed a fluctuating trend between 2015 and 2019, then increased in 2020. While the average hospitalization cost of patients with pneumonia showed an increasing trend, exceeding that of all patients with RDs and COPD, and then increased dramatically in 2020. The hospitalization cost of male patients with RD was higher than that of female patients. The age group of 65+ years old had the highest hospitalization cost in all age groups. The average LOS of patients with RD showed a decreasing trend from 10.14 days in 2015 to 8.41 days in 2019 and increased to 9.92 days in 2020. The LOS of patients with COPD was relatively consistent with the trend of all RDs, whereas the LOS of patients with pneumonia increased markedly in 2020 and exceeded all RDs and COPD.
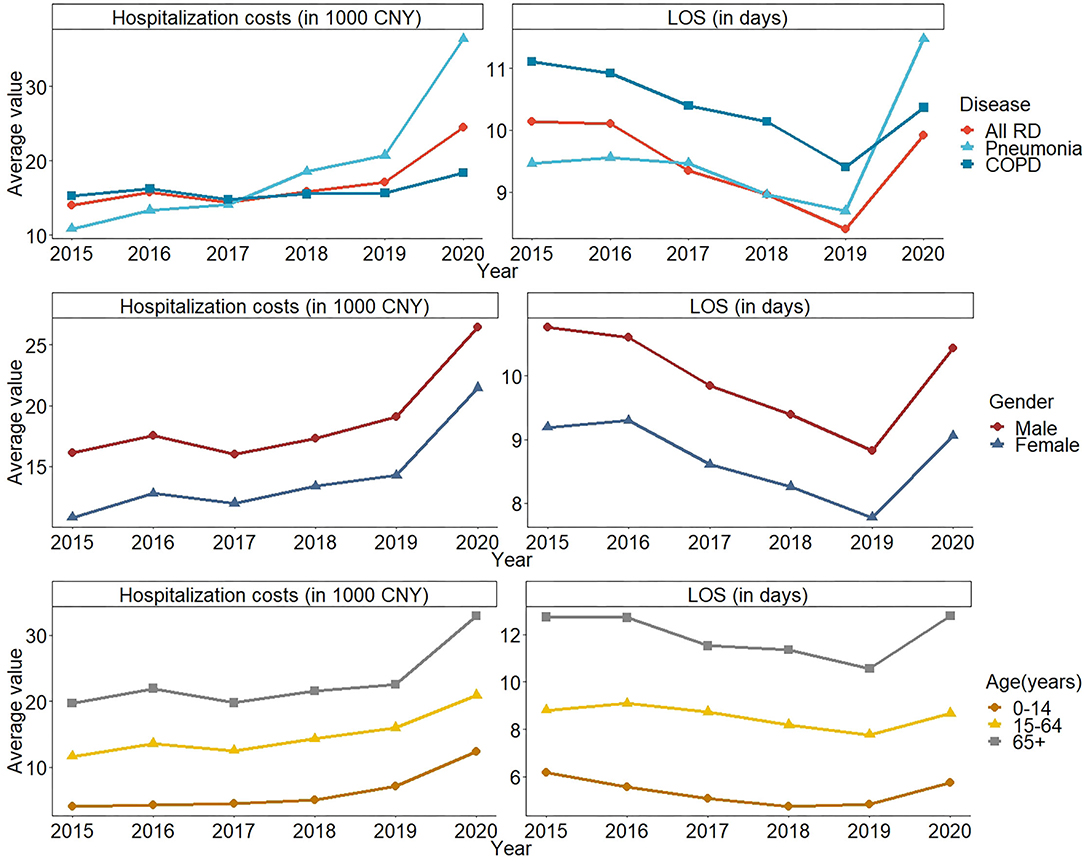
Figure 2. The trend of average hospitalization costs and LOS due to RD in Wuhan, China from 2015–2020 by disease, gender, and age group.
The Spearman rank correlation results are shown in Supplementary Table S3. Briefly, we observed positive correlations between PM2.5, PM10, SO2, NO2, and CO but a negative correlation between these pollutants and O3. The results of GAM are presented in Figure 3. When PM2.5 concentration increased by 10 μg/m3, the number of hospitalizations for all RDs increased by 1.23% (95% CI: 0.31, 2.15), 1.60% (0.68, 2.52), and 2.34% (1.42, 3.27) on lag5, lag6, and lag7, respectively. The number of pneumonia hospitalizations significantly increased on lag5, lag6, and lag7, by 1.28% (0.49, 2.07), 1.50% (0.71, 2.30), and 1.75% (0.95, 2.55), respectively. Although no statistical significance was found, we observed a negative association between increasing PM2.5 concentration and the number of all RD and pneumonia hospitalizations on lag0–lag4. PM2.5 increased COPD hospitalization on lag0 and lag7, by 0.9% (0.17, 1.63) and 1.75% (1.03, 2.48), respectively. Every 10 μg/m3 increase of PM10 concentration only caused hospitalization increase for all RDs and pneumonia on lag7; the PC was 0.77% (0.20, 1.33) and 0.73% (0.24, 1.23), respectively. Similarly, the increase of PM10 showed a decreased effect in the number of hospitalizations on lag0. Also, PM10 had no significant effect on COPD.
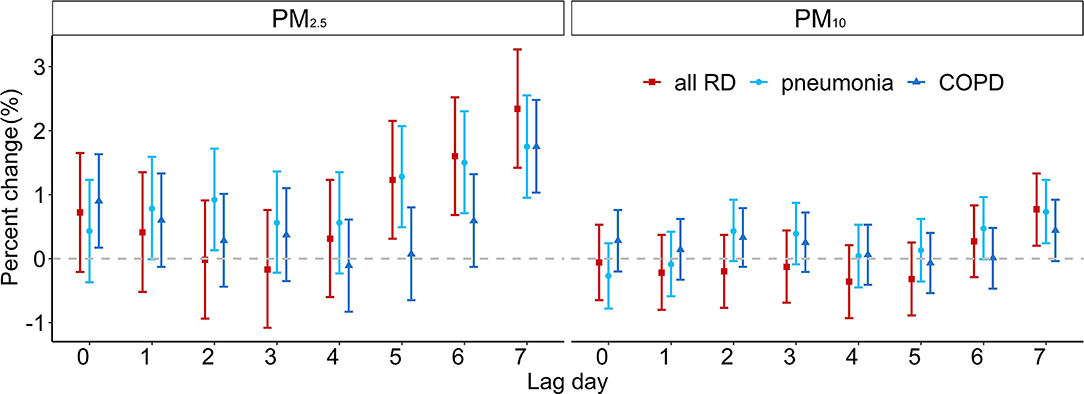
Figure 3. The estimated PC of RD hospitalizations per 10 μg/m3 increase in PM2.5 and PM10 concentrations.
Figure 4 shows the PC of hospitalizations attributable to the increase in PM2.5 and PM10 concentrations at different lag days by gender, age group, and season. The 10 μg/m3 increment in PM2.5 caused distinct hospitalization count rise on lag0, lag1, lag3, lag6, and lag7 for men and on lag0, lag1, and lag7 for women; both highest increases occurred on lag7 with 1.76% (1.27, 2.25) and 0.74% (0.14, 1.35). The effect of PM10 concentration increase was demonstrated on lag7 with 0.88% (0.57, 1.18) rise for men, and PM10 had no significant effect on women. In age-specific analyses, we found that increasing PM2.5 and PM10 concentration had the greatest effect on the 0–14-year age group, which resulted in 2.34% (1.42, 3.27) and 0.77% (0.20, 1.33) hospitalization increase on lag7. For the 15–64-year age group, the greatest effect associated with PM2.5 exposure on the number of hospitalizations appeared on lag7 with 1.08% (0.45, 1.72). For the age group of 65+, the highest PC of hospitalization with a 10 μg/m3 increment in PM2.5 was found on lag7 with 1.25% (0.70, 1.81). The effects of PM2.5 and PM10 concentration rise in the cold season were greater than those in the warm season. The largest effect of PM2.5 in the cold season was observed on lag7 with 0.76% (0.29, 1.23). The results of disease-specific analysis (pneumonia and COPD) are exhibited in Supplementary Tables S4, S5. On the whole, under the influence of the PM concentration increase, the number of hospitalizations of subgroup showed a trend of first rise, then decline and rise again, which was especially obvious in the influence of PM2.5 on women and on the 0–14-year age group.
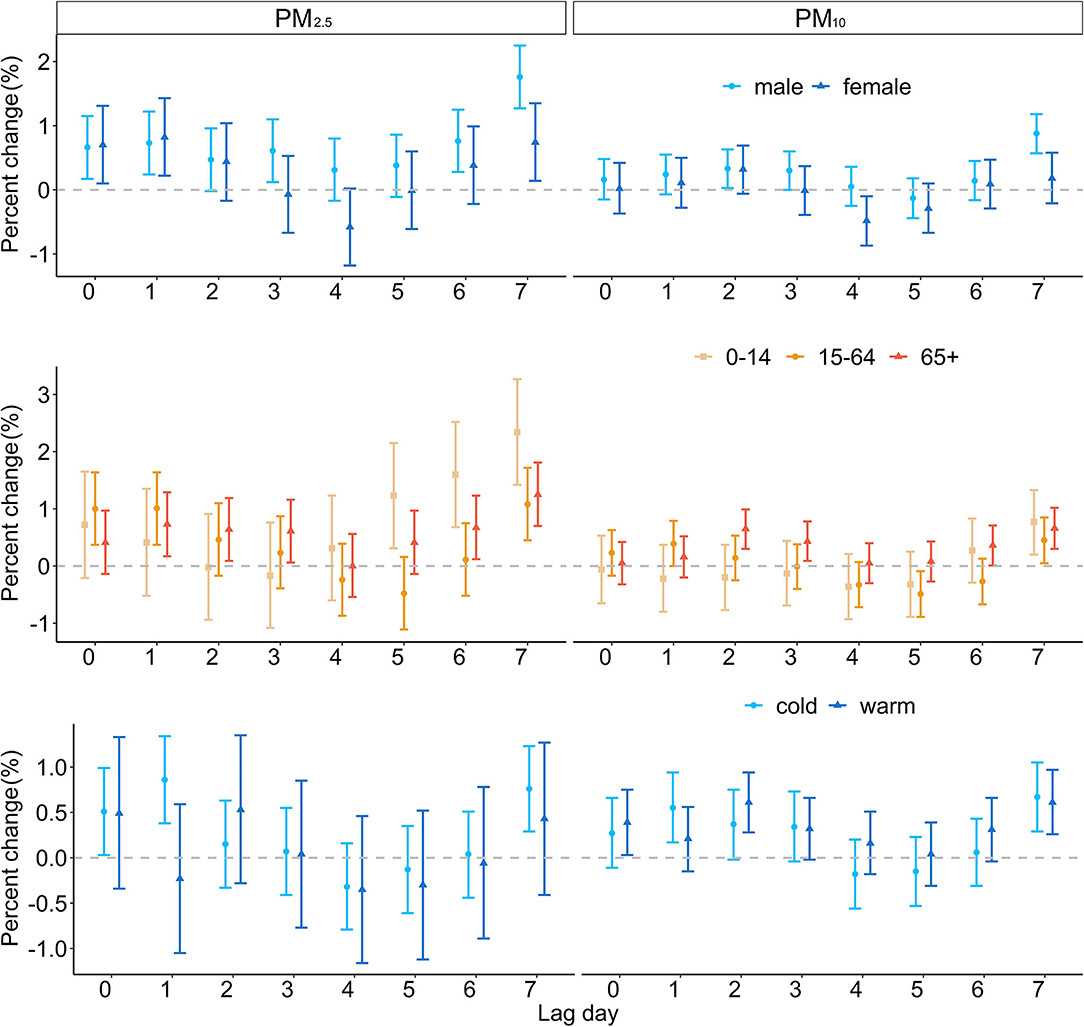
Figure 4. The estimated PC of RD hospitalizations per 10 μg/m3 increase in PM2.5 and PM10 concentrations by gender, age group, and season.
The result of sensitivity analyses is shown in Supplementary Table S6. After changing df for Time and establishing two-pollutant models, the effect of PM on hospitalizations remained stable, suggesting that the main model is stable and meaningful.
The lag days with the greatest impact of PM on RD hospitalization were selected for attribution analysis; the results of the RD hospitalization count and economic losses due to PM2.5 and PM10 are demonstrated in Table 2. The number of RD hospitalizations attributable to PM2.5 and PM10 was 59.40 thousand and 32.60 thousand, respectively. The economic losses attributed to PM2.5 and PM10 were 1,304.92 million CNY and 716.29 million CNY. Higher hospitalization count and economic losses were found in men and 65+ year-old age group.
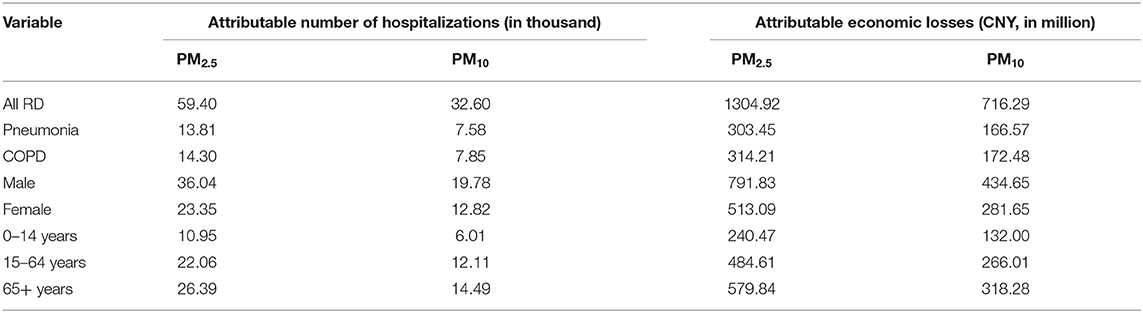
Table 2. The number of RD hospitalizations and economic losses attributable to PM2.5 and PM10 in Wuhan, China, from 2015 to 2020.
In the WHO 2020 global air quality guidelines, 4 interim target recommendations were proposed for annual concentrations of PM2.5 (35, 25, 15, and 10 μg/m3) and PM10 (70, 50, 30, and 20 μg/m3). Assuming that the concentrations of PM2.5 and PM10 from 2015 to 2020 can reach the WHO guidelines, the annual avoidable hospitalizations and the savable economic losses are displayed in Figures 5, 6. If the annual concentration of PM2.5 could reach 10 μg/m3, 4,580 hospitalizations and 100.57 million CNY economic losses could be avoided. If the annual concentration of PM2.5 could reach 20 μg/m3, 2,360 hospitalizations could be avoided for all RDs, and the corresponding cost reduction could be 51.77 million CNY.
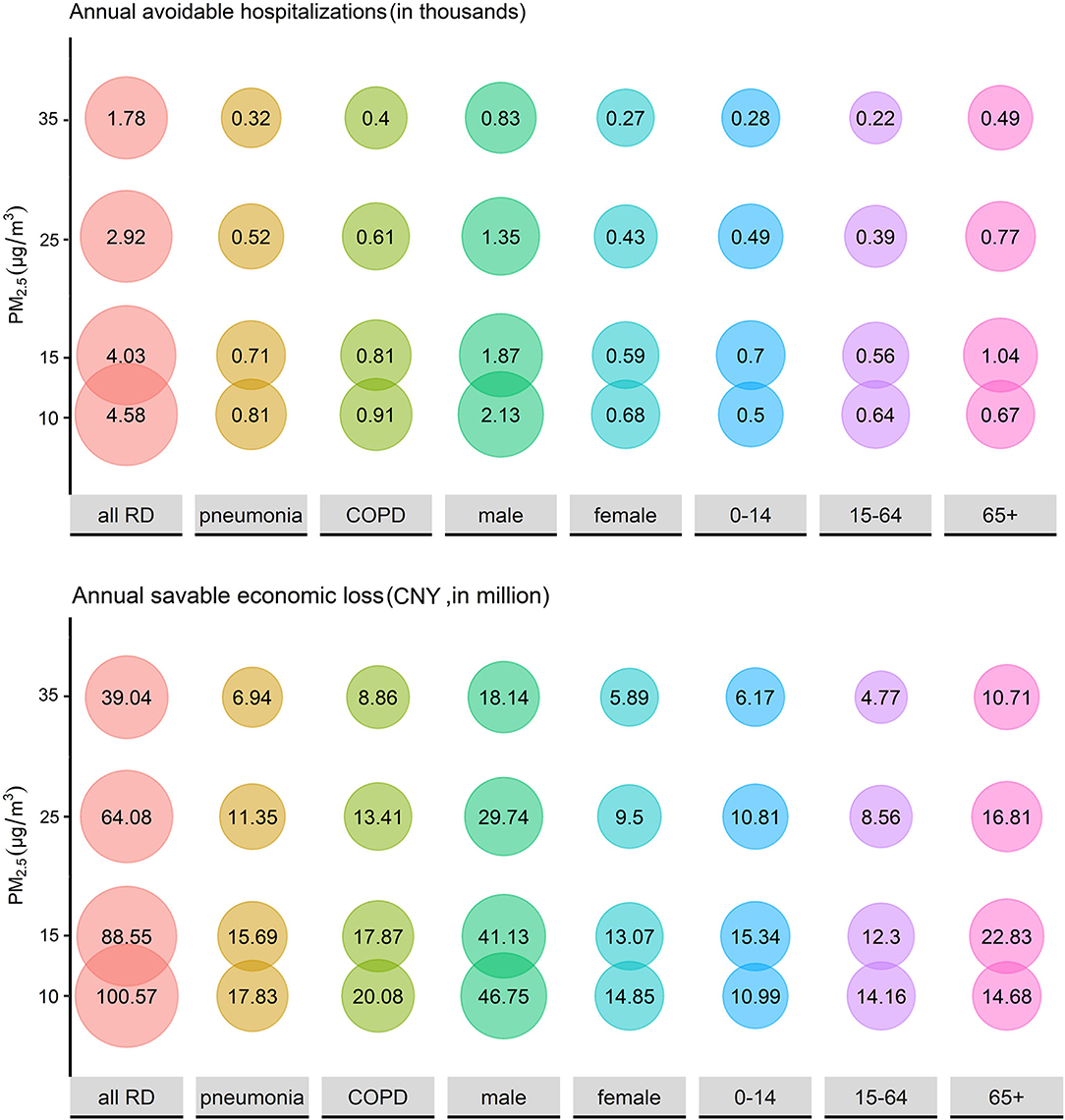
Figure 5. The estimated annual avoidable hospitalizations and savable economic losses if the historical concentration of PM2.5 could be maintained at relatively low levels.
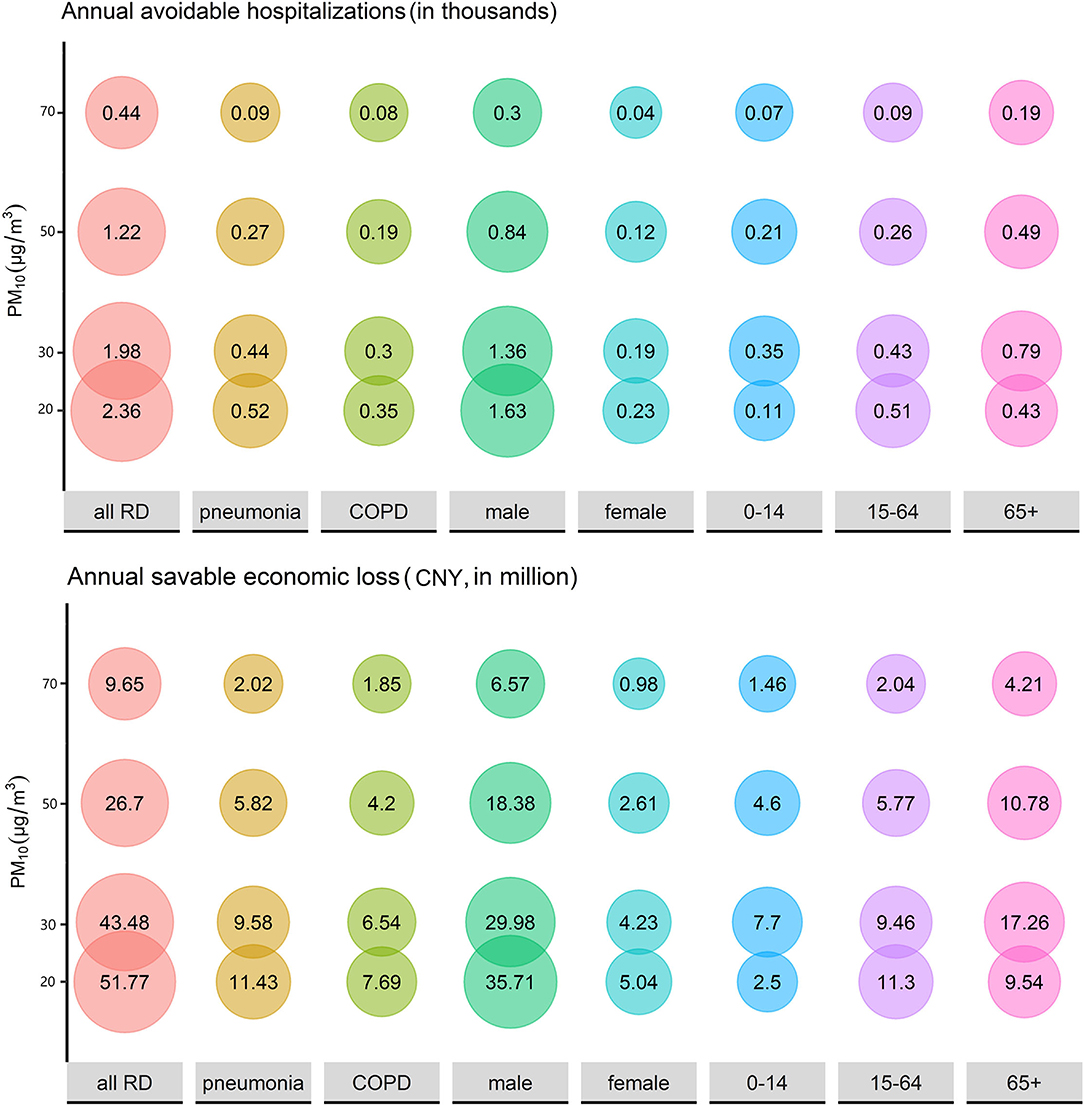
Figure 6. The estimated annual avoidable hospitalizations and savable economic losses if the historical concentration of PM10 could be maintained at relatively low levels.
Discussion
In this research, we used comprehensive data to examine the RD hospitalization risk attributable to PM exposure and evaluate the accompanying economic losses. PM2.5 and PM10 were demonstrated to increase hospitalization for RD, and this influence had a delay effect. Men and 0–14-year-old age group were most vulnerable. PM caused huge RD hospitalization costs; if the concentration of PM2.5 and PM10 could reach the guideline values recommended by WHO, enormous economic losses could be avoided.
From 2015 to 2019, hospitalizations for all RDs, pneumonia, and COPD showed a fluctuating upward trend, which is consistent with previous findings. In 2020, the number of hospitalizations decreased notably. In early 2020, the global outbreak of coronavirus disease 2019 (COVID-19) pandemic extremely affected people's behavior in work, outdoor activities, and medical treatment. Fears of COVID-19 and tightening hospital admission standards lead to a significant reduction in hospital admissions in 2020. The LOS of discharged patients is an important indicator of hospital performance evaluation (35). In this study, LOS showed a downward trend between 2015 and 2019, which may be related to the hospital actively improving the level of diagnosis and treatment and strengthening the management of hospitalization (36). The influencing factors of hospitalization cost mainly include the LOS, the age of the patient, complications, surgery or not, and intensive care vs. no intensive care (37). In this study, LOS decreased between 2015 and 2019, whereas the hospitalization cost increased at the same time. The increase in the elderly population and the aggravation of the disease may be one of the reasons. In 2020, the LOS and the hospitalization costs increased markedly, and pneumonia exceeded all RDs and COPD, which might have resulted from the COVID-19 pandemic.
The risk estimated in this study was generally higher than those observed in previous studies, especially for PM2.5. For every 10 μg/m3 increase of PM2.5 and PM10, we estimated a 2.34% and 0.77% increase in all RD hospitalizations. A study in Nanjing city concluded that every 10 μg/m3 increase of PM2.5 and PM10 concentrations was associated with 0.36% and 0.33% increase in hospital outpatient visits for RD (38). A Chinese national-level study covered 26 cites and concluded that a 10 μg/m3 increase of PM2.5 was associated with 0.26% increase in RD hospitalization (39). However, studies in New Mexico (40) and Arkansas (41) found no association between air pollution and emergency room visit for RD. PM concentrations and compositions varied substantially over geographical regions in China (42). The difference in the composition of PM, weather conditions, age structure, and population susceptibility may be responsible for the different associations.
Meanwhile, we also found a diverse delay effect model. A study in Nanjing demonstrated the acute response of RD hospital outpatients to PM exposure (38). In this case, the highest effect of PM2.5 and PM10 appeared on the current day (lag0). In this research, PM decreased RD hospitalization on lag0, and the highest risk appeared on lag7. This study is based on hospitalization date rather than the time of symptoms onset, and the gap may explain the diverse highest risk lag pattern. Although not statistically significant, PM10 exhibited a “protective effect” on pneumonia and COPD on lag0, and decreased hospitalizations of all RDs and pneumonia. The “protective effect” may result from the conscious behavior of the study population. The proportion of 65+ year age group was 44.43% in this study. Elderly people with underlying diseases may be more cautious about air pollution. When PM concentrations increase, they may choose to reduce outdoor activities during the day, which may lead to a decrease in hospitalizations on the days of pollution and even in the first 3 days (43). In subgroup analysis, the PC of hospitalization showed a trend of increase, then decrease and increase again, especially for women and 0–14 age groups. These two groups may have lower immunity but less attention to air quality in their daily activities (44). When the PM concentration increases significantly, the exposure on the current day/lag0 has acute effects, such as asthma and pneumonia, and has the greatest impact on chronic RDs, such as COPD, after a lag of 5–7 days.
In this study, we found that the estimated risk of PM2.5 was higher than PM10 on all lag days. PM10 is different from PM2.5 in sources, composition, and lung deposition patterns. PM2.5 can reach the bronchioles and deposit in the alveoli (13). In addition, PM2.5 has a larger surface area than PM10, so it can absorb more toxic substances per unit mass (13, 45). For specific diseases, PM2.5 exposure had a higher effect on pneumonia (2.11%) than COPD (1.90%), and PM10 only had an effect on pneumonia hospitalizations (0.82%). Pneumonia is an acute inflammation of the lower respiratory tract (46). PM caused emergency room visits for pneumonia, and hospitalization increase had been confirmed in the previous study (13, 47). COPD is a chronic RD, and acute exacerbations were the main cause of medical visits and hospitalizations for COPD (48). PM can damage the airway epithelium and can weaken the immune system by oxidative stress and then cause exacerbation of COPD (49).
The subgroup analysis demonstrated that men had a higher increase in PC of hospital admissions for RD than women. A possible explanation could be that men were more inclined to smoking and drinking and that behavioral factors had synergistic effects with air environmental factors (50). A study in Taiwan (51) also indicated that men were more sensitive to PM10 exposure. Age differences also existed. In our study, 65+ year age group had the longest LOS and the highest hospitalization cost, which may result in their weakened immune function. However, the 0–14-year age group had a greater increase of RD hospitalization than the older group. Children's respiratory systems are not fully developed, and they are more sensitive to pollutants than middle-aged and elderly people. Moreover, children's outdoor activities increase their exposure to outdoor air pollutants (44). PM had greater effect on RD hospitalization increase in cold season than in warm season, which was consistent with previous studies (41, 52).
Previous studies have found that PM is a risk factor for respiratory infection by carrying microorganisms and affecting body's immunity. The association between PM and COVID-19 pandemic drew attention. PM2.5 accelerated COVID-19 spread and its lethality (53), and significantly positive associations were observed in PM with newly COVID-19 confirmed cases (54). Meanwhile, the pandemic may have a different influence on other RDs such as COPD and asthma. Lockdown had a significant impact on the environment and air quality due to reduced industrial activity and traffic, which decreased PM concentration (55). Quarantines and wearing masks reduced PM exposure (56). Taking these factors into consideration, the increase of PM concentrations still leads to an addition in hospitalizations overall, further illustrating the significant impact of PM on RDs and the need for air quality intervention.
PM causes not only RD hospitalization rise but also substantial economic loss. According to our results, PM2.5 and PM10 exposure led to 92,000 hospitalizations and 2,021.21 million CNY economic loss from 2015 to 2020 in Wuhan. From another perspective, the economic benefits of air pollution control are also considerable. An economic modeling study in Beijing concluded that an incremental monetary benefit from cardiovascular disease decline can offset over two-thirds of the air pollution-control spending if the PM2.5 concentration can be reduced to 35 μg/m3 and offsets the total spending if the PM2.5 concentration can be reduced to 15 μg/m3 (24). The same significant effect can be achieved in RDs. A value assessment study calculated that avoided economic loss for RD mortality was 103.5 million dollars when PM2.5 dropped to 10 μg/m3 in 2017, accounting for 7.31% of all-cause deaths (57). In our study, when the concentration of PM2.5 dropped to 10 μg/m3, the annual avoidable hospitalization and the annual savable economic losses were 4,580 and 100.57 million CNY, respectively, equating to a 7.71% reduction in both hospital admissions and financial losses. In the same way, when the PM10 concentration reached 20 μg/m3, the annual avoidable hospitalization and economic losses were 2,360 and 51.77 million CNY, respectively, reducing for 7.24% hospitalization and 7.23% economic loss. Therefore, air pollution control investment can produce enormous monetary benefits, but effective measures should be taken to control PM pollution.
Nevertheless, our study had several limitations. The main limitation of the present study was the unavailability of data on individual exposure to PM pollution. Using monitoring data to represent individual exposure levels may cause measuring errors and underestimate exposure. Patients' information, such as smoke and case history, was unknown, which limited the ability to identify potentially vulnerable people. On the other hand, a combined effect may exist between PM and other air pollutants. Deeper researches are necessary to explore the independent effect of PM on RD. We used hospitalization data of two hospitals to estimate the situation of Wuhan due to data unavailability, and this leads to a certain lack of representativeness in our results, so more comprehensive data are needed in future research.
Conclusions
In summary, we assessed RD hospitalization and relevant economic loss contributed to PM during 2015–2020 in Wuhan, China. We observed that PM2.5 and PM10 concentrations at different lag days were positively associated with hospitalization for all patients with RD, pneumonia, and COPD. Men and children were more vulnerable to PM. Effective air pollution control measures can reduce hospitalizations significantly and save economic loss substantially.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
CY, XW, and GQ: design of study. GQ, TW, LH, and CY: data collection, analysis, and visualization. XW, GQ, and DN: writing the original manuscript. CY, YLi, YLiu, and HW: reviewing and editing the manuscript. CY: funding acquisition. All authors read and approved the final manuscript.
Funding
This work was funded by the National Natural Science Foundation of China (Grant No. 81773552) and the National Key Research and Development Program of China (Grant No. 2018YFC1315302).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We acknowledge the Hubei Environmental Protection Bureau for providing air pollution data and the China Meteorological Data Network for providing meteorological data. We greatly thank the two hospitals for providing the hospitalization data and the Health Commission of Hubei Province (the former Health and Family Planning Commission of Hubei Province) for undertaking the organization and communication works.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.797296/full#supplementary-material
References
1. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
2. GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
3. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
4. Cadelis G, Tourres R, Molinie J. Short-term effects of the particulate pollutants contained in Saharan dust on the visits of children to the emergency department due to asthmatic conditions in Guadeloupe (French Archipelago of the Caribbean). PLoS ONE. (2014) 9:e91136. doi: 10.1371/journal.pone.0091136
5. Ishii H, Fujii T, Hogg JC, Hayashi S, Mukae H, Vincent R, et al. Contribution of IL-1 beta and TNF-alpha to the initiation of the peripheral lung response to atmospheric particulates (PM10). Am J Physiol Lung Cell Mol Physiol. (2004) 287:L176–83. doi: 10.1152/ajplung.00290.2003
6. Rahman I, Adcock IM. Oxidative stress and redox regulation of lung inflammation in COPD. Eur Respir J. (2006) 28:219–42. doi: 10.1183/09031936.06.00053805
7. Beelen R, Raaschou-Nielsen O, Stafoggia M, Andersen ZJ, Weinmayr G, Hoffmann B, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet. (2014) 383:785–95. doi: 10.1016/S0140-6736(13)62158-3
8. Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, et al. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. (2019) 381:705–15. doi: 10.1056/NEJMoa1817364
9. Santus P, Russo A, Madonini E, Allegra L, Blasi F, Centanni S, et al. How air pollution influences clinical management of respiratory diseases. A case-crossover study in Milan. Respir Res. (2012) 13:95. doi: 10.1186/1465-9921-13-95
10. Liu L, Song F, Fang J, Wei J, Ho HC, Song Y, et al. Intraday effects of ambient PM1 on emergency department visits in Guangzhou, China: a case-crossover study. Sci Total Environ. (2021) 750:142347. doi: 10.1016/j.scitotenv.2020.142347
11. Raji H, Riahi A, Borsi SH, Masoumi K, Khanjani N, AhmadiAngali K, et al. Acute effects of air pollution on hospital admissions for asthma, COPD, and bronchiectasis in Ahvaz, Iran. Int J Chron Obstruct Pulmon Dis. (2020) 15:501–14. doi: 10.2147/COPD.S231317
12. Dong J, Liu Y, Bao H. Revalue associations of short-term exposure to air pollution with respiratory hospital admissions in Lanzhou, China after the control and treatment of current pollution. Int J Hyg Environ Health. (2021) 231:113658. doi: 10.1016/j.ijheh.2020.113658
13. Tian Y, Liu H, Wu Y, Si Y, Li M, Wu Y, et al. Ambient particulate matter pollution and adult hospital admissions for pneumonia in urban China: a national time series analysis for 2014 through 2017. PLoS Med. (2019) 16:e1003010. doi: 10.1371/journal.pmed.1003010
14. Li GX, Huang J, Xu GZ, Pan XC, Qian XJ, Xu JY, et al. The short term burden of ambient fine particulate matter on chronic obstructive pulmonary disease in Ningbo, China. Environ Health. (2017) 16:54. doi: 10.1186/s12940-017-0253-1
15. Pun VC, Kazemiparkouhi F, Manjourides J, Suh HH. Long-term PM2.5 exposure and respiratory, cancer, and cardiovascular mortality in older US adults. Am J Epidemiol. (2017) 186:961–9. doi: 10.1093/aje/kwx166
16. Global Burden of Disease Cancer Collaboration. Global, regional, and national burden of respiratory tract cancers and associated risk factors from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Respir Med. (2021) 9:1030–49. doi: 10.1016/S2213-2600(21)00164-8
17. Maji KJ, Ye WF, Arora M. Nagendra SMS. PM2.5-related health and economic loss assessment for 338 Chinese cities. Environ Int. (2018) 121:392–403. doi: 10.1016/j.envint.2018.09.024
18. Hanna R, Oliva P. The effect of pollution on labor supply: Evidence from a natural experiment in Mexico City. J Public Econ. (2015) 122:68–79. doi: 10.1016/j.jpubeco.2014.10.004
19. Chang TY, Zivin JG, Gross T, Neidell M. The effect of pollution on worker productivity: evidence from call center workers in China. Am Econ J Appl Econ. (2019) 11:151–72. doi: 10.1257/app.20160436
20. Lanzi E, Dellink R, Chateau J. The sectoral and regional economic consequences of outdoor air pollution to 2060. Energy Econ. (2018) 71:89–113. doi: 10.1016/j.eneco.2018.01.014
21. Yao M, Wu G, Zhao X, Zhang J. Estimating health burden and economic loss attributable to short-term exposure to multiple air pollutants in China. Environ Res. (2020) 183:109184. doi: 10.1016/j.envres.2020.109184
22. Tang D, Wang C, Nie J, Chen R, Niu Q, Kan H, et al. Health benefits of improving air quality in Taiyuan, China. Environ Int. (2014) 73:235–42. doi: 10.1016/j.envint.2014.07.016
23. Xiao C, Chang M, Guo P, Gu M, Li Y. Analysis of air quality characteristics of Beijing-Tianjin-Hebei and its surrounding air pollution transport channel cities in China. J Environ Sci (China). (2020) 87:213–27. doi: 10.1016/j.jes.2019.05.024
24. Jiang Y, Jiang S, Ni W. Burden of cardiovascular diseases associated with fine particulate matter in Beijing, China: an economic modelling study. BMJ Glob Health. (2020) 5:e003160. doi: 10.1136/bmjgh-2020-003160
25. Zhao X, Yu X, Wang Y, Fan C. Economic evaluation of health losses from air pollution in Beijing, China. Environ Sci Pollut Res. (2016) 23:11716–28. doi: 10.1007/s11356-016-6270-8
26. Lu X, Lin C, Li Y, Yao T, Fung JCH, Lau AKH. Assessment of health burden caused by particulate matter in southern China using high-resolution satellite observation. Environ Int. (2017) 98:160–70. doi: 10.1016/j.envint.2016.11.002
27. Lu X, Yao T, Fung JCH, Lin C. Estimation of health and economic costs of air pollution over the Pearl River Delta region in China. Sci Total Environ. (2016) 566–7:134–43. doi: 10.1016/j.scitotenv.2016.05.060
28. Wuhan Bureau of Statistics. Statistical Bulletin. (2021). Available online at: http://www.stats.gov.cn/enGliSH/ (accessed May 28, 2021).
29. Yin Z, Huang X, He L, Cao S, Zhang JJ. Trends in ambient air pollution levels and PM2.5 chemical compositions in four Chinese cities from 1995 to 2017. J Thorac Dis. (2020) 12:6396–410. doi: 10.21037/jtd-19-crh-aq-004
30. Zhu B, Zhang Y, Chen N, Quan J. Assessment of air pollution aggravation during straw burning in Hubei, Central China. Int J Environ Res Public Health. (2019) 16:1446. doi: 10.3390/ijerph16081446
31. Lin Y, Zou J, Yang W, Li CQ. A review of recent advances in research on PM2.5 in China. Int J Environ Res Public Health. (2018) 15:438. doi: 10.3390/ijerph15030438
32. Cheng J, Xu Z, Zhang X, Zhao H, Hu W. Estimating cardiovascular hospitalizations and associated expenses attributable to ambient carbon monoxide in Lanzhou, China: scientific evidence for policy making. Sci Total Environ. (2019) 682:514–22. doi: 10.1016/j.scitotenv.2019.05.110
33. Wu Z, Chen X, Li G, Tian L, Wang Z, Xiong X, et al. Attributable risk and economic cost of hospital admissions for mental disorders due to PM2.5 in Beijing. Sci Total Environ. (2020) 718:137274. doi: 10.1016/j.scitotenv.2020.137274
34. Nhung NTT, Schindler C, Dien TM, Probst-Hensch N, Künzli N. Association of ambient air pollution with lengths of hospital stay for Hanoi children with acute lower-respiratory infection, 2007-2016. Environ Pollut. (2019) 247:752–62. doi: 10.1016/j.envpol.2019.01.115
35. Khalifa M. reducing length of stay by enhancing patients' discharge: a practical approach to improve hospital efficiency. Stud Health Technol Inform. (2017) 238:157–60. doi: 10.3233/978-1-61499-781-8-157
36. Shilian R, Abraham T, Wynbrandt J, Jhaveri D, Hostoffer RW, Peppers BP. Daily integrated care conferences to reduce length of hospital stay for patients with chronic obstructive pulmonary disease. J Am Osteopath Assoc. (2020) 120:144–52. doi: 10.7556/jaoa.2020.027
37. Brotons P, Gelabert G, Launes C, Sicuri E, Pallares R, Muñoz-Almagro C. Cost of hospitalizing children with invasive pneumococcal pneumonia. Vaccine. (2013) 31:1117–22. doi: 10.1016/j.vaccine.2012.12.025
38. Wang C, Feng L, Chen K. The impact of ambient particulate matter on hospital outpatient visits for respiratory and circulatory system disease in an urban Chinese population. Sci Total Environ. (2019) 666:672–9. doi: 10.1016/j.scitotenv.2019.02.256
39. Liu H, Tian Y, Xiang X, Juan J, Song J, Cao Y, et al. Ambient particulate matter concentrations and hospital admissions in 26 of China's largest cities: a case–crossover study. Epidemiology. (2018) 29:649–57. doi: 10.1097/EDE.0000000000000869
40. Rodopoulou S, Chalbot MC, Samoli E, Dubois DW, San Filippo BD, Kavouras IG. Air pollution and hospital emergency room and admissions for cardiovascular and respiratory diseases in Doña Ana County, New Mexico. Environ Res. (2014) 129:39–46. doi: 10.1016/j.envres.2013.12.006
41. Rodopoulou S, Samoli E, Chalbot MG, Kavouras IG. Air pollution and cardiovascular and respiratory emergency visits in Central Arkansas: a time-series analysis. Sci Total Environ. (2015) 536:872–9. doi: 10.1016/j.scitotenv.2015.06.056
42. Yang F, Tan J, Zhao Q, Du Z, He K, Ma Y, et al. Characteristics of PM2.5 speciation in representative megacities and across China. Atmos Chem Phys. (2011) 11:5207–19. doi: 10.5194/acp-11-5207-2011
43. Li Y, Wu J, Hao J, Dou Q, Xiang H, Liu S. Short-term impact of ambient temperature on the incidence of influenza in Wuhan, China. Environ Sci Pollut Res Int. (2021) 29:18116–25. doi: 10.21203/rs.3.rs-697121/v1
44. Bono R, Romanazzi V, Bellisario V, Tassinari R, Trucco G, Urbino A, et al. Air pollution, aeroallergens and admissions to pediatric emergency room for respiratory reasons in Turin, northwestern Italy. BMC Public Health. (2016) 16:722. doi: 10.1186/s12889-016-3376-3
45. Lippmann M, Schlesinger RB. Toxicological bases for the setting of health-related air pollution standards. Annu Rev Public Health. (2000) 21:309–33. doi: 10.1146/annurev.publhealth.21.1.309
46. Reynolds JH, McDonald G, Alton H, Gordon SB. Pneumonia in the immunocompetent patient. Br J Radiol. (2010) 83:998–1009. doi: 10.1259/bjr/31200593
47. Yee J, Cho YA, Yoo HJ, Yun H, Gwak HS. Short-term exposure to air pollution and hospital admission for pneumonia: a systematic review and meta-analysis. Environ Health. (2021) 20:6. doi: 10.1186/s12940-020-00687-7
48. Miravitlles M, Murio C, Guerrero T, Gisbert R. Pharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPD. Chest. (2002) 121:1449–55. doi: 10.1378/chest.121.5.1449
49. Li J, Sun S, Tang R, Qiu H, Huang Q, Mason TG, et al. Major air pollutants and risk of COPD exacerbations: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. (2016) 11:3079–91. doi: 10.2147/COPD.S122282
50. Wang X, Yu Y, Yu C, Shi F, Zhang Y. Associations between acute exposure to ambient air pollution and length of stay for inpatients with ischemic heart disease: a multi-city analysis in central China. Environ Sci Pollut Res. (2020) 27:43743–54. doi: 10.1007/s11356-020-10256-7
51. Yalniz E, Uslu Ö, Bolat E, Altin S, Polat G. Does the hospital admission of patients with respiratory disease increase in izmir when the PM10 level is high? Turk Thorac J. (2020) 21:32–8. doi: 10.5152/TurkThoracJ.2019.180148
52. Tsai SS, Chiu HF, Liou SH, Yang CY. Short-term effects of fine particulate air pollution on hospital admissions for respiratory diseases: a case-crossover study in a tropical city. J Toxicol Environ Health A. (2014) 77:1091–101. doi: 10.1080/15287394.2014.922388
53. Copat C, Cristaldi A, Fiore M, Grasso A, Zuccarello P, Signorelli SS, et al. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ Res. (2020) 191:110129. doi: 10.1016/j.envres.2020.110129
54. Zhu Y, Xie J, Huang F, Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci Total Environ. (2020) 727:138704. doi: 10.1016/j.scitotenv.2020.138704
55. Rodríguez-Urrego D, Rodríguez-Urrego L. Air quality during the COVID-19: PM2.5 analysis in the 50 most polluted capital cities in the world. Environ Pollut. (2020) 266(Pt 1):115042. doi: 10.1016/j.envpol.2020.115042
56. Kyung SY, Jeong SH. Particulate-matter related respiratory diseases. Tuberc Respir Dis (Seoul). (2020) 83:116–21. doi: 10.4046/trd.2019.0025
Keywords: ambient particulate matter, respiratory diseases, hospitalization, economic loss, generalized additive model
Citation: Qin G, Wang X, Wang T, Nie D, Li Y, Liu Y, Wen H, Huang L and Yu C (2022) Impact of Particulate Matter on Hospitalizations for Respiratory Diseases and Related Economic Losses in Wuhan, China. Front. Public Health 10:797296. doi: 10.3389/fpubh.2022.797296
Received: 18 October 2021; Accepted: 23 March 2022;
Published: 25 May 2022.
Edited by:
Yuewei Liu, Sun Yat-sen University, ChinaReviewed by:
Tongjian Cai, Army Medical University, ChinaHaikun Wang, Nanjing University, China
Bin Luo, Lanzhou University, China
Copyright © 2022 Qin, Wang, Wang, Nie, Li, Liu, Wen, Huang and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuanhua Yu, eXVjaHVhQHdodS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Guiyu Qin
Guiyu Qin Xuyan Wang2†
Xuyan Wang2† Haoyu Wen
Haoyu Wen Chuanhua Yu
Chuanhua Yu