- 1School of Psychology, Beijing Sport University, Beijing, China
- 2China Wushu School, Beijing Sport University, Beijing, China
- 3Beihu Road Primary School, Liuzhou, Guangxi, China
Objective: The high rate of relapse has become the primary obstacle of drug rehabilitation. In this study, we explored the relationship between sleep disorders and relapse inclination in substance users, as well as the potential mediating mechanisms and corresponding interventions.
Methods: A total of 392 male substance users were recruited to complete the questionnaires on sleep disorders, quality of life and relapse inclination. On account of this, 60 participants with sleep disorders were randomly screened and allocated to the intervention and control groups. The former received 12 weeks of Health Qigong aimed at treating sleep disorders, whereas the latter performed their regular production work.
Results: Sleep disorders had a positive effect on relapse inclination, quality of life was a potential mediator of this relationship, and 12-week Health Qigong designed to treat sleep disorders improved not only their sleep quality but also their overall quality of life, which in turn reduce the tendency to relapse.
Conclusion: Current research not only explores the high-risk factors influencing relapse, but also develops customized intervention strategies, which have theoretical and practical implications for decreasing relapse and increasing abstinence.
1. Introduction
Drug relapse refers to the use, intake, or abuse of psychoactive substances by substance users who have undergone withdrawal treatment and rehabilitation (1). According to the most recent data in 2021, China has 1.801 million substance users, with a relapse rate of 91.4%. Relapse prevention has become a top priority in drug addiction intervention and treatment. According to Chinese law, mandatory isolation is the most important method of detoxification and relapse prevention (2). Substance users in mandatory isolation centers will receive 2 years of specialized education in detoxification, therapy, rehabilitation, and reintegration into society. Simultaneously, they will engage in necessary production activities, acquire vocational skills, gain insight into the dynamics of drug control, receive instruction in the prevention of relapse, and alter undesirable patterns of behavior. However, not much progress is made in alleviating drug cravings or preventing relapse due to this (3). In order to better the abstinence rate and decrease the relapse rate of substance users, it is imperative to explore the high-risk factors of relapse and develop specialized intervention programs.
1.1. Sleep disorders and relapse
Sleep disorders are the inability to get normal sleep in a suitable sleep environment. The most prominent clinical manifestations include difficulty in getting to sleep and maintaining sleep for a long time, waking up early and feeling tired after waking up, which sometimes lead to physical discomfort and even physical dysfunction (4). substance users in China are more likely to experience sleep problems than the general population. Specifically, the majority of individuals who used heroin (80.24%), methamphetamine (54.16%), or ketamine (81.98%) suffered from sleep disorders (5). Due to longer sleep latency, poorer subjective sleep quality, and less efficient sleep habits, substance users reported more frequent sleep disorders and an increased need for sleep medication than non-users (5).
The neurobiological processes underlying sleep and substance abuse are intertwined, and alterations to one can have repercussions on the other (6). Acute and chronic drug use (such as opioids, cocaine, methamphetamine, morphine, etc.) has been shown to disrupt sleep in various ways, including latency to sleep onset, sleep maintenance, and sleep quality (7–9). In turn, sleep quality was inversely associated with cravings for a range of substances, including alcohol, tobacco, opiates and marijuana during detoxification (10, 11). For example, poor sleep was linked to a higher risk of drug use in a study of 60,000 teenagers, and individuals with abnormal circadian rhythms (combined with secondary sleep disorders) were more likely to develop addiction (12). Other study using the Ecological Transient Assessment, which sent surveys to 122 people in addiction treatment once a day for 3 weeks, showed a stronger association between sleep quality and craving, indicating a potential cumulative effect of sleep disorders on craving (13). Increased sensitivity to pain, augmented negative emotions, cognitive impairment, and lack of willpower are just some of the consequences of interrupted sleep, which contribute to an increased risk of relapse (13–16). It is not difficult to draw the conclusion that sleep disorders have a positive effect on the relapse of substance users, and the more severe the sleep disorders, the greater the likelihood of relapse.
1.2. The mediating role of quality of life
Quality of life refers to an individual's subjective evaluations about his life according to his cultural background and value system. It is shaped by each person's unique set of priorities, aspirations, and standards (17). Quality of life is a broad multidimensional structure that can be influenced by numerous factors, one of which is the quality of sleep. Previous research has looked at the relationship between elderly people's quality of life and both subjective and objective sleep quality, as well as other related factors. The findings highlight the importance of efficiency and beliefs about sleep in relation to the quality of life in healthy older adults (18). Students with chronic insomnia have a significantly lower quality of life, as evidenced by poorer physical health, higher negative emotions, fewer leisure activities, and less housework and coursework. Furthermore, college students who participate in sleep training report significant enhancements in not only sleep quality but also overall mental health and quality of life (19). In addition, more so than demographics, smoking history, and disease severity, poor sleep is a potentially modifiable risk factor for the poor quality of life in chronic obstructive pulmonary disease patients (20). Despite the fact that there are few studies that have discussed the connection between substance users' sleep and quality of life, the pertinent scientific outcomes indirectly corroborate this association.
Quality of life is not only a critical outcome variable, but also increasingly a determinant of the prognosis of substance users (21). A systematic international review of opioid users in low–and middle-income countries has shown that opioid replacement treatment would improve participants' quality of life over time, resulting in lower addiction severity index scores (21). Further, a survey of 796 people from 21 alcohol/drug service centers in Victoria and Western Australia found that patients who had undergone improvements in their social, psychological, and physical quality of life were better able to sustain the reduction in substance use over the long term (22). In brief, as life satisfaction increases, so does withdrawal motivation (23). Consequently, sleep disorders in recovering addicts may diminish their quality of life, thereby increasing their likelihood of relapse.
1.3. Intervention effect of Health Qigong
A growing body of evidence supports the notion that exercise not only improves physical appearance, aids in weight loss, and increases muscle mass, but also has positive effects on mood, thinking, and other factors. However, recent studies have shown that participation in physical activity does not always yield positive outcomes (24). This might be brought on by variants in exercise's structural parameters like intensity, duration, frequency, and type. In comparison to Tai Chi and general aerobic exercise, Health Qigong has been proven more effective at enhancing sleep quality (25). Qi is the universal air, while Gong refers to practice and exercise (26). Qigong, a traditional Chinese health practice with a long and storied history, may be generally divided into internal Qigong and external Qigong (27). When engaging in internal Qigong, practitioners control their inner Qi by paying attention to their bodies and breathing, whereas external Qigong, also known as Medical Qigong, calls on qualified Qigong therapists to identify energy blockages and provide Qi to help patients' energy flow (28). Health Qigong falls under the area of internal Qigong and has the potential to serve as a complementary treatment for an array of physical and psychological disorders, such as fatigue, anxiety, and depression (29). However, the relevant study on Health Qigong and sleep disorders did not include individuals with substance use disorders. Accordingly, this study will target sleep disorders to explore whether a 12-week specialized Health Qigong intervention could improve sleep quality and reduce drug relapse.
1.4. The current study
In conclusion, the purpose of the current study was to investigate the relationship between sleep disorders and substance users' relapse, as well as the potential mediating mechanisms and corresponding interventions. The relapse inclination was used to predict the participants' post-treatment relapse behavior because they were all receiving mandatory isolation treatment in drug rehabilitation institutions and thus had no access to external drugs. Relapse inclination refers to the propensity of substance users to intake substances again after successful treatment. We proposed the following hypotheses in light of the literature review:
H1: Sleep disorders of substance users will be directly associated with relapse inclination.
H2: Quality of life will mediate the relationship between sleep disorders and relapse inclination.
H3: Health Qigong intervention targeting sleep disorders could effectively improve sleep quality, enhance the quality of life, and then reduce relapse inclination.
2. Materials and methods
2.1. Participants
2.1.1. Cross-sectional surveys (stage 1)
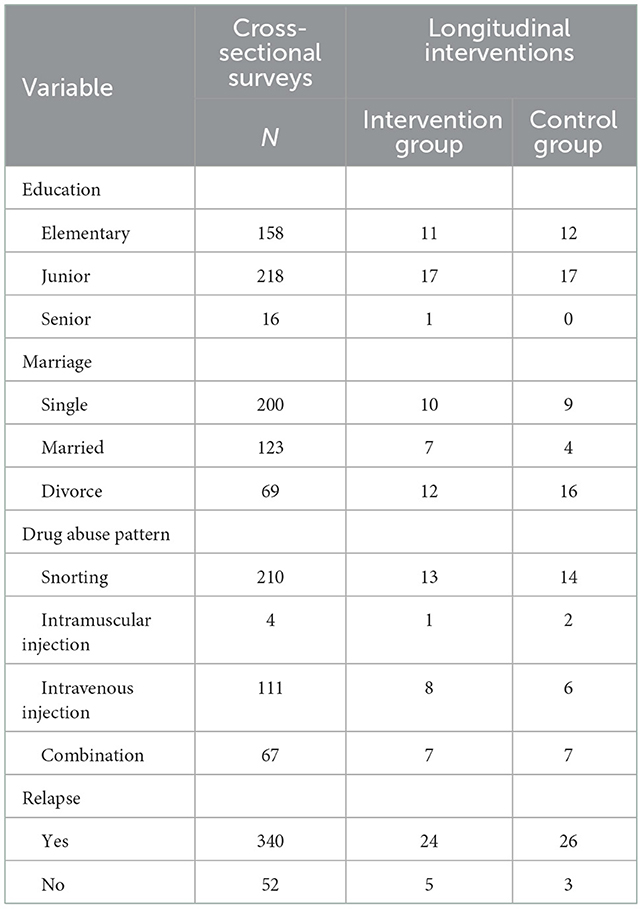
A total of 420 male substance users were recruited via convenience sampling from Guangxi rehabilitation facilities in China. The survey was conducted through a collective test of paper questionnaires, which were distributed and collected on-site. 392 valid questionnaires were gathered at the end, for a response rate of 93.33%, after invalid questionnaires were eliminated. The age of the participants was 38.78 ± 8.30 years, and the years of drug use were 4.51 ± 1.67 years. Table 1 provides a summary of the participants' demographic characteristics.
2.1.2. Longitudinal Health Qigong interventions (stage 2)
In accordance with the findings of the cross-sectional survey, 60 individuals with sleep disorders were randomly assigned to the intervention group or the control group. Exclusion criteria: (1) patients with a psychiatric diagnosis; (2) individuals with interpersonal communication disorders; (3) those who completed drug treatment in isolation within four months; and (4) individuals with benzodiazepine use disorders. Ultimately, each group contained 29 participants. There were no significant differences in age (36.86 ± 6.84 vs. 38.14 ± 5.76) and the years of drug use (4.69 ± 1.58 vs. 4.65 ± 1.88) between the intervention and the control group (p > 0.05). Additional demographic details for both groups are presented in Table 1. The drug rehabilitation center approved this study after conducting an ethics review. All individuals voluntarily participated and provided written informed consent.
2.2. Measures
2.2.1. Pittsburgh sleep quality index
This scale is administered to evaluate the sleep quality of an individual over the past month (30). It consists of 18 items, including 7 dimensions: subjective sleep quality, time to fall asleep, sleep duration, sleep efficiency, sleep disturbance, hypnotic drugs and daytime dysfunction, each of which ranged from 0 to 3, resulting in a total score from 0 to 21. The higher the score, the more severe the sleep disturbance. There is a consensus that a PSQI score of 7 or lower indicates healthy sleep, while a score above 7 implies sleep disorders. In current study, the Cronbach's alpha was 0.74.
2.2.2. The MOS item short from health survey (SF-36)
It's used to assess the composite indicator of both physiological and psychological well-being (31). This scale consists of 36 items, including eight dimensions: PF, physical functioning; RP, role physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role emotional; and MH, mental health. The higher the score, the better the quality of life. In current study, the Cronbach's alpha was 0.90.
2.2.3. Relapse inclination questionnaire
This scale is used to determine the likelihood that participants would resume substance use after completing drug treatment (32). It evaluates five dimensions: confidence in drug withdrawal, real influence of drugs, objective environment, degree of physical and mental damage and support system. It consists of 18 items with responses graded on a six-point Likert scale (least severe = 0 to most severe = 5). Higher scores indicate greater likelihood of relapse. In this investigation, the Cronbach alpha value was 0.89.
2.2.4. Intervention program and implementation of Health Qigong
From the perspective of traditional Chinese medicine, the normal sleep-wake pattern is determined by the balance of Yin and Yang. Yin deficiency and Yang excess are the primary causes of sleep disorders. Moreover, the kidney is the source of Yin and is connected directly or indirectly to all body functions. To put it another way, sleep disorders stem from a deficiency of kidney Yin (33). By engaging in specific Health Qigong movements like Deer Running and Golden Rooster Dawn, it is feasible to effectively accomplish the goals of nourishing Yin and tonifying the kidney. On the basis of this concept, we designed a set of targeted Health Qigong prescriptions, including the following actions: the ready form, Holding Sky with Hands, Shuangyu Xuange, Longdeng, Tiger Pounce, Rouji Style, Deer Running, Golden Rooster Dawn, Bird Flying, Returning Qi to the Source, and the ending form. Implementation environment: On the playground of Guangxi rehabilitation facilities. Qualifications of the intervener: It was carried out jointly by the ambassador of Health Qigong of Guangxi Province and the director of the Traditional Sports Health Research Center of the China Wushu Academy. All interventions took place from 4:00 to 5:00 p.m., four times per week, for a total of 12 weeks.
2.3. Procedures
In the cross-sectional questionnaire study, the PSQI, SF-36, and RIQ were administered in groups. The PSQI score was applied to screen participants with sleep disorders for the longitudinal intervention study, and 60 of them were randomly assigned to the intervention group and the control group. Besides, the questionnaire's results were taken as pre-test scores. There were no significant differences in PSQI (17.46 ± 2.32 vs. 16.78 ± 3.14), SF-36 (456.64 ± 117.36 vs. 499.85 ± 133.36) and RIQ (1.59 ± 0.51 vs. 1.32 ± 0.57) between the intervention and the control group (p > 0.05). Both groups then received the experimental intervention for a full 12 weeks. Whereas the control group performed their regular production work without any extra exercise, the intervention group engaged in Health Qigong. There are no other different settings. At the conclusion of the experiment, PSQI, SF-36, and RIQ were measured as the post-test score.
2.4. Statistical analysis
2.4.1. Data from cross-sectional surveys
To begin, Harman single-factor test was used to check for common method bias because all variables were measured by questionnaires. Secondly, descriptive analysis and Pearson correlation were conducted for the main variables. Subsequently, the PROCESS plug-in is used to test the mediation model employing bias corrected percentile bootstrap CI.
2.4.2. Data from longitudinal interventions
A 2 (group: intervention group, control group) ×2 (time: pre-test, post-test) two-factor mixed design analysis of variance was used to compare baseline and post-intervention scores on measures of sleep disorders, quality of life and relapse inclination between the intervention and control groups. Furthermore, correlation analysis was used to evaluate the relationships among the changes in PSQI, SF-36 and RIQ in the intervention group before and after the intervention to determine whether all variables altered to the same extent.
3. Results
3.1. Results of cross-sectional surveys
3.1.1. Common method deviation test
The Harman single factor test was used to examine the common method deviation. All the questionnaire items were included in exploratory factor analysis. The first factor explained 22.51% of the total variance, which was less than the 40% threshold, indicating that there was no common method deviation.
3.1.2. Descriptive statistics and correlations of variables
Based on the diagnostic criteria for sleep disorders (PSQI > 7), all participants suffered from sleep disturbances to varied degrees (M PSQI = 15.98, SD = 2.32; minimum = 9, maximum = 22.50). Table 2 revealed that PSQI was negatively correlated with SF-36 (r = −0.41, p < 0.01), and positively correlated with RIQ (r = 0.49, p < 0.01). SF-36 was negatively correlated with RIQ (r = −0.59, p < 0.01). In light of this, we can dig deeper into how the aforementioned factors interact with one another.
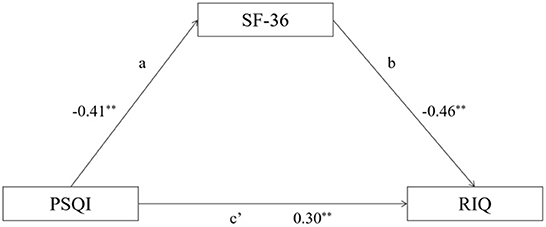
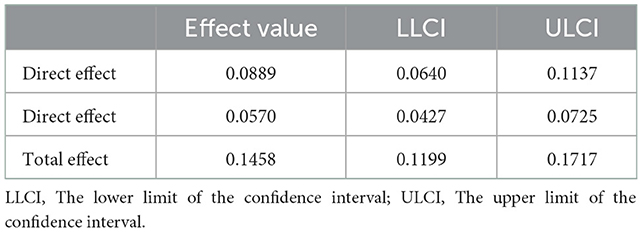
The model of this investigation is constructed in accordance with the theoretical hypothesis and the findings of the correlation analysis (as depicted in Figure 1). Model 4 in the PROCESS of SPSS macroprogram was used to test the mediating effect of quality of life, with PSQI serving as the independent variable, SF-36 as the mediating variable, and RIQ as the dependent variable. Table 3 demonstrated that the direct impact of PSQI on RIQ is 0.089, p < 0.01, while the indirect impact is 0.06, p < 0.01. The model's mediating effect is statistically significant, and indirect effect comprised 39.09% of the total effect.
3.2. Results of longitudinal interventions
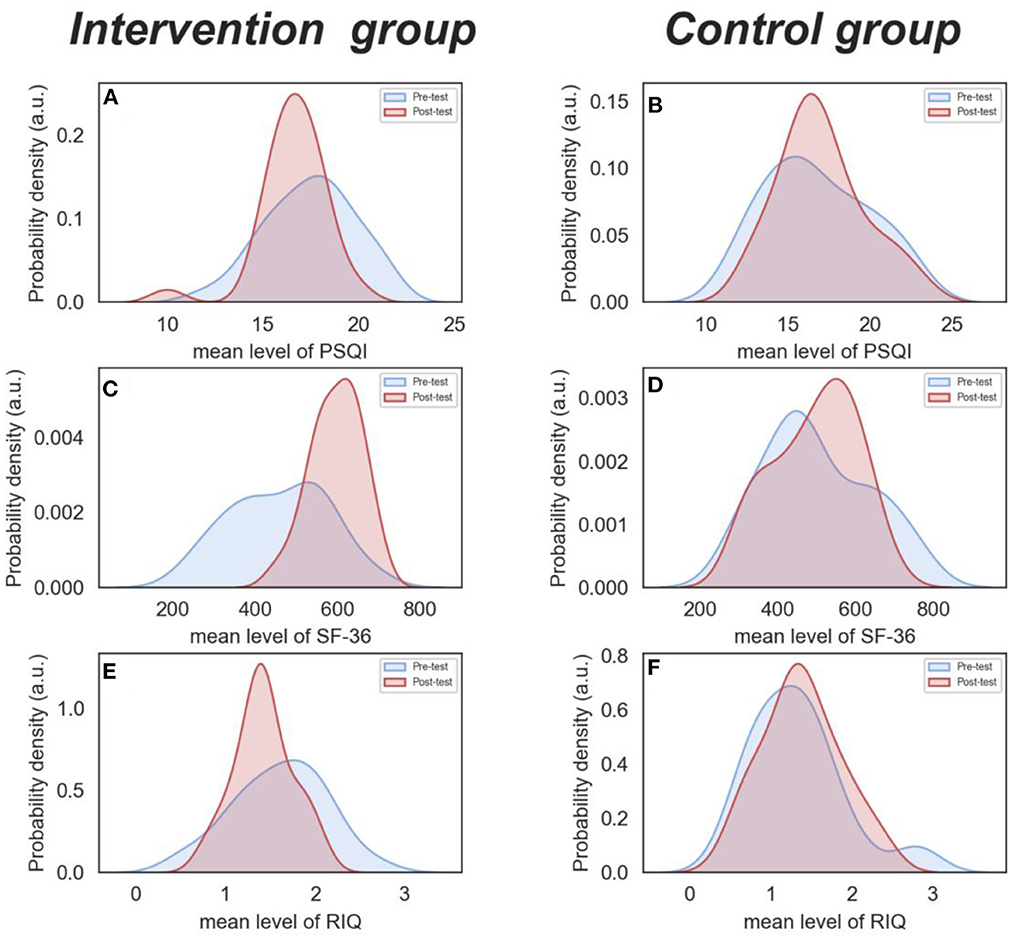
Using two-factor mixed design ANOVA, it was discovered that there was a statistically significant interaction between group and time in PSQI score (F = 8.05, p = 0.006, partial η2 = 0.126). The main effect of group (F = 0.04, p = 0.852, partial η2 = 0.001) and time (F = 2.48, p = 0.121, partial η2 = 0.042) were not significant. The simple effect analysis found that the pre-test scores (17.46 ± 2.32) of the intervention group were higher than the post-test scores (16.58 ± 1.76), while the control group's scores remained relatively stable (16.78 ± 3.14 vs. 17.03 ± 2.59) (see Figures 2A, B).
In terms of the SF-36 score, the interaction between group and time was statistically significant (F = 37.14, p < 0.001, partial η2 = 0.399). The main effect of group (F = 1.22, p = 0.274, partial η2 = 0.021) was not statistically significant. However, the main effect of time was significant (F = 31.66, p < 0.001, partial η2 = 0.361). The simple effect analysis revealed that the pre-test scores (456.64 ± 117.36) of the intervention group was lower than that of the post-test (594.55 ± 61.32), while the difference of the control group was not statistically significant (499.85 ± 133.36 vs. 494.36 ± 117.36) (see Figures 2C, D).
With regard to RIQ score, the interaction between group and time was statistically significant (F = 8.08, p = 0.006, partial η2 = 0.126). Nevertheless, the main effect of group (F = 1.77, p = 0.189, partial η2 = 0.031) and time (F = 2.22, p = 0.142, partial η2 = 0.038) were not significant. The simple effect analysis found that the pre-test scores (1.59 ± 0.51) of the intervention group were higher than the post-test scores (1.41 ± 0.32). However, the outcomes for the control group stayed relatively constant (16.78 ± 3.14 vs. 17.03 ± 2.59) (see Figures 2E, F).
The difference scores, which were calculated by subtracting the corresponding pretest scores from the posttest scores of PSQI, SF-36 and RIQ, were indicated as DPSQI, DSF-36, and DRIQ, respectively. Correlation analysis revealed that DPSQI was negatively correlated with DSF-36 (r = −0.31, p < 0.05), and positively correlated with DRIQ (r = 0.57, p < 0.01). DSF-36 was negatively correlated with DRIQ (r = −0.42, p < 0.01).
4. Discussion
4.1. Sleep disorders and relapse
Consistent with previous research, sleep disorders positively predicted relapse inclination in substance users, which supported hypothesis 1. Sleep disorders have been linked to an increase in amphetamine's sensitization (34), a enhance in conditioned place preference for methamphetamine (35), and a rise in the speed with which one learns to self-administer cocaine and respond on a progressive ratio schedule (36). Furthermore, the fragmentation of rapid-eye-movement sleep speeds up the emergence of cocaine cravings (37). Sleep disorders have a significant impact on dopamine-mediated mesolimbic circuits, which are also in charge of the regulation of reward. Sleep deprivation decreases the availability of D2/D3 dopamine receptors in the ventral striatum (38, 39), which increases the risk of risk-taking behavior and compulsive drug use (40, 41). Consequently, sleep disorders in the context of substance use are a profound research focus, and identifying and treating sleep disorders may be a crucial measure to prevent substance abuse and prevent relapse.
4.2. The mediating role of quality of life
This study further explored how sleep disorders contributed to relapse inclination and discovered that quality of life might be a mediator of this relationship, supporting hypothesis 2. The first path, wherein sleep disorders were negatively related to quality of life, was in line with previous research. According to the four-dimensional model of quality of life, there are four aspects of quality of life: physical health, mental health, social health, and spiritual health (42). In terms of physical health, sleep disorders are connected with dysfunction in the majority of body systems, such as nervous system disorders, higher cortical, endocrine and metabolic (43). When it comes to mental health, sleep disorders could cause or exacerbate a host of psychological disorders, including impulse control, behavioral suppression, and addiction (44). As for social health, sleep disorders were associated with increased interpersonal stress and worse evaluations of interpersonal effectiveness (45, 46). One more downside of poor sleep is a diminished capacity for empathy and connection with others (47). With regard to spiritual health, Muslim women's quality of sleep is closely related to their spiritual wellbeing and religious practice (48).
The second path of the mediation model, wherein quality of life was negatively related to relapse inclination, was supported by relevant studies. After implementing a “community intensification” strategy to enhance the social and environmental quality of life for alcohol-dependent individuals, Hunter and Azrin discovered that participants had high rates of abstinence (49). The decline in substance abuse may be attributable to the rise in satisfaction brought on by the enhancements in living conditions. The self-medication hypothesis postulated substance users might take substance abuse as a coping mechanism to manage psychological stress, pain, or severe/complex mental problems. Once they discovered alternatives to enhance their quality of life, they were more likely to give up drugs (50).
4.3. Intervention effect of Health Qigong
In stage 2, we proved that Health Qigong intervention targeting sleep disorders could successfully enhance sleep quality, raise quality of life, as well as reduce the likelihood of relapse, thereby confirming hypothesis 3. Health Qigong for 12 weeks has been consistently confirmed to improve various aspects of sleep, including latency to sleep onset, total sleep time, efficiency of sleep, and daytime dysfunction, among others (51, 52). Health Qigong, a mind-body exercise that emphasizes meditation and deep breathing, improves respiratory function and regulates all of the body's organs through relaxation (25). This may increase melatonin (53), reduce inflammation, and affect the stress response pathways (54), which will lessen sleep disorders. Healthy sleep can not only aid in the recovery from physical fatigue, but also make a significant and valuable contribution to the development of mental health. Accordingly, it stands to reason that better life quality will follow from fewer sleep disorders. Furthermore, addiction is merely a means of pursuing joy and happiness, and the allure of addiction can be diminished by leading a more fulfilling life (55). To put it another way, individuals are less likely to relapse if they are more content with their lives.
5. Conclusion
The current study identified sleep disorders is closely related to the relapse of substance users, and quality of life was a potential mediator of this relationship. In addition, a 12-week Health Qigong program designed to treat sleep disorders improves not only sleep quality but also the overall quality of life, which in turn reduces the tendency to relapse.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the School of Psychology at the Beijing Sport University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
The intervention of Health Qigong was carried out by XW and AL. CS performed data analysis and carried out the bulk of the literature review and manuscript writing. XW and YS played an editorial role when it came to writing up the research study. Material preparation and data collection were performed by all authors. All authors contributed to the study conception and design and read and approved the final manuscript.
Funding
This study was funded by Guangxi Zhuang Autonomous Region Drug Rehabilitation Administration (Grant No. BSU20210330).
Acknowledgments
Thanks to all the participants and volunteers who provided support for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1102115/full#supplementary-material
References
1. Brandon TH, Vidrine JI, Litvin EB. Relapse and relapse prevention. Annu Rev Clin Psycho. (2007) 3:257–84. doi: 10.1146/annurev.clinpsy.3.022806.091455
2. Zhang X, Zeng X. Effects of family functioning on relapse among individuals with drug addiction in compulsory isolation: a chained mediation model. Curr Psychol. (2021) 03:739–40. doi: 10.1007/s12144-021-01561-6
3. Tanguay P, Kamarulzaman A, Aramrattana A, Wodak A, Thomson N, Ali R, et al. Facilitating a transition from compulsory detention of people who use drugs towards voluntary community-based drug dependence treatment and support services in Asia. Harm Reduct J. (2015) 12:31. doi: 10.1186/s12954-015-0071-0
4. Sudhansu C. Overview of sleep & sleep disorderss. Indian J Med Res. (2010) 131:126–140. doi: 10.1016/S0030-6665(05)70123-7
5. Tang J, Liao Y, He H, Deng Q, Zhang G, Qi C, et al. Sleeping problems in Chinese illicit drug dependent subjects. BMC Psychiatry. (2015) 15:28. doi: 10.1186/s12888-015-0409-x
6. Valentino RJ, Volkow ND. Drugs, sleep, and the addicted brain. Neuropsychopharmacol. (2019) 45:3–5. doi: 10.1038/s41386-019-0465-x
7. Eacret D, Veasey S, Blendy J. Bidirectional relationship between opioids and disrupted sleep: putative mechanisms. Mol Pharmacol. (2020) 98:445–53. doi: 10.1124/mol.119.119107
8. Bjorness TE, Greene RW. Interaction between cocaine use and sleep behavior: a comprehensive review of cocaine's disrupting influence on sleep behavior and sleep disruptions influence on reward seeking. Pharmacol Biochem Be. (2021) 206:173194. doi: 10.1016/j.pbb.2021.173194
9. Vrajová M, Šlamberová R, Hoschl C, Ovsepian SV. Methamphetamine and sleep impairments: neurobehavioral correlates and molecular mechanisms. Sleep. (2021) 44:1–12. doi: 10.1093/sleep/zsab001
10. Serre F, Fatseas M, Swendsen J, Auriacombe M. Are sleep disturbances associated with craving intensity? What is the influence of psychiatric comorbidity and type of substance on this relationship? A computerized ambulatory monitoring study in patients beginning treatment for addiction. Drug Alcohol Depen. (2015) 146:e94. doi: 10.1016/j.drugalcdep.2014.09.623
11. Lahti T, Methuen T, Roine R, Seppä KL, Sinclair D, Partinen M, et al. The impacts of nitrous oxide gas on sleep quality during alcohol withdrawal. BMC Res Notes. (2011) 4:108. doi: 10.1186/1756-0500-4-108
12. Weaver MD, Barger LK, Malone SK, Anderson LS, Klerman EB. Dose-dependent associations between sleep duration and unsafe behaviors among US high school students. JAMA Pediatr. (2018) 172:1187. doi: 10.1001/jamapediatrics.2018.2777
13. Freeman LK, Gottfredson NC. Using ecological momentary assessment to assess the temporal relationship between sleep quality and cravings in individuals recovering from substance use disorders. Addict Behav. (2018) 83:95–101. doi: 10.1016/j.addbeh.2017.11.001
14. Roehrs T, Hyde M, Blaisdell B, Greenwald M, Roth T. Sleep loss and REM sleep loss are hyperalgesic. Sleep. (2006) 29:145–51. doi: 10.1093/sleep/29.2.145
15. Sagaspe P, Sanchez-Ortuno M, Charles A, Taillard J, Valtat C, Bioulac B, et al. Effects of sleep deprivation on color-word, emotional, and specific stroop interference and on self-reported anxiety. Brain Cognition. (2006) 60:76–87. doi: 10.1016/j.bandc.2005.10.001
16. Lim J, Dinges DF. Sleep deprivation and vigilant attention. Ann Ny Acad Sci. (2008) 1129:305–22. doi: 10.1196/annals.1417.002
17. Uysal M, Sirgy MJ, Woo E, Kim HL. Quality of life (QOL) and well-being research in tourism. Tourism Manage. (2016) 53:244–61. doi: 10.1016/j.tourman.2015.07.013
18. Sella E, Cellini N, Borella E. How elderly people's quality of life relates to their sleep quality and sleep-related beliefs. Behav Sleep Med. (2021) 20:112–24. doi: 10.1080/15402002.2021.1895792
19. Friedrich A, Claßen M, Schlarb AA. Sleep better, feel better? Effects of a CBT-I and HT-I sleep training on mental health, quality of life and stress coping in university students: a randomized pilot controlled trial. BMC Psychiatry. (2018) 18:268. doi: 10.1186/s12888-018-1860-2
20. Zeidler MR, Martin JL, Kleerup EC, Schneider H, Mitchell MN, Hansel NN, et al. Sleep disruption as a predictor of quality of life among patients in the subpopulations and intermediate outcome measures in COPD study (SPIROMICS). Sleep. (2018) 41:zsy044. doi: 10.1093/sleep/zsy044
21. Feelemyer JP, Jarlais DCD, Arasteh K, Phillips B, Hagan H. Changes in quality of life (WHOQOL-BREF) and addiction severity index (ASI) among participants in opioid substitution treatment (OST) in low and middle income countries: an international systematic review. Drug Alcohol Depen. (2014) 134:251–8. doi: 10.1016/j.drugalcdep.2013.10.011
22. Manning V, Garfield JBB, Lam T, Allsop S, Berends L, Best D, et al. Improved quality of life following addiction treatment is associated with reductions in substance use. J Vet Med A. (2019) 8:1407. doi: 10.3390/jcm8091407
23. Laudet AB, Stanick V. Predictors of motivation for abstinence at the end of outpatient substance abuse treatment. J Subst Abuse Treat. (2010) 38:317–27. doi: 10.1016/j.jsat.2010.01.007
24. Colledge F, Vogel M, Dürsteler-Macfarland K, Strom J, Schoen S, Pühse U, et al. A pilot randomized trial of exercise as adjunct therapy in a heroin-assisted treatment setting. J Subst Abuse Treat. (2017) 76:49–57. doi: 10.1016/j.jsat.2017.01.012
25. Ko LH, Hsieh YJ, Wang MY, Hou WH, Tsai PS. Effects of health qigong on sleep quality: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Med. (2022) 71:102876. doi: 10.1016/j.ctim.2022.102876
26. Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. Comprehensive review of health benefits of Qigong and Tai Chi. Am J Health Promot. (2010) 24:e1–e25. doi: 10.4278/ajhp.081013-LIT-248
27. Zou L, Sasaki JE, Wang H, Xiao Z, Fang Q, Zhang M. A systematic review and meta-analysis of Baduanjin Qigong for health benefits: randomized controlled trials. Evid-Based Compl Alt. (2017) 2017:1–17. doi: 10.1155/2017/4548706
28. Oh B, Butow P, Mullan B, Hale A, Lee MS, Guo X, et al. Critical review of the effects of medical qigong on quality of life, immune function, and survival in cancer patients. Integr Cancer Ther. (2011) 11:101–10. doi: 10.1177/1534735411413268
29. Greenlee H, DuPont-Reyes MJ, Balneaves LG, Carlson LE, Cohen MR, Deng G, et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. J Cancer Surviv. (2017) 67:194–232. doi: 10.3322/caac.21397
30. Smyth C. The Pittsburgh Sleep Quality Index (PSQI). J Gerontol Nurs. (1999) 25:10–10. doi: 10.3928/0098-9134-19991201-10
31. Ware JE. SF-36 Health Survey Update. Spine. (2000) 25:3130–9. doi: 10.1097/00007632-200012150-00008
32. Zhang Z, A. Stusy of heroin addicts' re-addiction tendency. J Psychol Sci. (2004) 03:739–40. doi: 10.16719/j.cnki.1671-6981.2004.03.061
33. Chang XH, Du MM. Discussion on “treating insomnia from kidney”. Lishizhen medicine and materia. Medica Research. (2014) 02:419. doi: 10.3969/j.issn.1008-0805.2014.02.073
34. Kameda SR, Fukushiro DF, Trombin TF, Sanday L, Wuo-Silva R, Saito LP, et al. The effects of paradoxical sleep deprivation on amphetamine-induced behavioral sensitization in adult and adolescent mice. Psychiat Res-Neuroim. (2014) 218:335–40. doi: 10.1016/j.psychres.2014.04.046
35. Karimi-Haghighi S, Haghparast A. Cannabidiol inhibits priming-induced reinstatement of methamphetamine in REM sleep deprived rats. Prog Neuro-Psychoph. (2018) 82:307–13. doi: 10.1016/j.pnpbp.2017.08.022
36. Puhl MD, Boisvert M, Guan Z, Fang J, Grigson PS, A. novel model of chronic sleep restriction reveals an increase in the perceived incentive reward value of cocaine in high drug-taking rats. Pharmacol Biochem Be. (2013) 109:8–15. doi: 10.1016/j.pbb.2013.04.010
37. Chen B, Wang Y, Liu X, Liu Z, Dong Y, Huang YH. Sleep regulates incubation of cocaine craving. J Comput Neurosci. (2015) 35:13300–10. doi: 10.1523/JNEUROSCI.1065-15.2015
38. Volkow ND, Tomasi D, Wang GJ, Telang F, Fowler JS, Logan J, et al. Evidence that sleep deprivation downregulates dopamine d2r in ventral striatum in the human brain. J Comput Neurosci. (2012) 32:6711–7. doi: 10.1523/JNEUROSCI.0045-12.2012
39. Wiers CE, Shumay E, Cabrera E, Shokri-Kojori E, Gladwin TE, Skarda E, et al. Reduced sleep duration mediates decreases in striatal D2/D3 receptor availability in cocaine abusers. Transl Psychiat. (2016) 6:e752–e752. doi: 10.1038/tp.2016.14
40. Linnet J, Møller A, Peterson E, Gjedde A, Doudet D. Dopamine release in ventral striatum during Iowa Gambling Task performance is associated with increased excitement levels in pathological gambling. Addiction. (2010) 106:383–90. doi: 10.1111/j.1360-0443.2010.03126.x
41. Dalley JW, Fryer TD, Brichard L, Robinson ESJ, Theobald DEH, Lääne K, et al. Nucleus accumbens D2/3 receptors predict trait impulsivity and cocaine reinforcement. Science. (2007) 315:1267–70. doi: 10.1126/science.1137073
42. Ferrell BR, Hassey DK, Grant M. Measurement of the quality of life in cancer survivors. Qual Life Res. (1995) 4:523–31. doi: 10.1007/BF00634747
43. K Pavlova M, Latreille V. Sleep disorderss. Am J Foren Med Path. (2019) 132:292–9. doi: 10.1016/j.amjmed.2018.09.021
44. Tkachenko O, Dinges DF. Interindividual variability in neurobehavioral response to sleep loss: a comprehensive review. Neurosci Biobehav R. (2018) 89:29–48. doi: 10.1016/j.neubiorev.2018.03.017
45. Gunn HE, Troxel WM, Hall MH, Buysse DJ. Interpersonal distress is associated with sleep and arousal in insomnia and good sleepers. J Psychosom Res. (2014) 76:242–8. doi: 10.1016/j.jpsychores.2013.11.010
46. Nowack K. Sleep, emotional intelligence, and interpersonal effectiveness: natural bedfellows. Consult Psych J. (2017) 69:66–79. doi: 10.1037/cpb0000077
47. Bai L, Whitesell CJ, Teti, DM. Maternal sleep patterns and parenting quality during infants' first 6 months. J Fam Psychol. (2020) 34:291–300. doi: 10.1037/fam0000608
48. Khoramirad A, Mousavi M, Dadkhahtehrani T, Pourmarzi D. Relationship between sleep quality and spiritual well-being/religious activities in muslim women with breast cancer. J Relig Health. (2014) 54:2276–85. doi: 10.1007/s10943-014-9978-0
49. Hunt GM, Azrin N, A. community-reinforcement approach to alcoholism. Behav Res Ther. (1973) 11:91–104. doi: 10.1016/0005-7967(73)90072-7
50. Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harvard Rev Psychiat. (1997) 4:231–44. doi: 10.3109/10673229709030550
51. Chen MC, Liu HE, Huang HY, Chiou AF. The effect of a simple traditional exercise programme (Baduanjin exercise) on sleep quality of older adults: A randomized controlled trial. Int J Nurs Stud. (2012) 49:265–73. doi: 10.1016/j.ijnurstu.2011.09.009
52. Carcelén-Fraile MDC, Aibar-Almazán A, Martínez-Amat A, Jiménez-García JD, Brandão-Loureiro V, García-Garro PA, et al. Qigong for mental health and sleep quality in postmenopausal women: a randomized controlled trial. Medicine. (2022) 101:e30897. doi: 10.1097/MD.0000000000030897
53. Martarelli D, Cocchioni M, Scuri S, Pompei P. diaphragmatic breathing reduces exercise-induced oxidative stress. Evid-Based Compl Alt. (2011) 2011:1–10. doi: 10.1093/ecam/nep169
54. Buric I, Farias M, Jong J, Mee C, Brazil IA. What is the molecular signature of mind–body interventions? a systematic review of gene expression changes induced by meditation and related practices. Front Immunol. (2017) 8. doi: 10.3389/fimmu.2017.00670
Keywords: sleep disorders, quality of life, relapse inclination, Health Qigong, substance users
Citation: Sun C, Wang X, Huang X, Shao Y, Ling A, Qi H and Zhang Z (2023) Sleep disorders as a prospective intervention target to prevent drug relapse. Front. Public Health 10:1102115. doi: 10.3389/fpubh.2022.1102115
Received: 18 November 2022; Accepted: 12 December 2022;
Published: 04 January 2023.
Edited by:
Mark Gold, Washington University in St. Louis, United StatesReviewed by:
Lantie Elisabeth Jorandby, Lakeview Health, United StatesYi Zhang, Xidian University, China
Copyright © 2023 Sun, Wang, Huang, Shao, Ling, Qi and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaojun Wang,  MTM5MTEwNzIzMTZAMTI2LmNvbQ==
MTM5MTEwNzIzMTZAMTI2LmNvbQ==
 Chao Sun
Chao Sun Xiaojun Wang
Xiaojun Wang Xuetong Huang2
Xuetong Huang2 Yongcong Shao
Yongcong Shao