
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 12 January 2023
Sec. Digital Public Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1042167
Objective: This study aimed to assess changes in joint range of motion (ROM) and knee joint function between patients who received the mobile health-based intervention and those who received regular care at 2 and 6 weeks after anterior cruciate ligament (ACL) reconstruction to provide better interventions in the future.
Methods: Patients who underwent ACL reconstruction were randomized into the experimental [Mobile health-based intervention (MHI); n = 62] and control (CON) groups (n = 63). The CON group underwent home-based rehabilitation exercise following the paper rehabilitation schedule, while the intervention group received additional mobile health-based education at weeks 1–6 after surgery. ROM, thigh circumference difference, and flexion pain were the primary outcomes. The secondary outcomes were the international knee documentation committee knee evaluation form (IKDC) scores and rehabilitation compliance scores. All the outcomes were measured 1 day before surgery as references and at 2 and 6 weeks after surgery.
Results: There was no statistical difference in the patients' ROM, thigh circumference difference, and VAS scores at the 2-week follow-up. At the 6-week follow-up, the ROM of the affected leg was (118.1 ± 20.5)° in the CON group and (126.6 ± 20.5)° in the MHI group, and the difference was statistically significant (P = 0.011). The difference in thigh circumference was 3.0 (2.0, 3.5) cm in the CON group and 2.5 (1.0, 3.0) cm in the MHI group. The difference was statistically significant (P < 0.001). The VAS score in the CON group was 3.0 (2.0, 4.0), and the MHI group was 2.5 (1.0, 3.0). The difference was statistically significant (P < 0.05). At the 6-week follow-up, the compliance score of patients in the MHI group was significantly higher than that in the CON group (P = 0.047, β = 2.243, 95%CI: 0.026–4.459). There is no statistically significant difference in IKDC scores.
Conclusion: Mobile health-based intervention positively affected patients undergoing ACL reconstruction surgery, particularly in improving the clinical outcome indicators of the knee joint.
• The rehabilitation management of patients after ACL reconstruction can be implemented according to the Health belief model.
• Mobile health-based intervention can improve patients' knee function, muscle atrophy, and joint pain by 6 weeks after ACL reconstruction.
• Mobile health-based education further promoted the improvement of clinical indicators but did not significantly improve the subjective results after ACL reconstruction.
With the increase in people's health awareness, more residents are engaged in physical exercise, which has led to annual increases in the incidence of anterior cruciate ligament (ACL) injuries (1, 2). ACL injuries account for about 40% of knee sports injuries (3). ACL reconstruction has been proven to be the best treatment for ACL injuries (3). Postoperative rehabilitation requires frequent physiotherapy sessions for both therapy and education (4). To ensure the functional rehabilitation of the knee joint after the operation, make the patient reach the rehabilitation goal according to the plan, and reduce the risk of the second operation, it is essential to guide the patient to carry out the proper rehabilitation training (5). However, owing to limited rehabilitation medical resources (6, 7), most patients lack professional rehabilitation guidance after undergoing ACL reconstruction after discharge. Most patients can only refer to the paper rehabilitation schedule prescribed by the rehabilitation physician after release. This results in poor compliance, making the target results challenging and affecting the patient's quality of life (8).
Mobile health (mHealth) facilities (smartphone-based educational apps, web-based tools, SMS text messaging, PDA physiological status monitoring, and connected captors) have been widely proven to be effective interventions in different health areas, which can realize the transition from “one-to-one” to “one-to-many” for doctors and patients (9, 10), making management more time-effective. And with the development of Internet technology, personalized management of patients has gradually become possible. MHealth-based education has been widely used in different health fields, such as managing behaviors in patients with chronic diseases (11, 12) and improving patient compliance after discharge (13, 14). Mhealth has also been applied to the out-of-hospital rehabilitation management of patients with sports injuries (15). Therefore, mHealth rehabilitation intervention may be more effective than traditional care. Mhealth intervention also provides new ideas to ensure rehabilitation in outpatients under the normalized management of coronavirus disease, reducing the risk of cross-infection in hospitals. Limited by evidence, whether mHealth-based education can reduce the burden of rehabilitation physicians and effectively improve the process and results of patient rehabilitation remains to be elucidated.
Regarding intervention content, the Health belief model (HBM) is one of the most widely used theories to examine the barriers and foundation of individual participation in programs that focus on preventing diseases and promoting healthy lifestyles (16). HBM enables the prediction of behaviors according to constructs consisting of perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy (17) and has been proven efficient in standardizing the rehabilitation exercise after hemodialysis (18), assisting patients with knee joint fractures to recover at home after surgery (17). Therefore, education strategies that the health belief model guides may be more effective than conventional interventions.
Therefore, the researchers have developed a mHealth-based intervention applet [MHI; “Rehabilitation Cloud Platform” (Beijing QianriQianyue Technology Ltd.)] for patients. The intervention content of the applet is designed based on HBM. This randomized controlled study aimed to compare the changes in knee joint clinical and subjective functional indicators in the MHI and the CON groups at 2 and 6 weeks after ACL reconstruction. This study hypothesized that a mobile health intervention would be more beneficial to the early recovery of patients after ACL reconstruction.
This is a randomized controlled trial in which patients were tested 1 day before surgery and 2 and 6 weeks after surgery. The patients were individually randomized to one of two parallel groups in a 1:1 ratio to receive either conventional or conventional care plus mHealth-based intervention. Physiotherapists divided the patients into two parallel groups according to the grouping tool designed by the statistician, who was not involved in the data collection. Group allocation was completed before surgery. Except for the physiotherapists administering the treatment, the patients and data collectors were blinded to the patients' group assignments.
Patients awaiting ACL reconstruction were recruited at Peking university third hospital from April 2019 to December 2019 under the direction of five orthopedic surgeons. The inclusion criteria were as follows: (1) age between 18 and 60 years; (2) isolated ACL reconstruction for the first time, which can be combined with cartilage injury and partial meniscus resection; (3) a consistent postoperative recovery plan; (4) essential reading and writing skills and no communication problems; (5) ability to use smartphones with WeChat installed. The patient exclusion criteria were as follows: (1) the previous history of joint infection, joint tuberculosis or osteomyelitis, or lower limb surgery within 6 months; (2) severe heart, brain, kidney, and other organ dysfunctions; (3) combined with other severe knee joint diseases and injuries; (4) patients with mental illness or cognitive impairment; (5) transfer to other medical institutions after discharge.
The pre- and post-injury physical activity levels were determined using the ROM.
All the ACL reconstructions for patients enrolled in the study were performed via anteromedial portal with autogenously hamstring single-bundle reconstruction. The femoral side of the autograft was fixated with Endobutton (Smith and Nephew, USA), and the tibial side was fixated to the tibial tunnel with Intrafifix (Smith and Nephew, USA).
In the CON group, patients were given a paper version of the rehabilitation plan before they were discharged from the hospital. A brief explanation was given to explain the plan and answer any related questions from the patients. The length of the explanation depended on the patient's level of understanding and was usually 5–10 min. After discharge from the hospital, the patients conducted rehabilitation training according to the plan, without any visits to other institutions or inpatient treatment. The control group could only use the data measurement function in the “Rehabilitation Cloud Platform” and could not use the rehabilitation instruction function, thus avoiding contamination in the control group.
In the MHI group, the mHealth intervention included these contents: sports medicine doctors will teach the patient how to properly use the “Rehabilitation Cloud Platform” the day before their surgery. The teaching included measuring data such as angle and circumference and how to view the rehabilitation guidance content. The platform then informs the patient before surgery about the knowledge related to the surgery and the importance of rehabilitation. In the home-based rehabilitation stage, the platform will remind the patient to complete their rehabilitation plan and explain the details of the plan for their reference. Patients can upload relevant data according to their needs and the platform's suggestions. The platform can provide feedback instructions to patients according to their uploaded data and suggest whether they should seek medical treatment in time.
In addition, the contact information of the doctor is also provided on the platform. If patients have questions about the teaching content in the platform, they can ask the doctor through the platform. The doctor would review and respond timely. The settings and content of the “Rehabilitation Cloud Platform” are shown in Figure 1 and Table 1, and the data collection system is shown in Figure 2.

Figure 1. Function settings of the “Rhabilitation Cloud Platform.” The figure shows the four functions of the “Rhabilitation Cloud Platform” and their detailed introduction.

Figure 2. Data collection interface of the “Rhabilitation Cloud Platform.” (A) After the patient uploads the photo, the platform can automatically measure the ROM; (B) Patients can record the VAS score of knee flexion pain through the platform; (C) Patients can record the thigh circumference through the platform.
The primary outcomes were ROM, the difference in thigh circumference, and the visual analog scale (VAS) score. Knee ROM (degrees) was assessed using the goniometer tool of the “Rehabilitation Cloud Platform,” with the participant lying supine following the previous procedures (19). ROM was measured before the operation and at 2 and 6 weeks postoperatively. The subjects were allowed a 3-min warm-up, which consisted of self-stretching within their available ROM. Knee extension measurements were taken with a towel roll under the heel of the involved extremity. Goniometric results measured with smartphone-based digital photography have been proven efficient in assessing joint function post-surgery (20, 21). The rehabilitation physician measured and recorded the difference in thigh circumference and the VAS score.
The secondary outcomes were the IKDC score and rehabilitation compliance score. The online questionnaire on the “Rehabilitation Cloud Platform” was used for measurement.
The IKDC scale consists of 10 items on knee joint function and 8 items on knee ligament examination, including joint pain, exercise level, and daily activity ability, with a total score of 0–100. A higher score indicates better joint function. The IKDC scale is reliable, valid, and sensitive to changes in the joint functions of patients who underwent ACL reconstruction (22). The IKDC questionnaire is also always utilized in ACL research and is easier to complete and understand than other questionnaires (23, 24).
The rehabilitation compliance scale was compiled according to the content of the patient's rehabilitation schedule (2019 version) after ACL reconstruction in the sports medicine department of Peking university third hospital. According to the actual degree of completion of the patients' home rehabilitation training, a 5-point Likert scale was used for classification and scoring, with scores ranging from 1 (totally disagree) to 5 (totally agree) for each item, including ankle pump training, muscle contraction training, leg lifting, stretching and bending, ice regimen, and brace wearing.
ROM was used as the primary outcome, and the attainment value of ROM at 6 weeks was 120°, referring to the patient's rehabilitation schedule (2019 version) after ACL reconstruction in the sports medicine department of Peking university third hospital. Previous studies have mostly grouped knee joints at a group distance of 10° when evaluating their functional status (25). Therefore, our study assumed a 10° difference between the two groups at 6 weeks and a degree of 125° for patients in the MHI group and 115° for patients in the CON group. Referring to the results of van der List and DiFelice GS (26), the standard deviation was set at 15° for both groups, with a significance level α of 0.05 and 1- β of 0.90. The study was a randomized controlled trial (RCT). The ratio of the number of people in the two groups was 1:1. Calculations were performed according to the formula.
The sample size of each group was calculated to be 48. Considering that the rate of missing secondary follow-up was about 20%, the total sample size was set to 120.
The data in the text and figures are presented as the mean (SD) or median (interquartile range). A modified intention-to-treat analysis was performed that included all patients who were randomized for treatment and attended at least two test sessions. Normality was checked for each variable. The group characteristics of the two groups were compared with a t-test when measured using a parametric variable and with the Kruskal–Wallis and chi-square tests when measured using non-parametric and count variables, respectively.
The subjective outcomes were analyzed using a multilevel analysis (SPSS version 24). A random intercept and slope model were used where repeated measurements (level 1) were nested within individual patients who underwent ACL reconstruction (level 2). After that, the following explanatory variables were added to the model: group [MHI and CON (as reference)], time [before surgery (as reference) and 2 and 6 weeks after surgery], and group-by-time interaction. The parameters of the multilevel model were estimated using the maximum-likelihood method. Only models with significantly better log-likelihood values were retained. The secondary outcomes were separately analyzed for the questionnaire and clinical indexes.
Additional multilevel analyses were performed to examine whether sex, BMI, ROM of the non-injured leg, and age affected the recovery after ACL surgery. The multilevel model was identical to the model mentioned above, with the exception that the explanatory variable group was replaced by sex (male or female), BMI (normal, underweight, overweight, or obese), and age (old or young). For age, the patients in the old group were ≥ 30 years old, and those in the young group were < 30 years old. The BMI was < 24 kg/m2 in the regular or underweight group, 24 to 28 kg/m2 in the overweight group, and ≥ 28 kg/m2 (Chinese standard) in the obese group. The target outcomes were the compliance score, VAS score, and the difference in thigh circumference. Cohen's d and 95% confidence intervals (CI) were calculated for significant effects. The level of significance (α) was set at P < 0.05.
The study protocol was approved by the Ethics Committee of Peking University Third Hospital, authorization number M2019069, and was registered at ClinicalTrials.gov (NCT03890848). In addition, all participants signed an informed consent form. This study conforms to all Consolidated Standards of Reporting Trial guidelines and reports the required information accordingly.
This study was conducted by sequential enrollment. A total of 125 study subjects were included at baseline, 63 in the control group and 62 in the intervention group. The flow of the participants is shown in Figure 3. Table 2 shows the group characteristics of the patients included in the final analysis.
At the 2-week follow-up, the qualified rates of ROM in the CON group and MHI group were 40.0 and 47.3%, and the angles were (83.8 ± 16.4)° and (86.6 ± 15.8)°, respectively. The MHI group was slightly higher, but no statistical difference (P = 0.361).
At the 6-week follow-up, the qualified rate of ROM in the CON group and the MHI group were 42.6 and 67.3%, respectively, which was statistically different (P = 0.008). The angle in the CON group was (118.1 ± 20.5)°, and the angle in the MHI group was (126.6 ± 13.0)°, which was statistically significant (P = 0.011).
At the 2-week follow-up, the difference in thigh circumference was 2.0 (1.0, 2.5) cm in the CON group and 1.5 (1.0, 2.5) cm in the MHI group, and the difference between the two groups was not statistically significant (P = 0.592). The difference in thigh circumference of the two groups at 2 weeks was higher than before the operation, and there was no statistical difference between the changes in the two groups (P = 0.421).
At the 6-week follow-up, the difference in thigh circumference was 3.0 (2.0, 3.5) cm in the CON group and 2.5 (1.0, 3.0) cm in the MHI group, and the difference was statistically significant (P < 0.001). The difference in thigh circumference at the 6-week follow-up was still higher than that at the 2-week follow-up, and there was a statistical difference in the change in the difference between the two groups (P = 0.038). See Figure 4 for details.
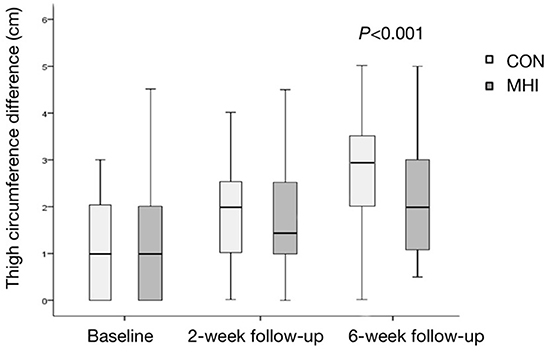
Figure 4. Box plot of thigh circumference difference. At the 6-week follow-up, the difference between the MHI and CON groups was statistically significant (P < 0.001). The difference in thigh circumference was more negligible in the MHI group, implying better rehabilitation.
At the 2-week follow-up, the VAS score was 4.0 (3.0, 5.0) in the CON group and 3.0 (3.0, 4.0) in the MHI group. The difference between the two groups was not statistically significant (P = 0.435). Compared with the baseline, the VAS scores of the two groups increased at 2 weeks, and there was no statistical difference between the increase in the two groups (P = 0.181).
At the 6-week follow-up, the VAS score was 3.0 (2.0, 4.0) in the CON group and 2.5 (1.0, 3.0) in the MHI group. The difference was statistically significant (P = 0.044). Compared with the 2 weeks, the pain of the two groups was alleviated at 6 weeks, and the change of VAS score between the two groups was not statistically different (P = 0.312). See Figure 5 for details.
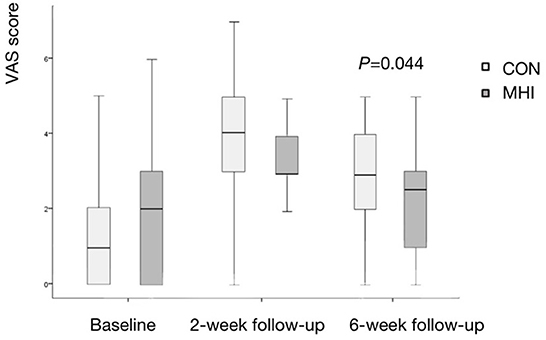
Figure 5. Box plot of VAS score. The difference between the MHI and CON groups was statistically significant at the 6-week follow-up. Less pain in the MHI group was detected, which means better recovery.
There were no statistically significant differences in IKDC scores and compliance scores between the CON group and the MHI group at 2 and 6 weeks of follow-up. A paired t-test for 6 weeks and 2 weeks showed that the compliance score of the CON group decreased by 1.4 ± 5.0, and the change in the MHI group was not statistically significant. Through the generalized linear model, after adjusting for age, gender, BMI, education level, and monthly income, it was found that the compliance score of patients in the MHI group was significantly higher than that in the CON group (P = 0.047, β = 2.243, 95%CI: 0.026–4.459 ), see Table 3 for details.
The immobilization was stable for 6 weeks after reconstruction, and no ligament laxity was found. At 6 weeks, the researchers conducted Lachman tests on the patients, and the results were all negative. No significant deep vein thrombosis (DVT) was observed in the patients owing to frequent postoperative ankle pump exercises. All the wounds healed in grade A. Twelve patients (23.1%) in the CON group were reported to have received additional guidance from the rehabilitation institution, which was 18 (33.3%) in the intervention group, showing no statistically significant difference (χ2 =1.37, P = 0.24). Within 6 weeks, the frequencies of visits in the CON and MHI groups were 13.8 (9.3) and 9.7 (8.6), respectively, without statistically significant differences between the two groups (T = 0.86, P = 0.41).
The primary finding of the present study was that for the primary endpoint of objective outcome based on knee joint function, Mhealth-based education had superior outcomes to the traditional paper schedule at 6 weeks.
Compared with those at 2-week follow-up, the significant and clinically important improvements in all the measures of knee function at 6 weeks that were observed in both the MHI and CON groups are in line with recent literature in patients who underwent ACL reconstruction (17, 27). Studies have shown that ROM is closely related to daily activity needs. Patients can meet the minimum standard of daily activities when they reach ≥90° (ROM) and can easily squat down when the ROM is > 120° (28). The earlier the patients are provided help to achieve greater ROM, the more patients will experience improvements in quality of life and satisfaction (29–31). In the present study, the ROM in the MHI group was slightly higher than that in the CON group at 2-week follow-up after reconstruction, and the values were similar to those in previous studies (32, 33), but the difference was not statistically significant. By 6 weeks, a more remarkable improvement in ROM was observed in the MHI group than in the CON group, similar to the results of a previous study (31). This is mainly related to the following two factors: First, the content of the patient's training 1 week after reconstruction was the basic training, and the content was increased after that. The patients in the MHI group had access to more engaging and varied instruction, such as pictures, videos and audio. Second, as time passed, the patients' attention to rehabilitation training showed a downward trend, and psychological barriers gradually increased, as demonstrated in previous studies (34, 35). At this time, timely mHealth-education and prescription could motivate patients to maintain relatively high compliance to achieve better rehabilitation effects.
The degree of atrophy of the quadriceps femoris (QF) muscle is recognized as one of the critical factors of poor knee function despite successful ACL reconstruction (36). The QF muscle activity is reduced due to problems such as limited knee flexion after ACL reconstruction. Meanwhile, skeletal muscle and ligament injuries cause a shortage of oxygen supply and damage to the adjacent capillaries, which leads to QF atrophy (37, 38). Previous studies showed an interaction between joint pain and QF atrophy, which might worsen with each other (39, 40). In the present study, the patients who underwent MHI received frequent training reminders, which led to better performance in reducing QF atrophy. The reduction in QF atrophy with greater pain reduction may have contributed to a greater improvement in ROM (41). No related complications were found between the two groups, and no statistically significant differences in the number and frequency of extra visits to medical institutions were observed.
Flexion pain after surgery is one of the essential reasons for patient dissatisfaction and increased incidence of secondary surgery, and standardized training plays an irreplaceable role in pain relief (42). Normative training can improve the medial femoral track and correct the abnormal patellofemoral joint, thus reducing patellofemoral pain syndrome (43). Another way to reduce postoperative flexion pain is to use an intensive icing regimen (44, 45). The two important aspects of the MHI were to offer normative training guidance and a timely icing regimen reminder, which contributed to the more significant reductions in flexion pain in the MHI group, ensuring that patients could normally train as expected. In addition, detailed surgical introduction, rehabilitation case sharing, and training guidance can enhance patients' perceptions of the training intensity, thus reducing patients' fear avoidance and ensuring a good target-reach rate, similar to a previous study (46).
At 2 and 6 weeks after surgery, the IKDC score in the MHI group was slightly higher than in the CON group, but the difference was not statistically significant. The scores in both groups improved, but the difference between the two groups decreased. In addition, all the patients who underwent ACL reconstruction at Peking University Hospital received detailed explanations on how to deal with pain at the time of discharge from the hospital. The pain levels of the patients were kept low. At the same time, in this study, the process of isolated ACL reconstruction was unified and standardized, and the wound healing of the patients was good, without complications during the 6-week follow-up, so no significant difference was found in the activities that could be performed. These results might explain why the two groups had no statistically significant difference in IKDC scores.
Regarding compliance, no significant difference was found in the scores between the two groups, which might indicate that within 6 weeks after the operation, all the patients could undergo rehabilitation training on time, following the rehabilitation plan. However, the understanding and standardization of specific actions showed differences, which led to differences in the clinical index.
This study focused on early knee function in patients who underwent ACL reconstruction, and its long-term impact remains to be further investigated. Owing to the late opening of the browsing record collection function, the Mhealth platform's usage record is not yet complete, so further evaluation of the patients' usage will be considered in the next step. Mhealth intervention requires patients to learn to use smartphones and corresponding software, so promotion has certain limitations. Considering this factor, in the later stage, you can consider adding an education column for caregivers in the mHealth platform and implementing interventions by intervening with caregivers.
Standardized rehabilitation exercises after surgery improved knee joint function and reduced muscle atrophy and flexion pain. Mhealth-based education further promoted the improvement of clinical indicators but did not significantly improve the subjective results after ACL reconstruction.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Peking University Third Hospital Medical Science Research Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
YG and DL were involved in data analysis and data interpretation. X-yS designed the study. All authors were involved in data collection and analysis as well as the write-up of the final manuscript.
This work was supported by 2018 (2018YFF0301100) and 2019 (2019YFF0302305) Nation Key Research and Development Program for Science and Technology Winter Olympics of China and Integrated application of technology and comprehensive demonstration Project of Scientific and Technological Winter Olympics of Zhangjiakou in 2020 (20110004D).
We thank the Department of Sports Medicine, Peking University Third Hospital, for assistance in data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002-2014. Sports Health. (2018) 10:523–31. doi: 10.1177/1941738118803616
2. Sanders TL, Kremers HM, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am J Sports Med. (2016) 44:1502–7. doi: 10.1177/0363546516629944
3. Lam M-H, Fong DT, Yung PS, Ho EP, Chan W-Y, Chan K-M. Knee stability assessment on anterior cruciate ligament injury: clinical and biomechanical approaches. Sports Med Arthrosc Rehabil Ther Technol. (2009) 1:20. doi: 10.1186/1758-2555-1-20
4. Shen X, Qin Y, Zuo J, Liu T, Xiao J. A systematic review of risk factors for anterior cruciate ligament reconstruction failure. Int J Sports Med. (2021) 42:682–93. doi: 10.1055/a-1393-6282
5. Beynnon BD, Fleming BC, Johnson RJ, Nichols CE, Renström PA, Pope MH, et al. Anterior cruciate ligament strain behavior during rehabilitation exercises in-vivo. Am J Sports Med. (1995) 23:24–34. doi: 10.1177/036354659502300105
6. Kong X, Ai B, Kong Y, Su L, Ning Y, Howard N, et al. Artificial intelligence: a key to relieve China's insufficient and unequally distributed medical resources. Am J Transl Res. (2019) 11:2632–40.
7. Chai K, Zhang Y, Chang K. Regional disparity of medical resources and its effect on mortality rates in China. Front Public Health. (2020) 8:8. doi: 10.3389/fpubh.2020.00008
8. Lee ASY, Yung PS, Mok KM, Hagger MS, Chan DKC. Psychological processes of ACL-patients' post-surgery rehabilitation: a prospective test of an integrated theoretical model. Soc Sci Med. (2020) 244:112646. doi: 10.1016/j.socscimed.2019.112646
9. Cheung K, Ling W, Karr CJ, Weingardt K, Schueller SM, Mohr DC. Evaluation of a recommender app for apps for the treatment of depression and anxiety: an analysis of longitudinal user engagement. J Am Med Inform Assoc. (2018) 25:955–62. doi: 10.1093/jamia/ocy023
10. Wei X, Hicks JP, Pasang P, Zhang Z, Haldane V, Liu X, et al. Protocol for a randomised controlled trial to evaluate the effectiveness of improving tuberculosis patients' treatment adherence via electronic monitors and an app versus usual care in Tibet. Trials. (2019) 20:273. doi: 10.1186/s13063-019-3364-x
11. Chao DY, Lin TM, Ma WY. Enhanced self-efficacy and behavioral changes among patients with diabetes: cloud-based mobile health platform and mobile app service. JMIR Diabetes. (2019) 4:e11017. doi: 10.2196/11017
12. Kang H, Park HA, A. Mobile app for hypertension management based on clinical practice guidelines: development and deployment. JMIR Mhealth Uhealth. (2016) 4:e12. doi: 10.2196/mhealth.4966
13. Timmers T, Janssen L, van der Weegen W, Das D, Marijnissen W-J, Hannink G, et al. The effect of an app for day-to-day postoperative care education on patients with total knee replacement: randomized controlled trial. JMIR Mhealth Uhealth. (2019) 7:e15323. doi: 10.2196/15323
14. Dong X, Yi X, Gao D, Gao Z, Huang S, Chao M, et al. The effects of the combined exercise intervention based on internet and social media software (CEIBISMS) on quality of life, muscle strength and cardiorespiratory capacity in Chinese postoperative breast cancer patients: a randomized controlled trial. Health Qual Life Outcomes. (2019) 17:109. doi: 10.1186/s12955-019-1183-0
15. Ramey L, Osborne C, Kasitinon D, Juengst S. Apps and mobile health technology in rehabilitation: the good, the bad, and the unknown. Phys Med Rehabil Clin N Am. (2019) 30:485–97. doi: 10.1016/j.pmr.2018.12.001
16. Kahlenberg CA, Lyman S, Joseph AD, Chiu YF, Padgett DE. Comparison of patient-reported outcomes based on implant brand in total knee arthroplasty: a prospective cohort study. Bone Joint J. (2019) 101-B (7_Supple_C):48–54. doi: 10.1302/0301-620X.101B7.BJJ-2018-1382.R1
17. Zhang M. Effect of HBM rehabilitation exercises on depression, anxiety and health belief in elderly patients with osteoporotic fracture. Psychiatr Danub. (2017) 29:466–72. doi: 10.24869/psyd.2017.466
18. Sutherland S, Penfold R, Doherty A, Milne Z, Dawes H, Pugh C, et al. A cross-sectional study exploring levels of physical activity and motivators and barriers towards physical activity in haemodialysis patients to inform intervention development. Disabil Rehabil. (2021) 43:1675–81. doi: 10.1080/09638288.2019.1672214
19. Norkin CC, White JD. Measurement of Joint Motion: A Guide to Goniometry. 3rd ed Philadelphia: FA Davis Co (2003).
20. Meislin MA, Wagner ER, Shin AY. A comparison of elbow range of motion measurements: smartphone-based digital photography versus goniometric measurements. J Hand Surg Am. (2016) 41:510–5. doi: 10.1016/j.jhsa.2016.01.006
21. Pereira LC, Rwakabayiza S, Lécureux E, Jolles BM. Reliability of the knee smartphone-application goniometer in the acute orthopedic setting. J Knee Surg. (2017) 30:223–30. doi: 10.1055/s-0036-1584184
22. Jia ZY, Zhang C, Zou Y, Huang X, Xu WD. Translation and validation of the simplified Chinese version of international knee documentation committee subjective knee Form. Arch Orthop Trauma Surg. (2018) 138:1433–41. doi: 10.1007/s00402-018-2973-2
23. Huang CC, Chen WS, Tsai MW, Wang WT. Comparing the Chinese versions of two knee-specific questionnaires (IKDC and KOOS): reliability, validity, and responsiveness. Health Qual Life Outcomes. (2017) 15:238. doi: 10.1186/s12955-017-0814-6
24. van de Graaf VA, Wolterbeek N, Scholtes VA, Mutsaerts EL, Poolman RW. Reliability and validity of the IKDC, KOOS, and WOMAC for patients with meniscal injuries. Am J Sports Med. (2014) 42:1408–16. doi: 10.1177/0363546514524698
25. Giesche F, Niederer D, Banzer W, Vogt L. Evidence for the effects of prehabilitation before ACL-reconstruction on return to sport-related and self-reported knee function: a systematic review. PLoS ONE. (2020) 15:e0240192. doi: 10.1371/journal.pone.0240192
26. van der List JP, DiFelice GS. Range of motion and complications following primary repair versus reconstruction of the anterior cruciate ligament. Knee. (2017) 24:798–807. doi: 10.1016/j.knee.2017.04.007
27. Shao C, Wang J, Liu J, Tian F, Li H. Effect of a health belief model-based education program on patients' belief, physical activity, and serum uric acid: a randomized controlled trial. Patient Prefer Adherence. (2018) 12:1239–45. doi: 10.2147/PPA.S166523
28. Cavill S, McKenzie K, Munro A, McKeever J, Whelan L, Biggs L, et al. The effect of prehabilitation on the range of motion and functional outcomes in patients following the total knee or hip arthroplasty: a pilot randomized trial. Physiother Theory Pract. (2016) 32:262–70. doi: 10.3109/09593985.2016.1138174
29. Çelik D, Turkel N. The effectiveness of pilates for partial anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. (2017) 25:2357–64. doi: 10.1007/s00167-015-3718-1
30. Kijkunasathian C, Limitlaohaphan C, Saengpetch N, Chanasit P, Sundarathiti P, Waratanarat P, et al. A comparison between modified Robert jones bandage and intermittent cold pack in arthroscopic anterior cruciate ligament reconstruction: a prospective randomized controlled trial. J Med Assoc Thai. (2017) 100:287–94.
31. Filbay SR, Roos EM, Frobell RB, Roemer F, Ranstam J, Lohmander LS. Delaying ACL reconstruction and treating with exercise therapy alone may alter prognostic factors for 5-year outcome: an exploratory analysis of the KANON trial. Br J Sports Med. (2017) 51:1622–9. doi: 10.1136/bjsports-2016-097124
32. Chan MC, Wee JW, Lim MH. Does kinesiology taping improve the early postoperative outcomes in anterior cruciate ligament reconstruction? A randomized controlled study. Clin J Sport Med. (2017) 27:260–5. doi: 10.1097/JSM.0000000000000345
33. Di Martino A, Tentoni F, Di Matteo B, Cavicchioli A, Presti ML, Filardo G, et al. Early viscosupplementation after anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med. (2016) 44:2572–8. doi: 10.1177/0363546516654909
34. Filbay SR, Grindem H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol. (2019) 33:33–47. doi: 10.1016/j.berh.2019.01.018
35. Burland JP, Toonstra JL, Howard JS. Psychosocial barriers after anterior cruciate ligament reconstruction: a clinical review of factors influencing postoperative success. Sports Health. (2019) 11:528–34. doi: 10.1177/1941738119869333
36. Grapar Zargi T, Drobnic M, Jkoder J, Strazar K, Kacin A. The effects of preconditioning with ischemic exercise on quadriceps femoris muscle atrophy following anterior cruciate ligament reconstruction: a quasi-randomized controlled trial. Eur J Phys Rehabil Med. (2016) 52:310–20.
37. Calvani R, Joseph A-M, Adhihetty PJ, Miccheli A, Bossola M, Leeuwenburgh C, et al. Mitochondrial pathways in sarcopenia of aging and disuse muscle atrophy. Biol Chem. (2013) 394:393–414. doi: 10.1515/hsz-2012-0247
38. Powers SK, Wiggs MP, Duarte JA, Zergeroglu AM, Demirel HA. Mitochondrial signaling contributes to the disuse muscle atrophy. Am J Physiol Endocrinol Metab. (2012) 303:E31–9. doi: 10.1152/ajpendo.00609.2011
39. Cai W-S, Li H-H, Konno S-I, Numazaki H, Zhou S-Q, Zhang Y-B, et al. Patellofemoral MRI alterations following single bundle ACL reconstruction with hamstring autografts are associated with quadriceps femoris atrophy. Curr Med Sci. (2019) 39:1029–36. doi: 10.1007/s11596-019-2138-8
40. Weiss K, Whatman C. Biomechanics associated with patellofemoral pain and ACL injuries in sports. Sports Med. (2015) 45:1325–37. doi: 10.1007/s40279-015-0353-4
41. Eckenrode BJ, Carey JL, Sennett BJ, Zgonis MH. Prevention and management of post-operative complications following ACL reconstruction. Curr Rev Musculoskelet Med. (2017) 10:315–21. doi: 10.1007/s12178-017-9427-2
42. Lepley AS, Pietrosimone B, Cormier ML. Quadriceps function, knee pain, and self-reported outcomes in patients with anterior cruciate ligament reconstruction. J Athl Train. (2018) 53:337–46. doi: 10.4085/1062-6050-245-16
43. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A, et al. prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the joint undertaking to monitor and prevent ACL injury (JUMP-ACL) cohort. Am J Sports Med. (2009) 37:2108–16. doi: 10.1177/0363546509337934
44. Ruffilli A, Buda R, Castagnini F, Di Nicolantonio D, Evangelisti G, Giannini S, et al. Temperature-controlled continuous cold flow device versus traditional icing regimen following anterior cruciate ligament reconstruction: a prospective randomized comparative trial. Arch Orthop Trauma Surg. (2015) 135:1405–10. doi: 10.1007/s00402-015-2273-z
45. Daniel DM, Stone ML, Arendt DL. The effect of cold therapy on pain, swelling, and range of motion after anterior cruciate ligament reconstructive surgery. Arthroscopy. (1994) 10:530–3. doi: 10.1016/S0749-8063(05)80008-8
Keywords: anterior cruciate ligament reconstruction, health education, knee function, mobile health (mHealth), health belief model, structural equation model (SEM)
Citation: Guo Y, Li D, Wu Y-b, Sun X, Sun X-y and Yang Y-p (2023) Mobile health-based home rehabilitation education improving early outcomes after anterior cruciate ligament reconstruction: A randomized controlled clinical trial. Front. Public Health 10:1042167. doi: 10.3389/fpubh.2022.1042167
Received: 12 September 2022; Accepted: 21 December 2022;
Published: 12 January 2023.
Edited by:
Liang-Tseng Kuo, Chiayi Chang Gung Memorial Hospital, TaiwanReviewed by:
Shangmin Chen, Shantou University, ChinaCopyright © 2023 Guo, Li, Wu, Sun, Sun and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin-ying Sun,  WHlzdW5AYmptdS5lZHUuY24=; Yu-ping Yang,
WHlzdW5AYmptdS5lZHUuY24=; Yu-ping Yang,  eXl5eXBwdmlwQHNpbmEuY29t
eXl5eXBwdmlwQHNpbmEuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.