- 1CATALYST—The Center for the Advancement of Team Science, Analytics, and Systems Thinking, College of Medicine, The Ohio State University Institute for Behavioral Medicine Research, Columbus, OH, United States
- 2Department of Biomedical Informatics, College of Medicine, The Ohio State University Institute for Behavioral Medicine Research, Columbus, OH, United States
- 3Department of Family Medicine, College of Medicine, The Ohio State University Institute for Behavioral Medicine Research, Columbus, OH, United States
- 4Department of Research Information Technology, College of Medicine, The Ohio State University, Columbus, OH, United States
- 5Ohio Colleges of Medicine Government Resource Center, The Ohio State University, Columbus, OH, United States
Objective: To describe the development of an area-level measure of children's opportunity, the Ohio Children's Opportunity Index (OCOI).
Data Sources/Study Setting: Secondary data were collected from US census based-American Community Survey (ACS), US Environmental Protection Agency, US Housing and Urban Development, Ohio Vital Statistics, US Department of Agriculture-Economic Research Service, Ohio State University Center for Urban and Regional Analysis, Ohio Incident Based Reporting System, IPUMS National Historical Geographic Information System, and Ohio Department of Medicaid. Data were aggregated to census tracts across two time periods.
Study Design: OCOI domains were selected based on existing literature, which included family stability, infant health, children's health, access, education, housing, environment, and criminal justice domains. The composite index was developed using an equal weighting approach. Validation analyses were conducted between OCOI and health and race-related outcomes, and a national index.
Principal Findings: Composite OCOI scores ranged from 0–100 with an average value of 74.82 (SD, 17.00). Census tracts in the major metropolitan cities across Ohio represented 76% of the total census tracts in the least advantaged OCOI septile. OCOI served as a significant predictor of health and race-related outcomes. Specifically, the average life expectancy at birth of children born in the most advantaged septile was approximately 9 years more than those born in least advantaged septile. Increases in OCOI were associated with decreases in proportion of Black (48 points lower in the most advantaged vs. least advantaged septile), p < 0.001) and Minority populations (54 points lower in most advantaged vs. least advantaged septile, p < 0.001). We found R-squared values > 0.50 between the OCOI and the national Child Opportunity Index scores. Temporally, OCOI decreased by 1% between the two study periods, explained mainly by decreases in the children health, accessibility and environmental domains.
Conclusion: As the first opportunity index developed for children in Ohio, the OCOI is a valuable resource for policy reform, especially related to health disparities and health equity. Health care providers will be able to use it to obtain holistic views on their patients and implement interventions that can tackle barriers to childhood development using a more tailored approach.
Introduction
Unmet basic needs are likely to result in poor health outcomes across the lifespan (1, 2) making children living in poverty extremely vulnerable. Approximately 2.6 million of Ohio's 11.5 million population are children. About 20% of these children in Ohio live in poverty, 16% are chronically absent from school, and 14–15% have a disability. Further, over 20,000 children in Ohio are homeless (3). Those who are most disadvantaged, while shouldering a disproportionately higher burden of poor health and risk factors for poor health, are also the least likely to access care when needed (4). Risk factors tend to cluster within individuals, families, and communities, worsening the inverse relationship between the need for healthcare and access to it (5). This phenomenon is apparent, for example, among vulnerable populations who have higher utilization of out-of-hours emergency health care rather than preventive health care, perpetuating the cycle of expensive, reactive care (6).
The high infant mortality in Ohio (7), especially the wide disparity between infants born to White vs. Black mothers prompted the Ohio Department of Medicaid (ODM) to develop the Ohio Opportunity Index (OOI) (8) and the Ohio Children's Opportunity Index (OCOI) through the Infant Mortality Research Partnership and as a general movement to monitor deprivation among individuals from childhood and onwards. The objective was to aid the identification of deprived areas for targeted allocation of resources to improve health care delivery and health services, which has been shown to decrease disparities (9). Area-level indices of deprivation have been used in New Zealand and the United Kingdom not simply to study risk factors and outcomes but also for incorporation into healthcare delivery (10).
Individual factors only partially capture determinants of health and disease, drawing attention to the “place” effect (11, 12)—the social, economic, and physical conditions in the environment where people live, also called social determinants of health (SDoH) (13). Several studies have formally decomposed the contributors of health outcomes into clinical care, health behaviors, socio-economic factors and physical environment (14–17). Characterizing the individual effect of any of these factors, particularly socioeconomic and environmental conditions that contribute between 20 and 50 percent to health outcomes, do not provide adequate guidance on how interventions or policies can be developed with greater precision for target populations (16, 18). Hence, there is a need for nuance about modifiable attributes within a domain that can truly influence health outcomes.
The influence of SDoH vary based on the ecological level at which they operate. Poverty places a greater health burden on society than either of the leading behavioral risk factors—smoking or obesity (19). Individual poverty combined with living in an affluent neighborhood was not associated with negative health consequences, whereas living in a deprived neighborhood was associated with adverse health outcomes more so among poorer individuals, who may be more dependent on collective neighborhood resources (20). Deprivation is “a state of observable and demonstrable disadvantage relative to the local community or the wider society or nation,” and poverty on the other hand is the lack of resources to escape deprivation (21). Many indices have been created to show deprivation or opportunity, including the Human Opportunity Index, but many of these operate at a country or state level without comparing inequality on a more granular level (22–24). An area-level deprivation index (ADI) reflects aggregate measures of SDoH at the neighborhood level.
Advances in computing power, geographic information systems (GIS), and statistical techniques like multi-level modeling allow for more sophisticated and detailed examination of area level SDoH than in the past (25). The Public Health Disparities Geocoding Project assessed a variety of single indicators and composite measures of socioeconomic deprivation and demonstrated gradients with outcomes like childhood lead poisoning, mortality, and low birth weight (26, 27). Moreover, Krieger and colleagues demonstrated that indices of area level deprivation facilitated detection of larger socioeconomic gradients than more focused area level measures of education and wealth. Linking the area deprivation index with county-level mortality revealed widening inequalities in area level mortality on account of slower declines in mortality in deprived areas (28). These are but a few examples of the wealth of research suggesting that place matters.
Neighborhoods possess physical and social attributes that could affect health (25). Empirical research examining neighborhood effects on children and adolescents have established that there is considerable socioeconomic and racial segregation and that indicators like crime, social, and physical disorder tend to cluster at the neighborhood level (29). Predictors common to many childhood outcomes include concentrated poverty and racial isolation (29). Neighborhood disadvantage has been shown to be associated with child health outcomes such as behavioral problems and verbal ability (30, 31). The influence of neighborhood can be recognized through the Moving to Opportunity Experiment. Moving to a more affluent neighborhood when children are younger than 13 was argued to have to an increase in college attendance and earnings (32). The seminal Whitehall studies have highlighted the social gradient or the socioeconomic differences in physical and mental illnesses and mortality (9).
The OCOI is a measure of SDoH at the census tract level conveying opportunity information for children across the state of Ohio. We define children as anyone between birth and below the age of 18. As a neighborhood's effect on children's health is not exerted by a single factor but by a combination of them, the OCOI is a composite index of 53 neighborhood indicators spanning eight domains associated with healthy child development. The OCOI is not the first index associated with healthy childhood. The similarly-named Child Opportunity Index consists of 29 indicators corresponding to three domains: educational, health and environment, and social and economic. The Child Opportunity Index is available for all US census tracts for both 2010 and 2015 (33). Our measure, however, consists of more, higher resolution variables measuring the prevalence of SDoH factors within the state.
In this article we describe the development of the OCOI. The purpose of the OCOI is to provide a measure of children's opportunity in Ohio. Public health practitioners, policymakers, researchers, and healthcare providers can use the OCOI to identify neighborhoods of low and high opportunity in Ohio. In this article we first discuss the process of domain and input data selection followed by data extraction. Next, we discuss the four-step process involved in the construction of the OCOI based on seminal approaches and their analysis across two time periods (34, 35). Finally, we report the association of the OCOI with life expectancy and proportions of minority populations to validate the index and report changes in children's opportunity in Ohio with time as explained by changes in the domain scores. The goal of our paper is to present an approach to developing an area deprivation index of higher resolution compared to what currently exists, and provide researchers and other key stakeholders the opportunity to pursue a similar approach regarding the development and validation of an area deprivation index for children.
Data and Methods
Measures of social determinants of children's health and well-being were collected at the census tract level for Ohio. Census tracts are geographical sub-divisions of counties that contain an average of 4,000 people (3). Because of similar neighborhood characteristics, federal and state agencies often collect tract level aggregates as a proxy for area-based information. Study data pertain to 2,940 tracts out of the total 2,952 census tracts in Ohio. Twelve tracts were excluded because of zero population. Data were procured from federal sources such as the US census based-American Community Survey (ACS) data set, which is a freely available resource, and other state and federal agency administrative data sets (e.g., Medicaid claims and Department of Education school report card data). The Government Resource Center at the Ohio State University compiled the measures used for the construction of the OCOI. Information was gathered to represent two time periods, 2010–2014 (Period I) and 2013–2017 (Period II), inclusive.
Domains and Variables
Deprivation indices are either represented by simple indicators measuring social deprivation alone, such as poverty (36), or as a composite score articulated from multiple mutually exclusive indicators or “domains” (35). Using the framework developed by Peter Townsend and Exeter (21, 37), the current study adopted a multi-dimensional and a multi-domain approach. The domains refer to a collection of constituent measures pertaining to economic, material, and psychosocial influences in humans. Additional details about these measures and associated attributes can be found in a study conducted by Pearce and colleagues (38). Guided by Townsend's framework (35), the subject matter experts (maternal-child health and geospatial area deprivation measure development) and the study team identified a list of eight domains: family stability, infant health, children's health, access (to health care and food), education, housing, environment, and criminal justice for OCOI construction. The study domains mostly overlap with the SDoH factors identified by the Center for Disease Control and Prevention (CDC) (life-enhancing resources such as food supply, housing, transportation, education, and health care) further substantiating their use (39). A brief description of the domains are as follows (40, 41):
(1) Family Stability: Measures early influences of family settings on children including family breakdown, parental relationship, and family income.
(2) Infant Health: Determinants of children's health that operate from before conception through birth. Maternal influences such as mother's health, lifestyle, and social and physical environments have immediate effect on children's health.
(3) Children's Health: Presence of chronic conditions in children that may affect their overall development.
(4) Access: Poor geographical access to key local services.
(5) Education: Scholastic attainment and skills in local population that may lead to low health literacy.
(6) Housing: Barriers to affordability of housing and stable housing conditions.
(7) Environment: Physical space and characteristics, both natural and built, that influence health.
(8) Criminal Justice: Likelihood for personal and material victimization at the local level.
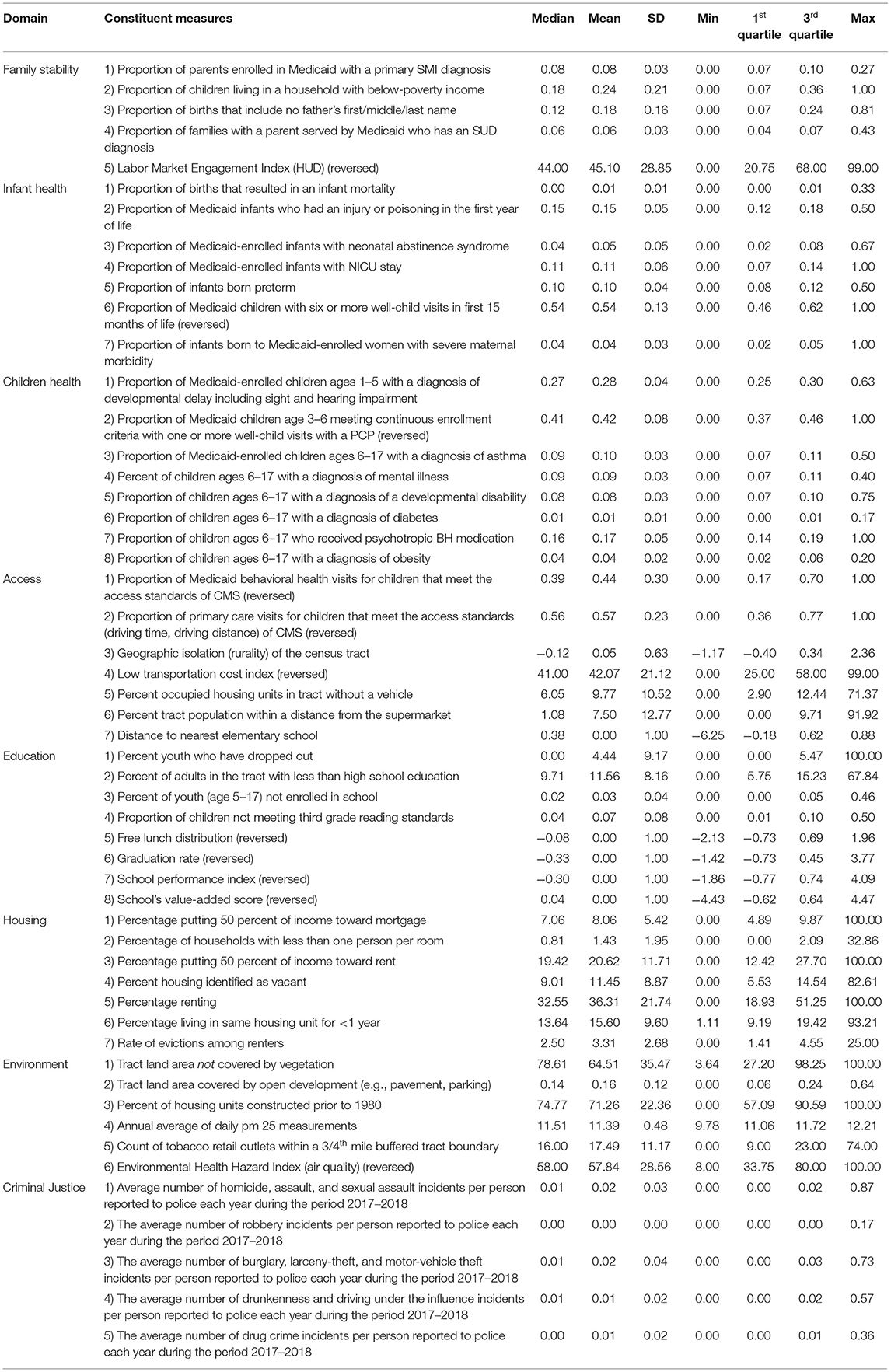
The number of constituent measures used in the study differed across the two-time frames due to their availability. Information was available for 37 constituent measures in Period I, and 53 constituent measures in Period II (including those from Period I). For comparison purposes, Period II was divided into two subsets: reduced and complete. The Period II reduced subset comprised of the 37 measures common to Period I, while the Period II complete subset included all the 53 constituent measures. We used the Period II complete dataset as an example for outlining the OCOI construction methodology in this paper and the same process was used to construct scores for the remaining datasets. The constituent measures in this along with their corresponding data sources are listed in Supplementary Table S1. These measures were summarized (within respective domains) to yield domain scores, which were further summarized to form the final OCOI. Figure 1 represents an outline of the process used to create the OCOI.
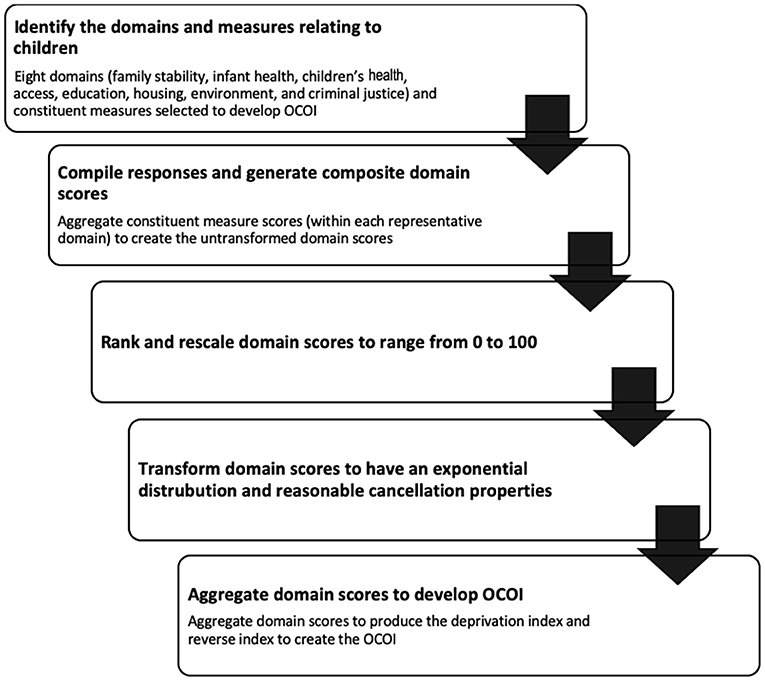
Figure 1. Flowchart representing steps involved in developing the Ohio children's opportunity index.
Of the 53 constituent measures, five were assigned to the family stability domain, seven to infant health, eight to children's health, seven to access, eight to education, seven to housing, six to environment, and five to the criminal justice domain. Some constituent measures were reverse coded to maintain a consistent direction with respect to what higher (opportunity) vs. lower (opportunity) values mean.
Validation Outcomes
The study-generated OCOI scores were tested for association with outcomes previously linked to area-level deprivation for construct validity (42). Probability of life expectancy was used as a health outcome criterion for prediction based on OCOI. Life expectancy represents the expected average years of survival at birth. Data for this outcome was collected at the census tract level from 2010–2015 and retrieved from National Center for Health Statistics, CDC (43). Variability in racial distribution in the population, for Black and minority groups were examined. Information regarding the percent of Black and minority population living within a tract were obtained from ACS (44). We assessed criterion validity by comparing the Period II complete OCOI and the national Child Opportunity Index scores (33).
Analysis
Statistical analyses were performed using R version 4.0.3. Raw data were obtained for measures across the 2,940 census tracts in Ohio. A multi-stage approach was adopted to generate the OCOI. First, univariate and bivariate analyses were conducted to explore the statistical distribution of variables, their missingness, and their relationship with other variables. Missing values were replaced with median values of the corresponding measure. Also, at this stage, we performed correlational analysis on the constituent measures to assess the grouping of the 53 variables (see Supplementary Figure S1 for the correlation matrix). The next steps included a series of transformations to create a composite measure from raw scores. Following Townsend (35) and Noble's (34) work, the OCOI was computed based on the following procedures:
(1) Standardizing and averaging:
Data were collected across 53 measures in different units such as proportions and counts. The first step in the analysis was to standardize these raw scores such that they have a mean of 0 and a standard deviation of 1 (i.e., z-scores) as illustrated in Equation 1, wherein Z is the standardized score, x is a value, μ and σ are the mean and standard deviation of a specific measure i within domain d:
The standardized scores were then averaged (within domains) to form domain scores, for example, Z is the standardized scores for measures i = 1 to n for the first domain and N is the total number of measures in the first domain, D1.
The scores are subsequently transformed in the following manner (37).
(2) Ranking:
The domain scores are ranked and scaled to range between zero and one, wherein R is the rank of census tract ct, d=domains between 1 and 8.
(3) Exponential distribution:
The scaled rankings were then transformed to have an exponential distribution. According to Noble et al. (34) this helps each domain to have a common distribution, the same range, and identical maximum and minimum values of 0 and 100 respectively. The exponential distribution stretches out the distribution so that greater levels of deprivation score more highly. The transformed domain was given by Noble et al. (34) Equation 4, wherein X is the transformed domain value, δ is a constant and R is the rank on the domain for census tract ct and d = domains between 1 and 8.
(4) Equal weighting:
These transformed final domain scores were then aggregated using a weighing technique. For this study we used the equal weighting method, wherein each domain was assigned a weight of 1/8 and aggregated to form the deprivation index. The equal weighting method is a seminal approach used by many European countries for calculating area-level deprivation scores (45). By doing so, we assume equal importance of all deprivation domains. This technique is known to produce valid area-level measures and significantly predict health outcomes such as mortality (45). The resultant tract-level scores represented deprivation index for Ohio and were reversed and scaled between 0 and 100 to create the OCOI for each census tract. Septiles were computed from the tract-level score to simplify interpretation.
(5) Validation and sensitivity analysis:
We used the same regression-based validation approach as previous studies to predict health-related outcomes (45). OCOI score categories (i.e., septiles) were used to predict life expectancy. The distribution of minority and Black population against OCOI categories were also examined using ordinary least squares (OLS) regression model specifications. R-squared values were calculated between the OCOI scores and the state normed and national normed Child Opportunity Index scores. Equation 6 represents an example regression with Outcome that is a vector for a validation measure such as life expectancy for census tract ct and β is a vector jth regression intercept and slope for each Domain (d = 1...8) of the COI.
Readers can refer to our github page: https://github.com/ChildrensOpportunityIndex/The-Ohio-Opportunity-Index-Project, which provides detailed information on the construction and applications of the OCOI and can aid with replication in future studies. The OCOI and domain scores data linked to census tract FIPS codes can be obtained at the main project page: https://grc.osu.edu/Projects/OhioOpportunityIndex.
OCOI Results
Univariate Descriptive Statistics
Table 1 presents descriptive statistics for the 53 constituent measures using aggregated data from 2013–2017. Out of 53 measures, responses for eleven measures were reversed to maintain a consistent direction: labor market engagement index, proportion of children with six or more well child primary care provider visits, proportion of children between ages three and six with one or more well-child primary care provider visits, low transportation cost index, behavioral health visits for children that meet access standards, proportion of primary care visits for children that meet the access standards of CMS, free lunch distribution, graduation rate, school performance index, schools value-added score, and environmental health hazard index.
OCOI Scores
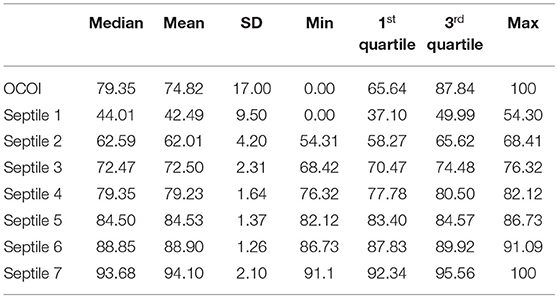
Graphical distribution and descriptive statistics for the study-generated OCOI scores are reported in Supplementary Figure S2 and Table 2 respectively. As shown by the histogram, the distribution of OCOI scores displayed a negative skew, indicating higher opportunities for children in Ohio for most tracts compared to normally distributed outcomes. The average OCOI score was 74.82 (SD, 17.00).
Figure 2 presents a choropleth map of the OCOI across the state census tracts. Census tracts in the metropolitan cities of Cleveland, Columbus, Cincinnati, Toledo, and Dayton contained 29.28, 15.47, 13.33, 9.4, and 8.09% (together a total of 75.7%) of the total census tracts in the lowest OCOI septile (Q1), respectively.
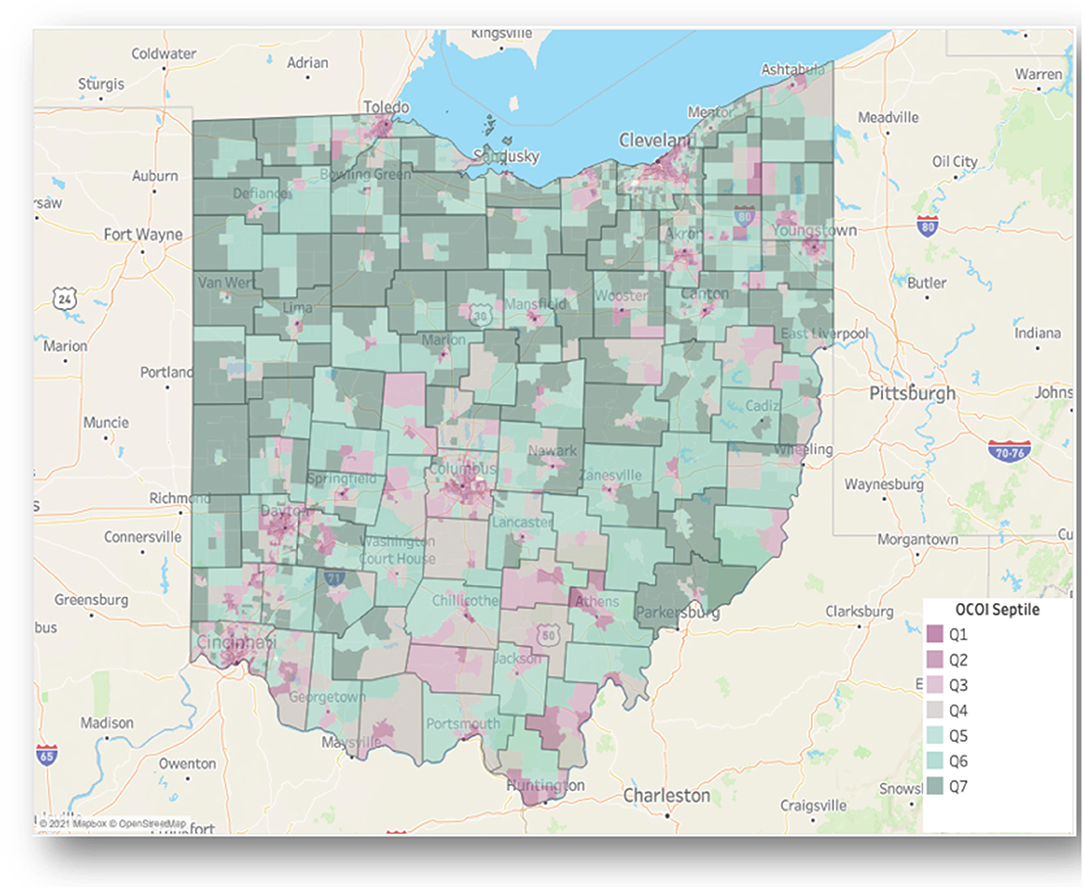
Figure 2. Ohio children's opportunity index scores on a choropleth map of Ohio. Ohio Children's Opportunity Index (OCOI) distribution (as septiles of scores) displayed across tracts and counties. Q1 represents least advantaged census tracts.
Figure 3 Illustrates patterns in OCOI scores within a single neighborhood in Columbus, Ohio. Upper Arlington anecdotally represents a neighborhood of high opportunity and living standards. There are 46% of tracts in Upper Arlington in the top three OCOI septiles, albeit 26% of the tracts in this neighborhood are in the bottom three septiles. The tracts with low OCOI scores in this neighborhood reflect a contrast to the immediately adjacent tracts in regard to domains such as children's health and family stability.
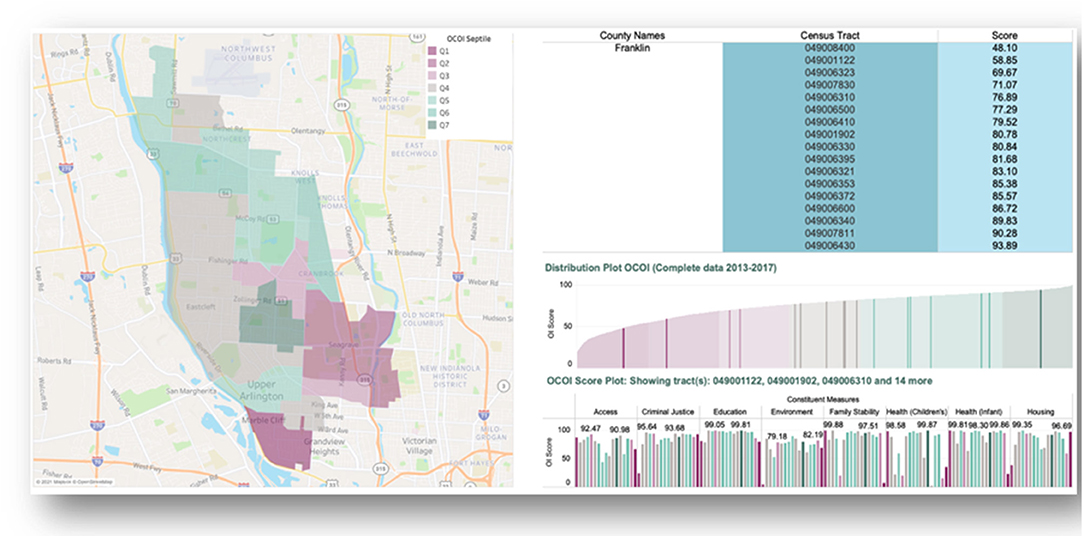
Figure 3. Illustrating distribution of Ohio children's opportunity index scores using a neighborhood view. Ohio Children's Opportunity Index (OCOI) distribution (as septiles of scores) and sub-domain scores displayed across tracts for one neighborhood in Columbus, Ohio. Q1 represents least advantaged census tracts.
Validation Results
We tested the construct validity of our OCOI measure using regression analysis wherein OCOI scores (collapsed to septiles, with the lowest used as the reference) were used as predictors for reference measures: health-related outcomes and neighborhood proportion of minority populations. OCOI scores were a significant predictor of each reference measure (p < 0.001). The average life expectancy of children born in septile 7 was approximately 9 years more than those born in septile 1. The variability in Black and Minority population on OCOI scores was also examined based on OCOI septiles. The percentage of Black population living in septile 7 was 48 points lesser than those in septile 1. Likewise, the percentage of Minority population living in septile 7 was 54 points lesser than septile 1. From our test of trends, we found that trends were present in our outcomes across the ordered levels or septiles of OCOI (p < 0.001). See Supplementary Table S2 for estimates from the validation analyses. In regard to criterion validity, the R-squared between the OCOI and Child Opportunity Index scores were 0.52 (state normed Child Opportunity Index) and 0.55 (nationally normed Child Opportunity Index). This demonstrates that our measure captures something very similar to those national indices. Differences are likely due to the finer grain of information we have available specific to Ohio.
Temporal Changes
Using the proposed steps, we developed OCOI scores for reduced datasets across Periods I and II, and compared them for temporal changes. The average OCOI reduced from 73.89 to 72.96 from Period I to Period II, which is a reduction by approximately 1%. We found, at the area level, notable declines (>10 points in COI score) across both rural and urban tracts and notable gains (>10 points in COI score) among urban tracts between the two time periods. We also investigated change in domains scores across the two-time periods. Our results, as indicated in Supplementary Table S3, indicate a noteworthy decline (>3% points) in the children's health and environment domains. Alternatively, improvements were present for domains representing housing stability, with the highest increase of 9% points over time, followed by family stability, education, criminal justice, and infant health.
Discussion
The OCOI was created to codify the geographic distribution of SDoH in the state of Ohio, particularly those that are likely to impact infants and children. The final OCOI was made up of eight domains comprising 53 variables that vary geographically. Analysis of the OCOI by census tract also shows that it captures variations by census tract that may be missed at coarser geographies. We found that increases in the OCOI scores were associated with higher tract-average life expectancy and minority population proportion.
The OCOI was inspired by the Ohio Opportunity Index (OOI), a related index that describes general deprivation of geographic areas in Ohio and consists of a different set of variables and domains. The researchers and stakeholders who developed the OOI realized that there were factors affecting children's health and development that do not affect adults in the same way, along with factors in the OOI that do not influence children as much, motivating the development of a more specific index for children. The OCOI domains of family stability, environment, infant health, and children's health are not in the OOI, but are important predictors of children's health because they are associated with adolescent and adult health, social, and educational development (46–50). There is significant evidence that children living in more deprived areas are more likely to experience poor social, behavioral, health, and economic outcomes not only in childhood but throughout life, highlighting the importance of a children's index (51–54). Moreover, both indices are based on data that contains information specific to Ohio and its population.
There is conflicting evidence regarding the extent to which children's outcomes are affected by poverty on the family level vs. the neighborhood level. Some research shows children in poor families may experience worse outcomes, a form of “double disadvantage,” when they live and attend school alongside more affluent vs. similarly positioned peers as opposed to those who live near peers in similar levels of poverty (55). Other research, including data from the Moving to Opportunity (MTO) Study, provides conflicting evidence that growing up in better quality neighborhoods can improve the adult earnings of low-income children that move out of more deprived areas (32). The OCOI shows that many of the census tracts with the lowest opportunity are in urban areas, where children may be very close to tracts with extremely different OCOI scores, which could negatively affect their subjective social status (55). In addition, there are some possible negative effects of moving children from a low opportunity area to a high opportunity area other than their comparatively low social status, including low academic achievement (56) and antisocial behavior (57). Efforts to improve OCOI scores should focus on providing resources and helping areas with the most deprivation to increase equality of opportunity, rather than moving children out of low opportunity areas at the expense of the children who remain in them.
This is the first children's opportunity index developed for the state of Ohio, however, there are similar efforts to map children's deprivation or opportunity in other parts of the United States. There is a national Children's Opportunity Index that uses data for all US neighborhoods and provides data for the overall Index, three domains, and individual component indicators (58). The Opportunity Atlas is a national index that shows the likelihood of a child in different census tracts experiencing certain economic and educational outcomes as an adult. This contrasts with the OCOI because it focuses more on economic outcomes including income, employment, graduation rates, and other individual variables rather than health. Additionally, the Opportunity Atlas focuses on the likelihood of adult outcomes but not problems that may affect the children living in those areas in the present, such as crime or family stability, which could influence stress and other mediators of those later outcomes. Other countries or groups of countries including South Africa (59) and the European Union (60) have also created deprivation or opportunity indices for children, and some states in the United States have limited indices studying childhood poverty alone (61, 62), but no sources were found for multidimensional child deprivation indices on a state or regional level.
When looking at changes in neighborhood indices, it is imperative to examine the performance of contributing domains/facets for completeness and accuracy. As indicated in our results, while the reported reduction in the overall OCOI with time was approximately 1% point, the increase in housing stability by 9% points provides a more nuanced picture in to the gains achieved for child development between our study periods. Likewise, declines in other domains such as children's health and environment indicate that opportunities for improvement in these domains exist. Recognizing these changes at the small area level provided increases clarity in to specific patterns in the improvement in child development. Studying child deprivation at this level offers state and local government agencies the ability to allocate funding for specific interventions on a local level. Moreover, the availability of domain specific information further helps to pin point specific areas for the judicious use of financial and other resources.
The OCOI showed a significant relationship between percentage of minorities in a census tract and overall scores, with higher minority populations associated with lower scores. This is similar to results from the National Opportunity Index, with their index showing across 100 metro regions Child Opportunity Scores for White children (score = 73) that were higher than for Black (score = 24) or Hispanic (score = 33) children (58). There is a complex relationship between race, geography, and deprivation in the United States due to segregation, discrimination, White flight, redlining, and institutional racism (63). The poverty rates for Black and Hispanic children are more than double that of White children in the United States (64, 65). The compounding of low family wealth and living in deprived regions make it even less likely for minority children to escape poverty. It was found that upward mobility, defined by a child in the lowest income quintile reaching the highest as an adult, was greatest for areas with less segregation, less income inequality, better schools, greater social capital, and more family stability (66). Investing in the most deprived areas by improving education and decreasing income inequality may help alleviate some of the effects that are continuing to disproportionately hurt minority neighborhoods (51).
The OCOI has potential for improvements that may further enhance its ability to communicate deprivation information. We are working on visual tools and dashboards that describe and map OCOI and the individual domains. These visual tools could incorporate race and ethnicity information to show the compounding of race and deprivation (67). These tools will allow researchers, public health, and government initiatives map areas to target for interventions, and learn more specifically which resources may be most needed in low opportunity areas. Additional years of data are being added as they become available, and will assist researchers in seeing changes in trends over time. Linking this change data with outcome data will enable researchers to study whether public programs and initiatives affected change in deprived areas and further inform decisions regarding specific resources needed.
Limitations
The OCOI has limitations that could affect its scope and intended use. There is individual variation in deprivation within census tracts, and these measures should not be used alone to infer an individual's risks. The use of varied data sources may limit the frequency of data updates, and some variables may update at different rates than others. We currently plan to update the OCOI measures on a biennial basis to account for this discrepancy. The lengthy reference time period of 2013–2017 averages over rapidly changing conditions. Therefore, the OCOI is most useful when the need is to understand longer-term health-relevant patterns in area-level social determinants (68). Those using deprivation measures should remain cautious when interpreting what “low opportunity” means and make efforts to not promote negative characterizations of neighborhoods that need help. The intention is to help reduce inequity. However, if resources are allocated improperly, tools like the OCOI could even further divide communities. For example, if the OCOI is used by businesses or housing developers to find higher opportunity areas and avoid lower opportunity areas, they may continue investing in and improving places that do not need help. Policymakers should use these tools to specifically target areas and outcomes that need the most help, and also be careful to not waste resources on interventions that are unnecessary based on the data.
Conclusion
Health is multifaceted and influenced by a constellation of physical, environmental, social, and economic factors that in turn interact with individual characteristics. Generally, individuals residing in more deprived areas suffer worse health outcomes. Children born and raised in more deprived neighborhoods may have more health, social, behavioral, and economic problems as adolescents and adults (51–54), and are less likely to escape their low economic positions than children with similar family socioeconomic status living in more affluent areas (69). Moreover, the factors affecting the health of adults and children differ somewhat, highlighting the importance of deprivation (or opportunity, conversely) measures targeted specifically for younger populations. Therefore, measuring age-appropriate area-level conditions is an important contribution to identifying and addressing health disparities. Collaboration between health and social services in lower opportunity areas could be encouraged to address the many needs, and the OCOI would be useful for geographically targeting those efforts to optimize the health returns from investments.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: Some of the data used for this study was provisioned by the Ohio Department of Medicaid. Requests to access these datasets should be directed to https://medicaid.ohio.gov/wps/portal/gov/medicaid/.
Author Contributions
NF, PS, PJ, CS, CO, and ND contributed to the conceptualization, analysis, and writing of this manuscript. All authors contributed to the article and approved the submitted version.
Funding
The project is sponsored by the Ohio Department of Medicaid and funded in part by the Ohio Medicaid Technical Assistance and Policy Program.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.734105/full#supplementary-material
References
1. Aber JL, Bennett NG, Conley DC, Li J. The effects of poverty on child health and development. Annu Rev Public Health. (1997) 18:463–83. doi: 10.1146/annurev.publhealth.18.1.463
2. Larson K, Halfon N. Family income gradients in the health and health care access of US children. Matern Child Health J. (2010) 14:332–42. doi: 10.1007/s10995-009-0477-y
3. U.S. Census Bureau. Population Estimates. The Census Bureau's Population Estimates Program (2017).
5. Fiscella K, Shin P. The inverse care law: implications for healthcare of vulnerable populations. J Ambul Care Manage. (2005) 28:304–12. doi: 10.1097/00004479-200510000-00005
6. Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. (2006) 6:35. doi: 10.1186/1471-2288-6-35
7. Ely DM, Driscoll AK. Infant mortality in the united states, 2018: data from the period linked birth/infant death file. Natl Vital Stat Rep. (2020) 69:1–18. doi: 10.15620/cdc:111053
8. Fareed N, Swoboda CM, Jonnalagadda P, Griesenbrock T, Gureddygari HR, Aldrich A. Visualizing opportunity index data using a dashboard application: a tool to communicate infant mortality-based area deprivation index information. Appl Clin Inform. (2020) 11:515–27. doi: 10.1055/s-0040-1714249
9. Marmot MG. Status syndrome: a challenge to medicine. JAMA. (2006) 295:1304–7. doi: 10.1001/jama.295.11.1304
10. Phillips RL, Liaw W, Crampton P, Exeter DJ, Bazemore A, Vickery KD, et al. How other countries use deprivation indices-and why the United States desperately needs one. Health Aff . (2016) 35:1991–8. doi: 10.1377/hlthaff.2016.0709
11. Blakely TA, Woodward AJ. Ecological effects in multi-level studies. J Epidemiol Community Health. (2000) 54:367–74. doi: 10.1136/jech.54.5.367
12. Diez-Roux AV. Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am J Public Health. (1998) 88:216–22. doi: 10.2105/AJPH.88.2.216
13. Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S, Commission Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. (2008) 372:1661–9. doi: 10.1016/S0140-6736(08)61690-6
14. McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff. (2002) 21:78–93. doi: 10.1377/hlthaff.21.2.78
15. Booske BC, Athens JK, Kindig DA, Park H, Remington PL. Different Perspectives for Assigning Weights to Determinants of Health. Madison, WI: University of Wisconsin: Population Health Institute (2010).
16. Hood CM, Gennuso KP, Swain GR, Catlin BB. County health rankings: relationships between determinant factors and health outcomes. Am J Prev Med. (2016) 50:129–35. doi: 10.1016/j.amepre.2015.08.024
17. Park KH, Kim D, Kim SK, Yi YH, Jeong JH, Chae J, et al. The relationships between empathy, stress and social support among medical students. Int J Med Educ. (2015) 6:103–8. doi: 10.5116/ijme.0
18. Frakt AB, Jha AK, Glied S. Pivoting from decomposing correlates to developing solutions: an evidence-based agenda to address drivers of health. Health Serv Res. (2020) 55:781–6. doi: 10.1111/1475-6773.13539
19. Muennig P, Fiscella K, Tancredi D, Franks P. The relative health burden of selected social and behavioral risk factors in the United States: implications for policy. Am J Public Health. (2010) 100:1758–64. doi: 10.2105/AJPH.2009.165019
20. Stafford M, Marmot M. Neighbourhood deprivation and health: does it affect us all equally? Int J Epidemiol. (2003) 32:357–66. doi: 10.1093/ije/dyg084
22. Molinas JR, De Barros RP, Saavedra J, Giugale M. Do our Children Have a Chance? The 2010 Human Opportunity Report for Latin America and the Caribbean. World Bank (2010).
23. Islam TM, Mitra S. Multidimensional human opportunity index. Social Indicators Research. (2017) 130:523–35. doi: 10.1007/s11205-015-1202-4
24. Newman J. Human Opportunity Index-National: Equality of Children's Opportunities in Pakistan. The World Bank (2012).
25. Diez Roux AV. Neighborhoods and health: where are we and were do we go from here? Rev Epidemiol Sante Publique. (2007) 55:13–21. doi: 10.1016/j.respe.2006.12.003
26. Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US). J Epidemiol Community Health. (2003) 57:186–99. doi: 10.1136/jech.57.3.186
27. Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the public health disparities geocoding project. Am J Epidemiol. (2002) 156:471–82. doi: 10.1093/aje/kwf068
28. Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. (2003) 93:1137–43. doi: 10.2105/AJPH.93.7.1137
29. Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects”: social processes and new directions in research. Annu Rev Sociol. (2002) 28:443–78. doi: 10.1146/annurev.soc.28.110601.141114
30. Caughy MO, Nettles SM, O'Campo PJ. The effect of residential neighborhood on child behavior problems in first grade. Am J Community Psychol. (2008) 42:39–50. doi: 10.1007/s10464-008-9185-9
31. Sampson RJ, Sharkey P, Raudenbush SW. Durable effects of concentrated disadvantage on verbal ability among African-American children. Proc Natl Acad Sci USA. (2008) 105:845–52. doi: 10.1073/pnas.0710189104
32. Chetty R, Hendren N, Katz LF. The effects of exposure to better neighborhoods on children: new evidence from the moving to opportunity experiment. Am Econ Rev. (2016) 106:855–902. doi: 10.1257/aer.20150572
33. Acevedo-Garcia D, McArdle N, Hardy EF, Crisan UI, Romano B, Norris D, et al. The child opportunity index: improving collaboration between community development and public health. Health Aff. (2014) 33:1948–57. doi: 10.1377/hlthaff.2014.0679
34. Noble M, Wright G, Smith G, Dibben C. Measuring multiple deprivation at the small-area level. Environ Plann A. (2006) 38:169–85. doi: 10.1068/a37168
35. Townsend P, Phillimore P, Beattie A. Health and Deprivation : Inequality and the North. London: Croom Helm. (1988).
36. Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. (2013) 48:539–59. doi: 10.1111/j.1475-6773.2012.01449.x
37. Exeter DJ, Zhao J, Crengle S, Lee A, Browne M. The New Zealand Indices of Multiple Deprivation (IMD): a new suite of indicators for social and health research in Aotearoa, New Zealand. PLoS ONE. (2017) 12:e0181260. doi: 10.1371/journal.pone.0181260
38. Pearce A, Dundas R, Whitehead M, Taylor-Robinson D. Pathways to inequalities in child health. Arch Dis Child. (2019) 104:998–1003. doi: 10.1136/archdischild-2018-314808
39. Ramirez LB, Baker EA, Metzler M. Promoting Health Equity; A Resource to Help Communities Address Social Determinants of Health. CDC (2008).
40. Institute of Medicine (US) committee on using performance monitoring to improve community health. In: Durch JS, Bailey LA, Stoto MA, editors. Improving Health in the Community: A Role for Performance Monitoring. Washington (DC): National Academic Press (US) (1997).
41. The The Area Based Analysis Unit Office for National Statistics 1. Understanding patterns of deprivation. Reg Trends. (2009) 41:93–114. doi: 10.1057/rt.2009.7
42. Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. (2014) 129:19–31. doi: 10.1177/00333549141291S206
43. Arias E, Escobedo LA, Kennedy J, Fu C, Cisewki JUS. Small-area life expectancy estimates project: methodology and results summary. Vital Health Stat 2. (2018) 181:1–40.
44. United States Census Bureau,. Census Population Estimates Program. The Census Bureau's Population Estimates Program (2016). Available online at: https://stacks.cdc.gov/view/cdc/58853/cdc_58853_DS1.pdf?download-document-submit=Download
45. Schederecker F, Kurz C, Fairburn J, Maier W. Do alternative weighting approaches for an index of multiple deprivation change the association with mortality? A sensitivity analysis from Germany. BMJ Open. (2019) 9:e028553. doi: 10.1136/bmjopen-2018-028553
46. Aarnoudse-Moens CSH, Oosterlaan J, Duivenvoorden HJ, van Goudoever JB, Weisglas-Kuperus N. Development of preschool and academic skills in children born very preterm. J Pediatr. (2011) 158:51–6. doi: 10.1016/j.jpeds.2010.06.052
47. de Kieviet JF, Zoetebier L, van Elburg RM, Vermeulen RJ, Oosterlaan J. Brain development of very preterm and very low-birthweight children in childhood and adolescence: a meta-analysis. Dev Med Child Neurol. (2012) 54:313–23. doi: 10.1111/j.1469-8749.2011.04216.x
48. Fomby P, Cherlin AJ. Family instability and child well-being. Am Sociol Rev. (2007) 72:181–204. doi: 10.1177/000312240707200203
49. Landrigan PJ, Miodovnik A. Children's health and the environment: an overview. Mt Sinai J Med. (2011) 78:1–10. doi: 10.1002/msj.20236
50. Currie J, Stabile M, Manivong P. Child health and young adult outcomes. J Human Res. (2010) 45:517–48. doi: 10.1353/jhr.2010.0013
51. Chen E, Paterson LQ. Neighborhood, family, and subjective socioeconomic status: how do they relate to adolescent health? Health Psychol. (2006) 25:704–14. doi: 10.1037/0278-6133.25.6.704
52. Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. (2011) 137:959–97. doi: 10.1037/a0024768
53. Santiago CD, Wadsworth ME, Stump J. Socioeconomic status, neighborhood disadvantage, and poverty-related stress: prospective effects on psychological syndromes among diverse low-income families. J Econ Psychol. (2011) 32:218–30. doi: 10.1016/j.joep.2009.10.008
54. Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. (2012) 129:e232–46. doi: 10.1542/peds.2011-2663
55. Odgers CL. Income inequality and the developing child: is it all relative? Am Psychol. (2015) 70:722–31. doi: 10.1037/a0039836
56. Crosnoe R. Low-income students and the socioeconomic composition of public high schools. Am Sociol Rev. (2009) 74:709–30. doi: 10.1177/000312240907400502
57. Odgers CL, Donley S, Caspi A, Bates CJ, Moffitt TE. Living alongside more affluent neighbors predicts greater involvement in antisocial behavior among low-income boys. J Child Psychol Psychiatry. (2015) 56:1055–64. doi: 10.1111/jcpp.12380
58. Acevedo-Garcia D, Noelke C, McArdle N, Sofer N, Hardy EF, Weiner M, et al. Racial and ethnic inequities in children's neighborhoods: evidence from the new child opportunity index 20. Health Aff. (2020) 39:1693–701. doi: 10.1377/hlthaff.2020.00735
59. Barnes H, Noble M, Wright G, Dawes A. A geographical profile of child deprivation in south africa. Child Indic Res. (2009) 2:181–99. doi: 10.1007/s12187-008-9026-2
60. UNICEF Innocenti Research Centre. Measuring Child Poverty: New League Tables of Child Poverty in the World's Rich Countries. UN (2012).
62. Smith S, Granja MR, Nguyen UT. New York State Profile of Young Children in Deep Poverty. NCCP (2017).
63. Systematic Inequality and Economic Opportunity—Center for American Progress. Available online at: https://www.americanprogress.org/issues/race/reports/2019/08/07/472910/systematic-inequality-economic-opportunity/ (accessed March 12, 2021).
64. Counting, All Kids in 2020: 4,.5 Million Kids Live in Hard-to-Count Census Tracts | KIDS COUNT Data Center. Available online at: https://datacenter.kidscount.org/updates/show/221-counting-all-kids-in-2020 (accessed March 12, 2021).
65. Benson PL. All Kids Are Our Kids: What Communities Must do to Raise Caring and Responsible Children and Adolescents. American Psychological Association (2006).
66. Chetty R, Hendren N, Kline P, Saez E. Where is the land of Opportunity? The Geography of Intergenerational Mobility in the United States. Q J Econ. (2014) 129:1553–623. doi: 10.1093/qje/qju022
67. Jonnalagadda P, Swoboda CM, Fareed N. Using area-level measures of social determinants of health to deliver improved and effective health care. J Hosp Manag Health Policy. (2020) 4:38–38. doi: 10.21037/jhmhp-20-100
68. Schnake-Mahl AS, Jahn JL, Subramanian SV, Waters MC, Arcaya M. Gentrification, neighborhood change, and population health: a systematic review. J Urban Health. (2020) 97:1–25. doi: 10.1007/s11524-019-00400-1
Keywords: area-level deprivation, opportunity, children well-being, social determinants of health (SDoH), neighborhood
Citation: Fareed N, Singh P, Jonnalagadda P, Swoboda C, Odden C and Doogan N (2022) Construction of the Ohio Children's Opportunity Index. Front. Public Health 10:734105. doi: 10.3389/fpubh.2022.734105
Received: 30 June 2021; Accepted: 17 June 2022;
Published: 22 July 2022.
Edited by:
Arlinda Cerga Pashoja, University of London, United KingdomReviewed by:
T. M. Tonmoy Islam, Elon University, United StatesYaojiang Shi, Shaanxi Normal University, China
Copyright © 2022 Fareed, Singh, Jonnalagadda, Swoboda, Odden and Doogan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Naleef Fareed, bmFsZWVmLkZhcmVlZEBvc3VtYy5lZHU=
 Naleef Fareed
Naleef Fareed Priti Singh
Priti Singh Pallavi Jonnalagadda
Pallavi Jonnalagadda Christine Swoboda
Christine Swoboda Colin Odden4
Colin Odden4