
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 06 January 2023
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1056123
This article is part of the Research TopicThe Developmental Origin of Childhood ObesityView all 4 articles
Objective: Food addiction (FA) is associated with a higher body mass index z-score (BMIZ) in children and adolescents; however, whether these two aspects evolve interdependently remains unknown. This study aimed to address this question using a cross-lagged study.
Methods: Weight status, including BMIZ, fat content (FC), and visceral fat level (VFL), was determined in 880 children and adolescents (mean age = 14.02 years [range = 8.83–17.52 years]) at two-time points with an interval of 6 months. FA was characterized using the Chinese version of the dimensional Yale Food Addiction Scale for Children 2.0. Furthermore, FC and VFL were measured using direct segmental multi-frequency bioelectrical impedance analysis at each time point.
Results: Higher FA was associated with increased BMIZ, FC, and VFL (P < 0.05). FA at T0 could predict increased FC at T1 (P < 0.05). The characteristics of females, primary students, and living in urban areas may aggravate the adverse effect of FA on weight status over time and age, particularly the increased VFL in participants aged > 14 years.
Conclusion: Children and adolescents with a high FA level were at risk for weight gain attributed to increased FC, and the adverse effect could be aggravated with time and age. Novel FA-targeting interventions may help mitigate the risk of getting obesity.
Obesity is a revertible but easily relapsing condition because of several reasons, and food addiction (FA) emerged as a novel perspective for understanding eating behavior and was observed to correlate with weight status characterized by body mass index (BMI). However, how FA contributes to obesity remains unknown. In this longitudinal study, it was found that higher FA was associated with increased body mass index z-score (BMIZ), fat content (FC), and visceral fat level (VFL). The higher FA level at T0 could predicate increased FC at T1, and children and adolescents with a high FA level were at risk for weight gain, which was attributed to the increased FC. The characteristics of females, primary students, and living in urban areas may aggravate the adverse effect of FA on weight status over time and age. Moreover, the increase in VFL was more significant in participants 14 years in junior high school. FA could be integrated into the weight loss program in future studies to help children and adolescents lose weight, particularly to improve the loss of FC at an early age.
What is already known about this subject?
• Obesity is a revertible but easily relapsing condition because of several reasons, including psychological factors.
• Compulsive and overeating behavior results in failed weight loss programs, and the limited and transient effect of constraining food intake encourages more exploration of the underlying reasons.
• Food addiction (FA) has emerged as a novel perspective for understanding eating behavior and has been observed to correlate with weight status characterized by body mass index (BMI).
What are the new findings in your manuscript?
• Higher FA was associated with increased body mass index z-score (BMIZ), fat content (FC), and visceral fat level (VFL).
• The higher FA level at T0 could predicate increased FC at T1, and children and adolescents with a high FA level were at risk for weight gain, which was attributed to the increased FC.
• The characteristics of females, primary students, and living in urban areas may aggravate the adverse effect of FA on weight status over time and age, particularly in participants aged > 14 years.
How might your results change the direction of research or the focus of clinical practice?
• FA could be integrated into the weight loss program to help children and adolescents lose weight, particularly to improve the loss of FC.
• Special attention should be given to females and primary students living in urban areas because they are at high risk for weight gain attributed to increased fat. The adverse effect of FA, including the increased VFL, will be aggravated at the age of >14 years and over time.
The prevalence of overweight and obesity has become a public health problem globally, with a rapid increase in the number of children and adolescents (1). It was reported that, by 2016, approximately 124 million school-aged children and adolescents will be living with excessive weight status (2). In developing countries (2), such as China, the prevalence rate of excessive weight has increased from 14.5 to 35.3% during decades (3). The overweight and obesity onset in early childhood could lead to metabolic dysfunction (4) and chronic diseases in adulthood (5). Furthermore, it is associated with negative psychological development (6). Moreover, obesity could impair cognitive and social function and results in low self-esteem (7).
Obesity has been recognized as a revertible but easily relapsing condition (8), and the effect of energy restraint-based intervention was limited (9). Moreover, concerns about negative impacts on growth and other aspects of development owing to diet in children and adolescents have been raised (10), calling for alternative interventions. To explore potential long-term effects and safer interventions, a growing number of researchers have shifted to focus on the psychological causes of obesity (11, 12). Food addiction (FA) has become one of the emerging underlying psychological factors (13).
Individuals with FA were characterized by compulsive and impaired control of eating behavior (13). These symptoms could be more severe in school-aged children and adolescents owing to their impulsive traits (14). Additionally, several addictive behaviors started from an early age and lasted to adulthood (15), and longer addictive behavior duration would result in worse intervention outcomes. Therefore, considering FA in children and adolescents to prevent further consequences is significant.
Although several cross-sectional studies revealed a close correlation between FA and body mass index z-score (BMIZ) (16, 17), the potential causal relationship between FA and weight status has not been identified. Moreover, studies concerning FA were rare in children and adolescents, particularly longitudinal studies (18). Despite FA has remained controversial, increasing studies have shown that highly processed food could be as addictive as other substances, such as tobacco (19). With the changing food environment, particularly the easily accessible highly processed food, more empirical evidence concerning FA is needed (20).
Furthermore, BMIZ, which is calculated by weight and height, may be incomplete to characterize weight status (8). For example, the fat mass is typically underestimated using BMIZ (21), and the adverse consequences of obesity result from excessive fat mass deposited in the subcutaneous and viscera, but not simply body weight because other body compositions, including the muscle, also contribute to weight status but not obesity (22). Thus, to characterize weight status, particularly fat distribution, complementary measures, including body composition, should be included (22).
Therefore, this study aimed to explore the temporal longitudinal associations between FA and weight status, which are characterized using BMIZ and fat distribution, in school-aged children and adolescents and analyze the interactive effect of time and demographic characteristics in the associations.
Participants aged 8–18 years were enrolled in a primary school, junior school, and high school in a town in Eastern China. The following were the exclusion criteria: participants diagnosed with endocrine diseases, including hyperthyroidism, or another disease that may impact weight status (e.g., depression and anxiety); those who were receiving therapies, surgery, or other treatments in recent 3 months; those who were on a diet in recent 3 months; and those who did not participate owing to physical concerns, such as feet hurt.
Participants' demographic information, including age, gender, school, and inhabitation, were collected. A short screening form was used to exclude the participants who did not meet the criteria at each time of the survey.
The participants' additive-like eating behavior was characterized using the FA scores assessed by the Chinese version of the dimensional Yale Food Addiction Scale for Children 2.0 (dYFAS-C 2.0) (23). In 2018, Schiestl and Gearhardt (24) developed the dYFAS-C 2.0 based on the Diagnostic and Statistical Manual for Mental Disorders, fifth edition. The dYFAS-C 2.0 has 35 items rated using a 7-point Likert scale on each item (24). A higher score of dYFAS-C 2.0-C indicated a higher FA level (24). The Chinese version of dYFAS-C 2.0-C was translated and validated with good internal reliability of 0.934 (23). In this study, the average score was used to indicate the FA level. An FA score of >0.7 was categorized as a high risk of FA according to our previous study (23).
The BMIZ was calculated using WHO AnthroPlus, using the height and weight measured by the researcher, with BMIZ > 1 indicating overweight or obesity (25). The FC and VFL were assessed using a machine based on direct segmental multi-frequency bioelectrical impedance analysis (DSM-BIA). The machine was equipped with an eight-pedal electrode system and took direct impedance measurements based on the assumption that the human body is consisted of five interconnecting cylinders (26). A previous study showed that the internal consistency between DSM-BIA and the accurate dual-energy X-ray absorptiometry was >0.9 (27), indicating the machine's reliability in measuring body composition. The FC indicated the proportion of fat in the whole body weight; a higher FC implied that the fat contributed more to the weight and was influenced by age. However, several studies showed that the fat mass change was more dispersed with age compared with other body composition, such as bone mineral content and lean tissue mass, and was prone to be stable after the age of 10 (28, 29). Considering the role of growth and development of children and the wide range of age groups, FC > 18% and 28% for males and females were grouped as high FC based on the study of Fomon's et al. (30). The VFL indicated that fat accumulated among the abdominal viscera; a VFL of >10 indicated abdominal obesity according to the instructions of the BIA machine.
A longitudinal study was conducted, and the participants' FA level and body composition were assessed twice at a 6-month interval. The participants' height, weight, and body composition were measured using the standard method after removing their coats, shoes, and socks (they must be barefooted to contact the plate electrode). To ensure accuracy, the height of the participants was measured twice, and the weight and body composition were measured using a body composition analyzer using the DSM-BIA method.
Following the measurements, each participant was provided with a card with individual information about their name, school, grade, and class, assigned number, measurements (height, weight, FC, and VFL), and a link to the online survey. They were allowed to complete the online survey at their most convenient time within 1 week.
Data collection was performed twice on May 2022 (T0) and November 2022 (T1) without any interventions being performed during the interval.
This study was approved by the ethics committee of the Children's Hospital of Zhejiang University (Approve Number: 2021-IRB-235). It was also approved by the schools and local education government. The participants and their families were informed about the survey through the school WeChat group (a social media platform). The introduction of the survey was recorded as a video, which depicted how the study aimed to explore the association between addictive eating behavior and weight status. Subsequently, the researcher measured the participants' height, weight, and body composition. An online survey must be completed by the participants within 1 week. Moreover, the video illustrated that the participants could quit at any time depending on their willingness. As compensation, to provide a reference of their growth status, the researcher calculated each participant's BMI and height percentages and provided their corresponding suggestion. Each participant could obtain a package of candy as a gift of participation. The participants' consent, both from the children and their parents or guardians, was acquired online before the online survey; only participants who agreed to participate in the survey and recognized their right to quit at any time could continue with the online survey.
The participants' age, FA, BMIZ, FC, and VFL were expressed using means and standard deviations (SDs) or medians and interquartile ranges. The participants' gender, education level, inhabitation, and FA, BMIZ, FC, and VFL categories were summarized using numbers and proportions.
The longitudinal association of FA at T0 with BMIZ, FC, and VFL at T1 was explored using linear regression after adjusting for age, gender, education level, and inhabitation. To further explore and interpret the association between FA at T0 and BMIZ, FC, and VFL at T1, the variables were categorized into dichotomous ones. The longitudinal association between the FA category at T0 and BMIZ, FC, and VFL categories at T1 was explored using binary logistics regression, with covariate adjustment including age, gender, education level, and inhabitation.
The prospective associations between repeated measures of FA and BMIZ, FC, and VFL were analyzed using linear mixed models, and the interactive effects of the participants' demographic characteristics on the association between FA and weight status were also analyzed to explore the moderate effect of demographic characteristics between FA and weight status.
The temporal associations of FA and BMIZ, FC, and VFL were explored using structural equation modeling with an autoregressive cross-lagged design. First, the cross-lagged model tested the association of FA at T0 with BMIZ, FC, and VFL at T1, separately. Subsequently, the associations of BMIZ, FC, and VFL at T0 with FA at T1 were tested. These models were adjusted for the effect of covariates of age, gender, education level, and inhabitation. Standardized estimation was reported. P < 0.05 was considered statistically significant.
Statistical analyses were performed using SPSS (IBM Corp., Armonk, NY, USA) and Mplus version 7.1 (Muthén & Muthén, LA, CA, USA).
A total of 880 participants aged 8.83–17.52 years completed the two-time survey, with a mean age of 14.02 years (SD = 2.71) at baseline (the flow chart of enrolment and the characteristics of the participants who remained and dropped from the study are shown in Figure 1 and Table 1). A total of 450 (51.1%) and 430 (48.9%) male and female participants, respectively, were included, with 312 (35.5%), 128 (14.5%), and 440 (50%) primary school, junior high, and high school students, respectively. Half of the students (58.1%) inhabited the rural areas, and 41.9% inhabited the urban areas. The detailed demographic information and BMIZ, FC, VFL, and FA at T0 (May 2021) and T1 (November 2021) are presented in Table 2. In this study, the reliability of dYFAS-C 2.0-C was 0.953 at baseline.
In linear regression analysis, the FA at T0 was significantly associated with BMIZ (β = 0.600, P < 0.001), FC (β = 4.202, P < 0.001), and VFL (β = 2.248, P < 0.001) at T1, with covariates of baseline age, gender, education level, and inhabitation being controlled. Further generalized line model for repeated measures showed that the FA at T0 was significantly associated with the variance of weight status. The effect size of FA on BMIZ, FC, and VFL were 0.072, 0.070, and 0.089, respectively. The effect size of covariables was also evaluated, and the results were presented in Table 3.
In logistics analysis, the FA category at T0 was significantly associated with the BMIZ category (β = 1.120, odds ratio [OR] = 3.066, 95% confidence interval [CI]: 2.182–4.308, P < 0.001, classification accuracy: 73.6%), FC category (β = 0.627, OR = 1.873, 95% CI: 1.300–2.697, P = 0.001, classification accuracy: 72.3%), and VFL category (β = 1.136, OR = 3.115, 95% CI: 2.163–4.485, P < 0.001, classification accuracy: 82.0%) at T1, with covariates of age, gender, education level, and inhabitation being controlled.
In mixed linear model analyses, the variance of FA was significantly associated with the variances of BMIZ (F = 89.646, P < 0.001), FC (F = 88.620, P < 0.001), and VFL (F = 123.390, P < 0.001) from T0 to T1, with covariates of age, gender, education level, and inhabitation (Table 4).
Further analysis showed that time, age, gender, education level, and inhabitation could significantly moderate the effect of FA on BMIZ, FC, and VFL (P < 0.05) (Table 5). The participants aged 8–14 years experienced more increase in BMIZ and FC, whereas those aged > 14 years experienced more increase in VFL. Primary school students shared more increased BMIZ and FC, whereas junior high school students shared a more increased VFL, which was consistent with previous findings in 14-year-old participants. The participants living in urban areas were more likely to experience higher weight gain and fat distribution than those living in rural areas. The effect of FA on weight status indicated by BMIZ, FC, and VFL could be aggravated by time (Figure 2).
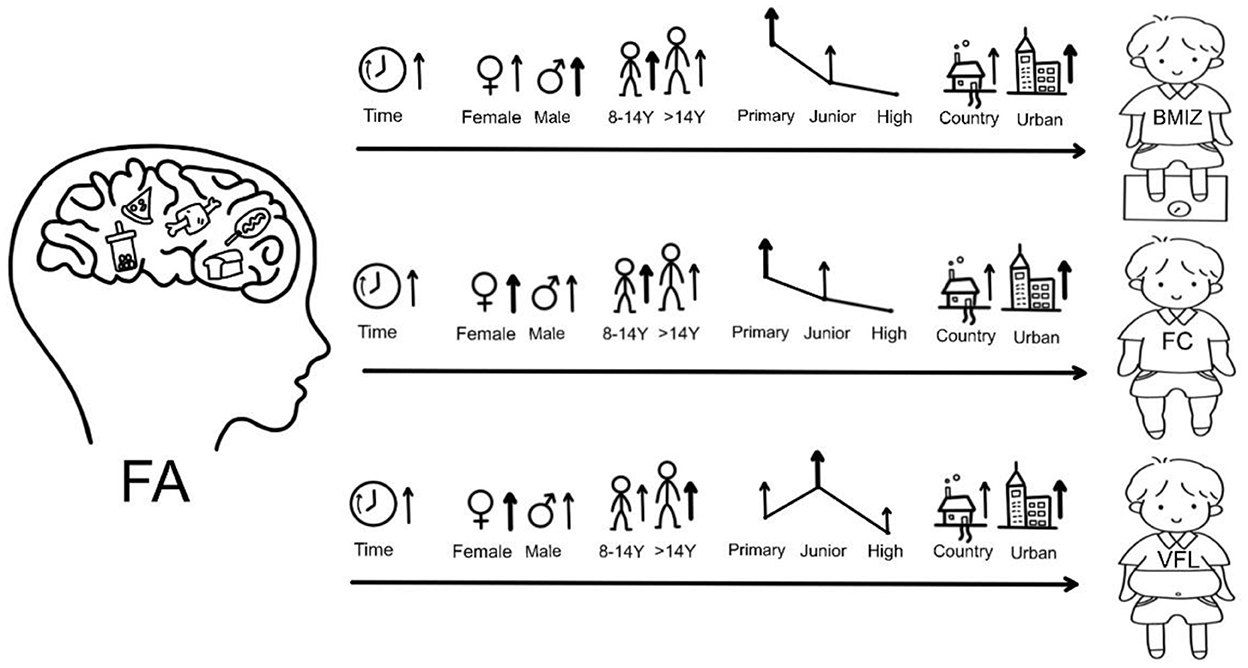
Figure 2. The moderate roles of participants' characteristics between FA and weight status (BMIZ, FC, and VFL). The “↑” indicates that this characteristic could aggravate the effect of FA on weight status characterized by BMIZ, FC, and VFL. The bold “↑” indicates more significant effect. FA, food addiction; BMIZ, body mass index z-score; FC, fat content; VFL, fat level.
FA at T0 was directly associated with FC at T1 (β = 0.044, P = 0.007), see Figure 3B. BMIZ (β = 0.060, P = 0.041), FC (β = 0.064, P = 0.041), and VFL (β = 0.073, P = 0.017) at T0 were directly associated with FA at T1, with covariates of age, gender, education level, and inhabitation being controlled (Figures 3A–C). The estimation of autoregressive and cross-lagged variables is presented in Table 6. The autoregression effects of FA, BMIZ, FC, and VFL at T0 and T1 were significant (P < 0.001). The cross-lagged effect was significant between FA and FC (P < 0.05).
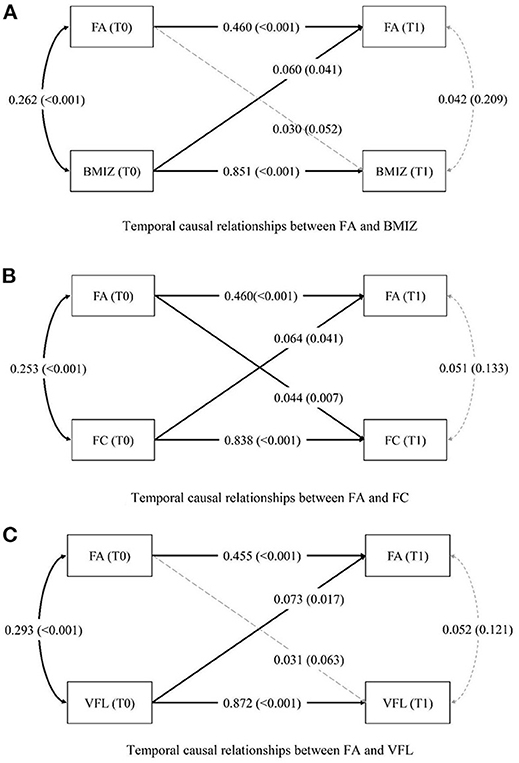
Figure 3. (A–C) Temporal and causal relationships between FA and weight status. The P-values are presented in brackets. The concert line indicates a significant pathway, whereas the dashed line indicates a nonsignificant pathway. FA, food addiction; BMIZ, body mass index z-score; FC, fat content; VFL, visceral fat level.
This study explored the temporal longitudinal associations between FA and weight status characterized using BMIZ, FC, and VFL. The results showed that children and adolescents with a high risk of FA were 2–3 times (OR: 1.873–3.115) more likely to be diagnosed with excessive weight status than those with low FA risk. FA was a distinguishable feature of participants with excessive weight, and higher FA was significantly associated with increased FC. The characteristics of females, primary school students, different age stages, and living in urban areas could exacerbate the effect of FA on weight gain and fat distribution.
Previous studies showed that FA is prevalent in children with overweight or obesity (31, 32). It was reported that approximately 19% of school-aged children with overweight/obesity were categorized with FA, even in the general population; however, 12% of children were found to have FA, and the overall prevalence of FA was 13–18% (18, 31). In our previous study, we identified that an average score of 0.7 was strongly associated with higher BMIZ and could be an indicator of high FA risk (23). In this study, participants with a high risk of FA at baseline had a 2–3 times probability of being diagnosed as excessive weight during follow-up. Further analysis of repeated measures showed that the higher level of FA was associated with increased BMIZ, FC, and VFL and resulted in weight gain and fat distribution. These results showed that FA was closely associated with increased weight and may play a role in maintaining a higher level of weight. The results were consistent with Almeida's weight loss intervention study, with the conclusion that FA contributed to the maintenance of weight and difficulties in weight loss (33).
Moreover, the effect of FA on weight status variance was moderated by time, participants' age, gender, education level, and inhabitation. After 6 months, the results showed that the adverse effect of FA on weight status may be more obvious than before. This indicates that with prolonged time, the FA may contribute to more rapid weight gain and fat distribution. Thus, timely intervention of FA is significant in a weight control program. This result was consistent with those of other studies on addiction, which implied that a longer duration of addiction symptoms would result in several adverse consequences (34), in the case of FA, leading to an aggressive weight gain, particularly the increase in fat mass.
This study showed that the effect of FA on weight status could be moderated by different age stages. Compared with participants aged > 14 years, the participants aged 8–14 years were more likely to experience an increased BMIZ and fat distribution with higher FA levels; however, those aged > 14 years were prone to experience more VFL increase due to severe FA over time compared with younger age group. The different effects could be attributed to the different body composition development features across ages (35). The subcutaneous fat rapidly developed before the age of 12, particularly before 10 years old (28, 29), and tended to persist at its peak at 13–14 years without a significant variance in a wide percentile scope (35). Conversely, the visceral adipose tissue still tended to increase after 14 years, particularly in individuals with visceral fat tissue at the 50 percentile and above (35), causing a more adverse effect on metabolic function (36). Moreover, visceral fat was significantly associated with chronic disease and cancer compared with subcutaneous fat (37), suggesting the significance of paying attention to the VFL at a young age in children with high FA risk. Additionally, particularly at the age of 14, a more detailed physical check should be performed to detect the adverse effect of FA and facilitate timely intervention.
In this study, although male participants' BMIZ was affected more by the FA, the female participants were more likely to experience an increased fat distribution rather than weight gain than the male participants, which was consistent with the results of previous studies (38). This may be because of the development feature of females (39) and gender-specific fat distribution patterns (40). Owing to the appearance of secondary sexual characteristics, females were prone to deposit adipose tissues during development (41). This may make the female participants easily impacted by the FA. Moreover, a study on the adult population showed that female participants were more prone to FA than their male counterparts (42). Gender itself may play a part in the efficiency of FA on weight status.
In this study, the primary students were affected more by the effect of FA than the junior and high school students, indicating that the impact of FA could be moderated by the education level. On one hand, the inhibitory ability will be improved with the development of brain function as the education level was improved (43). On the other hand, the intensive image attention emerging from junior high school primarily would help the students to shift their interest from food to other social activities (44), which may help them to decrease the effect of FA.
Moreover, students living in rural areas were less affected by the FA than their counterparts living in urban areas. This may be because of the limited number of shops or supermarkets selling highly processed snacks in rural areas. This indicated that the social environment was also significant for alleviating the effects of FA, and constraining the sales of highly processed food without adequate nutrition, such as sweetened drinks and chips, may be helpful (45). A multicenter intervention conducted in China also showed the efficiency of constraining certain food sales in primary schools (46).
After controlling the abovementioned covariates, the bidirectional association between FA and FC was clear in this study. Furthermore, the direct association between BMIZ and VFL to FA was significant. The results indicated that the FA was a distinguishable feature of participants with higher BMIZ and fat distribution. Additionally, the bidirectional association between FA–BMIZ and FA–VFL was close to a significant value, suggesting the potential of FA for the predicated temporal variance of both BMIZ and fat distribution. The only bidirectional association between FA and FC may be because of the sensitive change in FC compared with BMIZ and VFL. The prediction effect was similar to the effect of behavior problems on BMIZ in preschoolers (0.044 vs. 0.09) (47). The FC and VFL at baseline were both directly associated with FA and may also show the dysregulation of hormone and brain function resulting from increased adipose tissue. Studies showed that the increased fat mass could enhance insulin resistance (48), thereby leading to elevated energy intake. Moreover, a study showed that decreased glutamate/creatine ratio was observed in the hypothalamus of adolescents with obesity, indicating appetite regulation dysfunction (49). This may promote eating behaviors in children and adolescents with overweight and obesity and contribute to severe FA. Therefore, in a weight loss program, recording the variance of adipose distribution may be more effective than focusing on weight only. This could not only help the participants to lose weight but also decrease the effect of FA and consolidate the effect of weight loss in the long run.
This study had several limitations. First, although the results from a longitudinal design were more robust than those of a cross-sectional one, the causal relationship could not be firmly identified; only the temporal association of FA and weight status could be identified in this study. Second, the fat distribution was measured based on the bioelectrical impedance analysis method rather than dual X-ray, which may reduce the accuracy of the measurement. However, given the safety (50) and interchangeability between the two methods in a population-based study (51), the results were credible. Third, other covariates, including food intake and physical activities, were unavailable in the participants owing to large missing data; further studies should evaluate these important covariates as required from to ensure the integrity of the data set, and the follow-up duration may not be long enough to detect more variances. Lastly, the effect of pubertal development was not evaluated in this study; however, given the relatively short follow-up period and that most participants were above the age of 10 (92.8%), the results could be less influenced by the factor of pubertal development.
FA was predictive of FC increase and associated with increased BMIZ and VFL, and the characteristics of being female, primary school students, and those living in urban areas were factors that could aggravate the effect of FA on weight gain and fat distribution. The FA was significantly associated with BMIZ, FC, and VFL across different age groups. However, the different effects of FA on weight status between age groups should be noticed. The intervention of FA should be incorporated into weight loss programs to help children and adolescents with overweight or obesity lose weight and ensure a prolonged effect.
The raw data supporting the conclusions of this article will be made available upon reasonable request.
The studies involving human participants were reviewed and approved by the Children's Hospital of Zhejiang University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
DW research design, data collection, data analysis, and draft. HZ and YH revision. YC data visualizaztion. XY and JC data collection. JF resource and supervision. HX supervision. All authors contributed to the article and approved the submitted version.
We would like to thank the directors and teachers of the schools and the participants from the town.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bauman A, Rutter H, Baur L. Too little, too slowly: international perspectives on childhood obesity. Public Health Res Pract. (2019) 29:e2911901. doi: 10.17061/phrp2911901
2. Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. (2017) 390:2627–42. doi: 10.1016/S0140-6736(17)32129-3
3. Jia P, Xue H, Zhang J, Wang Y. Time trend and demographic and geographic disparities in childhood obesity prevalence in china-evidence from twenty years of longitudinal data. Int J Environ Res Public Health. (2017) 14:369. doi: 10.3390/ijerph14040369
4. Kumar S, Kelly AS. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin Proc. (2017) 92:251–65. doi: 10.1016/j.mayocp.2016.09.017
5. Richardson TG, Crouch DJM, Power GM, Morales-Berstein F, Hazelwood E, Fang S, et al. Childhood body size directly increases type 1 diabetes risk based on a lifecourse Mendelian randomization approach. Nat Commun. (2022) 13:2337. doi: 10.1038/s41467-022-29932-y
6. Smith JD, Fu E, Kobayashi MA. Prevention and management of childhood obesity and its psychological and health comorbidities. Annu Rev Clin Psychol. (2020) 16:351–78. doi: 10.1146/annurev-clinpsy-100219-060201
7. Pont SJ, Puhl R, Cook SR, Slusser W. Stigma experienced by children and adolescents with obesity. Pediatrics. (2017) 140:e20173034. doi: 10.1542/peds.2017-3034
8. De Lorenzo A, Romano L, Di Renzo L, Di Lorenzo N, Cenname G, Gualtieri P. Obesity: a preventable, treatable, but relapsing disease. Nutrition. (2020) 71:110615. doi: 10.1016/j.nut.2019.110615
9. Tobore TO. Towards a comprehensive theory of obesity and a healthy diet: the causal role of oxidative stress in food addiction and obesity. Behav Brain Res. (2020) 384:112560. doi: 10.1016/j.bbr.2020.112560
10. Hovinen T, Korkalo L, Freese R, Skaffari E, Isohanni P, Niemi M, et al. Vegan diet in young children remodels metabolism and challenges the statuses of essential nutrients. EMBO Mol Med. (2021) 13:e13492. doi: 10.15252/emmm.202013492
11. Hemmingsson E. Early childhood obesity risk factors: socioeconomic adversity, family dysfunction, offspring distress, and junk food self-medication. Curr Obes Rep. (2018) 7:204–9. doi: 10.1007/s13679-018-0310-2
12. Wiss DA, Avena N, Gold M. Food addiction and psychosocial adversity: biological embedding, contextual factors, and public health implications. Nutrients. (2020) 12:3521. doi: 10.3390/nu12113521
13. Adams RC, Sedgmond J, Maizey L, Chambers CD, Lawrence NS. Food addiction: implications for the diagnosis and treatment of overeating. Nutrients. (2019) 11:2086. doi: 10.3390/nu11092086
14. Rømer Thomsen K, Callesen MB, Hesse M, Kvamme TL, Pedersen MM, Pedersen MU, et al. Impulsivity traits and addiction-related behaviors in youth. J Behav Addict. (2018) 7:317–30. doi: 10.1556/2006.7.2018.22
15. Bos J, Hayden MJ, Lum JAG, Staiger PK. UPPS-P impulsive personality traits and adolescent cigarette smoking: a meta-analysis. Drug Alcohol Depend. (2019) 197:335–43. doi: 10.1016/j.drugalcdep.2019.01.018
16. Filgueiras AR, Pires de Almeida VB, Koch Nogueira PC, Alvares Domene SM, Eduardo da Silva C, Sesso R, et al. Exploring the consumption of ultra-processed foods and its association with food addiction in overweight children. Appetite. (2019) 135:137–45. doi: 10.1016/j.appet.2018.11.005
17. Pape M, Herpertz S, Schroeder S, Seiferth C, Färber T, Wolstein J, et al. Food addiction and its relationship to weight- and addiction-related psychological parameters in individuals with overweight and obesity. Front Psychol. (2021) 12:736454. doi: 10.3389/fpsyg.2021.736454
18. Praxedes DRS, Silva-Júnior AE, Macena ML, Oliveira AD, Cardoso KS, Nunes LO, et al. Prevalence of food addiction determined by the yale food addiction scale and associated factors: a systematic review with meta-analysis. Eur Eat Disord Rev. (2022) 30:85–95. doi: 10.1002/erv.2878
19. Gearhardt AN, DiFeliceantonio AG. Highly processed foods can be considered addictive substances based on established scientific criteria. Addiction. (2022) 1–10. doi: 10.1111/add.16065
20. LaFata EM, Gearhardt AN. Ultra-processed food addiction: an epidemic? Psychother Psychosom. (2022) 91:363–72. doi: 10.1159/000527322
21. Saure C, Caminiti C, Weglinski J, de Castro Perez F, Monges S. Energy expenditure, body composition, and prevalence of metabolic disorders in patients with Duchenne muscular dystrophy. Diabetes Metab Syndr. (2018) 12:81–5. doi: 10.1016/j.dsx.2017.08.006
22. Walowski CO, Braun W, Maisch MJ, Jensen B, Peine S, Norman K, et al. Reference values for skeletal muscle mass: current concepts and methodological considerations. Nutrients. (2020) 12:755. doi: 10.3390/nu12030755
23. Wang D, Huang K, Schulte E, Zhou W, Li H, Hu Y, et al. The association between food addiction and weight status in school-age children and adolescents. Front Psychiatry. (2022) 13:824234. doi: 10.3389/fpsyt.2022.824234
24. Schiestl ET, Gearhardt AN. Preliminary validation of the Yale Food Addiction Scale for Children 20: a dimensional approach to scoring. Eur Eat Disord Rev. (2018) 26:605–17. doi: 10.1002/erv.2648
25. World Health Organization. Growth reference data for 5–19 years. Geneva: World Health Organization (2007). Available online at: https://www.who.int/tools/growth-reference-data-for-5to19-years/application-tools (accessed June 8, 2021).
26. Kaido T, Uemoto S. Direct segmental multi-frequency bioelectrical impedance analysis is useful to evaluate sarcopenia. Am J Transp. (2013) 13:2506–7. doi: 10.1111/ajt.12373
27. Kafri MW, Potter JF, Myint PK. Multi-frequency bioelectrical impedance analysis for assessing fat mass and fat-free mass in stroke or transient ischaemic attack patients. Eur J Clin Nutr. (2014) 68:677–82. doi: 10.1038/ejcn.2013.266
28. Ellis KJ. Body composition of a young, multiethnic, male population. Am J Clin Nutr. (1997) 66:1323–31.
29. Ellis KJ, Abrams SA, Wong WW. Body composition of a young, multiethnic female population. Am J Clin Nutr. (1997) 65:724–31.
30. Fomon SJ, Haschke F, Ziegler EE, Nelson SE. Body composition of reference children from birth to age 10 years. Am J Clin Nutr. (1982) 35:1169–75.
31. Yekaninejad MS, Badrooj N, Vosoughi F, Lin CY, Potenza MN, Pakpour AH. Prevalence of food addiction in children and adolescents: a systematic review and meta-analysis. Obes Rev. (2021) 22:e13183. doi: 10.1111/obr.13183
32. Schulte EM, Jacques-Tiura AJ, Gearhardt AN, Naar S. Food addiction prevalence and concurrent validity in African American adolescents with obesity. Psychol Addict Behav. (2018) 32:187–96. doi: 10.1037/adb0000325
33. de Almeida VBP, Filgueiras AR, Nogueira PCK, Sesso R, Sawaya AL, Domene SMA. The impact of food addiction behaviours on the treatment of overweight students. Br J Nutr. (2021) 2021:1–23. doi: 10.1017/S0007114521004189
34. Dennis ML, Scott CK, Funk R, Foss MA. The duration and correlates of addiction and treatment careers. J Subst Abuse Treat. (2005) 28:S51–62. doi: 10.1016/j.jsat.2004.10.013
35. Marunowski K, Swietoń D, Bzyl W, Grzywińska M, Kaszubowski M, Bandosz P, et al. MRI-derived subcutaneous and visceral adipose tissue reference values for children aged 6 to under 18 years. Front Nutr. (2021) 8:757274. doi: 10.3389/fnut.2021.757274
36. Dong Y, Bai L, Cai R, Zhou J, Ding W. Visceral adiposity index performed better than traditional adiposity indicators in predicting unhealthy metabolic phenotype among Chinese children and adolescents. Sci Rep. (2021) 11:23850. doi: 10.1038/s41598-021-03311-x
37. Eibl G, Rozengurt E. Obesity and pancreatic cancer: insight into mechanisms. Cancers. (2021) 13:5067. doi: 10.3390/cancers13205067
38. Skinner J, Jebeile H, Burrows T. Food addiction and mental health in adolescents: a systematic review. Lancet Child Adolesc Health. (2021) 5:751–66. doi: 10.1016/S2352-4642(21)00126-7
39. Kapoor E, Faubion SS, Kling JM. Obesity update in women. J Womens Health. (2019) 28:1601–5. doi: 10.1089/jwh.2019.8041
40. Cohen CC, Sekkarie A, Figueroa J, Gillespie SE, Vos MB, Welsh JA. Longitudinal associations of total and trunk fat in childhood and adolescence and risk of hepatic steatosis at 24 years. Pediatr Obes. (2021) 16:e12773. doi: 10.1111/ijpo.12773
41. Cheuiche AV, da Silveira LG, de Paula LCP, Lucena IRS, Silveiro SP. Diagnosis and management of precocious sexual maturation: an updated review. Eur J Pediatr. (2021) 180:3073–87. doi: 10.1007/s00431-021-04022-1
42. Yu Z, Indelicato NA, Fuglestad P, Tan M, Bane L, Stice C. Sex differences in disordered eating and food addiction among college students. Appetite. (2018) 129:12–8. doi: 10.1016/j.appet.2018.06.028
43. McKay C, Wijeakumar S, Rafetseder E, Shing YL. Disentangling age and schooling effects on inhibitory control development: an fNIRS investigation. Dev Sci. (2021) 25:e13205. doi: 10.1111/desc.13205
44. Hartman-Munick SM, Gordon AR, Guss C. Adolescent body image: influencing factors and the clinician's role. Curr Opin Pediatr. (2020) 32:455–60. doi: 10.1097/MOP.0000000000000910
45. Katzmarzyk PT, Chaput JP, Fogelholm M, Hu G, Maher C, Maia J, et al. International study of childhood obesity, lifestyle and the environment (ISCOLE): contributions to understanding the global obesity epidemic. Nutrients. (2019) 11:848. doi: 10.3390/nu11040848
46. Liu Z, Gao P, Gao AY, Lin Y, Feng XX, Zhang F, et al. Effectiveness of a multi-faceted intervention for prevention of obesity in primary school children in China: a cluster randomized clinical trial. JAMA Pediatr. (2022) 176:e214375. doi: 10.1001/jamapediatrics.2021.4375
47. Martoccio TL, Senehi N, Brophy-Herb HE, Miller AL, Horodynski MA, Kaciroti N, et al. Cross-lagged associations between behaviour problems and obesity in head start preschoolers. Pediatr Obes. (2020) 15:e12627. doi: 10.1111/ijpo.12627
48. Petersen MC, Shulman GI. Mechanisms of insulin action and insulin resistance. Physiol Rev. (2018) 98:2133–223. doi: 10.1152/physrev.00063.2017
49. Neves TMG, Simoes E, Otaduy MCG, Calfat ELB, Bertolazzi P, da Costa NA, et al. Inverse association between hypothalamic N-acetyl aspartate/creatine ratio and indices of body mass in adolescents with obesity. J Nutr. (2022) 152:663–70. doi: 10.1093/jn/nxab415
50. Sergi G, De Rui M, Stubbs B, Veronese N, Manzato E. Measurement of lean body mass using bioelectrical impedance analysis: a consideration of the pros and cons. Aging Clin Exp Res. (2017) 29:591–7. doi: 10.1007/s40520-016-0622-6
Keywords: children, adolescents, food addiction, body composition, obesity, longitudinal study, cross-lagged analysis
Citation: Wang D, Zhou H, Hu Y, Che Y, Ye X, Chen J, Fu J and Xu H (2023) Prediction of body fat increase from food addiction scale in school-aged children and adolescents: A longitudinal cross-lagged study. Front. Public Health 10:1056123. doi: 10.3389/fpubh.2022.1056123
Received: 28 September 2022; Accepted: 08 December 2022;
Published: 06 January 2023.
Edited by:
Michelle Plusquin, University of Hasselt, BelgiumReviewed by:
Ashley Nicole Gearhardt, University of Michigan, United StatesCopyright © 2023 Wang, Zhou, Hu, Che, Ye, Chen, Fu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongzhen Xu,  NjE4NDAyMEB6anUuZWR1LmNu; Junfen Fu,
NjE4NDAyMEB6anUuZWR1LmNu; Junfen Fu,  ZmpmNjhAemp1LmVkdS5jbg==
ZmpmNjhAemp1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.