- 1Center for Urban Health Disparities Research and Innovation, Morgan State University, Baltimore, MD, United States
- 2Resident Services Inc., Housing Authority of Baltimore City, Baltimore, MD, United States
- 3Prevention Science Research Center, Morgan State University, Baltimore, MD, United States
- 4Department of Urban Public Health, Charles R Drew University of Medicine and Science, Los Angeles, CA, United States
- 5Department of Family Medicine, Charles R Drew University of Medicine and Science, Los Angeles, CA, United States
- 6School of Community Health and Policy, Morgan State University, Baltimore, MD, United States
Introduction: Tobacco use disproportionately affects low-income African American communities. The recent public housing smoke-free policy has increased the demand for effective smoking cessation services and programs in such settings.
Methods: This mixed-method pilot study explored feasibility and potential impact of a peer-mentoring program for smoking cessation in a public housing unit. The quantitative study used a quasi-experimental design while qualitative data were collected via focus group discussions with peer mentors and participants. Three residents of the public housing complex were trained as peer mentors. Each peer mentor recruited up to 10 smokers in the residence and provided them individual support for 12 weeks. All participants were offered Nicotine Replacement Therapy (NRT). A follow-up investigation was conducted 3 months after completion of the 12-week intervention. At baseline and follow-up, the participants' smoking status was measured using self-report and was verified using exhaled carbon monoxide (eCO) monitoring.
Results: The intervention group was composed of 30 current smokers who received the peer-mentoring intervention. The control group was composed of 14 individuals. Overall mean eCO levels dropped from 26 ppm (SD 19.0) at baseline to 12 (SD 6.0) at follow-up (P < 0.01). Participants who were enrolled in our program were more likely to have non-smoking eCO levels (<7 ppm) at follow-up (23.3%) compared to those who did not enroll (14.3%).
Conclusion: Our program is feasible for low-income predominantly African American communities. Using peers as mentors may be helpful in providing services for hard-to-reach populations. Given the non-randomized design of our study, randomized trials are needed to test the efficacy of our program in the future.
Introduction
After release of the first report of the Surgeon General's Advisory Committee on Smoking and Health in 1964, tobacco use began to decline. Subsequent interventions accelerated the decline, and today, the Centers for Disease Control and Prevention (CDC) reports that only 14.0% of adults in the U.S. smoke tobacco (1). Despite these overall gains from tobacco control programs, low income marginalized populations continue to be disproportionately harmed by smoking. The burden of tobacco is not evenly distributed; rather, shows large disparities by socioeconomic factors such as income, education, and race/ethnicity. Across the nation, smoking prevalence is inversely related to income and varies by racial and ethnic groups (1). In Maryland, Baltimore City has a higher prevalence of smoking and significantly greater health problems caused by smoking health disparities compared to the rest of the state. According to the Baltimore City Health Department, the 2014 smoking prevalence for Baltimore City was 33% while Maryland had a total smoking prevalence of 15.1% (2, 3).
Populations in the inner-city, including those living in assisted public housing, have some of the highest rates of tobacco use. Recipients of housing assistance in the U.S. are, by definition, socioeconomically disadvantaged (4–6). In 2017, more than one-third (33.6%) of adults receiving housing assistance were current smokers (7). The proportion of adults in U.S. public housing who reported excellent or good health was only 37.7%, compared to 48.7% of other low income people who did not live in public housing, and 66.8% of adults who were not poor (6).
The Department of Housing and Urban Development (HUD) implemented a Smoke-Free Housing policy on December 5, 2016, which became effective February 3, 2017. All Public Housing Agencies (PHAs) were to comply with the smoke-free policy within 18 months of the effective date. Managers and builders of these housing units were all expected to develop and implement plans to comply with the mandate. At the time of this study, fewer than 14% of public housing authorities in the U.S. had initiated smoke-free policies to limit smoking in residents' units (8). This mandate represented a valuable opportunity to test innovative smoking cessation services to help public housing authorities comply with the HUD initiative (9–11).
This study used a community-based participatory research (CBPR) approach, which is an effective model for reaching hard-to-reach populations with interventions based on behavior change. Because smoking is one of the biggest health threat that low income populations face, CBPR is especially important for reducing health disparities through smoking cessation. CBPR facilitates equitable engagement and participation of relevant community stakeholders in all aspects of the research to ensure shared ownership and more effective translation of the findings (12–16). CBPR-based interventions can be applied in diverse settings and facilitated by a diverse group of providers. The peer-facilitated CBPR approach is a promising model through which trained and experienced peers–an important group of stakeholders in CBPR–are engaged as educators, mentors, and sources for providing culturally relevant trainings and social support. Community-based peer-facilitated interventions have been shown to improve outcomes for interventions targeted at health-related behaviors (17–20), especially through providing smoking cessation services (20–22). Engaging peers brings valuable advantages for addressing health problems among vulnerable groups including those in mental health institutions, in drug recovery programs, and those who live in public housing (22, 23).
Given the role of feasibility studies to determine how programs can be more effectively implemented (24), we examined the feasibility and potential impact of a peer-mentoring smoking cessation program based in a public housing facility. The intervention adapted the structure, approach and curriculum of the Communities Engaged and Advocating for a Smoke-free Environment (CEASE), a well-established CBPR partnership in Baltimore Maryland (16, 25, 26). This intervention provided a valuable opportunity for a public housing complex to comply with the HUD initiative.
Methods
Study design and setting
This was a mixed method convergent parallel study design using quasi-experimental methods. The study was conducted in a federally subsidized public housing unit (Monument East apartments) in Baltimore City from 2016 to 2018. The unit was selected for the Peer Mentoring project because of its location in an underserved neighborhood and an anecdotal estimated smoking prevalence among its residents of 50%. In addition, Monument East had an existing relationship with community partners, provided accessibility to the target population (underserved residents of the apartments), and the facility's management were willing to support smoking cessation services for their residents.
Intervention
This intervention was guided by the Social support theory, a multi-faceted concept that has been applied to smoking cessation interventions with varying measures that assess the structure and function of social networks (27, 28). Social support encompasses any process through which social relationships can enhance health and wellbeing (29).
Mentor recruitment and training
Six former smokers who resided in Monument East Apartments were selected to participate as mentors in the program. These former smokers were trained on peer mentorship and smoking cessation, including motivational enhancement and relapse prevention, using the CEASE curriculum. They also received training on ethical considerations and the peer mentoring model for this project. At the end of their training, three participants were certified as peer mentors for smoking cessation. A toolbox of resources used in the CEASE program was provided to the mentors to supplement the support they provided to the participants based on individual needs. The mentors were trained and supported during the course of the intervention by experienced CEASE Peer Motivators (16, 25, 26).
Participant recruitment and training
Participants who were 18 years and older and were current smokers (defined as smoking at least three cigarettes per day in the past week) were recruited for the study through a baseline survey. Qualified participants who completed the baseline survey but did not enroll for the mentoring were regarded as controls. Participants were invited to take the survey through fliers posted in the building, word-of-mouth from mentors and other residents. Out of the 65 residents of the public housing unit who participated in the baseline survey, 44 were current smokers from whom 30 were enrolled and participated in the program.
The baseline survey was used to determine smoking rates among the residents and to recruit current smokers willing to join the program. Each peer mentor was instructed to reach out to approximately 10 participants who were qualified and willing to enroll in the program and establish a mentoring relationship preferably based on their existing relationships. Recruited participants received a single group counseling session facilitated by a CEASE Peer Motivator prior to entering into a “mentorship agreement” that included a quit-smoking plan and a follow-up plan. The Agreement described how mentors and participants would communicate and engage during the intervention. Options included face-to-face meetings, telephone calls, text messaging, emails, and any other modes of communication agreed upon by the parties. Mentors maintained logs of all communications with their participants and cessation outcomes. They kept track of the support they provided, their participants' experiences using NRT and participants' adherence to their quit plans.
NRT component
In addition, participants received a start-up dose of Nicotine replacement therapy (patch, gum or lozenges), depending on their level of nicotine dependency, which could be refilled if desired. While all participants received patch, receiving other forms of NRT was only based on request of the participant.
Incentive
Participants received cash incentives for participating in mentoring or counseling sessions ($10 per session) and follow-up interviews ($20). Participants received similar incentive at baseline and follow up regardless of their group membership. Thus, the incentive is not very likely to have biased the effect of participating in the intervention.
Quantitative methodology
Timeline
The mentoring sessions lasted for 12 weeks. Twelve to 16 weeks after the mentoring phase, participants were contacted by mentors to complete a follow-up survey and determine their smoking status using an expired carbon monoxide monitoring test.
Data collection
Data were collected using paper-based surveys. The baseline survey captured information on demographics, physical and behavioral health, smoking history, barriers to quitting, stages of change and other variables. Participants completed progress forms during their interactions with the mentors which captured information on their adherence to their quit plan, motivators and barriers to quitting and aids for success. The follow-up questionnaires captured information on participants' smoking status and barriers to quitting.
Measures
Independent variable
Participants were categorized as “intervention-group” or “control-group” depending on whether they enrolled in the program or not. “Intervention-group” was coded as 1 and “control-group” was coded as 0.
Covariates
Sociodemographic characteristics included race, age, gender, employment status, marital status, and educational attainment.
Tobacco dependence
At baseline all participants were administered the Fagerström Nicotine Dependency Test to determine the intensity of their physical addiction to nicotine (30–32). Scores on the Fagerström Test potentially range from 0 (low) to 10 (high dependence).
Outcome
Quit and smoking status of each participant was ascertained during the peer-mentoring sessions, at the completion of the cessation program, and through the 12–16 week follow-up survey. Participants were categorized as “quit” or “didn't quit” based on self-reported smoking abstinence.
Confirmatory CO measurement
Verified by expired-air CO (eCO) levels. A level of 7 ppm was considered as “quit” while > 7 ppm was considered as “didn't quit”(33, 34). A carbon monoxide breath monitor was used to verify the smoking status of participants at every stage (34). Research has used a threshold of 7 ppm to indicate successful or unsuccessful quit. While eCO >7 ppm has been considered as “quit”, eCO > 7 ppm is considered as failure to quit (33). In our study, however, quit outcome was based on self-report and eCO measure was only confirmatory rather than being a criteria for successful quit.
Quantitative data analysis
Data was entered into EpiData version 3.1 (35) without personal identifiers and exported into STATA 14 (36) for cleaning and analysis. Descriptive univariate and bivariate analyses were conducted to review each variable and summarize demographic and baseline information by intervention arm. A bivariate analysis was done to compare baseline variables by intervention arm, using chi-square tests of independence for categorical variables (gender, race, education, marital status and employment status), and one-way Analysis of Variance (ANOVA) tests for continuous variables (age and Fagerström score). In estimating the study outcome, participants who did not complete the follow-up assessments were classified as “didn't quit”. This penalized imputation approach where participants with missing data were assumed to still be smokers has been applied as a method of conservatively estimating smoking cessation outcomes (37, 38).
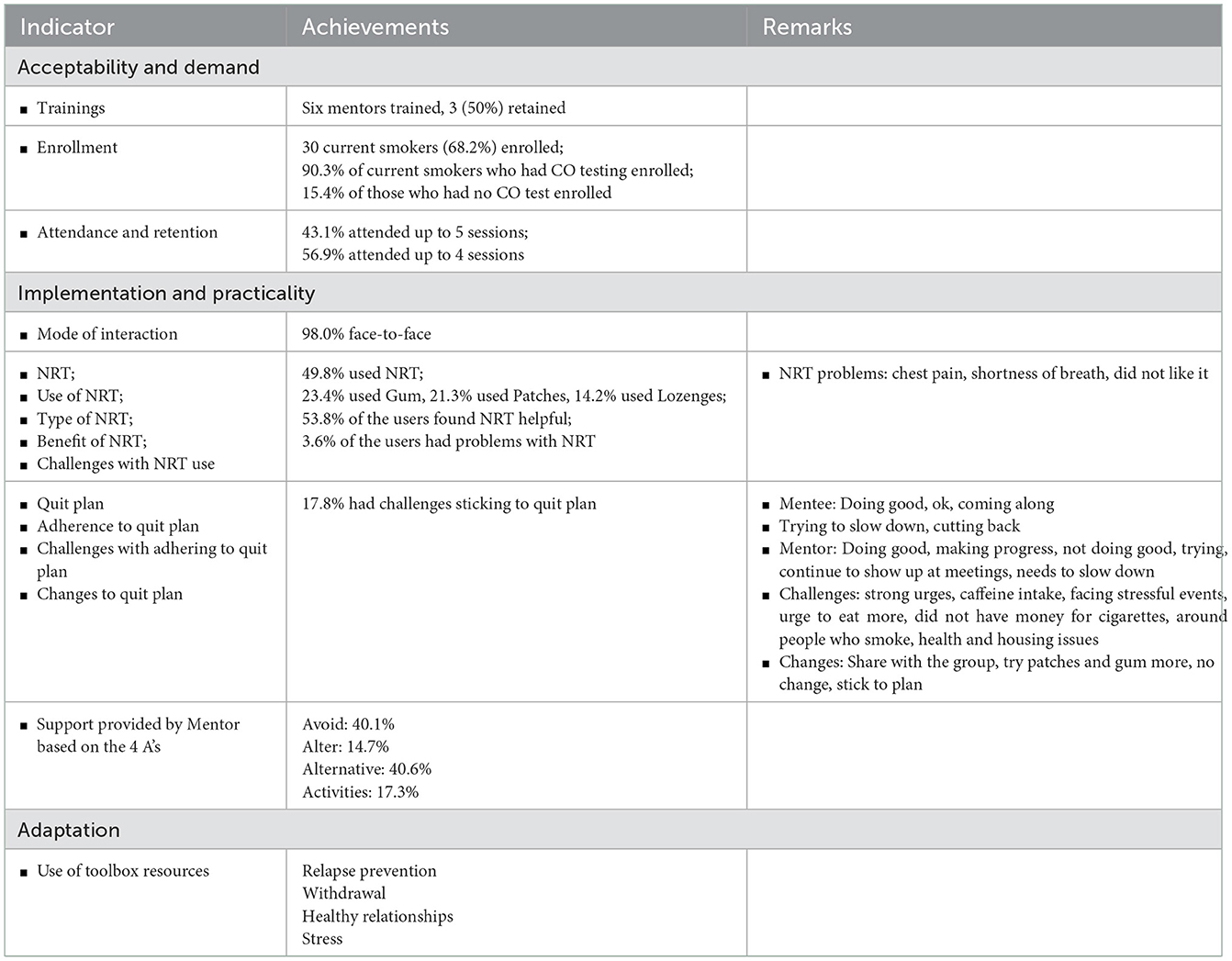
Assessing feasibility
Indicators used to assess feasibility included acceptability, demand, implementation, practicality, and adaptation (24, 39, 40). These indicators were measured by counting the number of trainings provided, enrollment into the program, session attendance and retention, mode of interactions, NRT use, adherence to quit plan, support provided by mentor, and use of the resources in the toolbox.
Qualitative methodology
Intervention design
Qualitative inquiry using a phenomenological approach was applied to better understand the motivators of and barriers to smoking cessation (41). Using a convergent parallel design, findings from the quantitative and qualitative components of this study are integrated to examine factors that influence smoking cessation.
Sampling and recruitment
Participants were recruited through phone calls or word of mouth by site coordinators, Peer Motivators and peer mentors. Flyers were also posted in the relevant communities with contact information for recruitment. Focus group discussion (FGD) participants received financial incentives ($20) for their participation.
Measures
Interview guides were developed to capture participants' past experiences with smoking, quitting and the CEASE interventions; perceived barriers to quitting; expected aids for success; interactions with peer mentors (including perceived levels of social support provided) (42), strengths and weaknesses of the program; and recommendations for improving the program. Other measures included knowledge of smoking cessation resources and the public housing smoke-free policy. The interview guides for the peer mentors captured information on smoking and quitting history, participation motivators or barriers, experiences with the CEASE program and mentees, knowledge of the smoke-free policy and recommendations for future programs.
Data collection
Triangulation was achieved by collecting data from multiple sources. Three focus group discussions (FGDs) were conducted with a subset of program participants (n = 12) and one FGD was conducted with five peer mentors; three who continued and two who dropped out of the program. Focus group discussion moderator's guides were developed using semi-structured questions to probe for detailed information about smoking history, experiences with the intervention, motivators that helped and barriers that challenged efforts to quit, perceptions of the program's strengths and weaknesses.
Data analysis
The focus group discussions were audio recorded and transcribed into word documents. Transcripts were reviewed independently by two researchers and coded manually by reading through each transcript, extracting participants' responses and organizing them into relevant themes or subthemes in a tabular format. The integrity of the coding was verified through comparing and consolidating any disagreements between the emerging codes and themes generated through independent works of the two researchers. A convergent parallel design was used to integrate the results of the quantitative and qualitative components.
Results
Quantitative results
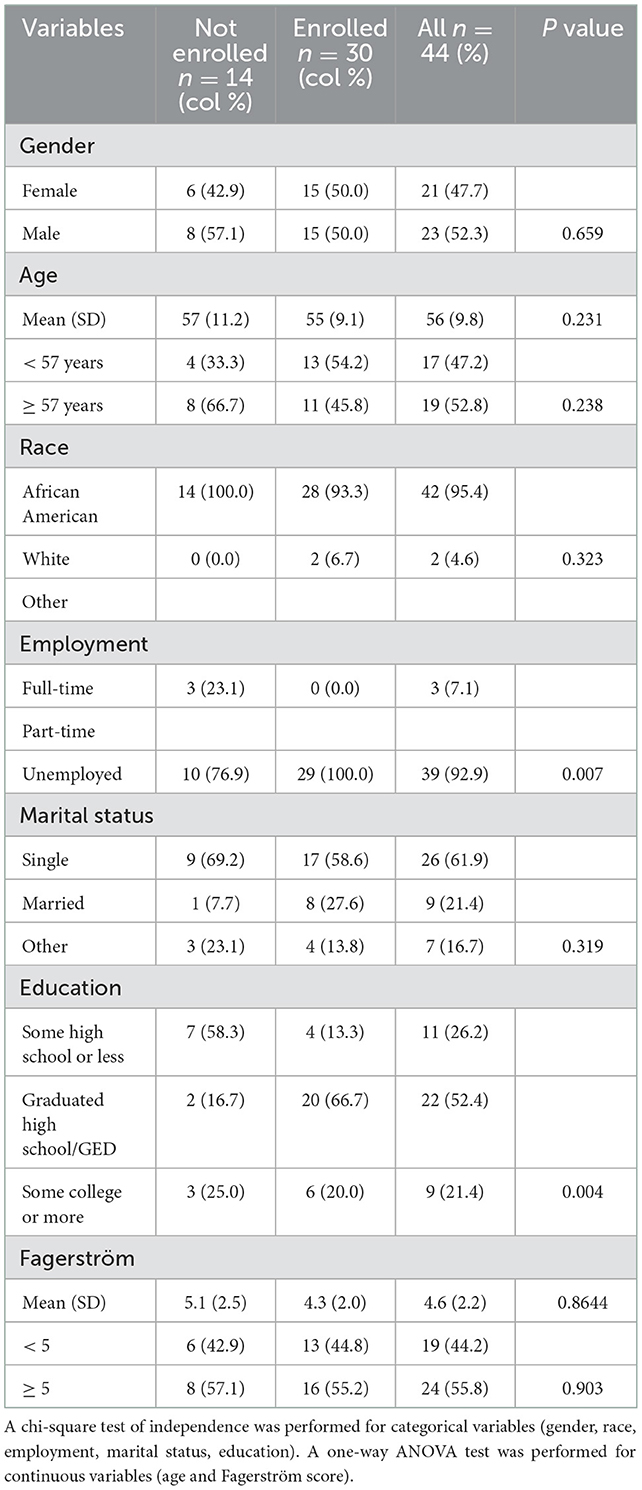
Table 1 shows the sociodemographic and baseline characteristics of intervention-group (n = 30) compared with the control group (n = 14). Men constituted 52.3% of overall participants, 52.8% were 55 years or older, and 95.4% were African American. Most participants (92.9%) were unemployed, 61.9% were single and 52.4% had graduated from high school. The mean Fagerström score was 4.6 (standard deviation = 2.2). All intervention group (100%) were unemployed, compared to 76.9% of the control group (P = 0.007). Of those who enrolled in the program, 66.7% had graduated from high school, compared to 16.7% of those who did not enroll (P = 0.004). Gender, age, race, marital status, and Fagerström scores were not significantly different in the group who enrolled, compared to those who did not.
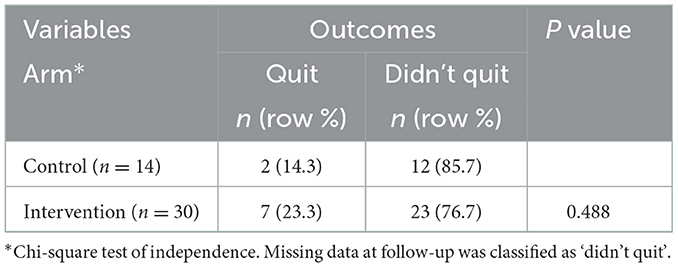
Selected quantitative outcomes are presented in Tables 2–4. The follow-up response rate was 80% (n = 24) for the intervention group and 71% (n = 10) for the control group, thus information on smoking status at three months post-intervention was only available for the 34 participants who completed the follow-up assessments. Sample sizes were not large enough to conduct multivariable or other more detailed analyses. The smoking cessation rate (CO levels <7 ppm) in the total population was 20.5% at follow-up. A chi-square test of independence compared smoking cessation rates between the intervention (23.3%) and control (14.3%) groups. This difference was not statistically significant (P = 0.488) (Table 2).
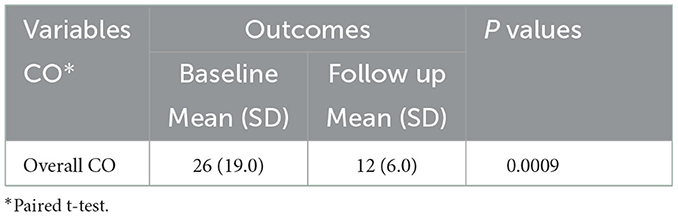
Using a paired t-test, the mean CO level at baseline was compared with the mean CO level at follow-up for all participants. Within the total population, the mean follow-up CO level decreased by 14 ppm from the mean baseline CO level (P = 0.0009) (Table 3).
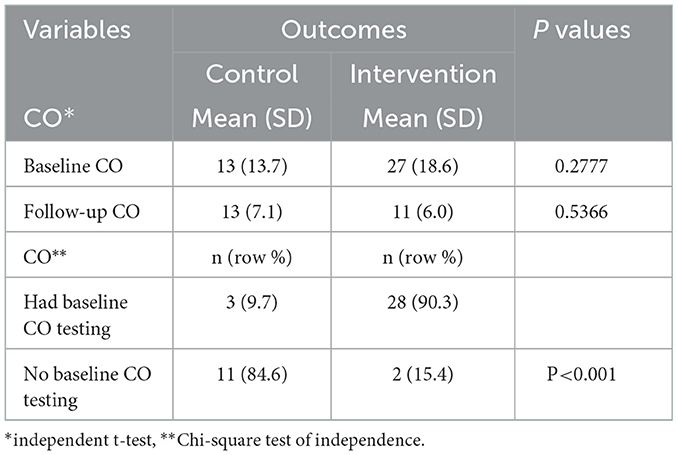
Two independent sample t-tests were performed to compare the difference in mean CO levels by enrollment status at baseline and at follow-up. At baseline, the enrolled residents had a higher mean CO level [27 (standard deviation = 18.6)] than those who had not enrolled [13 (standard deviation = 13.7)]. At follow-up, the difference in mean CO levels between the enrolled and non-enrolled residents narrowed [11 (standard deviation = 6.0) and 13 (standard deviation = 7.1) respectively], however, these differences were not statistically significant (Table 4). A chi-square test of independence comparing enrollment among residents who had CO breath tests at baseline with those who did not showed that having a CO breath test increased the likelihood of enrolling in the program; 90.3% of those who had a CO breath test enrolled in the program compared to 15.4% of those who did not have a CO breath test (P < 0.001) (Table 4).
An evaluation of the feasibility of the peer mentoring program based on selected indicators (acceptability, demand, implementation, practicality, and adaptation) is presented in Table 5. Six mentors were trained and three continued with the program while three others could not continue for personal reasons. Each of the 30 enrolled participants was expected to attend a maximum of seven sessions over the course of three months. Outcomes from a total of 197 interactions between participants and their mentors are presented. They show that 56.9% of participants completed four sessions out of the seven; 98.0%of these sessions were held as face-to-face meetings while 2% were through other means such as phone calls and text messages. Use of NRT was reported in 49.8% of these interactions from whom 53.8% found NRT to be helpful. Challenges with the NRT were reported in 3.6% of the interactions and 17.8% had challenges sticking to their quit plan. Support was provided to the participants by their mentors based on the four A's of dealing with challenges to quitting. Most interactions involved support for finding Alternatives to smoking (40.6%), and Avoiding situations that could trigger smoking (40.1%). Other support included alternative Activities in which to engage (17.3%) and Altering routine habits (14.7%) to curb the cravings. Based on options used from the toolbox provided to mentors the most common topics discussed included relapse prevention, withdrawal, healthy relationships and managing stress.
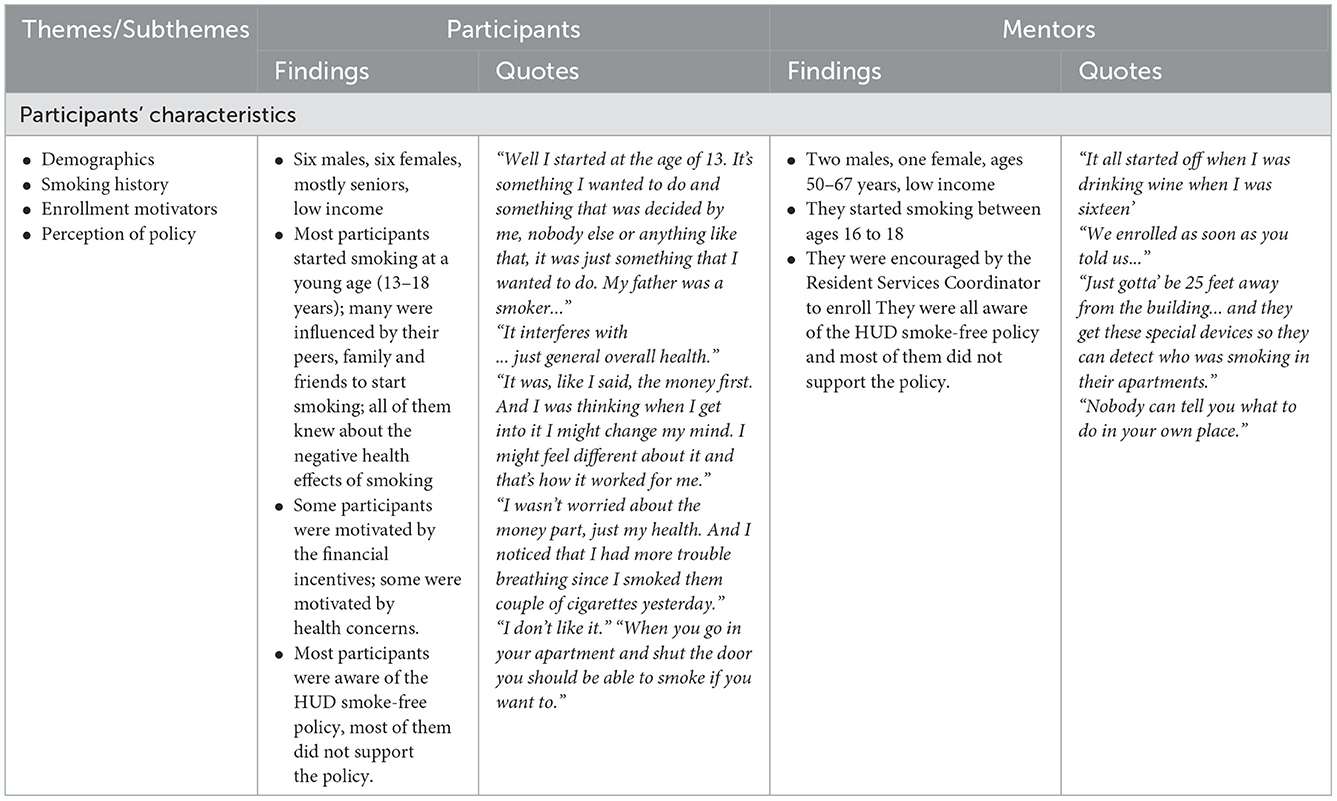
Qualitative results
Table 6 presents our findings from the qualitative assessment of the public housing peer mentoring program. Themes and subthemes from three FGDs held with a total of 12 participants. The themes describe participants' characteristics, their experiences with the program and their recommendations for future programs. FGD participants' ages ranged from 50-67 years; six of them were men, and six were women.
Smoking history
Most participants initiated smoking at a young age. Some participants were influenced by peers or family members to start smoking while others initiated smoking due to life stressors.
Enrollment motivators
The participants heard about the CEASE program mostly via word of mouth, and also through the site coordinator or flyers posted in the building.
Motivation to participate in the program
The motivation to join the program ranged from health reasons to family. For some of them, the incentives motivated them to participate and remain in the program. Some residents who did not participate cited not having enough time as a reason for not participating.
Experience with the peer mentoring program
Participants cut down the number of cigarettes smoked or stopped and started again. Some aids to quitting as mentioned by participants included the education they received in the CEASE classes, the peer support they received and the NRT provided. For some participants, they mentioned that NRT was not very helpful for them. Some barriers for quitting identified by participants included low self-efficacy and being around others who smoke. In terms of the program, most participants said that they found the curriculum helpful and educative. They also found the visual aids about harmful components of cigarettes helpful. A few participants noted an improvement in their health due to the change in their smoking behavior during the program. Almost all participants agreed that meeting in a group helped them stay involved and feel less alone.
Perception of the smoke-free policy
In terms of the smoke-free policy, most residents (intervention and control) were aware of the public housing smoke-free policy. A few of them were in support of it but most of them had certain misgivings about the policy.
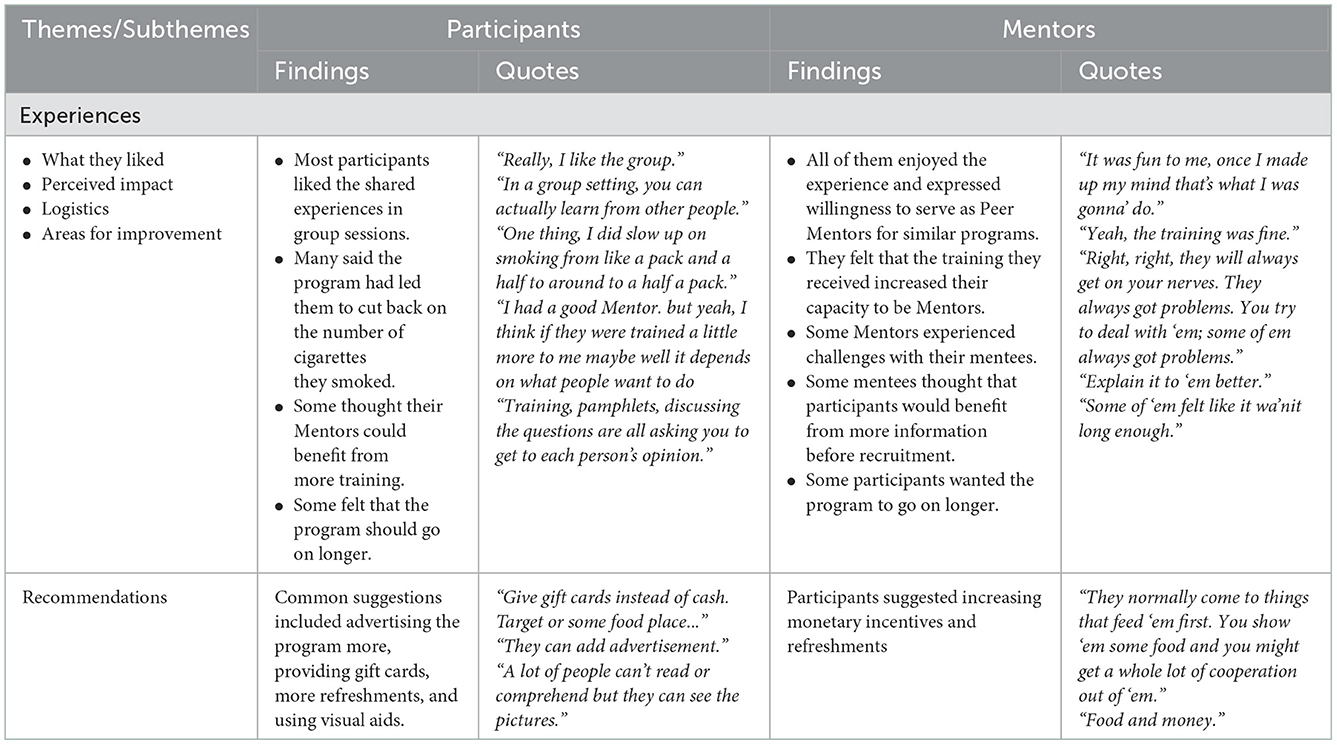
Table 7 also presents findings from the qualitative assessment of mentors who were trained for the public housing peer mentoring program. At the end of the training, three trained mentors decided not to continue with the program due to other conflicting time schedules. Themes and subthemes from three FGDs held with a total number of six mentors (three who continued in the program and three who were unable to continue) are presented in this table. The themes describe participants' characteristics, their experiences with the program and their recommendations for future programs.
Experience with the peer mentoring program
All mentors got to know about the program through the resident service coordinator who encouraged them to participate as mentors due to their non-smoking status. Most peer mentors felt that they would need further training to build their capacity as mentors. Overall, they enjoyed the mentoring experience and said they were willing function in that capacity for future programs. Some mentors however expressed having some challenges with the process of supporting the participants. They felt that they needed more time to work with mentees.
Perception of the smoke-free policy
The mentors were all aware of the smoke-free policy, however, some of them had reservations about the smoke-free policy being rolled out in their building.
Recommendations and areas for improvement
Most mentors recommended maintaining monetary incentives and providing refreshments to motivate participants to remain in the program. They also recommended reducing the amount of paperwork involved in implementing the program.
Discussion
Our pilot study applied a mixed methods design to explore the feasibility and potential efficacy of a peer-mentoring program in public housing in response to HUD's announcement of the smoke-free housing initiative. We found preliminary results suggestive of the potential efficacy of peer mentoring for tobacco cessation. We discuss some of our main quantitative and qualitative findings here but given the limitations of this study such as small sample size and quasi-experimental design with lack of randomization, future research is needed to further confirm these results.
In this pilot study which was conducted in a public housing unit in Baltimore City, residents were recruited and offered smoking cessation classes led by peer mentors who were themselves former smokers. Because the peer mentors lived in the same complex, they were able to have frequent and personal interactions with the participants outside the class setting. The participants could directly observe the smoke-free lifestyle of their mentors and model their healthy behaviors. Participants could easily contact their mentors when facing any challenges. Mentoring has been documented in prior research to be beneficial for addressing a wide range of behavioral and health problems including smoking (43, 44).
More than 23% of the intervention group had nonsmoking eCO levels at three-month follow-up compared to 14.3% of the control group. However, due to the small sample size, this difference did not reach statistical significance. Another notable finding was an overall decrease in the mean eCO levels for all participants (enrollees and non-enrollees) from 26 ppm at baseline to 12 ppm at follow-up (SD = 19.0 and 6.0 respectively). It is interesting that 14.3% of non-enrollees also achieved smoking cessation eCO levels, and that all participants achieved a decrease in mean eCO levels. While contamination of the control group (non-enrollees) due to diffusion of information from enrollees cannot be ruled out, other factors such as the prevalence of unassisted quitting in the general population might be considered. Enrollees and non-enrollees all lived in the same complex and in some cases were housemates or spouses. The information provided to enrollees and their lifestyle modifications resulting from the mentoring sessions could have been adopted by non-enrollees who knew them or lived with them. This could be considered a form of contamination of a control group (45). These results could have important implications for smoking cessation efforts in public housing and other residential complexes where lifestyle and behavioral changes introduced by a small group of persons diffuse to other residents causing unintended but positive health outcomes (46).
Certain indicators were utilized to determine the feasibility of this intervention and to examine its scalability. Almost 70% of surveyed residents who were current smokers enrolled in the mentoring program, suggesting the attractiveness of cessation services in this group even though prior research has shown that underserved populations have lower intentions to quit (47). The provision of cash incentives to participants could also have increased the interest in participation and engagement in the program. About 60% of residents who enrolled in the program attended at least four of the seven mentoring sessions offered. Considering the high risk of drop-out in this type of population (13, 48), this was a promising outcome that might have resulted from the convenience of the intervention being located in the same building where the participants resided. A summary of 197 interactions that the 30 mentees had with their mentors over the three-month period of the study revealed useful information about NRT use in this population. NRT use was reported in only about half of the sessions. The most commonly used form of NRT was gum (23.4%); the least used form was lozenges (14.2%). NRT use was reported to be helpful in 53.8% of interactions with those who used the products. However, 3.6% of the participants reported problems including chest pain and shortness of breath after using NRT, or that they just “did not like it.” Studies show that although adverse effects of NRT are rare, some people do experience discomfort with all forms of NRT. According to the authors of these studies, the adverse effects according are not sufficient to recommend discontinuation of NRT (49, 50).
Results showed that about 18% of participants had difficulty with adhering to their quit plans. Reported challenges included facing stressful events, having strong urges, and dealing with triggers such as caffeine. Barriers to quitting that have been well documented in prior research include being around people who smoke, having strong cravings and stressful events (51, 52). In describing the barriers to quitting, one participant said “When I'm around people that start smoking, the Jones start to kick in, the urge starts coming in and if I don't leave I am going to ask for one…” Most participants however, were motivated to at least cut back. They cited health problems, not having money for cigarettes and the peer support they received as factors that motivated them to adhere to their quit plans (53). One participant stated “I needed the program myself ‘cause I was in bad shape at that time with my lungs”.
Mentors supported participants by using the four A's for dealing with barriers to quitting. Of the 197 interactions, the most support was provided on “Alternatives” to smoking (40.6%), and “Avoiding” certain places or people (40.1%). The most discussed resources from the toolbox provided to mentors were relapse prevention, withdrawal, healthy relationships and stress (54–56).
Smoke-free public housing policies are intended to reduce secondhand smoke exposure for residents. Research shows that such policies also help to reduce smoking rates (57). Residents of public housing have been found to have higher rates of smoking compared to the general population. Public housing residents are typically of low socioeconomic status and tend to have a myriad of social and environmental factors that increase their chances of engaging in unhealthy behaviors such as smoking (4–7). They also experience poorer health compared to the general population, which interacts in a cyclical way to further increase their everyday stress and worsen their health and health behaviors (6).
Smoke-free initiatives are important steps in protecting the health of poor and underserved public housing residents, including smokers and nonsmokers (58–61). The reduction in secondhand smoke exposure for infants, children, seniors and persons with disabilities in public housing could be pivotal in addressing long-standing tobacco-related health disparities (58–61). The initiative is also expected to result in substantial cost savings in healthcare expenditures (62) and even in the costs of cleaning units for new tenants.
Determining the feasibility of this program in public housing is essential because of the documented challenges of involving these populations in smoking cessation research and interventions. Residents of public housing have traditionally been hard-to-reach populations with competing socio-environmental pressures that make them less willing to enroll (63) and participate in such programs (64). Residents may view interventions directed at changing their health behaviors as paternalistic, thereby creating mistrust and limiting their participation (65). Interventions that are not culturally specific or tailored to the target population may therefore not succeed (48). A study by Geller, Rees and Brooks (2016) showed that minorities in public housing reported a lower use of NRT than their White counterparts (58). As discussed previously, recruitment, class attendance and retention have been challenging for this population. That is why these specific indicators were assessed in the current study.
One of our lessons learned was that the location of the smoking cessation services in the same complex where participants lived may have contributed to the success of our program. Delivery of services by peers who resided in the same building and had lived through similar experiences was reported to be instrumental in establishing trust and building mentoring relationships with the participants. Additionally, providing cash incentives likely encouraged participation and engagement in the program. Lastly, strong partnership with involvement of diverse community stakeholders contributed to creation of a shared sense of ownership of the program and its successful implementation.
History of CEASE program, as a long-standing community-academic partnership, was critical to the overall successful implementation of this intervention. The engagement of all stakeholders in every step of this research promoted capacity-building of academic researchers and community leaders at every level. The shared decision-making process encouraged a feeling of ownership by all stakeholders that is a crucial element for sustainability. The use of feedback and the incorporation of lessons learned from each step of the process guided the development of the intervention in an iterative, progressive manner and was a unique strength of this study. The partnership was adept at balancing action with research with the overall mindset of doing research “with” the community and not “on” them.
A mixed method approach with triangulation was employed to improve the standard and quality of data. Examining the interventions using both quantitative and qualitative approaches provided ample depth about the outcomes. The strength of the CEASE partnership came from expertise in diverse fields and was valuable for addressing the limitations described at each stage of the interventions.
This study had a few limitations. Due to the small sample size, some of the differences were not statistically significant. We however included a qualitative component to provide a more in-depth understanding of the study results. In addition, some mentors who received the training were not able to continue for personal reasons. Several mentees were therefore reassigned to other mentors to ensure continuity. Other limitations included a quasi-experimental design and lack of randomization. We were however able to follow up smokers who did not enroll into the program as a control group. The control and intervention groups may not have been completely comparable as seen by the differences in willingness to participate in the program which was an enrollment criteria. We, however, included a variable in the baseline survey to measure the respondents' intention to quit based on Prochaska's stages of change theory (66). This variable which helped us determine the level of motivation to quit smoking, was not significantly different for the two groups at baseline. We also offered CO monitoring as a motivational tool to all respondents of the survey at baseline before they decided whether or not to enroll. Given all these limitations and given our design, we cannot attribute all positive results to the intervention without any consideration that there might be other causes for the findings. For example there were some baseline differences between those who took part in the intervention and those who didn't. Similarly, some people who didn't receive the intervention quit smoking, and we cannot attribute this finding to contamination.
Despite the limitations of this pilot study, our mixed-methods results introduce peer-mentoring smoking cessation interventions as an innovative strategy for high-need settings such as predominantly African American low-income public housing residential complexes. Although more research is needed, such an approach may create an important opportunity for quitting smoking through training local peers and empowering public housing residents so that they can get more involved in serving their own communities. Our intervention was successful because our tobacco cessation curriculum was culturally adapted to this setting. Similar cultural adaptation is needed for other diverse groups and vulnerable populations. For example, young people, who are targeted by tobacco companies, could benefit from an adapted version of this intervention (i.e., a web version of the program). Implementation and evaluation projects should test the effects of our peer mentoring model in other similar settings.
Data availability statement
Due to privacy and ethical concerns, neither the data nor the source of the data can be made available.
Ethics statement
This study involving human participants was reviewed and approved by Morgan State University Institutional Review Board. The participants provided their written informed consent to participate in this study.
Author contributions
Material preparation, data collection, and analysis were performed by JA, HT, EG, and OS. The first draft of the manuscript was written by JA and SA. PS reviewed and revised following versions of the manuscript. All other authors reviewed and commented on previous versions of the manuscript. All authors contributed to the study conception and design and read and approved the final manuscript.
Funding
This research received support from the National Institute of General Medical Sciences of the National Institutes of Health under Award Number RL5GM118972.
Acknowledgments
This study arises from the ASCEND (A Student-Centered, Entrepreneurship Development) CBPR small grant program. The small grant program was developed to address the health disparities experienced by vulnerable and underserved populations residing in underserved Baltimore communities. The overarching goals and methods of ASCEND have been described in another publication (67). The management of Monument East apartments was very supportive and instrumental to the implementation of this project. We also acknowledge Dr. Anne Marie O'Keefe for taking time to review and edit the manuscript and for her continued support for the project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
1. Centers for Disease Control and Prevention [CDC]. Current Cigarette Smoking Among Adults in the United States. Centers for Disease Control and Prevention. Available online at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm (accessed July 08, 2021).
2. Baltimore City Health Department [BCHD]. Stats and Data Baltimore City Health Department. (2014). Available online at: https://health.baltimorecity.gov/node/23 (accessed October 16, 2017).
3. Maryland Department of Health and Mental Hygiene [DHMH]. Monitoring Changing Tobacco Use Behaviors: 2000-2014. Available online at: https://phpa.health.maryland.gov/ohpetup/Documents/Maryland%20Tobacco%20Use%20Behaviors%20Summary%20Report%202000-2014.%20October%202016.pdf (accessed October 16, 2017).
4. Courtney RJ, Naicker S, Shakeshaft A, Clare P, Martire KA, Mattick RP. Smoking cessation among low-socioeconomic status and disadvantaged population groups: a systematic review of research output. Int J Environ Res Public Health. (2015) 12:6403–22. doi: 10.3390/ijerph120606403
5. Fenelon A, Mayne P, Simon AE, Rossen LM, Helms V, Lloyd P, et al. Housing assistance programs and adult health in the United States. Am J Public Health. (2017) 107:571–8. doi: 10.2105/AJPH.2016.303649
6. Howell E, Harris LE, Popkin SJ. The health status of HOPE VI public housing residents. J Health Care Poor Underserved. (2005) 16:273–85. doi: 10.1353/hpu.2005.0036
7. Helms VE, King BA, Ashley PJ. Cigarette smoking and adverse health outcomes among adults receiving federal housing assistance. Prev Med. (2017) 99:171–7. doi: 10.1016/j.ypmed.2017.02.001
8. Levy DE, Adams IF, Adamkiewicz G. Delivering on the promise of smoke-free public housing. Am J Public Health. (2017) 107:380–3. doi: 10.2105/AJPH.2016.303606
9. Farley SM, Waddell EN, Coady MH, Grimshaw V, Wright DA, Mandel-Ricci J, et al. Correlates of smoke-free housing policies and interest in implementing policies among multiunit housing owners in New York City. J Urban Health Bull N Y Acad Med. (2015) 92:291–303. doi: 10.1007/s11524-014-9934-z
10. Levy DE, Adamkiewicz G, Rigotti NA, Fang SC, Winickoff JP. Changes in tobacco smoke exposure following the institution of a smoke-free policy in the Boston housing authority. PLoS ONE. (2015) 10:e0137740. doi: 10.1371/journal.pone.0137740
11. Snyder K, Vick JH, King BA. Smoke-free multiunit housing: a review of the scientific literature. Tob Control. (2016) 25:9–20. doi: 10.1136/tobaccocontrol-2014-051849
12. Andrews JO, Bentley G, Crawford S, Pretlow L, Tingen MS. Using community-based participatory research to develop a culturally sensitive smoking cessation intervention with public housing neighborhoods. Ethn Dis. (2007) 17:331–7.
13. Andrews JO, Tingen MS, Jarriel SC, Caleb M, Simmons A, Brunson J, et al. Application of a CBPR framework to inform a multi-level tobacco cessation intervention in public housing neighborhoods. Am J Community Psychol. (2012) 50:129–40. doi: 10.1007/s10464-011-9482-6
14. Rhodes SD, Kelley C, Simán F, Cashman R, Alonzo J, McGuire J, et al. Using community-based participatory research (CBPR) to develop a community-level HIV prevention intervention for latinas: a local response to a global challenge. Womens Health Issues. (2012) 22:e293–301. doi: 10.1016/j.whi.2012.02.002
15. Rhodes SD, Duck S, Alonzo J, Daniel-Ulloa J, Aronson RE. Using community-based participatory research to prevent hiv disparities: assumptions and opportunities identified by the latino partnership. J Acquir Immune Defic Syndr. (2013) 63:S32–5. doi: 10.1097/QAI.0b013e3182920015
16. Sheikhattari P, Apata J, Kamangar F, Schutzman C, O'Keefe A, Buccheri J, et al. Examining smoking cessation in a community-based versus clinic-based intervention using community-based participatory research. J Community Health. (2016) 1–7. doi: 10.1007/s10900-016-0264-9
17. Albrecht S, Payne L, Stone CA, Reynolds MD. A Preliminary study of the use of peer support in smoking cessation programs for pregnant adolescents. J Am Acad Nurse Pract. (1998) 10:119–25. doi: 10.1111/j.1745-7599.1998.tb01205.x
18. Day C, Harwood J, Kendall N, Nicoll J. Impact of a peer-led, community-based parenting programme delivered at a national scale: an uncontrolled cohort design with benchmarking. BMC Public Health. (2022) 22:1377. doi: 10.1186/s12889-022-13691-y
19. Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions. BMJ. (2004) 328:1166. doi: 10.1136/bmj.328.7449.1166
20. Webel AR, Okonsky J, Trompeta J, Holzemer WL. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. Am J Public Health. (2010) 100:247–53. doi: 10.2105/AJPH.2008.149419
21. Malchodi CS, Oncken C, Dornelas EA, Caramanica L, Gregonis E, Curry SL. The effects of peer counseling on smoking cessation and reduction. Obstet Gynecol. (2003) 101:504. doi: 10.1097/00006250-200303000-00015
22. McKay CE, Dickerson F. Peer supports for tobacco cessation for adults with serious mental illness: a review of the literature. J Dual Diagn. (2012) 8:104–12. doi: 10.1080/15504263.2012.670847
23. Ford P, Clifford A, Gussy K, Gartner C. A systematic review of peer-support programs for smoking cessation in disadvantaged groups. Int J Environ Res Public Health. (2013) 10:5507–22. doi: 10.3390/ijerph10115507
24. Bowen DJ, et al. How we design feasibility studies. Am J Prev Med. (2009) 36:452–7. doi: 10.1016/j.amepre.2009.02.002
25. Apata J, Sheikhattari P, O'Keefe AM, Kamangar F, Freedman N. Examining Factors Related to Smoking Cessation in Underserved Populations: Lessons Learned from the CEASE Initiative. (2018). Available online at: https://search.proquest.com/docview/2198247858/abstract/67A4D997D76140F0PQ/1 (accessed October 29, 2018).
26. Zimmerman EB. Researching Health Together:Engaging Patients and Stakeholders, From Topic Identifiction to Policy Change. Thousand Oaks, CA: SAGE Publications, Inc. (2020).
27. Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the Functional Components of Social Support. In: Social Support: Theory, Research and Applications. Dordrecht: Springer. (1985) p. 73–94. doi: 10.1007/978-94-009-5115-0_5
28. Mark C, Paul N. Predicting Health Behaviour. New York: McGraw-Hill Education (UK). (2005). Available online at: https://books.google.com/books?hl=en&lr=&id=oeFDBgAAQBAJ&oi=fnd&pg=PP1&dq=predicting+health+behavior+mark+and+paul&ots=qMf3vW0zr2&sig=OFTTooO1XKYPawoNGqNDhRJy_sw#v=onepage&q=predicting%20health%20behavior%20mark%20and%20paul&f=false.
29. Leahy-Warren P. Social support theory. In: Theories Guiding Nursing Research and Practice: Making Nursing Knowledge Development Explicit. New York, NY, US: Springer Publishing Company, (2014) p. 85–101. doi: 10.1891/9780826164056.0006
30. Fagerström K Determinants Determinants of tobacco use and renaming the FTND to the fagerström test for cigarette dependence. Nicotine Tob Res. (2012) 14:75–78. doi: 10.1093/ntr/ntr137
31. Fagerstrom KO, Heatherton TF, Kozlowski LT. Nicotine addiction and its assessment. Ear Nose Throat J. (1990) 69:763–5.
32. Fagerstrom K-O, Schneider NG. Measuring nicotine dependence: a review of the fagerstrom tolerance questionnaire. J Behav Med. (1989) 12:159–82. doi: 10.1007/BF00846549
33. Deveci SE, Deveci F, Açik Y, Ozan AT. The measurement of exhaled carbon monoxide in healthy smokers and non-smokers. Respir Med. (2004) 98-551–6. doi: 10.1016/j.rmed.2003.11.018
34. Ryter SW, Choi AMK. Carbon monoxide in exhaled breath testing and therapeutics. J Breath Res. (2013) 7:017111. doi: 10.1088/1752-7155/7/1/017111
35. The Epidata Association. EpiData Software. Odense, Denmark: EpiData Association. (2008). Available online at: http://epidata.dk/.
36. StataCorp. Stata Statistical Software:Release 14. StataCorp LP. College Station, TX: StataCorp LP. (2015).
37. Blankers M, Smit ES P. van der Pol, de Vries HC. The missing=smoking assumption: a fallacy in internet-based smoking cessation trials? Nicotine Tob Res. (2016) 18:25–33. doi: 10.1093/ntr/ntv055
38. Barnes SA, Larsen MD, Schroeder D, Hanson A, Decker PA. Missing data assumptions and methods in a smoking cessation study. Addiction. (2010) 105:431–7. doi: 10.1111/j.1360-0443.2009.02809.x
39. Tickle-Degnen L, Nuts and bolts of conducting feasibility studies. Am J Occup Ther. (2013) 67:171–6. doi: 10.5014/ajot.2013.006270
40. Wuest J, Grey MM, Dube N, Hodgins MJ, Malcom J, Majerovich JA, et al. The process and challenges of feasibility studies conducted in partnership with stakeholders: a health intervention for women survivors of intimate partner violence. Res Nurs Health. (2015) 38:82–96. doi: 10.1002/nur.21636
41. vanManen MA. Uniqueness and novelty in phenomenological inquiry. Qual Inq. (2020) 26:486–490. doi: 10.1177/1077800419829788
42. Fleury J, Keller C, Perez A. Social support theoretical perspective. Geriatr Nurs N NY. (2009) 30:11–4. doi: 10.1016/j.gerinurse.2009.02.004
43. Dickerson F, Savage CLG, Schweinfurth LAB, Goldberg RW, Bennett M, Dixon L, et al. The experience of peer mentors in an intervention to promote smoking cessation in persons with psychiatric illness. Community Ment Health J. (2016) 52:416–23. doi: 10.1007/s10597-015-9967-0
44. Dickerson FB, Savage CLG, Schweinfurth LAB, Medoff DR, Goldberg RW, Bennett M, et al. The use of peer mentors to enhance a smoking cessation intervention for persons with serious mental illnesses. Psychiatr Rehabil J. (2016) 39:5–13. doi: 10.1037/prj0000161
45. Torgerson DJ Contamination in trials: is cluster randomisation the answer?. BMJ. (2001) 322:355–357. doi: 10.1136/bmj.322.7282.355
46. Burling TA, Seidner Burling A, Latini D. A controlled smoking cessation trial for substance-dependent inpatients. J Consult Clin Psychol. (2001) 69:295–304. doi: 10.1037/0022-006X.69.2.295
47. Reid JL, Hammond D, Boudreau C, Fong GT, Siahpush M. Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: Findings from the International Tobacco Control Four Country Survey. Nicotine Tob Res. (2010) 12:S20–33. doi: 10.1093/ntr/ntq051
48. Wallen J, Randolph S, Carter-Pokras O, Feldman R, Kanamori-Nishimura M. Engaging african americans in smoking cessation programs. Am J Health Educ. (2014) 3:151–7. doi: 10.1080/19325037.2014.893850
49. Moore D, Aveyard P, Connock M, Wang D, Fry-Smith A, Barton P. Effectiveness safety of nicotine replacement therapy assisted reduction to stop smoking: systematic review and meta-analysis. BMJ. (2009) 338:b1024. doi: 10.1136/bmj.b1024
50. Tang JL, Law M. Wald N. How effective is nicotine replacement therapy in helping people to stop smoking? BMJ. (1994) 308:21–6. doi: 10.1136/bmj.308.6920.21
51. Krukowski RA, Solomon LJ, Naud S. Triggers of heavier and lighter cigarette smoking in college students. J Behav Med. (2005) 28:335–45. doi: 10.1007/s10865-005-9003-x
52. Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. (2014) 4:e006414. doi: 10.1136/bmjopen-2014-006414
53. Vangeli E, West R. Sociodemographic differences in triggers to quit smoking: findings from a national survey. Tob Control. (2008) 17:410–5. doi: 10.1136/tc.2008.025650
54. Reid HH, Ledgerwood DM. Depressive symptoms affect changes in nicotine withdrawal and smoking urges throughout smoking cessation treatment: preliminary results. Addict Res Theory. (2016) 24:48–53. doi: 10.3109/16066359.2015.1060967
55. Townsend J, Wilkes H, Haines A, Jarvis M. Adolescent smokers seen in general practice: health, lifestyle, physical measurements, and response to antismoking advice. BMJ. (1991) 303:947–50. doi: 10.1136/bmj.303.6808.947
56. Vidrine JI, Businelle MS, Reitzel LR, Cao Y, Cinciripini PM, Marcus MT, et al. Coping mediates the association of mindfulness with psychological stress, affect, and depression among smokers preparing to quit. Mindfulness. (2015) 6:433–43. doi: 10.1007/s12671-014-0276-4
57. Levy DE, Friend K, Polishchuk E. Effect of clean indoor air laws on smokers: the clean air module of the SimSmoke computer simulation model. Tob Control. (2001) 10:345–51. doi: 10.1136/tc.10.4.345
58. Geller AC, Rees VW, Brooks DR. The proposal for Smoke-Free public housing: benefits, challenges, and opportunities for 2 million residents. JAMA. (2016) 315:1105–6. doi: 10.1001/jama.2016.1380
59. MacNaughton P, Adamkiewicz G, Arku RE, Vallarino J, Levy DE. The impact of a smoke-free policy on environmental tobacco smoke exposure in public housing developments. Sci Total Environ. (2016) 557–558:676–80. doi: 10.1016/j.scitotenv.2016.03.110
60. Debchoudhury I, Farley SM. Implementing Smoke-free housing policies among multiunit housing owners in New York City between 2012 and (2015). Tob Use Insights. (2019) 12:1179173X19859355. doi: 10.1177/1179173X19859355
61. Anthony J, Goldman R, Rees VW, Frounfelker RL, Davine J, Keske RR, et al. Qualitative assessment of smoke-free policy implementation in low-income housing: enhancing resident compliance. Am J Health Promot. (2019) 33:107–17. doi: 10.1177/0890117118776090
62. King BA. National and state cost savings associated with prohibiting smoking in subsidized and public housing in the United States. Prev Chronic Dis. (2014) 11. doi: 10.5888/pcd11.140222
63. Geller AC, Borrelli B, Davine JA, et al. Factors associated with recent use of nicotine replacement therapy among multiethnic smokers residing in public housing. J Smok Cessat. (2018) 13:162–70. doi: 10.1017/jsc.2017.21
64. Bonevski B, Randell M, Paul C, Chapman K, Twyman L, Bryant J, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol. (2014) 14:42. doi: 10.1186/1471-2288-14-42
65. Bower C. Attempts to Change Public Housing Residents' Behaviors Aspirations - A HOPE VI Neighborhood Run by a Phantom Homeowners' Association. (2016). Available online at: https://papers.ssrn.com/abstract=2832940 (accessed: February 19, 2018). doi: 10.2139/ssrn.2832940
66. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot AJHP. (1997) 12:38–48. doi: 10.4278/0890-1171-12.1.38
Keywords: smoking cessation, peer mentoring, community-based, health disparities, behavioral intervention
Citation: Apata J, Goldman E, Taraji H, Samagbeyi O, Assari S and Sheikhattari P (2023) Peer mentoring for smoking cessation in public housing: A mixed-methods study. Front. Public Health 10:1052313. doi: 10.3389/fpubh.2022.1052313
Received: 23 September 2022; Accepted: 07 December 2022;
Published: 05 January 2023.
Edited by:
Erin Rogers, New York University, United StatesReviewed by:
Emily Peckham, University of York, United KingdomNan Jiang, New York University, United States
Copyright © 2023 Apata, Goldman, Taraji, Samagbeyi, Assari and Sheikhattari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jummai Apata,  anVtbWFpLmFwYXRhMThAYWx1bW5pLm1vcmdhbi5lZHU=
anVtbWFpLmFwYXRhMThAYWx1bW5pLm1vcmdhbi5lZHU=
†Present address: Erica Goldman, Stepping Forward Training and Consulting LLC, Nottingham, MD, United States
 Jummai Apata
Jummai Apata Erica Goldman
Erica Goldman Hamideh Taraji
Hamideh Taraji Oluwatobi Samagbeyi
Oluwatobi Samagbeyi Shervin Assari
Shervin Assari Payam Sheikhattari
Payam Sheikhattari