
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 04 January 2023
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1024436
This article is part of the Research TopicMapping Symptom Networks among Co-occurrence of Psychological and Somatic SymptomsView all 6 articles
 Huan Wen1
Huan Wen1 Zheng Zhu2,3*
Zheng Zhu2,3* Tiantian Hu2
Tiantian Hu2 Cheng Li2
Cheng Li2 Tao Jiang2
Tao Jiang2 Ling Li2
Ling Li2 Lin Zhang4
Lin Zhang4 Yanfen Fu5
Yanfen Fu5 Shuyu Han6
Shuyu Han6 Bei Wu7
Bei Wu7 Yan Hu2,3*
Yan Hu2,3*Background: People living with HIV (PLWH) experience multiple psychological symptoms. Few studies have provided information on central and bridge psychological symptoms among PLWH. This information has implications for improving the efficiency and efficacy of psychological interventions. Our study aimed to identify the central and bridge psychological symptoms of PLWH and to explore the interconnectedness among symptoms and clusters.
Methods: Our study used data from the HIV-related Symptoms Monitoring Survey, a multisite, cross-sectional study conducted during 2017–2021. We used R to visualize the network of 16 symptoms and analyzed the centrality and predictability indices of the network. We further analyzed the bridge symptoms among the three symptom clusters.
Results: A total of 3,985 participants were included in the analysis. The results suggested that sadness had the highest strength (rS = 9.69) and predictability (70.7%) compared to other symptoms. Based on the values of bridge strength, feeling unsafe (rbs = 0.94), uncontrollable worry (rbs = 0.82), and self-abasement (rbs = 0.81) were identified as bridge symptoms. We also found a strong correlation between sadness and self-abasement (r = 0.753) and self-loathing and self-blame (r = 0.744).
Conclusion: We found that sadness was the central psychological symptom of PLWH, indicating that sadness was the center of the psychological symptom network from a mechanistic perspective and could be a target for intervention. Deactivating bridge symptoms, including “feeling unsafe,” “self-abasement,” and “uncontrollable worry,” could be more effective in preventing symptom activation from spreading (e.g., one symptom activating another).
According to the Joint United Nations Program on HIV/AIDS (UNAIDS), as of 2021, there were 38.4 million people living with HIV/AIDS (PLWH) worldwide (1). PLWH commonly experience multiple psychological symptoms due to the diagnosis of the disease, stigma, social discrimination and the side effects of antiretroviral therapy (2). Previous studies have shown that the prevalence of psychological symptoms is significantly higher in PLWH than in the general population (3, 4). A recent study in China indicated that 61% of PLWH had depressive symptoms (5). Kendall et al. (6) conducted a cross-sectional study and found that 41% of PLWH reported multiple simultaneous psychological symptoms compared to 22% of adults without HIV. High symptom prevalence and severity not only contribute to great mental suffering but also lead to physical comorbidities and a lower quality of life (7, 8). Another study focused on the psychological symptoms of PLWH confirmed that psychological symptoms play a role in risky sexual behaviors and that interventions targeting psychological symptoms might prevent the occurrence of risky sexual behaviors (7). Levy et al. (8) examined the associations between psychosocial risk factors and subclinical atherosclerosis among women living with HIV and among HIV-negative women and concluded that psychological symptoms could increase the risk of atherosclerosis in women living with HIV. PLWH living in poor areas also have a higher number of mental disorders or psychological symptoms because they tend to have less access to health care services (9, 10).
Current interventions for psychological symptoms in PLWH have some limitations; for example, they may ignore the interaction among multiple symptoms and strength of symptom connection experienced by PLWH in the real world. This may lead to low efficiency and accuracy in the management of co-occurring symptoms. For PLWH, the persistent range of psychological reactions is often caused by strong interactions and feedback loops among various negative emotions (11). By constructing a symptom network and finding symptoms with high centrality, we can identify the most influential symptoms in the network and discover the role of central symptoms on other symptoms, which would allow us to focus on precise symptom intervention (12). Bridge symptoms connect different clusters of symptoms or subgroups of symptoms within the same cluster (13). If we can identify the central and bridge symptoms among symptom clusters in PLWH, the effectiveness and efficiency of psychotherapeutic interventions could be increased.
Central symptoms are identified through the centrality indices of strength, betweenness, and closeness. Strength is an indicator of network connectivity and corresponds to the sum of the absolute edge weights connected to each node (14). Betweenness indicates the frequency of a node on the shortest path between other nodes. Closeness represents the inverse of the sum of distances from one node to all other nodes in the network (14). Among these three centrality indices, strength has been most emphasized. Some studies have concluded that betweenness centrality and closeness centrality are less applicable (15–17). Bringmann et al. (12) found that for psychological networks, betweenness and closeness were not suitable indices of node importance. We usually identify bridge symptoms based on bridge centrality indices (18).
Previous studies have shown that central and bridge symptoms play important roles in clinical psychotherapy for PLWH (19, 20). Central symptoms are the most central symptoms in the symptom network from a mechanistic perspective. They are strongly correlated with and have the most interactions with other symptoms in the symptom network. Therefore, targeting central symptoms for psychological intervention treatment can accelerate the deactivation of the network and improve the precision and efficiency of the intervention (19, 21–23). Although there is now controversy about bridge symptoms, most studies have shown that bridge symptoms are associated with comorbidity and cluster structures in the symptom network (13, 24–26). Comorbidity and clusters can impede the progress of interventions to treat psychological symptoms; therefore, bridge symptoms also deserve priority attention (27–29). Previous studies have suggested that interventions targeting bridge symptoms are more effective than those targeting other symptoms (18, 27–30).
However, few studies provided information regarding central and bridge symptoms in PLWH, which is crucial for enhancing the efficiency and efficacy of psychological interventions. Therefore, we aimed to identify the central and bridge psychological symptoms of PLWH and to explore the complex interconnectedness among symptoms by developing symptom networks.
Our study used data from the HIV-related Symptoms Monitoring Survey (HSMS), a multisite, cross-sectional dataset of Chinese PLWH collected by the authors during 2017–2021. Participants were recruited from 11 cities in eastern (Shanghai), central (Hengyang), and southwestern (Nanning, Ruili, Kunming, Tengchong, Longxing, Changning, Baoshan, Lincang, and Changning) China. The inclusion criteria were as follows: (1) diagnosed with HIV infection and (2) aged 18 years or older. The exclusion criteria were as follows: (1) unable to complete the self-rating scale and (2) a diagnosis of an HIV-associated neurocognitive disorder based on the DSM. A total of 3,985 questionnaires were obtained. All questionnaires were distributed and collected on the spot. Our study obtained the consent of the hospital. Written informed consent was obtained from all subjects before the study. The Institutional Review Board of Fudan University School of Nursing approved this study (IRB# TYSA2016-3-1, IRB# TYSQ2020-4-06). Additional details on the HSMS have been published elsewhere (31, 32). This questionnaire has been used in many published studies (32, 33).
We used a self-administered questionnaire to collect sociodemographic and clinical data. The sociodemographic variables included age, gender, ethnicity, education level, employment status, marital status, and primary caregiver. The clinical data included years since HIV diagnosis and latest CD4+ T-cell count.
We used a self-administered questionnaire to collect information on 16 highly prevalent HIV/AIDS-related psychological symptoms. These symptoms were selected based on previous studies and have high prevalence and high specificity for PLWH (32). In our team's previous study, according to severity, the 16 psychological symptoms were categorized into three clusters: emotions, personality traits, and cognitive processes (33). Emotions refer to a temporary state of mind or feeling. Symptoms in the emotion cluster can fluctuate and change over short periods, while symptoms in the personality trait cluster are persistent over time (34). Personality traits refer to a relatively stable, consistent, and enduring internal characteristic that is inferred from a pattern of behaviors, attitudes, feelings, and habits in the individual (34). Cognitive processes refer to the mental function involved in acquisition, storage, and interpretation (35). Emotions included “feeling nervous, anxious or on edge,” “feeling down, depressed or hopeless,” fear, anger, panic, sadness, loneliness, shame, and feeling overwhelming pressure. Personality traits included “not being able to stop or control worrying,” “little interest or pleasure in doing things,” impulsivity, and feeling unsafe. Cognitive processes included self-abasement, self-loathing, and self-blame (33). The participants were asked, “During the last 4 weeks, did you have the following symptoms? If you did, please rate the severity of these symptoms.” Symptoms were scored 0–3, with higher scores indicating more severe symptoms. To evaluate the psychometric properties of the questionnaire, we included five experts for validation. The questionnaire showed good validity and reliability (33). In our sample, the questionnaire showed high expert validity (the content validity index was 0.918) and internal consistency (Cronbach's α = 0.961) (33).
Statistical analyses were conducted using SAS 9.4. The demographic characteristics were described using frequencies, percentages, means, and standard deviations. We used the qgraph package in R to construct an undirected network model with all 16 symptoms. In the symptom network, each node represented one symptom, and the edges between two nodes represented Spearman correlation relationships between two symptoms. The thicker the edge was, the stronger the correlation between the two symptoms (18, 36–38). We used r to indicate the Spearman correlation coefficient. The Fruchterman-Reingold algorithm was used to visualize the network (39), with the strongest correlation nodes placed in the center of the network and nodes with similar characteristics placed relatively closer, while nodes with weak and few connections were placed on the periphery of the symptom network.
Strength centrality was used to identify central symptom. We used the R package qgraph to conduct centrality analysis. The strength is an indicator of network connectivity. When a symptom has a higher strength centrality, it is more likely to co-occur with other symptoms. The betweenness indicated the frequency of a node on the shortest path to any two other nodes. When a node had a higher betweenness centrality, it had more influence on the network. The closeness represented the average distance from a node to all other nodes. The larger the value of closeness centrality was, the shorter the overall path from that node to other nodes in the network was. Among these three centrality indices, strength was the main centrality indicator. Previous studies concluded that betweenness centrality and closeness centrality were less applicable (15, 40). Bridge strength centrality was used to identify bridge symptoms. Bridge symptoms were broadly defined as symptoms that connect different clusters of symptoms (13). The R package networktools was used to identify bridge symptoms and bridge strength among the three clusters. We used rS to indicate the strength centrality index and rbS to indicate the bridge strength centrality index.
We used the R package mgm to calculate the predictability for each node. Predictability is a metric that reflects the extent to which a node's variation can be explained by the variation in its connected nodes. The average predictability of all nodes in a network is usually used to reflect the extent to which the symptom network is influenced by external factors. When the average predictability of a group's symptom network is low, the difficulty of using external factors to alleviate symptoms may be higher (41). We used rp to indicate the predictability.
Bootstrapping methods were performed to assess the accuracy and stability of the network by using the R package bootnet. The accuracy was evaluated by calculating the 95% confidence intervals (CIs) for the edge weight values. We used non-parametric bootstrapping (1,000 bootstrap samples) to construct the CIs (42). The stability was evaluated by calculating the correlation stability coefficient of the strength centrality using a case-dropping subset bootstrap (1,000 bootstrap samples) (15, 16). The correlation stability coefficient should preferably be >0.5 but at the very least >0.25 (43). Finally, to identify whether the estimations of network connections and centrality for different variables differ, we performed bootstrapped difference tests among edge-weights and centrality indices in the LASSO regularization of partial correlation networks based on polychoric correlation matrices (15, 16). We used rcS to indicate the correlation stability coefficient. The significance was set at α = 0.05.
Table 1 shows the sample characteristics. The mean age of the participants was 39.60 ± 11.81 years, ranging from 18 to 87 years old. Among all participants, 73.5% were male. The majority of participants were employed (n = 3,818, 98.4%) and married (n = 1,705, 48.0%). Most of them were cared for by family members (n = 2,333, 58.9%). The majority had been diagnosed with HIV for 6 months to 3 years (n2 = 1,213, 30.6%), followed by 5–10 (n4 = 1,018, 25.7%), 3–5 (n3 = 620, 15.7%), >10 years (n5 = 571, 14.4%) and <6 months (n1 = 537, 13.6%). Most of them had undergone ART for <1 year (n = 1,055, 27.1%), followed by 5–10 (n = 984, 25.3%), 1–3 (n = 871, 22.4%), 3–5 (n = 648, 16.7%) and >10 years (n = 333, 8.6%).
Table 2 presents the prevalence and severity of all psychological symptoms. Feeling overwhelming pressure (n = 1,489, 37.37%) was the most prevalent symptom, followed by little interest or pleasure in doing things (n = 1,230, 30.87%) and feeling down, depressed or hopeless (n = 1,180, 29.61%). Feeling overwhelming pressure (0.55 ± 0.82) was the most severe symptom, followed by little interest or pleasure in doing things (0.40 ± 0.68) and feeling down, depressed or hopeless (0.39 ± 0.68).
We conducted regression analyses of age, gender, education level, employment status, marital status, primary caregiver, years since HIV diagnosis, and CD4+T-cell count with the total score of symptoms, and finally identified the covariates as age (P < 0.05), marital status (P < 0.05), primary caregiver (P < 0.05), and years since HIV diagnosis (P < 0.05). Covariates were controlled for in all network analyses.
Figure 1A shows the network of psychological symptoms. All the edges were positive. We found that four edges, uncontrollable worry and feeling nervous (r = 0.79), fear and panic (r = 0.75), sadness and self-abasement (r = 0.75), and self-loathing and self-blame (r = 0.74), were thicker than other edges, which means that these relationships were stronger than other correlations (P < 0.05).
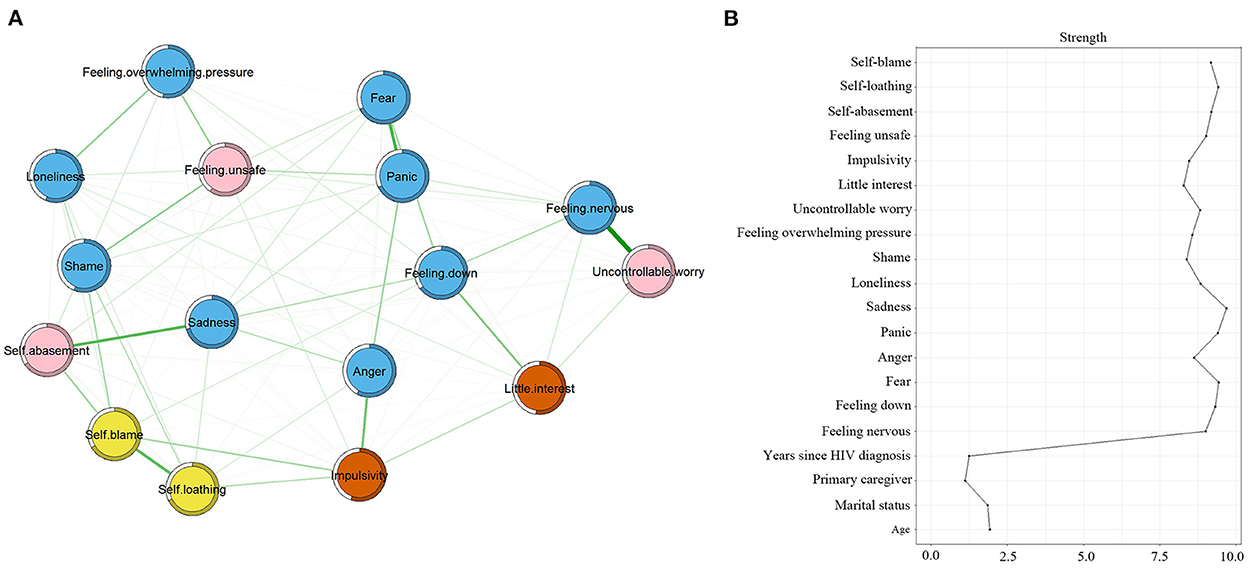
Figure 1. Symptom network and centrality index. (A) Symptoms network; (B) strength centrality index of the network. The same color represents the same symptom clusters and pink represents bridge symptoms. Bridge symptoms: feeling unsafe, self-abasement, and uncontrollable worry; Emotions: feeling nervous, feeling down, fear, anger, panic, sadness, loneliness, shame, feeling overwhelming pressure; Personality traits: uncontrollable worry, little interest, impulsivity, feeling unsafe; Cognitive processes: self-abasement, self-loathing, self-blame.
Figure 1A shows the bridge symptoms of the three domains. Figure 2 shows that feeling unsafe had the highest bridge strength centrality (rbS = 0.94), followed by uncontrollable worry (rbS = 0.82) and self-abasement (rbS = 0.81). The pink nodes represent bridge symptoms. Based on the values of strength centrality, feeling unsafe, self-abasement, and uncontrollable worry were identified as bridge symptoms. “Uncontrollable worry” and “feeling unsafe” connected the personality traits and emotion clusters, and “self-abasement” connected the cognitive processes and emotion clusters.
Figure 1B presents the strength centrality index. Sadness had the largest values for strength (rS = 9.69), followed by fear (rS = 9.44) and self-loathing (rS = 9.41). Predictability is presented as a circle around the node in Figure 1A. Table 2 shows that the node predictability values ranged from 52.2 to 70.7%. The average predictability value of 62.5% showed that neighboring nodes can explain 62.5% of the variance in the nodes in the symptom network on average. Sadness, feeling nervous, and panic had the highest predictability (rp), showing that 70.7, 69.8, and 68.2% of their variance can be explained by their neighbors.
Figure 3A shows the bootstrap analysis results of the edge weights. The bootstrapped CIs were small, which showed good accuracy of the network. For the subset bootstrap (Figure 3B), the correlation stability coefficient (rcS) was >0.5, suggesting that the network remained stable.
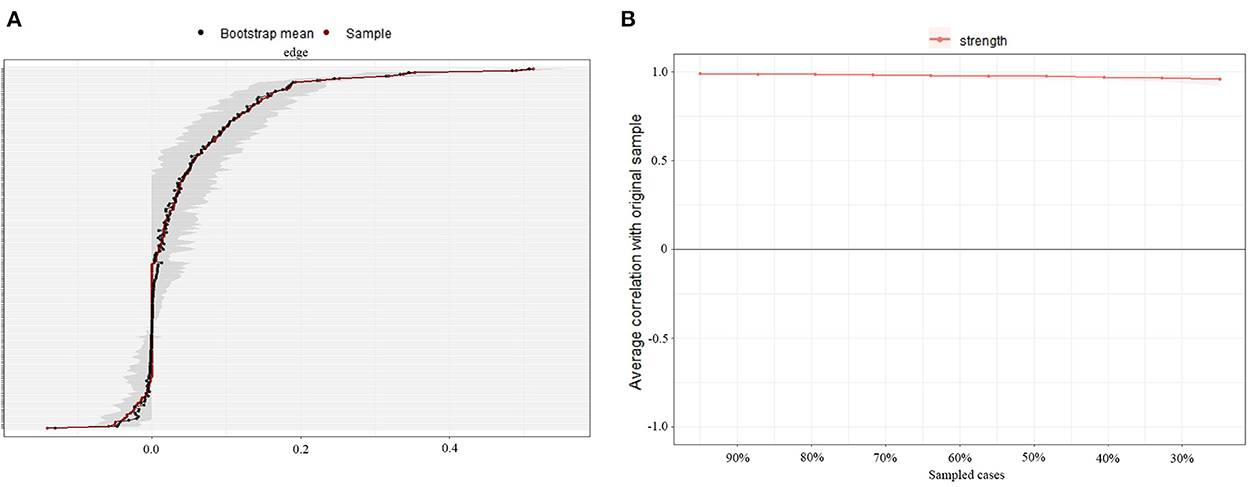
Figure 3. Accuracy and stability analysis of the symptom network. (A) Accuracy analysis of the edge weights; (B) Stability analysis of the strength centrality.
Figure 4 shows the results of the bootstrapped difference test. Black boxes represent statistically significant differences in two edge weights or two strength centralities of nodes (P < 0.05). Gray boxes represent differences that were not statistically significant (P > 0.05). The bootstrapped difference test for edge weights showed that the four strongest edge weights, uncontrollable worry and feeling nervous, fear and panic, sadness and self-abasement, and self-loathing and self-blame, were significantly different from ~95% of the other edge weights (Figure 4A). Bootstrapped difference tests for node strength show that in the current network, the strength centrality of sadness, panic, self-loathing, and feeling nervous are significantly different from that of other symptoms (Figure 4B).
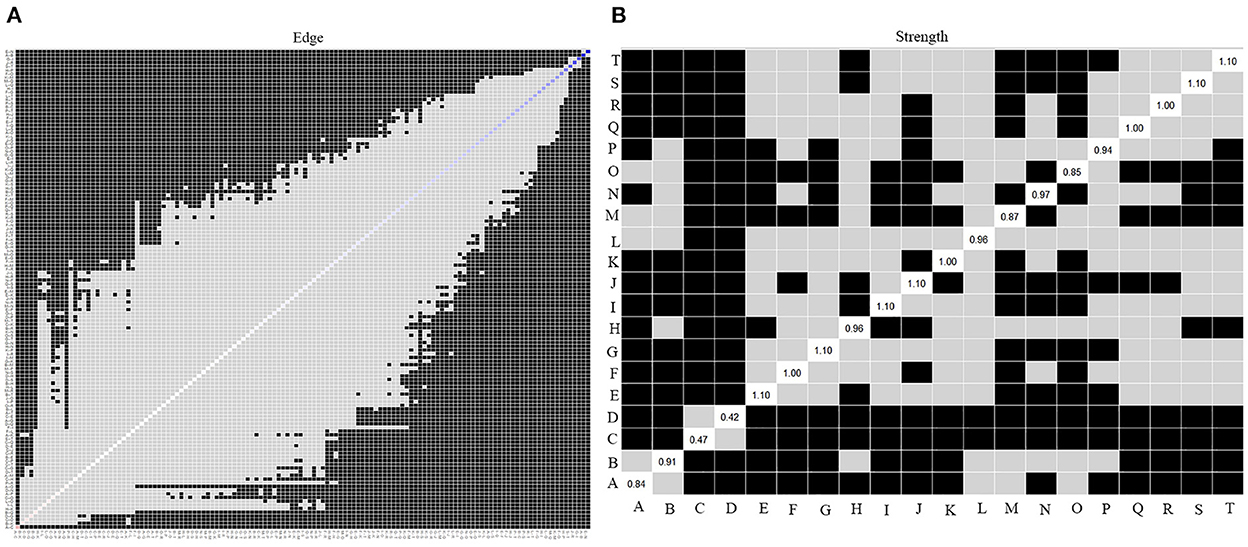
Figure 4. Bootstrapped difference test of the symptom network. (A) Bootstrapped difference test of the edge weights; (B) Bootstrapped difference test of the strength centrality. A, age; B, marital status; C, primary caregiver; D, years since HIV diagnosis; E, feeling nervous; F, feeling down; G, fear; H, anger; I, panic; J, sadness; K, loneliness; L, shame; M, feeling overwhelming pressure; N, uncontrollable worry; O, little interest; P, impulsivity; Q, feeling unsafe; R, self-abasement; S, self-loathing; T, self-blame.
This is the first study to develop a psychological symptom network based on a large sample of PLWH and identify the central and bridge psychological symptoms in PLWH. We found that sadness was the central symptom in PLWH and that three bridge symptoms existed among different clusters of psychological symptoms in PLWH. “Uncontrollable worry” and “feeling unsafe” connected the personality traits and emotions clusters, and “self-abasement” connected the cognitive processes and emotions clusters. Based on network theory, both central and bridge symptoms can represent promising intervention targets from different perspectives (13, 44–46). The network also showed four correlations between uncontrollable worry and feeling nervous, fear and panic, sadness and self-abasement, and self-loathing and self-blame that were significantly stronger than those of the other edges.
We found that sadness had the highest values of centrality and predictability of all the symptoms, indicating that sadness may be the central symptom in PLWH from a mechanism-based perspective. Previous studies reported that a central symptom could serve as the target in psychological interventions (44, 45). A central symptom may spread the intervention effects to the peripheral nodes of the central symptom, eventually leading to the remission or disappearance of the other symptoms (44). Targeting central symptoms in psychological intervention treatment can accelerate the deactivation of the symptom network and improve the precision and efficiency of the intervention (18, 20–23). Rodebaugh's study demonstrated that central symptoms can predict changes in other symptoms and can be good targets for treatment (45).
Sadness, as a highly self-focused negative emotion, is one of the emotional expressions of depressive states (47, 48). Most people with depression present with sadness at various stages of HIV survivorship (47). Daily stress, internalized stigma, perceived discrimination, and neurologic complications of ART were all risk factors and triggers for generating sadness. Sadness, as the central symptom, could activate other depressive symptoms and finally lead to the diagnostic criteria of depression.
In addition, previous studies have shown that sadness is closely related to physical, cognitive, and social factors and may aggravate other psychological symptoms. Previous studies found that sadness was associated with higher rates of mood reactivity, social impairment, physical complaints, and terminal insomnia (49, 50). Wu et al. concluded that there was a correlation between a greater level of sadness and more negative emotional tendencies based on a laboratory-based study (51). Rush et al. found that the presence of sadness was associated with a poor prognosis (52). Furthermore, long-term sadness has vital implications in terms of a high risk of suicide (53, 54). The relationship between sadness and the desire to commit suicide was noteworthy. It is accepted that PLWH may experience brief periods of sadness, which is regarded as a defense mechanism to protect them from stress and trauma (33). However, sadness may increase the connectivity of the symptom network, which is the prime property for detecting changes for prognosis (55). Healthcare providers should assess the duration of sadness and develop symptom networks for PLWH to evaluate connectivity by using mobile devices.
Fear and self-loathing also had high strength centrality values. The fear of PLWH involves “stigmatizing attitudes toward PLWH” and “fear of disclosure” (56). Previous studies have shown a positive correlation between fear of disclosure and reluctance to seek care, and addressing this fear can improve care-seeking behavior (56, 57). The factors that help PLWH overcome this fear include partner acceptance, peer, community and health professional support, and accurate knowledge of transmission risk (58). Self-loathing manifests through consistent negative thoughts. If self-loathing continues for too long, it can lead to more severe conditions, such as depression or anxiety (59). Fang et al. (60) conducted a repeated-measures survey and concluded that self-loathing may signal the personal depressive reactions of students to failure and unmet expectations of success.
Bridge symptoms were broadly defined as symptoms that connect different clusters of symptoms (13). Bridge symptoms help identify the interaction among different symptom clusters and, therefore, represent potential targets of effective intervention (46). Our network identified three bridge symptoms. “Uncontrollable worry” and “feeling unsafe” connected the personality traits and emotions clusters, and “self-abasement” connected the cognitive processes and emotions clusters. In clinical interventions and treatments, bridge symptoms could be considered psychotherapeutic targets for the deactivation of symptom cluster interactions (46). Kaiser et al. (61) study showed that interventions targeting bridge symptoms were more likely to be effective for all symptom clusters. Jones et al. (18) study found that deactivated symptoms based on bridge strength rather than symptom strength alone were more effective in preventing symptom activation from spreading. These studies suggested that interventions focusing on bridge symptoms were more effective than those focusing on random targets or non-targeted psychotherapeutic interventions. Therefore, based on our findings, the possibility of using bridge symptoms as targets to intervene in the severity and prevalence of symptom clusters of PLWH is proposed.
We also found that self-abasement, as a crucial self-focused emotion, demonstrated a strong correlation with sadness. A previous study showed that self-abasement manifested as a symptomatological pattern of depression in a society with a conservative culture (62). In our study, traditional Chinese health beliefs continued to exert an influence on the perception of HIV/AIDS. The stigma and discrimination experienced by PLWH may lead to a low level of self-esteem. To protect themselves from being discriminated against, PLWH may tend to solve various types of medical and health issues on their own, which may lead to a chronic habit of placing more focus on themselves. Stroumpouki et al. (2) also found that PLWH excessively focused on themselves in emotional coping processes. It is crucial to relieve self-focused emotions, such as self-abasement, self-loathing, and self-discrimination, not by exaggerating PLWH self-emotional distress but by placing more emphasis on the consequences of disease for society overall (36, 63). Future efforts and interventions should increase PLWH's ability to view their HIV infection from both individual and social perspectives.
Previous studies have shown that uncontrollable worry increased the risk of anxiety disorders (64, 65). Additionally, uncontrollable worry can lead to impaired functioning in social, occupational and academic settings (66). Feeling unsafe may be related to social isolation, concerns about the economy, and fear of exposure (67, 68). Feeling unsafe was an important factor that was linked to the mental and physical health of PLWH, especially older PLWH (69). Previous studies have shown that feeling unsafe was associated with various mental health problems, including emotional problems and suicidal behavior (70). A study conducted in PLWH in rural Zambia concluded that feeling unsafe was associated with medication non-adherence, a higher level of stress, and more barriers to pill taking (71).
PLWH may have multiple concurrent symptoms. However, there is a shortage of health care professionals to provide symptom management services for all symptoms simultaneously. By identifying central and bridge symptoms, we can find psychotherapeutic targets among all concurrent symptoms. This approach could also enhance the efficiency and precision of symptom management. In future clinical symptom assessments and interventions, it is important to focus on not only severity indicators but also strength centrality and bridge strength centrality. Symptom networks can visualize the connections among symptoms and symptom clusters. The centrality indicators were analyzed to reflect the symptom interactions in the real world and provide targets for precise interventions. Currently, there is a shortage of health care workers, and frontline health care workers do not have enough energy to provide personalized and precise symptom management services. If we can identify the central symptom and bridge symptoms of PLWH, the efficiency and precision of clinical symptom intervention will be improved. Cognitive-behavioral therapy, such as cognitive reconstruction and emotional support, can be used in later interventions to target sadness, feeling unsafe, self-abasement, and uncontrollable worry (72, 73). By locating key populations through central symptoms, we can find the critical points in the symptoms for targeted interventions. In clinical practice, regular dynamic assessments and focused interventions are conducted in key populations.
This is the first study to explore the relationships among the psychological symptom networks of PLWH in a large sample, however it has some limitations. First, the data were cross-sectional. Therefore, we can only describe the relationship among symptoms without making any causal inferences. Future studies are warranted to validate our results in a longitudinal sample. Second, our study used one item to assess each symptom. Future research should validate our results using multi-item measures. Third, PLWH who were willing to participate in the study might differ from those who were not, which could underestimate the centrality of central symptom. Due to the budget and scope of the study, our study only covered eastern, middle, and southern China. Further research could expand to the whole Chinese population. We did not conduct a subgroup analysis based on the regions in this study. Further research could compare multiple centers and the economic and cultural impacts of different regions.
Our study identified central and bridge psychological symptoms in a large sample of PLWH. We found that sadness was the central psychological symptom in PLWH. Feeling unsafe, self-abasement, and uncontrollable worry were the bridge symptoms of the 16 psychological symptoms. All central and bridge symptoms could be promising therapeutic targets, as they may accelerate the deactivation of network interactions among psychological symptoms. Healthcare providers should assess the duration of sadness and develop symptom networks for PLWH to evaluate symptom connectivity. Future interventions should also relieve self-focused emotions not by exaggerating PLWH self-emotional distress but by increasing PLWH's ability to view their HIV infection from both individual and social perspectives.
The datasets presented in this article are not readily available because to protect the privacy of PLWH. Requests to access the datasets should be directed to ZZ, emhlbmd6aHVAZnVkYW4uZWR1LmNu.
The studies involving human participants were reviewed and approved by Fudan University School of Nursing approved this study (IRB# TYSA2016-3-1, IRB# TYSQ2020-4-06). The patients/participants provided their written informed consent to participate in this study.
HW: conceptualization, data collection, data analysis, methodology, and writing the original draft. ZZ: methodology and writing—review and editing. TH, CL, TJ, LL, LZ, and YF: data collection. SH: writing—review and editing. YH and BW: supervision, conceptualization, and writing—review and editing. All authors contributed to the article and approved the submitted version.
This work was supported by the Shanghai Sailing Program (20YF1401800), China Medical Board Open Competition Program (#20-372), and National Natural Science Foundation of China (72104051). The funders had no involvement in or influence on this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
2. Stroumpouki T, Perrett S, Kasdovasilis P, Papatheodorou P, Paparizos V, Stavropoulou A. “A journey towards acceptance”: the process of adapting to life with HIV in Greece. A qualitative study. Appl Nurs Res ANR. (2020) 53:151249. doi: 10.1016/j.apnr.2020.151249
3. Moseholm E, Aho I, Mellgren Å, Pedersen G, Katzenstein TL, Johansen IS, et al. Psychosocial health in pregnancy and postpartum among women living with- and without HIV and non-pregnant women living with HIV living in the Nordic countries: results from a longitudinal survey study. BMC Pregnancy Childbirth. (2022) 22:20. doi: 10.1186/s12884-021-04357-5
4. Carney B, Daniels C, Xu X, Sunil T, Ganesan A, Blaylock JM, et al. Association between depression and HIV treatment outcomes in a US military population with HIV infection. AIDS Res Therapy. (2021) 18:29. doi: 10.1186/s12981-021-00350-2
5. Niu L, Luo D, Liu Y, Silenzio VM, Xiao S. The mental health of people living with HIV in China, 1998–2014: a systematic review. PLoS ONE. (2016) 11:e0153489. doi: 10.1371/journal.pone.0153489
6. Kendall CE, Wong J, Taljaard M, Glazier RH, Hogg W, Younger J, et al. A cross-sectional, population-based study measuring comorbidity among people living with HIV in Ontario. BMC Public Health. (2014) 14:161. doi: 10.1186/1471-2458-14-161
7. Miller CT, Solomon SE, Bunn JY, Varni SE, Hodge JJ. Psychological symptoms are associated with both abstinence and risky sex among men with HIV. Arch Sex Behav. (2015) 44:453–65. doi: 10.1007/s10508-014-0464-2
8. Levy ME, Anastos K, Levine SR, Plankey M, Castel AD, Molock S, et al. Depression and psychosocial stress are associated with subclinical carotid atherosclerosis among women living with HIV. J Am Heart Assoc. (2020) 9:e016425. doi: 10.1161/JAHA.120.016425
9. Le Dai D, Pham T, Bui T, Than T, Pham VT, Luong NK, et al. Symptom prevalence, burden and correlates among people living with HIV in Vietnam: a two-centre self-report study. AIDS Care. (2021) 34:1–7. doi: 10.1080/09540121.2021.1922577
10. Bertozzi SM, Gutierrez JP. Poverty, cash transfers, and risk behaviours. Lancet Global Health. (2013) 1:e315–316. doi: 10.1016/S2214-109X(13)70111-6
11. Brown MJ, Serovich JM, Kimberly JA, Hu J. Psychological reactance and HIV-related stigma among women living with HIV. AIDS Care. (2016) 28:745–9. doi: 10.1080/09540121.2016.1147015
12. Bringmann LF, Elmer T, Epskamp S, Krause RW, Schoch D, Wichers M, et al. What do centrality measures measure in psychological networks? J Abnorm Psychol. (2019) 128:892–903. doi: 10.1037/abn0000446
13. Castro D, Ferreira F, de Castro I, Rodrigues AR, Correia M, Ribeiro J, et al. The differential role of central and bridge symptoms in deactivating psychopathological networks. Front Psychol. (2019) 10:2448. doi: 10.3389/fpsyg.2019.02448
14. Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods. (2018) 23:617–34. doi: 10.1037/met0000167
15. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. (2018) 50:195–212. doi: 10.3758/s13428-017-0862-1
16. Epskamp S, Waldorp LJ, Mõttus R, Borsboom D. The Gaussian graphical model in cross-sectional and time-series data. Multivar Behav Res. (2018) 53:453–80. doi: 10.1080/00273171.2018.1454823
17. Forbes MK, Wright A, Markon KE, Krueger RF. Evidence that psychopathology symptom networks have limited replicability. J Abnorm Psychol. (2017) 126:969–88. doi: 10.1037/abn0000276
18. Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivar Behav Res. (2021) 56:353–67. doi: 10.1080/00273171.2019.1614898
19. Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Ann Rev Clin Psychol. (2013) 9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608
20. Borsboom D, Cramer AO, Schmittmann VD, Epskamp S, Waldorp LJ. The small world of psychopathology. PLoS ONE. (2011) 6:e27407. doi: 10.1371/journal.pone.0027407
21. McNally R, Robinaugh DJ, Wu GWY, Wang L, Deserno MK, Borsboom D. Mental disorders as causal systems: a network approach to posttraumatic stress disorder. Clin Psychol Sci. (2015) 3:836–49. doi: 10.1177/2167702614553230
22. Montazeri F, de Bildt A, Dekker V, Anderson GM. Network analysis of behaviors in the depression and autism realms: inter-relationships and clinical implications. J Autism Dev Disord. (2020) 50:1580–95. doi: 10.1007/s10803-019-03914-4
23. Olatunji BO, Levinson C, Calebs B. A network analysis of eating disorder symptoms and characteristics in an inpatient sample. Psychiatry Res. (2018) 262:270–81. doi: 10.1016/j.psychres.2018.02.027
24. Cramer AO, Waldorp LJ, van der Maas HL, Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. (2010) 33:137–50. doi: 10.1017/S0140525X09991567
25. Goldberg JF, Siu C, Mao Y, Tsai J, Pikalov A, Calabrese JR, et al. Major depressive disorder with mixed features and treatment response to lurasidone: a symptom network model. J Affect Disord. (2020) 277:1045–54. doi: 10.1016/j.jad.2020.08.048
26. Borsboom D. A network theory of mental disorders. World Psychiatry Off J World Psych Assoc. (2017) 16:5–13. doi: 10.1002/wps.20375
27. Solmi M, Collantoni E, Meneguzzo P, Tenconi E, Favaro A. Network analysis of specific psychopathology and psychiatric symptoms in patients with anorexia nervosa. Eur Eat Disord Rev J Eat Disord Assoc. (2019) 27:24–33. doi: 10.1002/erv.2633
28. Garabiles MR, Lao CK, Xiong Y, Hall BJ. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: a network approach. J Affect Disord. (2019) 250:85–93. doi: 10.1016/j.jad.2019.02.062
29. Rouquette A, Pingault JB, Fried EI, Orri M, Falissard B, Kossakowski JJ, et al. Emotional and behavioral symptom network structure in elementary school girls and association with anxiety disorders and depression in adolescence and early adulthood: a network analysis. JAMA Psychiatry. (2018) 75:1173–81. doi: 10.1001/jamapsychiatry.2018.2119
30. Konac D, Young KS, Lau J, Barker ED. Comorbidity between depression and anxiety in adolescents: bridge symptoms and relevance of risk and protective factors. J Psychopathol Behav Assess. (2021) 43:583–96. doi: 10.1007/s10862-021-09880-5
31. Zhu Z, Hu Y, Guo M. Urban and rural differences: unmet needs for symptom management in people living with HIV in China. J Assoc Nurses AIDS Care. (2019) 30:206–17. doi: 10.1097/JNC.0000000000000025
32. Zhu Z, Hu Y, Xing W, Guo M, Zhao R, Han S, et al. Identifying symptom clusters among people living with HIV on antiretroviral therapy in China: a network analysis. J Pain Sympt Manag. (2019) 57:617–26. doi: 10.1016/j.jpainsymman.2018.11.011
33. Zhu Z, Guo M, Dong T, Han S, Hu Y, Wu B. Assessing psychological symptom networks related to HIV-positive duration among people living with HIV: a network analysis. AIDS Care. (2021) 34:1–9. doi: 10.1080/09540121.2021.1929815
34. Hughes DJ, Kratsiotis IK, Niven K, Holman D. Personality traits and emotion regulation: a targeted review and recommendations. Emotion. (2020) 20:63. doi: 10.1037/emo0000644
35. Ramesh S. The theories of cognitive development. In: The Political Economy of Human Behaviour and Economic Development. Cham: Palgrave Macmillan (2022). p. 143–180. doi: 10.1007/978-3-031-12666-6_4
36. Zhu Z, Wen H, Yang Z, Han S, Fu Y, Zhang L, et al. Evolving symptom networks in relation to HIV-positive duration among people living with HIV: a network analysis. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. (2021) 108:503–9. doi: 10.1016/j.ijid.2021.05.084
37. Hevey D. Network analysis: a brief overview and tutorial. Health Psychol Behav Med. (2018) 6:301–28. doi: 10.1080/21642850.2018.1521283
38. Costantini G, Epskamp S, Borsboom D, Perugini M, Mõttus R, Lourens JW, et al. State of the aRt personality research: a tutorial on network analysis of personality data in R. J Res Person. (2015) 54:13–29. doi: 10.1016/j.jrp.2014.07.003
39. Fruchterman TMJ, Reingold EM. Graph drawing by force-directed placement. Softw Pract Exper. (1991) 21:1129–64.
40. Hallquist MN, Wright A, Molenaar P. Problems with centrality measures in psychopathology symptom networks: why network psychometrics cannot escape psychometric theory. Multivar Behav Res. (2021) 56:199–223. doi: 10.1080/00273171.2019.1640103
41. Haslbeck J, Fried EI. How predictable are symptoms in psychopathological networks? A reanalysis of 18 published datasets. Psychol Med. (2017) 47:2767–76. doi: 10.1017/S0033291717001258
43. Armour C, Fried EI, Deserno MK, Tsai J, Pietrzak RH. A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in US military veterans. J Anxiety Disord. (2017) 45:49–59. doi: 10.1016/j.janxdis.2016.11.008
44. Haslbeck J, Ryan O, Robinaugh DJ, Waldorp LJ, Borsboom D. Modeling psychopathology: from data models to formal theories. Psychol Methods. (2021). doi: 10.1037/met0000303. [Epub ahead of print].
45. Rodebaugh TL, Tonge NA, Piccirillo ML, Fried E, Horenstein A, Morrison AS, et al. Does centrality in a cross-sectional network suggest intervention targets for social anxiety disorder? J Consult Clin Psychol. (2018) 86:831–44. doi: 10.1037/ccp0000336
46. Christensen AP, Garrido LE, Golino H. What is bridge centrality? A comment on Jones, Ma, and McNally. PsyArXiv [Preprint]. (2019). doi: 10.31234/osf.io/a8svr
47. Lu L. Leisure and depression in midlife: a Taiwanese national survey of middle-aged adults. J Health Psychol. (2011) 16:137–47. doi: 10.1177/1359105310370501
48. Pressman SD, Matthews KA, Cohen S, Martire LM, Scheier M, Baum A, et al. Association of enjoyable leisure activities with psychological and physical well-being. Psycho Med. (2009) 71:725–32. doi: 10.1097/PSY.0b013e3181ad7978
49. Constant A, Hesp C, Davey CG, Friston KJ, Badcock PB. Why depressed mood is adaptive: a numerical proof of principle for an evolutionary systems theory of depression. Comput Psychiatry. (2021) 5:60–80. doi: 10.5334/cpsy.70
50. Buckner JD, Joiner TE, Pettit JW, Lewinsohn PM, Schmidt NB. Implications of the DSM's emphasis on sadness and anhedonia in major depressive disorder. Psychiatry Res. (2008) 159:25–30. doi: 10.1016/j.psychres.2007.05.010
51. Wu DJ, Svoboda RC, Bae KK, Haase CM. Individual differences in sadness coherence: associations with dispositional affect and age. Emotion. (2021) 21:465–77. doi: 10.1037/emo0000731
52. Rush AJ, Kraemer HC, Sackeim HA, Fava M, Trivedi MH, Frank E, et al. Report by the ACNP task force on response and remission in major depressive disorder. Neuropsychopharmacol Off Publ Am College Neuropsychopharmacol. (2006) 31:1841–53. doi: 10.1038/sj.npp.1301131
53. Yu Y, Yang X, Wang S, Wang H, Chang R, Tsamlag L, et al. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry. (2020) 20:460. doi: 10.1186/s12888-020-02870-z
54. Messias E, Castro J, Saini A, Usman M, Peeples D. Sadness, suicide, and their association with video game and internet overuse among teens: results from the youth risk behavior survey 2007 and 2009. Suicide Life Threat Behav. (2011) 41:307–15. doi: 10.1111/j.1943-278X.2011.00030.x
55. Schweren L, van Borkulo CD, Fried E, Goodyer IM. Assessment of symptom network density as a prognostic marker of treatment response in adolescent depression. JAMA Psychiatry. (2018) 75:98–100. doi: 10.1001/jamapsychiatry.2017.3561
56. Nkulu Kalengayi FK, Hurtig AK, Ahlm C, Krantz I. Fear of deportation may limit legal immigrants' access to HIV/AIDS-related care: a survey of Swedish language school students in Northern Sweden. J Immig Minor Health. (2012) 14:39–47. doi: 10.1007/s10903-011-9509-y
57. Pitasi MA, Chavez PR, DiNenno EA, Jeffries WL, Johnson CH, Demeke H, et al. Stigmatizing attitudes toward people living with HIV among adults and adolescents in the United States. AIDS Behav. (2018) 22:3887–91. doi: 10.1007/s10461-018-2188-0
58. Huntingdon B, Sharpe L, de Wit J, Duracinsky M, Juraskova I. A new grounded theory model of sexual adjustment to HIV: facilitators of sexual adjustment and recommendations for clinical practice. BMC Infect Dis. (2020) 20:31. doi: 10.1186/s12879-019-4727-3
59. Schwartz B. Self-Loathing: What It Is, Causes, & How to Cope. Choosingtherapy (2022). Available online at: https://www.choosingtherapy.com/self-loathing/
60. Fang J, Brown GTL, Hamilton R. Changes in Chinese students' academic emotions after examinations: pride in success, shame in failure, and self-loathing in comparison. Br J Educ Psychol. (2022) 2022:12552. doi: 10.1111/bjep.12552
61. Kaiser T, Herzog P, Voderholzer U, Brakemeier EL. Unraveling the comorbidity of depression and anxiety in a large inpatient sample: network analysis to examine bridge symptoms. Depression Anxiety. (2021) 38:307–17. doi: 10.1002/da.23136
62. Teja JS, Narang RL, Aggarwal AK. Depression across cultures. Br J Psychiatry J Mental Sci. (1971) 119:253–60.
63. Catona D, Greene K, Magsamen-Conrad K, Carpenter A. Perceived and experienced stigma among people living with HIV: examining the role of prior stigmatization on reasons for and against future disclosures. J Appl Commun Res. (2016) 44:136–55. doi: 10.1080/00909882.2016.1155726
64. Borkovec TD. The nature, functions and origins of worry. In: Davey G, Tallis F, editors. Worrying: Perspectives on Theory, Assessment and Treatment. New York, NY: John Wiley & Sons (1994). p. 5–33.
65. Gana K, Martin B, Canouet MD. Worry and anxiety: is there a causal relationship? Psychopathology. (2001) 34:221–9. doi: 10.1159/000049314
66. Purdon C, Harrington J. Worry in psychopathology. In: Worry and its Psychological Disorders: Theory, Assessment and Treatment. New York, NY: John Wiley & Sons Incorporated (2006). p. 41–50. doi: 10.1002/9780470713143.ch3
67. Yoo-Jeong M, Haardörfer R, Holstad M, Hepburn K, Waldrop-Valverde D. Is social isolation related to emotion dysregulation and retention in care among older persons living with HIV? AIDS Behav. (2021) 25:171–81. doi: 10.1007/s10461-020-02957-4
68. Santiago-Rodríguez EI, Rivas CE, Maiorana A, Pérez AE, Erguera X, Johnson MO, et al. Unpacking the “backpack of shame”: exploring intersections of stigma among Latinx people living with HIV in San Francisco, CA. Cult Divers Ethnic Minor Psychol. (2021) 27:630–7. doi: 10.1037/cdp0000487
69. Lee Y, Walton R, Jackson L, Batey DS. Community-level factors and HIV health among older people living with HIV (PLWH) in Alabama, United States: a qualitative analysis. J Assoc Nurses AIDS Care JANAC. (2021) 32:589–98. doi: 10.1097/JNC.0000000000000214
70. Mori Y, Tiiri E, Khanal P, Khakurel J, Mishina K, Sourander A. Feeling unsafe at school and associated mental health difficulties among children and adolescents: a systematic review. Children. (2021) 8:232. doi: 10.3390/children8030232
71. Masa R, Baca-Atlas S, Hangoma P. Walking and perceived lack of safety: correlates and association with health outcomes for people living with HIV in rural Zambia. J Transp Health. (2021) 22:101140. doi: 10.1016/j.jth.2021.101140
72. Han S, Hu Y, Lu H, Zhang L, Zhu Z, Luo J, et al. Cognitive behavioral therapy for persons living with HIV in China: a randomized pilot trial. J Affect Disord. (2020) 277:640–8. doi: 10.1016/j.jad.2020.08.085
Keywords: HIV/AIDS, PLWH, psychological network, network structure, symptom management
Citation: Wen H, Zhu Z, Hu T, Li C, Jiang T, Li L, Zhang L, Fu Y, Han S, Wu B and Hu Y (2023) Unraveling the central and bridge psychological symptoms of people living with HIV: A network analysis. Front. Public Health 10:1024436. doi: 10.3389/fpubh.2022.1024436
Received: 10 October 2022; Accepted: 13 December 2022;
Published: 04 January 2023.
Edited by:
Zhimin Tao, Jiangsu University, ChinaCopyright © 2023 Wen, Zhu, Hu, Li, Jiang, Li, Zhang, Fu, Han, Wu and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng Zhu,  emhlbmd6aHVAZnVkYW4uZWR1LmNu; Yan Hu,
emhlbmd6aHVAZnVkYW4uZWR1LmNu; Yan Hu,  aHV5YW5AZnVkYW4uZWR1LmNu
aHV5YW5AZnVkYW4uZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.