
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 16 December 2022
Sec. Aging and Public Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1091484
This article is part of the Research Topic Benefits and Challenges to Using Health-Related Information and Communication Technologies among Older Adults View all 13 articles
Aim: To evaluate the impact of a telemedicine medication management service in patients with hypertension.
Methods: Participants were allocated to either a telemedicine service (N = 173) or usual care (UC) (N = 179). The primary outcome was blood pressure (BP) reduction from baseline to the 6-month follow-up visit, the proportion of the target BP achievement, overall adherence to prescribed medication as well as a composite of non-fatal stroke, non-fatal myocardial infarction and cardiovascular death.
Results: At 6 months, BP was controlled in 89.6% (n = 155) of intervention patients and 78.8% (n = 141) of UC patients (OR = 1.14, 95% CI = 1.04–1.25, P = 0.006), giving a mean difference of −6.0 (−13.0 to −2.5 mmHg) and −2.0 mmHg (−4.0 to −0.1 mmHg) in SBP and DBP, respectively. 17.9% (n = 31) of the patients in the intervention group were non-adherent with medications, compared with 29.1% (n = 52) in the UC group (P = 0.014). The composite clinical endpoints were reached by 2.9% in the intervention group and 4.5% in the control group with no significant differences (OR = 1.566, 95% CI = 0.528–4.646).
Conclusion: Telemedicine medication management for hypertension management had led to better BP control and medication adherence improvement than UC during COVID-19 epidemic, resulting in a reduction of overall adverse cardiovascular events occurrence.
The COVID-19 pandemic has dramatically affected and overloaded healthcare systems across the globe and strained healthcare resources on many levels (1, 2). Services like medication counseling and care proved to be challenging for overloaded medical practitioners to provide (3). According to the 2018 Report on Cardiovascular Diseases in China, hypertension was an important public disease burden in China with 245 million patients (prevalence 23.2%) (4). Notwithstanding, the disease control was still suboptimal, well contributing to high risk of adverse cardiovascular outcomes, which requires long-term treatment with anti-hypertensives to control blood pressure (BP) (5). Appearing in person in clinic for routine hypertension monitoring and follow-up often exposed elderly and vulnerable patients to infectious risk. Telemedicine offers the prospect of remote management of BP for vulnerable individuals while avoiding the risks of in-person care in a pandemic (6, 7).
It was challenging to provide routine medication management for patients with hypertension and other chronic cardiovascular diseases during the pandemic (8, 9). To reduce the risk of infectious exposures, non-contact treatment models have been advocated in some settings, including China. The pharmaceutical department of the Zhongshan Hospital has built an efficient telemedicine pharmaceutical service model which leverages remote communication methods such as WeChat or telephone, to improve the service quality, reduce the risk of infection, and ensure the safety of patients (10). Telemedicine, by limiting person-to-person contact, might reduce the possibility of viral transmission, and offer the possibility of more timely care for chronic diseases. By leveraging pharmacist input, the telemedicine approach enables rapid remote review and evaluation of medication lists, indications, dosing particulars, storage methods, precautions and drug interactions.
Patients with adequate clear medication information are better equipped to make informed choices about managing their anti-hypertensives, and potentially might have more incentive and support to adhere to their prescribed medications. Therefore, this study aimed to evaluate the pharmaceutical telemedicine care service in patients with existing hypertension, as compared to usual care (UC).
This prospective single-site cohort study was designed to compare a telemedicine intervention to usual care for people with hypertension seeking care at the Zhogshan Hospital (Shanghai, China) between January 2021 and June 2021. In our study, hypertension was defined as an average office systolic BP of >140 mmHg or an average office diastolic BP of >90 mmHg or self-reported use of antihypertensive medication in the past 2 weeks according to the American Hypertension Management Guidelines (11). Patients with uncontrol hypertension were finally enrolled. Integrated care, such as health screenings, providing patient education and modifying medication regimens under collaborative practice agreements, was available for all patients who were diagnosed as hypertension including antihypertensive therapy and inconsistent approaches to cardiovascular risk reduction. All drugs were prescribed as single doses by pharmacists under the doctor's supervision. For follow-ups, BP was measured during outpatient clinic visits by specialized cardiologists or other certified specialists.
All patients involved met the following eligibility criteria: (1) age ≥ 18 years; (2) high risk for cardiovascular diseases in terms of diabetes, dyslipidemia, smoking, poor diet, and obesity; and (3) primary hypertension prescribed with antihypertensive drugs/daily. The main exclusion criteria included the following: (1) secondary hypertension; (2) severe renal dysfunction (estimated glomerular filtration rate [eGFR] <30 ml/min−1·1.73 m2); and (3) unable to communicate via WeChat or phone. This study was approved by the Ethics Committee of Zhongshan Hospital (Approval Number: B2021-021R). Written informed consent was signed by all participants before the commencement of the clinical studies.
The eligible participants were identified from clinical codes recorded in the electronic medical record system and invited to learn about this clinical study. Written informed consent for participation was obtained before the participants were determined to be eligible and we collected their baseline information via electronic health records. The BP was measured by standard mercury sphygmomanometers in a sitting position. At least two BP measurements should be taken in the sitting position, spaced 1–2 min apart and the average value was used for diagnosis (12). Consecutive participants were allocated to receive either the pharmacist-led telemedicine care and follow-up service or UC according to patients' demand and willingness.
The medication decision on patients' drugs was performed by clinicians' discretion throughout the whole study procedure. The participating pharmacists reviewed the medication for BP control and perform an individualized medication titration plan for the enrolled participants after allocation. Three and six months after allocation, scheduled follow-up appointments were performed to measure and record BP for attended participants for both groups.
Continuous participants were assigned to telemedicine pharmaceutical intervention or UC group according to patients' demand and willingness. In the intervention group, there were five cardiovascular pharmacists in total who provided the interventions, mainly including the administration time and dosage of antihypertension drugs, the management of adverse reactions, the drug interactions and BP monitoring, which as indicated in Supplementary Figure 1. The antihypertension medication guidance was listed in Supplementary Table 1. Firstly, medication review was established to collect participants' demographic and clinical factors, and their understanding of current medication status. Then, intervention was conducted based on medication guidance including educational materials and individualized pharmacotherapy.
The participants were well trained in: (i) reviewing how to use a mercury sphygmomanometer to measure their BP at home; (ii) visiting the Web-based dashboard through smartphone or WeChat, entering the personalized goals, and getting to know how to enter and view their data; and (iii) developing a personalized BP management plan (e.g., frequency of contacts for check-ins, goal-setting, and data upload) informed by the baseline home BP measurements. Then they were asked to: (i) measure their BP at home use a mercury sphygmomanometer, while sitting, after a rest period of at least 10 min; (ii) send their BP data report to the researcher through smartphone or WeChat; and (iii) set BP targets weekly. 2 The role of the pharmacist in this study was to make medical intervention or lifestyle recommendations according to the BP data and description retrieving. Participants could withdraw from the study at any time.
Participants who were allocated to UC group were not provided with an online drug counseling platform, but obtained online access for web information on hypertension control including classification and causes of hypertension, guidance for the hypertension management in terms of lifestyle improvement and medication adjustments. The participants received routine services by referring to an outpatient clinic for hypertension care which was typically composed of BP measurements for titrate drugs and antihypertensive adjustments to maintain target BP.
The demographic information and baseline assessments including age, sex, body mass index (BMI), complications, and initial BP were obtained through electronic medical recorder (EMR). Laboratory measurements including serum sodium, potassium, creatinine, estimated glomerular filtration rate, and concomitant medication record were collected from EMR.
For each eligible participants, follow-up controls were scheduled every 3 months, up to at least 6 month. BP measurements were performed at the screening visit. Physicians provided medication related interventions to make every reasonable effort to control BP in accordance with international and local hypertension management guidelines. The medication related interventions were classified into 8 categories by pharmacist in this study, including stopped therapy, side effect, adherence improvements, costs, drug-drug interaction, liver function, renal function and inappropriate doses. Other than this, duration for the first outpatient revisit and the time to first or recurrent cardio-cerebral vascular events were recorded throughout follow-ups.
Adherence to antihypertensive therapy was estimated by the self-report method at the point of 6-months follow-up via telephone interview or clinic visit (13, 14). Specifically, medication adherence was measured by proportion of days covered (PDC), defined as the number of days patients taking prescriptions divided by the interval of observation period. PDC above 80% was considered as full or high adherence (15). Conversely, the patient was considered to be non-adherent when he reported omitting dose of the medication, or making errors in dosage or frequency, or if he interrupted treatment. Reasons for medication non-adherence were recorded.
The primary outcome was systolic and diastolic BP and heart rate reduction from baseline to the 6-month follow-up visit, the proportion of the target BP achievement, overall adherence to prescribed medication as well as a composite of non-fatal stroke, non-fatal myocardial infarction and cardiovascular death.
The secondary outcomes were adherence and persistence to antihypertensive agents, antiplatelet agents, lipid-lowering agents, proton pump inhibitor (PPI) and antiarrythmic drugs and cumulative incidence of any cardio-cerebral vascular event.
A sample size of 140 consecutive participants per group were required to have 90% power according to previously reported literature (16). The level of the statistical significance test (Class I error rate α) is 0.05 (Using two-sided inspection), the statistical effect is 90% (Class II error rate β = 0.1), and the sample size is estimated using PASS 11 statistics software. To accommodate an anticipated dropout rate of 10%, 308 participants were enrolled to achieve 280 evaluable participants.
This clinical study is a single-center and prospective cohort study, whose primary endpoint was to detect a difference of systolic and diastolic BP between the telemedicine pharmaceutical intervention and usual care group. The baseline characteristics were compared between intervention and usual groups by t-tests and χ2 tests/Fisher's precision probability test where appropriate. The comparison including the changes of SBP/DBP/heart rate (presented as means ± standard deviations) to baseline were analyzed by t-tests; the proportion of the target BP achievement, adherence with anti-hypertensive medications and medication related interventions were expressed with frequencies or percentages n (%) and compared with χ2/Fisher's precision probability test. Kaplan–Meier curves were constructed to compare the duration for the first outpatient revisit and the time to first or recurrent cardio-cerebral vascular events.
A two-sided P-value was used to determine significance (threshold, P < 0.05). Statistical analysis was performed using SPSS (IBM SPSS Statistics 22.0) and Prism 5 (GrandPad Software). A P-value of 0.05 was considered to be the threshold for statistical significance.
After screening for eligibility, a total of 390 patients consented to participate in this study. The whole recruitment progress of the study and the exclusive reasons were presented in Figure 1. 14 patients declined to take part in this study and gave their reasons for the lack of mercury sphygmomanometers and no access to smartphone or WeChat. The remaining 376 (96.4%) participants were divided into intervention (N = 185) and usual care group (N = 191). During the whole recruitment period, 12 in the intervention and 12 in the usual care group were subsequently withdrawn due to the withdraw and follow-up failure of the study. The adherence rate to intervention and usual care was 93.5 and 93.7% throughout whole study.
There were 173 subjects in the intervention group and 179 subjects in the UC group at the end of the follow-up periods. No notable differences between the group were found regarding baseline demographics, clinical characteristics and laboratory indicators of the population (Table 1). Most participants were male (62.2%) with a mean age of 68.10 ± 8.82 years. The mean baseline clinical BP for intervention group and usual care group were 151.47/88.45 and 150.77/88.83 mmHg respectively.
Overall, greater BP lowering effects were observed after intervention from the numerical BP results. As for SBP, intervention group showed differences of −7.0 (−10.0 to −2.0) mmHg at Month 3 and −6.0 (−13.0 to −2.5) mmHg at Month 6 compared to UC group. The absolute reduction in DBP was also larger with intervention: −3.0 (−4.0 to −2.0) and −7.0 (−11.0 to −5.5) mmHg at Month 3 and 6, respectively, as shown in Figure 2. Besides, intervention showed difference on HR decrease with −5.0 (−7.0 to −1.5) and −4.0 (−9.0 to −3.0) beats/min as compared to UC group at Month 3 and 6, respectively.
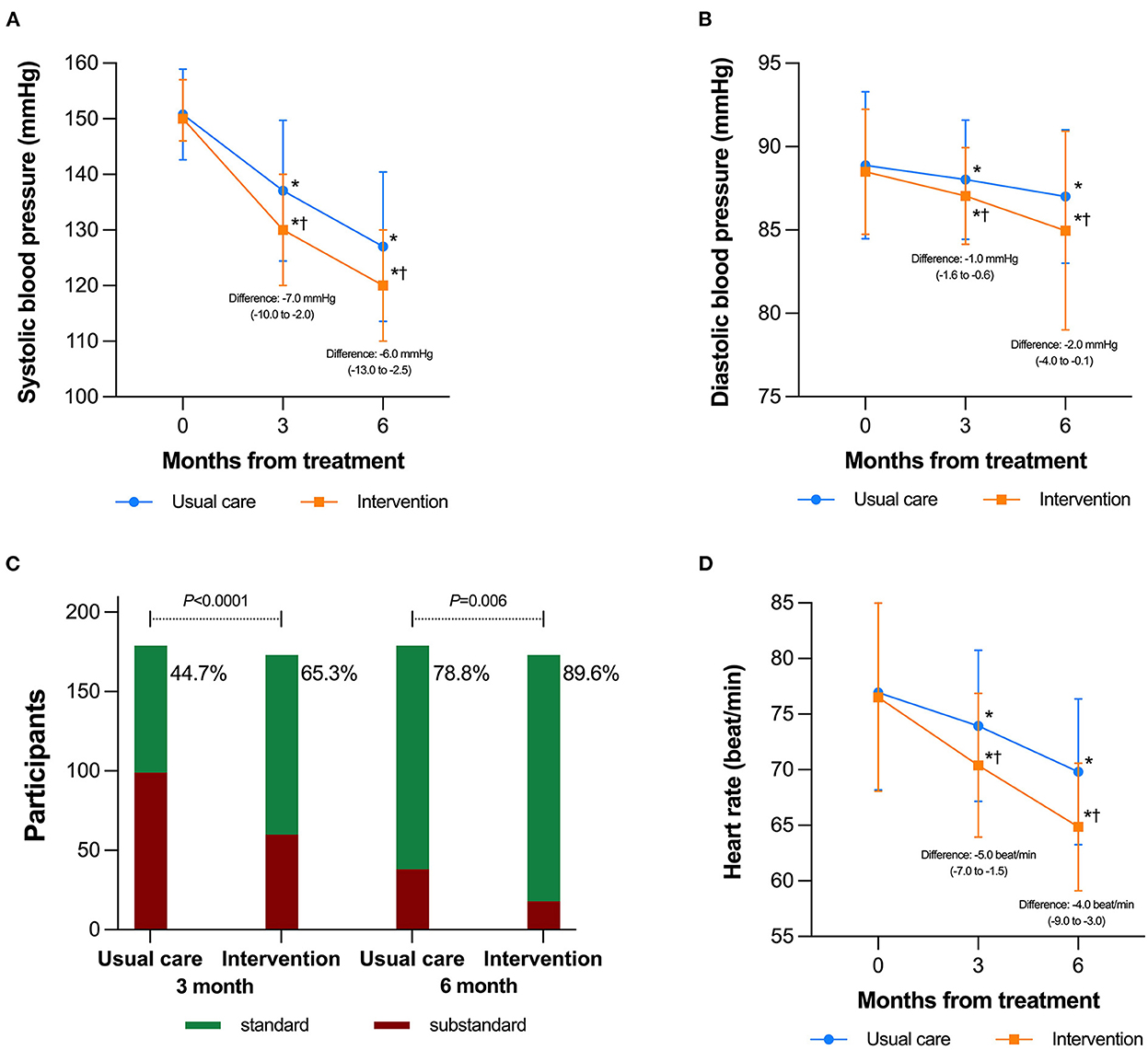
Figure 2. Blood pressure changes during the study period by group. (A) Mean values and standard deviations in systolic blood pressure (mmHg) among all participants; (B) Mean values and standard deviations in diastolic blood pressure (mmHg) among all participants; (C) Percentage of subjects achieving treatment goal; (D) Changes in heart rate, which were presented as mean and standard deviations (error bar). *P < 0.05 within group vs. baseline value;†P < 0.05 compared the intervention group with the usual care group.
Specifically, there was significant difference in the proportion of subjects who achieved target BP during the 3- and 6-month follow-ups. As shown in Figure 2C, 65.3 (n = 113/173) and 44.7% (n = 80/173) of patients achieved BP goals after receiving intervention and UC, respectively at month 3 (OR = 1.461, 95% CI = 1.202–1.778, P < 0.001), while the proportion of patients achieving target BP for intervention and UC group was 89.6 (n = 155) and 78.8% (n = 141) (OR = 1.137, 95% CI = 1.038–1.246, P = 0.006).
Throughout the treatment period, 142 (82.1%) persons in intervention group and 127 (71.0%) persons in usual care group reported full adherence (P = 0.014) (Figure 3A). Overall, medication adherence dropped as the number of prescribed medications increased (Figure 3B). Participants exhibited the highest compliance rates to antiarrhythmic agents of over 95%, while the lowest rate of below 75% was reported with PPI (Figure 3C). The most common causes of non-adherence were reported as having script but not refilling (37.4%) and forgetting (32.5%) (Figure 3D).
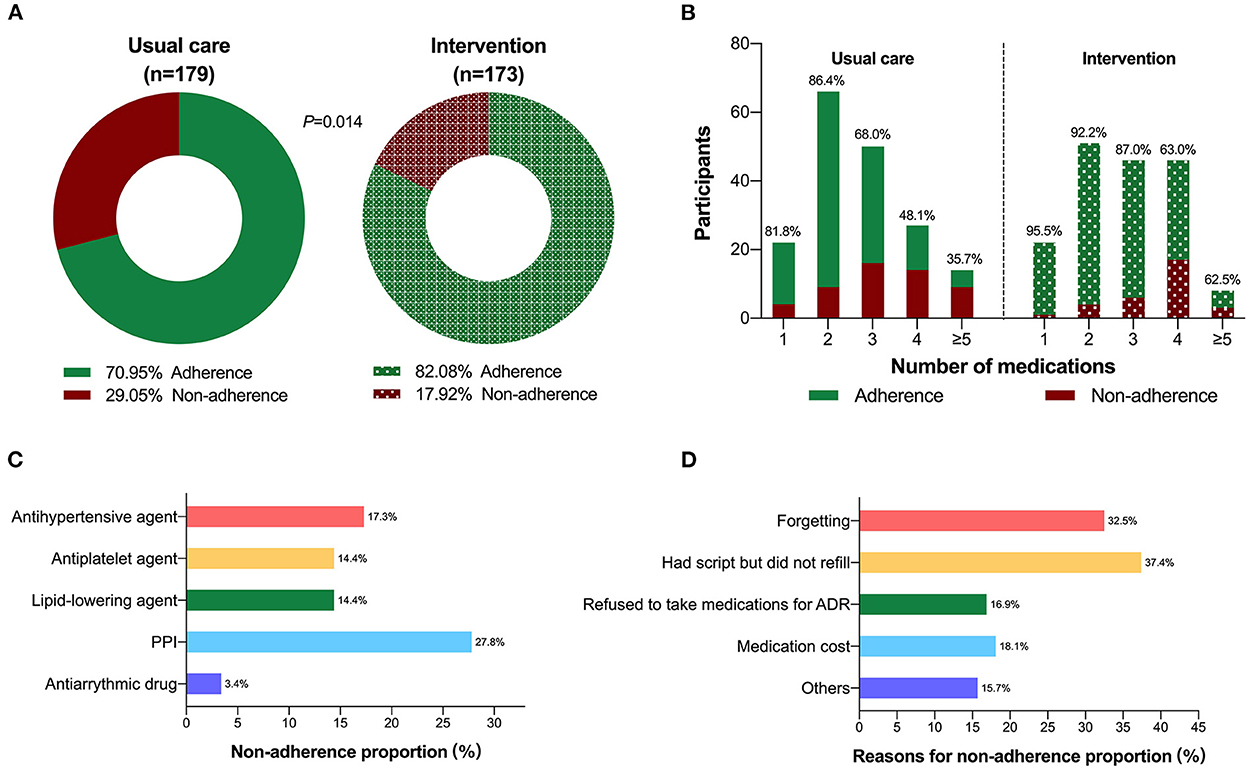
Figure 3. Rates of total adherence stratified by group. (A) Number of medication prescribed (B); (C) Drug nonadherence by different medication classes in all cohort; (D) Reasons for non-adherence among non-adherent patients.
During the follow-up period, the mean number of active outpatient revisits attended by participants was 2.22 ± 1.09 and 3.30 ± 1.37 in the intervention and usual care groups, respectively (P < 0.0001). In addition to the regular check-ups, 299 interventions were provided according to patient questioning online or at the clinic. A comparison of medication therapy interventions between non- and pharmacist intervention groups was shown in Supplementary Figure 2. Compared to usual care group, pharmacist-conducted patients had more concerns about enhancing medication adherence (19.1 vs. 7.3%, P = 0.001). Participants who received usual care were more likely to raise questions on drug-drug interaction, side effects and discontinuation of therapy (21.8 vs. 12.7%, P = 0.025; 11.2 vs. 5.2%, P = 0.042; 11.7 vs. 3.5%, P = 0.004, respectively).
There were 8 (4.5%) and 5 (2.9%) participants experiencing events as a composite of non-fatal stroke, non-fatal myocardial infarction and cardiovascular death in intervention and UC groups, respectively. As illustrated in Figure 4A, cumulative Kaplan-Meier results demonstrated that patients who belonged to UC group were more likely to experience major adverse cardiovascular events, but the difference was not statistically significant (P = 0.427, OR = 1.566, 95%CI: 0.528–4.646). Among all the events, 5 patients in the UC group and 4 patients in the intervention group developed non-fatal stroke (Figure 4B, P = 0.773, OR = 1.213, 95%CI: 0.328–4.482). With regards to non-fatal myocadiac infarction, cumulative incidence was similar between UC (n = 2) and intervention (n = 1) groups (P = 0.581, OR = 1.940, 95%CI: 0.202–18.660), as demonstrated in Figure 4C. During the study period, one subject from UC group died due to cardiovascular causes (Figure 4D).
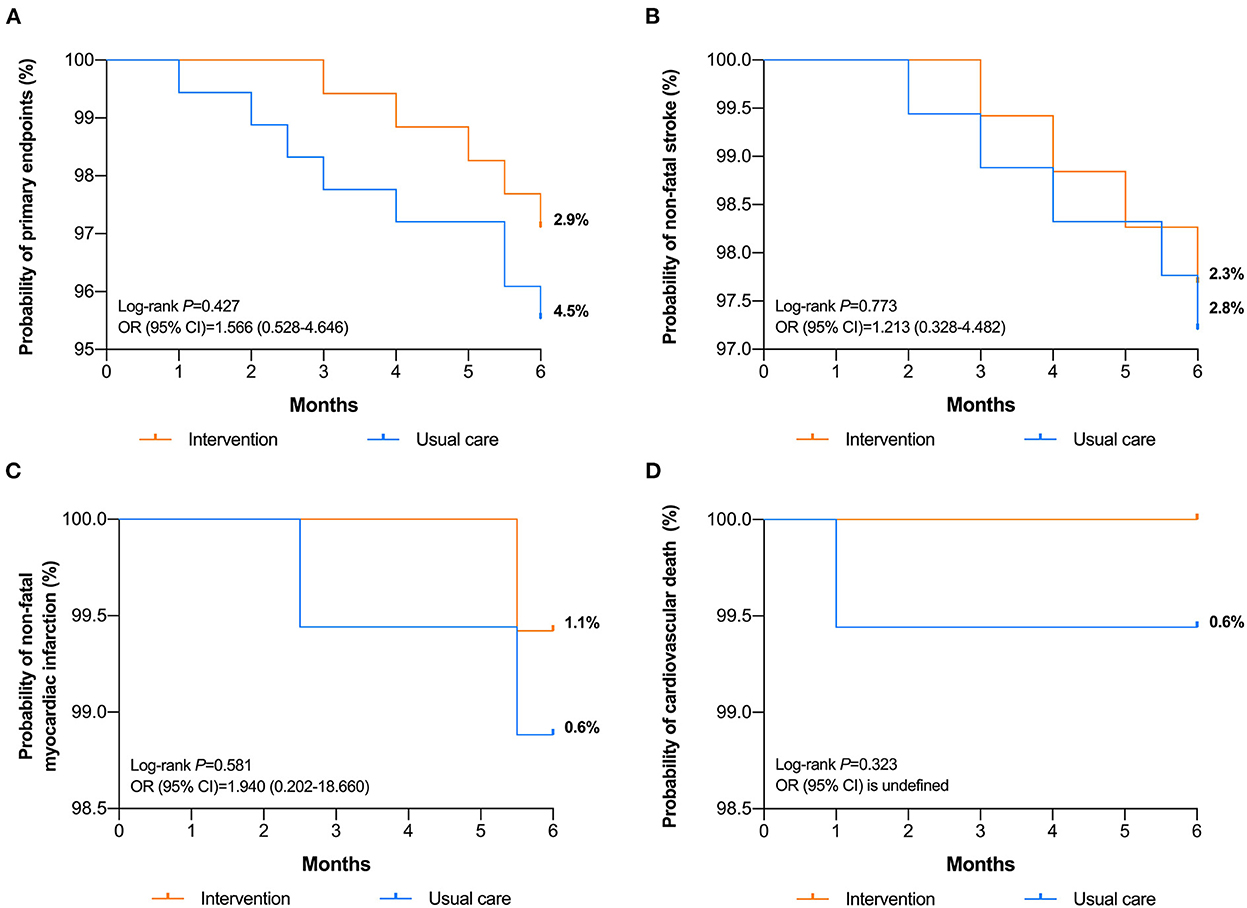
Figure 4. Kaplan-Meier cumulative curves for (A) composite of events, (B) non-fatal stroke, (C) non-fatal myocadiac infarction, and (D) cardiovascular death between intervention and UC groups.
This observational study elucidated the advantage of pharmacist-led telemedicine on antihypertensive pharmacotherapy during the COVID-19 Pandemic. Our findings highlighted that telemedicine could significantly reduce BP and improved medication adherence at the established endpoint of 6 months. Pharmacist-led telemedicine may prove effective in reducing cardiovascular events in terms of stroke, non-fatal myocardial infarction and cardiovascular death as compared to regular outpatients with a longer duration of intervention.
Providing primary healthcare during COVID-19 pandemic has brought a huge challenge mainly due to inadequate availability of personal protective equipment and high risks of infection from patients and medical practitioners for healthcare service providers (17–19). Telemedicine minimizes in-person communication and reducing face-to-face contact among clinicians and patients (20), which was first officially recommended in 2019 Chinese guidelines for the management of hypertension in the elderly and compliant with the Program for a Healthy China 2030 (21, 22). Currently, pharmacists are playing important role in patient-centered model for hypertension care which required a higher demand on interprofessional collaboration (23). Pharmacists might expand their medication interventions and provide remote services for patients by means of telemedicine. In this study, pharmacist-led telemedicine reduced the patients' offline healthcare consultations, leading to a lower risk of Covid-19 exposure, as well as the reduction of time and cost.
Our study showed that the BP reduction levels following pharmaceutical telemedicine intervention was larger than that in UC groups, either in 3 or 6 months. Telemedicine technology is widely available, inexpensive and widely accepted by doctors and patients (24). A randomized controlled trial about Home and Online Management and Evaluation of Blood Pressure demonstrated the digital intervention resulted in better BP control than UC (12). The improvement could be achieved by overcoming barriers to medication adherence in the management of hypertension. As for most cases, these interventions studies were team-based managements with pharmacist-led care (25, 26). One meta-analysis illustrated an average 10/4 mmHg decrease of SBP/DBP, and an absolute proportion within target BP improved by 20% after receiving telemedicine care (27). Another recent study reported a well-controlled BP at baseline (15 mmHg lower at 12 months follow-ups with a significant difference than UC) (28). Based on the current evidence, the most common practice model of telepharmacy utilized outside licensed pharmacy was scheduled health care interventions via WeChat for management of cardiovascular disease, mostly hypertension and diabetes (29). A previous study documented a promotion of adherence to BP monitoring and telemedicine management visits after telepharmacy intervention, thus revealing that this approach is feasible and effective (20). Telemedicine intervention by pharmacist can effectively improve the self-efficacy and medication compliance of patients with hypertension, the drug treatment management can especially reflect the professional value of pharmacists and is of great value to the management of hypertension. In addition, it also plays an important role in helping specialist pharmacists provide convenient, patient-centered pharmacy services.
Based on our findings, the benefits of pharmacist-led intervention became apparent with increasing numbers of medications. Pharmacist intervention might improve patients' understanding on medications, especially for polypharmacy patients, leading to better adherence (30). Our study also found patients exhibited worst adherence in taking PPIs, probably related with neglect and insufficient knowledge, indicating the need of more instruction from pharmacist in this aspect in the future. When regarding the reasons for non-adherence, patients not refilling medications despite having prescriptions and forgetting to take medications occupied more than half proportion, followed by fear of drug induced ADR, similar with one published study (31). Thus, pharmacist would better design a remote reminder tool to avoid omitting dose and provide guidance on precautions to cope with ADRs. Moreover, another retrospective study showed the initial pharmacist intervention could be considered most important, as patients completing the initial intervention were less likely to discontinue follow-up and more likely to be adherent (32).
Our study provided additional benefits of the pharmacist intervention. It seemed that pharmacist-conducted patients were more willing to enhance medication adherence (19.1 vs. 7.3%, P = 0.001). These positive findings could be replicated in the previous study which demonstrated that pharmacist-led medication counseling could achieve better optimal BP control and enhance compliance (33, 34). Although, another study had the opposite conclusion that there were no significant differences in medication compliance by pharmacist counseling, which may be attributed to the selection patients with low medication adherence in the study (35). Besides, we provided additional results associated with medication related interventions. Participants who received usual care were more likely to raise questions on drug-drug interaction, side effects and discontinuation of therapy (21.8 vs. 12.7%, P = 0.025; 11.2 vs. 5.2%, P = 0.042; 11.7 vs. 3.5%, P = 0.004, respectively). These results were partly supported by a previous pharmacist-led drug counseling study (36), which have evaluated 70–80% of patients were concerned about the solutions of adverse reactions and 50–60% focused on drug interactions. In a word, pharmacist-led interventions have the potential to magnify the health benefits of medications.
Although the incidence of major adverse cardiovascular events pointed in the direction in favor of pharmacists' intervention, no significant differences were found. Previous meta-analysis finds that good compliance to cardiovascular medications decrease 20% risk of cardiovascular events (37). Achievement of long-term BP target value also suggests better outcomes (38). The effects on adherence and BP targets reached in intervention group were not translated into remarkable decrease of cardiovascular events. The main reasons for the non-significant results were attributed to the small sample sizes and short follow-up time. Further large, long-term follow-up trials are required to evaluate the effect on composite endpoints.
Our study had some limitations. Firstly, this was a prospective analysis with relatively small sample size and further randomized controlled trials are needed to confirm the conclusions. Secondly, the adherence was based on self-report in this study, remaining a degree of subjectivity. Biological measurement and a validated daily reporting system considering medication refill rate are the best ways to measure medication adherence, which were not available at this time. Thirdly, this study was not placebo-controlled, therefore the findings on symptomatic status are subjective to a placebo effect. Finally, the follow-up was too short to detect long-term differences in clinical cardiovascular adverse outcomes.
In summary, pharmacist-led telemedicine for hypertension management had led to better BP control and medication adherence improvement than UC during COVID-19 epidemic, resulting in a reduction of overall adverse cardiovascular events occurrence. The further work is to realize clinical benefits for chronic illness care with this implementation strategy during COVID-19 epidemic.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Zhongshan Hospital. The patients/participants provided their written informed consent to participate in this study.
XiaoyeL and JH: writing, original draft preparation, and investigation and data curation. YY: investigation and formal analysis and software. CZ: methodology. ZW: software. XiaoyuL: conceptualization. QL: supervision and writing—reviewing and editing. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1091484/full#supplementary-material
1. Wahlster S, Sharma M, Lewis AK, Patel PV, Hartog CS, Jannotta G, et al. The coronavirus disease 2019 pandemic's effect on critical care resources and health-care providers: a global survey. Chest. (2021) 159:619–33. doi: 10.1016/j.chest.2020.09.070
2. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. (2021) 27:601–15. doi: 10.1038/s41591-021-01283-z
3. Greenhalgh T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. BMJ. (2020) 368:m1182. doi: 10.1136/bmj.m1182
4. Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, et al. Prevalence and treatment of diabetes in China, 2013–2018. JAMA. (2021) 326:2498–506. doi: 10.1001/jama.2021.22208
5. Burnier M, Egan BM. Adherence in hypertension. Circ Res. (2019) 124:1124–40. doi: 10.1161/CIRCRESAHA.118.313220
6. Omboni S, McManus RJ, Bosworth HB, Chappell LC, Green BB, Kario K, et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: an international expert position paper. Hypertension. (2020) 76:1368–83. doi: 10.1161/HYPERTENSIONAHA.120.15873
7. Wang JG, Li Y, Chia YC, Cheng HM, Minh HV, Siddique S, et al. Telemedicine in the management of hypertension: evolving technological platforms for blood pressure telemonitoring. J Clin Hypertens. (2021) 23:435–9. doi: 10.1111/jch.14194
8. Segal EM, Alwan L, Pitney C, Taketa C, Indorf A, Held L, et al. Establishing clinical pharmacist telehealth services during the COVID-19 pandemic. Am J Health Syst Pharm. (2020) 77:1403–8. doi: 10.1093/ajhp/zxaa184
9. Li H, Zheng S, Liu F, Liu W, Zhao R. Fighting against COVID-19: Innovative strategies for clinical pharmacists. Res Soc Adm Pharm. (2021) 17:1813–8. doi: 10.1016/j.sapharm.2020.04.003
10. Li X, Zuo C, Lu W, Zou Y, Xu Q, Li X, et al. Evaluation of remote pharmacist-led outpatient service for geriatric patients on rivaroxaban for nonvalvular atrial fibrillation during the COVID-19 pandemic. Front Pharmacol. (2020) 11:1275. doi: 10.3389/fphar.2020.01275
11. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. (2018) 71:e13–e115. doi: 10.1161/HYP.0000000000000065
12. McManus RJ, Little P, Stuart B, Morton K, Raftery J, Kelly J, et al. Home and online management and evaluation of blood pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial. BMJ. (2021) 372:m4858. doi: 10.1136/bmj.m4858
13. Kulkarni SP, Alexander KP, Lytle B, Heiss G, Peterson ED. Long-term adherence with cardiovascular drug regimens. Am Heart J. (2006) 151:185–91. doi: 10.1016/j.ahj.2005.02.038
14. Grymonpre RE, Didur CD, Montgomery PR, Sitar DS. Pill count, self-report, and pharmacy claims data to measure medication adherence in the elderly. Ann Pharmacother. (1998) 32:749–54. doi: 10.1345/aph.17423
15. Simpson RJ, Mendys P. The effects of adherence and persistence on clinical outcomes in patients treated with statins: a systematic review. J Clin Lipidol. (2010) 4:462–71. doi: 10.1016/j.jacl.2010.08.026
16. Rogers MA, Buchan DA, Small D, Stewart CM, Krenzer BE. Telemedicine improves diagnosis of essential hypertension compared with usual care. J Telemed Telecare. (2002) 8:344–9. doi: 10.1258/135763302320939239
17. Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. (2020) 20:1193. doi: 10.1186/s12889-020-09301-4
18. Golinelli D, Boetto E, Carullo G, Nuzzolese AG, Landini MP, Fantini MP. Adoption of digital technologies in health care during the COVID-19 pandemic: systematic review of early scientific literature. J Med Internet Res. (2020) 22:e22280. doi: 10.2196/22280
19. Hau YS, Kim JK, Hur J, Chang MC. How about actively using telemedicine during the COVID-19 pandemic? J Med Syst. (2020) 44:108. doi: 10.1007/s10916-020-01580-z
20. Bokolo Anthony J. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. (2020) 44:132. doi: 10.1007/s10916-020-01596-5
21. Hua Q, Fan L, Li J. 2019 Chinese guideline for the management of hypertension in the elderly. J Geriat Cardiol JGC. (2019) 16:67. doi: 10.11909/j.issn.1671-5411.2019.02.001
22. Tan X, Liu X, Shao H. Healthy China 2030: a vision for health care. Value Health Reg Issues. (2017) 12:112–4. doi: 10.1016/j.vhri.2017.04.001
23. Omboni S, Sala E. The pharmacist and the management of arterial hypertension: the role of blood pressure monitoring and telemonitoring. Exp Rev Cardiovasc Ther. (2015) 13:209–21. doi: 10.1586/14779072.2015.1001368
24. Sharma A, Harrington RA, McClellan MB, Turakhia MP, Eapen ZJ, Steinhubl S, et al. Using digital health technology to better generate evidence and deliver evidence-based care. J Am Coll Cardiol. (2018) 71:2680–90. doi: 10.1016/j.jacc.2018.03.523
25. Al Hamarneh YN, Houle SK, Padwal R, Tsuyuki RT. Hypertension Canada's 2016 Canadian hypertension education program guidelines for pharmacists: an update. Can Pharm J. (2016) 149:337–44. doi: 10.1177/1715163516671747
26. Omboni S, Tenti M. Telepharmacy for the management of cardiovascular patients in the community. Trends Cardiovasc Med. (2019) 29:109–17. doi: 10.1016/j.tcm.2018.07.002
27. Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. (2006) 44:646–57. doi: 10.1097/01.mlr.0000220260.30768.32
28. Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. (2013) 310:46–56. doi: 10.1001/jama.2013.6549
29. Niznik JD, He H, Kane-Gill SL. Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: a systematic review. Res Soci Adm Pharm. (2018) 14:707–17. doi: 10.1016/j.sapharm.2017.10.011
30. Delage C, Lelong H, Brion F, Blacher J. Effect of a pharmacist-led educational intervention on clinical outcomes: a randomised controlled study in patients with hypertension, type 2 diabetes and hypercholesterolaemia. Eur J Hosp Pharm. (2021) 28:e197–202. doi: 10.1136/ejhpharm-2021-002787
31. Pihau-Tulo ST, Parsons RW, Hughes JD. An evaluation of patients' adherence with hypoglycemic medications among Papua New Guineans with type 2 diabetes: influencing factors. Patient Prefer Adherence. (2014) 8:1229–37. doi: 10.2147/PPA.S66655
32. Abughosh S, Wang X, Serna O, Esse T, Mann A, Masilamani S, et al. motivational interviewing intervention by pharmacy students to improve medication adherence. J Manag Care Spec Pharm. (2017) 23:549–60. doi: 10.18553/jmcp.2017.23.5.549
33. Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. (2006) 296:2563–71. doi: 10.1001/jama.296.21.joc60162
34. Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. (2002) 22:1533–40. doi: 10.1592/phco.22.17.1533.34127
35. Wong MC, Liu KQ, Wang HH, Lee CL, Kwan MW, Lee KW, et al. Effectiveness of a pharmacist-led drug counseling on enhancing antihypertensive adherence and blood pressure control: a randomized controlled trial. J Clin Pharmacol. (2013) 53:753–61. doi: 10.1002/jcph.101
36. Fogg A, Staufenberg EF, Small I, Bhattacharya D. An exploratory study of primary care pharmacist-led epilepsy consultations. Int J Pharm Pract. (2012) 20:294–302. doi: 10.1111/j.2042-7174.2012.00207.x
37. Chowdhury R, Khan H, Heydon E, Shroufi A, Fahimi S, Moore C, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. (2013) 34:2940–8. doi: 10.1093/eurheartj/eht295
Keywords: telemedicine medication management, usual care, hypertension management, COVID-19 pandemic, blood pressure
Citation: Li X, Hu J, Yao Y, Zuo C, Wang Z, Li X and Lv Q (2022) Evaluation of pharmacist-led telemedicine medication management for hypertension established patients during COVID-19 pandemic: A pilot study. Front. Public Health 10:1091484. doi: 10.3389/fpubh.2022.1091484
Received: 07 November 2022; Accepted: 30 November 2022;
Published: 16 December 2022.
Edited by:
Alexander Seifert, University of Zurich, SwitzerlandReviewed by:
Sadia Shakeel, DOW University of Health Sciences (DUHS), PakistanCopyright © 2022 Li, Hu, Yao, Zuo, Wang, Li and Lv. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoyu Li,  bGkueGlhb3l1QHpzLWhvc3BpdGFsLnNoLmNu; Qianzhou Lv,
bGkueGlhb3l1QHpzLWhvc3BpdGFsLnNoLmNu; Qianzhou Lv,  MTM5MTYwODg5MzhAMTYzLmNvbQ==
MTM5MTYwODg5MzhAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.