- 1Department of Epidemiology, School of Public Health, Iran University of Medical Sciences, Tehran, Iran
- 2Department of Epidemiology and Biostatistics, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
- 3Department of Health Education and Promotion, School of Health Isfahan University of Medical Sciences, Isfahan, Iran
- 4School of Public Health, Dezful University of Medical Science, Dezful, Khuzestan, Iran
- 5Department of Health Education and Promotion, School of Health, Iran University of Medical Sciences, Tehran, Iran
Background: Since the occurrence of the COVID-19 pandemic, information dissemination has increased rapidly. Promoting health literacy is currently crucial to prepare people to respond quickly to situations, such as the COVID-19 pandemic. Due to the importance of health literacy in this critical situation, we are looking for a questionnaire to measure COVID-19 health literacy. The COVID-19 Germany Health Literacy Questionnaire (HLS-COVID-Q22) is an excellent tool, so the study aimed to create a cultural validity of this questionnaire for the Iranian population.
Methods: In this validation study, 880 samples were enrolled using a convenient sampling method. The questionnaire was translated through a backward forwarding procedure. Confirmatory factor analysis (CFA) and exploratory factor analysis (EFA) were employed for Persian version validity. McDonald's omega (Ω), Cronbach's alpha, and average inter-item correlation (AIC) coefficients were assessed for reliability.
Results: Using EFA on the random half sample (n = 440), the EFA indicated that the scale had four factors: accessing, understanding, appraising, and applying health-related information in the COVID-19 pandemic context, which explained 59.3% of the total variance. CFA was used for the sample's second part (n = 440) to evaluate the goodness of fit of the four-factor solution. CFA showed the model fit. All indices RMSEA = 0.067, CFI = 0.934, IFI = 0.934, PCFI = 0.772, PNFI = 0.747, and CMIN/DF = 2.972 confirmed the model fit. The convergent validity of the HLS-COVID-Q22 was confirmed. McDonald's omega and Cronbach's alpha were very good (α and Ω >0.80).
Conclusion: The Persian version of the HLS-COVID-Q22 had acceptable psychometric properties and is applicable to measure COVID-19 health literacy.
Introduction
The COVID-19 pandemic has become one of the biggest challenges for healthcare systems around the world (1). Since the occurrence of the COVID-19 pandemic, information dissemination has increased rapidly (2). In February 2020, the World Health Organization (WHO) introduced the term infodemic to describe fake news and information related to the COVID-19 pandemic. Infodemic is a “global epidemic of misinformation spreading rapidly through social media platforms and other outlets”. It has a significant impact on the COVID-19 pandemic (3).
The WHO guidelines emphasize increasing health literacy (HL) among the general public around the world to prevent the spread of infection. The concept of HL is commonly used in health communication to educate people about health-related issues. It is defined as “the degree to which individuals have the ability to acquire, process, and understand basic health” (1). HL is currently considered a set of cognitive and social skills that not only motivate but also enable individuals to acquire and use valid health-related information to promote health (4). HL is an important issue in slowing down the spread of the virus and preventing the disease. Therefore, it has been established as the global strategy to fight the COVID-19 pandemic (5).
HL may help people to understand the reasons for the recommendations and the results of their various possible actions (6). Promoting HL is more important than ever to prepare people to respond quickly to situations, such as the COVID-19 pandemic (7). Therefore, a study indicated that people who have higher levels of HL tend to be better at managing their health than those people who do not. Higher levels of HL among people are associated with increased protection, a better quality of life, less variation in health outcomes, and a more stable and equal society. People who do not have good HL cannot distinguish between fact and fiction and are more influenced by unreliable facts (2). The European HL Survey, which was conducted in eight countries, found that almost 50% of all adults have “inadequate” HL; this means that it is potentially difficult for them to understand, evaluate, and apply information to promote or protect health. Past research has shown that low HL is associated with various adverse health outcomes (3, 4). A recent study on fear of COVID-19 in medical students has shown that higher levels of HL may lower the level of fear (5). In another study, higher HL levels have shown protective effects against COVID-19-related depression (6).
Emphasis on promoting personal, community, and population HL is very important during the COVID-19 pandemic (8) which is why there is a need to explore COVID-19-related HL. However, HL is ignored or misjudged (5).
Highlight the different aspects of HL in different populations during pandemics is necessary (9). Seng et al. emphasized that “understanding the levels and determinants of HL related to the epidemic in different populations is essential for healthcare policymakers and formulating optimal and effective strategies” (7). Due to the importance of HL in this critical situation, we are looking for a questionnaire to measure COVID-19 HL. Different questionnaires have been created to measure the HL of COVID-19, and most of the studies have used COVID-19 Germany HL Questionnaire (HLS-COVID-Q22) (8) and created their own suitable questionnaire.
HLS-COVID-Q22 covers four subscales including, appraising, understanding, applying, and health-related information, while other questioners do not have these four subscales (9). In contrast, the methods of confirming the validity and reliability of some questionnaires are not enough (10). In addition, the number of questions on some scales was too many (11), which was beyond the interest of people, and finally, after many reviews, the HLS-COVID-Q22 was selected. Since the language of Iranians is different from that of Germans, as well as the different cultures of the two countries, we intend to create a culture and validity of this questionnaire for the Iranian population.
Methods
Study design and sample size
The current cross-sectional research was performed from 7th to 19th August 2021 on adults (equal and older than 18 years) in Iran. Inclusion criteria included age older than 18 years, having the ability to read and write, having access to the internet, and having informed consent for participation in the study. A convenient sampling method was used for online data collection. The questionnaire was prepared through Google Forms and shared its URL link through social network channels and groups (WhatsApp, Telegram, and Instagram). We included 20 participants per question in the study. Finally, 440 samples for exploratory factor analysis (EFA) and another 440 samples for evaluation confirmatory factor analysis (CFA) were enrolled (12). We used the STROBE checklist (cross-sectional studies) as a guideline for writing this article.
Measurements
In this study, we used a two-part questionnaire. One section was related to demographic characteristics and the other section was the Persian version of COVID-19-related HL (HLS-COVID-Q22) (8). Demographic variables were age, marital status, gender, economic status, educational level, employment status, and residence.
HLS-COVID-Q22 contains 22 items with four subscales including, appraising (six items), understanding (six items), applying (five items), and health-related information (five items) in the COVID-19 pandemic context. The minimum score of this questionnaire is 22 and the maximum score is 88. The minimum and maximum average scores of this questionnaire are 1 and 4, respectively. A mean score of ≤ 2.5 indicates “inadequate HL”, a score of 2.5–3 indicates “problematic HL”, and a score of ≥3 indicates “sufficient HL” (8).
Translation process
Before starting this study, written permission from the questionnaire's developer, Professor Orkan Okan, was obtained through email. First, the translation of the questionnaire was done into Persian by two expert independent translators. Then, the translation of the two people was compared and corrected, and a Persian questionnaire was created. In the next step, this Persian questionnaire was translated into English by a third expert translator. Two English versions were reviewed and harmonized by the research team (13).
Face validity
Quantitative and qualitative approaches evaluated face validity. In the qualitative approach (14, 15), eight experts in health education and promotion, epidemiologist, and the instrument's development assessed the scale regarding relevancy, difficulty, and ambiguity, and all reported understandable items of the scale. In the quantitative approach, the same experts assessed the items regarding suitability by a Likert scale of five points (1 = not suitable at all, 2 = less suitable, 3 = almost suitable, 4 = suitable, and 5 = completely suitable). The following formula calculated the impact score: impact score (IS) = frequency (%) × suitability. A score of more than 1.5 was regarded as acceptable (16).
Content validity
For content validity, quantitative and qualitative methods were used. In the qualitative approach, eight experts in health promotion and education, epidemiologist, and the instrument's development evaluated the items regarding wording and grammar, scaling, and item allocation. Then, their feedback was used to modify some items. In the quantitative method, the content validity of the scale was assessed using modified kappa statistic (K*) and content validity ratio (CVR).
In CVR, questions were evaluated using a three-point Likert scale (3 = essential, 2 = useful but not essential, and 1 = not essential). The formula [ne – (N/2)]/(N/2) was used to calculate CVR in which “ne” indicates the number of experts rating the items as “essential” and “N” indicates the total number of experts. The Lawshe rule was applied to interpret the result. A minimum acceptable score of 0.75 was considered (17).
The chance agreement is not considered by content validity index (CVI). Therefore, K* as of the combined CVI and kappa was used to correct this index.
PC indicates the chance agreement presented by the below equation:
“N” indicates the number of experts and “A” indicates the number of experts approving the question's relevance. Regarding kappa interpretation, data of more than 0.75, 0.60–0.74, and 0.40–0.59 were excellent, good, and fair, respectively (18).
Construct validity
Exploratory (EFA) and confirmatory factor analysis (CFA) assessed the construct validity.
EFA
Sample size adequacy and appropriateness were checked by KMO and Bartlett's tests. The favorable KMO value is >0.70 (19). Scree plot, principal axis factoring (PAF) EFA, and ProMax rotation were used to extract latent factors. The minimum acceptance value for factor loading was determined by the CV value [CV = 5.152 ÷ √ (n – 2)]. CV is regarded as the minimum value that each question has to remain in a latent factor (20), where “n” is the sample size. Finally, in the present study, CV was calculated at 0.33. Finally, the criteria of factor extraction including eigenvalues (should be more than one), commonalities (h2, which is more than 0.3), and scree plots with factor loading were reported (21).
CFA
The confirmatory factor analysis tested the standard HLS-COVID-Q22 structure fit. For running the model, we use the Bootstrap method. Many fit indicators are available to determine the model's goodness of fit. The fitness of the model was evaluated considering the comparative fit index (CFI >95% good and >90% acceptable), root mean square of error of approximation (RMSEA < 0.05 good and < 0.08 acceptable), parsimonious comparative fit index (PCFI >0.5 good), incremental fit index (IFI >95% good and > 90% acceptable), parsimonious normed fit index (PNFI >0.5 good), and (CMIN/DF < 3 good and < 5 acceptable) (22, 23).
Univariate and multivariate normality and outliers
In this study, univariate distribution was assessed by the Kolmogorov–Smirnov test, skewness, and kurtosis. The cut-off values for skewness and kurtosis were considered 3 and 7, respectively (24). For checking the multivariate normality and outliers, Mardia's and Mahalanobis distance tests were used, respectively.
Convergent and divergent validity
The divergent and convergent validity were examined by evaluating Pearson's correlations between items and factors of the HLS-COVID-Q22. We calculated Pearson's correlation between items and hypothesized factors as convergent validity and Pearson's correlation between items and other scales as divergent validity. We used a strong correlation cut-off point (r) equal to 0.70. Values of >0.70 are considered excellent correlation, and convergent correlations should always be higher than discriminant ones (25). Furthermore, construct reliability (CR), average variance extracted (AVE), and maximum shared variance (MSV) were reported. For convergent validity, CR must be greater than AVE and AVE of >0.5 (26). In divergent validity, MSV must be lower than AVE (27).
Reliability
McDonald's omega (Ω), Cronbach's alpha, and average inter-item correlation (AIC) coefficients were applied for checking the reliability (28). According to the general rule of thumb, Cronbach's alpha equal to 0.70 and higher is considered good, 0.80 and higher is considered better, and 0.90 and higher is considered best (29). As for Cronbach's alpha, McDonald's Omega of >0.80 is regarded as good internal reliability (30). The mean inter-item correlation for some items should be from 0.20 to 0.40, which suggests that the items are reasonably homogenous and have sufficiently unique variance so that they are not identical to each other (31). SPSS, https://webpower.psychstat.org/models/kurtosis, and AMOS version 22 were applied for statistical analyses.
Ethics
The proposal of this research was confirmed by the Ethics Committee of Isfahan University of Medical Sciences with code IR.MUI.RESEARCH.REC.1400.194. The subjects have completed a written informed consent form at the beginning of the questionnaire URL link.
Results
Participant characteristics
The participants' mean age was 31.09 ± 11.37 years. The majority of the participants were female (62.0%), single (56.1%), had a university education (81.1%), and were quiet in the city (94.0%). Approximately 60% of them had Fars ethnicity, 26.4% were students, and 31.9% had incomes of more than 400 dollars per month. The individuals' characteristics included in the AFA and CFA are provided separately in Table 1.
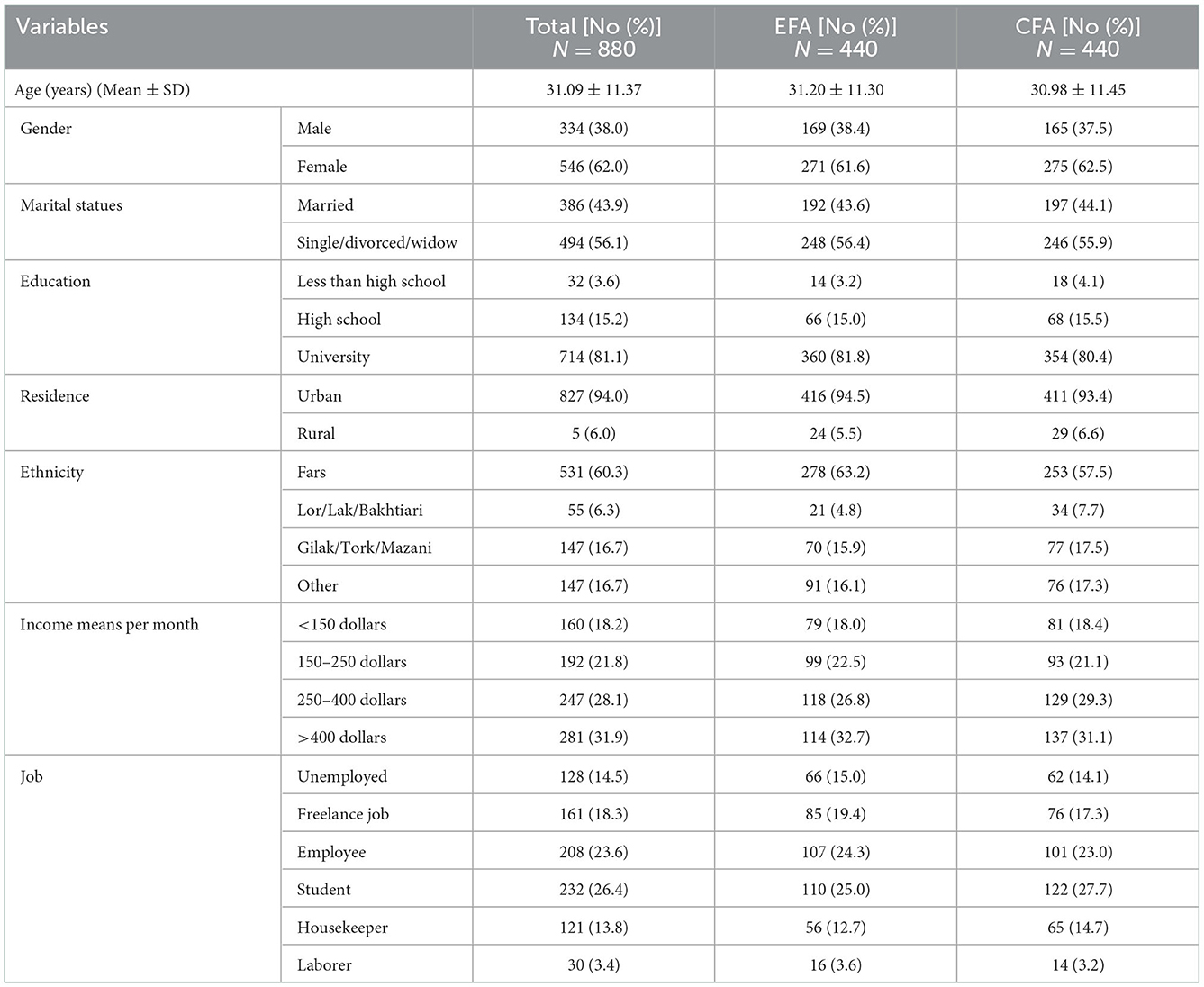
Table 1. Participant characteristics in the study in two exploratory (EFA) and confirmatory factor analysis (CFA) (n = 880).
Face validity
In the qualitative phase, the importance and wording of all questions were assessed and some modifications were made. There was no question with IS of smaller than 1.5 (Appendix Table 2).
Content validity
Modifications were made based on the opinions of the experts. The CVI, K*, and CVR for each question are shown in Appendix Table 2. All values were acceptable.
EFA
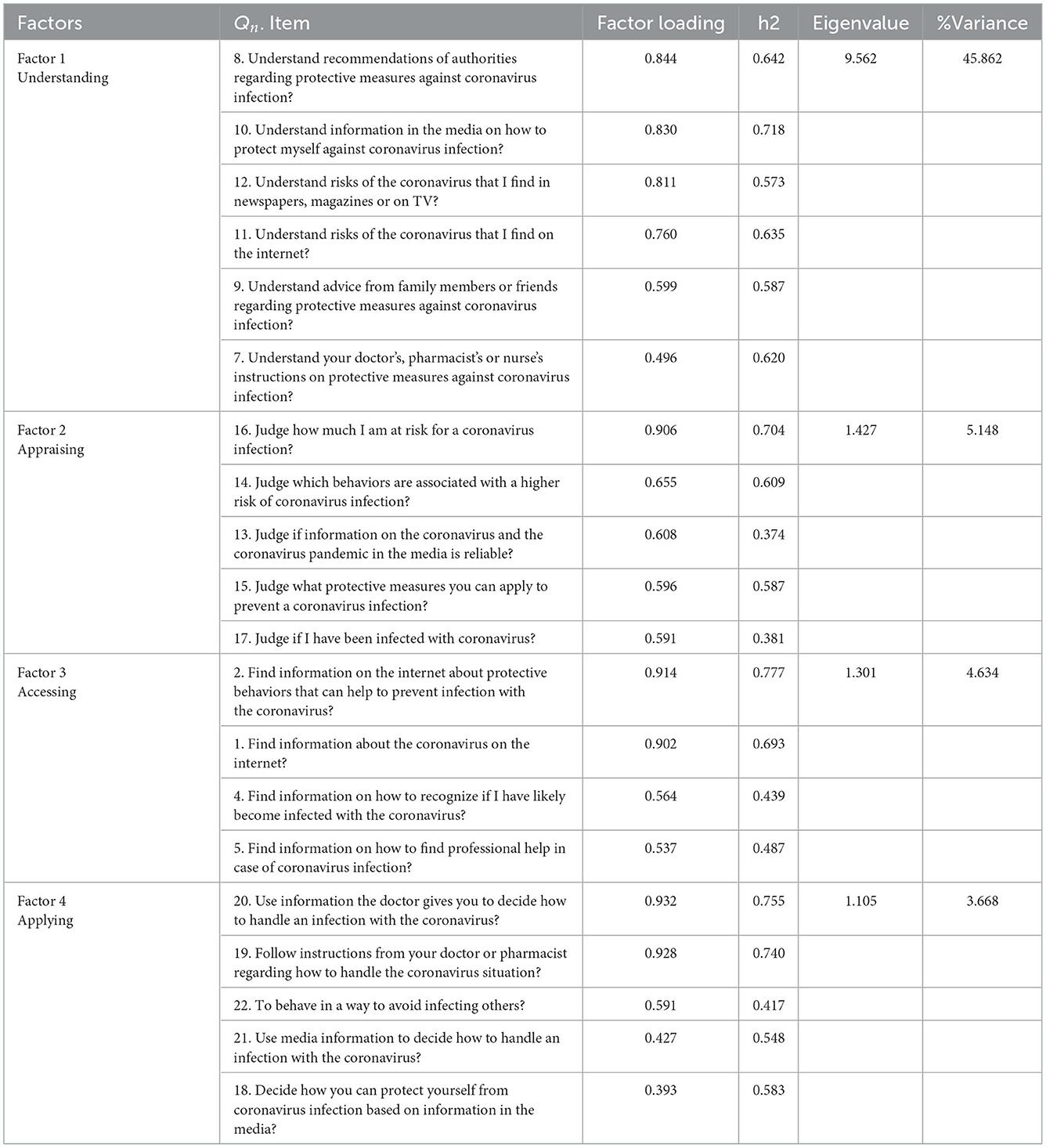
The KMO test value was 0.935, which showed sampling adequacy. Using PAF and ProMax rotation, four factors (accessing, understanding, appraising, and applying health-related information in the COVID-19 pandemic context) were extracted and explained 59.3% of the total variance (Table 2). In this model, four factors were extracted based on eigenvalues >1 (Table 2). Items 3 and 6 were removed due to cross-loading. Twenty items remained in the model because their factor load was >0.33. Eigenvalues, h2, and factor loading values are presented in Table 2.
CFA
To assess the best of fit of the factor structure of the 20-item COVID-19 HL scale, the chi-square goodness-of-fit test was evaluated (χ2 = 466.545, df = 157, n = 440, p < 0.0001) (Appendix Figure 1). Moreover, the fit of the model was examined by other indicators. All indices, such as RMSEA = 0.067, CFI = 0.934, IFI = 0.934, PCFI = 0.772, PNFI = 0.747, and CMIN/DF = 2.972, confirmed the model fit.
Tests for normality and outliers
The Kolmogorov–Smirnov test was significant which shows data has no normality. None of the data has univariate skewness and kurtosis (skewness < 3 and kurtosis < 7). However, in the assessment of Mardia's test, multivariate skewness and kurtosis were observed (p < 0.001) (Appendix Table 1).
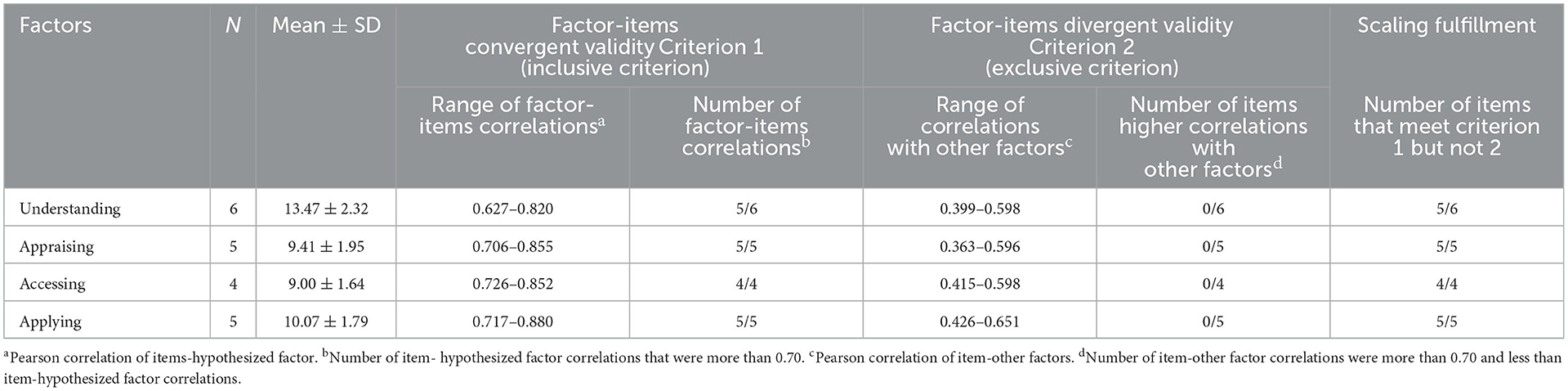
Convergent and divergent validity
The minimum and maximum range of item-factor correlation (hypothesized and other factors) showed in Table 3. All of the item-hypothesized factor correlations were >0.70. The minimum and maximum range of convergent correlations of all factors were higher than the discriminant correlation ranges (Table 3). Appendix Table 3 shows AVE for all factors. Except for the appraising factor, AVE was >0.5, and for all factors, CR was greater than AVE, indicating acceptable convergent validity. In contrast, MSV was greater than AVE for all factors, indicating a lack of divergent validity. However, divergent validity was established using the correlation method. Overall, the convergent validity of the HLS-COVID-Q22 was confirmed.
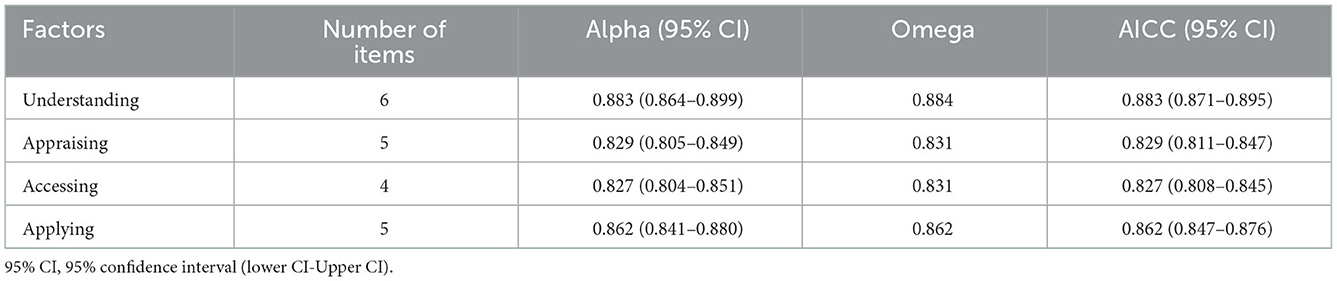
Reliability
According to McDonald's omega and Cronbach's alpha, the reliability of this questionnaire was very good (α and Ω > 0.80). The details of reliability are presented in Table 4.
Discussion
In this study, the four factors (understanding, appraising, applying, and health-related information in the COVID-19 pandemic context) extracted by exploratory factor analysis explained more than 59% of the variance. This study removed two items (items 3 and 6) due to cross-loading. The fitness indicators approved the construct of HLS-COVID-Q22.
The original version of HLS-COVID-Q22 (8) identified four factors with 22 items but this study identified four factors with 20 items. The four domains were the same in the two studies.
The definition of individuals' ability to deal with health information has changed. It emerged from referring to some technical skills applied, such as understanding, accessing, appraising, and applying health-related information (32). The present questionnaire has extracted all these skills in its factor analysis.
The first factor identified in the EFA was “understanding.” This item introduces approximately 45% of the total variance. The capability approach highlights the importance of “understanding” (33). This approach introduces the available resources as one of the essential preconditions for the potential to do actions. One of the most important conditions for turning such resources into the actions required to achieve the goal is the individual's understanding of these resources (34, 35). Our goal during the COVID-19 pandemic is to break the chain of transmission (36). Personal protective equipment, such as masks, disinfectants, physical distancing, and vaccines, are our resources, and people's understanding of these cases will lead to action, breaking the chain.
The potential to educate and guide individuals in the process of appraising health information is very important in the COVID-19 pandemic. Appraising ability can help people to identify information containing poor-quality arguments (false, irrelevant, or manipulative) (37). This subscale constitutes about 5% of the total variance in EFA in the current study.
The issue of access to HL is very important. With the spread of mobile phones, access to health-related information on the Internet has become more important. Older cases, as well as people who earn minimum wage or less, are less likely to have such devices (38). In addition, for people who can access digital media, there are other barriers, such as the requirement for a high level of general literacy to realize the content (39). Medical jargon and jargon, dense paragraphs, difficult formatting, and specialized language are barriers for cases that have limited HL (40).
The capability to use and process the information to guide health actions is an essential component of HL (41). A person with good health-related literacy knows when and where to search for, find, and retrieve printed data, as well as who to contact for information advice. It is very important to apply the information in making decisions at the individual and/or societal level (41).
Understanding other domains, such as appraising, applying, and information, is an appropriate tool for HL. One of the most important strengths of this questionnaire is that its questions measure both HL and electronic HL (eHL) (42). eHL and HL are crucial for decreasing the virus spread and mitigating its effect through making informed decisions regarding how to prevent and address the disease (35). HL is a social vaccine making individuals and communities able to mitigate the virus spread by using and understanding the information offered by governments and health authorities. This vaccine can be used similarly to biomedical vaccines to prevent infection from COVID-19 (43).
Despite the widespread injection of the COVID-19 vaccine in several doses and the emergence of various strains of the virus, the COVID-19 pandemic status is still present (44). This proves that other extensive and parallel interventions must perform to be able to complement the biological vaccine's effect (43). After more than 2 years of the pandemic, protocol compliance has declined. Many people, for various reasons, refuse to follow the protocols, causing the virus to spread in society and pandemics to remain dynamic (45, 46). Perhaps part of this is related to the infodemic (47). This misinformation is spread among the people and the people act far from the truth (48). HL and eHL play an important role in COVID-19 pandemic control by improving individuals' access to true health information and their ability to use it effectively (43).
Limitations
Our most important limitation was using the self-report method leading to errors in the reports. Our sample was limited to people with Internet access and may not be representative of all Iranian people. Therefore, the study's findings should be generalized with caution. Another limitation is the lake of divergent validity based on MSV and AVE.
Strengths of the study
This is the first study to accurately investigate the psychometric properties of the HL instrument in Iran. Strong methodology and analysis were performed in the study is an important positive point. Dealing with all aspects of validity and reliability is one of the other points.
Conclusion
The Persian version of the HLS-COVID-Q22 scale can be an acceptable tool. Because of the characteristics, such as simple scoring, proper reliability, and validity, being answered in a short period, the questionnaire is an appropriate instrument.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Isfahan University of Medical Sciences with code IR.MUI.RESEARCH.REC.1400.194. The patients/participants provided their written informed consent to participate in this study.
Author contributions
ST, MM, and FE conceived the presented idea. ST, RR, ME, and FE contributed to the data gathering. ST and MM performed the analysis. ST and HS wrote the first draft. All authors discussed the results and contributed to the final manuscript.
Acknowledgments
We would like to acknowledge the Isfahan University of Medical Sciences for supporting this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1085861/full#supplementary-material
References
1. Nutbeam D. The evolving concept of health literacy. Soc Sci Med. (2008) 67:2072–8. doi: 10.1016/j.socscimed.2008.09.050
2. Spring H. Health literacy and COVID-19. Health Info Libr J (2020) 37:171–2. doi: 10.1111/hir.12322
3. Berkman ND, Sheridan SL., Donahue KE, Halpern DJ, Viera A, Crotty K, et al. Health literacy interventions and outcomes: an updated systematic review Evidence report/technology assessment. Evid Rep Technol Assess. (2011) 199:1–941. doi: 10.7326/0003-4819-155-2-201107190-00005
4. Sørensen K, Pelikan JM, Röthlin F, Ganahl K, Slonska Z, Doyle G, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health. (2015) 25:1053–8. doi: 10.1093/eurpub/ckv043
5. Nguyen HT, Do BN, Pham KM, Kim GB, Dam HT, Nguyen TT, et al. Fear of COVID-19 scale—associations of its scores with health literacy and health-related behaviors among medical students. Int J Environ Res Public Health. (2020) 17:4164. doi: 10.3390/ijerph17114164
6. Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TT, Pham KM, et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J Clin Med. (2020) 9:965. doi: 10.3390/jcm9040965
7. Seng JJB, Yeam CT, Huang CW, Tan NC, Low LL. Pandemic related Health literacy–A Systematic Review of literature in COVID-19, SARS and MERS pandemics. Medrxiv. (2020). doi: 10.1101/2020.05.07.20094227
8. Okan O, Bollweg TM, Berens E-M, Hurrelmann K, Bauer U, Schaeffer D. Coronavirus-related health literacy: A cross-sectional study in adults during the COVID-19 infodemic in Germany. Int J Environ Res Public Health. (2020) 17:5503. doi: 10.3390/ijerph17155503
9. Çeviker SA, Akkaya B, Akar SS. COVID-19 Health Literacy Scale Development. Int Health Trends Perspect. (2022) 2:67–79. doi: 10.32920/ihtp.v2i1.1509
10. Savci C, Zengin N, Akinci AC. Development of the Health Literacy Scale for Protection Against COVID-19. Electron J Gener Med. (2021) 18:em332. doi: 10.29333/ejgm/11319
11. Sanaeinasab H, Saffari M, Rashidi-Jahan H, Rahmati F, Koenig H, Lin C-Y, et al. Development and psychometric assessment of the COVID-19 health literacy scale: preliminary testing and factor structure. J Health Liter. (2022) 6:32–46. doi: 10.22038/jhl.2021.61484.1238
13. Ozolins U, Hale S, Cheng X, Hyatt A, Schofield P. Translation and back-translation methodology in health research–a critique. Expert Rev Pharmacoecon Outcomes Res. (2020) 20:69–77. doi: 10.1080/14737167.2020.1734453
14. Mazloomy Mahmoodabad SS, Sadeghi R, Fallahzadeh H, Rezaeian M, Bidaki R, Khanjani N. Validity and reliability of the preventing hookah smoking (PHS) questionnaire in adolescents based on the protection motivation theory. Int J Pediatr. (2018) 6:8327–37.
15. Al-Dhaqm A, Razak S, Ikuesan RA. R., Kebande V, Hajar Othman S. Face validation of database forensic investigation metamodel. Infrastructures. (2021) 6:13. doi: 10.3390/infrastructures6020013
16. Ebadi A, Zarshenas L, Rakhshan M, Zareiyan A, Sharifnia S, Mojahedi M. Principles of Scale Development in Health Science. Tehran: Jame-e-negar (2017).
17. Ayre C, Scally AJ. Critical values for Lawshe's content validity ratio: revisiting the original methods of calculation. Measur Eval Counsel Dev. (2014) 47:79–86. doi: 10.1177/0748175613513808
18. Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. Am J Ment Defic. (1981) 86:127–37.
19. Aslan H, Aktürk Ü, Erci B. Validity and reliability of the Turkish version of the nurse spiritual care therapeutics scale. Palliat Support Care. (2020) 18:707–12. doi: 10.1017/S1478951520000267
20. Goudarzian AH, Sharif Nia H, Harry KM, Jannati Y. Assessment of the psychometric properties of the persian version of the Cardiac Self-Blame Attribution (CSBA-P) scale in patients with cardiovascular disease. OMEGA-J Death Dying. 2020:0030222820947224. doi: 10.1177/0030222820947224
21. Guad RM, Mangantig E, Low WY, Taylor-Robinson AW, Azzani M, Sekaran SD, et al. Development and validation of a structured survey questionnaire on knowledge, attitude, preventive practice, and treatment-seeking behaviour regarding dengue among the resident population of Sabah, Malaysia: an exploratory factor analysis. BMC Infect Dis. (2021) 21:1–11. doi: 10.1186/s12879-021-06606-6
22. Gaskination's StatWiki CFA (2020). Available from: http://statwiki.gaskination.com/index.php?title=CFA#Measurement_Model_Invariance (accessed on April 9, 2021).
23. Brown TA. Confirmatory Factor Analysis for Applied Research. New York, NY: Guilford publications (2015).
24. Rozenberg R, Thornhill RE, Flood TA, Hakim SW, Lim C, Schieda N. Whole-tumor quantitative apparent diffusion coefficient histogram and texture analysis to predict Gleason score upgrading in intermediate-risk 3+ 4= 7 prostate cancer. Am J Roentgenol. (2016) 206:775–82. doi: 10.2214/AJR.15.15462
25. Campbell DT, Fiske DW. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol Bull. (1959) 56:81. doi: 10.1037/h0046016
26. Shrestha N. Factor analysis as a tool for survey analysis. Am J Appl Math Stat. (2021) 9:4–11. doi: 10.12691/ajams-9-1-2
27. Afework T, Wondimagegnehu A, Alemayehu N, Kantelhardt EJ, Addissie A. Validity and reliability of the Amharic version of supportive care needs survey-short form 34 among cancer patients in Ethiopia. BMC Health Serv Res. (2021) 21:1–10. doi: 10.1186/s12913-021-06512-2
28. Ercan I, Yazici B, Sigirli D, Ediz B, Kan I. Examining Cronbach alpha, theta, omega reliability coefficients according to sample size. J Modern Appl Stat Methods. (2007) 6:27. doi: 10.22237/jmasm/1177993560
29. Punyasettro S, Wangwongwiroj T, Yasri P. An Assessment Tool for Measuring Learners' Self-Efficacy. Psychol Educ J. (2021) 58:104–10. doi: 10.17762/pae.v58i4.4500
30. Feißt M, Hennigs A, Heil J, Moosbrugger H, Kelava A, Stolpner I, et al. Refining scores based on patient reported outcomes–statistical and medical perspectives. BMC Med Res Methodol. (2019) 19:1–9. doi: 10.1186/s12874-019-0806-9
31. Denis F, Rouached I, Siu-Paredes F, Delpierre A, Amador G, El-Hage W, et al. Psychometric properties of the schizophrenia oral health profile: preliminary results. Int J Environ Res Public Health. (2021) 18:9090. doi: 10.3390/ijerph18179090
32. Diviani N. On the centrality of information appraisal in health literacy research. HLRP: Health Liter Res Pract. (2019) 3:e21–e4. doi: 10.3928/24748307-20181214-01
33. Robeyns I. Capability approach. Handbook of Economics and Ethics. Cheltenham, United Kingdom: Edward Elgar Publishing (2009).
34. Diener E. The Science of Well-Being: The Collected Works of Ed Diener. Berlin, Germany: Springer (2009).
35. Falk Erhag H, Lagerlöf Nilsson U, Rydberg Sterner T, Skoog I. A Multidisciplinary Approach to Capability in Age and Ageing. Berlin, Germany: Springer Nature (2022). p. 70.
36. WHO. Breaking the chain of COVID-19 transmission: the key role of Camp-wise Rapid Investigation and Response Teams. (2020). Available online at: https://www.who.int/bangladesh/news/detail/10-11-2020-breaking-the-chain-of-covid-19-transmission-the-key-role-of-camp-wise-rapid-investigation-and-response-teams (accessed November 10, 2020).
37. Rubinelli S, Ort A, Zanini C, Fiordelli M, Diviani N. Strengthening critical health literacy for health information appraisal: an approach from argumentation theory. Int J Environ Res Public Health. (2021) 18:6764. doi: 10.3390/ijerph18136764
38. Smith B, Magnani JW. New technologies, new disparities: the intersection of electronic health and digital health literacy. Int J Cardiol. (2019) 292:280–2. doi: 10.1016/j.ijcard.2019.05.066
39. Janiak E, Rhodes E, Foster AM. Translating access into utilization: lessons from the design and evaluation of a health insurance Web site to promote reproductive health care for young women in Massachusetts. Contraception. (2013) 88:684–90. doi: 10.1016/j.contraception.2013.09.004
40. Thies K, Anderson D, Cramer B. Lack of adoption of a mobile app to support patient self-management of diabetes and hypertension in a federally qualified health center: interview analysis of staff and patients in a failed randomized trial. JMIR Human Factors. (2017) 4:e7709. doi: 10.2196/humanfactors.7709
41. Liu C, Wang D, Liu C, Jiang J, Wang X, Chen H, et al. What is the meaning of health literacy? A systematic review and qualitative synthesis. Family Med Commun Health. (2020) 8:e000351. doi: 10.1136/fmch-2020-000351
42. Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res. (2006) 8:e507. doi: 10.2196/jmir.8.4.e27
43. Okan O, Messer M, Levin-Zamir D, Paakkari L, Sørensen K. Health literacy as a social vaccine in the COVID-19 pandemic. Health Promot Int. (2022). doi: 10.1093/heapro/daab197
44. Khandia R, Singhal S, Alqahtani T, Kamal MA, Nahed A, Nainu F, et al. Emergence of SARS-CoV-2 Omicron (B. 1.1. 529) variant, salient features, high global health concerns and strategies to counter it amid ongoing COVID-19 pandemic. Environ Res. (2022) 2022:112816. doi: 10.1016/j.envres.2022.112816
45. Cartaud A, Quesque F, Coello Y. Wearing a face mask against Covid-19 results in a reduction of social distancing. PLoS ONE. (2020) 15:e0243023. doi: 10.1371/journal.pone.0243023
46. Abeya SG, Barkesa SB, Sadi CG, Gemeda DD, Muleta FY, Tolera AF, et al. Adherence to COVID-19 preventive measures and associated factors in Oromia regional state of Ethiopia. PLoS ONE. (2021) 16:e0257373. doi: 10.1371/journal.pone.0257373
47. Siebenhaar KU, Köther AK, Alpers GW. Dealing with the COVID-19 infodemic: Distress by information, information avoidance, and compliance with preventive measures. Front Psychol. (2020) 2020:2981. doi: 10.3389/fpsyg.2020.567905
Keywords: COVID-19, psychometric, health literacy, transcultural, validation
Citation: Torkian S, Ebrahimi F, Shahnazi H, Rashti R, Emami M and Maracy MR (2023) Psychometrics of the Persian version of the COVID-19-related health literacy in the Iranian population. Front. Public Health 10:1085861. doi: 10.3389/fpubh.2022.1085861
Received: 31 October 2022; Accepted: 13 December 2022;
Published: 10 January 2023.
Edited by:
Ihua Chen, Qufu Normal University, ChinaReviewed by:
Chunyu Zhang, Guangxi Normal University, ChinaIvan Santolalla Arnedo, University of La Rioja, Spain
Copyright © 2023 Torkian, Ebrahimi, Shahnazi, Rashti, Emami and Maracy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammad Reza Maracy,  bWFyYWN5QG1lZC5tdWkuYWMuaXI=
bWFyYWN5QG1lZC5tdWkuYWMuaXI=
†ORCID: Samaneh Torkian orcid.org/0000-0002-7913-2801
Fatemeh Ebrahimi orcid.org/0000-0002-0360-9730
Hossein Shahnazi orcid.org/0000-0002-5901-3901
Roya Rashti orcid.org/0000-0002-6408-9759
Mahasti Emami orcid.org/0000-0002-8204-6218
Mohammad Reza Maracy orcid.org/0000-0002-3695-0863
 Samaneh Torkian
Samaneh Torkian Fatemeh Ebrahimi2†
Fatemeh Ebrahimi2† Hossein Shahnazi
Hossein Shahnazi Roya Rashti
Roya Rashti Mahasti Emami
Mahasti Emami Mohammad Reza Maracy
Mohammad Reza Maracy