- 1Business School, University of Shanghai for Science and Technology, Shanghai, China
- 2Emergency Management Office, Shanghai Municipal Center for Disease Control and Prevention, Shanghai, China
Introduction: In 2020, the COVID-19 epidemic swept the world, and many national health systems faced serious challenges. To improve future public health responses, it's necessary to evaluate the performance of each country's health system.
Methods: We developed a resilience evaluation system for national health systems based on their responses to COVID-19 using four resilience dimensions: government governance and prevention, health financing, health service provision, and health workers. We determined the weight of each index by combining the three-scale and entropy-weight methods. Then, based on data from 2020, we used the Technique for Order of Preference by Similarity to Ideal Solution (TOPSIS) method to rank the health system resilience of 60 countries, and then used hierarchical clustering to classify countries into groups based on their resilience level. Finally, we analyzed the causes of differences among countries in their resilience based on the four resilience dimensions.
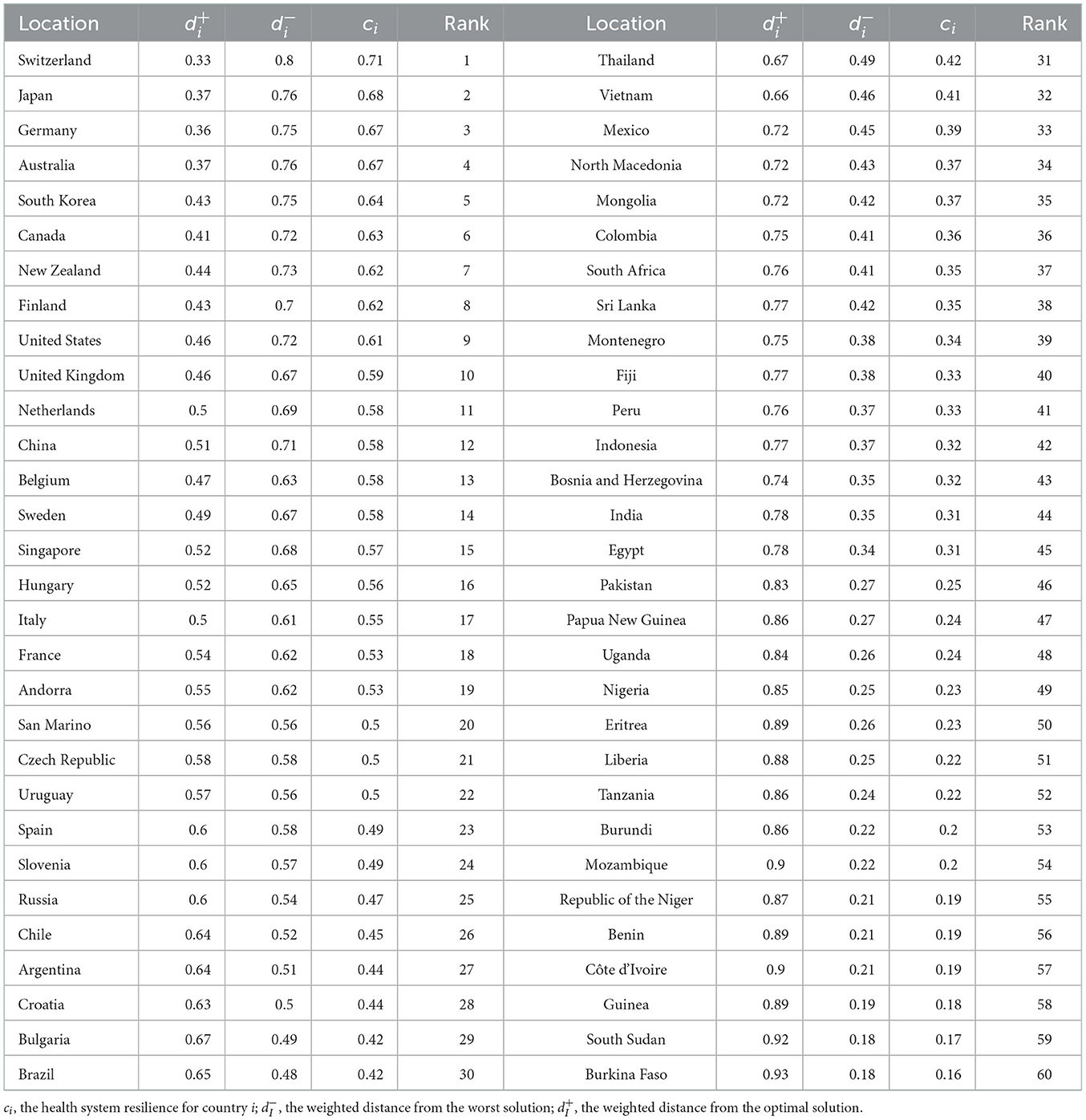
Results: Switzerland, Japan, Germany, Australia, South Korea, Canada, New Zealand, Finland, the United States, and the United Kingdom had the highest health system resilience in 2020. Eritrea, Nigeria, Libya, Tanzania, Burundi, Mozambique, Republic of the Niger, Benin, Côte d'Ivoire, and Guinea had the lowest resilience.
Discussion: Government governance and prevention of COVID-19 will greatly affect a country's success in fighting future epidemics, which will depend on a government's emergency preparedness, stringency (a measure of the number and rigor of the measures taken), and testing capability. Given the lack of vaccines or specific drug treatments during the early stages of the 2020 epidemic, social distancing and wearing masks were the main defenses against COVID-19. Cuts in health financing had direct and difficult to reverse effects on health systems. In terms of health service provision, the number of hospitals and intensive care unit beds played a key role in COVID-19 clinical care. Resilient health systems were able to cope more effectively with the impact of COVID-19, provide stronger protection for citizens, and mitigate the impacts of COVID-19. Our evaluation based on data from 60 countries around the world showed that increasing health system resilience will improve responses to future public health emergencies.
1. Introduction
The COVID-19 outbreak in 2019 was a global pandemic caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) (1). As of 14 April 2022, the World Health Organization (WHO) reported 500.2 million confirmed cases and 6.19 million COVID-19 deaths worldwide (2). In the early stages of the response to COVID-19, the performance of the health systems of different countries varied significantly.
Italy was the first European country to respond to the COVID-19 outbreak (3). They experienced a high mortality rate due to the aging of their population, and the large and increasing number of patients overwhelmed the health system. As of 17 March 2020, the overall mortality rate of confirmed COVID-19 patients in Italy had reached 7.2% (1625 deaths / 22512 cases), which was much higher than the 2.3% rate in China (4, 5). The United States was one of the most strongly affected countries (6). Although the United States has a robust and diverse, high-quality health system, the demand for hospital resources far exceeded the hospital capacity in many areas (7, 8). For example, on 10 April 2020, the demand for intensive care unit (ICU) beds in New York was 8,380, but only 718 beds were available. France was one of the most strongly affected European countries due to the limited number of ICU beds and a severely under-prepared health system (9, 10). As of 27 October 2020, the number of COVID-19 deaths reached 35,018 (11). The performance of these health systems in responding to COVID-19 was far below the level their health systems should have been able to attain.
In contrast, the health systems of several countries performed relatively well in responding to COVID-19. China was the first country to face the COVID-19 outbreak, but it took swift and effective measures to control the first wave of the outbreak. At the same time, it continued to donate medical supplies to countries around the world to help them combat the epidemic. Exports of critical supplies grew from 12.6% of the total global trade in these supplies in 2019 to 26.7% in 2020, ranking first in the world and 2.3 times that of the United States, which ranked second (12). Uruguay excelled in testing, and was one of the first countries to adopt contact tracing (13). It tested an average of 233.7 people per confirmed case of COVID-19, vs. only 1.7 in Argentina, 1.9 in Mexico, and 3.0 in Colombia (14). The rapid and effective measures taken by the Vietnamese government were recognized by international organizations (15). Through early risk assessment, timely emergency response policies, and immediate actions taken by government departments, the domestic epidemic was controlled at a very low level, which greatly alleviated the impact on the health system.
The performance of countries in responding to COVID-19 varied greatly. What factors led to such a wide variation in the performance of health systems? In this paper, we examine the health systems of 60 representative countries around the world. We constructed an evaluation system from the perspective of resilience, and used it to evaluate the performance of health systems based on their response to COVID-19 in 2020. We then explore the causes of the differences to provide policy suggestions for countries that will improve their response to future public health emergencies.
The concept of resilience originates from the Latin word resillo, which is translated as “elasticity”. The earliest disciplinary definition of resilience comes from ecology (16). It has been gradually applied to many fields such as engineering and psychology. In all these different disciplines, the main concept of resilience reflects the ability of an individual, group, or system to absorb shocks while still maintaining its basic functions in or near their original state (17). Resilience is a relatively new concept in the context of health systems. Health system resilience refers to the ability of a health system to maintain its core system functions when a crisis hits, to respond effectively to the crisis, and to improve and upgrade the system based on the lessons learned during the crisis (18). Since the end of the 20th century, the need to build resilient health systems has gradually become one of the core issues discussed in the World Health Report (19). Health system resilience is an important element of system adaptability, responsiveness, and stability, so it is critical for countries to learn from their response to COVID-19 and build a more resilient system (20, 21).
When we reviewed previous studies, we found that the concept of resilience has been applied to health system evaluations. Among this research, Ammar et al. (22) used a case study approach to examine health system resilience in Lebanon under the impact of the Syrian refugee crisis. Ling et al. (23) assessed health system resilience in Liberia during the Ebola crisis using semi-structured interviews and focus group discussions to support thematic analysis. Watts et al. (24) quantitatively assessed health system resilience in 101 countries by conducting a national survey in the context of climate change. Haldane et al. (25) used a new health systems resilience framework to qualitatively analyze the response to COVID-19 in 28 countries; they summarized four important elements of an effective national response, and made recommendations accordingly. By reviewing the literature, we found that analysis of health system resilience in response to emergencies is extremely important, and especially quantitative analysis, which can reflect the problem more intuitively. However, there is a lack of quantitative analysis on health system resilience based on the responses to COVID-19, and this has prevented us from attaining a comprehensive understanding of the response of each country. How to quantitatively analyze health system resilience in this context was therefore the focus of this paper.
In 2020, COVID-19 had a severe impact on the health system of each country. This provided a unique opportunity to assess health system resilience around the world. To quantify the health system response to COVID-19, we need to develop a quantitative evaluation system. In the present study, we rethought the WHO assessment framework for resilience and explored relevant evaluation indicators to more accurately assess the actual situation. The WHO framework consists of six components: leadership and governance, health financing, health information systems, medical technologies and products, health service provision, and the health workforce (26). As COVID-19 has been a public health emergency, government information is critical, so we combined the leadership and governance component with the health information systems component to produce a single composite government governance and prevention component. In addition, at the beginning of the epidemic in 2020, most countries had no specific drugs available to treat COVID-19 and no vaccines, and medical knowledge, technologies, and products for COVID-19 treatment were not mature, and did not differ greatly among countries, so we did not account for medical technologies and products (27, 28). Governance is not effective if there is no money to pay for health workers, medicines, and hospitals, and none of the factors can help if there is no access to them. We therefore added health financing and access to healthcare as key dimensions. Finally, because infected patients must be cared for and treated, the health workforce was clearly essential and became our final dimension. To accurately and objectively describe the real situation in each country, we defined our new assessment framework based on the abovementioned four dimensions: government governance and prevention, health financing, health service provision, and health workers. Technique for Order of Preference by Similarity to Ideal Solution (TOPSIS) method is a commonly used comprehensive evaluation method, which can make full use of the information of the original data, and its results can accurately reflect the gap between the evaluation schemes. Silva Araujo et al. used TOPSIS method to analyze the performance of the Brazilian public health system (29). We used this approach to assess differences in health system resilience in response to COVID-19 across countries.
2. Materials and methods
2.1. Study area and data sources
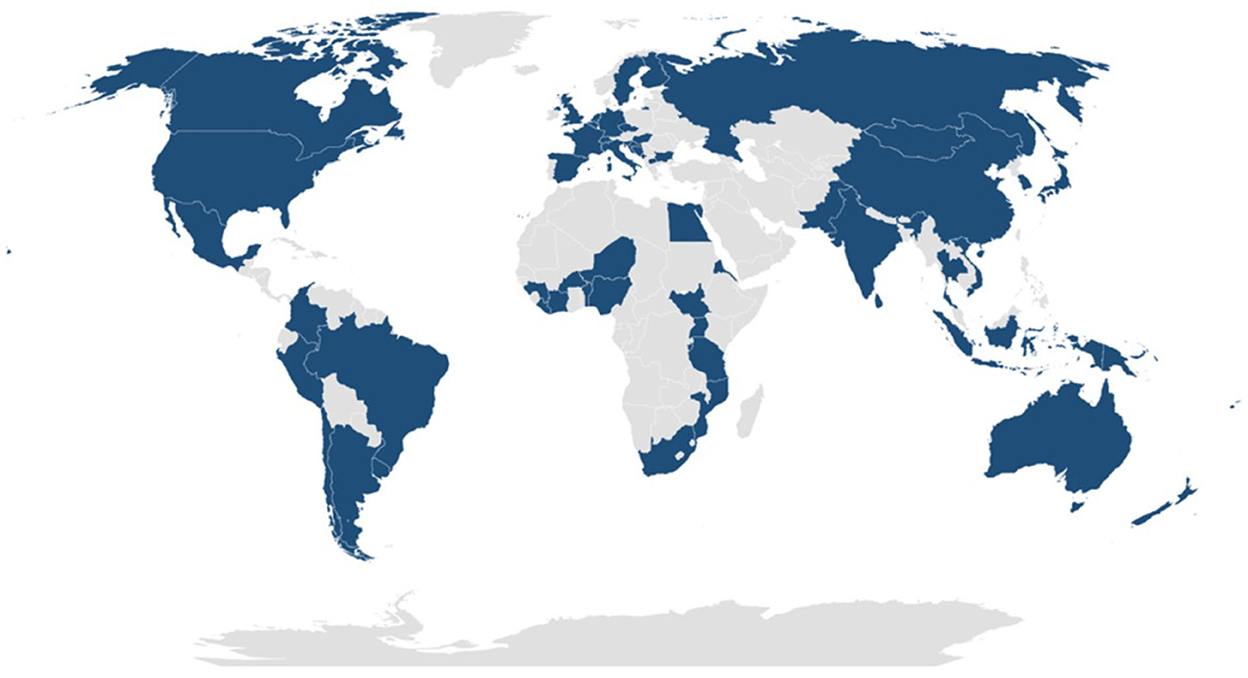
To provide coverage of the overall global situation in 2020, we sampled the 20 countries with the highest number of COVID-19 deaths per million citizens, the 20 countries with the lowest number of deaths, and 20 countries from different regions with intermediate death tolls and with large populations and very different health systems (Figure 1). We excluded the Middle East region because death tolls were confounded by ongoing war and by a lack of reliable statistics. The selected countries have a total population of 5.633 billion people, which represented 74.3% of the total global population in 2020; a land area of 83,470,400 km2, accounting for 61.4% of the total land area of all countries; and a total GDP of US$80.7 trillion in 2020, which amounted to 94.5% of the total global GDP (30).
We obtained indicator data from the latest publicly available datasets and databases produced by international organizations (WHO, the World Bank, specialized agencies of the United Nations, non-profit organizations, the Oxford COVID-19 Government Response Tracker, and the COVID-19 Regional Security Assessment Security Committee). Supplementary Table 1 describes the indicators and data sources.
2.2. Methods
TOPSIS method, developed by Hwang and Yoon in 1981, uses the concept of positive and negative ideal solutions as a reference for estimating and ranking performance in units of analysis (31). The method of ranking according to the degree of proximity between a finite number of evaluation objects and the idealized target is to evaluate the relative merits and demerits of the existing objects. The ranking is carried out by detecting the distance between the evaluation object and the optimal solution and the worst solution. If the evaluation object is closest to the optimal solution and farthest from the worst solution, it is the best. Otherwise, it is not optimal. Each index value of the optimal solution reaches the optimal value of each evaluation index. Each index value of the worst solution reaches the worst value of each evaluation index (32). TOPSIS method has strong objectivity, avoids the interference of subjective factors, and can make full use of the original data with less information loss (33). Therefore, it has been successfully applied to a variety of research fields, including supply chain, logistics, engineering, and business systems, suitable for risk assessment and system performance assessment.
In this paper, we describe the following aspects of our study:
First, we developed a health system resilience evaluation system based on the four dimensions (government governance and prevention, health financing, health service provision, and health workforce).
Second, we determined the weights of each of these indicators using a combination of weighting methods, and then calculated a composite index that let us rank the health system resilience of 60 representative countries worldwide using data from 2020, with an emphasis on the TOPSIS method.
Third, we used hierarchical clustering to group the countries based on the evaluation results and classify the health system resilience level of each country.
Fourth, by calculating each country's resilience scores for each of the four dimensions, we identified deficiencies in countries with different levels of resilience, and use these difference to support policy recommendations for strengthening the global health system's resilience against future pandemics.
3. Health system resilience assessment analysis
3.1. Construction of an indicator system for assessing the resilience of health systems
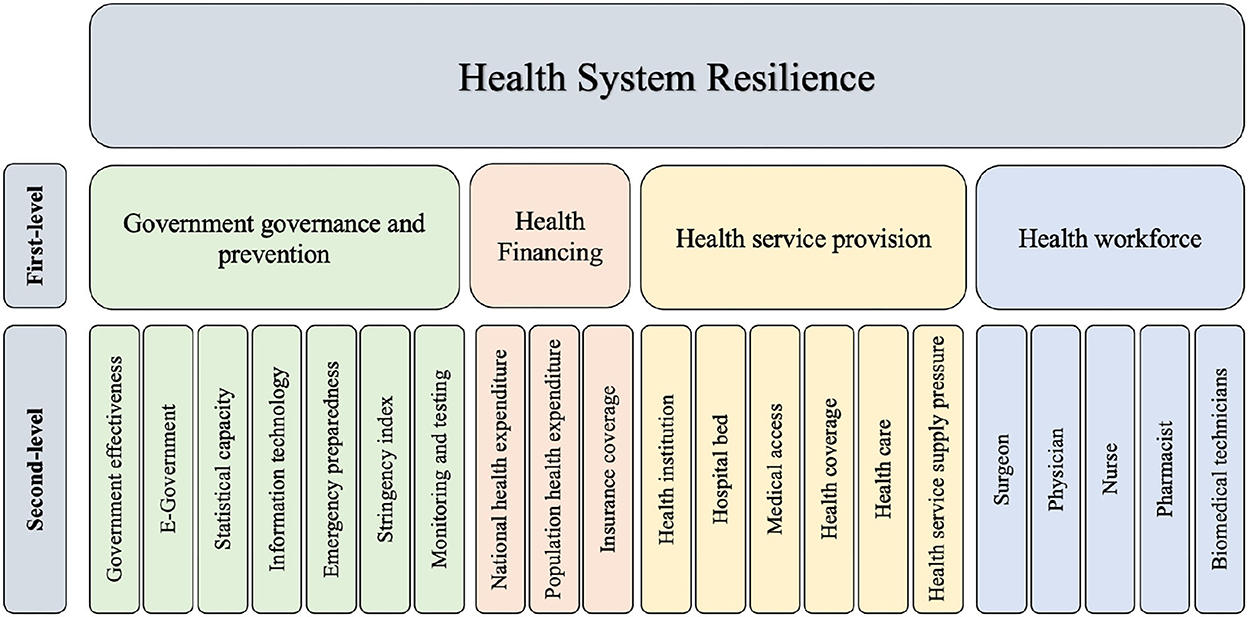
By analyzing WHO's definition of a resilient health system framework and combining it with insights from relevant studies on health system resilience, we constructed an evaluation index framework for health system resilience (25, 26, 34). We started by dividing the framework into four first-level indicators: government governance and prevention, health financing, health service provision, and health workers. We then subdivided each first-level indicator into 3 to 7 second-level indicators to facilitate more accurate qualitative and quantitative analysis.
3.1.1. Government governance and prevention
Government governance and prevention is the most important factor in the health system's response to COVID-19. The timeliness and effectiveness of the government's response to COVID-19 and the efficiency of the formulation and implementation of relevant epidemic prevention policies will both greatly influence the development of the epidemic. The ability of the country to collect and compile data on the epidemic will affect the speed of information dissemination. The infrastructure level of the country's information technology determines the quality of the public services the government can provide to citizens, and the sharing of information and data can guide citizens to take effective response measures (35). Strict prevention and control measures can greatly reduce the scope of the epidemic; extensive surveillance and detection are extremely important in containing its spread (36). On this basis, we divided government governance and prevention into seven evaluation indicators: government effectiveness, e-government, statistical capacity, information technology, emergency preparedness, stringency (a measure of the number and rigor of the measures taken), and monitoring and testing.
3.1.2. Health financing
Health financing is one of the key ways to support the development of a health system. Improved funding can drive improvements in the provision of primary health care and enable the system to respond effectively to changing population health needs and to mitigate shocks from public health emergencies (37). Thus, the monetary input of a country's or region's health system is particularly important for the emergency response of its health system. On this basis, we divided health financing into three evaluation indicators: national health expenditures, population health expenditures, and insurance coverage.
3.1.3. Health service provision
Health service provision has been a common concern in all regions (38). The physical accessibility of health facilities is one of the most important factors affecting the use of health services by patients during a public health emergency (18). Universal health care attempts to improve the quality of the health system through effective health coverage (39). However, health service provision is still influenced by a variety of factors such as ease of access to basic health services and the level of health care. On this basis, we divided health service provision into six evaluation indicators: the number of health institutions, the number of hospital beds, medical access, health coverage, health care, and health service supply pressure.
3.1.4. Health workforce
Health workers face a larger and more stressful workload than usual during an epidemic, so they need to be more resilient and adapt quickly to the changing situation (40). Health workers are a fundamental part of the health system; they perform duties that include carrying out medical research with the aim of improving disease prevention, diagnosis and treatment, clinical consultation, and provision of care to safeguard each patient. When faced with a public health crisis, health workers are often the first to respond. Adequate mobilization and coordination of health workers and medical supplies can significantly reduce mortality (34). On this basis, we divided health workers into five evaluation indicators: the numbers of surgeons, physicians, nurses, pharmacists, and biomedical technicians.
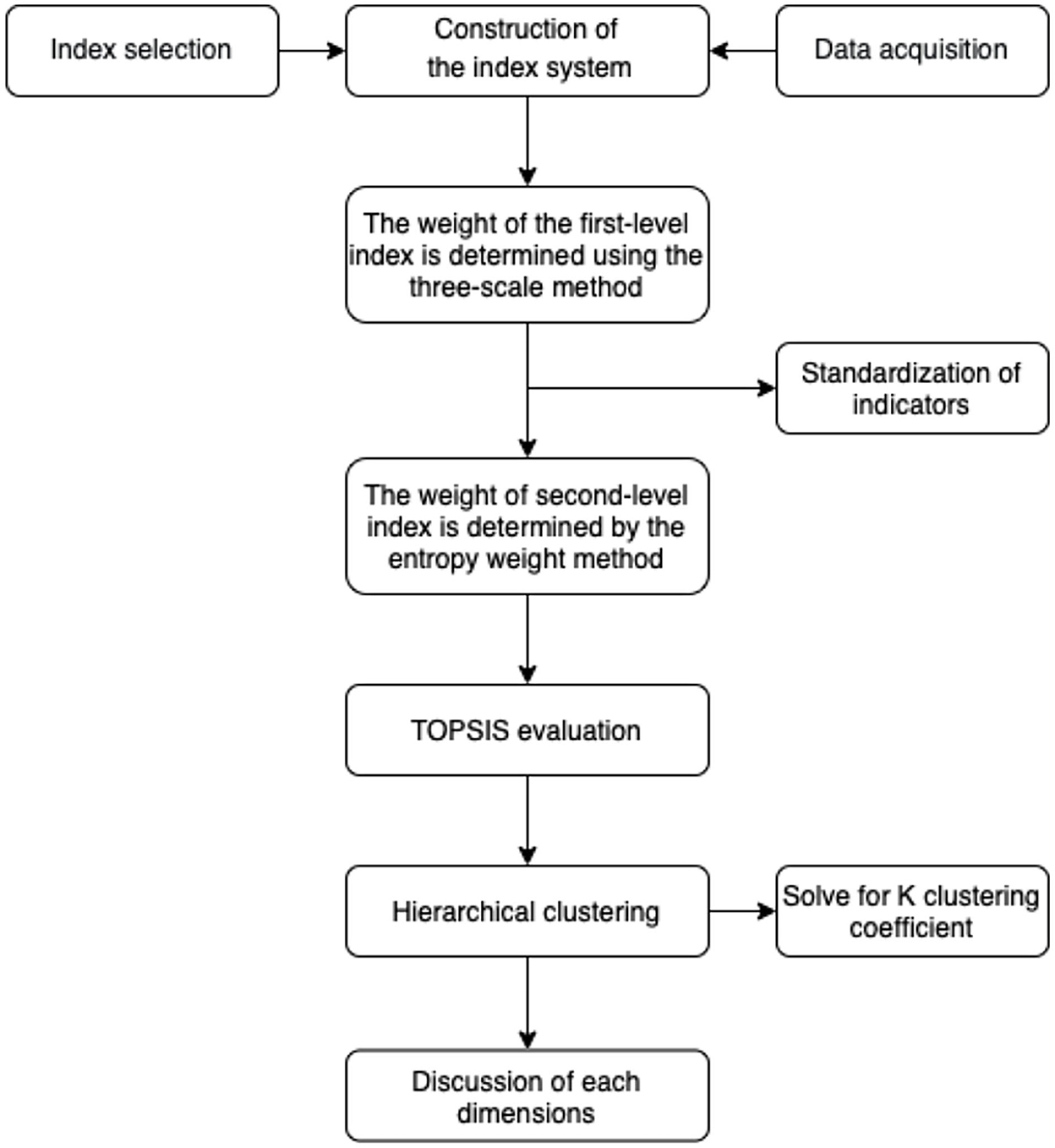
3.2. Calculation methodology
We started with a three-scale method to determine the weight of the four first-level indicators; in this method, the weight has three values that define whether an indicator's value is equal to, less than, or greater than the weight of another indicator. We then used the entropy-weight method to determine the weights of the second-level indicators, and finally used TOPSIS. Based on the results, we performed hierarchical clustering to group the 60 countries based on their health system resilience. In the final step, we analyzed the first-level indicators for each country to determine the factors that most strongly promoted or decreased resilience.
The calculation process is described in Sections 3.2.1 to 3.2.2. Figure 2 provides an overview of these steps.
3.2.1. Index weighting
In this paper, we determined the final indicator weights by combining the three-scale method with the entropy-weighting method. This goes beyond following the subjective will of the decision makers to use objective goals and real data, thereby combining the benefits of subjectivity and objectivity. We used the three-scale method to determine the weights of the first-level indicators, followed by the entropy method to determine the weights of the second-level indicators under each first-level indicator. We obtained the final weights of the 21 secondary indicators by multiplying the first-level indicator weights by the proportional contribution of each second-level indicator to the total weight of the first-level indicator it supports.
The three-scale method is easy for experts to judge, makes it easy to construct a priority judgment matrix that summarizes these judgments, and provides a logical tool (the judgment matrix) for ranking priorities. Therefore, we used the three-scale method in this paper to determine the weight of the first-level indicators (41) (For more details, see Supplementary material). Government governance and coordination are essential for any country, and at the heart of the global health and public service system is the prevention, detection, and response to public health threats (42, 43). When responding to an outbreak of infectious disease, timely government control and a tested emergency response plan can contain the outbreak most quickly. Therefore, government governance and prevention was the most important first-level indicator. Health workers are a fundamental part of the health system, but because they are trainable, responsive, and flexible, they are less important. Health financing is the driving force of the health system, but the input of health financing has a certain periodicity (e.g., because governments plan budgets annually), and it takes some time to see the effect of changes in budget, so we considered financing to be the second-most important first level indicator (37). Health service provision is an important component of the health system, since it requires the development of a health infrastructure, the provision of medical care, and the provision of basic health services. On this basis, we consider it the third-most important indicator.
The entropy weighting method constructs weights using the original (raw) data. The greater the variation in the data (i.e., differences between countries), the greater the amount of information contained in that indicator (i.e., the higher the entropy value) and the more important it is. We used the entropy method to objectively assess the weighting of the indicators (Supplementary material describes details of the calculation for the second-level indicators). We collected data for each indicator in the indicator system to construct the original (non-standardized) data matrix. The matrix contains data on the 21 second-level health system resilience indicators for 60 countries around the world. We standardized the indicators differently according to their characteristics. We then separately calculated the entropy value and weight of the second-level indicators. We then multiplied the weights of the first-level indicators by the proportional contribution of each second-level indicator to the corresponding first-level indicator, thereby obtaining the final weights of the 21 second-level indicators (That is, the sum of these weights equaled the value of the corresponding first-level indicator).
3.2.2. Assessment of health system resilience by means of TOPSIS
We used the TOPSIS method to evaluate the decision matrix formed by each second-level indicator to obtain a ranking of the health system resilience of each country. TOPSIS evaluation is a multi-attribute decision-support method that is widely used in various areas of decision making or evaluation (44). In this paper, we use TOPSIS to evaluate the health system resilience matrix (Ci) for the 60 countries and rank them from most to least resilient (Supplementary material provides details). The values of Ci are in the range (0, 1); the higher the score (i.e., the closer to 1), the more resilient the country.
3.3. Classification of health system resilience
We used version 26.0 of the SPSS software (45) to perform hierarchical clustering of the health system resilience scores for the 60 countries. We used the contour coefficients to determine the optimal clustering scheme.
The first step is hierarchical clustering, which is a well-known clustering algorithm. Compared with K-means clustering, it offers the advantage of adaptive clustering, which does not require setting the number of classes (K) in advance, and the sample can be flexibly divided into different numbers of classes according to the actual needs of the analysis. Specifically, hierarchical clustering first regards each sample as a separate category and then calculates the minimum distance between pairwise samples. Next, the two classes with the smallest distance are merged into a single new class. Then the distance is recalculated between the new class and all other classes. This procedure iterates until all the samples finally merge into a single category (18, 46).
The second step is to calculate the contour coefficient. The contour coefficient reflects the quality of the clustering scheme, and its value is in the range (−1, 1). The larger the contour value, the better the effect. The contour coefficient S(i) combines two factors, the degree of cohesion a(i) and the degree of dispersion b(i), to evaluate the clustering performance. For details of the calculation method, see Supplementary material.
3.4. Resilience of a health systems in terms of the four dimensions
In this paper, we standardized the original (raw) data and multiplied the standardized values by the final weight of each second-level indicator that was obtained by the combined weighting method described in Supplementary material. We then summed the values of each dimension to obtain the resilience score of each country under each dimension. Supplementary material provides details of the calculations. By comparing the health system resilience of 60 countries based on their responses to COVID-19 under the four first-level indicators, we obtained additional insights into the health system resilience of the 60 countries, which let us discuss the factors most strongly responsible for a country's health system resilience and propose policy recommendations to improve its future performance.
4. Results and discussion
4.1. Construct evaluation index system results
Figure 3 shows the results of the constructed health system resilience framework for COVID-19.
4.2. Ranking results
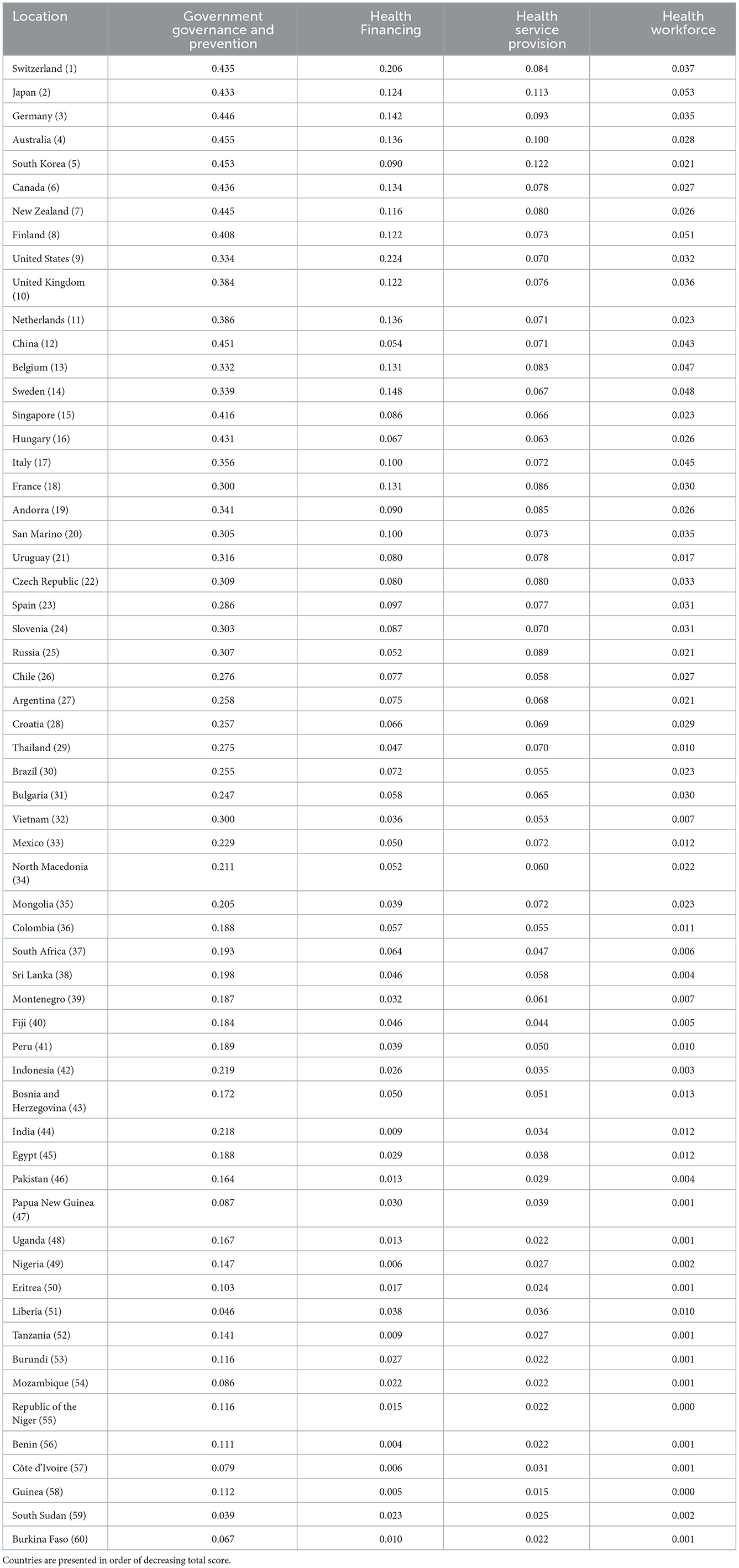
Table 1 presents the ranking of the health system resilience of the 60 countries. The 10 countries with the highest health system resilience were Switzerland, Japan, Germany, Australia, South Korea, Canada, New Zealand, Finland, the United States, and the United Kingdom. The 10 countries with the lowest health system resilience were (from best to worst) Liberia, Tanzania, Burundi, Mozambique, Nigeria, Benin, Côte d'Ivoire, Guinea, South Sudan, and Burkina Faso.
4.3. Clustering results
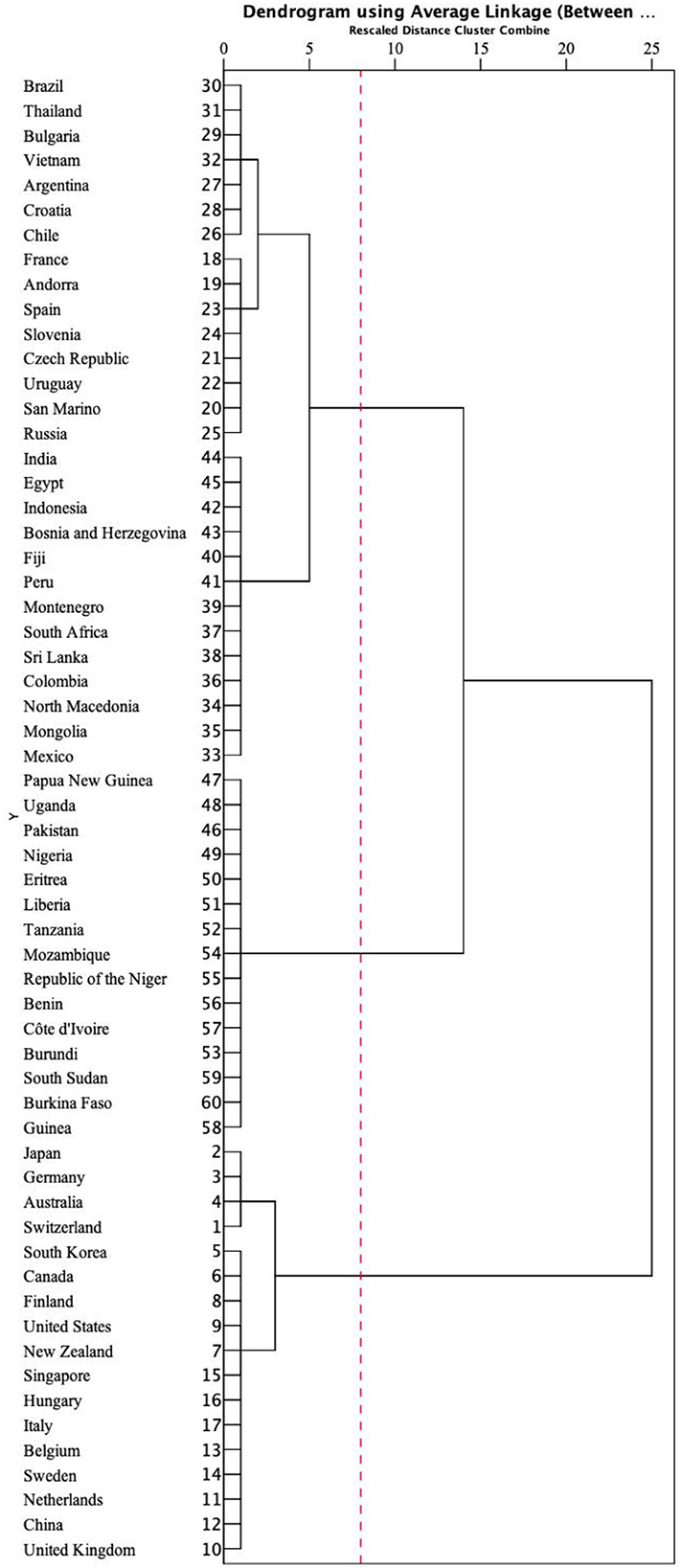
Based on the contour coefficient calculations (Supplementary Figure 1), the optimal result was K = 3 clusters, which produced the highest contour coefficient (0.846). We therefore divided the 60 countries into three categories to discuss the resilience of their health systems. Figure 4 shows the cluster chart produced by the hierarchical cluster analysis.
Table 2 shows the division of the 60 countries into three categories: high, moderate, and low resilience.

Table 2. Ranking of health system resilience by the clustering analysis shown in Figure 4.
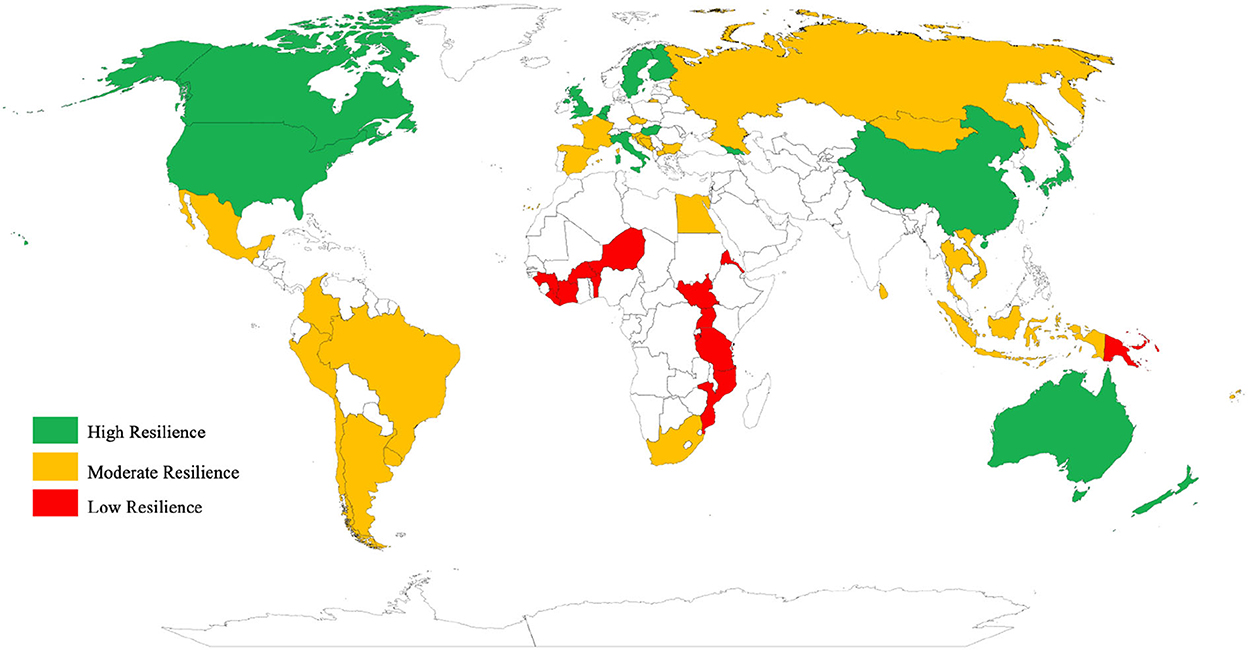
Next, we mapped the health system resilience values (Figure 5) to provide a visual representation of the global distribution of health system resilience. Most of the countries with high resilience are located in Western Europe, East Asia, North America, and Southern Oceania. Africa had a generally low resilience level, except for South Africa and Egypt, which had moderate resilience. Moderate resilience levels dominated South America, South Asia, and Eastern Europe.
4.4. Discuss health system resilience from the four first-level dimensions
Table 3 presents the scores for each of the four first-level indicators of resilience. Note that each of the four dimensions has a different range of index values because of the different weights assigned to these dimensions. The government governance and prevention score averaged 0.257, vs. 0.068 for health financing, 0.059 for health service provision, and 0.019 for health workers.
The 17 countries with a high resilience level had an average resilience score of 0.651. Most of these countries are developed countries with globally leading health systems, but there was significant variation in government governance, with values ranging from 0.332 to 0.455. The Swiss government responded strongly and effectively to the public health emergency by placing a high priority on surveillance and detection of COVID-19, with an indicator score of 0.435 (47). Switzerland's health financing indicator had an average score of 0.206, indicating a well-developed healthcare infrastructure and the most resilient health system based on its response to COVID-19.
Germany has one of the most advanced health care systems in the European countries, with a proactive health care strategy and the lowest mortality rate through early diagnosis and extensive detection, despite the fact that 21% of the population is over 65 years old (48).
Australia, South Korea, Canada, and New Zealand, the four countries with the highest ranking for government governance, were able to contain the spread of the epidemic through effective outbreak prevention and control, and high levels of detection and tracking (49). However, health workers in these four countries scored low, with a mean score (0.025) that was only in the middle of the sample. This represented a high burden on health workers.
The US ranked first in health financing (0.224), with health expenditure accounting for 16.9% of domestic GDP and per capita health expenditure of US$10,623.9, with both values ranking first in the world. However, the US government ranked 17th in governance and prevention (0.334) and 26th in surveillance and detection, as the lack of a unified public health system led to poor coordination of surveillance and detection, making the epidemic worse (50). Similarly, the United Kingdom, which has a universal health care system and the highest health insurance coverage, ranked 13th in government governance and prevention (0.384), with low government emergency preparedness, lax prevention and control measures, and abrupt suspension of surveillance and detection, leaving the entire health system in distress (51).
China and Hungary ranked high in Government Governance and Prevention, with both governments using their experience in efficient government governance and emergency preparedness to quickly contain the outbreak. However, the average health financing score in both countries was only 0.06, and there was a huge gap in health investment and a serious problem with uneven distribution of health resources.
Italy's public health system has been adversely affected by privatization, with cuts of more than €37 billion in national healthcare services from 2010 to 2019, a continued decline in public health spending to 6.6% of GDP from 2018 to 2020, and an aging population, which was hit hard by COVID-19 (52).
There were 28 countries at the moderate resilience level, with an average resilience score of 0.388. These countries have a mid-range score for their health system, with some shortcomings and pre-existing problems within the country that were exacerbated by travel restrictions during the epidemic. France was 9th in health financing (with a score of 0.131) and has a high level of health investment, but its government stringency index was only medium, since the government took preventive and control measures only when the infection rate began to rise rapidly (53, 54).
In terms of health service provision, Andorra (0.085), the Czech Republic (0.080), and Uruguay (0.078) have relatively robust health systems, with complementary public and private health care institutions, and a combination of clinics and mobile aid stations that provide multiple channels of care and protection for the population. Spain had one of the worst ratings for government governance and prevention in Europe, ranking 24th in emergency preparedness, with travel restrictions being implemented 1 week after the implementation of this policy in Italy (55). Surveillance and detection ranked 45th, with a very decentralized surveillance and detection system. Health financing (0.097) was below the average for developed countries, and decades of austerity measures have severely weakened the national health care system (56).
Russian health financing (0.052) was below average (0.068). It ranked 46th on the stringency index, with lax epidemic control and lagging prevention and control measures that left the national health system in crisis. The rating of Russia's health workforce (0.021) was only medium, with a shortage of health workers, stressful workloads, and a shortage of protective supplies. Russian health workers were therefore 16 times more likely to die from COVID-19 than health workers in other countries (57).
Chile's health service provision (0.058) was close to the average (0.059), with a low density of health care facilities and hospital beds that left many patients without timely care. Argentina and Mexico are deep in debt, and the epidemic prompted both countries to endure double pressure from a combination of their debt with other economic factors (greatly decreased trade and increased medical expenses). Argentina adopted strict preventive and control measures and ranked in the top 6 in terms of the stringency index. The trade blockade created by the epidemic hit the domestic economy hard, leading to frequent social crises that exacerbated Argentina's deep debt. Mexico's health service provision (0.072) was above average (0.059) and the country had a high health insurance coverage ratio, but was also affected by the country's debt crisis, making health financing unsustainable and leaving the Mexican health system struggling.
Brazil saw a significant boost in health financing following the health system reform between 2000 and 2014, with total health expenditure rising from 7.0% of GDP to 8.3% and per capita health expenditure increasing from US$263 in 2000 to US$947 in 2014 (58). However, their health system reform is incomplete, and the provision of basic health services is unevenly distributed. There are significant disparities across the country.
Thailand has received global recognition for its healthcare services, having been ranked 6th in the world (59). The government health department used integrated technology to quickly carry out surveillance, detection, tracing, quarantine, and other prevention and control measures to achieve early control of the outbreak (60).
The Vietnamese government showed excellent leadership in responding to COVID-19, ranking in the top quarter of countries in terms of its emergency preparedness performance and its surveillance and detection performance. Vietnam initiated the first public health emergency response at the beginning of the outbreak, sealing the border and taking the initiative to take early measures beyond WHO recommendations to minimize the outbreak (61).
South Africa has one of the best health systems in Africa, but faces significant import pressure due to its close ties with Europe (leading to entry of infected individuals into the country and the spread of infection) and lax preventive and control measures (due to a failure to prevent imported infections), with government governance and prevention (0.193) well below average (0.257).
Sri Lanka has a weak health system, with a health workforce rating (0.04) equal to only about 20% of the average and below-average health financing, but the government was able to reduce the pressure on the health system by taking strict and effective control measures to limit the epidemic's spread (62). In Indonesia, the government delayed the public health emergency response to avoid a large economic impact, and as a result, had the highest number of confirmed cases in March 2020 in Southeast Asia. This exacerbated a significant imbalance in access to health services (63).
The Indian government governance and prevention rating (0.218) resulted from reduced air travel and increased road traffic control, but its surveillance and detection equipment were limited and their implementation was dubious because the quality of the government data has been questioned (64).
There were 15 countries in the low-resilience category, with an average resilience score of 0.149. All of these countries had health system indicators well below those of countries with good and medium resilience. As a result, the health systems of these countries had serious potential for collapse at any time under the shock of an epidemic. Pakistan and Uganda, which had the same level of health financing (0.013) and similar government governance and prevention (0.164 and 0.167, respectively), had severely uneven distribution of health facility coverage and of health resources. The vast majority of the population lacks access to health care.
Libya's and South Sudan's public health efforts were more difficult to coordinate as they were often embroiled in war and conflict, greatly diminishing the public health infrastructure and other social benefits. Continued humanitarian crises will significantly reduce the ability of both countries to coordinate their response to COVID-19 (65). Their government governance and prevention scores were only about 10% of Switzerland's, with the worst emergency preparedness and lax prevention and control measures. This put the entire country's society and economy at risk if an epidemic spreads.
Tanzania's health financing score was only 0.009. Even though its government is implementing the Health Sector Strategic Plan IV 2015–2020 to improve the health system, implementation has faced huge obstacles to health financing reform due to low income and low demand, and the lack of health investment will make it difficult to improve the coverage of public health services (66, 67).
Nigeria (0.006), Benin (0.004), and Côte d'Ivoire (0.006) scored the lowest in health financing, with structural imbalances and problems such as a lack of basic health coverage. Under the impact of COVID-19, their health systems were overburdened and health care was placed under serious pressure (50). Basic health services are severely lacking and vulnerable groups are not covered by health care. The Republic of the Niger and Guinea did well in emergency preparedness and in surveillance and detection, but health workers scored lowest because of very low health care coverage, severe health care shortages, and an overburdened system. Burkina Faso was rated 0.067 in government governance and prevention and 0.022 in health service provision. The number of health facilities per capita and medical beds per capita were among the lowest in the world, so the country's health system faces a high risk of collapse during an epidemic.
5. Policy implications
Resilient health systems can respond effectively to the epidemic, providing strong national protection and mitigating the negative impact of the epidemic. Our results demonstrated that all four first-level indicators contributed to resilience, and that success in achieving resilience required high scores for all indicators; no single indicator was sufficient to compensate for low scores in other indicators. To achieve resilience, we have the following additional policy recommendations:
First, countries with higher levels of resilience, excellent health systems, and adequate medical resources have significant international responsibilities during the global fight against a pandemic. They should, while doing their best to prevent and control the domestic epidemic, play a leadership role in organizing the world's response. They must show innovative global health development assistance, possibly using means such as telemedicine to help developing and less developed countries, must increase medical research investment and output, and must base their decisions on science. They must also learn from less-developed countries, many of which had better ratings in some resilience indicators.
Second, for countries with a moderate level of resilience, governments should devote their resources to identifying and correcting deficits in their health system, which is particularly difficult given the need to balance containment of the epidemic with economic stability. They must take full advantage of medical policy suggestions revealed by the responses of the developed countries to bridge the gap between research and policy. The government should rapidly formulate scientific epidemic prevention policies based on the best practices that were revealed during the epidemic. They must adjust domestic public health funding to ensure that the health system covers their entire population, including both COVID-19 treatment and follow-up treatment once someone has recovered from the initial infection. In addition, they must enhance their capacity to absorb and adapt to shocks, while maintaining social stability. Some countries that are fortunate in having more than adequate resources should allocate excess resources to support the international community and help it fight the pandemic.
Third, for countries with low resilience, governments should take the strictest prevention and control measures possible and adopt stricter requirements for personal protection to prevent the spread of the epidemic while still ensuring people's ability to earn their livelihood as much as possible. Given constraints on their resources, they must allocate resources in the most effective ways. They should work with domestic and foreign non-governmental organizations to maximize their roles. Governments must obtain good statistics so they understand the current state of the epidemic and its trend, and must communicate an accurate description of their situation to international organizations such as WHO. They must carefully manage their budget to allocate funds to the most important and effective social assistance and economic support programs, and seek aid from the international community to avoid the collapse of health systems and increased poverty and social inequalities that follow public health emergencies.
The COVID-19 epidemic has taken a huge toll around the world, and has exposed problems in national health systems around the world. There is an urgent need to reimagine and repair the broken global health system (68). Through assessments of health system resilience, problems can be identified so that targeted measures can be taken to remedy them. In particular, more attention needs to be paid to the allocation of global health resources. Collecting more information will help determine the priority countries that need the most support and explore new methods of providing health aid. Governments should prioritize countries and regions with less resilient health systems and help them to build a more resilient health system that can better respond to future public health emergencies. Only by improving the resilience of global health systems can we hope to respond successfully to future epidemics, improve human health, and move toward a healthier future.
6. Conclusions
We found large differences in the resilience of national health systems around the world. The regions with high health system resilience scores were mainly located in Western Europe, East Asia, North America, and Southern Oceania, whereas the regions with low scores were mainly located in Africa; Eastern Europe, South America, and parts of Southeast Asia had intermediate resilience. The differences were strongly related to differences in economic and social development, exacerbated by differences in national healthcare strategies. The degree of government governance and prevention greatly influenced the response to the epidemic, which is mainly influenced by government emergency preparedness, the rigor of their responses (i.e., the stringency index), and their testing capability. On the other hand, detection and isolation remain the main ways to detect and treat infectious diseases. These measures can greatly reduce mortality and control the spread of an epidemic (69). Health financing was a core indicator of resilience, as national health spending determines the base level of health systems in society as a whole. Cuts in health financing have direct and difficult to reverse impacts on health systems. Low investment in health systems has left public health systems fragmented in South American countries. In terms of health service provision, hospitals and intensive care unit beds played a key role in clinical care during the epidemic, but the role of primary health care systems and facilities was less prominent (70). Aging was a major factor in the higher mortality rates in developed countries. Health workers generally responded well to COVID-19, despite working long hours under exhausting and demoralizing conditions, but the lack of preparedness, facilities, vaccines, protective gear, and critical medicines left health workers in most countries in a precarious environment, with serious implications for their health and for health system stability.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Author contributions
LZha and YJ designed research, performed research, analyzed data, and wrote the paper. LZho provided a lot of suggestions on the revision of the paper. PY provided the guidance of the calculation method. All authors contributed to the writing and revisions.
Funding
This work was supported by grants from the National Social Science Foundation of China (Project No. 22BGL240 and the related Nos. 21BGL217 and 22CGL050).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1081068/full#supplementary-material
References
2. World Health Organisation. COVID-19 Dashboard. Geneva: WHO (2021). Available online at: https://covid19.who.int (accessed May 20, 2021).
3. Carroll WD, Strenger V, Eber E, Porcaro F, Cutrera R, Fitzgerald DA, et al. European and United Kingdom COVID-19 pandemic experience: the same but different. Paediatr Respir Rev. (2020) 35:50–6. doi: 10.1016/j.prrv.2020.06.012
4. Livingston E, Bucher K. Coronavirus Disease 2019 (COVID-19) in Italy. J Am Med Assoc. (2020) 323:1335–35. doi: 10.1001/jama.2020.4344
5. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. J Am Med Assoc. (2020) 323:1775–76. doi: 10.1001/jama.2020.4683
6. Fullman N, Yearwood J, Abay SM, Abbafati C, Abd-Allah F, Abdela J, et al. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. (2018) 391:2236–71. doi: 10.1038/s0140-6736(18)30994-2
7. Team IC-1F. Modeling COVID-19 scenarios for the United States. Nat Med. (2021) 27:94–105. doi: 10.1038/s41591-020-1132-9
8. Tromberg BJ, Schwetz TA, Pérez-Stable EJ, Hodes RJ, Woychik RP, Bright RA, et al. Rapid scaling up of Covid-19 diagnostic testing in the United States—the NIH RADx initiative. New Engl J Med. (2020) 383:1071–77. doi: 10.1056/NEJMsr2022263
9. Naumann E, Möhring K, Reifenscheid M, Wenz A, Rettig T, Lehrer R, et al. COVID-19 policies in Germany and their social, political, and psychological consequences. Eur Policy Anal. (2020) 6:191–202. doi: 10.1002/epa2.1091
10. Hassenteufel P. Handling the COVID-19 crisis in France: paradoxes of a centralized state-led health system. Eur Policy Anal. (2020) 6:170–79. doi: 10.1002/epa2.1104
11. Worldometer. Report coronavirus cases 2020. Available online at: https://www.worldometers.info (accessed July 18, 2021).
12. World Trade Organization. Trade in medical goods in the context of tackling Covid-19. WTO's Secratariat Information Note (2021).
13. Milano G, Vallespir D, Viola A, A. technological and innovative approach to COVID-19 in Uruguay. Commun ACM. (2020) 63:53–5. doi: 10.1145/3422826
14. Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Coronavirus Pandemic (COVID-19) (2020). Available online at: https://ourworldindata.org/coronavirus (accessed May 22, 2021).
15. Dung T. WHO speaks highly of VN's approach to COVID-19 combat. Government of Vietnam, News Report. (2020).
16. Holling CS. Resilience and stability of ecological systems. Annu Rev Ecol Syst. (1973) 4:1–23. doi: 10.1146/annurev.es.04.110173.000245
17. Baggio JA, Brown K, Hellebrandt D. Boundary object or bridging concept? A citation network analysis of resilience. Ecol Soc. (2015) 20:2. doi: 10.5751/ES-07484-200202
18. Kruk ME, Myers M, Varpilah ST, Dahn BT. What is a resilient health system? Lessons from Ebola. The Lancet. (2015) 385:1910–12. doi: 10.1016/S0140-6736(15)60755-3
19. Singh A. Strengthening health systems to meet MDGs. Health Policy Plan. (2006) 21:326–28. doi: 10.1093/heapol/czl008
20. Topp SM. Power and politics: the case for linking resilience to health system governance. BMJ Global Health. (2020) 5:e002891. doi: 10.1136/bmjgh-2020-002891
21. Kruk ME, Ling EJ, Bitton A, Cammett M, Cavanaugh K, Chopra M, et al. Building resilient health systems: a proposal for a resilience index. BMJ. (2017) 357:j2323. doi: 10.1136/bmj.j2323
22. Ammar W, Kdouh O, Hammoud R, Hamadeh R, Harb H, Ammar Z, et al. Health system resilience: Lebanon and the Syrian refugee crisis. J Glob Health. (2016) 6:020704. doi: 10.7189/jogh.06.020704
23. Ling EJ, Larson E, Macauley RJ, Kodl Y, VanDeBogert B, Baawo S, et al. Beyond the crisis: did the Ebola epidemic improve resilience of Liberia's health system? Health Policy Plan. (2017) 32:40–7. doi: 10.1093/heapol/czx109
24. Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, Boykoff M, et al. The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet. (2018) 391:581–630. doi: 10.1016/S0140-6736(17)32464-9
25. Haldane V, De Foo C, Abdalla SM, Jung A-S, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. (2021) 27:964–80. doi: 10.1038/s41591-021-01381-y
26. World Health Organization. Monitoring the Building Blocks of Health Systems: a Handbook of Indicators and Their Measurement Strategies. World Health Organization. (2010).
27. Haug N, Geyrhofer L, Londei A, Dervic E, Desvars-Larrive A, Loreto V, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav. (2020) 4:1303–12. doi: 10.1038/s41562-020-01009-0
28. Abd El-Aziz TM, Stockand JD. Recent progress and challenges in drug development against COVID-19 coronavirus (SARS-CoV-2)-an update on the status. Infect Genet Evol. (2020) 83:104327. doi: 10.1016/j.meegid.2020.104327
29. Silva Araujo CA, Wanke P, Siqueira MM, A. performance analysis of Brazilian public health: TOPSIS and neural networks application. Int J Product Perfor Manage. (2018) 67:1526–49. doi: 10.1108/IJPPM-11-2017-0319
30. United Nations Statistics Division. United Nations Statistical Yearbook (2020). Available online at: http://data.un.org (accessed June 11, 2022).
31. Hwang CL, Yoon K. Multiple Attribute Decision Making: Methods and Applications. New York: CRC press. (1981). doi: 10.1007/978-3-642-48318-9
32. Chakraborty S. TOPSIS and Modified TOPSIS: A comparative analysis. Decis Anal J. (2022) 2:100021. doi: 10.1016/j.dajour.2021.100021
33. Zhao L, Li D, Guo X, Xue J, Wang C, Sun W. Cooperation risk of oil and gas resources between China and the countries along the Belt and Road. Energy. (2021) 227:12. doi: 10.1016/j.energy.2021.120445
34. Hanefeld J, Mayhew S, Legido-Quigley H, Martineau F, Karanikolos M, Blanchet K, et al. Towards an understanding of resilience: responding to health systems shocks. Health Policy Plan. (2018) 33:355–67. doi: 10.1093/heapol/czx183
35. Heymann DL. Data sharing and outbreaks: best practice exemplified. Lancet. (2020) 395:469–70. doi: 10.1016/S0140-6736(20)30184-7
36. He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. (2020) 26:672–5. doi: 10.1038/s41591-020-0869-5
37. Hanson K, Brikci N, Erlangga D, Alebachew A, De Allegri M, Balabanova D, et al. The Lancet Global Health Commission on financing primary health care: putting people at the centre. Global Health. (2022) 10:e715–e72. doi: 10.1016/S2214-109X(22)00005-5
38. Legido-Quigley H, Asgari N, Teo YY, Leung GM, Oshitani H, Fukuda K, et al. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. (2020) 395:848–50. doi: 10.1016/S0140-6736(20)30551-1
39. Kruk ME, Gage AD, Arsenault C. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Global Health. (2018) 6:E1162. doi: 10.1016/S2214-109X(18)30386-3
40. Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:15–6. doi: 10.1016/S2215-0366(20)30078-X
41. Zhao L, Zhao Y, Hu Q, Li H, Stoeter J. Evaluation of consolidation center cargo capacity and locations for China Railway Express. Transp Res Part E- Logist Transp Rev. (2018) 117:58–81. doi: 10.1016/j.tre.2017.09.007
42. Legido-Quigley H, Mateos-García JT, Campos VR, Gea-Sánchez M, Muntaner C, McKee M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health. (2020) 5:e251–52. doi: 10.1016/S2468-2667(20)30060-8
43. Heymann DL, Chen L, Takemi K, Fidler DP, Tappero JW, Thomas MJ, et al. Global health security: the wider lessons from the west African Ebola virus disease epidemic. Lancet. (2015) 385:1884–901. doi: 10.1016/S0140-6736(15)60858-3
44. Dai LX, Wang JF. Evaluation of the profitability of power listed companies based on entropy improved TOPSIS method. Procedia Eng. (2011) 15:4728–32. doi: 10.1016/j.proeng.2011.08.885
45. International Business Machines Corporation. IBM SPSS Statistics 2017. Available online at: https://www.ibm.com/analytics/spss-statistics-software (accessed July 21, 2021).
46. Nielsen F. Introduction to HPC with MPI for Data Science. Switzerland: Springer. (2016). doi: 10.1007/978-3-319-21903-5
47. Salathé M, Althaus CL, Neher R, Stringhini S, Hodcroft E, Fellay J, et al. COVID-19 epidemic in Switzerland: on the importance of testing, contact tracing and isolation. Swiss Med Wkly. (2020) 150:w20225. doi: 10.4414/smw.2020.20225
48. The World Bank. World Development Indicators. (2020). Available online at: https://datacatalog.worldbank.org/dataset/world-development-indicators (accessed June 17, 2021).
49. Adam D. Special report: The simulations driving the world's response to COVID-19. Nature. (2020) 580:316–18. doi: 10.1038/d41586-020-01003-6
50. Lal A, Ashworth HC Dada S, Hoemeke L, Tambo E. Optimizing pandemic preparedness and response through health information systems: lessons learned from Ebola to COVID-19. Disast Med Public Health Prep. (2022) 16:333–40. doi: 10.1017/dmp.2020.361
51. Pollock AM, Roderick P, Cheng KK, Pankhania B. Covid-19: why is the UK government ignoring WHO's advice? Br Med J. (2020) 368:m1284. doi: 10.1136/bmj.m1284
52. Armocida B, Formenti B, Ussai S, Palestra F, Missoni E. The Italian health system and the COVID-19 challenge. Lancet Public Health. (2020) 5:253. doi: 10.1016/S2468-2667(20)30074-8
53. Desson Z, Weller E, McMeekin P, Ammi M. An analysis of the policy responses to the COVID-19 pandemic in France, Belgium, and Canada. Health Policy Technol. (2020) 9:430–46. doi: 10.1016/j.hlpt.2020.09.002
54. Pullano G, Di Domenico L, Sabbatini CE, Valdano E, Turbelin C, Debin M, et al. Underdetection of cases of COVID-19 in France threatens epidemic control. Nature. (2020) 590:134–9. doi: 10.1038/s41586-020-03095-6
55. Henríquez J, Gonzalo-Almorox E, García-Goñi M, Paolucci F. The first months of the COVID-19 pandemic in Spain. Health Policy Technol. (2020) 9:560–74. doi: 10.1016/j.hlpt.2020.08.013
56. European Observatory on Health Systems Policies. Spain: health system review 2018. Health Systems in Transition. (2018). Available online at: https://eurohealthobservatory.who.int/publications/i/spain-health-system-review-2018 (accessed July 18, 2021).
57. The Lancet. Salient lessons from Russia's COVID-19 outbreak. The Lancet. (2020) 395:1739. doi: 10.1016/S0140-6736(20)31280-0
58. Massuda A, Hone T, Leles FAG, de Castro MC, Atun R. The Brazilian health system at crossroads: progress, crisis and resilience. BMJ Global Health. (2018) 3:829. doi: 10.1136/bmjgh-2018-000829
60. Intawong K, Olson D, Chariyalertsak S. Application technology to fight the COVID-19 pandemic: lessons learned in Thailand. Biochem Biophys Res Commun. (2021) 534:830–36. doi: 10.1016/j.bbrc.2020.10.097
61. Ha BTT, Quang LN, Mirzoev T, Tai NT, Thai PQ, Dinh PC. Combating the COVID-19 epidemic: experiences from Vietnam. Int J Environ Res Public Health. (2020) 17:3125. doi: 10.3390/ijerph17093125
62. Wickramaarachchi WPTM, Perera SSN, Jayasinghe S. COVID-19 Epidemic in Sri Lanka: a mathematical and computational modelling approach to control. Comput Math Methods Med. (2020) 404:4045064. doi: 10.1101/2020.04.21.20073734
63. Olivia S, Gibson J, Nasrudin R. Indonesia in the time of Covid-19. Bull Indones Econ Stud. (2020) 56:143–74. doi: 10.1080/00074918.2020.1798581
64. Bhutta ZA, Basnyat B, Saha S, Laxminarayan R. Covid-19 risks and response in South Asia. Br Med J. (2020) 368:m1190. doi: 10.1136/bmj.m1190
65. Munive J. Resilience in displacement and the protection of civilians in South Sudan. J Refug Stud. (2021) 34:1879–99. doi: 10.1093/jrs/fey068
66. United Republic of Tanzania. Health Sector Strategic Plan July 2015 – June 2020 (HSSP IV): Reaching All Households With Quality Health Care. Ministry of Health and Social Welfare, Dar es Salaam. (2015). Available online at: https://www.prb.org/wp-content/uploads/2020/06/Tanzania-Health-Sector-Strategic-Plan-IV-2015-2020-1-4.pdf (accessed August 20, 2021).
67. Afriyie DO, Hooley B, Mhalu G, Tediosi F, Mtenga SM. Governance factors that affect the implementation of health financing reforms in Tanzania: an exploratory study. BMJ Global Health. (2021) 6:e005964. doi: 10.1136/bmjgh-2021-005964
68. Shamasunder S, Holmes SM, Goronga T, et al. COVID-19 reveals weak health systems by design: why we must remake global health in this historic moment. Glob Public Health. (2020) 15:1083–89. doi: 10.1080/17441692.2020.1760915
69. Director-general of the World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19. (2020). Available online at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-−18-march-2020 (accessed March 18, 2020).
Keywords: COVID-19, health system, resilience, evaluation, multi-country, TOPSIS
Citation: Zhao L, Jin Y, Zhou L, Yang P, Qian Y, Huang X and Min M (2023) Evaluation of health system resilience in 60 countries based on their responses to COVID-19. Front. Public Health 10:1081068. doi: 10.3389/fpubh.2022.1081068
Received: 02 November 2022; Accepted: 19 December 2022;
Published: 09 January 2023.
Edited by:
Simon Ching Lam, Tung Wah College, Hong Kong SAR, ChinaReviewed by:
Kei Shing Ng, The University of Hong Kong, Hong Kong SAR, ChinaBenny Hon, City University of Hong Kong, Hong Kong SAR, China
Copyright © 2023 Zhao, Jin, Zhou, Yang, Qian, Huang and Min. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yajun Jin,  MjAyNzIxMTYzQHN0LnVzc3QuZWR1LmNu
MjAyNzIxMTYzQHN0LnVzc3QuZWR1LmNu
 Laijun Zhao
Laijun Zhao Yajun Jin
Yajun Jin Lixin Zhou1
Lixin Zhou1 Ying Qian
Ying Qian