
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 12 December 2022
Sec. Occupational Health and Safety
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1037246
This article is part of the Research TopicEmployee Experience, Occupational Health, and Organizational Supportive Factors: From an Integrated PerspectiveView all 40 articles
 Ling Zhang1†
Ling Zhang1† Siqi Chen2†
Siqi Chen2† Zhuowang Chen2†
Zhuowang Chen2† Wenjun Yin2
Wenjun Yin2 Wenjuan Fu2
Wenjuan Fu2 Fang He2
Fang He2 Zhen Pan2
Zhen Pan2 Guilin Yi2*
Guilin Yi2* Xiaodong Tan1*
Xiaodong Tan1*Background: Occupational noise is one of the most common and prevalent occupational hazards worldwide and may induce adverse auditory and/or non-auditory health effects. However, the relationship between occupational noise exposure and hypertension is controversial and has long been debated.
Methods: Based on large sample cross-sectional data from all registered occupational health examination units from 2021 to 2022 (N = 101,605), this study aimed to analyze the prevalence of hearing loss and hypertension and to explore the influencing factors of hypertension of workers in Wuhan. Descriptive statistics, univariate analyses and multivariate analyses were used. Forest plot and nomograms were constructed for the visualization of predictive results. The ROC curve, AUC, C-index and calibration curves were used to assess the predictive accuracy and validity. DCA was performed to evaluate the net benefit that workers could receive.
Results: Higher rate of high-frequency hearing loss (25.3%), speech frequency hearing loss (8.8%), ECG abnormalities (31.9%) and hypertension (21.0%) were found in workers exposed to occupational noise in Wuhan. Occupational noise exposure (OR = 1.09, 95% CI: 1.01–1.18, p = 0.04), growth of age (OR: 1.07, 95% CI: 1.07–1.07, p < 0.001), overweight (OR: 1.82, 95% CI: 1.73–1.92, p < 0.001), obesity (OR: 3.62, 95% CI: 3.42–3.83, p < 0.001), hyperglycemia (OR: 1.84, 95% CI: 1.73–1.96, p < 0.001), hypercholesterolemia (OR = 1.34; 95% CI 1.22–1.48; p < 0.001), ECG abnormalities (OR = 1.11; 95% CI 1.07–1.15; p < 0.001) and family history of hypertension (OR = 1.69; 95% CI 1.58–1.81; p < 0.001) were risk factors of hypertension for workers. Male workers had a relatively higher hypertension risk than female workers (OR = 1.61; 95% CI 1.54–1.69; p < 0.001). Ear protective measures could not reduce the risk of hypertension in workers. Our nomogram has good predictive accuracy and validity. A dynamic nomogram to predict the workers' risk of hypertension was established publicly available online.
Conclusion: Occupational noise exposure may elevate workers' hypertension risk. More effective and relevant prevention measures should be taken. Our nomogram may help identify high-risk workers and facilitate timely interventions.
Hypertension (ICD10 I10-I15) is a common chronic non-communicable disease and the main risk factor of cardiovascular and cerebrovascular diseases (1, 2). Besides high disability and high mortality, it may also cause a heavy burden to the patient, family and society (3). According to Global Burden of Disease Study 2019 (GBD 2019), there were about 10.85 million deaths caused by hypertension worldwide in 2019, accounting for 31% of all causes of death (4). From 1990 to 2019, the deaths induced by hypertension among Chinese residents increased from 1.2 to 2.6 million (5). Apart from socioeconomic and personal factors (such as dietary and exercise habits) (6–8), incidence of hypertension might be influenced by environmental risks such as air pollution and noise (9–13).
Occupational noise is one of the most common and prevalent occupational hazards of the modern world and health effects of noise were first recognized in occupational settings (14). With the development of modern industrialization, occupational noise exposure related to occupational injury has gradually attracted public attention. It has long been established that occupational noise exposure may induce adverse auditory health effects (14–16) and non-auditory health effects (17–20), while the effect of occupational noise exposure on hypertension has been controversial. Existing studies report conflicting results on it (21–23). A prospective cohort study shows that workers exposed to noise levels between 82 and 106 dB for 3–17 years may increase the risk of hypertension with a non-linear exposure-response pattern (22). A landmark finding from animal studies was the demonstration that a chronic exposure to noise with average sound pressure level (SPL) of 85 dB may elicit sustained elevations in monkeys' blood pressure by 30 mmHg without a return to baseline values after the noise ended (24). Some systematic review studies support the association between occupational noise exposure and hypertension (23, 25, 26), while a systematic review with meta-analysis from the WHO/ILO Joint suggests that there is insufficient evidence on the burden of cardiovascular disease (CVD) attributable to occupational exposure to noise appears (21). Yet this research was quickly criticized and questioned by peers (27). Although the authors have responded to the doubts (28), it may not be that much convincing. There is still uncertainty about whether hypertension is associated with occupational noise exposure to date.
As data beyond traditional clinical trials, real-world data (RWD) come from the real medical environment and may reflect the health status of the population under real conditions. According to the latest definition from US Food and Drug Administration (FDA) (29), RWD are data relating to patient health status and/or the delivery of healthcare routinely collected from a variety of sources. RWD play an increasing important role in healthcare decisions (30) while many of them are not sufficiently used, such as physical data from physical examination organizations, leading to data waste and the efficiency of physical examination. Medical records of regular occupational health examinations is such RWD. To prevent occupational diseases, Chinese government require enterprises engage third-party organizations to identify and detect occupational hazards to which workers may be exposed. Workers identified with occupational hazards exposure would attend regular occupational health examinations.
Using occupational health examination data from all registered occupational health examination units (37 units) in Wuhan from 2021 to 2022, the objectives of this study were: (1) estimate the current prevalence of hearing loss and hypertension in workers with occupational risk exposure in Wuhan; (2) examine whether there is potential association between hypertension and occupational noise exposure.
Our study population were workers with occupational hazards exposure in Wuhan. Data used in this study were medical records of regular occupational health examinations from all registered occupational health examination units (37 units) in Wuhan from January 2021 to May 2022. One lakh six thousand nine hundred thirty-one workers aged 18–60 years exposed to different occupational hazards from 1,264 enterprises in Wuhan, Hubei were enrolled.
Data used in this study comprised of two parts: questionnaire survey and physical examination data. Questionnaire survey contained the workers' demographic information, sociological information and medical history. The demographic information module included workers' sex, age, conscious symptoms and their occupational history (e.g., unit, occupational hazard factors exposed and the duration of exposure). The sociological information module mainly investigated the disease history of the respondents' immediate relatives (parents, grandparents). The medical history module included the type of disease, time, treatment process, disease outcome and so on. Based on the technical specifications for occupational health monitoring GBZ188-2014 (31), physical examination data included height, weight, blood pressure, pulse, blood routine, urine routine, blood lipids, blood glucose, electrocardiogram (ECG), liver function and audiologic testing. All physical examinations were performed by occupational health physicians from 37 registered occupational health examination units in Wuhan. Each worker had the right to refuse participation in health examinations or questionnaire survey partially or completely.
Blood pressure was measured after 5 min of rest in a quiet area. Hypertension was defined as systolic blood pressure (SBP) ≥ 140 mm Hg and/or diastolic blood pressure (DBP) ≥ 90 mm Hg, or antihypertensive medication use (3).
The mean body mass index (BMI) was computed by the ratio of body weight (kg) to height squared (m2). Overweight (including obesity) was defined as BMI ≥ 24, normal as 18.5 ≤ BMI < 24 and underweight as BMI < 18.5 using the Working Group on Obesity in China criteria (32). Obesity as defined as BMI ≥27 in this study.
The normal level range of Chinese fasting blood glucose (FBG) is 3.9–6.0 mmol/L (33). Hyperglycemia was defined as FBG > 6.0 mmol/L and hypoglycaemia was defined as FBG < 3.9 mmol/L. Hypercholesterolemia was defined as total cholesterol(TC) ≥ 6.2 mmol/ L (34). The blood samples were collected in the morning on an empty stomach.
Pure-tone audiometry was used to measure the workers' thresholds of hearing at 0.5, 1, 2, 3, 4 and 6 kHz on the basis of diagnostic criteria GBZ 49-2014 (35). Only workers at positions exposed to noise would participate in audiometric examinations. The symbols HL500Hz, HL1000Hz, HL2000Hz, HL3000Hz, HL4000Hz, HL6000Hz represented the listener's hearing level threshold at a particular pure-tone frequency, in decibels (dB). The subscript L stood for the left ear and L for the right. The binaural high frequency threshold average (BHFTA) and monaural threshold of weighted value (MTMV) were calculated using formula (1) and formula (2), the units were dB. It was defined as high-frequency hearing loss when BHFTA exceeded 25 dB, and normal high-frequency hearing function when BHFTA was < 25 dB. The lower MTMV value of two ears was labeled as MTMVbetter. It was defined as speech frequency hearing loss when MTMVbetter exceeded 25 dB.
Ethical approval was granted by the ethics committee of Wuhan Prevention and Treatment Center for Occupational Diseases (approval number 2022-WZF03).
Data analysis and visualization were performed using R statistical software (version 4.2.1). Group differences of continuous data were analyzed by Student's t-test and categorical data by chi-square test (α = 0.05). Multivariate analysis was performed using binary logistic regression. Forest plot (36) and nomograms (37) were constructed for the visualization of statistical predictive models based on binary logistic regression model. The receiver operating characteristic (ROC) curve, area under the ROC curve (AUC), concordance indexes (C-index) and calibration curves were used to assess the predictive accuracy, the discrimination and calibration of the nomogram and internally validated. Decision curve analysis (DCA) was performed to evaluate the net benefit that workers could receive. Internal validation and external validation were carried out, respectively. The bilatera P < 0.05 was considered to be statistically significant.
After elimination of respondents who had absence of blood pressure records (n = 2,690), occupational history (n = 421), or had hypertension before work (n = 2,215), 101,605 respondents were finally included in our analysis. The mean age of the respondents was 37.2 ± 9.4 years and 79.5% were male. 57.6% respondents were exposed to occupational noise while only 56.9% of them took ear protection measures. The mean BMI value of the respondents was 24.0 ± 3.7 and 69.3% was overweight (BMI ≥ 24). Sixty-three thousand one hundred sixty-one respondents (99.6% of self-reported occupational noise exposed) participated in the pure tone audiometry tests and the mean BHFTA value of them was 22.5 ± 10.8 with 25.7% had high-frequency hearing loss (BHFTA > 25dB). The mean MTMV value of better ear was 18.8 ± 6.4 with 8.6% had impairment on speech frequency hearing functions (MTMVbetter>25dB). Thirty-one thousand one hundred eighty-four respondents had ECG abnormalities and 20.6% had hypertension. Detailed descriptive characteristics of the respondents are listed in Table 1.
There were more male in workers exposed to occupational noise (83.6%) than other risk factors (74.1%) (p < 0.001). Compared to workers exposed to other risk factors, workers exposed to occupational noise were younger (37.1 ± 9.5) (p < 0.001), yet had a higher mean BMI (24.1 ± 3.7) (p < 0.001) and 30.4% were overweight or obese (48.4% in those had BMI records). Only 56.9% workers would use hearing protective equipment though they were exposed to occupational noise. Higher rate of high-frequency hearing loss (25.3%), speech frequency hearing loss (8.8%), ECG abnormalities (31.9%) and hypertension (21.0%) were found in workers exposed to occupational noise than others (3.3% high-frequency hearing loss, 0.7% speech frequency hearing loss, 30.2% ECG abnormalities and 20.0% hypertension, respectively, all ps < 0.001). Results of comparisons of the characteristics between workers exposed to different risk factors are listed in Table 2.
Univariate analyses were used to identify risk factors of speech frequency hearing loss, ECG abnormalities and hypertension. According to our analysis, workers exposed to occupational noise had a statistically significant (p < 0.001) higher prevalence of high-frequency hearing loss (25.3%), speech frequency hearing loss (8.8%), ECG abnormalities (31.6%) and hypertension (21.0%) than those not (0.7, 29.5 and 20.0%, respectively).The prevalence of hearing loss and hypertension increased with the time of exposure to occupational hazards (p < 0.001). For workers exposed to occupational hazards for over 20 years, the prevalence rates of high-frequency hearing loss, speech frequency hearing loss and hypertension reached 29.0, 13.1, and 36.9%, respectively. Besides, workers who bore abnormal BHFTA or MTMV had higher rate of ECG abnormalities and hypertension. More details are shown in Table 3.
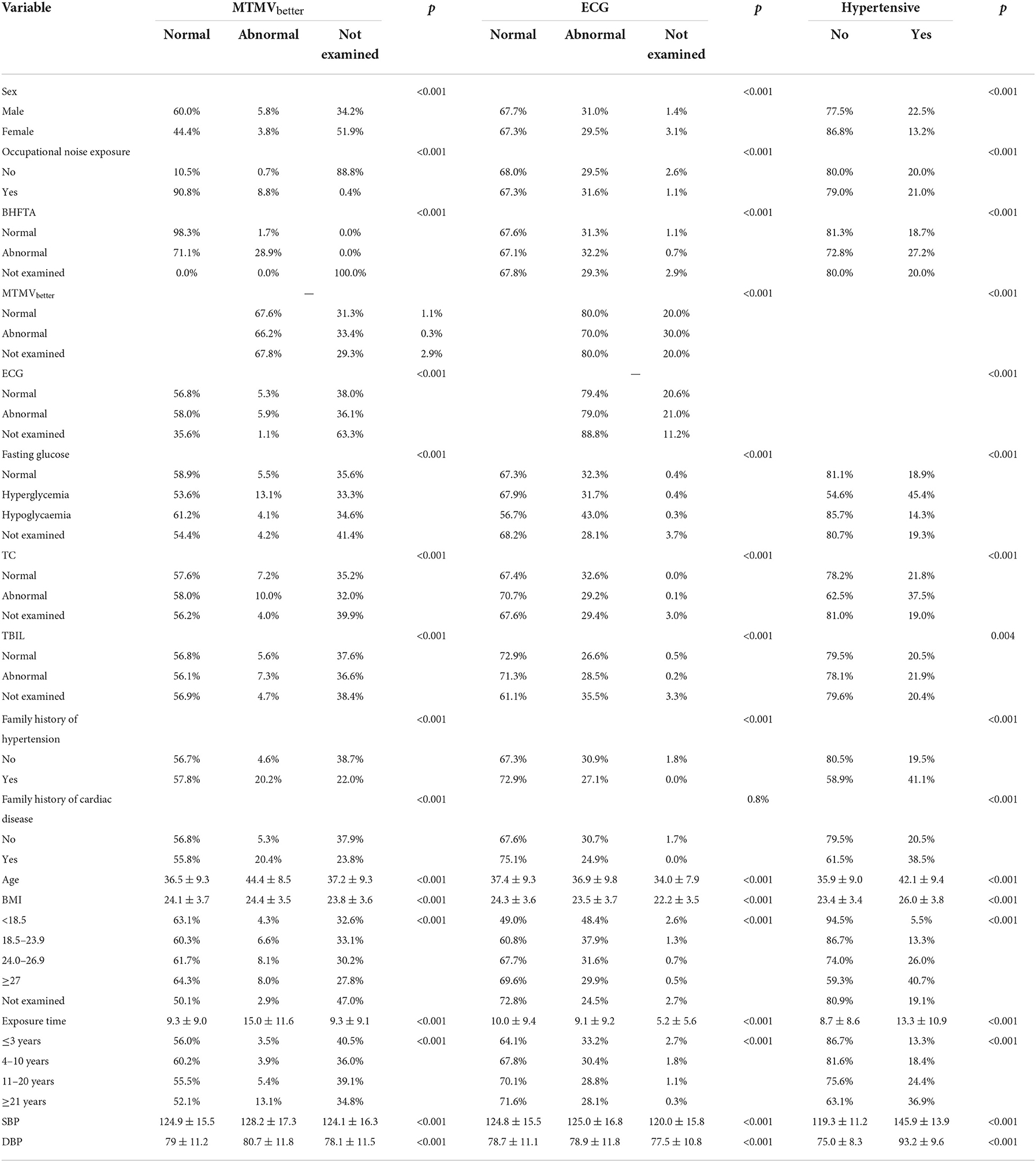
Table 3. Univariate analysis for the possible predictive factors of speech frequency hearing loss, ECG abnormalities and hypertension.
Binary logistic regressions were performed to calculate odds ratios (ORs) for the risk of hypertension (Figure 1). Occupational noise exposure (OR = 1.09, 95% CI: 1.01–1.18, p = 0.04), growth of age (OR: 1.07, 95% CI: 1.07–1.07, p < 0.001) and BMI, hyperglycemia (OR: 1.84, 95% CI: 1.73–1.96, p < 0.001), hypercholesterolemia (OR = 1.34; 95% CI 1.22–1.48; p < 0.001), ECG abnormalities (OR = 1.11; 95% CI 1.07–1.15; p < 0.001) and family history of hypertension (OR = 1.69; 95% CI 1.58–1.81; p < 0.001) were risk factors of hypertension for workers. Male workers had a relatively higher hypertension risk than female workers (OR = 1.61; 95% CI 1.54–1.69; p < 0.001).
Nomograms were the visualization of statistical predictive models specifically developed to enable individualized prognosis prediction and may convey the results of a various statistical models. In our study, the intention was to predict a binary outcome of workers' hypertension (yes/no) based on the above results. After listwise deletion of participants with missing values, 37,406 workers were included in the analysis. For internal validation, the workers were randomly assigned into two groups with a ratio of 7:3 following a randomization sequence:training set (n = 26,004) and internal validation set (n = 11,402). For external validation, we used data from a survey conducted in a cigarette factory in Wuhan from July 2020 to August 2020. Eight hundred seventy-nine workers were included in this study for external validation. With the results in Figure 1, we incorporated sex, age, BMI, noise exposure, BHFTA, ECG results, TC results, family history of hypertension and blood glucose results into the nomogram to predict incidence risk of hypertension [R2 = 0.225, C-index = 0.760 (95% CI 0.754–0.767)] (Figure 2). The characteristics of participants in training set, internal validation set and external validation set are shown in Table 4.
The nomogram had good accuracy in training set (AUC, 0.760; 95% CI 0.754–0.767) (Figure 3A), internal validation set (AUC, 0.760; 95% CI 0.750–0.770) (Figure 3B) and external validation set (AUC, 0.766; 95% CI 0.715–0.817) (Figure 3C). The calibration curves were close to the ideal diagonal line and showed good calibration in training set (Figure 4A), internal validation set (Figure 4B) and external validation set (Figure 4C). Moreover, the DCA showed significant net benefit of the predictive model (Figure 5A), as well as that in the validation cohorts (Figures 5B,C). These data demonstrated that our nomogram had a high potential for clinical utility.
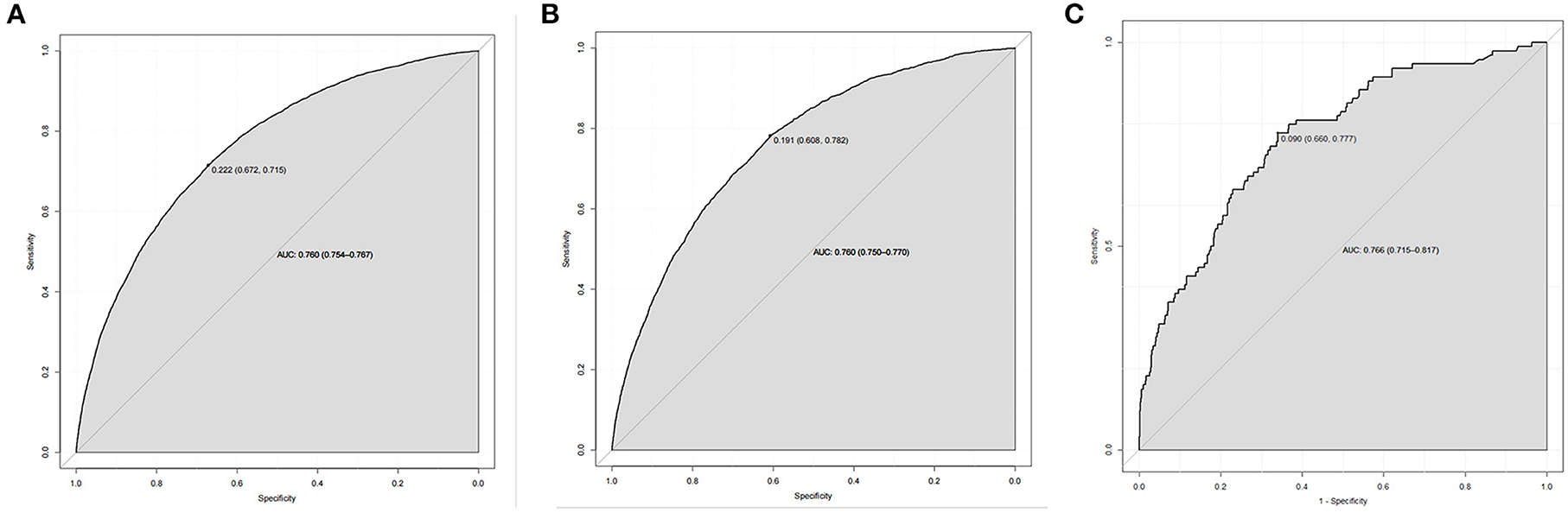
Figure 3. ROC curves. (A) Training set. (B) Internal validation set. (C) External validation set. ROC, receiver operating characteristic; AUC, area under the ROC curve.
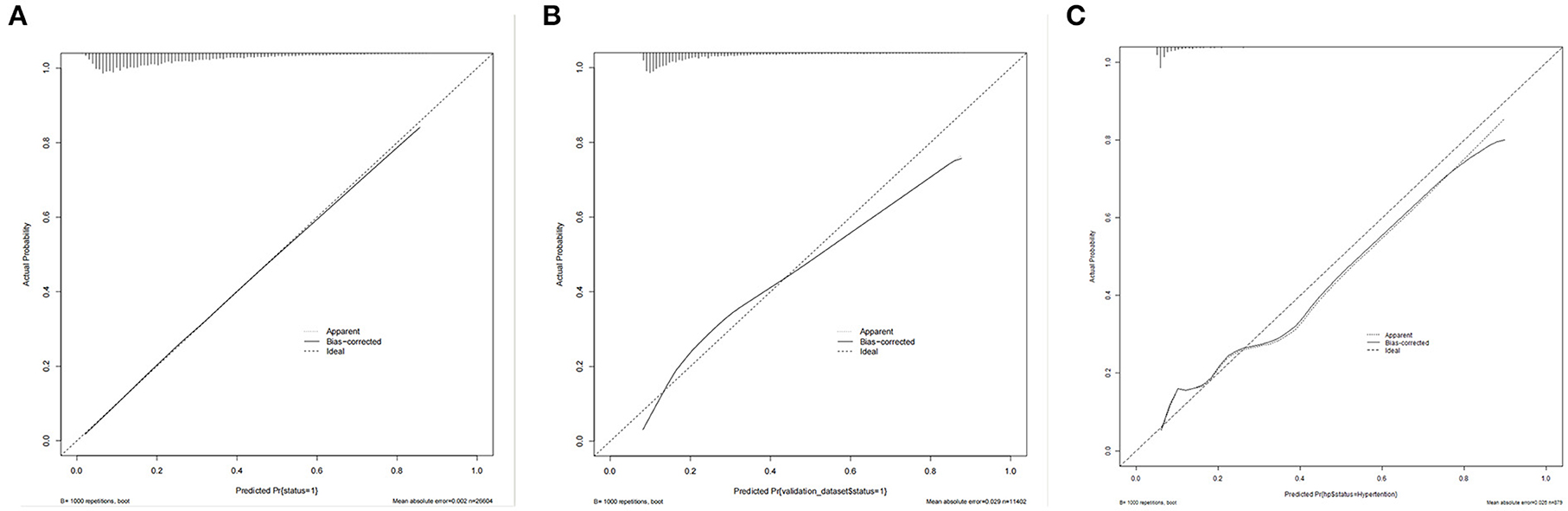
Figure 4. Calibration curve for predicting probability of hypertension. (A) Training set. (B) Internal validation set. (C) External validation set.
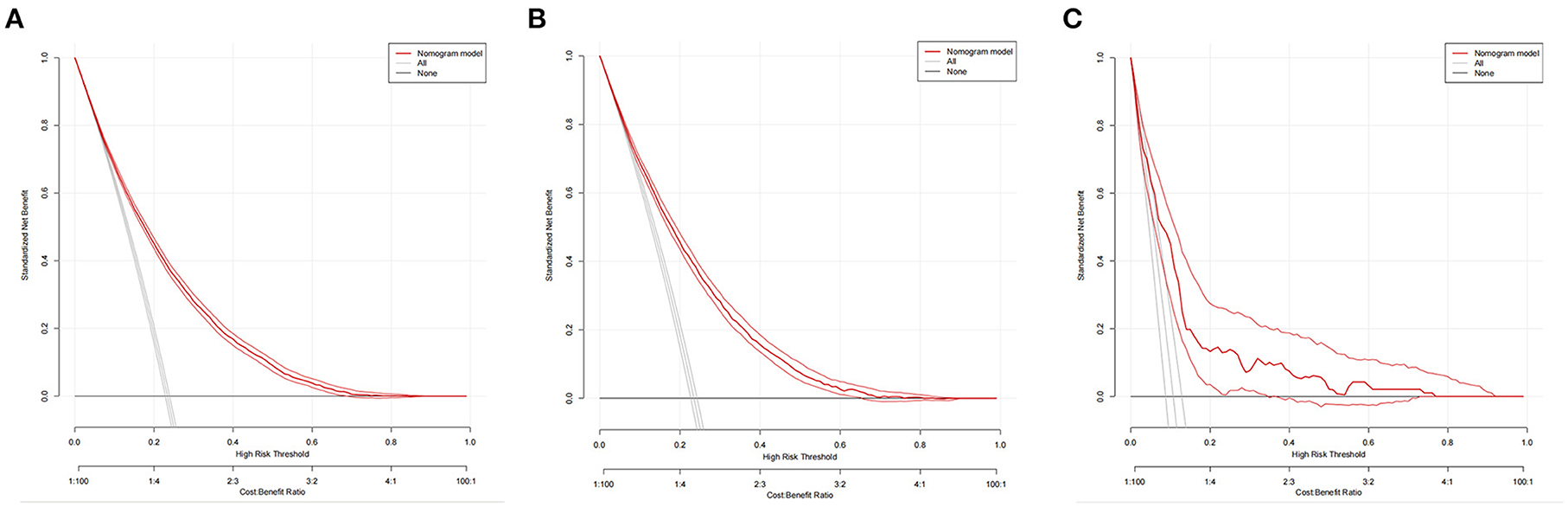
Figure 5. Decision curve analysis in prediction of hypertension. (A) Training set. (B) Internal validation set. (C) External validation set.
To facilitate use of our prediction model, a dynamic nomogram was established publicly available online (https://hbpdynnomo.shinyapps.io/DynNom_HBP_workers/) using the DynNom package of R. It may dynamically predict the hypertension risk of workers on the website in a user-friendly way.
Based on occupational health examination data, this study analyzed the current prevalence of hearing loss, ECG abnormalities and hypertension among workers with different occupational risks exposure in Wuhan. We further explored the risk factors of workers' hypertension. According to our study, occupational noise was the most exposed occupational hazard factor for workers in Wuhan and 57.6% respondents were exposed to it. 31.2% workers showed ECG abnormalities and 20.6% had hypertension. Such a high frequency of occupational noise exposure suggests that importance should be placed on monitoring the hazards of occupational noise and targeted occupational protection measures should be taken as early as possible. Among respondents participated in pure tone audiometry tests, 25.7% had high-frequency hearing loss and 8.6% had speech frequency hearing loss. Workers exposed to occupational noise had higher rate of high-frequency hearing loss (25.3%), speech frequency hearing loss (8.8%), ECG abnormalities (31.6%) and hypertension (21.0%), reconfirming the negative effect of occupational noise on auditory system and cardiovascular system (1, 14, 38).
Studies have suggested that acoustic overstimulation may contribute to the pathogenesis and biochemical changes that result in hearing loss (39, 40). The continued and evolving research involving noise-induced hearing loss (NIHL) has determined that there is a close relationship between the occurrence of NIHL and changes in some genes, cell metabolism, cell apoptosis and so forth (41). Thus, workers exposed to occupational noise may have heightened risk for hearing loss. Damaging effects of occupational noise on cardiovascular system have been presented in previous studies (17, 19, 20) as well. Several mechanisms through which noise contribute to cardiovascular system impairment are proposed: changes to gene net-works, epigenetic pathways, the gut microbiota, circadian rhythm, neuronal excitability and signal transduction, oxidative stress, inflammation and metabolism (13). Experimental evidence shows that noise may cause an increase in stress hormone release and in circulating angiotensin II (Ang II) levels with significant stress-induced increase in blood pressure (38). The effects of noise exposure on cognitive function (18), mental health (42) and spiritual wellbeing (43) may also play an important role in the process of occupational noise exposure affecting cardiovascular health. Surprisingly, we found that protective measures such as wearing ear muffs and earplugs could not reduce the risk of hypertension in workers. One possibility is that protective measures of the workers are not in place. Workers do not wear or do not wear ear protection equipment correctly, or the protective effect of ear protection equipment is limited. Common occupational ear protection articles are more used to protect workers against high-frequency noise, while protection against low-frequency noise is limited. Alternatively, the influence of occupational noise on hypertension has nothing to do with ear protection and more valid and relevant measures should be taken. Effects of wearing protective equipment and impacts of occupational noise at different frequencies and intensities on the cardiovascular system of workers deserve further exploration. Besides, we found a sex-dependent effect of noise on hypertension, which is consistent with the previous study (44). It may be related with the fact that the risk pattern for hypertension (45) and nature of the work (46) are different for male and female.
Although univariate analysis showed that workers with hearing loss had greater prevalence of hypertension, multivariate analysis showed that the relationships between the two were not significant. In our study, workers exposed to occupational noise (OR = 1.09; 95% CI 1.01–1.18; p = 0.04) faced higher risk of hypertension than those not and the association between hypertension and occupational noise exposure was confirmed existed regardless whether the worker had hearing loss. A systematic review suggested that exposure to noise at work was consistently positively associated with hypertension [Hazard ratio (HR) = 1.68; 95% CI 1.10–2.57] (26). Previous research suggests that noise could raise blood pressure without impairing auditory sensitivity (24). However, the healthy worker survivor effect (47) should not be ignored as well. Aside from the muting effects of hearing loss, the healthy worker survivor effect would also conceal the impacts of occupational noise on blood pressure. In addition, the muting correlation between hearing loss and hypertension may also be related to their positive correlations with age. Hyperglycemia (OR = 1.84; 95% CI 1.73–1.96; p < 0.001), hypercholesterolemia (OR = 1.34; 95% CI 1.22–1.48; p < 0.001) and ECG abnormalities (OR = 1.11; 95% CI 1.07–1.15; p < 0.001) were significant predictors as well. It should be noted that hypertension, dyslipidemia and dysglycemia are risk factors of CVD (48) and hypertension combined with dysglycemia may greatly exacerbate the risk of CVD (49).
We provided a visualization of workers' hypertension prediction using nomogram based on binary logistic regression analysis. Available sociodemographic characteristics and clinical parameters were used in the nomograms, which was convenient and quick for screening the high-risk individuals. Previous nomogram suggests that age, sex, early life factors, family history of the disease, and lifestyle factors may predict the risk of hypertension (44, 50). Given the research subjects of this study are workers exposed to occupational hazards and data limit, this study finally included age, sex, occupational noise exposure status and physical examination results. Results revealed that sex, age, BMI, occupational noise exposure status, ECG results, TC results, family history of hypertension and blood glucose results were predictors of hypertension in workers with different occupational hazards in Wuhan. Our nomogram showed good predictive accuracy and validity. It may help identify high-risk workers and facilitate timely, effective and targeted prevention interventions so as to improve occupational health.
There are several limitations in our study as follows. First, occupational health examination data are by their nature observational studies, where data tend to be collected by clinicians rather than investigators. Data used for this study were cross-sectional and we can only demonstrate associations rather than prove causality, nor did we verify the mechanism. Secondly, we only studied whether exposure to occupational noise had an impact on the risk of hypertension, but did not specifically estimate the impact of noise at different frequencies and intensities on health. Last but not least, despite adjusting some factors in the present study, there are still some confounders that may influence the results not included, which should be considered in subsequent studies.
Occupational noise exposure of workers may elevate their hypertension risk. Standard ear protection measures should be strengthened and more effective and relevant hypertension prevention measures should be taken. Our nomogram may help identify high-risk workers and facilitate timely interventions so as to improve occupational health.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
LZ and XT designed the study. LZ, ZC, WY, WF, FH, ZP, and GY collected the data. LZ performed statistical analysis. LZ, SC, and ZC drafted this manuscript. LZ, XT, and GY revised the manuscript. XT and GY had primary responsibility for final content. All authors were involved in the revisions and approved the final version of the manuscript.
This work was funded by Hubei Province Health and Family Planning Scientific Research Project [Grant Number WJ2018H0101] and Wuhan Municipal Health Commission Scientific Research Project [Grant Number WG19Y03].
We thank the medical workers of Wuhan Occupational Disease Prevention and Control Hospital for their contributions to this project, and express our sincere support and gratitude to them.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ALAT, Alanine aminotransferase; AUC, area under the ROC curve; BHFTA, binaural high frequency threshold average; BMI, mean body mass index; CI, confidence intervals; C-index, concordance indexes; CVD, cardiovascular disease; dB, decibels; DBP, diastolic blood pressure; DCA, decision curve analysis; ECG, electrocardiogram; FBG, fasting blood glucose; FDA, US Food and Drug Administration; GBD 2019, Global Burden of Disease Study 2019; HR, Hazard ratio; MTMV, monaural threshold of weighted value; MTMVL, monaural threshold of weighted value of the left ear; MTMVR, Monaural threshold of weighted value of the right ear; NIHL, noise-induced hearing loss; OR, odds ratio; ROC, receiver operating characteristic; RWD, real-world data; SBP, systolic blood pressure; SD, Standard deviation; SPL, sound pressure level; TBIL, total bilirubin; TC, total cholesterol.
1. Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. (2021) 18:785–802. doi: 10.1038/s41569-021-00559-8
2. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. (2020) 16:223–37. doi: 10.1038/s41581-019-0244-2
3. Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. (2015) 386:801–12. doi: 10.1016/S0140-6736(14)61468-9
4. Murray CJ, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49.
5. Xu T, Zhou M, Liu J, Wang L, Dong W. Death burden attributable to hypertension in 1990 and 2019 in China. Chin J Prev Contr Chron Dis. (2022) 30:327–31. doi: 10.16386/j.cjpccd.issn.1004-6194.2022.05.002
6. Falaschetti E, Mindell J, Knott C, Poulter N. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet. (2014) 383:1912–9. doi: 10.1016/S0140-6736(14)60688-7
7. Lawes CM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part 1: estimates of blood pressure levels. J Hypertens. (2006) 24:413–22. doi: 10.1097/01.hjh.0000199801.72563.6f
8. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. (2005) 365:217–23. doi: 10.1016/S0140-6736(05)17741-1
9. Mannuccio MP, Carla A. Noise and air pollution as triggers of hypertension. Eur Heart J. (2021) 42:2085–7. doi: 10.1093/eurheartj/ehab104
10. Münzel T, Schmidt FP, Steven S, Herzog J, Daiber A, Sørensen M. Environmental noise and the cardiovascular system. J Am Coll Cardiol. (2018) 71:688–97. doi: 10.1016/j.jacc.2017.12.015
11. Jarup L, Babisch W, Houthuijs D, Pershagen G, Katsouyanni K, Cadum E, et al. Hypertension and exposure to noise near airports: the HYENA study. Environ Health Perspect. (2008) 116:329–33. doi: 10.1289/ehp.10775
12. De Kluizenaar Y, Gansevoort RT, Miedema HM, de Jong PE. Hypertension and road traffic noise exposure. J Occup Environ Med. (2007) 49:484–92. doi: 10.1097/JOM.0b013e318058a9ff
13. Münzel T, Sørensen M, Daiber A. Transportation noise pollution and cardiovascular disease. Nat Rev Cardiol. (2021) 18:619–36. doi: 10.1038/s41569-021-00532-5
14. Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet. (2014) 383:1325–32. doi: 10.1016/S0140-6736(13)61613-X
15. Tikka C, Verbeek JH, Kateman E, Morata TC, Dreschler WA, Ferrite S, et al. Interventions to prevent occupational noise-induced hearing loss. Cochrane Database Syst Rev. (2017) 7:CD006396. doi: 10.1002/14651858.CD006396.pub4
16. Li X, Dong Q, Wang B, Song H, Wang S, Zhu B. The influence of occupational noise exposure on cardiovascular and hearing conditions among industrial workers. Sci Rep. (2019) 9:11524. doi: 10.1038/s41598-019-47901-2
17. Wang D, Xiao Y, Feng X, Wang B, Li W, He M, et al. Association of occupational noise exposure, bilateral hearing loss with atherosclerotic cardiovascular disease risk in Chinese adults. Int J Hyg Environ Health. (2021) 235:113776. doi: 10.1016/j.ijheh.2021.113776
18. Deal JA, Gross AL, Sharrett AR, Abraham AG, Coresh J, Carlson M, et al. Hearing impairment and missing cognitive test scores in a population-based study of older adults: the atherosclerosis risk in communities neurocognitive study. Alzheimers Dement. (2021) 17:1725–34. doi: 10.1002/alz.12339
19. Yang Y, Zhang E, Zhang J, Chen S, Yu G, Liu X, et al. Relationship between occupational noise exposure and the risk factors of cardiovascular disease in China. Medicine. (2018) 97:e11720. doi: 10.1097/MD.0000000000011720
20. Yang L, Dai X, Wu L, Xu T, Chen Z, Min Z, et al. Stress hormone biosynthesis-based genes and lifestyle moderated the association of noise exposure with blood pressure in a cohort of Chinese tobacco factory workers: a cross-sectional analysis. Int J Hyg Environ Health. (2022) 239:113868. doi: 10.1016/j.ijheh.2021.113868
21. Teixeira LR, Pega F, Dzhambov AM, Bortkiewicz A, Correa da Silva DT, de Andrade CAF, et al. The effect of occupational exposure to noise on ischaemic heart disease, stroke and hypertension: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-Related Burden of Disease and Injury. Environ Int. (2021) 154:106387.
22. Lin YT, Chen TW, Chang YC, Chen ML, Hwang BF. Relationship between time-varying exposure to occupational noise and incident hypertension: a prospective cohort study. Int J Hyg Environ Health. (2020) 226:113487. doi: 10.1016/j.ijheh.2020.113487
23. Bolm-Audorff U, Hegewald J, Pretzsch A, Freiberg A, Nienhaus A, Seidler A. Occupational noise and hypertension risk: a systematic review and meta-analysis. Int J Environ Res Public Health. (2020) 17:6281. doi: 10.3390/ijerph17176281
24. Peterson EA, Augenstein JS, Tanis DC, Augenstein DG. Noise raises blood pressure without impairing auditory sensitivity. Science. (1981) 211:1450–2. doi: 10.1126/science.7466404
25. Tomei G, Fioravanti M, Cerratti D, Sancini A, Tomao E, Rosati MV, et al. Occupational exposure to noise and the cardiovascular system: a meta-analysis. Sci Total Environ. (2010) 408:681–9. doi: 10.1016/j.scitotenv.2009.10.071
26. Skogstad M, Johannessen HA, Tynes T, Mehlum IS, Nordby KC, Lie A. Systematic review of the cardiovascular effects of occupational noise. Occup Med. (2016) 66:10–6. doi: 10.1093/occmed/kqv148
27. Bolm-Audorff U, Hegewald J, Pretzsch A, Freiberg A, Nienhaus A, Seidler A. Letter to the editor regarding, “The effect of occupational exposure to noise on ischaemic heart disease, stroke and hypertension: A systematic review and meta-analysis from the WHO/ILO joint estimates of the work-related burden of disease and injury”. Environ Int. (2022) 161:107104. doi: 10.1016/j.envint.2022.107104
28. Teixeira L Dzhambov AM Gagliardi Gagliardi D; WHO/ILO Working Group of Individual Experts on Occupational Exposure to Noise on Ischaemic Heart Disease Stroke and Hypertension. Response to Letter to the Editor Regarding “The effect of occupational exposure to noise on ischaemic heart disease, stroke and hypertension: A systematic review and meta-analysis from the WHO/ILO joint estimates of the work-related Burden of disease and injury”. Environ Int. (2022) 161:107105. doi: 10.1016/j.envint.2022.107105
29. FDA. Framework for FDA's Real-World Evidence Program. (2018). Available online at: https://www.fda.gov/media/120060/download
30. McMahon AW, Quinto K, Abernethy A, Corrigan-Curay J. Summary of literature on pediatric real-world evidence and effectiveness. JAMA Pediatr. (2021) 175:1077–9. doi: 10.1001/jamapediatrics.2021.2149
31. Ruan Y, Zhang X, Xie L, Chen W, Sun D. GBZ 188-2014 Revision of technical specifications for occupational health monitoring. Chin J Indust Hygiene Occup Dis. (2016) 34:146–7. doi: 10.3760/cma.j.issn.1001-9391.2016.02.020
32. Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. (2002) 15:83–96. doi: 10.1046/j.1440-6047.11.s8.9.x
33. CDS. CDS Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes Mellitus. (2021) 13:315–409. doi: 10.3760/cma.j.cn115791-20210221-00095
34. Gao RL, Zhao SP. 2016 Chinese guideline for the management of dyslipidemia in adults. Chin J Cardiol. (2016) 44:833–53.
35. P. National Health Commission P. National Health Commission. National Health Commission of Peoples Republic of China: People's Republic of China. (2014).
36. Kim J, Kaufman JS, Bang H. Graphing ratio measures on forest plot. J Am Coll Cardiol. (2018) 71:585–6. doi: 10.1016/j.jacc.2017.10.098
37. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. (2008) 26:1364–70. doi: 10.1200/JCO.2007.12.9791
38. Münzel T, Daiber A, Steven S, Tran LP, Ullmann E, Kossmann S, et al. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur Heart J. (2017) 38:2838–49. doi: 10.1093/eurheartj/ehx081
39. de Iriarte Rodríguez R, Magarinos M, Pfeiffer V, Rapp UR, Varela-Nieto I. C-Raf deficiency leads to hearing loss and increased noise susceptibility. Cell Mol Life Sci. (2015) 72:3983. doi: 10.1007/s00018-015-1919-x
40. Finneran JJ. Noise-induced hearing loss in marine mammals: a review of temporary threshold shift studies from 1996 to 2015. J Acoust Soc Am. (2015) 138:1702–26. doi: 10.1121/1.4927418
41. Carlsson PI, Van Laer L, Borg E, Bondeson ML, Thys M, Fransen E, et al. The influence of genetic variation in oxidative stress genes on human noise susceptibility. Hear Res. (2005) 202:87–96. doi: 10.1016/j.heares.2004.09.005
42. Ma J, Li C, Kwan MP, Kou L, Chai Y. Assessing personal noise exposure and its relationship with mental health in Beijing based on individuals' space-time behavior. Environ Int. (2020) 139:105737. doi: 10.1016/j.envint.2020.105737
43. McLean EK, Tarnopolsky A. Noise, discomfort and mental health a review of the socio-medical implications of disturbance by noise. Psychol Med. (1977) 7:19–62. doi: 10.1017/S0033291700023138
44. Liang JH, Zhao Y, Chen YC, Huang S, Zhang SX, Jiang N, et al. Development and validation of a nomogram-based prognostic model to predict high blood pressure in children and adolescents-findings from 342,736 individuals in China. Front Cardiovasc Med. (2022) 9:884508. doi: 10.3389/fcvm.2022.884508
45. Stokholm ZA, Bonde JP, Christensen KL, Hansen ÅM, Kolstad HA. Occupational noise exposure and the risk of hypertension. Epidemiology. (2013) 24:135–42. doi: 10.1097/EDE.0b013e31826b7f76
46. Wang D. The relationship of occupational noise, smoking and shift work with hearing loss and hypertension (Doctoral dissertion) Huazhong University of Science and Technology, Wuhan, China. (2018). p. 130.
47. Brown DM, Picciotto S, Costello S, Neophytou AM, Izano MA, Ferguson JM, et al. The healthy worker survivor effect: target parameters and target populations. Curr Environ Health Rep. (2017) 4:364–72. doi: 10.1007/s40572-017-0156-x
48. Isomaa BO, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. (2001) 24:683–9. doi: 10.2337/diacare.24.4.683
49. Tian J, Sheng CS, Sun W, Song X, Wang H, Li Q et al. Effects of high blood pressure on cardiovascular disease events among chinese adults with different glucose metabolism. Diabetes Care. (2018) 41:1895–900. doi: 10.2337/dc18-0918
Keywords: occupational health, occupational noise, hearing loss, hypertension, nomogram
Citation: Zhang L, Chen S, Chen Z, Yin W, Fu W, He F, Pan Z, Yi G and Tan X (2022) Relationship between occupational noise exposure and hypertension: Cross-sectional evidence from real-world. Front. Public Health 10:1037246. doi: 10.3389/fpubh.2022.1037246
Received: 05 September 2022; Accepted: 21 November 2022;
Published: 12 December 2022.
Edited by:
Shengnan Wang, Henan University, ChinaReviewed by:
Jinghong Liang, Sun Yat-sen University, ChinaCopyright © 2022 Zhang, Chen, Chen, Yin, Fu, He, Pan, Yi and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaodong Tan, MDAzMDA0NjlAd2h1LmVkdS5jbg==; Guilin Yi, MTU5MjczOTUyMTBAMTI2LmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.