
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 13 January 2023
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1042750
This article is part of the Research TopicStrengthening the Community Health Worker PracticeView all 12 articles
 Ashley Wennerstrom1,2*
Ashley Wennerstrom1,2* Catherine G. Haywood3
Catherine G. Haywood3 Denise O. Smith4
Denise O. Smith4 Dakshu Jindal5
Dakshu Jindal5 Carl Rush6
Carl Rush6 Geoffrey W. Wilkinson7
Geoffrey W. Wilkinson7Introduction: Community health workers (CHWs) have historically worked in community-based settings. Medicaid managed care organizations (MCOs) are integrating CHWs into their teams, largely to support social determinants of health. Little is known about how teams are structured in these environments or how CHWs and their supervisors perceive CHW roles in MCOs.
Methods: In 2021, two CHW professional associations and a university partnered to conduct a national cross-sectional survey of CHWs working with MCOs.
Results: A total of 146 CHWs representing 29 states and 55 supervisors working in 34 states completed the survey. Although two-thirds of supervisors said only a high school diploma or equivalent was required for hiring, over half of CHWs reported having a bachelors or graduate degree. The majority of CHWs (72.6%) and employers (80%) said CHWs receive training in core competencies. Under half of CHWs reported working with a registered nurse (RN) (45.8%) or social worker (43.8%), and about a third work with a behavioral health (36.3%) or primary care provider (33.6%). Among supervisors, 70.9% identified social workers as CHWs' team members and over half indicated CHW work with RNs (56.4%), behavioral health (54.5%) and primary care providers (52.7%). Over half of CHWs (52.1%) and roughly two thirds (63.6%) of supervisors indicated that CHWs use electronic health records. Roughly 85% of CHWs make referrals and roughly three quarters conduct social screenings. Around half of CHWs said they assist with care planning (54.1%), conduct health screenings (52.1%) or participate in case reviews (49.3%). About three quarters of CHWs (75.3%) and over two thirds of supervisors (67.3%) believed that CHWs are utilized to their full potential. Under three quarters of CHWs (72.6%) and over half of supervisors (54.4%) believe CHWs are equitably compensated for their work.
Discussion: Overall, CHWs roles in MCOs appear to focus on supporting clinical care and making referrals for social issues, rather than addressing community-level concerns. Health plans should ensure that CHWs have the professional freedom to develop community-based solutions to common social needs. MCOs should also ensure that CHWs receive equitable compensation and ensure that CHWs have opportunities for promotion.
Community health workers (CHWs) are a critical frontline public health workforce defined by their trusted relationships with the communities they serve (1). Operating under a number of job titles including promotores de salud and community health representatives, for at least 60 years, they have linked individuals and communities with health and social services, helped people navigate complex systems, and advocated for structural changes in policies related to social determinants of health (2–4). While CHWs' roots are primarily in social justice focused, community-based settings, their work has expanded to a variety of agencies including federally qualified health centers, health departments, and universities, among others (5). There is a nationally recognized set of CHW roles and competencies (6), but programs employing CHWs vary based on community strengths and needs, as well as employer structure, focus, capacity, and funding limitations. Although CHWs are difficult to enumerate, in part due to their various job titles, as of 2021, an estimated 61,000 CHWs worked throughout the United States (7).
In the last decade, as health systems have begun to understand the necessity of addressing social issues, many have moved to integrate CHWs into their care teams. The addition of CHWs to clinical service delivery has been found to improve health outcomes (8) and enhance the patient experience of care (9), and support access to culturally appropriate care (10). For example, integrating CHWs into patient-centered medical homes helps teams better understand patients' backgrounds, challenges, and preferences related to care, which can help improve health outcomes (11). Hospital readmission rates have been reduced among patients who receive care from teams with CHWs (9, 12). An investigation of over a hundred innovative care delivery models revealed that only those using CHWs lowered cost (13). There is also some evidence that adding CHWs to clinical care teams has improved adherence to medications and timely utilization of healthcare services (14).
Researchers seeking to understand factors that promote successful integration have identified clarity of team member roles, clearly defined workflows, and positive culture as important (14, 15). Healthcare team members, including CHWs, have reported that the presence of leaders who support CHWs, as well as a clinic culture that focuses on social, rather than exclusively medical needs, is also critical (16). However, there is some evidence that integration can present challenges to CHWs in maintaining their unique identities as community advocates (17). Healthcare settings tend to value formal education and training above lived experience when hiring CHWs (17), raising questions about whether clinical integration may pull CHWs away from their roots in social justice.
Another area in which CHWs newly find themselves engaged is in Medicaid managed care. Managed care organizations (MCOs), which enter contracts with states to provide health services to Medicaid members, usually on a per member per month basis (18, 19), are highly motivated to achieve two aims in which CHWs are skilled: improving outcomes and reducing costs of care (13, 20–23). MCOs generally have flexibility in their staffing and service delivery models, and some have opted to hire CHWs or contract with external organizations for CHW services. With an increasing emphasis on addressing population health, some states have started to require that MCOs employ CHWs. As of 2021, 10 of 41 states (including DC) that have managed care have instituted some sort of requirement that their contracted MCOs offer CHW services to enrollees. An additional six states indicated that they would also require CHW services in their contracts in the following year (24). As one example, managed care contracts in New Mexico require that at least 3% of enrollees must receive CHW support (25).
Although there is clear momentum for integrating CHWs into MCOs, there is a dearth of national information about MCO priorities for hiring and training CHWs, how teams are structured in these environments, and how CHWs and their supervisors perceive CHW participation in work with MCOs. A few state-level studies provide some important insight. New Mexico-based Molina Healthcare, an early adopter of CHWs employment in an MCO, provided a week of training in many core CHW skills and hired CHWs to support frequent users of the emergency department through education, social support and advocacy, resulting in reduced emergency department visits and overall costs of care (22). In California, providers reported positive experiences when collaborating with CHWs through an MCO initiative that focused on ensuring that CHWs hired held credibility in their communities (26). A 2018 study found that hiring practices and qualifications for CHW employment varied widely among MCOs in Arizona (27) and coordination care organizations in Oregon have found that a lack of understanding of CHW roles among leadership has proved a barrier to CHW integration (28).
This national study aimed to add to the evidence base regarding CHW-MCO integration by surveying CHWs about their experiences working with MCOs. CHW program supervisors working with MCOs were also surveyed, as supervision is critical to successful CHW-team integration (29). Survey questions focused on employer-offered training, CHW responsibilities within their teams, team structure and supervision, reporting structure, and perceptions of team integration. The research team expected that CHWs roles and responsibilities within MCOs would largely be focused on improving clinical outcomes.
A researcher from LSU Health Sciences Center—New Orleans and CHWs from the Louisiana Community Health Outreach Network (LACHON) and the National Association of Community Health Workers (NACHW) with longstanding relationships collaborated to carry out this study. Two subject matter experts who are founding board members of NACHW provided additional guidance.
The research team based its study methods on previous recommendations for conducting CHW workforce survey research, which include engaging CHWs in survey design, collaborating with CHW networks to distribute the survey, and piloting the survey with CHWs (30). The team collaboratively agreed upon a general list of survey topics including demographics, CHW responsibilities, team structure, and perceptions of team integration. Working from a prior survey (31), the team then selected relevant questions to address the topics identified. Questions and response categories were updated and added, as needed.
The survey was distributed online via LACHON's listserv of over 400 CHWs and allies and through NACHW's member newsletter. It remained open from March to July 2021. Over 20 local, state, and regional CHW networks and associations, as well as a dozen national organizations (e.g., policy-focused think tanks and trade organizations for health insurers), were enlisted to support survey distribution. Criteria for participation included: (1) being an adult (18+ years of age) and (2) being employed as a CHW or CHW supervisor at an MCO or at another organization (e.g., a community-based organization) that receives a contract from an MCO to provide CHW services. Interested participants were entered into a raffle for a pre-paid $50 Visa gift card.
Informed consent language was included at the beginning of the survey. The IRB at LSU Health Sciences Center reviewed and approved all research procedures. All data were analyzed using SPSS version 26. Descriptive statistics are reported.
A total of 146 CHWs representing 29 states and 55 supervisors working in 34 states (among 41 with managed care) completed the survey. Among CHWs, over one quarter (27.4%) of respondents were from the West. Just under one quarter (22.6%) reported being from the Midwest. Another 18.5% worked in the Mid-Atlantic region, while 16.4% were from the South, and 15.1% the Northeast. Supervisors often worked across state lines, with 45.5% working in the South and over four in 10 (41.8%) working in the Midwest. Almost one third (30.9%) had work activities in the West, while another 14.5% were in the Northeast. Just 10.9% reported working in the Mid-Atlantic region.
The vast majority of CHWs (87%) and supervisors (76.4%) were women. About four in 10 CHWs were Black, 30.8% were white, and roughly one-quarter were Hispanic/Latinx. Almost six in 10 supervisors were white, just under a quarter were Black, and 7.3% were Hispanic/Latinx. CHWs in this sample most commonly reported having completed some college (37.7%) or a bachelor's degree (37.7%). Nearly three-quarters of the supervisors had a graduate degree. Demographics are summarized in Table 1.
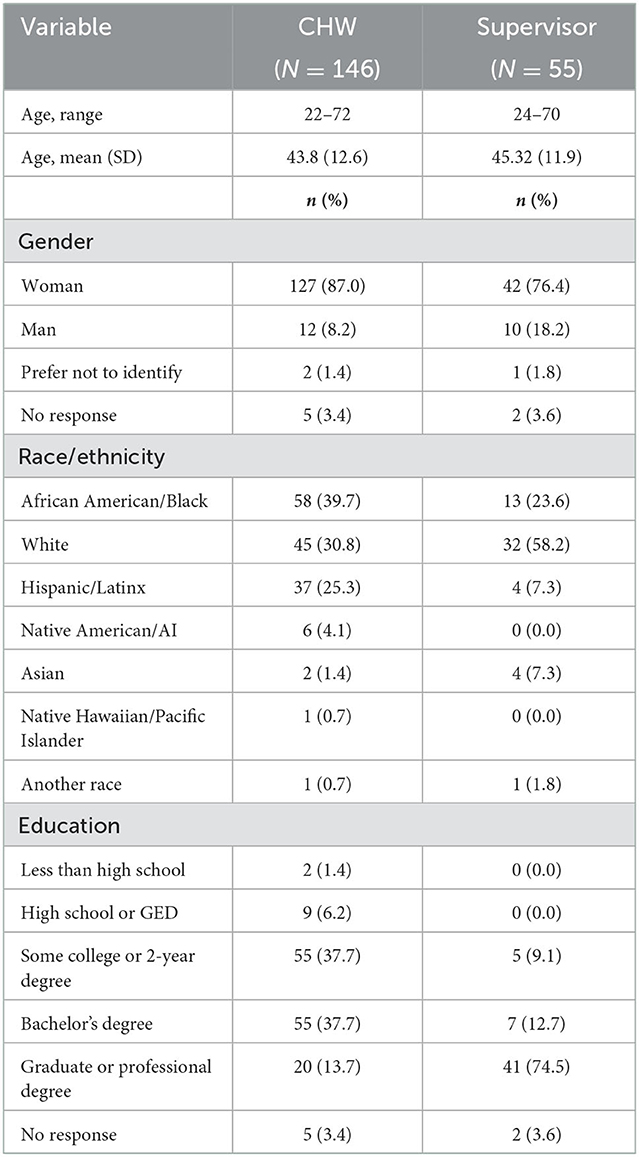
Table 1. Demographics of national sample of CHWs and CHW supervisors working with Medicaid managed care organizations.
In response to a question about professional requirements for hiring CHWs, just under 10% of supervisors said there was no minimum. About two-thirds of supervisors said a high school diploma or equivalent was necessary. Roughly 9% looked for some college or an associate's degree and about 11% required a bachelor's degree. Table 2 contains these results.
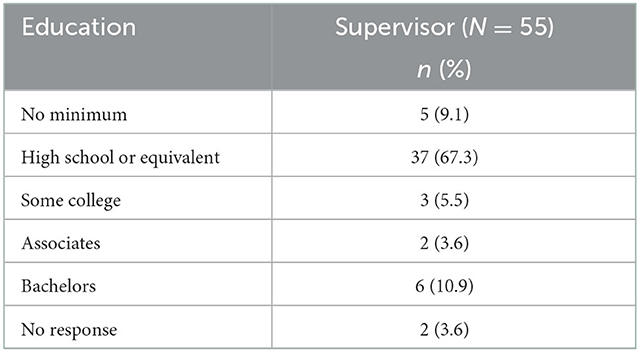
Table 2. Minimum CHW education required for hiring as reported by supervisors working with Medicaid managed care organizations.
The vast majority of CHWs (72.6%) and employers (80%) reported that CHWs receive training in core competencies. Over half of CHWs indicated that they received training in motivational interviewing and advocacy from their employer. Results are detailed in Table 3.
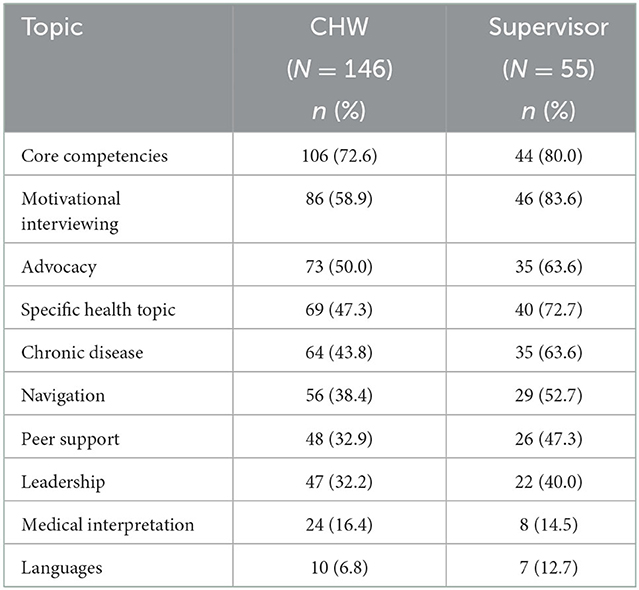
Table 3. Employer-offered training for CHWs reported by a national sample of CHWs and CHW supervisors working with Medicaid managed care organizations.
In terms of team structure, around 8 in 10 CHWs (82.2%) and supervisors (78.2%) indicated that CHWs collaborate with other CHWs. Over half of CHWs and nearly three quarters of supervisors said there was a program manager or director involved. Nearly half of CHWs (47.0%) and about 6 in 10 supervisors (58.2%) said case managers were part of teams. With regard to clinical staff, just under half of CHWs indicated working with a registered nurse (RN) (45.8%) or social worker (43.8%) and about a third said they work with a behavioral health (36.3%) or primary care provider (33.6%). Supervisors more frequently endorsed clinical staff as members of teams, with 70.9% identifying social workers as team members and over half indicating RNs (56.4%), behavioral health (54.5%) and primary care providers (52.7%). Around one in six in both groups indicated that CHWs collaborate with dieticians or nutritionists.
CHWs and employers largely agree that supervision is most commonly provided by a program manager. Fully one quarter of supervisors indicated that social workers supervise CHWs, in contrast to just 5% of CHWs. About one in six CHWs listed another job title as a supervisor. These included the clinic manger, manager of population health, and chief operating officer.
In terms of work documentation, 72.6% of CHWs and 63.6% of employers indicated that CHWs meet with supervisors. About two thirds of CHWs (63.0%) and half (49.1%) of supervisors reported that CHWs use an internal database to track activities. Just over half of CHWs (52.1%) and roughly two thirds (63.6%)of supervisors said that CHWs use electronic health records. About a third of both groups noted that CHWs use narrative reports. These results are summarized in Table 4.
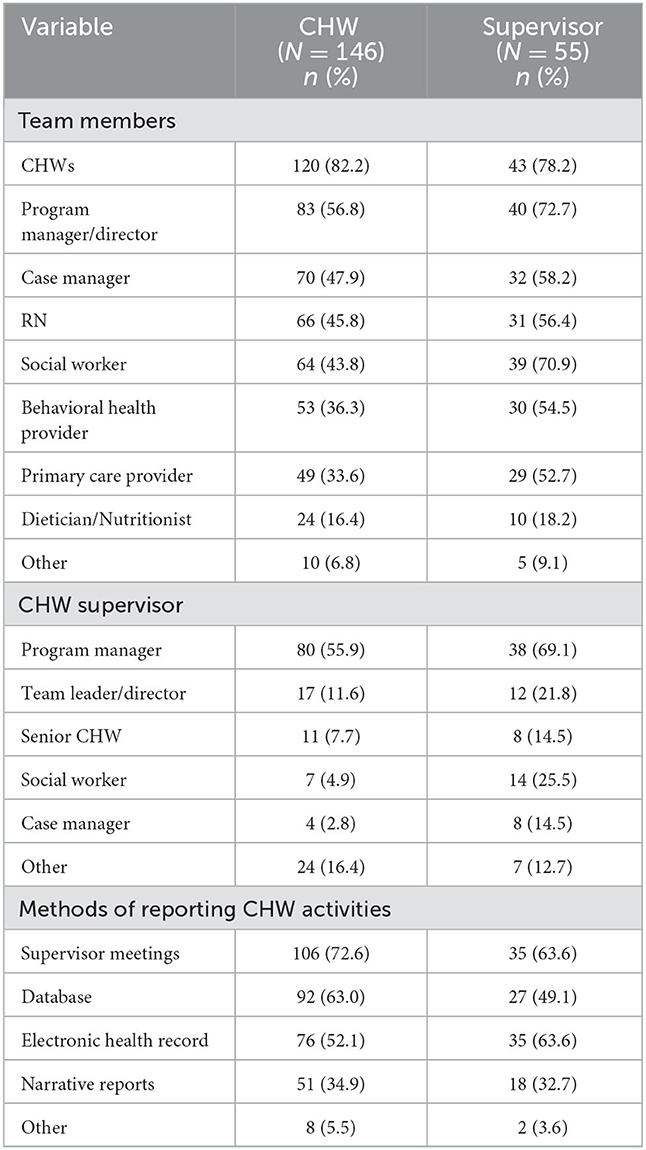
Table 4. Team structure and reporting methods among a national sample of CHWs and CHW supervisors working with Medicaid managed care organizations.
Making referrals was the most common responsibility that CHWs indicated. About three quarters of CHWs indicated that they receive referrals and conduct social screenings while 85.5% of supervisors endorsed such activities. Over 6 in 10 CHWs and 7 in 10 supervisors said that CHWs conduct home visits. Around half of CHWs said they assist with care planning (54.1%), conduct health screenings (52.1%) or participate in case reviews (49.3%). Supervisors' reports of these activities were all slightly higher. CHWs and employers alike reported that < 3 in 10 CHWs provide medical interpretation. Results are reported in Table 5.
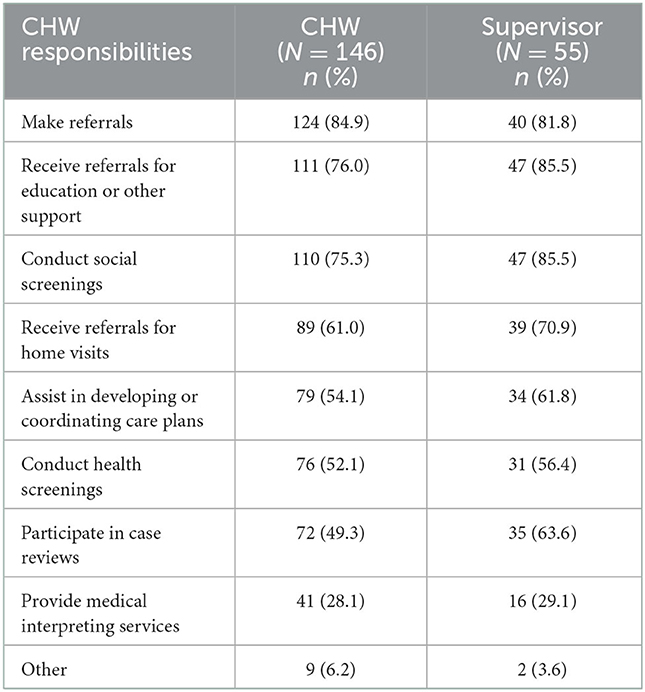
Table 5. CHW responsibilities reported by a national sample of CHWs and CHW supervisors working with Medicaid managed care organizations.
Roughly 93 percent of CHWs and supervisors agreed that CHW work is valued at their organization. Nine in 10 CHWs and 94.5% of supervisors agreed that supervisors understand the work CHWs do. Over eight in 10 CHWs and supervisors indicated that CHWs are well-integrated into teams. Almost nine in 10 CHWs believed their teams understand their work (89.0%) and that they are valued (85.6%). Similarly, 83.6% of supervisors agree that CHWs roles are understood and 89.1% believe CHWs are valued by other team members. About three quarters of CHWs (75.3%) and just over two thirds of supervisors (67.3%) believed that CHWs are utilized to their full potential. Just under three quarters of CHWs (72.6%) and over half of supervisors (54.4%) indicated that CHWs are equitably compensated for their work. Among both CHWs and supervisors, about 6 in 10 agreed that CHWs have opportunities for promotion. These results are detailed in Table 6.
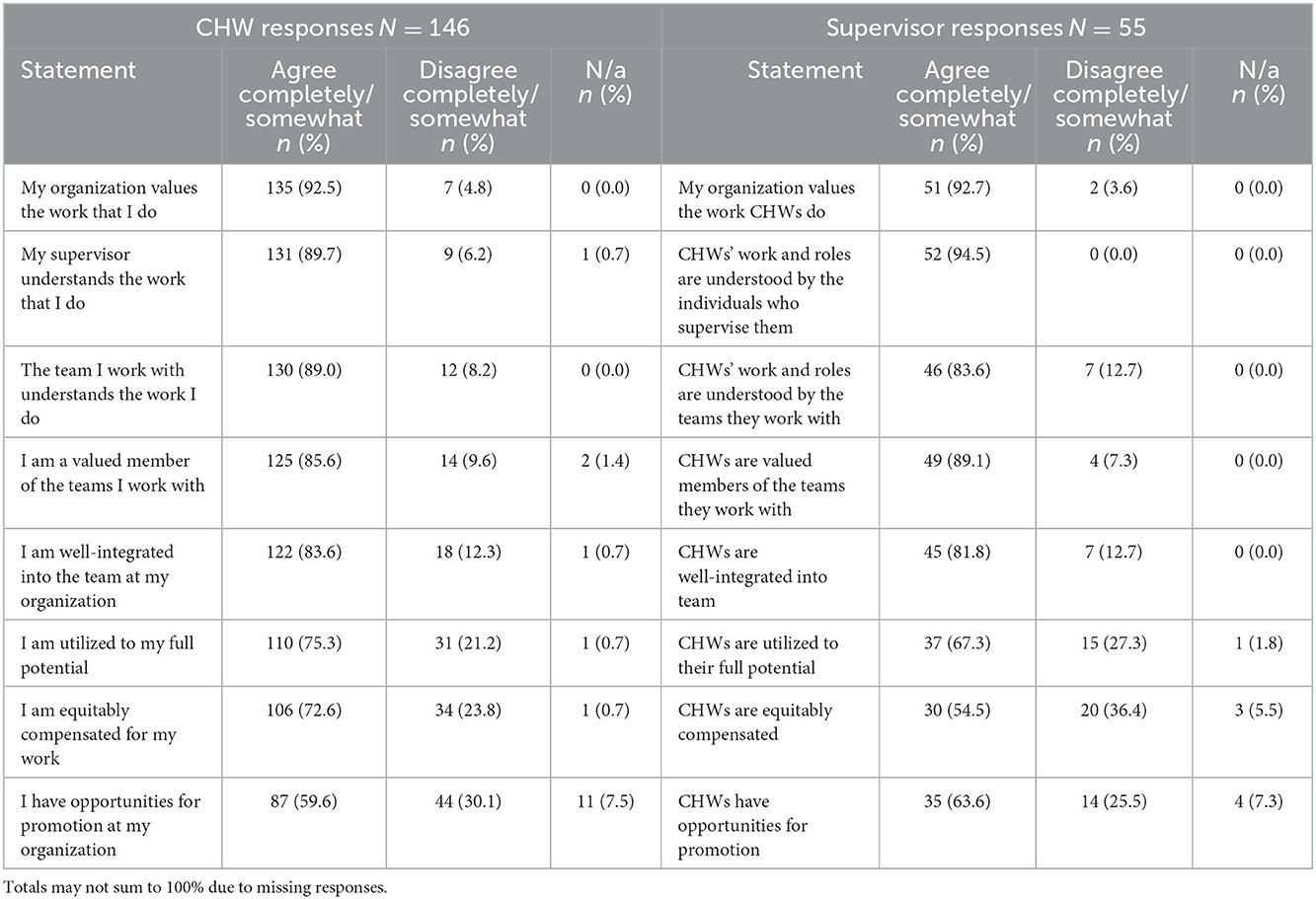
Table 6. Perception of CHW value and team integration among a national sample of CHWs and CHW supervisors working with Medicaid managed care organizations.
This study examined the responsibilities, team structure, and perceptions of integration among MCO-supported CHWs and their employers.
The sample of CHW respondents is similar to other studies of CHWs working across sectors, in that the majority are women and people of color (32). In terms of hiring CHWs, MCOs largely report they are not imposing formal educational requirements beyond high school, but the educational level reported by CHWs—with just 7.6% having a high school education or less and over half having a college or graduate degree—suggests that in practice, MCOs prioritize hiring people with higher levels of education. This finding is concerning, given that CHWs' primary qualification has always been community trust. It also suggests that those making hiring decisions may be unfamiliar with CHWs, which is consistent with a prior study (28).
Overall, there are several indicators that CHWs roles are being conceptualized in terms of supporting clinical care. Supervisor responses to the types of training CHWs receive, which largely included CHW training in skills such as motivational interviewing, chronic disease, and navigation, are directly related to helping patients manage chronic conditions and, ultimately, reducing costs of care. In addition, CHWs' use of electronic health records, along with their participation in conducting case reviews and developing care plans alongside clinically trained providers demonstrate that CHWs are largely focused on improving health outcomes among individual Medicaid members. This medicalized approach suggests that CHWs may have limited time to engage in more community-based, social justice work that is the historical hallmark of the profession (2, 4), and appears to be consistent with a prior study of coordinated care organizations that found individually-focused CHW activities were more common than community-level advocacy (28).
The finding that CHWs make and receive referrals is consistent with nationally recognized CHW roles (6). Although a study in 2018 found limited CHW engagement in conducing assessments (27), the finding that CHWs are now conducting screenings for social needs is unsurprising, given the increasing interest in addressing social determinants of health and that some state Medicaid contracts specifically outline that role (24). As MCOs continue to engage CHWs in their service delivery models, it will be critical to ensure that CHWs' efforts to address social determinants of health are not limited to merely making referrals for social issues identified through screening. CHWs will need freedom to not only develop relationships with agencies that receive member referrals, but also to develop community-based solutions to common social needs. For example, CHWs may collaborate with one another and local leaders to develop a food bank in an area with limited resources. CHWs working in teams have identified the opportunity to network as being critical to their roles (33). Furthermore, ensuring that CHWs have the flexibility to respond to community-level issues could help address the substantial proportion of CHWs and supervisors who report that CHWs are not utilized to their full potential.
It is encouraging that CHWs and supervisors alike generally perceive that CHWs roles are understood and valued by fellow team members. However, it is concerning that over one quarter of CHWs do not feel that CHWs are equitably compensated, as do nearly one half of supervisors, who likely have greater insight than CHWs into compensation levels for various positions. Broadly, CHW contributions have often been conceptualized in terms of return on investment (i.e., how does the cost of CHW salaries, benefits, and supervision compare to costs saved through reduced health care services use?), and MCOs may be developing CHW salary scales based on this approach. If so, they would be wise to consider that much of the value CHWs bring in terms of addressing health related service needs issues (e.g., education, housing, food, transportation, re-entry) for individuals and families may not immediately be reflected in healthcare costs. As health financing reform shifts risk to providers and drives care “upstream,” equitable compensation for CHWs, reflecting their value in addressing social determinants of health and promoting health equity, should be considered a prudent investment. Fair compensation may also be an important step toward addressing the inherent power differential between CHWs and clinically trained providers.
In addition to concerns about salaries, health plans should make efforts to address the substantial proportion of CHWs and supervisors who do not perceive that CHWs have opportunities for promotion. It is worth noting that CHWs are largely being supervised by people who are not CHWs, and likely do not have experience in the field. MCOs might consider collaborating with CHWs to develop career pathways (e.g., promotion to CHW supervision or program management) to ensure that CHWs do not perceive themselves to be in “dead end” jobs.
This study has several limitations. Because it is a cross sectional study, it is not possible to draw causal inferences. The sample size is also relatively small. Due to the survey distribution method (i.e., requesting that CHW networks share the survey with their members), it is not possible to calculate a response rate because we cannot ascertain the number of CHWs who received the survey and met the inclusion criteria. There may also be some selection bias if the group that was most likely to receive the survey—those who are members of a professional network—has different characteristics than those unaffiliated with CHW networks. Statistical testing to assess differences between supervisors and CHWs was not conducted because members of each group did necessarily work at the same organizations (i.e., the supervisors who responded may not have supervised the CHWs who did). Furthermore, CHWs and supervisors are substantially different and would reasonably be expected to have different perspectives. Despite these limitations, the sample was nationally representative, and it sheds light on a topic that is under-studied.
Overall, CHWs roles in MCOs appear to focus on supporting clinical care and making referrals for social issues, rather than addressing community-level concerns. Health plans should ensure that CHWs have the professional freedom to develop community-based solutions to common social needs. MCOs should also ensure that CHWs receive equitable compensation and ensure that CHWs have opportunities for promotion.
The datasets presented in this article are not readily available to protect the confidentiality of participants. Requests to access the datasets should be directed to YXdlbm5lQGxzdWhzYy5lZHU=.
The studies involving human participants were reviewed and approved by LSU Health Sciences Center—New Orleans IRB. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AW: conceptualization, methodology, investigation, formal analysis, writing—original draft, and funding acquisition. CH and GW: conceptualization, methodology, and data curation. DS: conceptualization, methodology, data curation, and writing—review and editing. DJ: data curation, writing—original draft, and writing—review and editing. CR: conceptualization, data curation, and writing—review and editing. All authors contributed to the article and approved the submitted version.
This research was funded by the Robert Wood Johnson Foundation Research in Transforming Health and Health Care Systems Program (grant number 77255), administered by Academy Health.
The authors are grateful to the community health worker networks that distributed the survey.
CR was employed by Community Resources, LLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. American Public Health Association. Support for Community Health Workers to Increase Health Access and Reduce Health Inequities. (2009). Available online at: https://www.apha.org/Policies-and-Advocacy/Public-Health-Policy-Statements/Policy-Database/2014/07/09/14/19/Support-for-Community-Health-Workers-to-Increase-Health-Access-and-to-Reduce-Health-Inequities (accessed September 12, 2022).
2. Pérez LM, Martinez J. Community health workers: social justice and policy advocates for community health and well-being. Am J Public Health. (2008) 98:11–4. doi: 10.2105/AJPH.2006.100842
3. Sabo S, Ingram M, Reinschmidt KM, Schachter K, Jacobs L, Guernsey de. Zapien J, et al. Predictors and a framework for fostering community advocacy as a community health worker core function to eliminate health disparities. Am J Public Health. (2013) 103:e67–73. doi: 10.2105/AJPH.2012.301108
4. Witmer A, Seifer SD, Finocchio L, Leslie J, O'Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. (1995) 85:1055–8. doi: 10.2105/AJPH.85.8_Pt_1.1055
5. Brownstein JN, Hirsch GR, Rosenthal EL, Rush CH. Community health workers “101” for primary care providers and other stakeholders in health care systems. J Ambul Care Manage. (2011) 34:210–20. doi: 10.1097/JAC.0b013e31821c645d
6. Community Health Worker Core Consensus Project. C3 Project Findings: Roles and Competencies. (2013). Available online at: https://www.c3project.org/roles-competencies (accessed September 12, 2022).
7. United States Bureau of Labor Statistics. Occupational Employment and Wage Statistics. (2021). Available online at: https://www.bls.gov/oes/current/oes211094.htm (accessed September 12, 2022).
8. Community Preventive Services Task Force,. The Community Guide. Diabetes Management: Interventions Engaging Community Health Workers. (2017). Available online at: https://www.thecommunityguide.org/findings/diabetes-management-interventions-engaging-community-health-workers (accessed September 12, 2022).
9. Kangovi S, Mitra N, Grande D, Huo H, Smith RA, Long JA. Community health worker support for disadvantaged patients with multiple chronic diseases: a randomized clinical trial. Am J Public Health. (2017) 107:1660–7. doi: 10.2105/AJPH.2017.303985
10. Wennerstrom A, Bui T, Harden-Barrios J, Price-Haywood EG. Integrating community health workers into a patient-centered medical home to support disease self-management among Vietnamese Americans: lessons learned. Health Promot Pract. (2015) 16:72–83. doi: 10.1177/1524839914547760
11. Findley S, Matos S, Hicks A, Chang J, Reich D. Community health worker integration into the health care team accomplishes the triple aim in a patient-centered medical home: a Bronx tale. J Ambul Care Manage. (2014) 37:82–91. doi: 10.1097/JAC.0000000000000011
12. Burns ME, Galbraith AA, Ross-Degnan D, Balaban RB. Feasibility and evaluation of a pilot community health worker intervention to reduce hospital readmissions. Int J Qual Health Care. (2014) 26:358–65. doi: 10.1093/intqhc/mzu046
13. Day T, Bir A, Smith K, Kahwati L, Derzon J, Freeman N, et al. Health Care Innovation Awards (HCIA) Meta-Analysis and Evaluators Collaborative Annual report Year 3. (2018). North Carolina: RTI International.
14. Payne J, Razi S, Emery K, Quattrone W, Tardif-Douglin M. Integrating Community Health Workers (CHWs) into Health Care Organizations. J Community Health. (2017) 42:983–90. doi: 10.1007/s10900-017-0345-4
15. McCarville EE, Martin MA, Pratap PL, Pinkser E, Seweryn SM, Peters KE. Framing the integration of community health workers into health care systems along health care and community spectrums. J Ambul Care Manage. (2021) 44:271–80. doi: 10.1097/JAC.0000000000000396
16. Rogers EA, Manser ST, Cleary J, Joseph AM, Harwood EM, Call KT. Integrating community health workers into medical homes. Ann Fam Med. (2018) 16:14–20. doi: 10.1370/afm.2171
17. Malcarney MB, Pittman P, Quigley L, Horton K, Seiler N. The changing roles of community health workers. Health Serv Res. (2017) 52:360–82. doi: 10.1111/1475-6773.12657
18. Kaiser Family Foundation,. Survey of Medicaid Managed Care Plans. (2017). Available online at: https://files.kff.org/attachment/Report-Medicaid-Managed-Care-March-Plans-and-Access-to-Care (accessed September 12, 2022).
19. Medicaid, Managed Care,. Managed Care Centers for Medicare and Medicaid Services. Available online at: https://www.medicaid.gov/medicaid/managed-care/index.html (accessed September 12, 2022).
20. Brown 3rd HS, Wilson KJ, Pagán JA, Arcari CM, Martinez M, Smith K, et al. Cost-effectiveness analysis of a community health worker intervention for low-income Hispanic adults with diabetes. Prev Chronic Dis. (2012) 9:E140. doi: 10.5888/pcd9.120074
21. Felix HC, Mays GP, Stewart MK, Cottoms N, Olson M. The Care Span: Medicaid savings resulted when community health workers matched those with needs to home and community care. Health Aff (Millwood). (2011) 30:1366–74. doi: 10.1377/hlthaff.2011.0150
22. Johnson D, Saavedra P, Sun E, Stageman A, Grovet D, Alfero C, et al. Community health workers and medicaid managed care in New Mexico. J Community Health. (2012) 37:563–71. doi: 10.1007/s10900-011-9484-1
23. Moffett ML, Kaufman A, Bazemore A. Community health workers bring cost savings to patient-centered medical homes. J Community Health. (2018) 43:1–3. doi: 10.1007/s10900-017-0403-y
24. Kaiser Family Foundation,. 10 Things to Know About Medicaid Managed Care. (2022). Available online at: https://www.kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-managed-care/ (accessed September 12, 2022).
25. Commonwealth Fund,. How New Mexico's Community Health Workers are Helping to Meet Patients' Needs. (2020). Available online at: https://www.commonwealthfund.org/publications/case-study/2020/feb/new-mexico-community-health-workers (accessed September 12, 2022).
26. Paulson CA, Durazo EM, Purry LD, Covington AE, Bob BA, Peters RA, et al. Adding a seat at the table: a case study of the provider's perspective on integrating community health workers at provider practices in California. Front Public Health. (2021) 9:690067. doi: 10.3389/fpubh.2021.690067
27. Sabo S, Wexler N, O'Meara L, Dreifuss H, Soto Y, Redondo F, et al. Organizational readiness for community health worker workforce integration among medicaid contracted health plans and provider networks: an Arizona case study. Front Public Health. (2021) 9:601908. doi: 10.3389/fpubh.2021.601908
28. George R, Gunn R, Wiggins N, Rowland R, Davis MM, Maes K, et al. Early lessons and strategies from statewide efforts to integrate community health workers into medicaid. J Health Care Poor Underserved. (2020) 31:845–58. doi: 10.1353/hpu.2020.0064
29. Brown O, Kangovi S, Wiggins N, Alvarado CS. Supervision Strategies and Community Health Worker Effectiveness in Health Care Settings NAM Perspect. Washington, DC: National Academy of Medicine (2020).
30. Sabo S, Allen CG, Sutkowi K, Wennerstrom A. Community health workers in the United States: challenges in identifying, surveying, and supporting the workforce. Am J Public Health. (2017) 107:1964–9. doi: 10.2105/AJPH.2017.304096
31. Sugarman M, Ezouah P, Haywood C, Wennerstrom A. Promoting community health worker leadership in policy development: results from a louisiana workforce study. J Community Health. (2021) 46:64–74. doi: 10.1007/s10900-020-00843-7
32. Sabo S, Wennerstrom A, Phillips D, Haywoord C, Redondo F, Bell ML, et al. Community health worker professional advocacy: voices of action from the 2014 national community health worker advocacy survey. J Ambul Care Manage. (2015) 38:225–35. doi: 10.1097/JAC.0000000000000089
Keywords: community health workers (CHWs), Medicaid, managed care organization (MCO), integration, social determinants of health
Citation: Wennerstrom A, Haywood CG, Smith DO, Jindal D, Rush C and Wilkinson GW (2023) Community health worker team integration in Medicaid managed care: Insights from a national study. Front. Public Health 10:1042750. doi: 10.3389/fpubh.2022.1042750
Received: 12 September 2022; Accepted: 21 December 2022;
Published: 13 January 2023.
Edited by:
E. Lee Rosenthal, Texas Tech University Health Sciences Center El Paso, United StatesReviewed by:
Limei Jing, Shanghai University of Traditional Chinese Medicine, ChinaCopyright © 2023 Wennerstrom, Haywood, Smith, Jindal, Rush and Wilkinson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashley Wennerstrom,  YXdlbm5lQGxzdWhzYy5lZHU=
YXdlbm5lQGxzdWhzYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.