- 1Faculty of Medicine, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 2JC School of Public Health and Primary Care, Centre for Health Systems and Policy Research, The Chinese University of Hong Kong, Hong Kong, Hong Kong SAR, China
Introduction: Health literacy (HL) refers to an individual's ability to process and use health information to make health-related decisions. However, previous HL scales did not fully cover all aspects of this concept. This study aimed to develop a comprehensive Hong Kong HL scale (HLS-HK) and evaluate its psychometric properties among Chinese adults.
Methods: A scale of 31-item covering Nutbeam's framework, namely functional and interactive HL (FHL and IHL), and critical HL (CHL) within three subdomains: critical appraisal of information, understanding of social determinants of health, and actions to address social determinants of health, was developed based on previous literature review and Delphi survey. Cognitive interviews were performed to examine all items' face validity in terms of three aspects: comprehensiveness, clarity, and acceptability. A cross-sectional survey was conducted to investigate the scale's psychometric properties, including its internal consistency reliability, factorial structure validity, convergent validity, and predictive validity.
Results: Nine interviewees participated in the cognitive interviews in October 2021. Based on the input from respondents, two items were deleted, two items were combined, and several items' wording was revised. The other items were clear and readable. Finally, 28 items remained. A total of 433 adults completed the questionnaire survey between December 2021 and February 2022. After excluding one item with low inter-item correlations, the scale's internal consistency reliability was acceptable, with a Cronbach's alpha of 0.89. Exploratory factor analysis produced a five-factor model, as shown in the original theoretical framework. These factors accounted for 53% of the total variance. Confirmatory factor analysis confirmed that the fit indices for this model were acceptable (comparative fit index = 0.91, root mean square error of approximation = 0.06, and root mean square residual = 0.06). The scale is also significantly correlated with theoretically selected variables, including education and self-rated health.
Conclusion: The HLS-HK is a valid and reliable tool for evaluating HL. Compared with existing tools, this scale extended the operationalization of FHL, IHL, and CHL and fully operationalized the CHL via three subdomains. It can be used to understand the difficulties and barriers that people may encounter when they use health-related information and services.
Introduction
Health literacy (HL) is crucial to empower individuals to make informed health decisions. It is usually described as one individual's ability to process and use health information to promote health (1). Previous studies suggested that people with limited HL skills tend to have poorer health outcomes (2–4), less utilization of preventive health services (5), higher hospitalizations (6), and healthcare costs (7, 8). One survey in eight European countries reported that at least 1 out of 10 participants had inadequate HL skills (9). There are challenges in embedding HL-related skills into effective disease prevention and health self-management. Assessing HL at a population level provides great potential to recognize populations most in need of support, deliver tailored interventions, and achieve better health outcomes in communities.
The measurement instrument is essential to understand people's HL levels. More than one hundred HL measurements have been developed during the last decades (10). The early HL measurement tools were criticized for their narrow focus on the capacity to read and understand written health information in a medical context (11–13). For example, the most commonly used HL tools, including the Test of Functional Health Literacy in Adults (TOFHLA) (11) and the Newest Vital Sign (NVS) (12), solely assess the reading ability of health-related materials through medical term recognition and numeracy test. Along with advancements in technology and the complex demands of health in modern society, scholars have realized that a broader set of competence is needed to access and use health-related information in everyday life. Align with this, several HL tools (14–17) expended to measure information seeking, communication skills, decision making, and critical thinking. However, recent systematic reviews highlighted that there is still no widely adopted measurement tool that could thoroughly reflect the current understanding of HL (18–22). Taking the lately dominant scales as examples, the Health Literacy Questionnaire (HLQ) (15) and the European Health Literacy Survey Questionnaire (HLS-EU) (23) did not include the skills necessary to address health concerns through civic engagement, which are essential HL skills to understand the social constructal cause of health-related issues and promote individual and community health. The ongoing evolution of HL measurement tools indicated the complexity of this concept and a demand for a comprehensive and reliable measure in this research field.
The construct underlying the measure is one of the most critical aspects of choosing and developing an appropriate measure. Nutbeam's framework of HL is widely cited as the conceptual basis and is seen by many HL researchers as useful in analyzing HL skills required in various contexts (24). This framework divides the primary skills of HL into three levels: functional health literacy (FHL), referring to individuals' basic literacy and numeracy skills for them to function effectively in their daily life; interactive health literacy (IHL), referring to individuals' cognitive and social skills to extract information from all kinds of forms of communication and to use this information for achieving better health outcomes; and critical health literacy (CHL), that is, individuals' higher level of cognitive and social skills which can be applied to critically analyze information and to use this information to gain better control over life events that affect health. The integrated model of HL proposed by Sørensen et al. is another vital framework in this research area. It described the competencies needed to access, understand, judge, and apply health information across the domains of health care, disease prevention, and health promotion (25).
Nutbeam's model was selected as the theoretical basis for the study because of its multifaceted understanding of CHL. Applying CHL has never been more needed than in these days when people have greater access to information and are expected to be actively engaged in healthcare. Compared with Sørensen's framework, Nutbeam emphasized that CHL includes the ability to question information and the awareness of the social determinants of health and the actions to modify these determinants (24). This emphasis is more explicitly linked to the latest understanding of CHL, that is, a range of abilities to read health-related information in a critical, active, and reflective manner to achieve an in-depth understanding of the world and explore political and social change in daily life (26–29). Taking the current pandemic of COVID-19 as an example, individuals need to know how to critically assess information when they are overwhelmed by the abundance of information, as well as how to make informed decisions to sacrifice some part of one's benefits for the sake of public good when they are asked to take certain interventions (e.g., vaccination and quarantine) to control infection. Therefore, CHL is needed to be seen in relation to critical consciousness and social responsibilities in promoting community health (27).
However, current HL measures using Nutbeam's framework and targeting adults failed to capture the full breadth of the ideas embedded in CHL. Previous scales (14, 30–35) mainly included the ability to question information quality as the component of CHL. For example, the 14-items HL scale (HLS-14) (30), which is widely cited in this research area, adopted items to measure subjects' ability to judge the quality of the information in terms of its reliability, validity, credibility, and applicability. Other competencies involved in CHL, namely realizing social and structural factors influencing health and taking social responsibilities for public health, were rarely addressed, and their operationalizations are still in progress. Chinn and colleagues made efforts to cover all aspects of CHL. But they faced the challenges of building items to thoroughly assess understandings of and ability to act on social determinants of health. They simply adopted three items involved in the capabilities for community empowerment and social engagement for health to reflect these abilities (14). The above revealed that the operationalization of CHL remains underexplored and more discussion is needed to explicitly link the theory and measurement in this domain.
Additionally, there is no rigorously validated HL scale for the general population in Hong Kong. Although several studies explored HL in the local community, the scales they used were either disease-specific or population-specific (36–40) or directly translated from existing ones without psychometric testing (41, 42). Hong Kong is facing the challenges posed by the increasing disease burden from chronic diseases and has a dual-track healthcare system encompassing public and private sectors. This system has been criticized for the long waiting times in public hospitals and high healthcare costs in private hospitals (43, 44). Under such circumstances, patients with chronic diseases are expected to actively engage in self-management, which requires adequate HL skills. With this respect, one reliable and valid HL scale will be useful to identify the attributes and barriers related to HL.
With all these in mind, our goal was to develop a new Chinese Hong Kong version of HL scale (HLS-HK) based on Nutbeam's framework and evaluate its psychometric properties among Chinese adults. Given that the theory and measurements of HL are still in the exploratory stage, our work would be feedback loops to improve the underlying theory of HL. We also expect that the scale would provide regional-level information related to health competency and facilitate more efforts to understand HL skills and their impact on health outcomes in Hong Kong.
Methods
A four-stage research approach was adopted, including literature review, Delphi study, individual cognitive interview, and cross-sectional survey to develop and validate a comprehensive scale for HL. In the first stage, we conceptualized the framework of HLS-HK by conducting two scoping reviews (45, 46). In the next stage of the Delphi study (47), we deductively generated items based on the framework resulting from the first stage and invited stakeholders (i.e., healthcare providers and healthcare consumers) to assess the content validity of all draft items and provide additional items. The face validity accessed via individual cognitive interviews and psychometric analysis using a cross-section survey were reported in this paper.
Cognitive interview
The cognitive interviews were conducted to test the face validity of the 31 items derived from previous literature reviews and the Delphi survey. In the interviews, interviewees were first asked to complete the scale and then were invited to give feedback on all items' comprehensiveness, clarity, and acceptability. Participants were recruited through a convenience sampling strategy. The eligibilities of participants were as follow: (a) permanent Hong Kong citizen; (b) aged 18 and above; (c) understand Cantonese. To keep the recruitment costs low, we sought the participation of individuals working or visiting our school to participate in the interview. To achieve a representative sample, we selected interviewees by considering a balance of gender, age, educational attainment, and income. The sample size for cognitive interviews was set between 5 and 15 subjects (48). Participant recruitment stopped when data saturation reached (48, 49).
Cross-sectional validation survey
A psychometric evaluation was performed to examine the internal consistency, factorial structural validity, convergent validity, and predictive validity of the revised version of HLS-HK.
Participants
Participants were recruited from registrants of an internet research service company Qualtrics to complete an online survey. Quota sampling was used to match the distribution of participants by gender, age group, and living district (i.e., New Territories, Kowloon, Hong Kong Island) to the results of the 2020 Hong Kong census (50). Facing resource constraints and challenges to reach the fixed quotas, the flexibility on all quotas was ±5%. The recommendation for a sample size used to scale validation should be at least 10 participants per item of the scale (51, 52). Therefore, in the present study, the sample size should be over 310 (=31*10). To ensure sufficient evidence for the reliability and validity of the newly developed scale and also consider the budget, the sample size of our survey was expected to be 400 participants.
Measures
The questionnaire consisted of two parts: (1) health literacy assessment; (2) social demographic and health factors. It was built on Qualtrics survey software (version Dec 2021). All questions were designed to force response. We also set up one attention check question to maintain data quality by excluding respondents who were not paying close attention to survey questions.
Health literacy assessment
Participants' HL levels were measured using our newly developed scale HLS-HK and the 12-item short-form of the health literacy questionnaire (HL-SF12) (53). Regarding HLS-HK, items were rated on a 5-point Likert Scale, and the scores were summed. A sample item was “How often do you need help when you fill out medical forms?”. The item responses ranged from 1 = always to 5 = never. The HL-SF12 was developed based on Sørensen and colleagues' framework of HL (25). It is the short version of the HLS-EU (23) and has been validated in six Asia countries (54). Given the importance of Sørensen's framework in this research area, we used HL-SF12 as the reference scale. We contacted the authors of HL-SF12 and got their approval to use it in our study. In HL-SF12, the perceived difficulty of each health-related task was rated on 4-point Likert scales (ranging from 1 = very difficult to 4 = very easy). Example items included “On a scale from very easy to very difficult, how easy would you say it is to judge the advantages and disadvantages of different treatment options.”
Social demographic and health factors
The following social demographic characteristics were collected from the respondents: age, gender, district, education attainment, occupation, and monthly household income. Participants were also asked to self-report their health status and health behaviors. Health status was examined by participants' responses to the questions “In general, how would you rate your health” with five outcomes (1–5, ranging from “poor” to “excellent”). This question is often used to assess a person's overall wellbeing in terms of social, biological, and psychological health in epidemiological health field surveys (55, 56). Health behaviors were assessed by asking about participants' lifestyles related to smoking, physical activity, and alcohol use.
Data analysis
Descriptive statistics were used to summarize study participants' demographic information and other health-related variables. Continuous variables were shown as mean and standard deviation (SD), and categorical variables were presented as numbers and frequencies. The reliability and validity analyses were performed to examine the psychometric properties of the HLS-HK. Data were analyzed using the SPSS (version 23) and R software (“psych” and “lavaan” package). The statistical significance level was set at a p < 0.05.
Reliability analysis
In reliability analysis, we focused on the internal consistency of the scale and subscales by testing Cronbach's alpha values. An alpha coefficient of 0.70 or greater is considered acceptable for reliability (57). Furthermore, corrected item-total correlations were tested. Two levels of inter-item correlations were suggested as acceptable: 0.2 (58, 59) and 0.3 (60, 61). We used the more liberal level of ≥0.2 in this study in order not to exclude some items on which some participants got high scores while others got low scores due to the heterogeneity within social demographic and health factors among subjects.
Validity analysis
We used exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) to assess the construct validity of HLS-HK. The sample was randomly split into two independent subsets to undertake separate EFA and CFA analysis.
EFA was first performed to discover the common factor influencing a group of measured variables of HLS-HK. Before performing an EFA, we used Bartlett's Test of Sphericity and the Kaiser-Meyer-Olkin (KMO) test to evaluate whether the data was worth factor analysis. If the probability of Bartlett's Test of Sphericity is <0.05 or KMO is >0.7, we can move to the EFA (62). Next, EFA was performed using principal component analysis, oblimin rotation, and parallel analysis. The criterion for selecting the optimal number of factors is based on: eigenvalue >1 and scree test (57). It is recommended that the retain items have factor loading of 0.4 and above and without significant cross-loading onto other factors (i.e., those that load on over one factor were excluded) (57, 63, 64).
CFA was then performed using maximum likelihood estimation to validate the factor structure of the HLS-HK. In the present study, the following indices of model fitness were used: comparative fit index (CFI), root mean square error of approximation (RMSEA), and root mean square residual (SRMR). A CFI value ≥0.90 indicated an acceptable model fit; an RMSEA value ≤0.08 shows a good fit; and an SRMR value ≤0.08 can be considered a good fit, based on suggestions in previous literature (57, 65).
Bivariate analysis
We performed the bivariate analysis between the HLS-HK scores and HL-SF12 scores to examine the convergent validity using Pearson correlation coefficients. In the present study, HL-SF12 was considered as the reference. We expected the two scales produce similar results. Namely, a participant who got a high score of HLS-HK is likely to have a high score of HL-SF12. In addition, as both HLS-HK and HL-SF12 measured the main skills related to HL, all subscales from the two scales should be somewhat related.
Regarding predictive validity, we examine the relationship between HLS-HK and other theoretically selected variables (including age, education attainment, income, self-rated health status, and health behaviors) using the Mann-Whitney U test (two samples) or Kruskal-Wallis test (more than two samples). Given previous studies highlighted that people with low HL skills were likely to be older (66, 67), less educated (67, 68), with lower-income (68, 69), poorer self-rated health status (69, 70), and less healthy behaviors (70, 71), we hypothesized that HLS-HK levels were significantly correlated with the above variables.
Ethical consideration
The Survey and Behavioral Research Ethics Committee of the Chinese University of Hong Kong accessed the protocol of this study and approved the study (Reference No. SBRE-20-793). The protocol for this study conformed to the principles embodied in the Declaration of Helsinki.
Results
The results of the first two stages were published elsewhere (45–47) and briefly presented below. In the first stage, five content areas that we aimed to measure were identified, including FHL, IHL, and the following three subdomains of CHL: CHL-1: “critical appraisal of information” means an individual's ability to evaluate the quality of information; CHL-2: “understanding of social determinants of health” coveys an individual's understanding of the social structural factors that influence health outcomes; CHL-3: “actions to address social determinants of health” focuses on an individual's competency to translate knowledge into action to address the modifiable determinants of health (45, 46). In the second stage, the Delphi study was completed (47). We generated the first draft of the HLS-HK consisting of 34 items. A diverse panel of professionals (n = 12) and laypeople (n = 12) rated the relevance of all 34 items. The consensus, which was predefined as ≥70% of participants agreeing that the individual item is relevant in Round 3, was reached for 31 items with excellent content validity. This HLS-HK with 31 items was used to test its face validity in cognitive interviews.
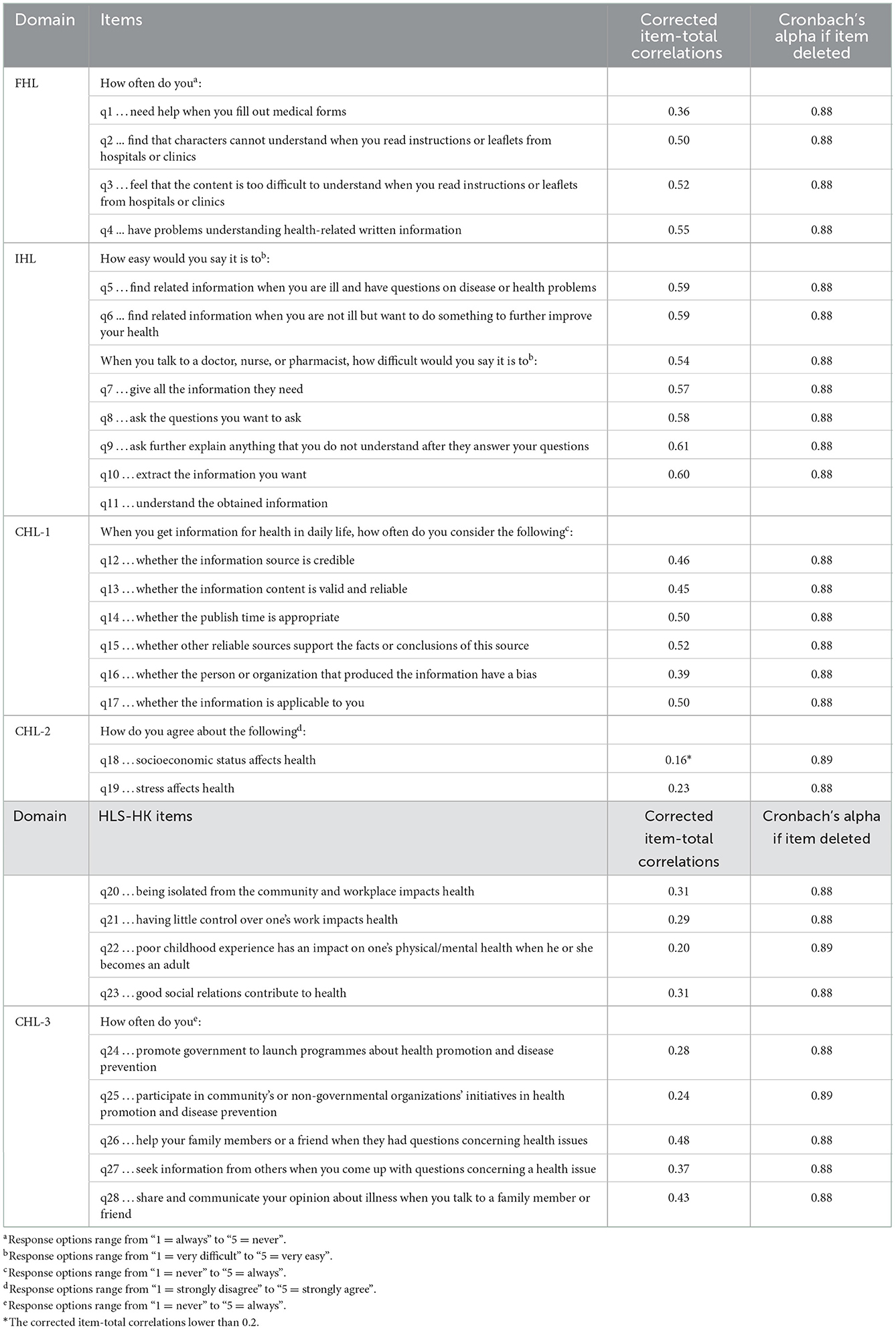
Cognitive interviews
Data saturation was achieved after nine interviews in October 2021. Table 1 presents the social demographic characteristics of the participants. Based on the input from interviewees, we deleted one item in FHL and one item in CHL-2, combined two items in CHL-3, and made a minor revision on several items' wording to make the scale concise. The other items were comprehensive, clear, and acceptable. Detailed results of cognitive interviews are presented in Appendix 1. Finally, a total of 28 items remained (Table 2). The revised version of HLS-HK within 28 items was adopted to test its psychometric properties in the following cross-sectional survey.
Cross-sectional validation survey
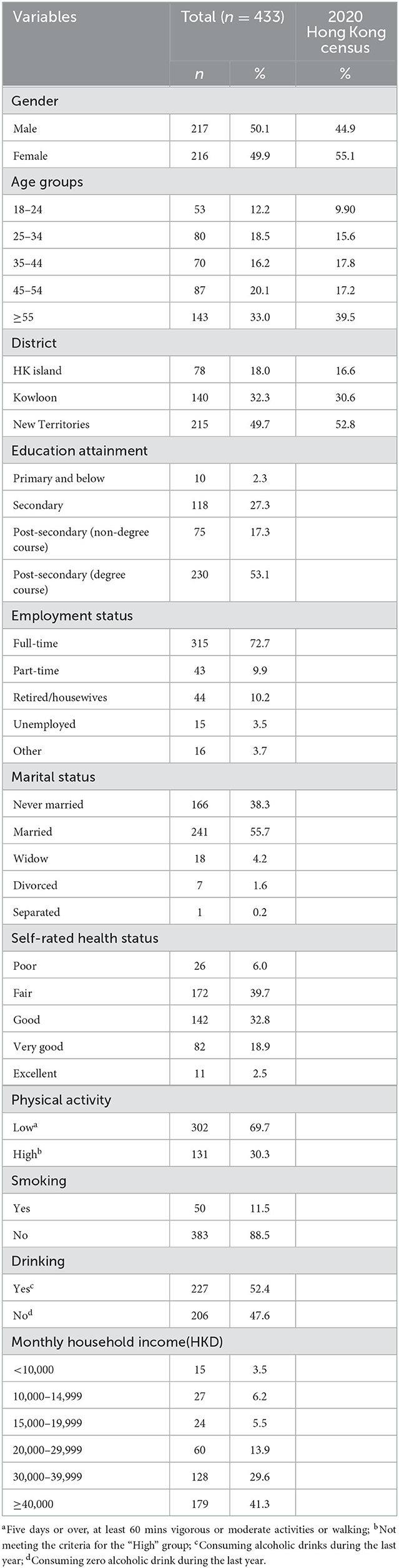
Social-demographic and health-related characteristics
The questionnaire survey was performed from December 2021 to February 2022. A total of 433 valid responses were collected after excluding those with data entry errors and speeders (i.e., respondents who completed the survey much more rapidly compared to others). In this study, we defined the cut-off point of speeders' completion time according to a soft launch of the survey (n = 40). In the soft launch, the median time to completion is 7.8 min, and we added half of the median completion time (i.e., 4 min) as the speeding check. The participants' social-demographic characteristics are displayed in Table 3.
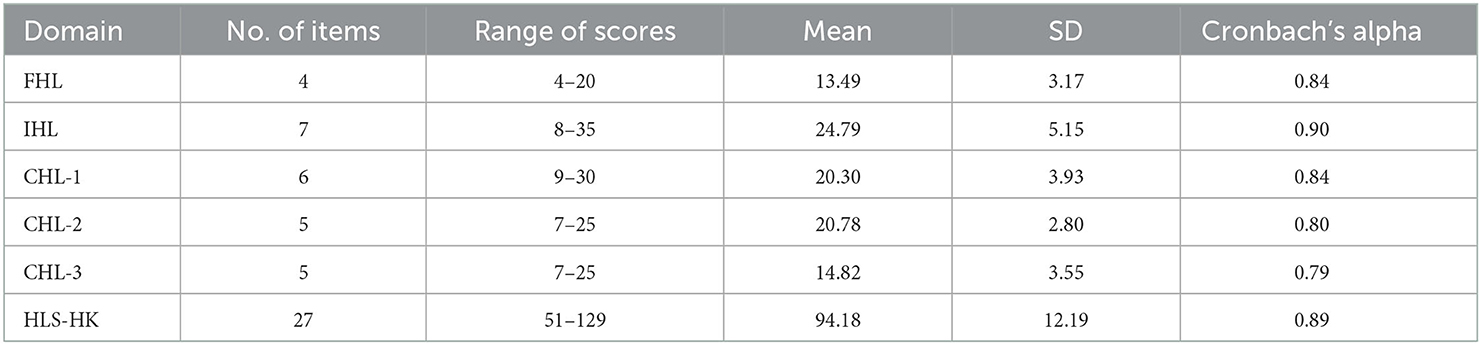
Reliability
According to the corrected item-total correlations (see Table 2), one item with low inter-item correlations (i.e., q18, item-total correlation < 0.2) was deleted. Table 4 summarizes the means, SD, and internal consistency for the scale and subscales without q18. Cronbach's alpha of the total score scale was 0.89, which is satisfactory. The Cronbach's alpha of the subscales ranged from 0.79 to 0.90. The internal consistencies of all subscales are satisfactory. Finally, the scale was composed of 27 items.
Validity
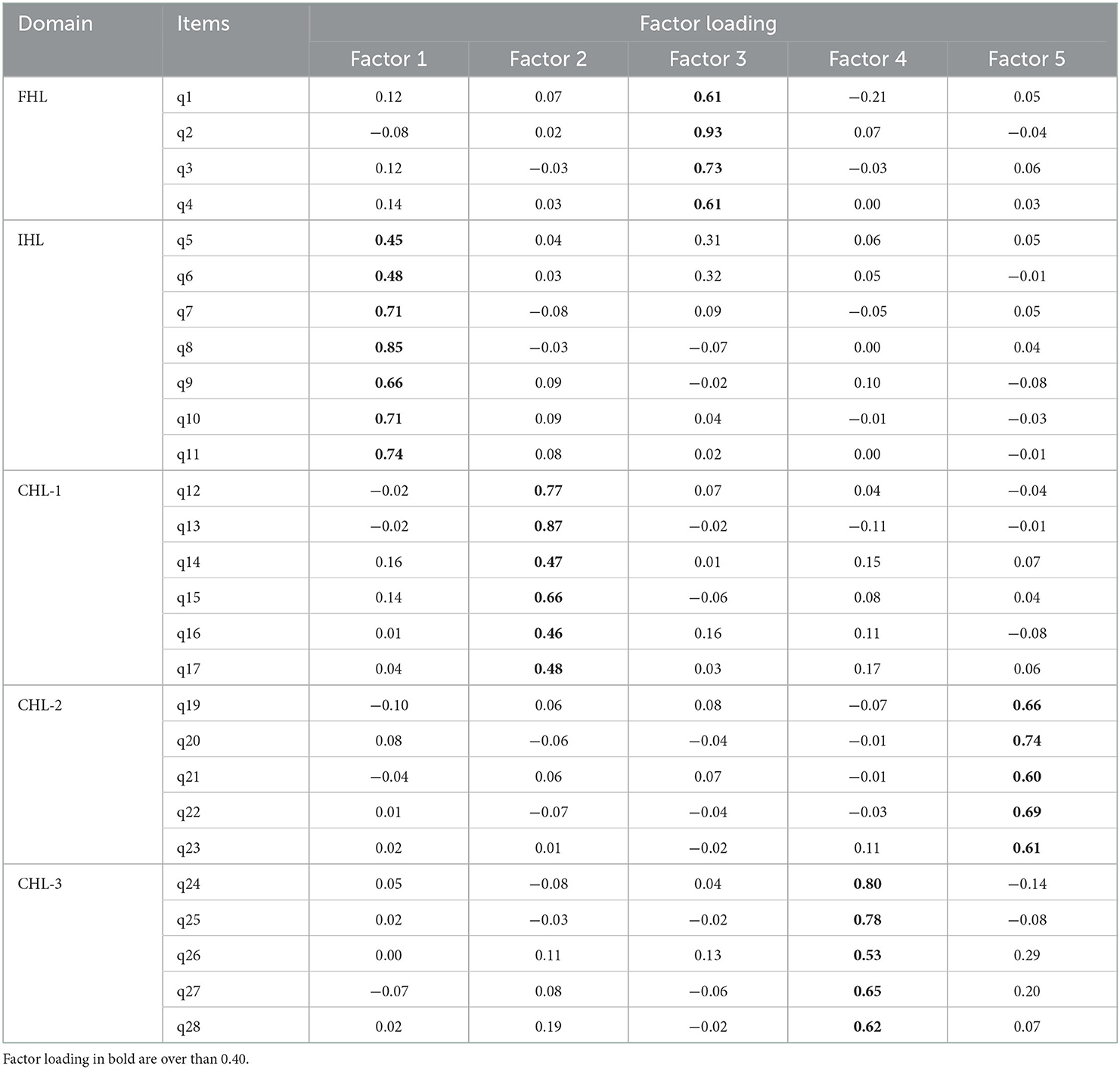
The dataset was randomly split into two subsets: for the EFA (n = 216), and the other for the CFA (n = 217). The sample size for each subsample satisfied the requirement for the sample size, which is larger than 5 times the number of variables for EFA (72), and at least 200 cases for CFA (73).
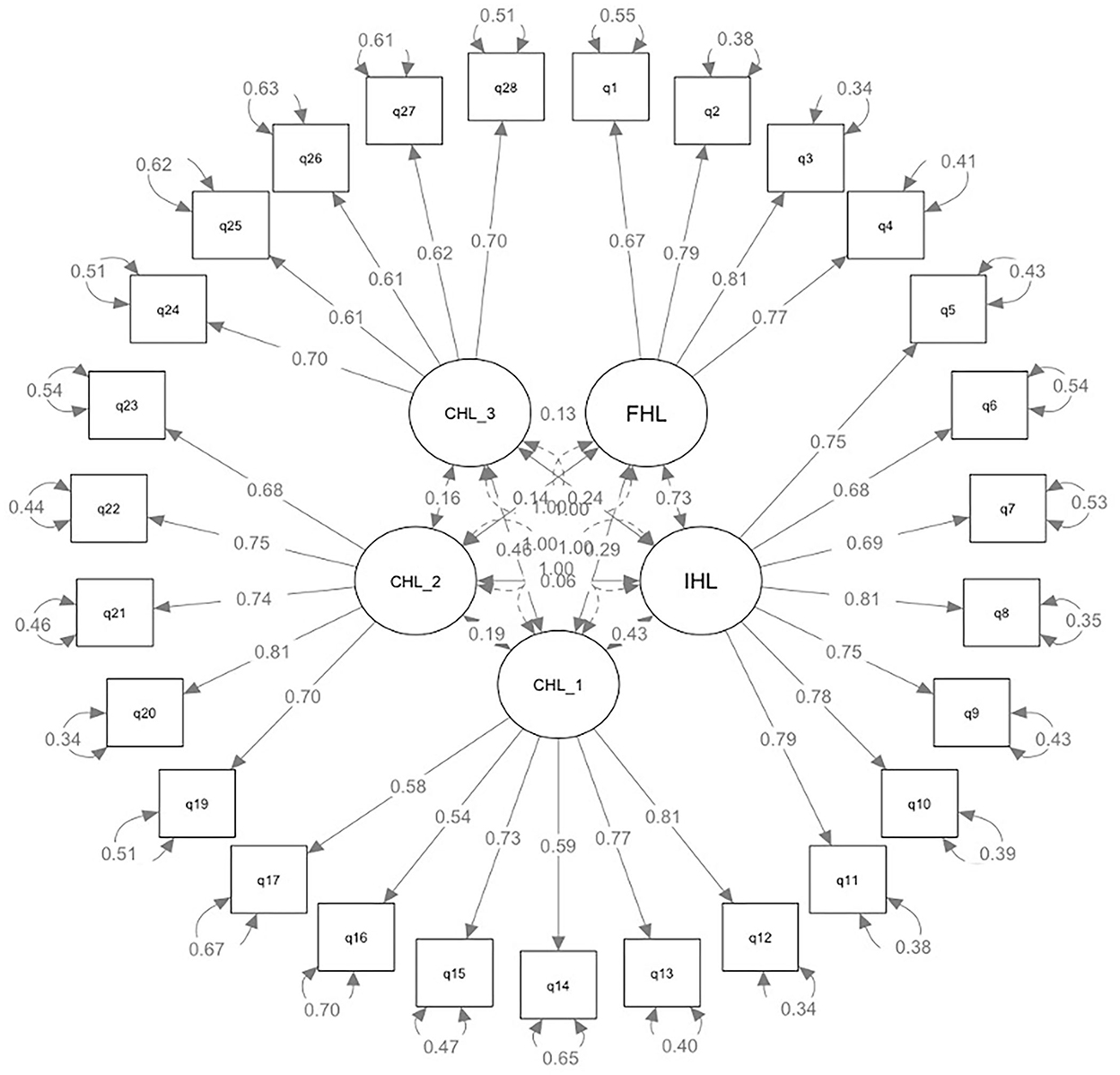
The KMO test showed a score of 0.86, which is above the required 0.70 for conducting EFA. Bartlett's test of sphericity was significant (chi-square = 2,772.356, p < 0.000). Therefore, our dataset is suitable for EFA. Regarding the results of EFA, the parallel analysis and scree plot examination suggested five factors with eigenvalues (7.36, 3.15, 2.78, 1.84, and 1.39, respectively) >1, accounting for 53% of the variance (14, 10, 10, 10, and 9%, respectively). Table 5 presents the factor structure of HLS-HK. The four items of FHL all loaded onto the third factor, and seven items of IHL loaded on the first factor. Among the items of CHL, six items of CHL-1 loaded on the second and five items of CHL-2 loaded on the fifth factor, and five items of CHL-3 loaded on the fourth factor. The CFA analysis revealed an acceptable fit of the five-factor model (see Figure 1), with a CFI = 0.91, SRMR =0.06, and RMSEA = 0.06.
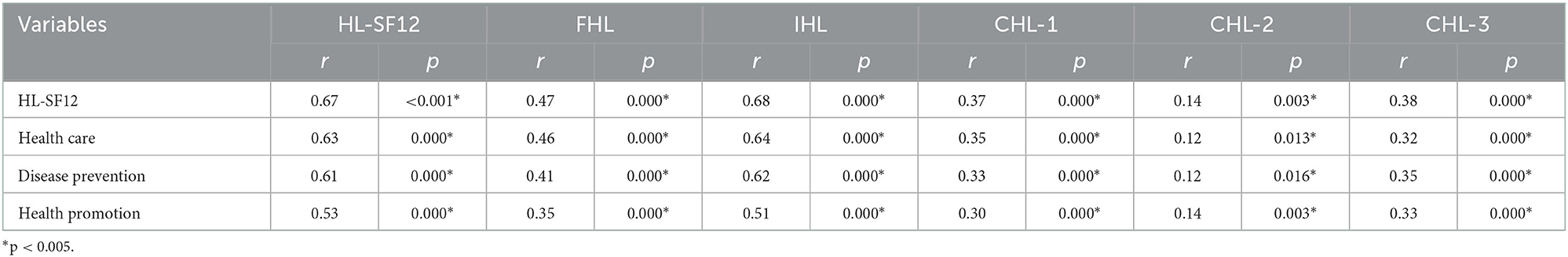
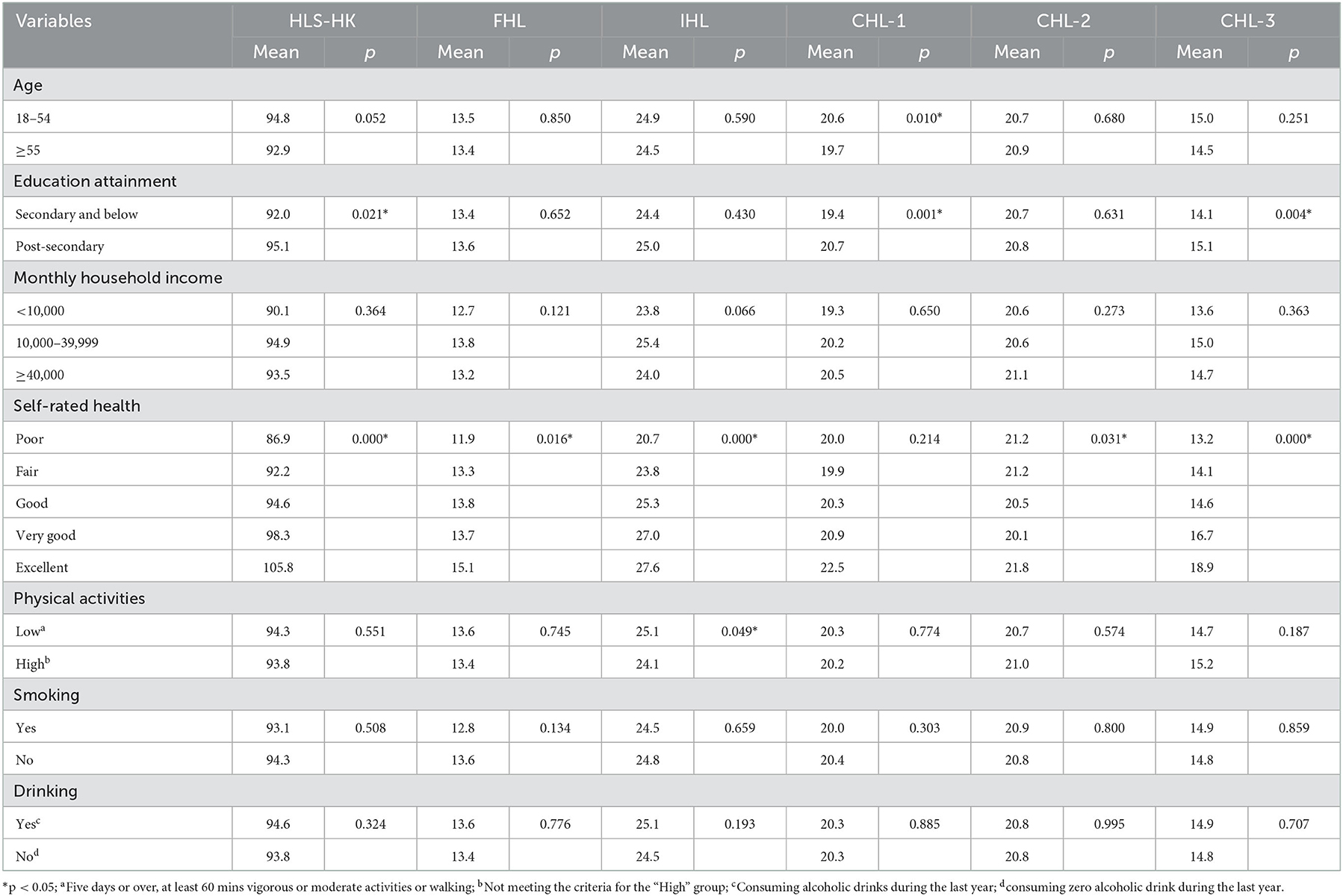
Bivariate analysis
The bivariate analysis showed a strong correlation between the HLS-HK and the HL-SF12 (r = 0.67, p < 0.001). All subscales of the two scales were significantly associated with each other (Table 6). Compared with FHL (r: 0.35–0.46, p = 0.000) and IHL (r: 0.51–0.64, p = 0.000), the three subdomains of CHL (r: 0.12–0.35, p = 0.000) had lower correlations with the subscales of HL-SF12. The scores on the HLS-HK were significantly associated with education level (H = 7.292, p < 0.05), as well as self-rated health status (H = 32.292, p < 0.001). However, there was no association between HLS-HK scores and age, income, and health behaviors (Table 7). We further examined the association between these selected variables and scores on the subscales of HLS-HK. There were statistically significant differences in physical activity groups' scores of IHL and age groups' scores of CHL-1 (Table 7).
Discussion
We proposed a scale within 27 items encompassing a range of HL competencies and addressed the shortage of HL measurement in Hong Kong. In the scale development process, we generated the original items by systematically searching the published literature relevant to the construct of HL to cover its full breadth and depth. We invited healthcare users and providers to examine the newly developed scale's content validity and face validation. The scales' two novel aspects related to Nutbeam's framework are discussed in the below section.
Scale novelty
First, compared with previous scales (14, 30–35), this scale fully operationalized the three domains identified by Nutbeam. In the domain of FHL, we formulated five items to examine subjects' abilities to read and understand health-related information in clinical and non-clinical settings. To measure IHL, seven items were generated to examine the abilities that people need to gain health-related information in daily life as well as healthcare consulting. Regarding CHL, this scale is more explicitly linked to the latest understanding of this domain. As introduced, scholars advocated that CHL is more than the ability to analyze health-related information critically and should reflect societal influences on health knowledge, beliefs, and behaviors (26–28, 74, 75). Therefore, we built a set of items to thoroughly measure this domain and divided them into three categories. Specifically, in CHL-1, we drew items from existing research to examine subjects' skills to judge the quality of information; In CHL-2, we selected the most fundamental and non-medical causes of individuals' lifestyles from the WHO report to test people's knowledge of SDH (76); In CHL-3, we examined people's activities to address SDH at the social level and interpersonal level.
Second, this scale provides new insights into the domain of CHL in Nutbeam's framework, as it was developed in non-western countries. Previous studies (74, 77–79) emphasized the importance of collective action to address social determinants of health to measure CHL. They argued that individuals with sufficient CHL skills tended to participate in social and political movements for change, including informed voting and advocacy for health issues. However, we proposed that the action should not be narrowed to this social level. This is because solely focusing on participation in collective action may not fully capture the CHL level of certain population groups with limited resources to participate in political action to shape a better society, such as Hong Kong people. In fact, emerging studies (28, 80–84) recognized the importance of interpersonal-level activities to address social determinants of health. It can be assumed that people with sufficient CHL skills may transfer the knowledge of social structural factors of health into actions to get peer support or build a supportive environment for health at the interpersonal level. For instance, one newly developed scale focusing on adolescents' CHL also included individuals' ability to provide social support and participate in democratic actions about health as its component (84). In HLS-HK, we formulated three questions (i.e., q26-q28) to complement the measurement of interpersonal-level actions to address social determinants of health and, in turn, increase this domain's cultural sensitivity across different cultures.
Scale validation
Overall, the scale is reliable and valid. The internal consistency for the scale and subscales are satisfactory. EFA produced a five-factor solution, and CFA revealed an acceptable fit of the five-factor model. These results confirmed that the 27-item of HLS-HK represents the framework as initially designed. The convergent validity of HLS-HK was achieved by using HL-SF12 as the reference tool. Further, we compared the correlation between the subscales from the two scales. The three domains under the CHL level rather than FHL or IHL, had weak relationships with the subscales of HL-SF12. This may be because our scale measured several HL skills missed in HL-SF12. This result supports the research gap mentioned at the beginning: limited operationalization of CHL in previous scales.
The q18 was excluded because of its low item-total correlation. Our previous Delphi study already showed divergent opinions on this item among health professionals and laypeople. Although laypeople acknowledged the influence of socioeconomic factors on health, they tended to believe personal lifestyle substantially affects health. In contrast, health professionals can fully understand the effect of social structural factors on health, which can be more important than lifestyle choices at some point. Regarding this divergence, previous studies highlighted that laypeople might be more likely to understand and express the idea about social disadvantage and health through a contextualized narrative description of their own experiences compared with answering fixed choice questions (74). Hence, it is not surprising that we did not get concise answers on this item, which caused its low correlation with other items.
This study showed that HLS-HK is significantly associated with education. It was possible to observe a higher proportion of individuals with a high level of education (i.e., post-secondary) among those with a better score on HLS-HK. This finding is similar to studies elsewhere (85, 86). There are two potential explanations for this finding. First, highly educated groups have access to information and resources needed for better health outcomes, while low-educated groups often lack these resources. Second, advanced education usually provides a higher level of cognitive skills to process and use information compared with primary education. For instance, in Hong Kong, health promotion programmes under the Healthy School Policy in primary and secondary schools mainly cover basic health knowledge (87–89). Contrarily, health education among local university students focuses on problem-solving skills for a range of health issues (90, 91), which are beneficial for them to develop sophisticated HL skills. Hence, it is crucial to set up systems for universal access to health-related sources and create easy-to-understand health education materials for the general public. Moreover, HL is dynamic, not unchangeable. It can be improved by providing information, effective communication, and structured health education programs. In this respect, HL is a critical concept for reducing health inequalities.
Besides, a positive association between HLS-HK and self-rated health was obtained. This result is consistent with previous studies (9, 92, 93). However, there is no association between the whole scores of HL and health behaviors, age, and income in our study. It is still unclear how health literacy competencies might contribute to individual or community health outcomes and how such competencies might be affected by social status factors. Several conceptual models of the pathways linking HL to health outcomes have been proposed (94, 95). As noted in the models, the paths among antecedent factors (e.g., income and age), HL, and health-related behaviors and outcomes are complicated (94). Health system-level moderators (e.g., healthcare system and healthcare providers) and societal-level moderators (e.g., culture, community resources, and family) can affect the pathway between HL and health outcomes (94). In the present study, the association between these health-related variables and scores on the subscales of HL provided more details on the paths. For instance, the negative association between CHL-1 and age was evidenced in the study. It seems reasonable that critically analyzing information is more difficult for older individuals because of age-related cognitive decline. To summarize, comprehensive knowledge of HL in the general population is essential to guide health systems and organizations to achieve better health outcomes. More empirical studies are warranted to better understand the pathways and guide effective health promotion policies and programs in the future.
Study limitations
Several limitations of this study should be noted. First, selection biases might exist. The study subjects were recruited from an online questionnaire platform registers who may be better at seeking and understanding information and are interested in health issues. It is not surprising that in the present dataset, most participants were highly educated or have high incomes who may have more resources to access and use information, and healthy people who may often use the Internet to search for healthy lifestyle advice. Moreover, because we set up an attention check question, older adults who were more easily distracted may have failed to return a complete form and therefore were excluded from the analysis. Further study is needed to examine whether the HLS-HK is acceptable to people with a wide range of HL levels. Second, respondents may overestimate their HL using a self-reported scale. Due to resource limitations, the present study did not use a performance-based measure as the comparison scale, so the overestimation effect needs to be further explored. Third, it might be possible that some aspects of CHL were not included in the measure due to the complexity of this domain. Although we used a deductive approach via literature review to generate items, more diverse views may be considered to reflect more comprehensive perspectives of this domain. For example, further research to study residents' insights about transferring knowledge into action to address social determinants of health via focus groups may be needed.
Implications for policy and practice
Despite its limitations, the implication of this study should be highlighted. First, this scale HLS-HK can be used to comprehensively measure FHL, IHL, and CHL. The true promise of one HL scale is not to simply screen people according to their HL level but also should be to inform and tailor future interventions to enhance their HL. Therefore, using a comprehensive HL measurement such as HLS-HK can benefit healthcare workers, policymakers, and researchers to better understand the difficulties and barriers that service users may encounter when they use health-related information and services (e.g., found difficulty in understanding medical jargon, embarrassed to ask questions during medical consultation, overwhelmed by information overload, didn't realize the societal benefit of vaccination, and low interests to take action for public health) and further design interventions to address these issues. Next, a further possible use of HLS-HK is as a tool to explore the path between HL and health outcomes. A clear link between HL and health outcomes could result in higher quality and more effective interventions. As noted, more empirical studies (e.g., cross-sectional survey and longitudinal study) are needed to examine the impacts of HL on healthcare, such as how HL leads to healthy behaviors across different age groups and different utilization rates of screening programmes by place of residence in Hong Kong. Finally, HL is an evolving construct, and there is no consensus on its components. We hope our work could contribute to a more comprehensive understanding of HL as a social construct rather than a set of skills related to information transmission. Of course, the scale needs to undergo rigorous testing with diverse population groups so that it can be used to evaluate and compare HL across cultures. Other researchers can use or amend this scale for their research interests and target populations' needs. For example, scholars in a democratic country can use this scale to learn how citizens transfer their understanding of health into actions for personal health and community health in depth. For scholars in an autocratic society, however, they may need to contextualize the items of CHL as residents might have low motivation and resources for social participation for health.
Conclusion
The HLS-HK is valid and reliable for evaluating HL in Hong Kong. This scale can measure FHL, IHL, and CHL in clinical and public health contexts. It also extended the operationalization of the above domains and fully operationalized the CHL via three subdomains. HLS-HK, with a testable framework and multifaceted attributes, will be validated in more countries and populations to advance this field of science further.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Survey and Behavioral Research Ethics Committee of the Chinese University of Hong Kong. The patients/participants provided their written informed consent to participate in this study.
Author contributions
EW, PM, DD, and CT designed the study. CT collected and analyzed the data, wrote the draft manuscript, and critically revised the manuscript. EW was responsible for data curation and project administration. DD and PM were incharge of project administration and supervision. AC assisted with the funding acquisition and project administration. EW, PM, and DD commented and edited the whole draft. All authors read and approved the final manuscript.
Funding
The study was funded by the Direct Grant from The Chinese University of Hong Kong (Reference No. 2020.027).
Acknowledgments
The authors would like to thank all participants who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1043197/full#supplementary-material
References
1. Nutbeam D. Health promotion glossary. Health Promot Int. (1998) 13:349–64. doi: 10.1093/heapro/13.4.349
2. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
3. Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. (1997) 87:1027–30. doi: 10.2105/AJPH.87.6.1027
4. Song L, Mishel M, Bensen JT, Chen RC, Knafl GJ, Blackard B, et al. How does health literacy affect quality of life among men with newly diagnosed clinically localized prostate cancer? Findings from the North Carolina-Louisiana Prostate Cancer Project (PCaP). Cancer. (2012) 118:3842–51. doi: 10.1002/cncr.26713
5. Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. (2002) 40:395–404. doi: 10.1097/00005650-200205000-00005
6. Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. (2002) 92:1278–83. doi: 10.2105/AJPH.92.8.1278
7. Rasu RS, Bawa WA, Suminski R, Snella K, Warady B. Health literacy impact on national healthcare utilization and expenditure. Int J Health Policy Manag. (2015) 4:747–55. doi: 10.15171/ijhpm.2015.151
8. Eichler K, Wieser S, Brügger U. The costs of limited health literacy: a systematic review. Int J Public Health. (2009) 54:313–24. doi: 10.1007/s00038-009-0058-2
9. Sørensen K, Pelikan JM, Röthlin F, Ganahl K, Slonska Z, Doyle G, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health. (2015) 25:1053–8. doi: 10.1093/eurpub/ckv043
10. Shed HLT. Health Literacy Tool Shed. (2022). Available online at: https://healthliteracy.bu.edu/ (accessed October 01, 2022).
11. Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults. - a new instrument for measuring patients literacy skills. J Gen Intern Med. (1995) 10:537–41. doi: 10.1007/BF02640361
12. Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. (2005) 3:514–22. doi: 10.1370/afm.405
13. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Health. (2004) 588:594. Retrieved from https://journals.stfm.org/familymedicine/
14. Chinn D, McCarthy C. All Aspects of Health Literacy Scale (AAHLS): developing a tool to measure functional, communicative and critical health literacy in primary healthcare settings. Patient Educ Counsel. (2013) 90:247–53. doi: 10.1016/j.pec.2012.10.019
15. Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health. (2013) 13:658. doi: 10.1186/1471-2458-13-658
16. Jordan JE, Buchbinder R, Briggs AM, Elsworth GR, Busija L, Batterham R, et al. The health literacy management scale (HeLMS): a measure of an individual's capacity to seek, understand and use health information within the healthcare setting. Patient Educ Counsel. (2013) 91:228–35. doi: 10.1016/j.pec.2013.01.013
17. Tavousi M, Haeri-Mehrizi A, Rakhshani F, Rafiefar S, Soleymanian A, Sarbandi F, et al. Development and validation of a short and easy-to-use instrument for measuring health literacy: the Health Literacy Instrument for Adults (HELIA). BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-08787-2
18. Haun JN, Valerio MA, McCormack LA, Sørensen K, Paasche-Orlow MK. Health literacy measurement: an inventory and descriptive summary of 51 instruments. J Health Commun. (2014) 19:302–33. doi: 10.1080/10810730.2014.936571
19. Liu H, Zeng H, Shen Y, Zhang F, Sharma M, Lai W, et al. Assessment tools for health literacy among the general population: a systematic review. Int J Environ Res Public Health. (2018) 15:1711. doi: 10.3390/ijerph15081711
20. Guzys D, Kenny A, Dickson-Swift V, Threlkeld G. A critical review of population health literacy assessment. BMC Public Health. (2015) 15:215. doi: 10.1186/s12889-015-1551-6
21. Pleasant A, Maish C, O'Leary C, Carmona R. Measuring health literacy in adults: An overview and discussion of current tools. Int Handb Health Lit. (2019) 67. doi: 10.51952/9781447344520.ch005
22. Urstad KH, Andersen MH, Larsen MH, Borge CR, Helseth S, Wahl AK. Definitions and measurement of health literacy in health and medicine research: a systematic review. BMJ Open. (2022) 12:e056294. doi: 10.1136/bmjopen-2021-056294
23. Sørensen K, Van den Broucke S, Pelikan JM, Fullam J, Doyle G, Slonska Z, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health. (2013) 13:1–10. doi: 10.1186/1471-2458-13-948
24. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. (2000) 15:259–67. doi: 10.1093/heapro/15.3.259
25. Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:80. doi: 10.1186/1471-2458-12-80
26. Renwick K, editor Critical health literacy in 3D. Front Educ. (2017) 2:1–5. doi: 10.3389/feduc.2017.00040
27. Abel T, McQueen D. Critical health literacy and the COVID-19 crisis. Health Promot Int. (2020) 35:1612–3. doi: 10.1093/heapro/daaa040
28. De Wit L, Fenenga C, Giammarchi C, Di Furia L, Hutter I, de Winter A, et al. Community-based initiatives improving critical health literacy: A systematic review and meta-synthesis of qualitative evidence. BMC Public Health. (2018) 18:1–11. doi: 10.1186/s12889-017-4570-7
29. Pavelić A, Špiranec S. Critical health literacy and critical information literacy: bridging research discourses from different domains. In: European Conference on Information Literacy. Paris: Springer. (2022).
30. Suka M, Odajima T, Kasai M, Igarashi A, Ishikawa H, Kusama M, et al. The 14-item health literacy scale for Japanese adults (HLS-14). Environ Health Prev Med. (2013) 18:407–15. doi: 10.1007/s12199-013-0340-z
31. Kang SJ, Lee TW, Paasche-Orlow MK, Kim GS, Won HK. Development and evaluation of the Korean health literacy instrument. J Health Commun. (2014) 19:254–66. doi: 10.1080/10810730.2014.946113
32. Chung MH, Chen LK, Peng LN, Chi MJ. Development and validation of the health literacy assessment tool for older people in Taiwan: Potential impacts of cultural differences. Arch Gerontol Geriatr. (2015) 61:289–95. doi: 10.1016/j.archger.2015.06.015
33. Intarakamhang U, Kwanchuen Y. The development and application of the ABCDE-health literacy scale for Thais. Asian Biomedicine. (2016) 10:587–94. doi: 10.5372/1905-7415.1006.527
34. Abel T, Hofmann K, Ackermann S, Bucher S, Sakarya S. Health literacy among young adults: a short survey tool for public health and health promotion research. Health Promot Int. (2015) 30:725–35. doi: 10.1093/heapro/dat096
35. Steckelberg A, Hülfenhaus C, Kasper J, Rost J, Mühlhauser I. How to measure critical health competences: Development and validation of the Critical Health Competence Test (CHC Test). Adv Health Sci Educ. (2009) 14:11–22. doi: 10.1007/s10459-007-9083-1
36. Wong HM, Bridges SM, Yiu CK, McGrath CP, Au TK, Parthasarathy DS. Development and validation of Hong Kong rapid estimate of adult literacy in dentistry. J Investig Clin Dent. (2012) 3:118–27. doi: 10.1111/j.2041-1626.2012.00113.x
37. Wong HM, Bridges SM, Yiu CKY, McGrath CPJ, Au TK, Parthasarathy DS. Validation of the Hong Kong oral health literacy assessment task for paediatric dentistry (HKOHLAT-P). Int J Paediatr Dent. (2013) 23:366–75. doi: 10.1111/ipd.12021
38. Leung AYM, Cheung MKT, Lou VWQ, Chan FHW, Ho CKY, Do TL, et al. Development and validation of the chinese health literacy scale for chronic care. J Health Commun. (2013) 18(Suppl. 1):205–22. doi: 10.1080/10810730.2013.829138
39. Chau PH, Leung AYM, Li HLH, Sea M, Chan R, Woo J. Development and validation of Chinese Health Literacy Scale for low salt consumption - Hong Kong population (CHLSalt-HK). PLoS ONE. (2015) 10. doi: 10.1371/journal.pone.0132303
40. Leung AY, Yu EY, Luk JK, Chau P, Levin-Zamir D, Leung IS, et al. Rapid Estimate of Inadequate Health Literacy (REIHL): development and validation of a practitioner-friendly health literacy screening tool for older adults. Hong Kong Med J. (2020) 26:404–12. doi: 10.12809/hkmj208395
41. Zhang F, Or PPL, Chung JWY. The effects of health literacy in influenza vaccination competencies among community-dwelling older adults in Hong Kong. BMC Geriatr. (2020) 20:1–7. doi: 10.1186/s12877-020-1504-5
42. Or PPL, Wong BYM, Chung JWY. To investigate the association between the health literacy and hand hygiene practices of the older adults to help them fight against infectious diseases in Hong Kong. Am J Infect Control. (2020) 48:485–9. doi: 10.1016/j.ajic.2019.12.021
43. Tsui YM, Fong BY. Waiting time in public hospitals: case study of total joint replacement in Hong Kong. Public Adm Policy. (2018) 21:120–33. doi: 10.1108/PAP-10-2018-009
44. Lee CP. Health care system and pharmacy practice in Hong Kong. Can J Hosp Pharm. (2018) 71:140. doi: 10.4212/cjhp.v71i2.1865
45. Tian CY, Xu RH, Mo PKH, Dong D, Wong ELY. Generic health literacy measurements for adults: a scoping review. Int J Environ Res Public Health. (2020) 17:7768. doi: 10.3390/ijerph17217768
46. Tian CY, Ng CW, Xu RH, Mo PKH, Dong D, Wong ELY. Critical health literacy in the Post-COVID-19 Era. Hong Kong College of Community Medicine Annual Scientific Meeting. Hong Kong (2021). p. 75. Available online at: http://www.hkccm.org.hk/pdffile/210924093700422.pdf
47. Tian CY, Wong ELY, Xu RH, Cheung AWL, Dong D, Mo PKH. Developing a comprehensive health literacy scale for adults in Hong Kong: a modified e-Delphi study in healthcare consumers and providers. Health Expect. (2022) 1–11. doi: 10.1111/hex.13651
48. Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. National Cancer Institute: Sage Publications. (200)4.
49. Ryan K, Gannon-Slater N, Culbertson MJ. Improving survey methods with cognitive interviews in small-and medium-scale evaluations. Am J Eval. (2012) 33:414–30. doi: 10.1177/1098214012441499
50. Census and Statistics Department TGotHKSAR. Hong Kong in Figures (Latest Figures). 2020 Available from: https://www.censtatd.gov.hk/hkstat/hkif/index.jsp. (accessed August 01, 2022).
51. Anthoine E, Moret L, Regnault A, Sébille V, Hardouin JB. Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes. (2014) 12:1–10. doi: 10.1186/s12955-014-0176-2
52. Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. (2018) 6:149. doi: 10.3389/fpubh.2018.00149
53. Van Duong T, Chang PW, Yang SH, Chen MC, Chao WT, Chen T, et al. A new comprehensive short-form health literacy survey tool for patients in general. Asian Nurs Res. (2017) 11:30–5. doi: 10.1016/j.anr.2017.02.001
54. Duong TV, Aringazina A, Kayupova G, Nurjanah, Pham TV, Pham KM, et al. Development and validation of a new short-form health literacy instrument (HLS-SF12) for the general public in six Asian countries HLRP. Health Lit Res Pract. (2019) 3:e91–e102. doi: 10.3928/24748307-20190225-01
55. Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life: a conceptual model of patient outcomes. JAMA. (1995) 273:59–65. doi: 10.1001/jama.1995.03520250075037
56. Idler EL. Self-assessed health and mortality: a review of studies. Int Rev Health Psychol. (1992) 1:33–54.
58. Jatau Abubakar I, Wimmer BC, Bereznicki LR, Dwan C, Black JAM, Bezabhe W, et al. Development and Validation of an Atrial Fibrillation Knowledge Assessment Tool (AFKAT). Int J Environ Res Public Health. (2020) 17:1721. doi: 10.3390/ijerph17051721
59. Kliemann N, Wardle J, Johnson F, Croker H. Reliability and validity of a revised version of the General Nutrition Knowledge Questionnaire. Eur J Clin Nutr. (2016) 70:1174–80. doi: 10.1038/ejcn.2016.87
60. Lang L, Zhang L, Zhang P, Li Q, Bian J, Guo Y. Evaluating the reliability and validity of SF-8 with a large representative sample of urban Chinese. Health Qual Life Outcomes. (2018) 16:1–8. doi: 10.1186/s12955-018-0880-4
61. Cristobal E, Flavian C, Guinaliu M. Perceived e-service quality (PeSQ): Measurement validation and effects on consumer satisfaction and web site loyalty. Manag Serv Qual. (2007) 17:317–40. doi: 10.1108/09604520710744326
63. Kebede Y, Alemayehu G, Abebe L, Sudhakar M, Birhanu Z. Messenger students' engagement scale: Community perspectives on school-based malaria education in Ethiopia. Health Soc Care Community. (2021) 29:1391–400. doi: 10.1111/hsc.13193
64. Ogedegbe G, Mancuso CA, Allegrante JP, Charlson ME. Development and evaluation of a medication adherence self-efficacy scale in hypertensive African-American patients. J Clin Epidemiol. (2003) 56:520–9. doi: 10.1016/S0895-4356(03)00053-2
65. Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. (1999) 6:1–55. doi: 10.1080/10705519909540118
66. Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. J Gerontol Ser B. (2000) 55:S368–S74. doi: 10.1093/geronb/55.6.S368
67. Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. (2005) 20:175–84. doi: 10.1111/j.1525-1497.2005.40245.x
68. Wu Y, Wang L, Cai Z, Bao L, Ai P, Ai Z. Prevalence and risk factors of low health literacy: a community-based study in Shanghai, China. Int J Environ Res Public Health. (2017) 14:628. doi: 10.3390/ijerph14060628
69. Wolf MS, Feinglass J, Thompson J, Baker DW. In search of ‘low health literacy’: Threshold vs. gradient effect of literacy on health status and mortality. Soc Sci Med. (2010) 70:1335–41. doi: 10.1016/j.socscimed.2009.12.013
70. Jayasinghe UW, Harris MF, Parker SM, Litt J, van Driel M, Mazza D, et al. The impact of health literacy and life style risk factors on health-related quality of life of Australian patients. Health Qual Life Outcomes. (2016) 14:1–13. doi: 10.1186/s12955-016-0471-1
71. Wolf MS, Gazmararian JA, Baker DW. Health literacy and health risk behaviors among older adults. Am J Prev Med. (2007) 32:19–24. doi: 10.1016/j.amepre.2006.08.024
72. Heckler CE. A Step-by-step Approach to Using the SAS™ System for Factor Analysis and Structural Equation Modeling. Taylor & Francis. SAS Institute, Inc. (1996).
73. Kyriazos TA. Applied psychometrics: sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology. (2018) 9:2207. doi: 10.4236/psych.2018.98126
74. Chinn D. Critical health literacy: a review and critical analysis. Soc Sci Med. (2011) 73:60–7. doi: 10.1016/j.socscimed.2011.04.004
75. Sykes S, Wills J, Rowlands G, Popple K. Understanding critical health literacy: a concept analysis. BMC Public Health. (2013) 13:1–10. doi: 10.1186/1471-2458-13-150
76. Organization WH. Social Determinants of Health: The Solid Facts. World Health Organization. Regional Office for Europe. (2003). p. 7–10. Available online at: https://www.euro.who.int/_data/assets/pdf_file/0005/98438/e81384.pdf
77. Corcoran T. Critical psychologies for critical health literacies. Asia Pac J Health Sport Phys Educ. (2014) 5:281–95. doi: 10.1080/18377122.2014.940813
78. Wang RT. Critical health literacy: a case study from China in schistosomiasis control. Health Promot Int. (2000) 15:269–74. doi: 10.1093/heapro/15.3.269
79. Crondahl K, Karlsson LE. The Nexus Between Health Literacy and Empowerment: A Scoping Review. Denmark: Sage Open. (2016). p. 6.
80. Levin-Zamir D, Peterburg Y. Health literacy in health systems: perspectives on patient self-management in Israel. Health Promot Int. (2001) 16:87–94. doi: 10.1093/heapro/16.1.87
81. Fredriksen EH, Harris J, Moland KM, Sundby J. “They ask whether this is real or fake”: A qualitative norwegian study of pregnancy complaints and access to social benefits. Health Care Women Int. (2014) 35:266–84. doi: 10.1080/07399332.2013.794463
82. Liu C, Wang D, Liu C, Jiang J, Wang X, Chen H, et al. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam Med Community Health. (2020) 8:e000351. doi: 10.1136/fmch-2020-000351
83. Guo S, Davis E, Yu X, Naccarella L, Armstrong R, Abel T, et al. Measuring functional, interactive and critical health literacy of Chinese secondary school students: reliable, valid and feasible? Glob Health Promot. (2018) 25:6–14. doi: 10.1177/1757975918764109
84. Haugen ALH, Riiser K, Esser-Noethlichs M, Hatlevik OE. Developing Indicators to Measure Critical Health Literacy in the Context of Norwegian Lower Secondary Schools. Int J Environ Res Public Health. (2022) 19:3116. doi: 10.3390/ijerph19053116
85. Huang CH, Talley PC, Lin CW, Huang RY, Liu IT, Chiang IH, et al. Factors associated with low health literacy among community-dwelling women in Taiwan. Women Health. (2020) 60:487–501. doi: 10.1080/03630242.2019.1662872
86. Jansen T, Rademakers J, Waverijn G, Verheij R, Osborne R, Heijmans M. The role of health literacy in explaining the association between educational attainment and the use of out-of-hours primary care services in chronically ill people: a survey study. BMC Health Serv Res. (2018) 18:1–13. doi: 10.1186/s12913-018-3197-4
87. Li MH, Sit CHP, Wong SHS, Wing YK, Ng CK, Sum RKW. Promoting physical activity and health in Hong Kong primary school children through a blended physical literacy intervention: protocol and baseline characteristics of the “Stand+ Move” randomized controlled trial. Trials. (2021) 22:1–15. doi: 10.1186/s13063-021-05925-y
88. Sobko T, Jia Z, Kaplan M, Lee A, Tseng Ch. Promoting healthy eating and active playtime by connecting to nature families with preschool children: Evaluation of pilot study “Play&Grow”. Pediatr Res. (2017) 81:572–81. doi: 10.1038/pr.2016.251
89. Education Bureau TgotHKSAR. Healthy School Policy. (2022). Available online at: https://www.edb.gov.hk/en/edu-system/primary-secondary/healthy-sch-policy/index.html (accessed December 10, 2022).
90. Ahorsu DK, Sánchez Vidaña DI, Lipardo D, Shah PB, Cruz González P, Shende S, et al. Effect of a peer-led intervention combining mental health promotion with coping-strategy-based workshops on mental health awareness, help-seeking behavior, and wellbeing among university students in Hong Kong. Int J Ment Health Syst. (2021) 15:1–10. doi: 10.1186/s13033-020-00432-0
91. Mak WW, Chan AT, Cheung EY, Lin CL, Ngai KC. Enhancing Web-based mindfulness training for mental health promotion with the health action process approach: randomized controlled trial. J Med Internet Res. (2015) 17:e3746. doi: 10.2196/jmir.3746
92. Storey A, Hanna L, Missen K, Hakman N, Osborne RH, Beauchamp A. The association between health literacy and self-rated health amongst Australian university students. J Health Commun. (2020) 25:333–43. doi: 10.1080/10810730.2020.1761913
93. Levin-Zamir D, Baron-Epel OB, Cohen V, Elhayany A. The association of health literacy with health behavior, socioeconomic indicators, and self-assessed health from a national adult survey in Israel. J Health Commun. (2016) 21:61–8. doi: 10.1080/10810730.2016.1207115
94. Squiers L, Peinado S, Berkman N, Boudewyns V, McCormack L. The health literacy skills framework. J Health Commun. (2012) 17:30–54. doi: 10.1080/10810730.2012.713442
Keywords: health literacy scale, scale development, scale validation, Hong Kong Chinese adults, factor analysis
Citation: Tian CY, Mo PK-H, Dong D, Cheung AW-l and Wong EL-Y (2023) Development and validation of a comprehensive health literacy tool for adults in Hong Kong. Front. Public Health 10:1043197. doi: 10.3389/fpubh.2022.1043197
Received: 13 September 2022; Accepted: 20 December 2022;
Published: 10 January 2023.
Edited by:
Ferdinando Petrazzuoli, Center for Primary Health Care Research, Lund University, SwedenReviewed by:
Veronika Rasic, NHS England, United KingdomKazunori Nagasaka, The University of Tokyo, Japan
Shoumei Jia, Fudan University, China
Copyright © 2023 Tian, Mo, Dong, Cheung and Wong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eliza Lai-Yi Wong,  bHl3b25nQGN1aGsuZWR1Lmhr
bHl3b25nQGN1aGsuZWR1Lmhr
 Cindy Yue Tian
Cindy Yue Tian Phoenix Kit-Han Mo
Phoenix Kit-Han Mo Dong Dong
Dong Dong Annie Wai-ling Cheung
Annie Wai-ling Cheung Eliza Lai-Yi Wong
Eliza Lai-Yi Wong