- 1Division of Intramural Research, National Institute on Minority Health and Health Disparities, National Institutes of Health, Bethesda, MD, United States
- 2Department of Psychology, University of Maryland, College Park, MD, United States
- 3Division of Social Science, Seaver College, Pepperdine University, Malibu, CA, United States
Background: COVID-19-related health perceptions may differentially impact college students' stress, and in turn, their mental and physical health. This study examined racial/ethnic differences in college students' underlying perceptions of COVID-19 threat, healthcare discrimination, and U.S. healthcare system inequities and their associations with self-rated mental and physical health.
Methods: Four-hundred-thirty-two university students completed an online survey (December 2020–December 2021). Latent class analyses identified classes of perceived COVID-19 threat (i.e., severity, susceptibility), healthcare discrimination, and U.S. healthcare system inequities. Regression analyses examined whether class membership varied by race/ethnicity and was associated with self-rated mental and physical health.
Results: Class 1 members (27.3% of the sample) were more likely to identify as Hispanic or Latino, Non-Hispanic Asian, Non-Hispanic Black or African American, and Non-Hispanic Multiracial vs. Non-Hispanic White (vs. Class 4). Class 1 had high perceived COVID-19 threat, medium perceived healthcare discrimination, and high perceived U.S. healthcare system inequities, as well as higher odds of poorer mental and physical health (vs. Class 4).
Conclusions: College students' underlying perceptions of COVID-19 threat, healthcare discrimination, and U.S. healthcare system inequities were associated with poorer health. Given that students with these perceptions were more likely to belong to minoritized racial/ethnic groups, concerns over COVID-19 risk and healthcare may partially explain racial/ethnic disparities in college students' health. This study contributes to a limited body of evidence on college students' perceptions of the U.S. healthcare system and suggests important ways that structural inequalities and racial/ethnic disparities in COVID-19 risk, healthcare discrimination, and concerns over U.S. healthcare system inequity may affect college students' health.
Introduction
College campuses in the United States (U.S.) have been one of the highest-risk settings for SARS-CoV-2 viral transmission during the Coronavirus disease 2019 (i.e., COVID-19) pandemic (1). In 2020, close to 400,000 cases of COVID-19 infection were reported at 1,800 colleges and universities in the U.S. (2). More recently, after gradual declines in national COVID-19 cases, COVID-19 cases rose nationally by 61% in April 2022 and colleges across the U.S. reinstated indoor mask mandates and/or limited large gatherings (3, 4).
Amid these national COVID-19 outbreaks, college students across the U.S. reported heightened levels of stress [e.g., high levels of worry and/or emotional distress related to COVID-19 (5)]. In addition, COVID-19-related stressors disproportionately affected students from minoritized racial/ethnic groups1 [e.g., increased discrimination among Asian American students (6), high risk of losing someone close to them due to COVID-19 for students from Black, Latinx, and Pacific Islander communities (7, 8), high proportions of grief/loss reported by students from American Indian/Alaska Native and Native Hawaiian or Pacific Islander communities (9)]. Consequently, recent studies emphasized the importance of examining racial/ethnic disparities in college students' stress during the COVID-19 pandemic (10, 11).
Previous studies identified the fear of COVID-19 infection (e.g., fear of contracting the virus, concerns over its spread, high perceived COVID-19 severity and/or susceptibility) as a major driver of college students' COVID-19-related stress (12–14). Moreover, prior studies revealed racial/ethnic differences in college students' COVID-19 fears (14, 15) and suggested that racial/ethnic structural inequalities in the U.S. (e.g., disparities in housing, working conditions, and/or healthcare access) likely exacerbated COVID-19 fears among students from minoritized racial/ethnic groups by contributing to racial/ethnic disparities in COVID-19 exposure, morbidity, and mortality (15, 16). Considering that COVID-19-related stressors can exist at multiple socio-ecological levels [e.g., intrapersonal risk perceptions, interpersonal stressors, structural/system-level concerns (17)], college students' COVID-19-related stress may be influenced by concerns that span these levels (collectively referred to as “health-related perceptions”). These perceptions include fear of COVID-19 infection, the potential stress of engaging with health care providers due to experiences of healthcare discrimination, and concerns over U.S. healthcare system inequities [e.g., racial/ethnic disparities in treatment, access to testing, and/or distribution of the COVID-19 vaccine (18–20)].
Moreover, prior research suggested that college students' health-related perceptions can serve as stressors that influence both their mental and physical health. Among Chinese college students, fears of contagion were associated with poorer psychological and physiological health through higher perceived stress (21). Among college students in the U.S., fears of COVID-19 were associated with increased panic, worry and/or anxiety/depression (22, 23). However, with respect to racial/ethnic differences in college students' health, the evidence is mixed [e.g., whereas some studies found poorer mental health among students who identified as Hispanic or Latinx, Non-Hispanic Black, or Non-Hispanic Asian compared to Non-Hispanic White (5, 24), other studies did not reveal racial/ethnic differences in college students' mental and/or physical health (14, 25)].
These discrepancies may be partially attributed to measurement (e.g., measuring mental health as diagnoses of anxiety and/or depression may only capture stress for students who used health services, measuring physical health using COVID-19 diagnoses may not capture other ways stress can influence physical health). Importantly, there is a lack of research examining college students' health-related perceptions and global measures of self-rated health, despite prior findings that self-rated health was associated with college students' systemic inflammation (26) and was a robust predictor of future morbidity and mortality in adult populations (27). It is plausible that self-rated health may capture perceived changes in health prior to formal diagnoses (26) and could reveal important racial/ethnic differences in college students' stress and health.
Furthermore, much of the evidence on health-related perceptions and college students' health focused on mental health with limited studies on physical health, particularly for college students in the U.S. In addition, most studies focused on fear of the COVID-19 virus as a stressor, and did not include U.S. college students' perceptions of healthcare discrimination and U.S. healthcare system inequities (28, 29). Although one recent study addressed this research gap by examining college students' perceived COVID-19 severity and susceptibility, perceived healthcare discrimination, and perceived U.S. healthcare system inequities (28), the study outcomes included COVID-19 preventive behaviors (i.e., intentions to wear a face mask, social distance, and receive the COVID-19 vaccine). No studies to date examined how these health-related perceptions affect college students' mental and physical health and whether underlying health-related perceptions vary across racial/ethnic groups.
The present study addressed these gaps in the literature by conducting latent class and logistic regression analyses in a population of college students in the U.S. to (i) identify latent classes of health-related perceptions, (ii) examine racial/ethnic differences in latent class membership, and (iii) assess whether these latent classes were associated with college students' self-rated mental and physical health.
Methods
Data source
This study used data from the Weighing Factors in COVID Health Decisions survey conducted from December 2020 to December 2021 at the University of Maryland, College Park. College students who were 18 years of age or older completed a self-administered online survey using Qualtrics software and received university course credit for their participation. Informed consent was obtained using an electronic consent form and study procedures were approved by the University of Maryland, College Park Institutional Review Board.
Survey responses were collected from 491 students. Surveys were excluded from the analysis if they were incomplete (n = 38) or due to small samples within sociodemographic categories (n = 21, see “Race/ethnicity and sociodemographic covariates” under Measures). The final analysis included 432 students.
Measures
Latent class indicators
Drawing on recent latent class analyses (28), latent classes were generated using six indicators related to perceived COVID-19 severity and susceptibility, healthcare discrimination, and U.S. healthcare system inequities (28) (Supplementary Table S1). Consistent with prior Health Belief Model studies (20, 21), perceived COVID-19 severity and susceptibility (i.e., collectively referred to as “perceived COVID-19 threat”) were measured. Perceived COVID-19 severity was measured using the item “You believe COVID-19 is serious and life threatening” and perceived susceptibility was measured using the item “You are concerned about contracting COVID-19”. Response options for both items included “Very true,” “Somewhat true,” and “Not true” and were dichotomized (i.e., “Not true” and “Somewhat true” coded as 0; “Very true” coded as 1).
Perceived healthcare discrimination was measured using a 7-item modified version of the Everyday Discrimination Scale for health care settings (i.e., how often students encountered situations when receiving health care due to their race or ethnicity such as “Treated with less respect than other people” or “Felt like a doctor or nurse was not listening to what you were saying”) (23, 24). Students' responses (i.e., “Never,” “Once,” “2–3 times,” “4 times or more”) were dichotomized (i.e., mean scores of 0: no experiences of healthcare discrimination coded as 0; mean scores > 0: one or more experiences of healthcare discrimination coded as 1).
Perceived U.S. healthcare system inequities included three items related to treatment, access to COVID-19 testing, and distribution of the COVID-19 vaccine (30). Perceived treatment of COVID-19 patients from minoritized racial/ethnic groups was measured using the item “How often have racial and ethnic minority patients with COVID-19 been treated unfairly by the U.S. healthcare system because of their race or ethnicity?” with response options of “Very often,” “Somewhat often,” and “Never” dichotomized (i.e., “Never” coded as 0; “Somewhat often” and “Very often” coded as 1). Perceived access to COVID-19 testing for minoritized racial/ethnic groups was measured using the item “How true is it that racial and ethnic minority groups have less access to COVID-19 testing compared to Whites?” with response options of “Very true,” “Somewhat true,” and “Not true” dichotomized (i.e., “Not true” coded as 0; “Somewhat true” and “Very true” coded as 1). Perceived distribution of the COVID-19 vaccine across racial/ethnic groups was measured using the item “How confident are you that the COVID-19 vaccine will be distributed fairly across racial and ethnic groups?” with response options of “Very confident,” “Somewhat confident,” and “Not confident” dichotomized (i.e., “Very confident” coded as 0; “Somewhat confident” and “Not confident” coded as 1).
Self-rated mental and physical health
Self-rated mental and physical health were measured using the items “In general, how would you rate your overall mental health?” and “In general, how would you rate your overall physical health?”, respectively. Response options for each item included “Poor,” “Fair,” “Good,” “Very Good,” and “Excellent.” (31, 32) and were dichotomized (i.e., “Poor” and “Fair” coded as 0; “Good,” “Very Good,” and “Excellent” coded as 1). A combined self-rated mental and physical health item was also created: (i) good to excellent mental health and good to excellent physical health; (ii) good to excellent mental health and poor to fair physical health or good to excellent physical health and poor to fair mental health; and (iii) poor to fair mental health and poor to fair physical health.
Race/ethnicity and sociodemographic covariates
Students self-identified their race and ethnicity in two separate items. Students selected their race from the U.S. Census categories allowing for multiple selections of “American Indian or Alaska Native,” “Asian,” “Native Hawaiian or Other Pacific Islander,” “Black or African American,” “White,” and “Other” (i.e., with the option to fill-in another race when selecting “Other”). Students self-identified Hispanic ethnicity as “Hispanic or Latino” or “Not Hispanic or Latino”. Students' responses to the race and ethnicity items were combined into the categories of “Non-Hispanic Asian,” “Non-Hispanic Black or African American,” “Non-Hispanic Multiracial,” “Non-Hispanic White,” and “Hispanic or Latino.” Students who self-identified as Non-Hispanic Other Race (n = 12) were not included in the analysis given the small sample size. Students self-identified their gender as male, female, transgender male, transgender female, gender non-conforming, or gender “not listed”. Students who identified as transgender (n = 1), gender non-conforming (n = 6), or indicated their gender was “not listed” (n = 3) were not included in the analysis given small sample sizes. Students' gender identity (i.e., male, female) and household income (i.e., <$50,000, $50,000–99,999, >$100,000) were included as categorical covariates and age in years was included as a continuous covariate.
Analyses
Chi-square and Analysis of Variance tests were conducted using R version 4.1.2 to describe sociodemographic characteristics of the study population and group differences when stratified by race/ethnicity. Latent class analysis was conducted in Mplus Version 8.6 (25) to identify latent classes of students' health-related perceptions, assess racial/ethnic differences in latent class membership, and examine whether latent classes were associated with self-rated mental and physical health.
Identification of latent class health-related perceptions
Robust maximum likelihood estimation was used to generate a series of latent class models from the six latent class indicators. Stepwise model comparisons using sample-size adjusted Bayesian Information Criterion (SA-BIC), entropy, Lo-Mendell Rubin (LMR) likelihood ratio tests, and bootstrapped likelihood ratio tests were used to select the best fitting solution. Direct effects of the sociodemographic covariates on the latent class indicators were assessed in the final step of model selection (i.e., comparing SA-BIC across models) to test for measurement invariance (26).
Racial/ethnic differences in latent class membership
Multinomial logistic regression was used to assess racial/ethnic differences in latent class membership. A three step approach estimated latent classes while accounting for individuals' fractional probabilities of membership in more than one class (33). Latent class membership was regressed on race/ethnicity, household income, age, gender, and survey completion date (i.e., the month in which students completed the study; included as a continuous variable). Odds ratios (ORs) with 95% confidence intervals (CIs) were used to assess the conditional probabilities of each covariate being present within the latent class.
Associations between latent class health-related perceptions and self-rated mental and physical health
Logistic regression models using ORs and 95% CIs were used to examine the associations between the latent classes and mental and physical health. First, self-rated mental health and physical health were each regressed separately on latent class membership using the three-step estimation approach (33), adjusting for direct effects of race/ethnicity, household income, gender, age, and survey completion date on mental and physical health. Next, ordinal logistic regression, adjusting for covariates, examined the association between the latent classes and the combined categorical outcome of mental and physical health.
Results
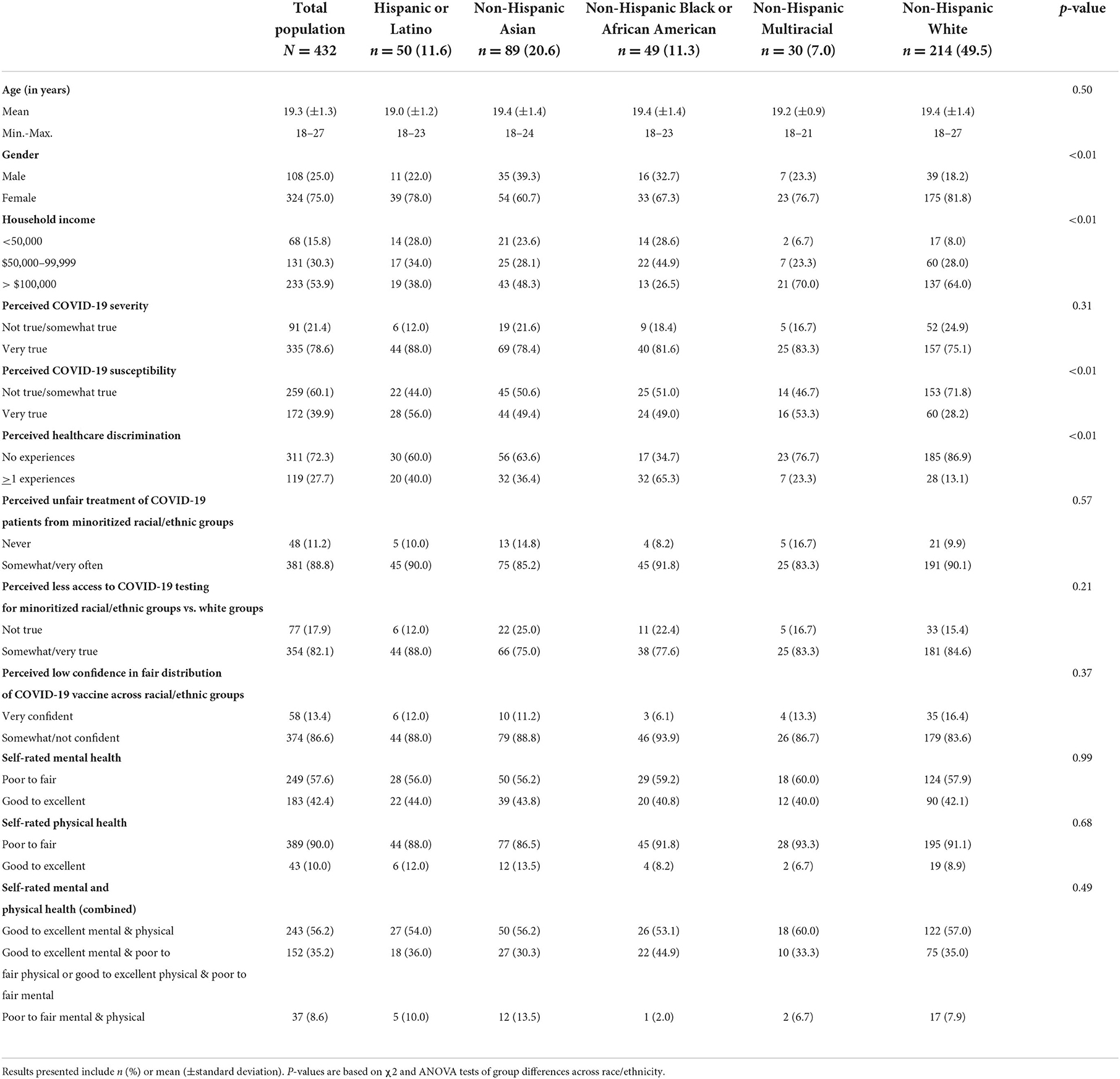
Most students identified as Non-Hispanic White (49.5%), identified as female (75.0%), had a household income >$100,000 (53.9%), and were on average 19.3 years of age (Table 1). There were significant differences across race/ethnicity observed for gender (p < 0.01), and household income (p < 0.01) (Table 1).
Identification of latent class health-related perceptions
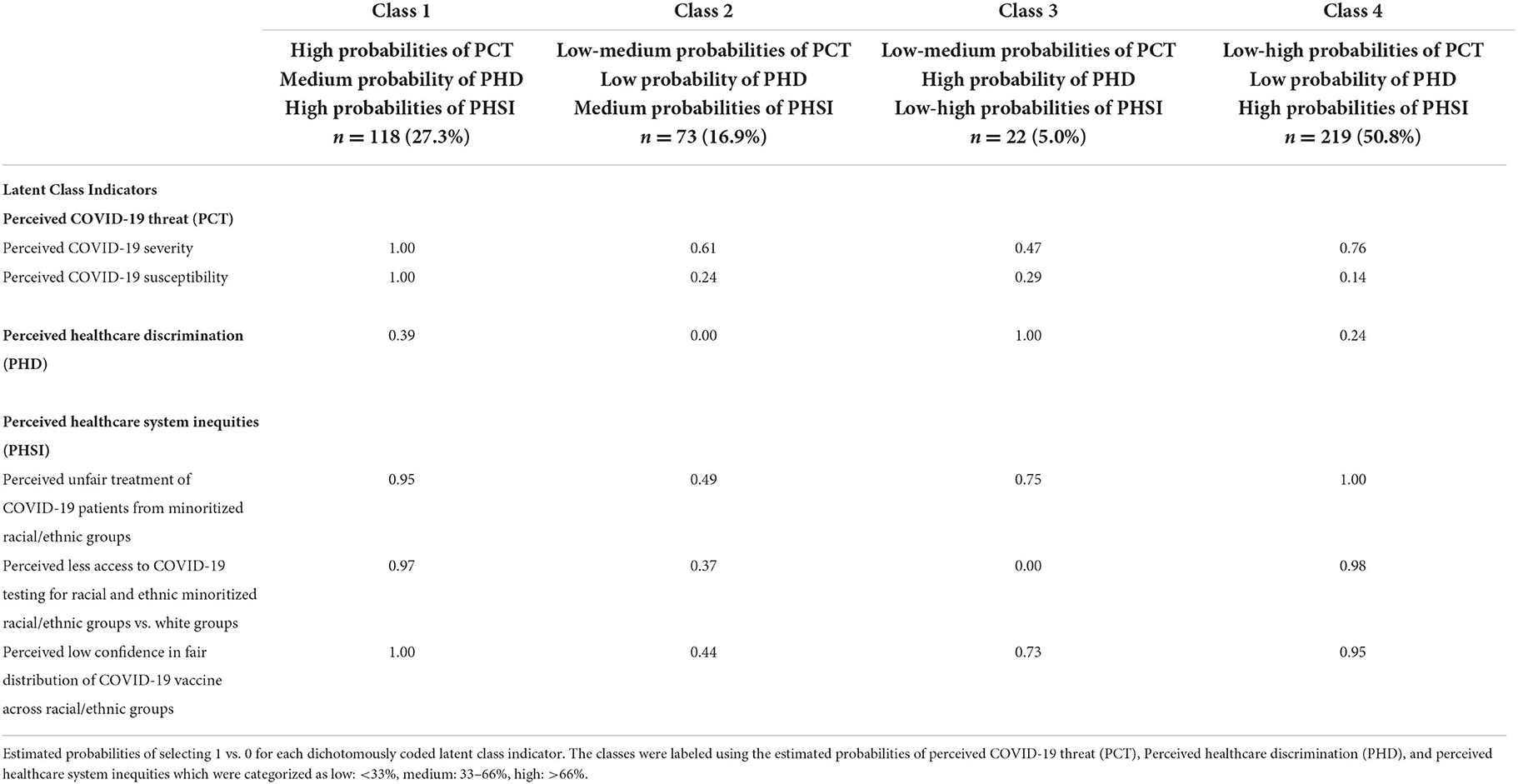
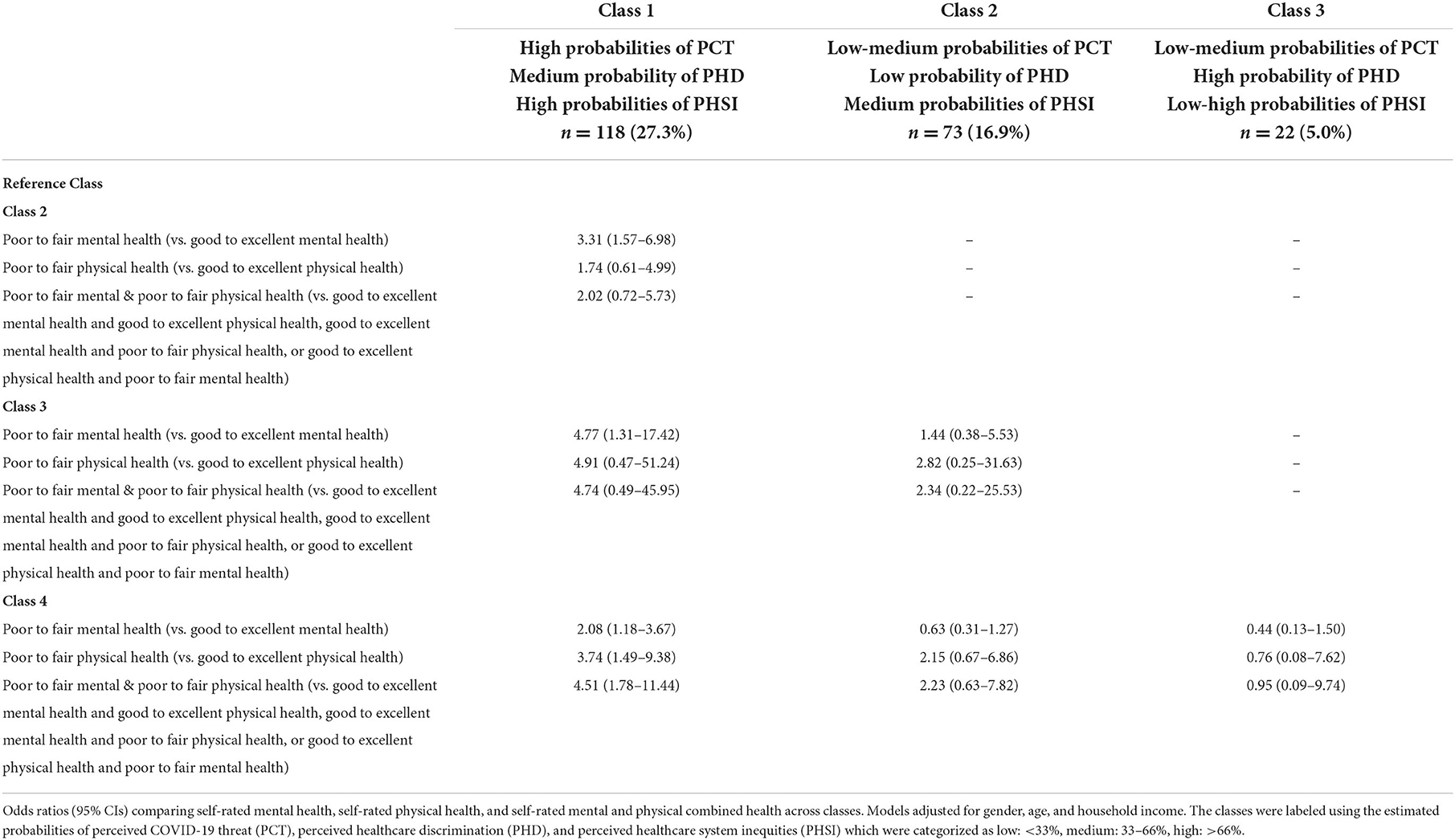
The four-class solution was selected as the best fitting model (Supplementary Table S2). The model without direct effects of the sociodemographic covariates on the indicators had lower SA-BIC than the model including these direct effects, therefore the final model did not include the direct effects. Classes were labeled using the estimated probabilities of perceived COVID-19 threat, healthcare discrimination, and U.S. healthcare system inequities (Table 2; Figure 1). Students in Class 1 (27.3% of the sample) had high probabilities of perceived COVID-19 threat, a medium probability of perceived healthcare discrimination, and high probabilities of perceived U.S. healthcare system inequities. Students in Class 2 (16.9%) had low to medium probabilities of perceived COVID-19 threat, a low probability of perceived healthcare discrimination, and medium probabilities of perceived U.S. healthcare system inequities. Students in Class 3 (5.0%) had low to medium probabilities of perceived COVID-19 threat, a high probability of perceived healthcare discrimination, and low to high probabilities of perceived U.S. healthcare system inequities. Students in Class 4 (50.8%) had low to high probabilities of perceived COVID-19 threat, a low probability of perceived healthcare discrimination, and high probabilities of perceived U.S. healthcare system inequities.
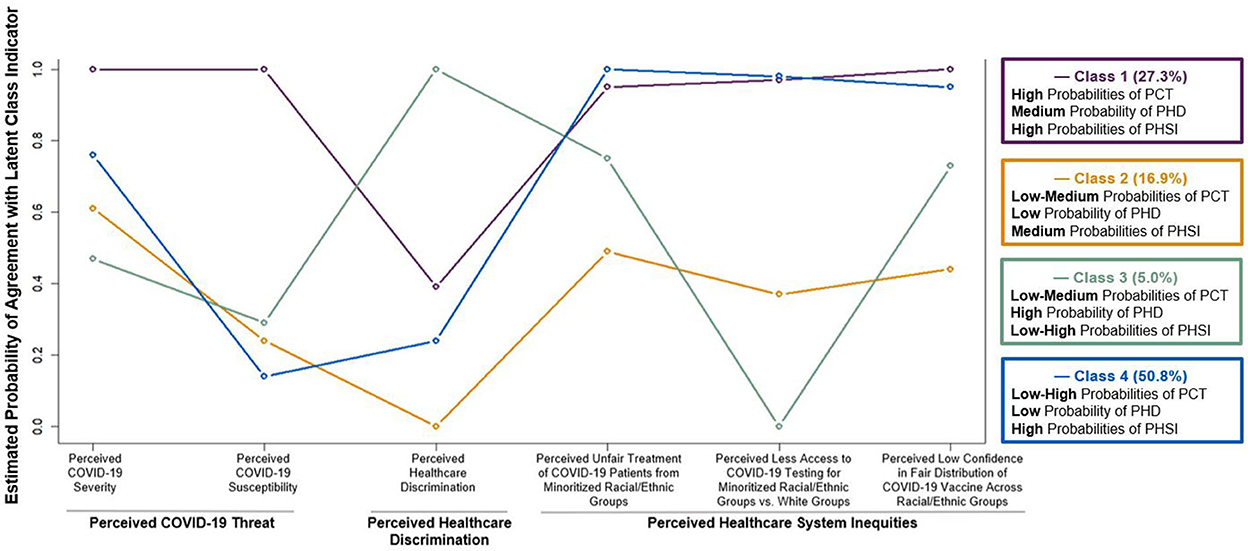
Figure 1. Four-class solution of perceived COVID-19 threat (PCT), perceived healthcare discrimination (PHD), and perceived healthcare system inequities (PHSI). Estimated probabilities of selecting 1 vs. 0 for each dichotomously coded latent class indicator. The classes were labeled using the estimated probabilities of perceived COVID-19 threat, perceived healthcare discrimination, and perceived healthcare system inequities which were categorized as low: <33%, medium: 33–66%, high: >66%.
Racial/ethnic differences in latent class membership
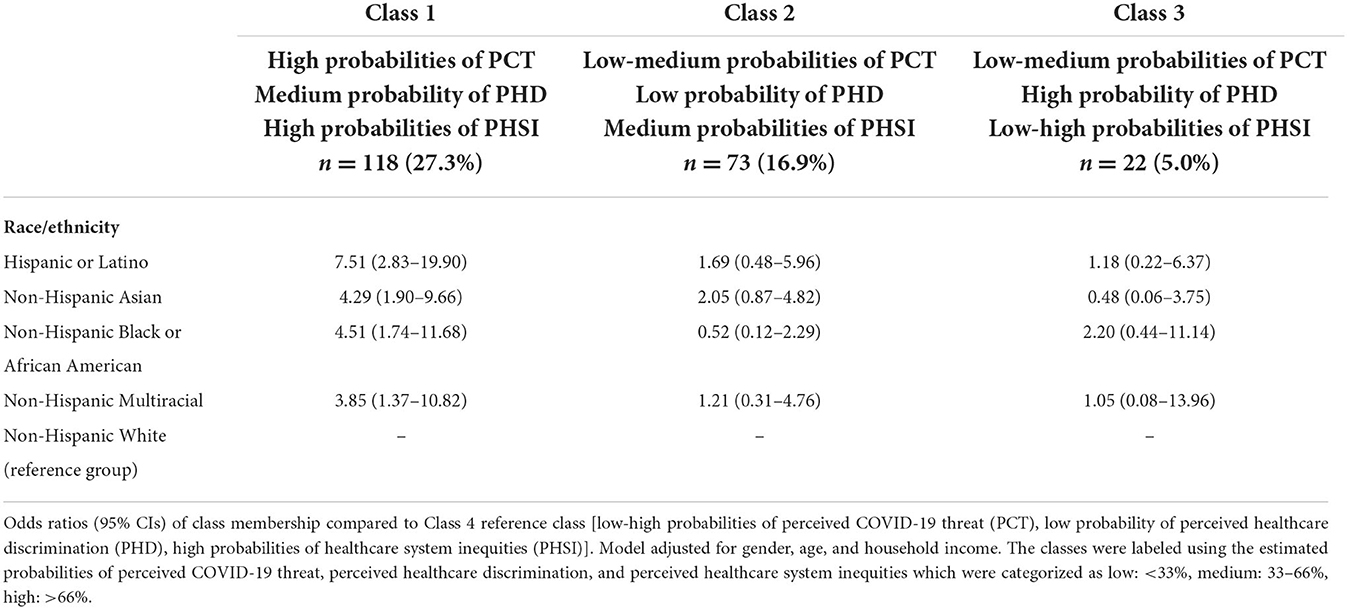
Compared to students in Class 4 (reference group), students in Class 1 had higher odds of self-identifying as Hispanic or Latino, Non-Hispanic Asian, Non-Hispanic Black or African American, and Non-Hispanic Multiracial compared to Non-Hispanic White [OR: 7.51 (95% CI: 2.83–19.90), OR: 4.29 (95% CI: 1.90–9.66), OR: 4.51 (95% CI: 1.74–11.68), OR: 3.85 (95% CI: 1.37–10.82), respectively] (Table 3). Students' race/ethnicity did not vary between the remaining classes.
Associations between latent class health-related perceptions and self-rated mental and physical health
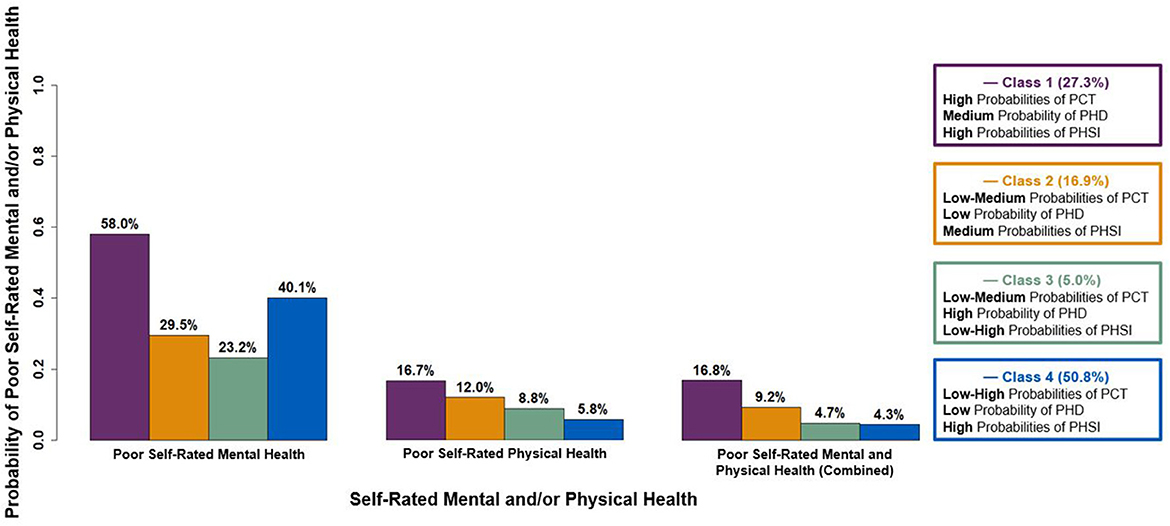
The probabilities of poor self-rated mental and/or physical health for each latent class are presented in Figure 2. Compared to all other classes, students in Class 1 had higher odds of poor to fair mental health vs. good to excellent mental health [Class 1 vs. Class 2 OR: 3.31 (95% CI: 1.57–6.98), Class 1 vs. Class 3 OR: 4.77 (95% CI: 1.31–17.42), Class 1 vs. Class 4 OR: 2.08 [95% CI: 1.18–3.67)] (Table 4). Compared to Class 4, students in Class 1 had higher odds of poor to fair physical health vs. good to excellent physical health [OR: 3.74 (95% CI: 1.49–9.38)]. Class 1 had higher odds of poorer combined health compared to Class 4 (i.e., poor to fair mental and physical health vs. other categories of combined health that included good to excellent mental and/or physical health) [OR: 4.51 (95% CI: 1.78–11.44)]. In addition, Class 1 had higher odds of poorer combined health compared to all other classes (i.e., categories of combined health that included poor to fair mental and/or physical health vs. good to excellent mental and physical health) [Class 1 vs. Class 2 OR: 2.84 (95% CI: 1.37–5.90), Class 1 vs. Class 3 OR: 3.92 (95% CI: 1.14–13.43), Class 1 vs. Class 4 OR: 1.91 (95% CI: 1.08–3.37)] (Supplementary Table S3).
Discussion
The present study revealed racial/ethnic differences in latent class membership of health-related perceptions in a sample of college students. Students in Class 1 were more likely to identify as Hispanic or Latino, Non-Hispanic Asian, Non-Hispanic Black or African American, and Non-Hispanic Multiracial vs. Non-Hispanic White (compared to Class 4, reference group). Students in Class 1 had high probabilities of perceived COVID-19 threat, medium probability of perceived healthcare discrimination, and high probabilities of perceived U.S. healthcare system inequities and were more likely to report poorer mental and physical health compared to Class 4.
These findings are consistent with research that separately examined perceived COVID-19 threat, healthcare discrimination, and U.S. healthcare system inequities as predictors of mental and physical health outcomes (6, 14, 34–38). The present study examined the constructs collectively as indicators of underlying perceptions of COVID-19 threat, healthcare discrimination, and U.S. healthcare system inequities and found that distinct classes of these perceptions were associated with students' mental and physical health. In the COVID-19 context, much of the existing literature on college students' health-related perceptions examined the influence of perceived COVID-19 threat on preventive behaviors (39), therefore, this study extends prior research by focusing on the association between these health-related perceptions and self-rated mental and physical health. This extension has wide-reaching implications given that self-rated health is a rich, complex construct previously associated with biomarkers of stress, chronic disease, and mortality (40).
In addition, this study suggests potential processes underlying racial/ethnic differences in latent class membership and mental and physical health. Given that perceived COVID-19 threat was previously associated with greater stress and/or anxiety (41, 42), it is possible that higher perceived COVID-19 threat contributed to greater stress, and in turn, poorer mental and physical health for students in Class 1 compared to students in other classes with lower perceived COVID-19 threat. Moreover, since students in Class 1 were more likely to belong to minoritized racial/ethnic groups, their higher perceived COVID-19 threat may have been due to national racial/ethnic disparities in COVID-19 rates (43) as suggested in recent studies (15). The present study aligns with prior suggestions that racial/ethnic structural inequalities and national COVID-19 disparities may contribute to increased stress among college students (15), particularly for students from minoritized racial/ethnic groups. However, there is also recent evidence that students who identified as female and Black, Indigenous, and/or students of color had lower perceived stress over the course of the COVID-19 pandemic (44). Given the mixed evidence on racial/ethnic disparities in college students' health (5, 14, 24, 25), it is important for future studies to continue examining stress processes related to perceived COVID-19 threat and racial/ethnic differences in these relationships.
Furthermore, consistent with evidence in general adult populations (45, 46), students in Class 1 were more likely to perceive healthcare discrimination and report poorer mental and physical health compared to Class 4. Students in Class 1 may have expected a greater likelihood of interacting with healthcare providers due to their higher concerns over contracting the COVID-19 virus. Given that anticipated discrimination was previously associated with increased stress among African American and Latina American college students (47, 48), higher probability of healthcare discrimination for students in Class 1 may have resulted in greater stress and poorer mental and physical health compared to those in Class 4. Again, since students in Class 1 were more likely to belong to minoritized racial/ethnic groups, these findings may help explain recent evidence of racial/ethnic disparities in college students' mental health (5, 24).
Lastly, students in Classes 1 and 4 had relatively equal probabilities of perceiving U.S. healthcare system inequities. It is possible, however, that perceived racial/ethnic disparities in health inequity were more stressful for students in Class 1 as their greater likelihood of belonging to minoritized racial/ethnic groups may have increased their perceived risk of experiencing these disparities compared to Class 4. Additionally, since individuals can experience stress from injustices committed against others within their same social group (49), it is also possible that students experienced stress due to racial/ethnic healthcare system inequities affecting others from their racial/ethnic groups. These proposed explanations suggest potential harms of structural inequalities on college students' stress and health, even for those who have not personally experienced disparities in COVID-19 services.
Several limitations should be considered. The study was cross-sectional, which limits the ability to establish causality and address bidirectionality (i.e., poorer self-rated health could influence health-related perceptions). In addition, study interpretations are based on health-related perceptions serving as stressors among college students, in turn affecting their mental and physical health. However, since this study did not directly measure stress, it is possible that alternative processes may explain differences in students' health. Additional research is needed to directly measure stress and examine its mediating role of health-related perceptions and self-rated mental and physical health. Furthermore, the study was conducted at one university with a relatively small sample of students who self-selected into the study. Additionally, students who selected their race as “Other” or identified as transgender, gender non-conforming, or selected gender as “not listed” were excluded due to small sample sizes, resulting in a lack of representation across all gender identities and racial/ethnic groups. These factors limit generalizability as the findings may not be representative of all college students in the U.S. Lastly, the survey was collected over a relatively long time period, and it is possible that the relationships between health-related perceptions and self-rated mental and physical health changed over the course of the study. To address this limitation, survey completion date was included as a covariate in the analysis to control for the potential effects of time. However, future studies may wish to further examine these potential relationships.
Despite these limitations, the study had many strengths. This study included both self-rated mental and physical health, which were previously understudied in prior literature, and examined these measures separately and in combination. Moreover, this study addressed multiple socio-ecological factors related to health-related perceptions (i.e., intrapersonal COVID-19 threat perceptions, interpersonal factors related to healthcare discrimination, and perceived structural issues in the U.S. healthcare system). The racial/ethnic group characteristics of the study sample were also highly reflective of the university's undergraduate population (50).
These findings highlight ways that the multilevel nature of health-related perceptions may contribute to racial/ethnic disparities in college students' health, particularly in relation to the COVID-19 pandemic. In addition to academic and social stressors (51), the present study suggests that COVID-19-related stressors can influence college students' mental and physical health and further emphasizes the unique needs of college students during the COVID-19 pandemic (7). Continued research in this area is warranted given worsening mental health among college students (52) and rising racial/ethnic disparities in college students' health due to COVID-19 health concerns (14, 15). Public health research may also consider the unique circumstances of COVID-19 that influence health-related perceptions [e.g., stronger alignment of perceived COVID-19 threat and objective COVID-19 risk among minoritized racial/ethnic groups compared to other diseases (53)]. This may present an opportunity to apply evidence from the COVID-19 pandemic to other chronic illnesses that disproportionately burden minoritized racial/ethnic populations. Together, this study contributes to a limited body of evidence on college students' perceptions of the U.S. healthcare system and suggests important ways that structural inequalities and racial/ethnic disparities in COVID-19 risk, healthcare discrimination, and concerns over U.S. healthcare system inequity may affect college students' health.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the University of Maryland, College Park Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
JRF: conceptualization, data curation, formal analysis, methodology, project administration, and writing—original draft. JSS: data curation, formal analysis, project administration, and writing—review and editing. YJC, JN, and NTJ: writing—review and editing. ATF: conceptualization, supervision, and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the Division of Intramural Research, National Institute on Minority Health and Health Disparities, and National Institutes of Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The contents and views in this manuscript are those of the authors and should not be construed to represent the views of the National Institute on Minority Health and Health Disparities, National Institutes of Health, or the Department of Health and Human Services.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1028344/full#supplementary-material
References
1. Lederer AM, Stolow JA. Will student contracts keep campuses safe from COVID-19? A behavioral science perspective. Public Health Rep. (2021) 136:274–80. doi: 10.1177/0033354921994899
2. Lu H, Weintz C, Pace J, Indana D, Linka K, Kuhl E. Are college campuses superspreaders? A data-driven modeling study. Comp Methods Biomech Biomed Eng. (2021) 24:1136–45. doi: 10.1080/10255842.2020.1869221
3. Smith-Schoenwalder C. U.S. Coronavirus Cases Increase as BA.2 Spreads. Washington, DC: U.S. News & World Report (2022).
4. Hollingsworth H, Khalil A. Mask Mandates Return to US College Campuses as Cases Rise. New York, NY: The Associated Press (AP) News (2022).
5. Browning MHEM, Larson LR, Sharaievska I, Rigolon A, McAnirlin O, Mullenbach L, et al. Psychological impacts from COVID-19 among university students: risk factors across seven states in the United States. PLoS ONE. (2021) 16:e0245327. doi: 10.1371/journal.pone.0245327
6. Chen AC-C, Han S, Li W, Leong KJ, Ou L. COVID-19 and Asian American college students: discrimination, fear, and mental health. J Emerg Manag. (2021) 19:121–31. doi: 10.5055/jem.0598
7. Lederer AM, Hoban MT, Lipson SK, Zhou S, Eisenberg D. More than inconvenienced: the unique needs of US college students during the COVID-19 pandemic. Health Educ Behav. (2021) 48:14–9. doi: 10.1177/1090198120969372
8. Harper SR. COVID-19 and the racial equity implications of reopening college and university campuses. Am J Educat. (2020) 127:153–62. doi: 10.1086/711095
9. Goldberg SB. Education in a Pandemic: The Disparate Impacts of COVID-19 on America's Students. Washington, DC: Department of Education (2021).
10. Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students' mental health in the United States: interview survey study. J Med Internet Res. (2020) 22:e21279–e21279. doi: 10.2196/21279
11. Reyes-Portillo JA, Masia Warner C, Kline EA, Bixter MT, Chu BC, Miranda R, et al. The psychological, academic, and economic impact of COVID-19 on college students in the epicenter of the pandemic. Emerg Adulth. (2022) 10:473–90. doi: 10.1177/21676968211066657
12. Farris SG, Kibbey MM, Fedorenko EJ, DiBello AM. A qualitative study of COVID-19 distress in university students. Emerg Adulth. (2021) 9:462–78. doi: 10.1177/21676968211025128
13. Perz CA, Lang BA, Harrington R. Validation of the fear of COVID-19 scale in a US college sample. Int J Ment Health Addict. (2022) 20:273–83. doi: 10.1007/s11469-020-00356-3
14. Trammell Ph DJ, Joseph Ph DN, Harriger Ph DJ. Racial and ethnic minority disparities in COVID-19 related health, health beliefs and behaviors, and well-being among students. J Am Coll Health. (2021) 1–7. doi: 10.1080/07448481.2021.1890606
15. Correia KM, Bierma SR, Houston SD, Nelson MT, Pannu KS, Tirman CM, et al. Education racial and gender disparities in COVID-19 worry, stress, and food insecurities across undergraduate biology students at a southeastern university. J Microbiol Biol Educ. (2022) 0:e00224-00221.
16. Hoyt LT, Cohen AK, Dull B, Maker Castro E, Yazdani N. “Constant stress has become the new normal”: stress and anxiety inequalities among US college students in the time of COVID-19. J Adolesc Health. (2021) 68:270–6. doi: 10.1016/j.jadohealth.2020.10.030
17. Cowan E, Khan MR, Shastry S, Edelman EJ. Conceptualizing the effects of the COVID-19 pandemic on people with opioid use disorder: an application of the social ecological model. Addict Sci Clin Pract. (2021) 16:4. doi: 10.1186/s13722-020-00210-w
18. Wiltz JL, Feehan AK, Molinari NM, Ladva CN, Truman BI, Hall J, et al. Racial and ethnic disparities in receipt of medications for treatment of COVID-19 — United States, March 2020–August 2021. Morbid Mortal Wkly Rep. (2022) 71:96–102. doi: 10.15585/mmwr.mm7103e1
19. Artiga S, Corallo B, Pham O. Racial Disparities in COVID-19: Key Findings from Available Data Analysis. Kaiser Family Foundation (KFF) (2020). Available online at: https://www.kff.org/report-section/racialdisparities-in-covid-19-key-findings-from-available-data-and-analysis-issue-brief/
20. Njoku A, Joseph M, Felix R. Changing the narrative: structural barriers and racial and ethnic inequities in COVID-19 vaccination. Int J Environ Res Public Health. (2021) 18:9904. doi: 10.3390/ijerph18189904
21. Yang C, Chen A, Chen Y. College students' stress and health in the COVID-19 pandemic: the role of academic workload, separation from school, and fears of contagion. PLoS ONE. (2021) 16:e0246676. doi: 10.1371/journal.pone.0246676
22. Hasratian AM, Nordberg HO, Meuret AE, Ritz T. Fear and coping in students during the early stages of the COVID-19 pandemic: a combined cross-sectional and longitudinal study. Int J Environ Res Public Health. (2021) 18:6551. doi: 10.3390/ijerph18126551
23. Wheaton MG, Prikhidko A, Messner GR. Is fear of COVID-19 contagious? The effects of emotion contagion and social media use on anxiety in response to the coronavirus pandemic. Front Psychol. (2021) 11:567379. doi: 10.3389/fpsyg.2020.567379
24. Freibott CE, Stein MD, Lipson SK. The influence of race, sexual orientation and gender identity on mental health, substance use, and academic persistence during the COVID-19 pandemic: a cross-sectional study from a national sample of college students in the healthy minds study. Drug Alcohol Depend Rep. (2022) 3:100060. doi: 10.1016/j.dadr.2022.100060
25. Goldmann E, Hagen D, Khoury EE, Owens M, Misra S, Thrul J. An examination of racial and ethnic disparities in mental health during the Covid-19 pandemic in the US South. J Affect Disord. (2021) 295:471–8. doi: 10.1016/j.jad.2021.08.047
26. Shanahan L, Bauldry S, Freeman J, Bondy CL. Self-rated health and C-reactive protein in young adults. Brain Behav Immun. (2014) 36:139–46. doi: 10.1016/j.bbi.2013.10.020
27. Benyamini Y. Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologists. Psychol Health. (2011) 26:1407–13. doi: 10.1080/08870446.2011.621703
28. Sherchan J, Fernandez JR, Qiao S, Kruglanski AW, Forde AT. Perceived COVID-19 threat, perceived healthcare system inequities, personal experiences of healthcare discrimination and their associations with COVID-19 preventive behavioral intentions among college students in the U.S. BMC Public Health. (2022). doi: 10.1186/s12889-022-14438-5
29. Rich R, Paschal A. US college students' perceptions of social determinants of health, health equity and racial health disparities. Health Educ J. (2020) 79:700–11. doi: 10.1177/0017896920910175
30. Race-Related Stressors and Health Disparities Laboratory. Bethesda, MD: National Institute on Minority Health and Health Disparities, National Institutes of Health (2021).
31. Magwene EM, Quiñones AR, Marshall GL, Makaroun LK, Thielke S. Older adults rate their mental health better than their general health. J Public health Res. (2017) 6:967–967. doi: 10.4081/jphr.2017.967
32. Bowling A. Just one question: If one question works, why ask several? J Epidemiol Commun Health. (2005) 59:342–5. doi: 10.1136/jech.2004.021204
33. Vermunt JK. Latent class modeling with covariates: two improved three-step approaches. Polit Anal. (2010) 18:450–69. doi: 10.1093/pan/mpq025
34. Lee J, Solomon M, Stead T, Kwon B, Ganti L. Impact of COVID-19 on the mental health of US college students. BMC Psychol. (2021) 9:95. doi: 10.1186/s40359-021-00598-3
35. Zhang W, Xiong S, Zheng Y, Wu J. Response efficacy and self-efficacy mediated the relationship between perceived threat and psychic anxiety among college students in the early stage of the COVID-19 pandemic. Int J Environ Res Public Health. (2022) 19:2832. doi: 10.3390/ijerph19052832
36. Ahnquist J, Wamala SP, Lindström M. What has trust in the health-care system got to do with psychological distress? Analyses from the national Swedish survey of public health. Int J Qual Health Care. (2010) 22:250–8. doi: 10.1093/intqhc/mzq024
37. Mays VM, Jones AL, Delany-Brumsey A, Coles C, Cochran SD. Perceived discrimination in health care and mental health/substance abuse treatment among Blacks, Latinos, and Whites. Med Care. (2017) 55:173–81. doi: 10.1097/MLR.0000000000000638
38. Lee C, Ayers SL, Kronenfeld JJ. The association between perceived provider discrimination, healthcare utilization and health status in racial and ethnic minorities. Ethn Dis. (2009) 19:330–7.
39. Alsulaiman SA, Rentner TL. The use of the health belief model to assess US college students' perceptions of COVID-19 and adherence to preventive measures. J Public Health Res. (2021) 10:2273. doi: 10.4081/jphr.2021.2273
40. Bombak AE. Self-rated health and public health: a critical perspective. Front Public Health. (2013) 1:15–15. doi: 10.3389/fpubh.2013.00015
41. Shinan-Altman S, Levkovich I. Emotional reactions towards COVID-19 among persons with diabetes. Int Health. (2021) 14:170–5. doi: 10.1093/inthealth/ihab024
42. Eichenberg C, Grossfurthner M, Andrich J, Hübner L, Kietaibl S, Holocher-Benetka S. The relationship between the implementation of statutory preventative measures, perceived susceptibility of COVID-19, and personality traits in the initial stage of corona-related lockdown: a German and Austrian Population Online Survey. Front Psychiatry. (2021) 12:596281. doi: 10.3389/fpsyt.2021.596281
43. Renelus BD, Khoury NC, Chandrasekaran K, Bekele E, Briggs WM, Ivanov A, et al. Racial disparities in COVID-19 hospitalization and in-hospital mortality at the height of the New York City pandemic. J Racial Ethn Health Dispar. (2021) 8:1161–7. doi: 10.1007/s40615-020-00872-x
44. Burt KG, Eubank JM, Orazem J. Female black, indigenous, and students of color demonstrate greater resilience than other students during a global pandemic. Equity Educ Soc. (2022) 1:202–15. doi: 10.1177/27526461221105094
45. Hausmann LRM, Jeong K, Bost JE, Ibrahim SA. Perceived discrimination in health care and health status in a racially diverse sample. Med Care. (2008) 46:905–14. doi: 10.1097/MLR.0b013e3181792562
46. Schulson LB, Paasche-Orlow MK, Xuan Z, Fernandez A. Changes in perceptions of discrimination in health care in California, 2003 to 2017. JAMA Netw Open. (2019) 2:e196665. doi: 10.1001/jamanetworkopen.2019.6665
47. Sawyer PJ, Major B, Casad BJ, Townsend SSM, Mendes WB. Discrimination and the stress response: psychological and physiological consequences of anticipating prejudice in interethnic interactions. Am J Public Health. (2012) 102:1020–6. doi: 10.2105/AJPH.2011.300620
48. Clark R. Perceptions of interethnic group racism predict increased vascular reactivity to a laboratory challenge in college women. Ann Behav Med. (2000) 22:214–22. doi: 10.1007/BF02895116
49. Chae DH, Yip T, Martz CD, Chung K, Richeson JA, Hajat A, et al. Vicarious racism and vigilance during the COVID-19 pandemic: mental health implications among Asian and Black Americans. Public Health Rep. (2021) 136:508–17. doi: 10.1177/00333549211018675
50. University of Maryland College Park Office of Institutional Research PA: UMD Undergraduate Student Profile (2021).
51. Haikalis M, Doucette H, Meisel MK, Birch K, Barnett NP. Changes in college student anxiety and depression from pre- to during-COVID-19: perceived stress, academic challenges, loneliness, and positive perceptions. Emerg Adulth. (2022) 10:534–45. doi: 10.1177/21676968211058516
52. Copeland WE, McGinnis E, Bai Y, Adams Z, Nardone H, Devadanam V, et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. (2021) 60:134–41.e132. doi: 10.1016/j.jaac.2020.08.466
53. Edwards LV, Lindong I, Brown L, Hawkins AS, Dennis S, Fajobi O, et al. None of us will get out of here alive: the intersection of perceived risk for HIV, risk behaviors and survival expectations among African American emerging adults. J Health Care Poor Underserved. (2017) 28:48–68. doi: 10.1353/hpu.2017.0052
Keywords: college students, race/ethnicity, COVID-19 threat, healthcare discrimination, U.S. healthcare system inequities
Citation: Fernandez JR, Sherchan JS, Cho YJ, Nanaw J, Joseph NT and Forde AT (2023) College students' underlying perceptions of COVID-19 threat, healthcare discrimination, and healthcare system inequities associated with self-rated health across racial/ethnic groups in the U.S. Front. Public Health 10:1028344. doi: 10.3389/fpubh.2022.1028344
Received: 25 August 2022; Accepted: 23 November 2022;
Published: 06 January 2023.
Edited by:
Mingwei Wang, Affiliated Hospital of Hangzhou Normal University, ChinaReviewed by:
Jenny Flagler-George, University of Waterloo, CanadaDeukwoo Kwon, University of Miami, United States
Copyright © 2023 Fernandez, Sherchan, Cho, Nanaw, Joseph and Forde. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jessica R. Fernandez, amVzc2ljYS5mZXJuYW5kZXpAbmloLmdvdg==
 Jessica R. Fernandez
Jessica R. Fernandez Juliana S. Sherchan
Juliana S. Sherchan Yong Ju Cho
Yong Ju Cho Judy Nanaw1
Judy Nanaw1