- 1Department of Community Medicine, School of Public Health, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
- 2Public Health Master's Program, School of Medicine and Health Research Institute (HRI), University of Limerick, Limerick, Ireland
- 3Faculty of Human and Health Sciences, Swansea University, Swansea, United Kingdom
- 4Department of Psychiatry, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
- 5Department of Pharmacology, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
- 6National Health Mission, Department of Health and Family Welfare Government of Punjab, Chandigarh, India
- 7Department of Health and Family Welfare, Government of Punjab, Chandigarh, India
- 8Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, New Delhi, India
- 9Department of Tobacco and NCD Control, International Union Against Tuberculosis and Lung Disease (The Union), South-East Asia Office, New Delhi, India
Background: Providing patients with personalized tobacco cessation counseling that is culturally sensitive, and disease-specific from healthcare providers (HCPs) as part of their routine consultations is an approach that could be incorporated, using existing healthcare systems such as the Non-Communicable Disease (NCD) clinics. This paper describes the development of a multi-component culturally tailored, patient-centric, disease-specific tobacco cessation package utilizing multiple approaches of intervention development for healthcare providers and patients attending these clinics in Punjab, India, along with a proposed framework for implementation.
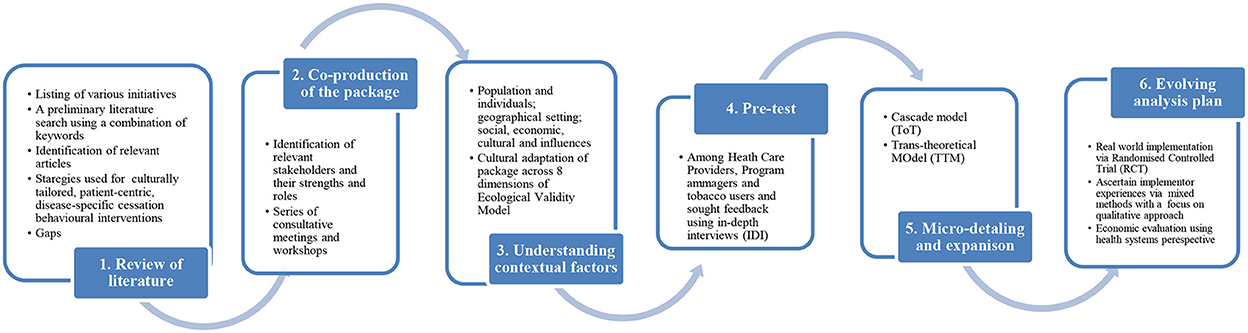
Methods: The proposed intervention package was developed in 6 stages. These included a review of literature for identifying successful cessation interventions for ethnic minority groups, co-production of the package with all stakeholders involved via a series of consultative meetings and workshops, understanding contextual factors of the state and ‘factor-in’ these in the package, pre-test of the package among HCPs and tobacco users using in-depth interviews, micro detailing and expansion of the package by drawing on existing theories of the Cascade Model and Trans-Theoretical Model and developing an evolving analysis plan through real-world implementation at two pilot districts by undertaking a randomized controlled trial, assessing implementer's experiences using a mixed-method with a primary focus on qualitative and economic evaluation of intervention package.
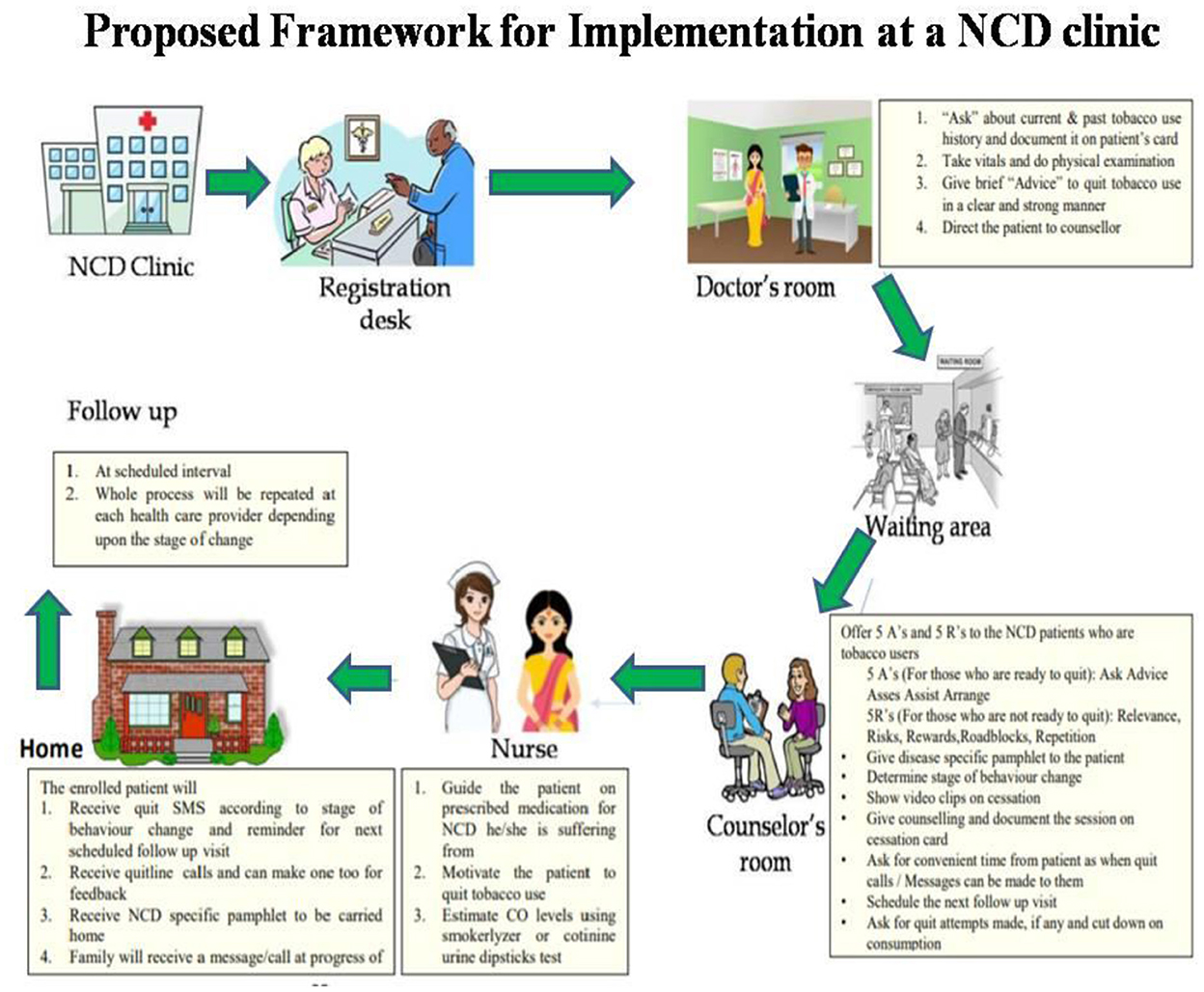
Results: A multi-component package consisting of a booklet (for HCPs), disease-specific pamphlets and short text messages (for patients; bilingual), and an implementation framework was developed using the 6-step process. A major finding from the in-depth interviews was the need for a specific capacity-building training program on tobacco cessation. Therefore, using this as an opportunity, we trained the in-service human resource and associated program managers at the state and district-level training workshops. Based on the feedback, training objectives were set and supported with copies of intervention package components. In addition, the role and function of each stakeholder were defined in the proposed framework.
Conclusion: Consideration of tobacco users' socio-cultural and patient-centric approach makes a robust strategy while developing and implementing an intervention providing an enlarged scope to improve care services for diversified socio-cultural communities.
Background
Non-Communicable Diseases (NCDs) account for a major share of the overall global disease burden claiming 44 million lives annually. NCDs disproportionately affect populations in low- and middle-income nations, which account for 31.4 million global NCD deaths (1). In the Indian sub-continent, NCDs account for 62 percent of all deaths. Besides, the contribution of total “Disability-Adjusted Life Years” (DALYs) from NCDs has increased from 30% (1990) to 55% (2016) (2). In addition, one-eighth of households with NCD burden were pushed to poverty with poverty, deepening the effect to the magnitude of 30.1% among those already below poverty in the year 2017–18 (3).
Article 14 of the WHO- Framework Convention on Tobacco Control envisions member countries take appropriate “demand reduction measures concerning tobacco dependence and cessation” (4). According to Global Adult Tobacco Survey (GATS-2) data, India had the second-lowest quit rate among GATS-2 countries, despite a high prevalence of knowledge about the health consequences of smoking and/or chewing tobacco. Only 55.4 percent of smokers and 50.4 percent of SLT users have ever considered or intended to quit tobacco use (5).
Evidence suggests that a combination of population-wide and individual interventions (pharmacological/non-pharmacological) to modify NCD risk factors are great economic investments because they can prevent the need for more expensive treatment if given to patients early enough (6). Target 3.4 of the Sustainable Development Goals (SDG) aims to reduce premature mortality from NCDs by one-third by 2030. Besides, reducing tobacco use is critical to global efforts to achieve the SDG target (7). The health, social and economic benefits of quitting tobacco use are well established (8). Tobacco cessation is recommended as one of the 'best buys' interventions for preventing and controlling NCDs (9). Evidence from developed countries suggests that brief interventions delivered by diverse health professionals effectively tobacco cessation. Tobacco cessation needs to be urgently expanded by training health professionals in providing routine clinical interventions (10). However, there is a dire need to train healthcare providers to offer brief tobacco cessation interventions (11).
The WHO- Package of Essential Non-communicable Interventions (PEN) also suggests developing programs to address NCD's risk factors, including tobacco in low-resource settings by adapting plans that suit local contexts (including cultural and educational backgrounds) (12). Family members must understand that encouragement from the family can help people adopt healthy living, e.g., cessation of tobacco (6).
Tobacco use is a learned behavior, and nicotine addiction involves biological, behavioral, psychological, and cultural factors. The interplay between these factors results in the continued use of tobacco products among users (13, 14). In an LMIC like India which is culturally diverse and has a dual burden of NCDs and tobacco use, it experiences enormous costs imposed on the nation's health care system. Consequentially, it potentiates stress on the public health care system (15). This calls for low-technology interventions, which could reap future savings in terms of reduced medical costs, improved quality of life, and productivity if delivered effectively. Tobacco's causal association with several long-term conditions [e.g., coronary heart disease (CHD), chronic obstructive pulmonary disease (COPD)] has long been established (16, 17). This requires culture-specific, patient-centric, disease-specific care that reinforces health system strengthening with efficient use of limited health care resources and is sustainable (6).
Data from the Indian Global Health Professionals Students Survey (GHPSS, 2005–2008) between 2005 and 2008 showed a general lack of training among health professionals in patient cessation counseling techniques (18). In a study in Bihar, over two-thirds of medical doctors felt the need to increase their tobacco cessation training (10). Besides, it is essential to address smokeless tobacco cessation in a country like India, where the use of SLT is widespread. Given the higher prevalence of tobacco use in rural populations, extending tobacco cessation services to rural people is imperative. Behavior counseling is applicable and acceptable in rural settings, where access to pharmacotherapy may be limited. In low-resource settings, there is also a need to evaluate cost-effective behavioral interventions, particularly for smokeless forms of tobacco use, for further expansion of tobacco cessation activities (19).
However, there is meager literature on the development or effectiveness of a cessation intervention for NCD patients that is culture-specific, patient-centric, disease-specific, and tested in NCD outpatient settings (20). Therefore, it's crucial to develop that evidence-based interventions are developed and tested in such settings along with co-production with all stakeholders in the development process. This paper describes the development of a multi-component culturally tailored, patient-centric, disease-specific tobacco cessation package utilizing multiple approaches of intervention development for healthcare providers and patients attending non-communicable disease clinics in Punjab, India, and its implementation framework.
Methods
Settings
This intervention package was developed for implementation at NCD clinics in Punjab, India. The “NCD clinics” are established by the Government of India under the National Programme for Prevention and Control of Cancers, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS, 2010–2011) at the district level and Community Health Center Level (CHC). The human resource provisioned at the NCD clinic (at the district hospital) includes a General Physician(1), GNM (2), Technician (1), Physiotherapist (1), Counselor (1), and Data Entry Operator(1). The staff provides emergency and OPD services, counseling, rehabilitative services, and care and management of cancer, diabetes, hypertension, and acute cardiovascular diseases. The clinic shall run on all working days or at least thrice a week (21).
The proposed culturally-specific, patient-centric, disease-specific intervention package was developed in 6 stages. These included the following (Figure 1):
1. Review of literature for identifying successful cessation interventions for ethnic minority groups.
2. Co-production of the package with all stakeholders involved via a series of consultative meetings and workshops.
3. Understanding contextual factors of the state and ‘factor-in’ these in the package.
4. Pre-test of the package among HCPs and tobacco users using in-depth interviews (IDI).
5. Micro detailing and expansion of the package by drawing on existing theories of the Cascade Model and TTM model.
6. Developing an evolving analysis plan through real-world implementation at two pilot districts by undertaking a randomized controlled trial, assessing implementers' experiences using a mixed methods study, and economic evaluation of the intervention package.
Stage 1: Review of literature
A preliminary literature search was undertaken using Pubmed, Scopus, and Embase databases by using a combination of keywords like “tobacco cessation,” “tobacco use cessation,” “smoking cessation,” “smokeless tobacco cessation,” “quitting smoking,” “quitting tobacco” “behavior change,” “interventions,” “cessation counseling,” “tailor made,” “culture-specific,” “non-communicable,” “chronic disease,” “disease specific,” “customized,” “behavior therapy,” “behavioral intervention,” “review”. Relevant articles from the preliminary search were identified; related article links were also explored to expand the search till 2017. References from reviews on customized cessation interventions or customized cessation support were also reviewed for the inclusion of relevant studies.
The literature review indicated that most of the culturally-tailored interventions were delivered in the West (22–24) and catered to either one chronic disease or two and primarily among tobacco smokers (25, 26). Besides, the evidence of such an intervention that is tailored to the current disease, and culturally relevant for tobacco users (especially SLT) from Indian settings was limited (20). Literature suggested a need to develop standards for designing culturally tailored interventions besides using theoretical frameworks that can be applied in various healthcare settings. Therefore, research needs to consider such constraints, such as having intervention sites that are accessible to the study participants (27). Several studies used mobile phone text messages for follow-up services and websites to provide culturally and linguistically tailored education (28). Studies also reported the use of bilingual technology platforms to encourage participants to change their lifestyle-related risk factors and demonstrated the importance of involving families to improve efficient care (29). A culturally targeted (CT) smoking cessation intervention conducted among African–American smokers reported high levels of acceptability, better adherence to nicotine replacement therapy, higher quit rates, and better retention and follow-up (30). The update on the Tobacco Use and Dependence Clinical Practice Guidelines (31) stressed the need for additional research to determine the effectiveness of culturally targeted smoking cessation interventions for racial and ethnic minorities (32). In addition, the literature reported that cessation interventions are more effective if they address the different social norms driving tobacco consumption and the difficulties associated with quitting tobacco use. The social context of tobacco users, such as language and culture, can profoundly influence an individual's experience with tobacco, including quitting (33). The existing literature also reported that interventions to improve patient-centered care (PCC) for persons with multimorbidity are in constant growth (34). In a study conducted to elicit patient perspectives on tobacco use treatment in primary care, the participants suggested addressing smoking at every visit and acknowledging and helping patients deal with addiction issues in written and spoken communications (35). Besides, it highlighted that the most important characteristic of PCC is patients' active involvement in the decision-making process (36). Evidence among patients with long-term conditions reported that such a group is generally more receptive to smoking cessation messages with several “teachable moments” during their care (37). Similarly, patients with diabetes, hypertension, and CHD had higher motivation to quit and desire to receive support compared to the general population (38). It further reported that continued smoking with long-term conditions contributes to excess mortality and morbidity by expediting disease progression, worsening outcomes, increasing complication rates, and reducing treatment compliance (39). The Transtheoretical Model (TTM) (40) has been widely used in the development of cessation interventions especially smoking cessation (41) and very few on smokeless tobacco among disease-specific groups, especially in India, where the burden of SLT use remains relatively high (42).
Gaps in the existing literature
The previous literature from India suggested that there is a need to establish effective tobacco cessation services in diverse health settings with optimal use of existing infrastructure, minimal support, and innovative technology such as mobile phones to improve access. The physicians, in general, lacked knowledge of tobacco cessation protocols and felt uncomfortable or at a loss in their ability to handle the needs of their patients for tobacco cessation (19, 43). Addressing cultural competence through training among the health workforce could help in improving the quality of health service for culturally and ethnically diverse groups (44). However, the evidence does indicate a service provision gap (45). These gaps include a lack of advice to quit from their doctor (46), not realizing the risk of developing diabetic complications with smoking (25), belief that “the damage has already been done” (47), not considering the issue of tobacco use as part of mainstream management (48), etc. There is an urgent need for studies that develop and test well-defined context-specific, tailored, and comprehensive packages for tobacco cessation, especially for high-risk patients (49). Further, the need of the hour is to determine ways to integrate these within existing mechanisms along with the inclusion of economic evaluations. Research is also required to understand the barriers to service provision, as the literature is particularly sparse on the perspectives of healthcare providers (48).
In India, multiple government led and other initiatives including various modules on tobacco cessation under the National Cancer Control Programme (2005) (50), tobacco dependence guidelines (2011) (51), a training manual on tobacco cessation for nurses, health workers and doctors by World Health Organization (52) and a toolkit for delivering five As and five Rs by World Health Organization (53), and various modules under NPCDCS program describing the management of various risk factors including tobacco use (21). However, despite the availability of all these resources for healthcare providers, their preparedness for the delivery of tobacco-cessation services remains low in India (54).
Stage 2: Co-production of the package
Based on the findings of the literature review, prototypes of package components were developed. The components included a booklet for the health care providers at NCD clinics and disease-specific pamphlets and short text messages for the patients attending these NCD clinics in Punjab. Thereafter, a series of consultative meetings and workshops with stakeholders were carried out and multiple iterations were undertaken.
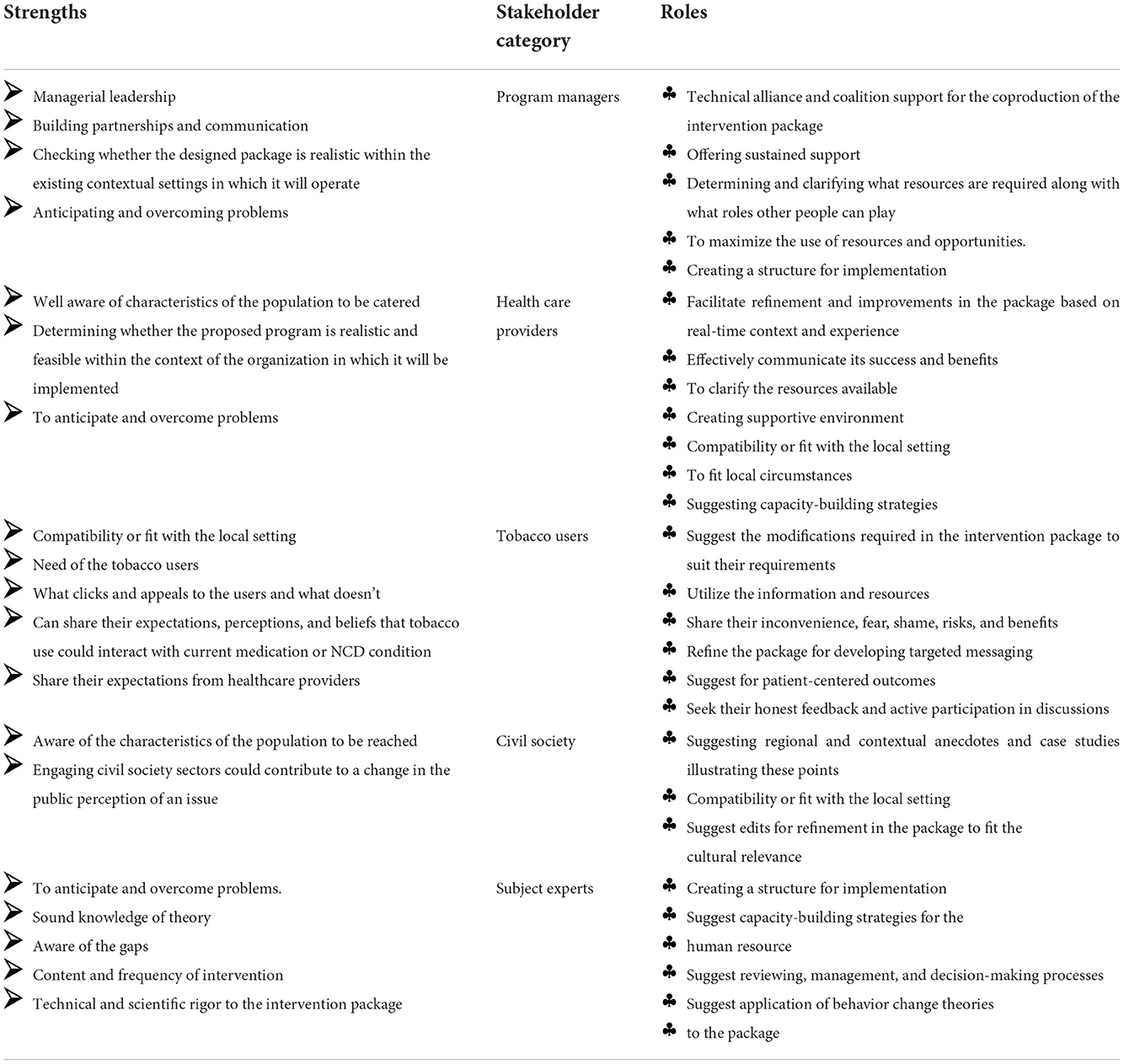
Identification of stakeholders and their strengths and roles in the development process
The stakeholders included the following:
 The program managers of both the programs viz, National Tobacco Control Program (NTCP) and NPCDCS (district and state level),
The program managers of both the programs viz, National Tobacco Control Program (NTCP) and NPCDCS (district and state level),
 Healthcare providers at the NCD clinics,
Healthcare providers at the NCD clinics,
 Tobacco users,
Tobacco users,
 Representatives from civil society,
Representatives from civil society,
 Subject experts of tobacco cessation and NCDs.
Subject experts of tobacco cessation and NCDs.
Each group of stakeholders was involved at various stages of the development and refinement of the package based on their roles and strengths. In order to ensure sustained support during the development of the intervention package and implementation, decisions were made in collaboration with all. Adaptation decisions were made collaboratively by the original intervention designer, who knew the theory and central operational features of the intervention, and those hosting the new intervention, know their setting, the target population, and the local culture (43). Collaborative working relationships are crucial for making wise decisions regarding fidelity and adaptation (44). The strengths and roles are summarized in the table below (Table 1).
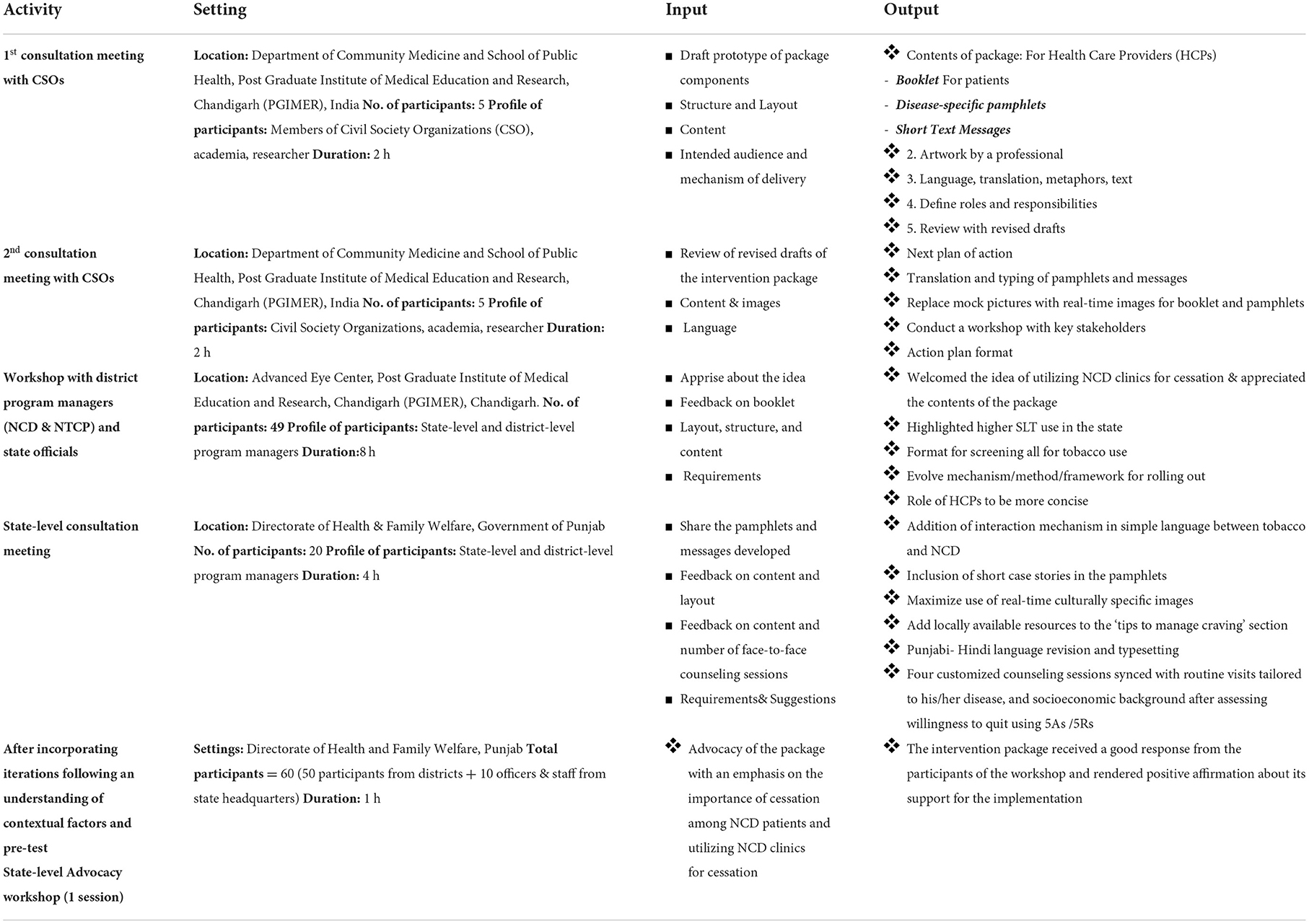
Series of consultative meetings and workshops
Workshops expand the perspective to encompass the participants' mutual experience enabling us to undertake an iterative process of design-based research. The workshop as a research approach is an explicit method choice that allows us to iterate, and thus refine and moderate, our research design over time and in different contexts. Consultative meetings with the civil society (n = 2), workshop with program managers (n = 1), consultative meetings with healthcare providers (n = 1), and an advocacy workshop with program managers, administrative authorities, and health café providers (n = 1) were undertaken. The objectives of each activity and its outcome are described in Table 2.
Stage 3: Understanding contextual factors of the state and “factor-in” these in the package
The rural population forms 62.51% of the total population in the state of Punjab. The state's economy has predominantly been agrarian and has rich culture and heritage. Punjabi is the state's official language and has a literacy rate of 75.84 %. Punjab has the largest population of Sikhs in India numbering around 16 million comprising 57.69% of the state population. Sikhism is the main religion practiced by about two-thirds of the people (55). Tobacco consumption is strictly prohibited in Sikhism and using tobacco is listed in the Sikh Rehat Maryada- the Sikh code of conduct as one of the four transgressions (Kurahits) (56, 57).
However, the agricultural transformation in Punjab led to internal migration within the population of Punjab from central India. A retrospective review on contextualizing tobacco use in Punjab's social, economic, and political transformation reports that tobacco use in Punjab is determined by the sociopolitical transition from a pre-colonial province to an autonomous Indian State. It also added that although a complex historical process marked these events, the state's retention of its culture offers an interesting aspect of this development. For instance, these events have been marked from the conception of Sikhism to the changing borders of Punjab territory while positioning tobacco use within these boundaries. Additionally, the transitions in the social, economic, and developmental structure of Punjab have played a vital role in the population's health and health behavior. Through various dimensions, the present state of Punjab places the subject of tobacco addiction within the state's social, economic, and political boundaries (58).
Despite tobacco use being a sensitive subject in Punjab, there has been an increase in tobacco use prevalence among adults from 11.7% (Global Adult Tobacco Survey, 2009–2010) (59) to 13.4 % (GATS-2, 2016-2017) (5).
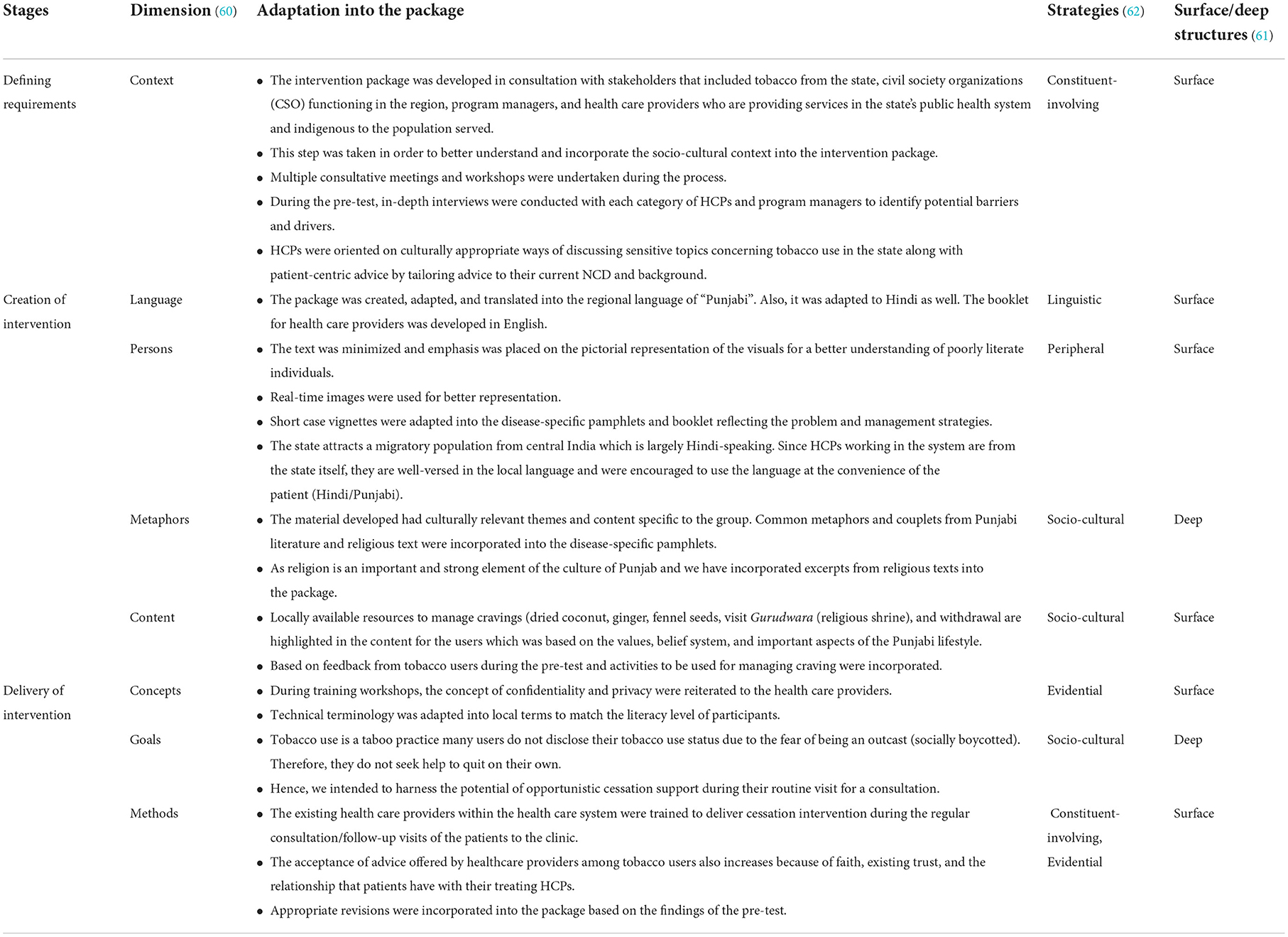
Cultural adaptation of package to ecological validity model across the eight dimensions
The ecological Validity Model (EVM) has been recurrently applied to the development and adaptation of psychological interventions. The EVM proposes eight dimensions to guide cultural adaptations across- “language, persons, metaphors, content, concepts, goals, methods and context.” The explicit adaptation of interventions across these eight dimensions is thought to increase the ecological and external validity of an intervention. The framework can serve as a guide for developing culturally sensitive treatments and adapting existing psychosocial treatments to specific ethnic minority groups (60). The photographs from the community that were used in the disease-specific pamphlets were real-time and culturally relatable. Couplets and adages from local and religious contexts were incorporated into the intervention package. The text messages and pamphlets were translated into the vernacular language (Punjabi). The local role models were highlighted for adopting a tobacco-free lifestyle. The tips designed to manage craving due to tobacco withdrawal revolved around the available local cultural resources and real-time experiences of tobacco users from the community. Besides, we have tried to adapt various other cultural frameworks as suggested by Reniscow and colleagues (61) and Kreuter (62) and into the development process of the package (Table 3).
Stage 4: Pre-test of the package
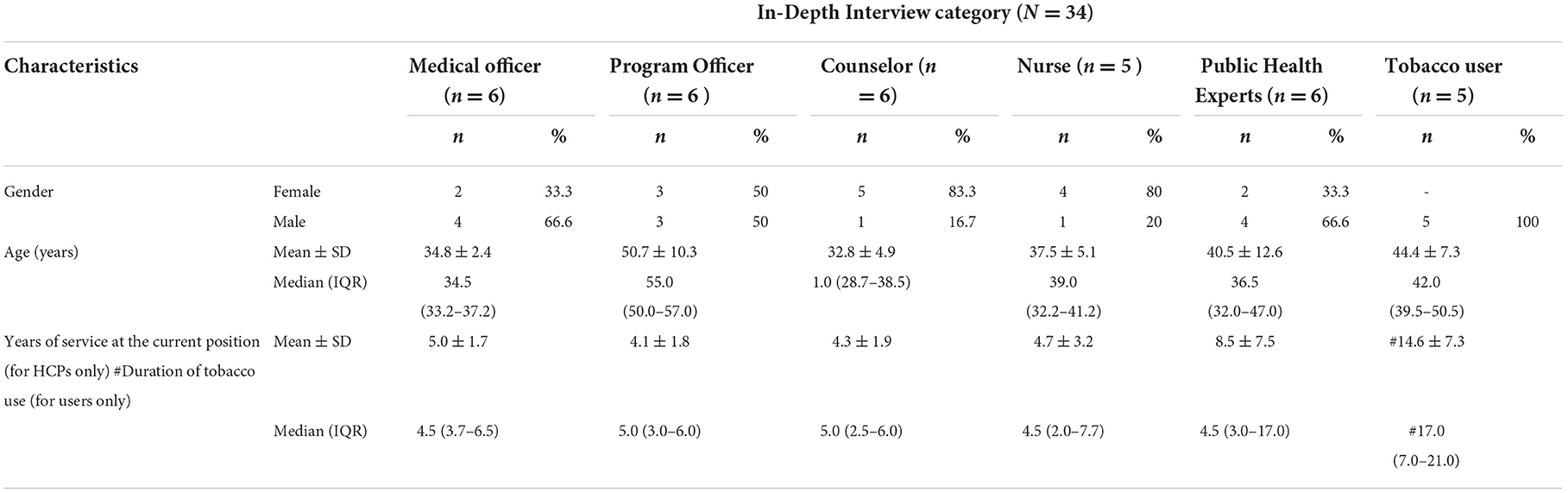
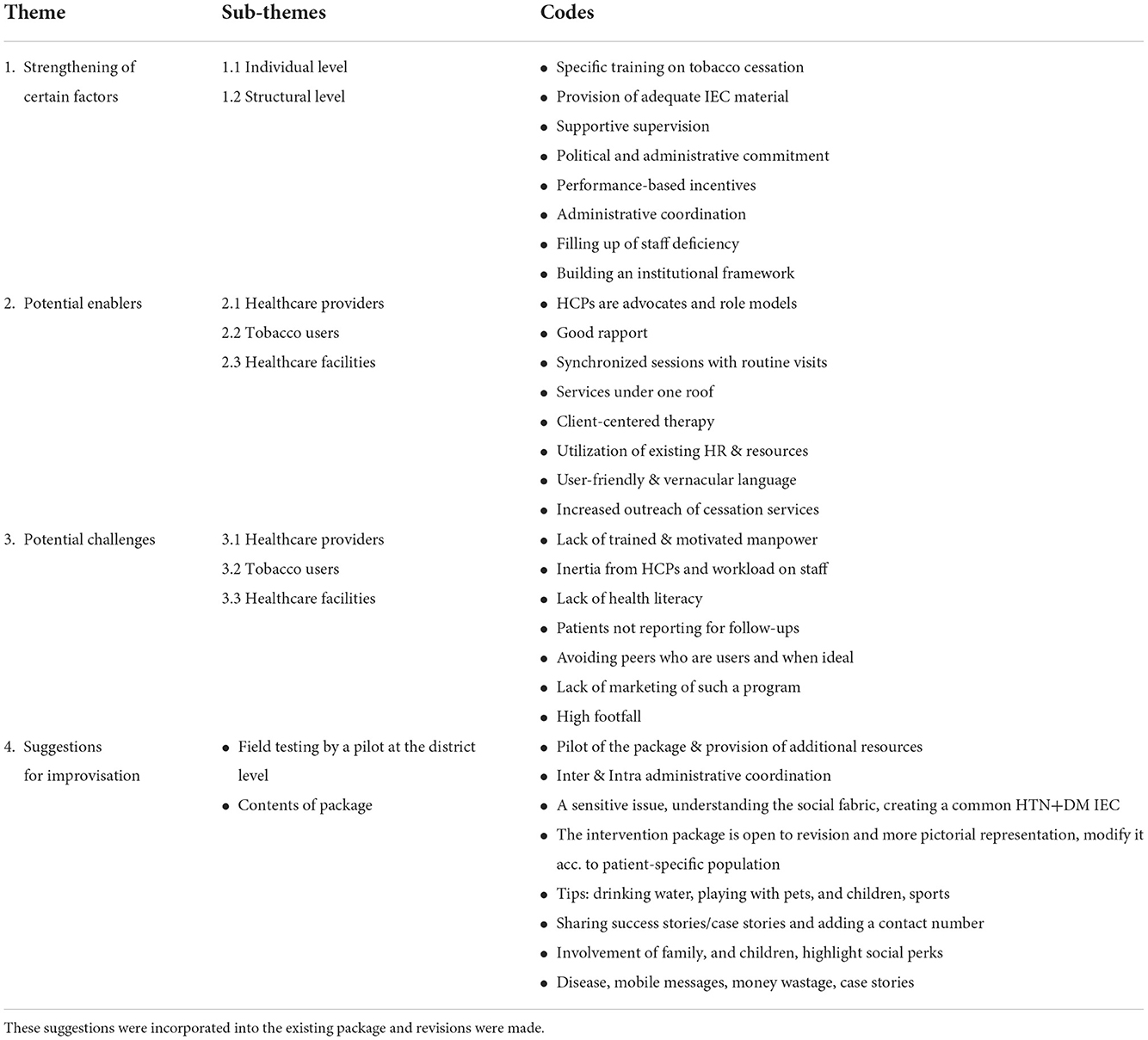
A pre-test of the intervention package was carried out. Each respondent was given a copy of the booklet, disease-specific pamphlets, and short text messages, and feedback was sought on the format, content, and delivery. We conducted five to six in-depth interviews with each category of stakeholder (not involved in the designing process- program managers, medical officers, counselors, nurses, public health experts) and tobacco users. Each interview lasted for 25–30 min. The interview data were analyzed using thematic analysis. The background characteristics of the participants are given in Table 4. The interviews were transcribed followed by data extraction and an analysis worksheet was made. Thereafter, codes were generated and categories were made. Categories were clubbed into themes and sub-themes. The major themes, sub-themes, and codes that emerged from the data are summarized in Table 5.
Stage 5: Micro detailing and expansion of the package by drawing on existing theories of the cascade model and TTM model
“Cascade training” is extensively used as an effective and efficient approach for addressing the scarcity of healthcare professionals in LMICs by upgrading their skills and eventually improving their job performance and participation (63). The objective remains to enhance the diffusion of innovation. The cascade model is used mainly for in-service training, as this strategy can train large numbers of people within a limited time (64). A major finding from the in-depth interviews was that HCPs and program managers highlighted the need for a specific capacity-building training program on tobacco cessation. Therefore, using this as an opportunity, we trained the in-service human resource and associated program managers at the state and district-level training workshops. Based on the feedback, training objectives were set and supported with copies of intervention package components. Besides, the master trainers were subject experts with a comprehensive understanding of the knowledge and skills required to be transferred. In addition, the role and function of each stakeholder were defined in the proposed framework (Figure 2). A systematic review of TTT in health and social care found that the TTT programs helped to increase knowledge, improve clinical behavior, and produce better patient outcomes (65).
Transtheoretical model
The Transtheoretical Model (TTM) of behavior change provides a framework for both understanding and measuring behavior change. It facilitates the development of individually tailored intervention strategies that can be easily modified to fit diverse populations (66). TTM recognizes change as a process toward desired behavior through a series of stages. While progression through the Stages of Change can occur linearly, a nonlinear progression is common. It suggests that smokers move through a series of motivational stages before they manage to stop smoking. These are pre-contemplation (no thoughts of quitting), contemplation (thinking about quitting), preparation (planning to quit in the times to come, say days or weeks), action (quitting successfully for up to for a considerable duration, usually, six months), and maintenance (no smoking for more than 6 months). According to this TTM, programs that help people to stop smoking should be matched to their stage of readiness to quit (67). The backdrop of this model was utilized in developing and sending stage-based short text messages to tobacco users. The assessment was carried out using the “stage of change” questionnaire. Besides, these were bilingual (Punjabi and Hindi) suited according to the preference of the patient.
Stage 6: Evolving analysis plan
The developed intervention package would be implemented at two district-level NCD clinics through a randomized controlled trial (RCT) comparing two groups (one receiving package and the other receiving usual care). These participants would be followed up for 1 year with follow-ups at the 3rd month, 6th month, 9th month, and 12th month. Besides, the biochemical assessment would also be undertaken for the participants to assess their quit status using plasma cotinine levels (LC-MS). However, this would be restricted only to two pilot districts. In addition, a mixed-methods study would also be undertaken to understand the barriers and facilitators of package implementation from the perspective of healthcare providers and program managers. The emphasis on the qualitative part would assist to understand the factors in a detailed manner. Also, an economic evaluation would be carried out for the package development phase and implementation phase using a health systems perspective. Cost analysis of the intervention package is important from an implementation viewpoint, for policymakers to help resource allocation between various interventions available in the basket and sustain newly developed programs.
Discussion
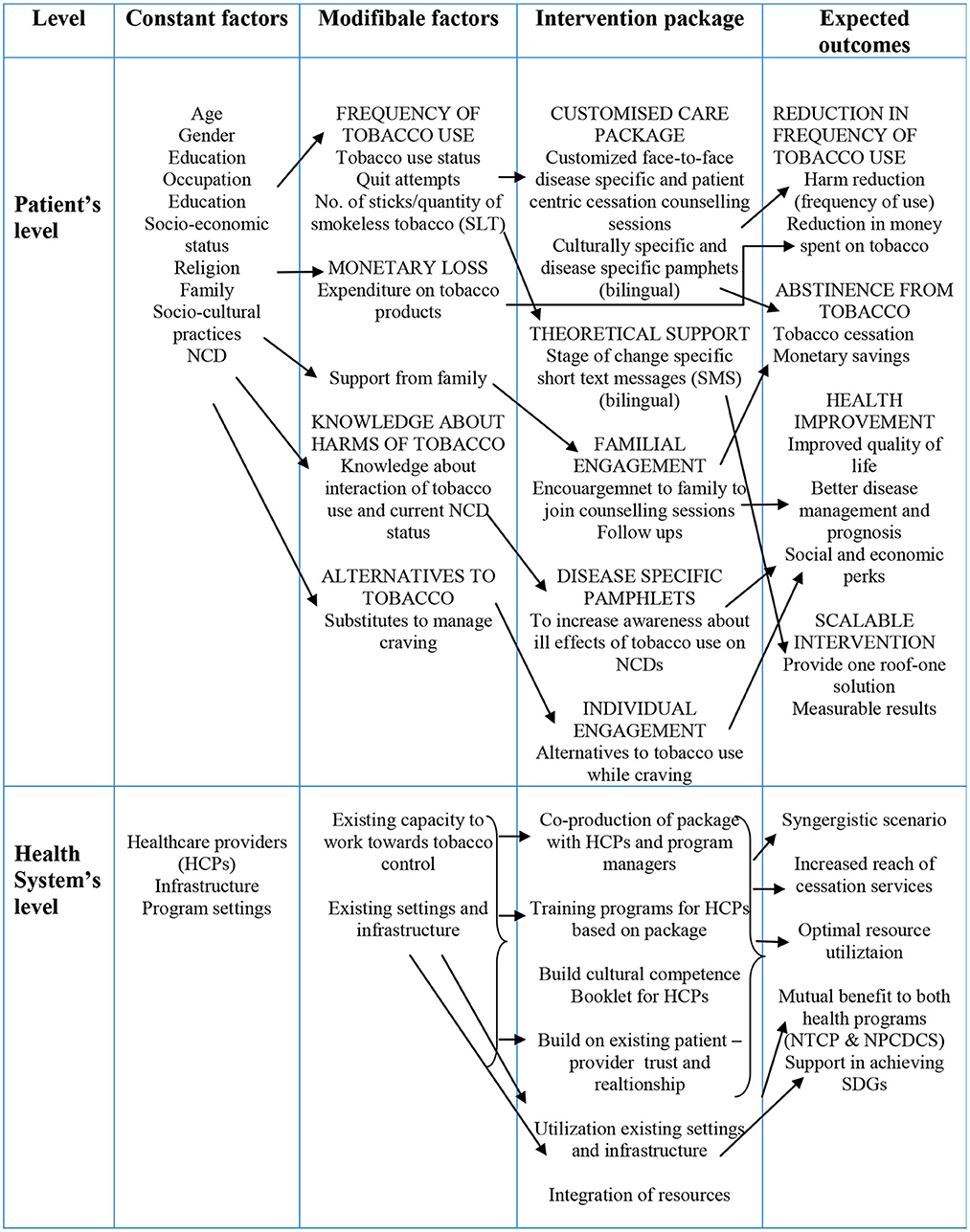
During this exercise, we developed a multi-component culturally-specific, disease-specific, and patient-centric tobacco cessation intervention package utilizing multiple approaches of intervention development for the health care providers and patients attending NCD clinics in Punjab, India. We adapted and incorporated successful non-pharmacological strategies from existing cessation interventions available. The novelty of the intervention developed lies in it being culturally tailored, patient-centric, NCD specific, bilingual (Punjabi/Hindi)- SMS, pamphlets and counseling sessions, and encouragement to family members to be involved in counseling sessions. While developing and implementing an intervention, consideration of tobacco users' socio-cultural and patient-centric approach makes it a robust strategy that is adaptable in similar settings elsewhere. Further, it better assists HCPs who can then enhance their potential to deliver the required service by easy understanding of the patient's cultural aspects through the medium of intervention. The intervention underlines both the negative implications of tobacco and the benefits of quitting, as well as how quitting is relevant to the patient's health, social, and family contexts. The entire package was developed in co-production with relevant stakeholders through a series of exhaustive consultative meetings and workshops. It aims to provide “opportunistic quitting assistance” to NCD patients who are currently using tobacco in any form (smoked /smokeless tobacco). In addition, the package enhances the capacity development of present human capital at NCD clinics via training workshops and helps to build cultural competence. This has the potential to optimize resources and long-term sustainability within the existing healthcare system. The use of mobile technology to deliver culturally, linguistically, and stage of change appropriate short text messages could be an efficient strategy to trigger constant motivational behavior change at regular intervals, to compensate for the loss of motivation over a specific duration, which is commonly observed when it comes to sustaining the attitude and practice of changed behavior. There is inadequate focus on the healthcare promotion aspects concerning NCD risk factors in the present educational landscape of medical education in India (68). Besides, during the pre-test, we gauzed feedback from users as well as beneficiaries that helped to improvise the package. The conceptual framework of the intervention package is represented in Figure 3.
The study's limitation includes a purposive selection of the participants for the IDI therefore the views and suggestions may not be generalizable. The cascade model is often criticized for distortion of the messages transferred during the training, resulting in dilution through miscommunication and different interpretations of the same messages (64). In addition, the TTM model ignores the social context in which change occurs (such as SES and income). The model assumes that individuals make coherent and logical plans in their decision-making process when this is not always true. Given that tobacco use is a sensitive issue in the intervention implementation state, we expect that culture-specific intervention materials would bridge the gap. Furthermore, the results may help healthcare decision-makers introduce large-scale projects to provide culturally relevant patient-centric care and improve care services for diversified socio-cultural communities.
Data availability statement
The data supporting the study findings are available upon request from the corresponding author (SGo). The data are not available publicly due to restrictions (such as the presence of information that may compromise the confidentiality of research participants).
Ethics statement
The Ethics approval was granted by the Institute Ethics Committee (IEC) of the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India (IEC number: INT/IEC/2017/1361). Prior permissions were obtained from the State Tobacco Control Cell and the NCD Control Cell, Department of Health and Family Welfare, Government of Punjab, India. The main study's protocol has been registered with India's Clinical Trials Registry, with the registration number CTRI/2018/01/011643. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SGo conceptualized the idea. SGo, BM, and SGr developed the methodology. GB performed the data collection, analysis, and prepared the first draft. GS and SGi facilitated the administration. LS, RS, SGo, BM, SGr, GS, and SGi gave technical inputs to the first draft. The final draft was approved by all authors. All authors contributed to the article and approved the submitted version.
Funding
This current manuscript is the Ph.D. work of GB. She is a recipient of the Junior Research Fellowship by the Indian Council of Medical Research [ICMR-JRF (No. 3/1/3/JRF-2016/HRD)] to pursue her Ph.D. Program.
Acknowledgments
The authors thank the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, and the State Tobacco Control Cell and State NCD Control Cell, Department of Health and Family Welfare, Government of Punjab for their technical support during the study. In addition, the authors also thank the Indian Council of Medical Research (ICMR), New Delhi, India for granting Junior Research Fellowship (ICMR-JRF) to the first author (GB) for pursuing Ph.D. program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Non-Communicable Diseases Factsheet. World Health Organization (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
2. Salvi S KG, Dhaliwal RS, Paulson K, Agrawal A, Koul PA, Mahesh PA, et al. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. (2018) 6:e1363–74. doi: 10.1016/S2214-109X(18)30409-1
3. Verma VR KP, Dash U. Assessing the household economic burden of non-communicable diseases in India: evidence from repeated cross-sectional surveys. BMC Public Health. (2021) 21:1–22. doi: 10.1186/s12889-021-10828-3
4. World Health Organization. World Health Organization Framework Convention on Tobacco Control. World Health Organization (2003). Available online at: https://apps.who.int/iris/handle/10665/42811
5. Tata Institute of Social Sciences, Ministry of Health and Family Welfare Government of India. Global Adult Tobacco Survey (GATS) second round 2016–17. (2017). Available online at: https://main.mohfw.gov.in/sites/default/files/GlobaltobacoJune2018_0.pdf
6. World Health Organization. Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings. World Health Organization (2010). Available online at: https://apps.who.int/iris/handle/10665/44260
7. Bennett JE KV, Mathers CD, Guillot M, Rehm J, Chalkidou K, Kengne AP, et al. Countdown 2030: pathways to achieving Sustainable Development Goal target 3.4. Lancet. (2020) 396:918–34. doi: 10.1016/S0140-6736(20)31761-X
8. United States Public Health Service Office of the Surgeon General; National Center for Chronic Disease Prevention Health Promotion (US) Office on Smoking and Health. Smoking Cessation: A Report of the Surgeon General. Washington, DC: US Department of Health and Human Services (2020). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK555591/
9. World Health Organization. Tackling NCDs: ‘Best Buys’ and other recommended interventions for the prevention and control of Noncommunicable Diseases. World Health Organization (2017). Available online at: https://apps.who.int/iris/handle/10665/259232
10. Murthy P, Saddichha S. Tobacco cessation services in India: Recent developments and the need for expansion. Indian J Cancer. (2010) 47:69. doi: 10.4103/0019-509X.63873
11. Sampath H, Sharma D, Soohinda G, A. Study of Knowledge, Attitudes, And Practices Towards Tobacco Cessation Services (TCS) Among Clinicians In A Tertiary Care Teaching Hospital. Int J Life Sci Pharma Res. (2019) 9:1–10. doi: 10.22376/ijpbs/lpr.2019.9.3.L1-10
12. WHO Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care. (2020).
13. Office of the Surgeon General (US), Office on Smoking Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. National Center for Biotechnology Information. U.S. National Library of Medicine (2010). Available online at: https://www.ncbi.nlm.nih.gov/books
14. Heishman S. Behavioral and cognitive effects of smoking: Relationship to nicotine addiction. Nicotine Tobacco Res. (1999) 1:143–7. doi: 10.1080/14622299050011971
15. Thakur J, Prinja S, Garg CC, Mendis S, Menabde N. Social and economic implications of noncommunicable diseases in India. Indian J Community Med. (2011) 36:S13. doi: 10.4103/0970-0218.94704
16. Doyle JT, Dawber TR, Kannel WB, Heslin AS, Kahn HA. Cigarette smoking and coronary heart disease: combined experience of the Albany and Framingham studies. N Engl J Med. (1962) 266:796–801. doi: 10.1056/NEJM196204192661602
17. Zhang H, Cai B. The impact of tobacco on lung health in China. Respirology. (2003) 8:17–21. doi: 10.1046/j.1440-1843.2003.00433.x
18. Surani N, Pednekar M, Sinha D, Singh G, Warren C, Asma S, et al. Tobacco use and cessation counseling in India-data from the Global Health Professions Students Survey, 2005-09. Indian J Cancer. (2012) 49:425. doi: 10.4103/0019-509X.107751
19. Varghese C, Kaur J, Desai NG, Murthy P, Malhotra S, Subbakrishna D, et al. Initiating tobacco cessation services in India: challenges and opportunities. WHO South-East Asia J Public Health. (2012) 1:159–68. doi: 10.4103/2224-3151.206929
20. Thankappan K, Mini G, Daivadanam M, Vijayakumar G, Sarma P, Nichter M. Smoking cessation among diabetes patients: results of a pilot randomized controlled trial in Kerala, India. BMC Public Health. (2013) 13:1–8. doi: 10.1186/1471-2458-13-47
21. Directorate General of Health Services. Ministry of Health and Family Welfare: Government of India. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS); Operational Guidelines. Ministry of Health and Family Welfare: Government of India (2022). Available online at: https://main.mohfw.gov.in/Major-Programmes/non-communicable-diseases-injury-trauma/Non-Communicable-Disease-II/National-Programme-for-Prevention-and-Control-of-Cancer-Diabetes-Cardiovascular-diseases-and-Stroke-NPCDCS
22. Haddad LG, Al-Bashaireh AM, Ferrell AV, Ghadban R. Effectiveness of a culturally-tailored smoking cessation intervention for Arab-American men. Int J Environ Res Public Health. (2017) 14:411. doi: 10.3390/ijerph14040411
23. Smith SS, Rouse LM, Caskey M, Fossum J, Strickland R, Culhane JK, et al. Culturally tailored smoking cessation for adult American Indian smokers: a clinical trial. Couns Psychol. (2014) 42:852–86. doi: 10.1177/0011000014542601
24. Wu D, Ma GX, Zhou K, Zhou D, Liu A, Poon AN. The effect of a culturally tailored smoking cessation for Chinese American smokers. Nicotine Tobacco Res. (2009) 11:1448–57. doi: 10.1093/ntr/ntp159
25. Padmawati RS, Ng N, Prabandari YS, Nichter M. Smoking among diabetes patients in Yogyakarta, Indonesia: cessation efforts are urgently needed. Trop Med Int Health. (2009) 14:412–9. doi: 10.1111/j.1365-3156.2009.02241.x
26. Hennrikus D, Joseph AM, Lando HA, Duval S, Ukestad L, Kodl M, et al. Effectiveness of a smoking cessation program for peripheral artery disease patients: a randomized controlled trial. J Am Coll Cardiol. (2010) 56:2105–12. doi: 10.1016/j.jacc.2010.07.031
27. Joo JY, Liu MF. Culturally tailored interventions for ethnic minorities: a scoping review. Nurs Open. (2021) 8:2078–90. doi: 10.1002/nop2.733
28. Chandler J, Sox L, Kellam K, Feder L, Nemeth L, Treiber F. Impact of a culturally tailored mHealth medication regimen self-management program upon blood pressure among hypertensive Hispanic adults. Int J Environ Res Public Health. (2019) 16:1226. doi: 10.3390/ijerph16071226
29. Islam NS, Wyatt LC, Taher M, Riley L, Tandon SD, Tanner M, et al. A culturally tailored community health worker intervention leads to improvement in patient-centered outcomes for immigrant patients with type 2 diabetes. Clin Diabetes. (2018) 36:100–11. doi: 10.2337/cd17-0068
30. Matthews AK, Sánchez-Johnsen L, King A. Development of a culturally targeted smoking cessation intervention for African American smokers. J Community Health. (2009) 34:480–92. doi: 10.1007/s10900-009-9181-5
31. Tobacco Use Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update - NCBI Bookshelf. Rockville, MD: US Department of Health and Human Services (2008). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK63952/
32. Kreuter MW, McClure SM. The role of culture in health communication. Annu Rev Public Health. (2004) 25:439–55. doi: 10.1146/annurev.publhealth.25.101802.123000
33. Smith PH BA, Weinberger AH, Sheffer CE, McKee SA. Sex/gender differences in smoking cessation: a review. Prev Med. (2016) 92:135–40. doi: 10.1016/j.ypmed.2016.07.013
34. Poitras ME, Maltais ME, Bestard-Denommé L, Stewart M, Fortin M. What are the effective elements in patient-centered and multimorbidity care? A scoping review. BMC Health Serv Res. (2018) 18:1–9. doi: 10.1186/s12913-018-3213-8
35. Halladay JR, Vu M, Ripley-Moffitt C, Gupta SK, O'Meara C, Goldstein AO. Patient perspectives on tobacco use treatment in primary care. Prevent Chron Dis. (2015) 12:140408. doi: 10.5888/pcd12.140408
36. Barry MJ, Edgman-Levitan S. Shared decision making–pinnacle of patient-centered care. New England J Med. (2012) 366:780–1. doi: 10.1056/NEJMp1109283
37. Hansen EC, Nelson MR. How cardiac patients describe the role of their doctors in smoking cessation: a qualitative study. Aust J Prim Health. (2011) 17:268–73. doi: 10.1071/PY10082
38. Wilkes S, Evans A. A cross-sectional study comparing the motivation for smoking cessation in apparently healthy patients who smoke to those who smoke and have ischaemic heart disease, hypertension or diabetes. Fam Pract. (1999) 16:608–10. doi: 10.1093/fampra/16.6.608
39. Gerber Y, Rosen LJ, Goldbourt U, Benyamini Y, Drory Y. Infarction ISGoFAM. Smoking status and long-term survival after first acute myocardial infarction: a population-based cohort study. J Am Coll Cardiol. (2009) 54:2382–7. doi: 10.1016/j.jacc.2009.09.020
40. Prochaska JO. he transtheoretical model of health behavior change. Am J Health Promot. (1997) 12:38–48. doi: 10.4278/0890-1171-12.1.38
41. Andersen S, Keller C, McGowan N. Smoking cessation: the state of the science: the utility of the transtheoretical model in guiding interventions in smoking cessation. Online J Knowl Synth Nurs. (1999) 6:112–26. doi: 10.1111/j.1524-475X.1999.00112.x
42. Kumar A, Tiwari A, Gadiyar A, Gaunkar RB, Kamat AK. Assessment of readiness to quit tobacco among patients with oral potentially malignant disorders using transtheoretical model. J Educ Health Promot. (2018) 7:9–19. doi: 10.4103/jehp.jehp_75_17
43. Thankappan K. Tobacco cessation in India: a priority health intervention. Indian J Med Res. (2014) 139:484.
44. Jongen C, McCalman J, Bainbridge R. Health workforce cultural competency interventions: a systematic scoping review. BMC Health Serv Res. (2018) 18:1–15. doi: 10.1186/s12913-018-3001-5
45. Kotseva K, Wood D, De Backer G, De Bacquer D, Pyörälä K, Reiner Ž, et al. EUROASPIRE III. Management of cardiovascular risk factors in asymptomatic high-risk patients in general practice: cross-sectional survey in 12 European countries. Eur J Prev Cardiol. (2010) 17:530–40. doi: 10.1097/HJR.0b013e3283383f30
46. Thresia C, Thankappan K, Nichter M. Smoking cessation and diabetes control in Kerala, India: an urgent need for health education. Health Educ Res. (2009) 24:839–45. doi: 10.1093/her/cyp020
47. Jones R, Hyland ME, Hanney K, Erwin J. A qualitative study of compliance with medication and lifestyle modification in Chronic Obstructive Pulmonary Disease (COPD). Prim Care Respir J. (2004) 13:149–54. doi: 10.1016/j.pcrj.2004.05.006
48. Siddiqi K, Dogar OF, Siddiqi N. Smoking cessation in long-term conditions: is there “an opportunity in every difficulty”. Int J Popul Res. (2013) 2013:10. doi: 10.1155/2013/251048
49. Bhatt G, Goel S. Using non-communicable disease clinics for tobacco cessation: a promising perspective. Natl Med J India. (2018) 31:172–5. doi: 10.4103/0970-258X.255763
50. Directorate General of Health Services. Ministry of Health and Family Welfare Government of India. Manuals for Training in Cancer Control. National Cancer Control Programme (2005). Available online at: https://cdn.who.int/media/docs/default-source/searo/india/health-topic-pdf/tobacco/tobacco-free-initiative-manual-for-tobacco-cessation.pdf?sfvrsn=79ae2551_2
51. Directorate General of Health Services. Ministry of Health & Family Welfare Government of India. Tobacco Dependence Treatment Guidelines. National Tobacco Control Programme (2011). Available online at: http://ntcp.nhp.gov.in/assets/document/Guideline-manuals/Tobacco-Dependence-Treatment-Guidelines.pdf
52. World Health Organization. Regional Office for South-East Asia. Tobacco Cessation: A Manual for Nurses, Health Workers and Other Health Professionals. WHO Regional Office for South-East Asia (2010). Available online at: https://apps.who.int/iris/handle/10665/206012
53. World Health Organization. Toolkit for Delivering the 5A's and 5R's Brief Tobacco Interventions in Primary Care. World Health Organization (2014). Available online at: https://apps.who.int/iris/handle/10665/112835
54. Panda R, Jena PK. Examining physicians' preparedness for tobacco cessation services in India: findings from primary care public health facilities in two Indian states. Australas Med J. (2013) 6:115. doi: 10.4066/AMJ.2013.1617
55. Government of Punjab, India. (2022). Available online at: https://punjab.gov.in/
56. Sikh Rehat Maryada in English. Official Website of Shiromani Gurdwara Parbandhak Committee (S.G.P.C.). (2022). Available online at: https://sgpc.net/?page_id=656
57. Singh K. Shiromani Gurdwara Parbandhak Committee: An Overview. Oxford Handbooks Online (2013). doi: 10.1093/oxfordhb/9780199699308.013.039
58. Menon S, Bisht R, Nair B. Contextualising tobacco use in the social, economic and political transformation of Punjab. J Ethn Subst Abuse. (2020) 21:793–822. doi: 10.1080/15332640.2020.1808871
59. World Health Organization. International Institute for Population Sciences (IIPS) and Ministry of Health and Family Welfare, Government of India, Global Adult Tobacco Survey India (GATS India); 2009–2010. World Health Organization (2022). Available online at: https://nada.searo.who.int/index.php/catalog/55
60. Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: Issues for the cultural adaptation and development of psychosocial treatments with Hispanics. J Abnorm Child Psychol. (1995) 23:67–82. doi: 10.1007/BF01447045
61. Ahluwalia J, Baranowski T, Braithwaite R, Resnicow K. Cultural sensitivity in public health: defined and demystified. Ethn Dis. (1999) 9:10–21.
62. Kreuter MW, Lukwago SN, Bucholtz DC, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. (2003) 30:133–46. doi: 10.1177/1090198102251021
63. Mormina M, Pinder S, A. conceptual framework for training of trainers (ToT) interventions in global health. Global Health. (2018) 14:1–11. doi: 10.1186/s12992-018-0420-3
64. Suzuki T. The effectiveness of the cascade model for in-service teacher training in Nepal. In: IMSCI 2008 - 2nd International Multi-Conference on Society, Cybernetics and Informatics, Proceedings. International Institute of Informatics and Systemics (2008). p. 272–7.
65. Pearce J, Mann MK, Jones C, Van Buschbach S, Olff M, Bisson JI. The most effective way of delivering a train-the-trainers program: a systematic review. J Contin Educ Health Prof. (2012) 32:215–26. doi: 10.1002/chp.21148
66. Nigg CR, Geller KS, Motl RW, Horwath CC, Wertin KK, Dishman RK, et al. research agenda to examine the efficacy and relevance of the transtheoretical model for physical activity behavior. Psychol Sport Exerc. (2011) 12:7–12. doi: 10.1016/j.psychsport.2010.04.004
67. Cahill K, Lancaster T, Green N. Stage-Based Interventions for Smoking Cessation. Cochrane Database of Systematic Reviews (2010). doi: 10.1002/14651858
Keywords: intervention development, multi-component, tobacco cessation, socio-cultural, behavior, NCD clinics, India
Citation: Bhatt G, Goel S, Grover S, Medhi B, Singh G, Gill SS, Swasticharan L and Singh RJ (2022) Development of a multi-component tobacco cessation training package utilizing multiple approaches of intervention development for health care providers and patients attending non-communicable disease clinics of Punjab, India. Front. Public Health 10:1053428. doi: 10.3389/fpubh.2022.1053428
Received: 25 September 2022; Accepted: 08 November 2022;
Published: 02 December 2022.
Edited by:
Allen C. Meadors, Independent Researcher, Seven Lakes, United StatesReviewed by:
Jeff Bolles, University of North Carolina at Pembroke, United StatesTimothy Lynn Taylor, University of North Carolina at Pembroke, United States
Copyright © 2022 Bhatt, Goel, Grover, Medhi, Singh, Gill, Swasticharan and Singh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sonu Goel, c29udWdvZWwwMDdAeWFob28uY28uaW4=
 Garima Bhatt
Garima Bhatt Sonu Goel
Sonu Goel Sandeep Grover
Sandeep Grover Bikash Medhi
Bikash Medhi Gurmandeep Singh6
Gurmandeep Singh6