- 1Institute for STI and HIV Control and Prevention, Jiangsu Provincial Center for Disease Control and Prevention, Nanjing, Jiangsu, China
- 2Jiangsu Key Laboratory of Molecular Medicine, Medical School, Nanjing University, Nanjing, Jiangsu, China
- 3Project-China, University of North Carolina, Guangzhou, China
Background: This study aimed to assess the trends and determine the factors associated with late presentation (LP) and advanced HIV disease (AHD) among newly diagnosed people living with HIV (PLWH) from 2008 to 2020 in Jiangsu, China.
Methods: Newly diagnosed PLWH registered in the HIV surveillance system from 2008 to 2020 were included. Multivariable logistic regression models were used to analyze the factors associated with LP and AHD. The LP and AHD trends were assessed using Joint-point analysis.
Results: Of 37,251 newly diagnosed PLWH identified, 30,251(81.2%) patients met the inclusion criteria. Among those, 16,672 (55.1%) were considered LP, and 8,691 (28.7%) had AHD. LP trends steadily increased from 2008 (39.0%) to 2020 (59.4%), but AHD trends decreased visibly from 2016 (32.3%) to 2020 (23.4%). The overall median CD4 trends decreased slowly from 389 to 305 cells/mm3 between 2008 and 2020. Married patients and those older than 35 years were more likely to be LP and have AHD. Patients infected via heterosexual transmission had a higher risk of being classified as AHD (aOR: 1.13, 95%CI: 1.06–1.21) than patients infected via homosexual transmission. Patients that were diagnosed at sexually transmitted infections (STIs) clinics (aOR: 1.10, 95%CI: 1.01–1.20) and in hospitals (aOR: 1.69, 95%CI: 1.59–1.79) were more likely to be classified as LP compared with patients diagnosed at voluntary counseling and testing (VCT) centers. Similar, patients diagnosed at STIs clinics (aOR: 1.23, 95%CI: 1.11–1.36) and hospitals (aOR: 2.27, 95%CI: 2.12–2.43) were more likely to have AHD than patients diagnosed in VCT.
Conclusion: Our findings indicate an alarming burden of LP in Jiangsu, suggesting the need for more attention toward HIV diagnosis at early CD4 stages. National HIV control programs must strengthen comprehensive interventions for HIV prevention and promote HIV services. Also, strategies for HIV prevention (PrEP and PEP), testing, and treatment must be extended, especially among the general population.
Introduction
Timely linkage to the care and antiretroviral therapy (ART) initiation plays multiple beneficial roles in HIV control and prevention (1). The timely diagnosis of an HIV infection is the first and crucial step to achieving benefits like preventing onward transmission and reducing the risks of acquired immune deficiency syndrome (AIDS) through early treatment initiation. Late presentation (LP) is a valuable marker that reflects the attendance of patients seeking HIV-related care early (2). LP could cause many consequences, such as increasing HIV related morbidity and mortality (3–7), high risks of onward HIV transmission (8–10), and cost of care (10). Advanced HIV disease (AHD) meant a lower CD4+ cell count when PLWH sought HIV related health care, which reduced their probability of survival even though they initiated ART immediately (11, 12). Meanwhile, AHD increases the odds of severe HIV-related clinical events like tuberculosis (13), severe bacterial infections, Cryptococcal meningitis, and toxoplasmosis (14). Therefore, monitoring trends in LP/AHD could identify HIV-related healthcare early and prevent further transmission.
Additionally, LP is a global issue of great concern to researchers as it hinders the achievement of the UNAIDS 95-95-95 goals toward ending HIV by 2030 (15, 16). Many studies have investigated the prevalence of LP and AHD using cross-sectional studies. One large cross-sectional study in Metropolitan France in 2014 found that 47.7% of participants were LP, and 29.3% were AHD (8). Another study found that the LP prevalence in Europe between 2010 and 2016 varied considerably by region, from 64.2% in central Europe to 47.1% in East Europe and 48.4% in the West (17). In 2012, Tang et al. observed that 63.8% of LP-categorized HIV diagnoses were from four areas in China (Henan, Guangxi, Guangdong, and Yunnan) (18). The rate of LP remained high and stable for many years in many cohort studies. One study, conducted in Canada from 1999 to 2013, found that the prevalence of LP varied slightly from 50.9 to 57.4% (19). Results from a multicenter cohort study during 2004–2018 revealed that the prevalence of LP decreased from 51.8% (2004–2008) to 40.9% (2009–2012), then remained stable at 42.0% during 2013 to 2018 in Spain (20). However, information on the long-term change in LP and AHD trends, a valuable indicator for HIV testing promotion programs, is limited in China. A study in southwestern China reported a 5-year trend on LP and AHD and saw that the percentage of LP and AHD remained stable at 70.2 and 45.1%, respectively (2).
Jiangsu, located in eastern China, belongs to the Yangtze-river economic zone, one of China's three the most developed areas, but this zone's data on LP and AHD over a long period is limited. Our study findings may be more representative in showcasing the LP and AHD trends since the duration span over 13 years and were conducted within the Yangtze-river economic zone. Understanding the LP and AHD situations and trends is essential in guiding future HIV prevention and care programs in Jiangsu province. So, the purpose of this study was to firstly assess the rate trends of LP and AHD in Jiangsu from 2008 to 2020, and secondly identify the potential driving forces of LP and AHD to provide evidence for decreasing the rate of LP and AHD in the province.
Materials and methods
Ethical statement
This was a serial cross-sectional study using annual data extracted from the web-based Comprehensive Response Information Management System (CRIMS). CRIMS is a real-time case reporting system for all notifiable infectious diseases in China. For HIV/AIDS, the newly diagnosed people will get into the healthcare system, and be recorded sequential information using a standard questionnaire for every follow-up visit. The eligible data were de-identified before the data analysis. The study's process and contents were reviewed and approved by the National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention (No. of IRB Application: X140121318).
Study population
We included data on newly diagnosed PLWH registered in the CRIMS in Jiangsu Provincial Center for Disease Control and Prevention between January 2008 and December 2020. The inclusion criteria were as follows: (1) HIV positive, (2) aged at least 15 years, (3) had a CD4+ T-cell count test within 6 months after HIV diagnosis, (4) ART-naïve when the first CD4+ T-cell count was detected.
Study design
Information was collected using the standard surveillance forms on the following variables: socio-economic data, including age at HIV diagnosis, gender, ethnicity, level of education, marital status, migration status, and history of sexually transmitted infections (STIs). We determined migratory status based on patients' official household registrations. Patients who did not have official household registration in Jiangsu when first diagnosed with HIV were deemed immigrants (21). We also recorded the information on ethnicity from the identification card, a standard definition in the census.
The information of route of HIV infection was judged by professional clinicians when patients were diagnosed HIV infection firstly based on self-report risk behaviors. There are four types of route transmission, named as homosexual, heterosexual, inject drug user (IDU), others did not disclose their potential transmission routes. We classified routes of HIV infection as homosexual, heterosexual, IDU and others in this study.
Clinical data also recorded by CRIMS, included: the year of HIV diagnosis, CD4+ T-cell count after HIV diagnosis and place of HIV testing.
LP in this study referred to patients having the first-ever CD4 testing (<350cells/mm3) or presented a AIDS-defining illness regardless of the CD4+ T-cell count during HIV diagnosis. If patients had the first-ever CD4 testing (≥350 cells/mm3) during HIV diagnosis, we defined these patients as non-LP. AHD was defined as patients had first-ever CD4+ T-cell count (<200 cells/mm3) or presented a AIDS-defining illness regardless of the CD4+ T-cell count during HIV diagnosis (22). On the contrary, if patients had the first-ever CD4 testing (≥200 cells/mm3) during HIV diagnosis, we defined these patients as non-AHD.
Statistical analysis
Join-point regression was estimated for general and transmission group to identify changes in the proportion of LP and AHD trends and the median CD4 levels. This analysis was done using the Join-point regression Program, Version 4.9.1.0 (Statistical Research and Applications Branch, National Cancer Institute). In brief, by using LP and AHD proportions and median of CD4 as inputs, this method identifies the years when a trend change is produced. It calculates the annual percentage change (APC) between trend-change points. It also estimates the average annual percentage (APPC) in the whole period. We obtained the number of join points via Monte Carlo resampling (23). Based on the disparities of variables, a maximum number of two points was allowed, ensuring the results were credible. We choose the exact join points owing to the smallest Bayesian Information Criterion (24). All results were presented in the Supplementary material.
We assessed factors associated with LP and AHD in a univariate logistic regression, firstly. Variables with P-values <0.2 were entered into a multivariable logistic regression model. Results were presented based on odds ratios (OR) and their 95% confidence interval (CI). All analyses were performed using IBM SPSS STATISTICS (version 19.0, SPSS Inc., Chicago, IL, USA).
Results
Characteristics of LP and AHD
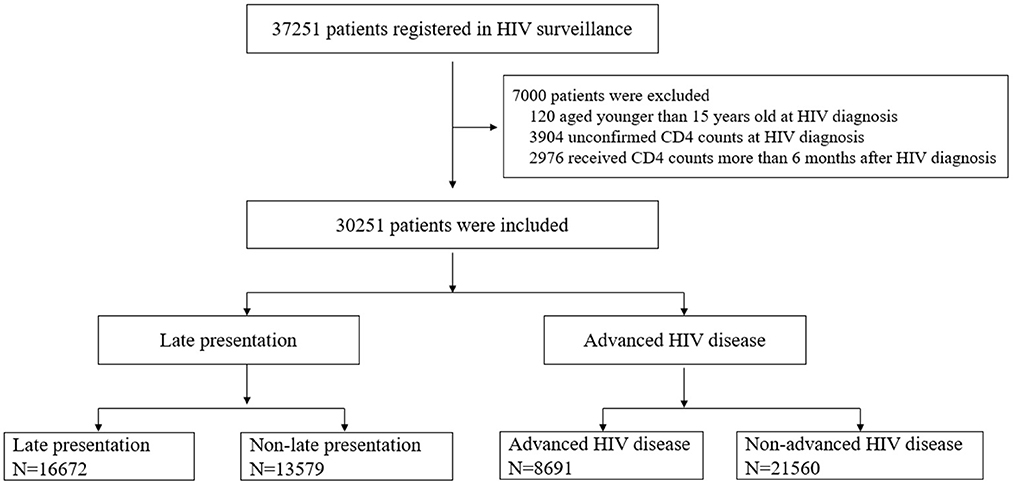
In total, 37,251 patients were identified during the study period, of which 30,251(81.2%) met the inclusion criteria. 7,000(18.8%) patients were excluded from the study. Among the excluded patients, 120(0.3%) were below 15 years old at first HIV diagnosis, and 3,904(10.5%) PLWH did not receive CD4+ T-cell count tests after the first HIV diagnosis. 2,976(8.0%) PLWH did not receive CD4+ T-cell count within 6 months after HIV diagnosis. The median age of the included cases was 38 years old (IQR: 26–49). Further details are in Figure 1.
Overall, 16,672 (55.1%) patients were LP, and 8,691 (28.7%) were AHD based on the 2008 to 2020 retrieved study data. The overall rate trends of LP and AHD were presented in Supplementary Table 1.
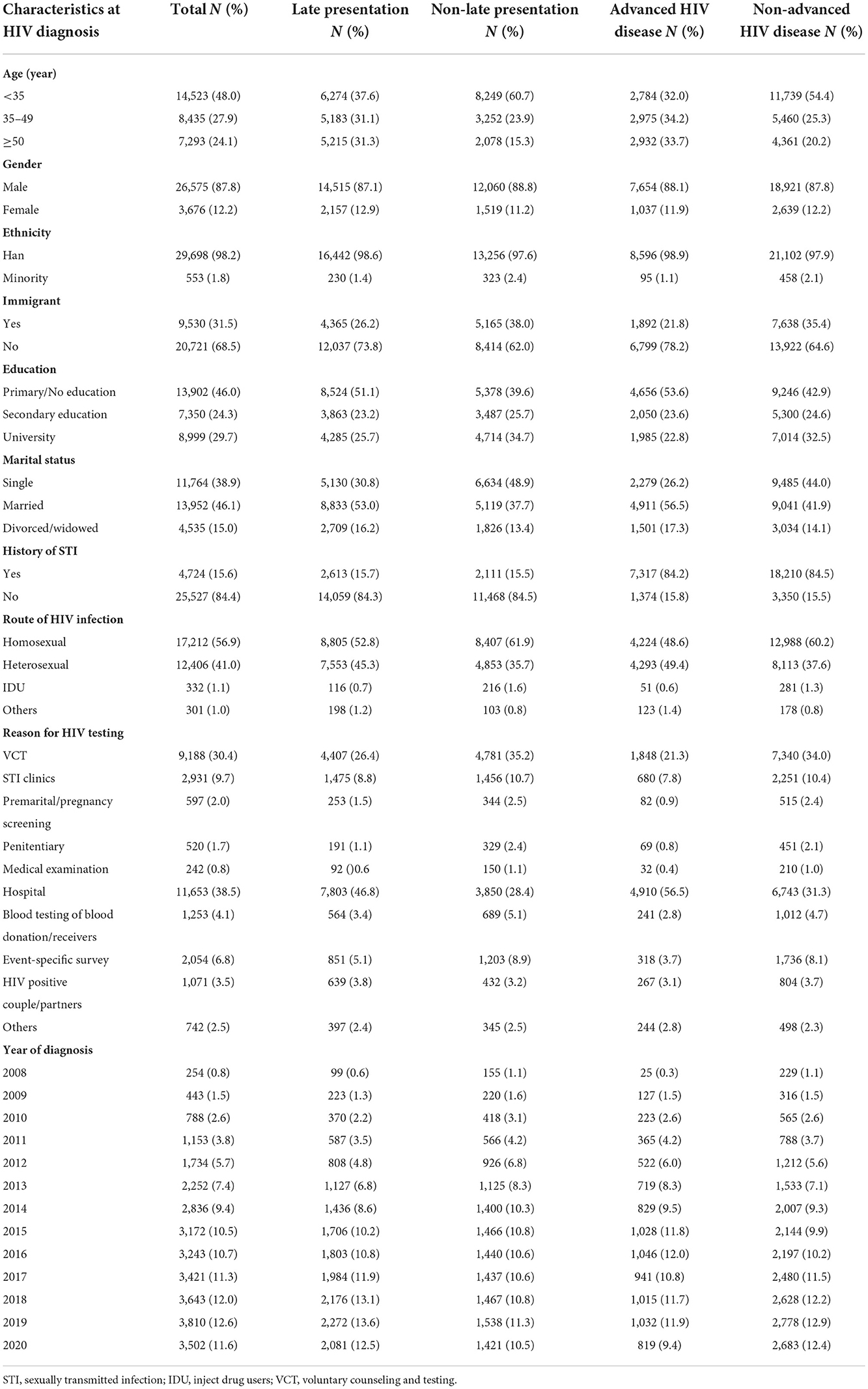
Most LP patients were <35 years old (37.6%), of Han ethnicity (98.6%), residents of Jiangsu (73.8%), with primary education or below (51.1%), and married (53.0%). Additionally, 52.8% of LP patients became HIV infected via homosexual transmission, 46.8% were diagnosed in hospitals, and 26.4% received their first-ever diagnosis at voluntary counseling and testing (VCT) center. However, LP was high among hospital diagnosed patients (67.0%) (Table 1).
Among AHD patients, 33.7% were over 50 years, 98.9% were of Han ethnicity, 78.2% were residents of Jiangsu province, 53.6% had primary education or below, and 56.5% were married. Most AHD patients became HIV infected through heterosexual transmissions (49.4%), and AHD was more prominent among patients diagnosed in hospitals (56.5%) (Table 1).
Trends of LP and AHD by transmission routes
The rate of LP increased from 39.0 to 59.4% between 2008 to 2020 (APC = 2.7, 95%CI (2.0, 3.4), P < 0.001). The rate of AHD increased from 9.8 to 32.3% from 2008 to 2016 (APC = 1.6, 95%CI (−2.8, 6.2), P = 0.433), then decreased from 32.3 to 23.4% during 2016 to 2020 (APC = −6.8, 95%CI (−13.4, 0.3), P = 0.057) (Figure 2; Supplementary Tables 1, 5). The APPC in the whole period was 2.7 (95%CI: 2.0, 3.4) and −1.3 (95%CI: −4.5, 2.0) for LP and AHD, respectively (Supplementary Table 5).
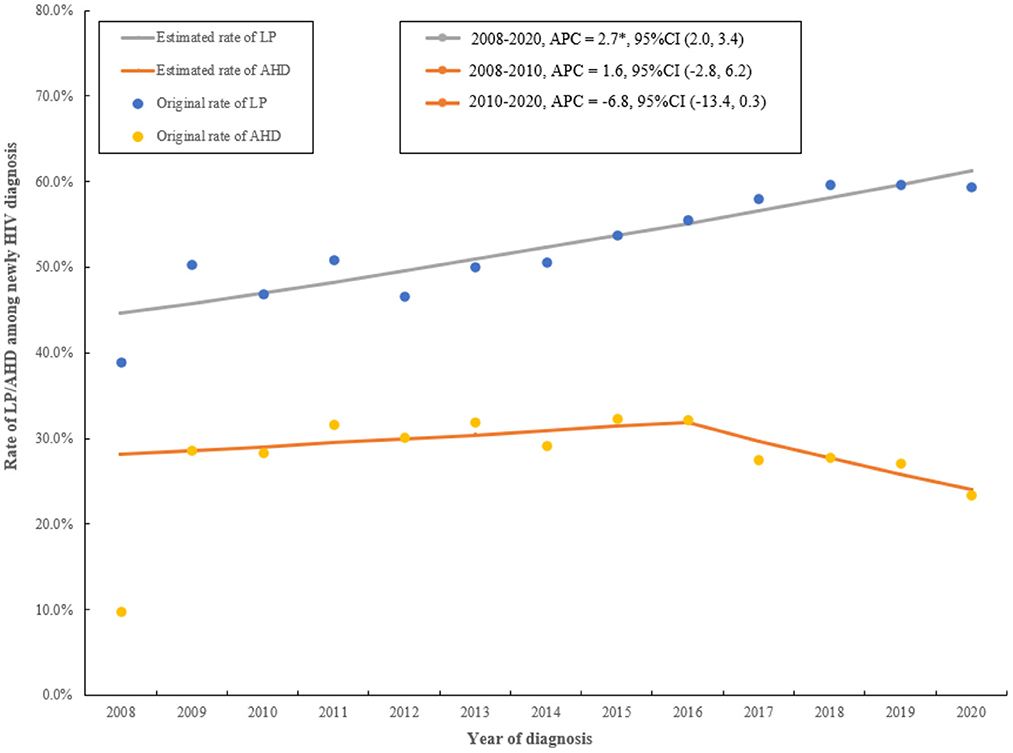
Figure 2. The trends of original and estimated rate for LP and AHD from 2008 to 2020, in Jiangsu, China. LP, late presentation; AHD, advanced HIV disease; APC, annual percentage change; CI, confidence interval; *P < 0.05.
Figure 3 and Supplementary Tables 2, 3 demonstrates the trends of LP and AHD between 2008 and 2020 by transmission groups, respectively. The rate of LP rose from 34.5 to 55.6% (APC = 3.2, 95%CI (2.2, 4.1), P < 0.001) (Figure 3A) for homosexual transmission, 38.1 to 64.4% (APC = 2.2, 95%CI (1.5, 2.9), P < 0.001) (Figure 3B) for heterosexual transmission, and 40.0 to 75.0% (APC = 7.2, 95%CI (1.5, 13.2), P = 0.017) (Figure 3C) for IDU between 2008 and 2020, respectively. The proportion of AHD dropped from 28.3 to 19.4% (APC = −5.8, 95%CI (−10.4, −1.0), P = 0.025) (Figure 3E) for homosexual transmission group, and 39.9 to 28.6% (APC = −6.4, 95%CI (−12.2, −0.3), P = 0.043) (Figure 3F) for heterosexual transmission during 2015 to 2020, respectively.
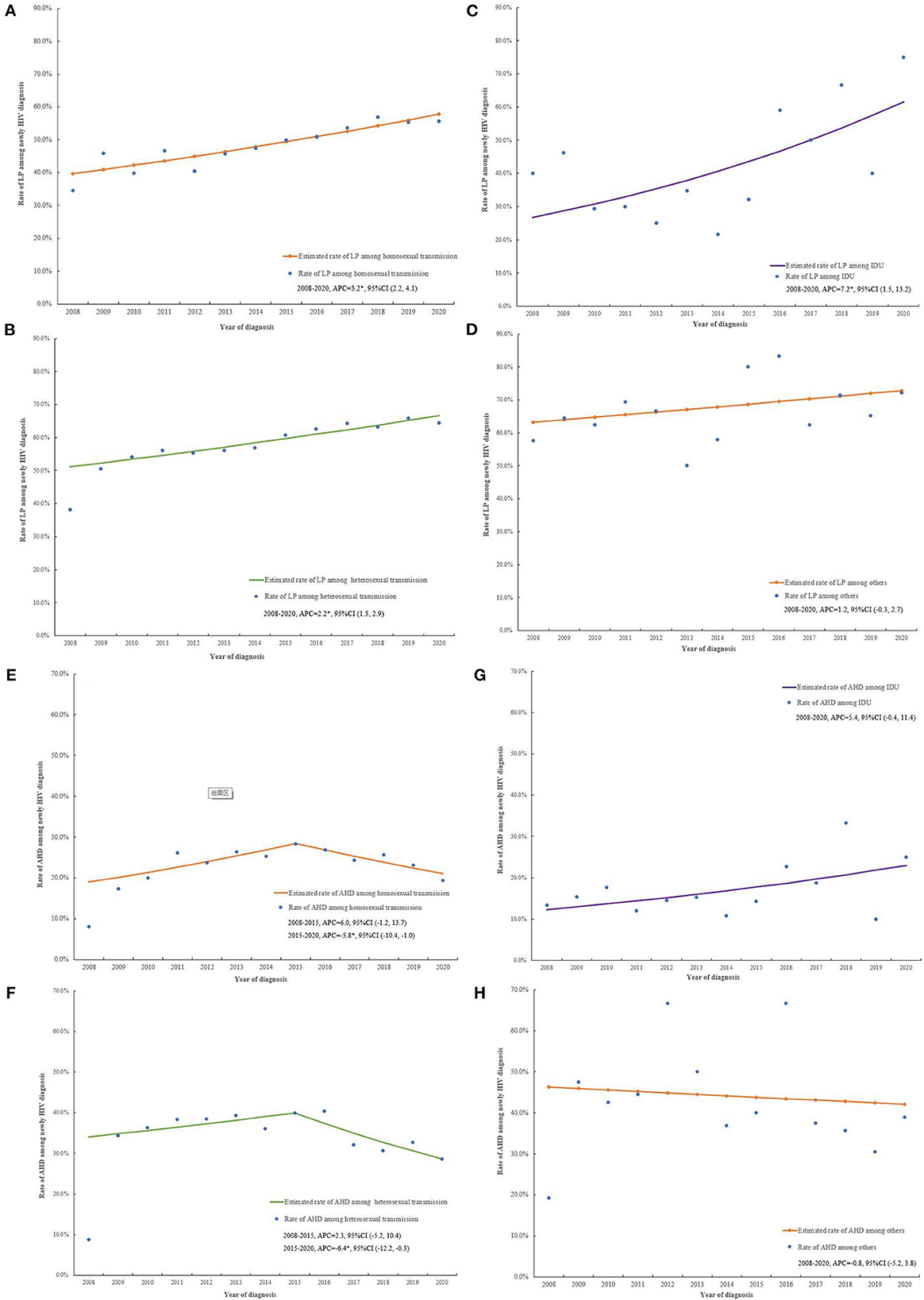
Figure 3. The trends of original and estimated rate for LP and AHD by transmission routes. The rate trends of LP among homosexual transmission (A), heterosexual transmission (B), IDU (C), and others (D) from 2008 to 2020 in Jiangsu. The rate trends of AHD among homosexual transmission (E), heterosexual transmission (F), IDU (G), and others (H) from 2008 to 2020, in Jiangsu, China. LP, late presentation; AHD, advanced HIV disease; APC, annual percentage change; CI, confidence interval; *P < 0.05.
The APC and APPC of LP and AHD between 2008 and 2020 by transmission groups were in Supplementary Table 6.
Trends of median CD4 level by transmission routes
The general median CD4 level dropped from 389 to 305 cells/mm3 (APC = −2.0, 95%CI (−2.5, −1.5), P < 0.001) between 2008 and 2020 (Figure 4A, Supplementary Table 4). The median CD4 level dropped from 419 to 322 cells/mm3 (APC = −1.9, 95%CI (−2.6, −1.3), P < 0.001) (Figure 4B) for homosexual transmission, 405 to 312 cells/mm3 (APC = −1.7, 95%CI (−4.0, 0.6), P = 0.132) for IDU (Figure 4D), 308 to 252 cells/mm3 (APC = 0.0, 95%CI (−1.5, 1.5), P = 0.998) for others (Figure 4E) between 2008 and 2020, respectively. For heterosexual transmission, median CD4 level decreased slightly from 327 to 281 cells/mm3 (APC = −1.8, 95%CI (−2.3, −1.3), P < 0.001) during 2010 and 2020 (Figure 4C).

Figure 4. The trends of median CD4 level for general (A), homosexual transmission (B), heterosexual transmission (C), IDU (D), and others (E) from 2008 to 2020, in Jiangsu, China. APC, annual percentage change; CI, confidence interval; *P < 0.05.
The APC and APPC of median CD4 levels by general and transmission groups between 2008 and 2020 were presented in Supplementary Tables 7, 8.
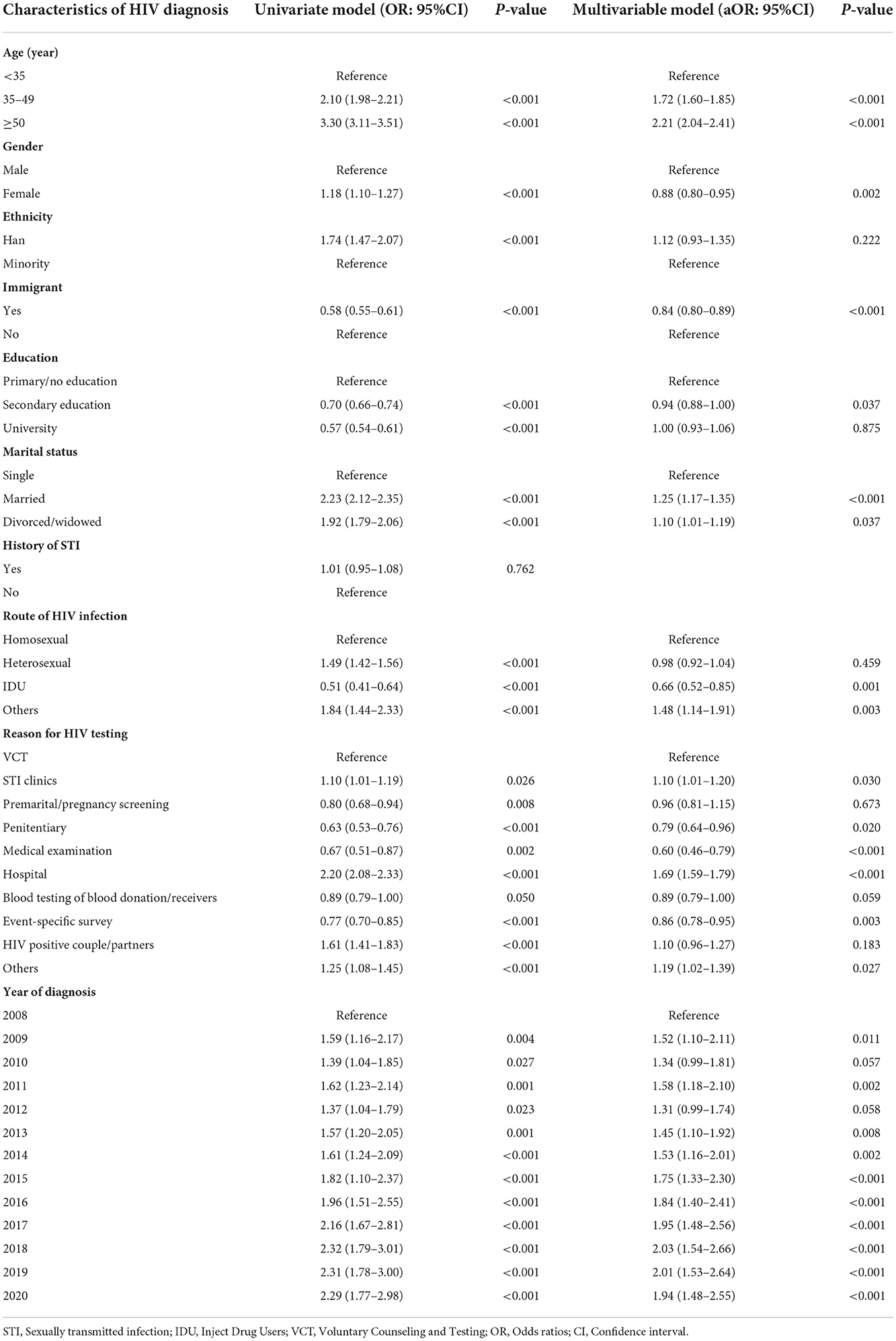
Factors associated with LP
In the univariate model, risk factors associated with LP were being older than 35 years, female, of Han ethnicity, married or divorced/widowed, getting HIV from heterosexual transmission, diagnosed at STIs clinics or hospitals, having partners living with HIV, diagnosed after 2008 (Table 2).
In the multivariable model, risk factors associated with LP were: being older than 35 (35–49: aOR: 1.72,95%CI: 1.60–1.85; P < 0.001; ≥50 years old: aOR: 2.21, 95%CI: 2.04–2.41; P < 0.001) and being married (aOR: 1.25, 95%CI: 1.17–1.35; P < 0.001). Additionally, patients diagnosed at STIs clinics (aOR: 1.10, 95%CI: 1.01–1.20; P = 0.030), and hospitals (aOR: 1.69, 95%CI: 1.59–1.79; P < 0.001) tended to be LP. On the contrary, immigrants (aOR: 0.84, 95%CI: 0.80–0.89; P < 0.001), received secondary education (aOR: 0.94, 95%CI: 0.88–1.00; P = 0.037), transmitted by IDU (aOR: 0.66, 95%CI: 0.52–0.85; P = 0.001) were less likely to LP. Meanwhile, PLWH diagnosed at penitentiary sites (aOR: 0.79, 95%CI: 0.64–0.96; P = 0.020), or medical examination sites (aOR: 0.60, 95%CI: 0.46–0.79; P < 0.001), or event-specific survey (aOR: 0.86, 95%CI: 0.78–0.95; P = 0.003) were less likely to LP (Table 2).
Being female were tended to be LP in univariate model, but turned to be a protective factor in multivariable model. PLWH were of Han ethnicity, received university education, getting HIV from heterosexual transmission, diagnosed by premarital or pregnancy screening were tended to be LP in univariate model, but these factors did not confirm as risk factors in multivariable model (Table 2).
Factors associated with AHD
In the univariate model, patients older than 35, of Han ethnicity, and married or divorced/widowed, infected through heterosexual transmission, obtained HIV tests at STIs clinics or hospital, having partners living with HIV, and diagnosed after 2008 tended to be AHD (Table 3).
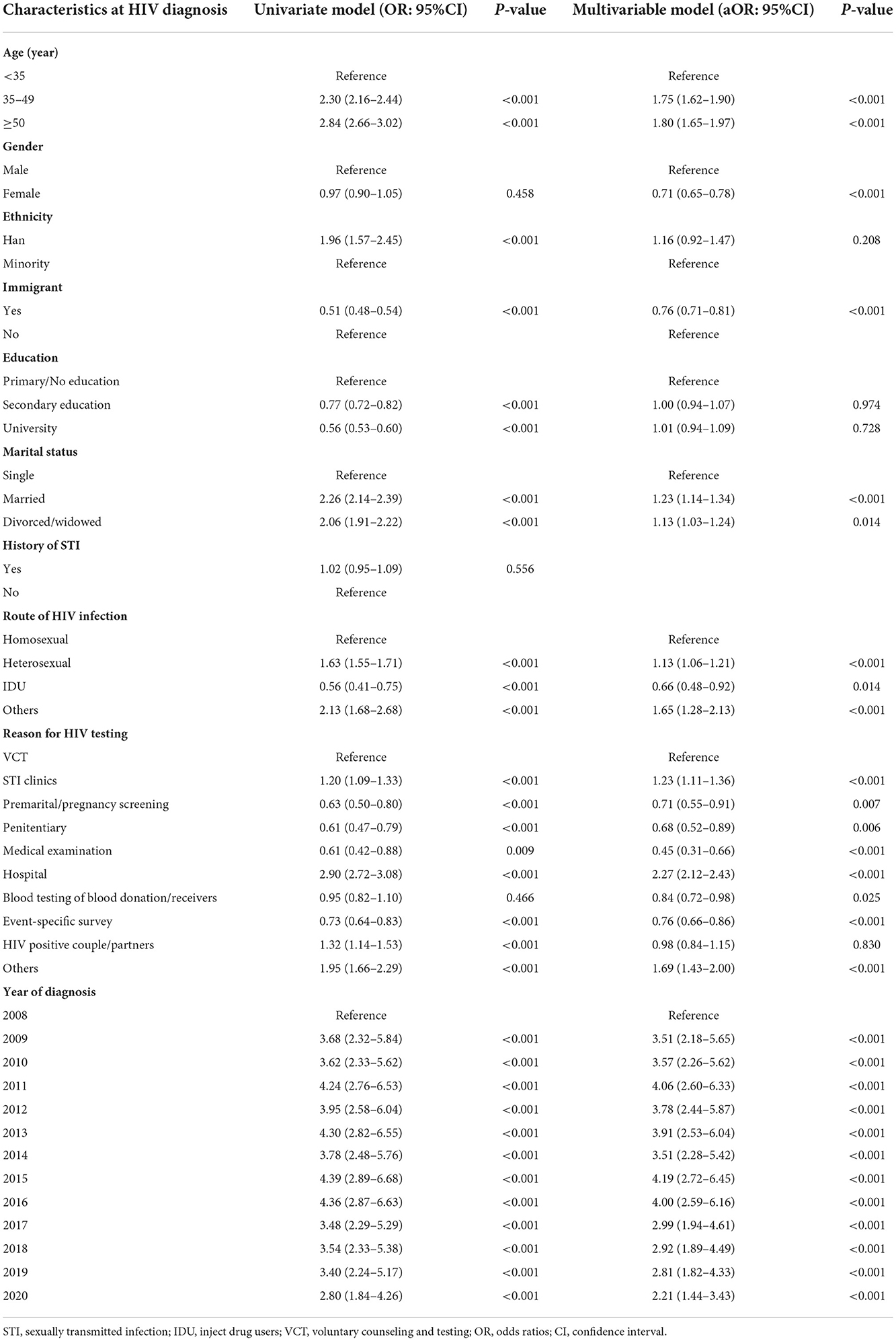
Table 3. Risk factors associated with advanced HIV disease presentation in Jiangsu province, China, 2008–2020.
In the multivariable model, factors associated with AHD were: older than 35(35–49: aOR: 1.75,95%CI: 1.62–1.90; P < 0.001; ≥50 years old: aOR: 1.80, 95%CI: 1.65–1.97; P < 0.001), and married (aOR: 1.23, 95%CI: 1.14–1.34; P < 0.001) or divorced/widowed (aOR: 1.13, 95%CI: 1.03–1.24; P = 0.014). Patients infected via heterosexual transmission (aOR: 1.13, 95%CI: 1.06–1.21; P < 0.001) were more likely to be AHD. Patients diagnosed in STIs clinics (aOR: 1.23, 95%CI: 1.11–1.36; P < 0.001), hospital (aOR: 2.27, 95%CI: 2.12–2.43; P < 0.001) tended to be AHD. However, PLWH were immigrants (aOR: 0.76, 95%CI: 0.71–0.81; P < 0.001), transmitted by IDU (aOR: 0.66, 95%CI: 0.48–0.92; P = 0.014) less likely to have AHD. Meanwhile, PLWH received HIV testing from premarital or pregnancy screening sites (aOR: 0.71, 95%CI: 0.55–0.91; P = 0.007), penitentiary sites (aOR: 0.68, 95%CI: 0.52–0.89; P = 0.006), medical examination (aOR: 0.45, 95%CI: 0.31–0.66; P < 0.001), blood testing of blood donation (aOR: 0.84, 95%CI: 0.72–0.98; P = 0.025), or event-specific survey (aOR: 0.76, 95%CI: 0.66–0.86; P < 0.001) were less likely to have AHD (Table 3).
PLWH were of Han ethnicity, received secondary or university education, and having seroconvert partners were tended to have AHD in univariate model, but these factors did not confirm as risk factors in multivariable model (Table 3).
Discussion
In this serial cross-sectional study, we enrolled 81.2% (25, 26) of all newly diagnosed PLWH registered in the CRIMS in Jiangsu province. We observed that the percentage of LP and AHD was high and posed an alarming problem to HIV prevention and control interventions in Jiangsu. More than 50% of patients were LP, and nearly one third were AHD patients. The AHD trend has visibly decreased since 2016. However, LP trend increased steadily from 2008 to 2020 during the study period, indicating that LP was a consistent problem in Jiangsu, China. LP may be due to HIV testing policies and the complexities of transmission dynamics, including complicated high-risk subgroups, interlaced and multiple transmission routes in Jiangsu.
The coverage disparity in HIV testing between high-risk and general population might facilitate the increasing trend of LP. The Chinese government initiated a policy, “the Five expand and six strengthen,” to cope with the increasing challenges since 2010 (25). With the “Five Expands, Six Strengthens” policy, HIV testing increased from 4.87 million to 10.92 million in the study period in Jiangsu. However, most HIV testing was facility-based as testing pre-surgery and in-patient, which is a mandatory test in hospitals, accounted for 56% of testing recorded. A high rate of LP implies a gap in accessibility to testing services or that people lack the willingness or sensitivity for HIV testing, especially among the general population (27–30). Previous studies reported an HIV testing coverage of 77.3% for men who have sex with men (MSM), 76.7% for female sex workers, and 53.8% for drug users, among high-risk populations (26, 31). At the same time, the prevalence of any HIV testing service uptake in a lifetime was only 25.2% among the general population (32). In addition, proportion of HIV diagnosed cases over 50 years old has increased steadily, which may facilitate the increasing trend of LP. The proportion of sexual transmission has been the dominant route of HIV transmission since 2007 (33), and the more and more evidence showed increased HIV prevalence among older adults compared with the general population. The knowledge of HIV/AIDS prophylaxis in this population group was lower than other population groups in China (34, 35). Meanwhile, the 86.2% rate of unprotected sexual activities among older adults, especially during commercial sex, was much higher than in the younger population (36–38). Also, our study findings indicated that older age was a risk factor for LP. Hence, the government must allocate more resources to increase HIV awareness in the general population and encourage provider-initiated HIV testing and counseling (PITC) to facilitate early HIV diagnosis.
AHD trend varied slightly over years since 2009. Then, AHD trend declined visibly during 2016 and 2020. The declining AHD trend is encouraging and may be attributed to the successful progress of multiple HIV interventions, such as HIV testing expansion, treat all policy, continual improvement on linkage to care and awareness of AIDS prevention work. Evidence shows that the rate of new HIV infections is declining nationwide in China (39, 40). However, the number of newly diagnosed HIV infections still increases annually, which means that many undiagnosed HIV cases exist (41). So, the Chinese government encouraged regular HIV testing every 3–6 months among high-risk population. With this policy, HIV testing coverage in the past 12 months increased from 43.7 to 64.4% from 2009 to 2022, which gave them more opportunities for early diagnosis (31, 42). For general population, the government had initiated PITC for older who attend hospital for medical examination and patients who attend STIs clinics. Based on the subgroup analysis in this study, the trend of AHD decreased visibly in the subpopulation aged older than 50 years, signified the amazing progress on the HIV testing expansion. Followed the contrasting trends of LP and AHD, the policy to expand HIV testing may have provided more chances to enroll the concealed sub-population who were less willing to get tested but aware of possible HIV infection based on the progression of CD4+ T-cell count.
Additionally, China's ART policy has undergone a series of adjustments over the study period. From 2008 to 2009, the indicator for free ART initiation was CD4+ T-cell count of <200 cells/mm3 or advanced AIDS status. That changed to CD4+ T-cell count <350 cells/mm3 from 2010 to 2013, and <500 cells/mm3 between 2014 to 2015. Currently, treat all without considering the CD4+ T-cell count since 2016 (43). As it overlapped with the 'immediate treatment' policy, AHD trends decreased visibly from 32.3 to 23.4% from 2016 to 2020. The variations in AHD trends following the ART policy suggest that the treatment policy encouraged the presentation of hidden HIV infections. Meanwhile, the chain of linkage to care continued improving in China. In China, multiple steps might interrupt the linkage chain, such as confirmatory testing, obtaining HIV testing result, being evaluated ART eligibility, and receiving ART and care at designated hospital (44). One study found that 21% of MSM with a HIV positive screening test did not receive confirmatory testing in 2014 (45). With trained peers providing point-of-care testing and case management, nearly 0.2% of MSM lost to receive confirmatory testing (46). Meanwhile, center of “one-stop service,” might short duration between HIV diagnosis and linkage to care, also improve the healthcare system service (47). Compared with prior to implementing one-stop service, the coverage rate of CD4 testing rose by 69.2%, and proportion of ART initiation rose by 3 times within 30 days after HIV diagnosed (48). Furthermore, the risk of opportunistic infection increased with CD4 decline, which may have given patients more prompting to seek healthcare and diagnosis. The decreasing AHD trend may also signify the benefits of declining HIV-related disease burden, such as opportunistic infections, morbidity, and mortality.
In this study, LP and AHD trends among persons infected via homosexual transmission were always lower than the heterosexual transmission. A few reasons could explain this phenomenon. First, the coverage of HIV testing in the last 12 months among homosexuals and other high-risk groups has increased rapidly over the past few years in Jiangsu (49, 50), which give them more opportunities for early diagnosis. Our data also showed that the section of homosexuals diagnosed with HIV within the given period was younger than the group of diagnosed heterosexuals. Young homosexual patients were more likely to know about HIV prevention and HIV testing (29). Also, provisions like training by community-based organizations enable peers to provide rapid HIV testing with social support and case management also expanded HIV testing and maybe decreased the chance of LP since 2014 in Jiangsu (46). However, there were no effective strategies for HIV testing among heterosexuals in China. The success in expanding HIV testing in homosexuals can give some clues to HIV testing strategies to reduce LP rates.
The results in this study are consistent with previous literatures finding that women are less likely than men to be LP or AHD (19, 47). One possible reason was that women have a high likelihood of being tested in their lifetime; for example, they are tested during routine prenatal testing or gynecological follow-up (48). Another explanation was that women who get infected with HIV experience a slower disease development than men (49). However, men do not have enough resources or reasons for HIV testing, especially in their young age. Lack of opportunities to get HIV testing might led to LP and AHD.
Some previous studies have identified IDU as a population at high risk of LP (12, 13). However, in our data, IDU, had a lower risk of LP. In China, drugs are the prohibited activity. When IDU are apprehended by the government, HIV testing is a mandatory test in IDU. Meanwhile, the government built many methadone maintenance therapy (MMT) facilities for drug users to help them. These MMT facilities also provide basic medical care. In addition, IDU usually have poor health, which give them more reasons to visit a hospital or some other health care facilities. In these conditions, IDU have an increased chance of being tested for HIV (50).
The disparity of LP and AHD should be concerned among different marital status. In our study, current married was identified as risk factor for LP and AHD. This finding is supported by previous researches conducted in other provinces in China (51, 52). PLWH faced a highly stigma nationwide, associated with lower rate of HIV testing and lower willingness to linkage to health care (53–55). Highly stigma might delay or inhibit presentation to HIV care (56). A cross-sectional study conducted in 2014 in China found that only half of participants disclosed their HIV status to spouses (57). Without enough social support, PLWH received ART at home also increased the risk of HIV disclosure.
Our study may have some limitations. First, 18.8% of patients did not receive CD4+ T-cell count tests or receive CD4+ T-cell count tests within 6 months after their initial HIV diagnosis. There were significant differences in the basic characteristics between included and excluded patient data. These differences could have resulted in selection bias and underestimated the overall percentages of LP and AHD. Second, most patients self-reported their high-risk behaviors. Hence, some misreporting may have occurred due to fear of stigma or misunderstanding, especially for patients who have had homosexual contact or have a history of IDU (32, 58). Third, we also lack data on CD4+ T-cell count before HIV infection in our database, since we could not evaluate the dynamic of CD4 level to correct the LP proportion based on the disparity of HIV genotypes (59). Even though, China's national guidelines of Prep and Pep were promulgated in 2021. There still some people got access to PrEP or PeP by purchasing the drug on the internet or neighboring countries, especially MSM (60). That might underestimate the rate of LP and AHD. Finally, we could not ignore the impact of COVID-19 pandemic on the continuum of HIV related healthcare system, which might overestimate the rate of LP (61). However, the sample size was large, and the study period was lengthy. The risk factors associated with LP and AHD identified in this study are consistent with the findings of previous similar studies. So, our study could be representative of the whole province.
Conclusions
This study provides provincial representative data on LP and AHD trends among PLWH in Jiangsu. The percentage of LP was relatively high and increased steadily over the years, so we should focus more on expanding early HIV diagnosis strategies. Meanwhile, AHD trends decreasing visibly in 2016 suggest that the comprehensive intervention strategies for HIV prevention are effective and should be strengthened. Especially the awareness of HIV prophylaxis and HIV testing rates among the general population should be scaled-up through provider-initiated HIV testing and counseling methods.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by China National Center for AIDS/STD Control and Prevention and the Center for Disease Control and Prevention. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
LS and GF had the original idea. XL, HH, TQ, YuhC, XX, YunC, ZZ, YZ, and JL collected the data. LS, WT, and YuhC analyzed the data. LS wrote the main manuscript text. All authors contributed to manuscript revision and approved the submitted version.
Acknowledgments
The authors acknowledge Center for Disease Control and Prevention staff in Jiangsu. The authors also acknowledge Gifty Marley for language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1054765/full#supplementary-material
Abbreviations
ART, Antiretroviral therapy; AIDS, Acquired immune deficiency syndrome; LP, Late presentation; PLWH, Persons living with HIV; AHD, Advanced HIV disease; CRIMS, Comprehensive Response Information Management System; STIs, Sexually transmitted infections; IDU, Inject Drug Users; APC, Annual percentage change; APPC, Average annual percentage; VCT, Voluntary Counseling and Testing; MSM, Men who have sex with men; PITC, Provider-initiated HIV testing and counseling; MMT, Methadone maintenance therapy.
References
1. Sun C, Li J, Liu X, Zhang Z, Qiu T, Hu H, et al. Hiv/Aids late presentation and its associated factors in china from 2010 to 2020: a systematic review and meta-analysis. Aids Res Ther. (2021) 18:96. doi: 10.1186/s12981-021-00415-2
2. Hu X, Liang B, Zhou C, Jiang J, Huang J, Ning C, et al. Hiv late presentation and advanced hiv disease among patients with newly diagnosed hiv/aids in southwestern china: a large-scale cross-sectional study. Aids Res Ther. (2019) 16:6. doi: 10.1186/s12981-019-0221-7
3. Li MC, Ko NY, Wang LY. The moderator effect of retention in care on late presentation in HIV-infected patients. Aids Care. (2020) 32:93–7. doi: 10.1080/09540121.2019.1640848
4. Tominski D, Katchanov J, Driesch D, Daley MB, Liedtke A, Schneider A, et al. The late-presenting hiv-infected patient 30 years after the introduction of HIV testing: spectrum of opportunistic diseases and missed opportunities for early diagnosis. HIV Med. (2017) 18:125–32. doi: 10.1111/hiv.12403
5. Luma HN, Jua P, Donfack OT, Kamdem F, Ngouadjeu E, Mbatchou HB, et al. Late presentation to hiv/aids care at the douala general hospital, cameroon: its associated factors, and consequences. Bmc Infect Dis. (2018) 18:298. doi: 10.1186/s12879-018-3204-8
6. Deen L, Cowan S, Wejse C, Petersen JH, Norredam M, et al. Travellers refugees and family-reunified immigrants have a high incidence of hiv diagnosis and late presentation compared with Danish born: a nationwide register-based cohort. Study Infect. (2018) 46:659–67. doi: 10.1007/s15010-018-1167-8
7. Guaraldi G, Zona S, Menozzi M, Brothers TD, Carli F, Stentarelli C, et al. Late presentation increases risk and costs of non-infectious comorbidities in people with HIV: an Italian cost impact study. Aids Res Ther. (2017) 14:8. doi: 10.1186/s12981-016-0129-4
8. Wilson K, Dray-Spira R, Aubriere C, Hamelin C, Spire B, Lert F, et al. Frequency and correlates of late presentation for hiv infection in France: older adults are a risk group - results from the Anrs-Vespa2 Study, France. Aids Care. (2014) 1:S83–93. doi: 10.1080/09540121.2014.906554
9. Hall HI, Holtgrave DR, Tang T, Rhodes TP. Hiv transmission in the united states: considerations of viral load, risk behavior, and health disparities. Aids Behav. (2013) 17:1632–6. doi: 10.1007/s10461-013-0426-z
10. Rampaul M, Edun B, Gaskin M, Albrecht H, Weissman HS. Cost-effectiveness analysis of early vs late diagnosis of hiv-infected patients in South Carolina. South Med J. (2018) 111:355–8. doi: 10.14423/SMJ.0000000000000819
11. Palella FJ. Jr., Armon C, Chmiel JS, Brooks JT, Hart R, et al. Cd4 cell count at initiation of art, long-term likelihood of achieving cd4 >750 cells/mm3 and mortality risk. J Antimicrob Chemother. (2016) 71:2654–62. doi: 10.1093/jac/dkw196
12. Lifson AR, Workneh S, Hailemichael A, Maclehose RF, Horvath KJ, Hilk R, et al. Advanced Hiv disease among males and females initiating Hiv care in rural Ethiopia. J Int Assoc Provide Aids Care. (2019) 18:2325958219847199. doi: 10.1177/2325958219847199
13. Prabhu S, Harwell JI, Kumarasamy JIN. Advanced Hiv: diagnosis, treatment, and prevention. Lancet Hiv. (2019) 6:E540–51. doi: 10.1016/S2352-3018(19)30189-4
14. Ford N, Meintjes G, Calmy A, Bygrave H, Migone C, Vitoria M, et al. Managing advanced HIV disease in a public health approach. Clin Infect Dis. (2018) 66:S106–Ss110. doi: 10.1093/cid/cix1139
15. Hamilton A, Shin S, Taggart T, Whembolua GL, Martin I, Budhwani H, et al. HIV testing barriers and intervention strategies among men, transgender women, female sex workers and incarcerated persons in the caribbean: a systematic review. Sex Transm Infect. (2020) 96:189–96. doi: 10.1136/sextrans-2018-053932
16. The Lancet H. Time to tackle late diagnosis. Lancet Hiv. (2022) 9:E139. doi: 10.1016/S2352-3018(22)00040-6
17. Late Presentation Working Groups in Euro S, Cohere. (2020). Estimating the burden of Hiv late presentation and its attributable morbidity and mortality across Europe 2010–2016. BMC Infect Dis. 20:728. doi: 10.1186/s12879-020-05261-7
18. Tang HL, Mao YR, Zhang TJ, Han H, He JN. Analysis on late diagnosis reasons of newly diagnosed Hiv/Aids patients. Chinese J Prevent Med. (2012) 46:1004–8.
19. Wilton J, Light L, Gardner S, Rachlis B, Conway T, Cooper C, et al. Late diagnosis, delayed presentation and late presentation among persons enrolled in a clinical Hiv cohort in Ontario, Canada (1999-2013). HIV Med. (2019) 20:110–20. doi: 10.1111/hiv.12686
20. Rava M, Domínguez-Domínguez L, Bisbal O, López-Cortés LF, Busca C, Antela A, González-Ruano P, et al. Late presentation for Hiv remains a major health issue in Spain: results from a multicenter cohort study, 2004-2018. Plos One. (2021) 16:E0249864. doi: 10.1371/journal.pone.0249864
21. Wu J, Wu H, Li P, Lu PC. Hiv/Stis risks between migrant msm and local msm: a cross-sectional comparison study in China Peerj. (2016) 4:E2169. doi: 10.7717/peerj.2169
22. Antinori A, Coenen T, Costagiola D, Dedes N, Ellefson M, Gatell J, et al. Late Presentation of Hiv infection: a consensus definition. HIV Med. (2011) 12:61–4. doi: 10.1111/j.1468-1293.2010.00857.x
23. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Statistics Med. (2000) 19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z
24. Zhang NR, Siegmund DO, A. Modified bayes information criterion with applications to the analysis of comparative genomic hybridization data. Biometrics. (2007) 63:22–32. doi: 10.1111/j.1541-0420.2006.00662.x
25. The central people's government of the People's Republic of China. Strengthen the Prevention and Control of Aids. (2011). Available online at: http://www.gov.cn/zwgk/2011-02/16/content_1804536.htm (accessed July 13, 2022).
26. Wu D, Cheng WB, Xiong Y, Lu Y, Ni, & Tang YX WM. Changing trends of hiv Testing and hiv self-testing in men who have sex with men on a gay social networking app. Chinese J Epidemiol. (2021) 42:269–72. doi: 10.3760/cma.j.cn112338-20200624-00882
27. Liang H, Tang K, Cao W, Guo Y, Jiao Y, Zhu W, et al. Factors influencing the acceptability of hiv/aids voluntary counseling and testing: a quantitative study of 41336 female university students in China. Sex Health. (2021) 18:119–21. doi: 10.1071/SH20038
28. Zhao DH, Hui S, Song X, Tong X, Ma J, Zhang XL, et al. Effects of unsafe sexual behavior and sexual orientation on previous hiv testing and hiv testing willingness among college students in Harbin. Chinese J Epidemiol. (2022) 43:254–9. doi: 10.3760/cma.j.cn112338-20210616-00477
29. Hachfeld A, Darling K, Calmy A, Ledergerber B, Weber R, Battegay M, et al. Why do sub-saharan africans present late for Hiv care in Switzerland? HIV Med. (2019) 20:418–23. doi: 10.1111/hiv.12727
30. Gray C, Crawford G, Reid A, Lobo AR. Hiv knowledge and use of health services among people from South-East Asia and sub-saharan Africa living in Western Australia health. Promot J Austr. (2018) 29:274–81. doi: 10.1002/hpja.168
31. Jiao K, Wei R, Li H, Chow EPF, Piqueiras E, Lewis T, et al. Hiv testing frequency and associated factors among five key populations in ten cities of China: a cross-sectional study. Bmc Infect Dis. (2022) 22:195. doi: 10.1186/s12879-022-07189-6
32. Broady TR, Brener L, Hopwood M, Cama E, Treloar C, Holt CM. Hiv stigma by association among australian gay and bisexual men aids. Suppl. (2020) 1:S53–61. doi: 10.1097/QAD.0000000000002565
33. Wu ZY. Characteristics of hiv sexually transmission and challenges for controlling the epidemic in China. Chinese J Epidemiol. (2018) 39:707–9. doi: 10.3760/cma.j.issn.0254-6450.2018.06.002
34. Wang YY, Yang Y, Chen C, Zhang L, Ng CH, Ungvari GS, et al. Older adults at high risk of Hiv infection in China: a systematic review and meta-analysis of observational studies. PeerJ. (2020) 8:E9731. doi: 10.7717/peerj.9731
35. Lian J, Chen X, Su X, Si M, Dai Z, Fu J, et al. Hiv Testing and related factors among 50 years and older msm in China: results from a cross-sectional study. Aids Care. (2022) 2:1–6. doi: 10.1080/09540121.2022.2060493
36. Liu Z, Chen Y, Yao T, Zhang T, Song D, Liu Y, et al. Factors related to Hiv testing frequency in msm based on the 2011-2018 survey in Tianjin, China: a hint for risk reduction strategy. BMC Public Health. (2021) 21:1900. doi: 10.1186/s12889-021-11948-6
37. Xiao Q, Liu B, Wu HB. How bachelorhood and migration increase the HIV transmission risk through commercial sex in China? Aids Behav. (2020) 24:791–801. doi: 10.1007/s10461-019-02640-3
38. Chen L, His JH, Wu X, Shen Z, Lu H, Chen H, et al. Disparities in Hiv and syphilis prevalence and risk factors between older male clients with and without steady sex partners in southwestern rural China. Bmc Infect Dis. (2017) 17:269. doi: 10.1186/s12879-017-2367-z
39. Sun X, Yang W, Tang S, Shen M, Wang T, Zhu Q, et al. Declining trend in Hiv new infections in guangxi, china: insights from linking reported Hiv/Aids cases with Cd4-At-diagnosis data. BMC Public Health. (2020) 20:919. doi: 10.1186/s12889-020-09021-9
40. Xiao My, Fu Lr, Luo Hb, Song Lj, Zhang Zx, Wang Xw, et al. Application of spectrum/Epp model in Hiv/Aids epidemic trend assessment of Yunnan Province. Chinese J Aids And Std. (2020) 26:1221–5. doi: 10.13419/j.cnki.aids.2020.11.20
41. Lyu P, Chen FF. National Hiv/aids epidemic estimation and interpretation in China. Chinese J Epidemiol. (2019) 40:1191–6. doi: 10.3760/cma.j.issn.0254-6450.2019.10.004
42. Chow EP, Wilson L, Zhang L. The rate of Hiv testing is increasing among men who have sex with men in China. Hiv Med. (2012) 13:255–63. doi: 10.1111/j.1468-1293.2011.00974.x
43. Cao W, Hsieh E, Li T. Optimizing treatment for adults with HIV/aids in China: successes over two decades and remaining challenges. Curr Hiv/Aids Rep. (2020) 17:26–34. doi: 10.1007/s11904-019-00478-x
44. Zhang X, Wang N, Vermund SH, Zou H, Li X, Zhang F, et al. Interventions to improve the HIV continuum of care in China. Curr HIV/AIDS Rep. (2019) 16:448–57. doi: 10.1007/s11904-019-00469-y
45. Zhang D, Li C, Meng S, Qi J, Fu X, Sun J. Attrition of Msm with Hiv/Aids along the continuum Of care from screening To Cd4 testing in China. AIDS Care. (2014) 26:1118–21. doi: 10.1080/09540121.2014.902420
46. Yan H, Zhang R, Wei C, Li J, Xu J. Yang, et al. A peer-led, community-based rapid hiv testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sexually Transmitt Infect. (2014) 90:388–93. doi: 10.1136/sextrans-2013-051397
47. Elgalib A, Shah S, Al-Wahaibi A, Al-Habsi Z, Al-Fouri M, Lau R, et al. Predictors of late presentation and advanced Hiv disease among people living with Hiv in Oman (2000-2019). BMC Public Health. (2021) 21:2029. doi: 10.1186/s12889-021-12048-1
48. Jeong SJ, Italiano C, Chaiwarith R, Ng OT, Vanar S, Jiamsakul A, et al. Late presentation into care of hiv disease and its associated factors in Asia: results of Tahod. AIDS Res Hum Retroviruses. (2016) 32:255–61. doi: 10.1089/aid.2015.0058
49. Siwak E, Horban A, Witak-Jedra M, Cielniak I, Firlag-Burkacka E, Leszczyszyn-Pynka M, et al. Long-term trends in Hiv care entry: over 15 years of clinical experience from Poland. HIV Med. (2019) 20:581–90. doi: 10.1111/hiv.12762
50. Raffetti E, Postorino MC, Castelli F, Casari S, Castelnuovo F, Maggiolo F, et al. The risk of late or advanced presentation of hiv infected patients is still high, associated factors evolve but impact on overall mortality is vanishing over calendar years: results from the Italian master cohort. BMC Public Health. (2016) 16:878. doi: 10.1186/s12889-016-3477-z
51. Qiu C, Deng L, Geng P, Wang L, Bao W. Factors influencing the late detection of hiv infection cases in Qujing from 2014 To 2019. Chinese J Aids Std. (2021) 27:177–9. doi: 10.13419/j.cnki.aids.2021.02.16
52. Yang Q, Luo Y, Hu Q. Late diagnosis of newly identified hiv/aids cases and influencing factors in Jiangxi Province during 2014 And 2018. Chinese J Aids Std. (2019) 25:1153–6. doi: 10.13419/j.cnki.aids.2019.11.15
53. Armoon B, Higgs P, Fleury MJ, Bayat AH, Moghaddam LF, et al. Socio-demographic, clinical and service use determinants associated with Hiv related stigma among people living with hiv/aids: a systematic review and meta-analysis. Bmc Health Services Res. (2021) 21:1004. doi: 10.1186/s12913-021-06980-6
54. Gunn J, Rooks-Peck C, Wichser ME, Denard C, Mccree DH, Jeffries WL, et al. Effectiveness of Hiv stigma interventions for men who have sex with men (Msm) with and without HIV in the United States: a systematic review and meta-analyses. Aids Behav. (2022) 26:51–89. doi: 10.1007/s10461-021-03358-x
55. Molina Y, Ulrich A, Greer AC, Primbas A, Wandell G, Sanchez H, et al. Impact of pre-diagnosis awareness of Hiv-related stigma and dispositional coping on linkage to Hiv care among newly diagnosed Hiv+ peruvian patients. AIDS Care. (2019) 31:848–56. doi: 10.1080/09540121.2018.1563282
56. Belay GM, Endalamaw A, Ayele AD. Late Presentation of Hiv positive adults and its predictors to Hiv/aids care in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis. (2019) 19:534. doi: 10.1186/s12879-019-4156-3
57. Li Z, Morano JP, Khoshnood K, Hsieh E, Sheng Y. Hiv-related stigma among people living with HIV/aids in rural central China. BMC Health Serv Res. (2018) 18:453. doi: 10.1186/s12913-018-3245-0
58. Cobos Manuel I, Jackson-Perry D, Courvoisier C, Bluntschli C, Carel S, Muggli E, et al. [Stigma And Hiv: Relevant For Everyone]. Rev Med Suisse. (2020) 16:744–8. doi: 10.53738/REVMED.2020.16.690.0744
59. Li Y, Han Y, Xie J, Gu L, Li W, Wang H, et al. Crf01_Ae subtype is associated with x4 tropism and fast HIV progression in Chinese patients infected through sexual transmission. Aids. (2014) 28:521–30. doi: 10.1097/QAD.0000000000000125
60. Wang Z, Lau J, Fang Y, Ip M, Gross DL. Prevalence Of actual uptake and willingness to use pre-exposure prophylaxis to prevent HIV acquisition among men who have sex with men in Hong Kong, China. PLoS One. (2018) 13:E0191671. doi: 10.1371/journal.pone.0191671
Keywords: HIV, late presentation, advanced HIV disease, associated factors, China
Citation: Shi L, Tang W, Liu X, Hu H, Qiu T, Chen Y, Xu X, Chen Y, Zhang Z, Zhou Y, Lu J and Fu G (2022) Trends of late HIV presentation and advance HIV disease among newly diagnosed HIV cases in Jiangsu, China: A serial cross-sectional study from 2008 to 2020. Front. Public Health 10:1054765. doi: 10.3389/fpubh.2022.1054765
Received: 27 September 2022; Accepted: 23 November 2022;
Published: 08 December 2022.
Edited by:
Diego Ripamonti, Papa Giovanni XXIII Hospital, ItalyReviewed by:
Silvia Nozza, San Raffaele Hospital (IRCCS), ItalyMarta Rava, Carlos III Health Institute (ISCIII), Spain
Ali Elgalib, Ministry of Health, Oman
Copyright © 2022 Shi, Tang, Liu, Hu, Qiu, Chen, Xu, Chen, Zhang, Zhou, Lu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gengfeng Fu, ZnVnZkBqc2NkYy5jbg==
 Lingen Shi
Lingen Shi Weiming Tang
Weiming Tang Xiaoyan Liu1
Xiaoyan Liu1 Haiyang Hu
Haiyang Hu Tao Qiu
Tao Qiu Yuheng Chen
Yuheng Chen Yunting Chen
Yunting Chen Gengfeng Fu
Gengfeng Fu