
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 16 December 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1021495
This article is part of the Research Topic Health Literacy and Disease Prevention, Volume II View all 23 articles
 Roy Rillera Marzo1,2*
Roy Rillera Marzo1,2* Mohamed ElSherif3
Mohamed ElSherif3 Muhd Siv Azhar Merican Bin Abdullah4
Muhd Siv Azhar Merican Bin Abdullah4 Hui Zhu Thew5
Hui Zhu Thew5 Collins Chong6
Collins Chong6 Shean Yih Soh7
Shean Yih Soh7 Ching Sin Siau8
Ching Sin Siau8 Shekhar Chauhan9
Shekhar Chauhan9 Yulan Lin10*
Yulan Lin10*Introduction: The healthcare setting is a stressful and demanding work environment, and healthcare workers face a continuous expansion of their job roles and responsibilities. Past studies have shown that factors affecting burnout, resilience, and quality of life among healthcare workers merit further research, as there were inconsistent findings, especially with regards to the influence of demographic and work-related factors. Therefore, this study aims to determine whether demographic and work-related factors are associated with burnout, resilience, and quality of life among healthcare workers.
Method: This cross-sectional study was conducted between February 15, 2022 and March 15, 2022, among 394 healthcare workers from Putrajaya and Selangor hospitals, Malaysia. Maslach Burnout Inventory, World Health Organization Quality of Life-BREF 26 inventory, and Brief Resilience Scale were utilized to capture information on burnout, quality of life, and resilience, respectively.
Results: The mean score of physical health of participants who work more than 10 h (11.38) is lower than participants who work from 8 to 10 h (13.00) and participants who work 7 h daily (13.03), p-value < 0.001. Similarly, the mean score of psychological health of participants who work more than 10 h (12.35) is lower than participants who work from 8 to 10 h (13.72) and participants who work 7 h daily (13.68), p-value = 0.001. Higher income levels were associated with high resilience and quality of life.
Conclusion: It is imperative that healthcare practitioners and policy makers adopt and implement interventions to promote a healthy workplace environment, address ethical concerns, and prevent burnout among healthcare workers during the COVID-19 pandemic. Managing the issue of long working hours could possibly result in improved resilience, burnout, and quality of life among healthcare workers. Despite this study able to tickle out some policy specific areas where interventions are needed, identifying effective solutions and evaluating their efficiency will require larger and interventional studies.
The healthcare setting is a stressful and demanding work environment, and healthcare workers (HCWs) face a continuous expansion of their job roles and responsibilities, such as increasing bureaucratic tasks and computerization of the healthcare system (1, 2). With the advent of the coronavirus disease 2019 (COVID-19) pandemic, a worldwide medical emergency, additional stress was put upon the healthcare system, resulting in high levels of psychological distress and burnout among HCWs (3–7). General population across countries is also affected by COVID-19 pandemic in terms of their health (8–10). This study explored burnout, resilience, and quality of life (QoL) among HCWs in Malaysia.
Burnout refers to a state of exhaustion resulting from prolonged stress, and is typified by three syndromes, including emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA) (11). An individual who experiences burnout would typically report physical and emotional overextension, feelings of cynicism and callousness toward his/her work, and a worse level of professional efficacy (11). In the latest version of the International Classification of Diseases-11 (12), burnout has now been redefined as a workplace phenomenon involving the three syndromes described above, rather than as a result of difficulty in the management broad life circumstances. The prevalence of burnout in the healthcare setting has been high, both before and during the COVID-19 pandemic (13, 14). During the COVID-19 pandemic, the level of burnout among HCWs was expected to be higher due to longer working hours, sleep deprivation, and the need to adhere to preventive measures against the virus (15, 16). The pooled prevalence of burnout found in thirty observational studies was 52.0%, with DP being the highest syndrome (52.0%), followed by EE (51.0%), and low PA (28.0%) (17).
Burnout is an important area for further investigation, as burnout syndrome among HCWs has been shown to have service implications such as worse patient safety (18). A number of factors are associated with burnout among HCWs. Systematic reviews showed that job stress, time pressure, high workload, long working hours, low job satisfaction, and low organizational support were factors associated with burnout (19, 20). Demographic factors associated with burnout were younger age, female sex, and marital status (20). A study in Malaysia during the COVID-19 pandemic showed that workload, uncertainties caused by the pandemic, challenging work-family balance, and stretched workplace relationships influenced burnout among HCWs (21).
As HCWs are among the professionals most affected by the COVID-19 pandemic, it is important to study how psychological resilience helped them to cope (22). Resilience refers to an individual's ability to adapt to and rebound from negative workplace stresses such as conflict, failure, and uncertainty (23, 24). Inculcating resilience involves developing coping strategies in order to pre-empt reactions to stressful situations (25). A study showed that nurses with a higher education (postgraduate degree vs. bachelor's degree) exhibited higher resilience against developing posttraumatic stress (26). Demographic factors were inconsistently associated with resilience. For example, systematic reviews among doctors and nurses found differing results in the significance of age, education level, income, marital status, work experience, and job status on resilience (27, 28). Other factors, such as burnout and high psychological distress, however, were consistently associated with lower resilience among HCWs (27, 28). During the COVID-19 pandemic, a study among Portuguese HCWs showed that psychological resilience had a mediating effect in the relationship between depression and burnout (29).
The World Health Organization (WHO) defines QoL as “the individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” (30). Apart from biomedical outcomes, QoL has been increasingly used as a yardstick to measure wellbeing in health research (31). However, while it has been used extensively among patients, there is less research on HCW's QoL. A study in Saudi Arabia showed that a high proportion of nurses reported good QoL (32). Another study in India during the COVID-19 pandemic showed that low QoL was prevalent among HCWs, at 45.0% (33). Factors associated with QoL among HCWs were not consistent across studies. For example, a study among Iranian nurses found that work experience, gender, job position and group of patients treated were unrelated with QoL (34). However, another study from Saudi Arabia showed that demographic and work factors such as age, marital status, having children, income, education, working experience, and department were associated with QoL (32).
Past studies have shown that factors affecting burnout, resilience, and QoL among HCWs merit further research, as there were inconsistent findings, especially with regards to the influence of demographic and work-related factors. During the COVID-19 pandemic, HCWs are also exposed to unique factors that may affect their levels of burnout, resilience, and QoL. COVID-19 infection status may affect an individual in all aspects of their lives. For example, an individual will experience negative physical symptoms, psychological fear, and social isolation when infected by the virus (35), thus affecting their QoL. Being infected by the COVID-19 will also exacerbate burnout symptoms (36). Therefore, it is important to study the association between COVID-19 infection status and HCWs' burnout, resilience, and QoL.
Due to the medical crisis of the COVID-19 pandemic, prolonging into an endemic, identification of factors affecting burnout, resilience, and QoL among HCWs could help to focus on specific points for intervention in order to build a strong healthcare workforce. Therefore, this study aims to determine whether gender, specialty, age, education level, income level, work duration, duration of socialization, and COVID-19 infection status are associated with burnout, resilience, and QoL among HCWs.
This cross-sectional study was conducted between February 15, 2022 and March 15, 2022 to evaluate the level of burnout, QoL, and resilience among HCWs from Putrajaya and Selangor hospitals of Malaysia. The study was conducted during the fifth wave fuelled by the Omicron variant that led to maximum daily cases in February and March 2022 (37, 38), but is marked by lower numbers of hospitalizations and deaths than during the spread of the Delta variant (38). As of March 2022, the BA.2 Omicron sub-variant was projected to be the dominant strain in the country (39). The country's vaccination programme, which commenced in late February 2021 (40), has fully inoculated over 80% of the population and 97% of adults as of April 24, 2022 (41). On February 13, 2022, the total number of cases in Malaysia exceeded the 3 million mark, reaching 3,040,235 (41). By February 24, 2022, the total number of recoveries had reached the 3 million mark, reaching 3,018,172 (41).
The study used a convenience sampling method for recruitment. The online survey was disseminated via various social media platforms such as Instagram, Twitter, LinkedIn, Facebook, WhatsApp, and Telegram. The target population was adult Malaysian HCWs aged 18 years old and above. We invited Malaysian assistant medical officers, doctors, health inspectors, hospital food preparation personnel, medical laboratory technologists, nurses, paramedics, pharmacists, physicians, physiotherapists, dieticians, therapists, psychologists, counselors, radiographers, and social workers from public and private healthcare services to enroll in this study. All respondents were informed that their participation was anonymous and voluntary at the beginning of the survey. Consent was implied if the participants started answering the questionnaire. This research complied with the tenets of the Declaration of Helsinki.
Cochran's formula was used to calculate the minimum recommended sampling size (42). The minimal sample size required for this study with a confidence level of 95%, ± 5% precision and 0.5 estimated proportion was 385 study participants. A total of 394 completed responses were collected. The Institutional Review Board granted approval and the requirement for written informed consent was waived based on the recognition that answering the survey instrument implied consent. Participation was voluntary and anonymity was assured. All personal information was kept confidential. Furthermore, researchers analyzed only de-identified data.
The data collection instrument comprised of five parts. The first part of the tool asked questions pertaining sociodemographic and work-related characteristics. The choice of variables was informed by the available literature and inputs from the investigators. Participants were requested to indicate their age, gender, marital status, specialty, educational level, income, number of family members, job title, place of work, years of experience, hours of working, and socialization time per week. This section also asked whether the respondent had been attending COVID-19 patient directly, had been infected with COVID-19, and their willingness to have another COVID-19 vaccine's booster doses in the future.
The second part of the study tool was a translated version of Maslach burnout inventory (MBI) (11). To limit the study to burnout related to COVID-19, the phrase “due to COVID-19” was added to each item. MBI is an internationally recognized, validated, self-report questionnaire for measuring the severity of workplace burnout, using the three dimensions of EE, DP, and PA. The questionnaire has 22 items and each item is answered on a seven-point Likert scale. This tool has been extensively used in many studies in different parts of the world and the Malaysian translation has also been validated previously (43, 44).
Burnout is expressed by scores of each of the three MBI subscales, with a high score meaning a high level of burnout. Each subscale score is calculated by adding up all scores of all items in that subscale, with the notion that the items on PA domain are reversely scored (11). Scores range from 0 to 54 for EE, from 0 to 30 for DP, and from 0 to 48 for PA subscale. Scales are scored such that higher scores indicate more of each construct. Higher scores on the EE and DP subscales indicate a higher burnout symptom burden; lower scores on the PA subscale indicate a higher burnout symptom burden. The standard cut-off values were used to define low, moderate, and high levels in each dimension (11). The Cronbach's alpha was 0.86.
The WHOQOL-BREF is a 26-item instrument consisting of four domains: physical health (seven items), psychological health (six items), social relationships (three items), and environmental health (eight items); it also contains QOL and general health items. Each individual item of the WHOQOL-BREF is scored from 1 to 5 on a response scale, which is stipulated as a five-point ordinal scale (45).
The physical health domain questions are based on daily activities, medical aid, energy, mobility, the extent of pain, sleeping pattern, and working capacity. The psychological domain focuses on participants' personal beliefs, positive and negative feelings, self-esteem, body image, thinking, and learning capabilities. The social relationships domain explores the respondent's overall satisfaction with their personal and social life. Lastly, the environment domain comprises questions about safety and security, contentment with one's property and physical surroundings, finances (does one have enough money to satisfy one's requirements), access to the necessary care, information, and transport. Moreover, the questionnaire has two specific questions regarding participants' opinions regarding their overall QoL and health. We used the Bahasa melayu validated version of the original WHOQOL-BREF questionnaire (46, 47). The Cronbach's alpha was 0.89.
The last section is the Brief Resilience Scale (BRS) questionnaire to assess the perceived ability to bounce back or recover from stress (48). The scale was developed to assess a unitary construct of resilience, including both positively and negatively worded items.
The BRS has six items presented in Table 1. Items 1, 3, and 5 are positively worded, and items 2, 4, and 6 are negatively worded. The BRS is scored by reverse coding items 2, 4, and 6 and finding the mean of the six items. The following instructions are used to administer the scale: “Please indicate the extent to which you agree with each of the following statements by using the following scale: 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree.” The possible score range on the BRS is from 1 (low resilience) to 5 (high resilience). It composes of 6 questions with a score on interpretation 1.00–2.99 as low resilience, 3.00–4.30 as normal resilience and lastly 4.31–5.00 as high resilience. The Cronbach's alpha was 0.76.
At first, normality of the data was checked. Descriptive statistics are presented in the form of numbers and percentages for the categorical variables. Mean and standard deviation (SD) are reported for numerical variables. Chi square and exact test were used to compare categorical variables (burnout, resilience levels) across different variables. The independent samples t-test and one way ANOVA test were used to compare numerical variables (quality of life) across different variables. IBM SPSS 28 for windows software was used for the analysis, and a P-value < 0.05 is considered statistically significant.
The study was designed and conducted in line with the declaration of Helsinki (49) and was approved by the Ethics Committee of Management and Science University (Ethics Code: MSU-RMC-02/FR01/09/L1/085). Respondents were informed that their participation was voluntary, and written consent was implied on the completion of the questionnaire. All participants were aged 18 years or older.
A total of 394 respondents were included in this study. About 87.1% of the participants were females. Age of 43.1% of the participants ranged from 25 to 35 years, 31.2% from 36 to 55 years, 20.6% were < 25 years, and 5.1% were more than 55 years. About 62.9% of participants were nurses, 14% were doctors, and the remaining were from other specialties in the medical field (Table 1).
As depicted in Table 2, burnout, resilience, and QoL levels showed no statistically significant differences between males and females.
Burnout showed no statistically significant differences between different specialties among the HCWs (Table 3). Levels of QoL and resilience showed statistically significant differences between different specialties. The mean score of physical health of nurses is higher than that of doctors (13.13 vs. 11.79, p-value ≤ 0.001). The mean score of psychological health of nurses is higher than doctors (13.78 vs. 12.70, p-value = 0.009). The mean score of social relationships of nurses is higher than doctors (14.61 vs. 13.24, p-value = 0.003). Of all the participants with low resilience, 19.1% of participants were doctors, 53.2% were nurses, and 27.7% were from other professions. Similarly, about 11.9% of participants who have normal resilience were doctors, 66.7% were nurses, and 21.4% were from other specialty (p-value = 0.038).
Burnout and resilience levels showed no statistically significant differences between different age groups (Table 4). The only variable that showed statistically significant differences between different age groups is the level of QoL. The mean score of physical health of participants from 25 to 36 years old (12.25) was lower than participants <25 years old (13.09) and participants from 36 to 55 years old (13.31; p-value < 0.001). Table 5 shows that burnout and resilience levels had no statistically significant differences between different levels of education. The only variable that showed statistically significant differences between different education levels was level of QoL. The mean score of physical health of participants who had secondary education was higher than participants who had tertiary education (13.12 vs. 12.44, p-value = 0.020). The mean score of psychological health participants who had secondary education was higher than participants who had tertiary education (13.91 vs. 13.26, p-value = 0.013). Table 6 depicts that burnout showed no statistically significant differences between different levels of income. The variables that showed statistically significant differences between different levels of income were levels of QoL and resilience. The mean score of environment level of participants who took < RM 4,850 was lower than participants who took between RM 4,850 and RM 10,959 and participants who took more than RM 10,959 per month (p-value < 0.001). About 16.7% of participants who had high resilience took <RM 4,850, 33.3% took RM 4,850 to RM 10,959, and 50.0% took more than RM 10,959 per month (p-value = 0.001).
Table 7 shows that burnout and resilience levels had no statistically significant differences between participants with different work duration. The only variable that showed statistically significant differences between different work duration was level of QoL. The mean score of physical health of participants who worked more than 10 h (11.38) was lower than participants who worked from 8 to 10 h (13.00) and participants who worked for 7 h daily (13.03; p-value < 0.001). The mean score of psychological health of participants who worked more than 10 h (12.35) was lower than participants who worked from 8 to 10 h (13.72) and participants who worked 7 h daily (13.68; p-value = 0.001). The mean score of social relationships of participants who worked more than 10 h (12.65) was lower than participants who worked from 8 to 10 h (14.38) and participants who worked 7 h daily (14.55), p-value = 0.003. The mean score of environment level in participants who worked more than 10 h (12.87) was lower than participants who worked 7 h daily (14.21) and participants who worked from 8 to 10 h (14.56; p-value < 0.001).
Differences in burnout, quality of life, and resilience levels based on socializing duration were also measure in Table 8. No statistically significant differences were however found. Burnout, QoL, and resilience levels showed no statistically significant differences between HCWs who were infected and not infected with COVID-19 as shown in Table 9.
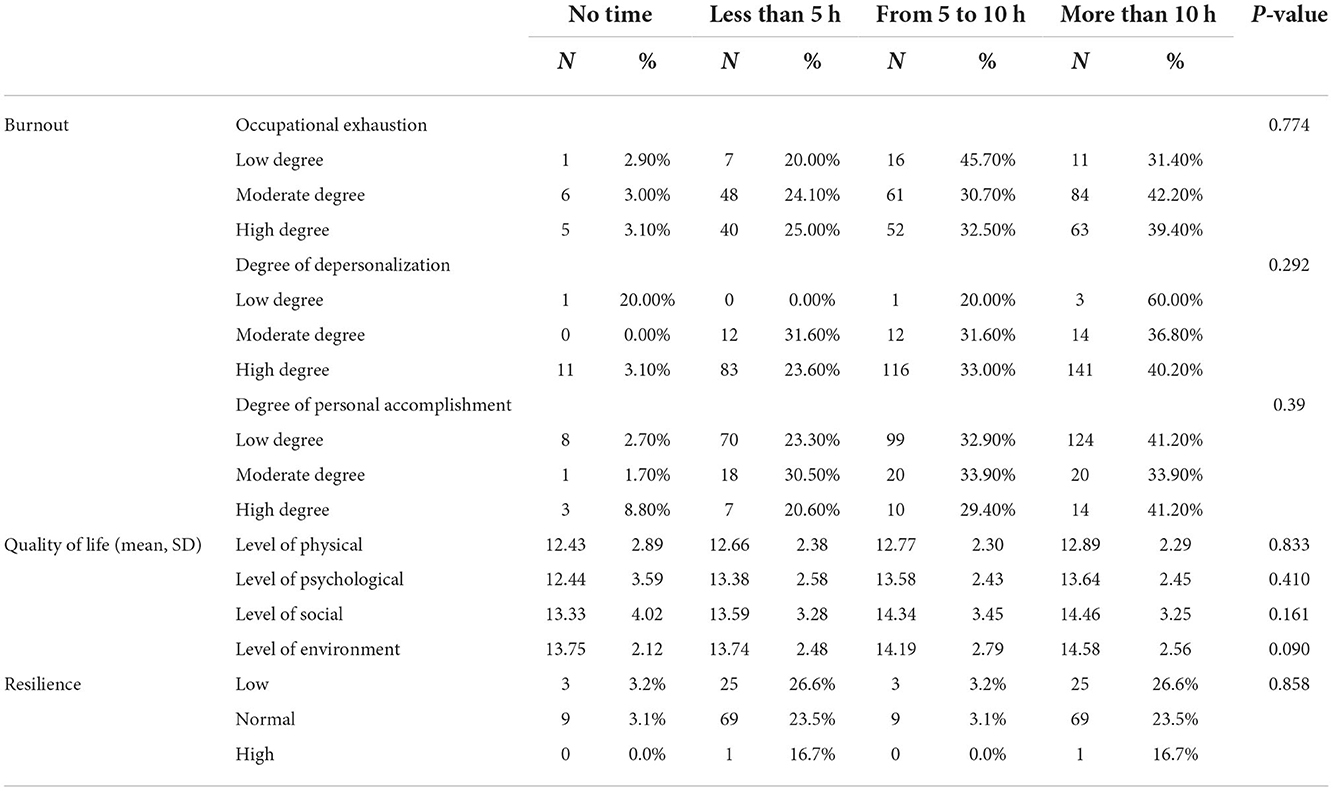
Table 8. Differences in burnout, quality of life, and resilience levels based on socializing duration.
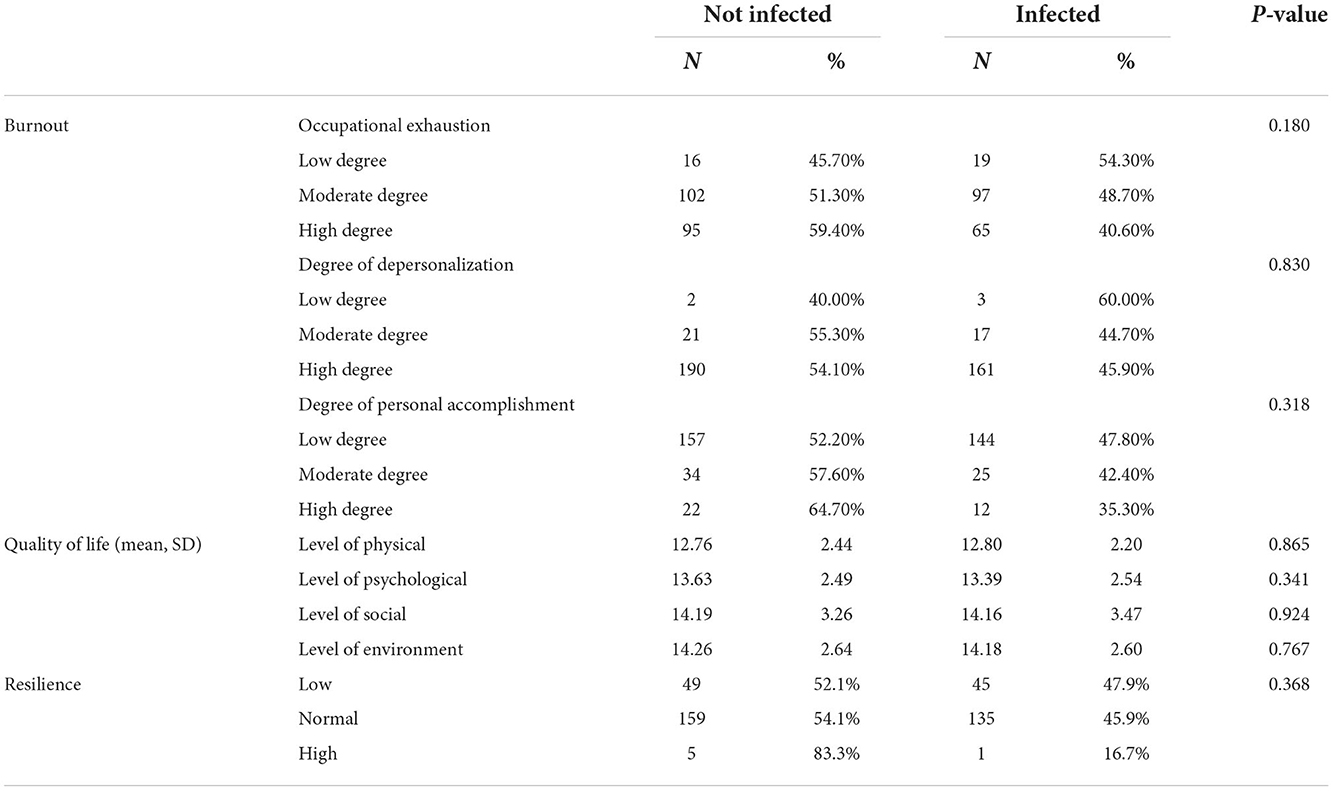
Table 9. Differences in burnout, quality of life, and resilience levels between health worker who were infected and not infected with COVID-19.
This study aimed to determine whether gender, specialty, age, education level, income level, work duration, duration of socialization, and COVID-19 infection status were associated with burnout, resilience, and QoL among HCWs. To summarize, the bivariate analyses found that in terms of resilience, there was a significant difference between males and females, and number of hours socializing. In terms of QoL, level of physical health was different in terms of specialty, age, education level, and work duration; levels of psychological and social health were associated with specialty, age, education level, and work duration; level of environment was associated with only specialty, age, and income level. No significant differences were found among the demographic categories in terms of burnout.
An interesting finding of our study was that more females reported low resilience compared to males. The results are in contrast with a study from the UK among HCWs, which found females to have a higher resilience level than males (50). Likewise, during the COVID-19 pandemic, female HCWs showed higher resilience in the domain of social support compared to males (51). However, a study among radiology workers from China showed that females had lower resilience scores than males (52). Moreover, a meta-analysis on gender and resilience found that males had higher resilience scores than females (53). According to Hirani et al. (54), females usually scored lower on resilience measures due to existing definitions of resilience not adequately reflect how various factors (e.g., gender roles, social factors, and the environment) interact to shape women's experience of and responses to facing difficulties in life (54).
Meanwhile, we found that a higher proportion among those who spent the highest number of hours socializing (>10 h) reported low resilience. It has been shown in a number of studies that social support is an integral aspect of resilience (55, 56). The results found in this study shows that the number of hours spent socializing may not equal social support, as social support includes elements such as a subjective perception of how much an individual is being supported by others (57). In contrast, an individual who spends high number of hours socializing (i.e. more than 10 h) may find that their energy and time are depleted due to excessive socializing. There is a need to further investigate in future studies the content of one's socialization activities which contributes to one's resilience.
QoL in terms of physical health, psychological health and social relationships of nurses was higher than doctors in this study. The results are not consistent with another study by Çelmeçe and Menekay (58), who found no difference in the QoL of nurses and doctors in Turkey during the COVID-19 pandemic (58). On the other hand, another study conducted in Spain during the COVID-19 pandemic found that primary care doctors had lower professional QoL compared to nurses (59). Doctors who are responsible for significant clinical decisions may report lower QoL due to assuming greater responsibilities during this period in time. In addition, according to Li et al. (60), doctors undergo more negative work-related experiences compared with nurses (60). These may be possible reason that the participant doctors suffered from lower QoL in all domains in this study, and it warrants further examination.
In terms of age, QoL of older HCWs were generally higher than that of younger HCWs in all aspects of QoL. The findings are consistent with another study on QoL among nurses in Saudi Arabia, where nurses who were older consistently reported higher QoL in comparison to those who were younger (<30 years old) (32). During the COVID-19 pandemic, a study among COVID-19 recovered HCWs in Bangladesh indicated that QoL was also higher among those with older age (61). Older age may be associated with higher QoL because increase in experience in professional work usually grows in tandem with age; greater experience at work has been proposed to be a factor leading to higher QoL (62).
We found an inverse relationship between participants' education level and QoL, where participants with a secondary education reported higher QoL in all aspects in comparison with participants with a tertiary education. Studies have reported that individuals with higher educational level reported higher QoL (63–65), possibly due to the beneficial influence of higher health literacy among those with more educational years (66). However, a study among HCWs in Malaysia during the COVID-19 pandemic showed that there were no differences in all QoL domains in terms of education level (67). In our study, individuals with a tertiary education may have lower QoL due to assuming responsibilities and making decisions which would more directly impact patients, in comparison with those who had secondary education. The greater responsibility assumed in patient healthcare may have contributed to lower QoL due to experiencing more job-related stress.
All domains of QoL were lower among HCWs who worked more than 10 h per day. To cope with the rising demands for healthcare during the COVID-19 pandemic, accompanied by the depletion of HCWs due to infection of COVID-19 virus, there were a number of strategies used to increase HCW capacity (68). The most common strategy reported was extending the working hours of HCWs, and this includes working overtime, canceling leaves, and allowing back-to-back shifts (69). The length of working hours among HCWs has been associated with a number of negative physical, psychological, and safety outcomes among HCWs, such as musculoskeletal pain (70), fatigue and isolation (71), and less time to participate in social activities (69). All this may have negatively affected the QoL of the HCWs who worked for longer hours.
In this study, HCWs who earned <RM 4,850 reported lower QoL in their environmental level in comparison with those who earned more per month. The results are consistent with past studies, in which individuals from a lower-income background may suffer from lower environment QoL (61, 72–74). For example, a large-scale survey in Malaysia with 18,607 rural residents found that compared with individuals with low income, those enjoying middle and high income had higher perceived QoL in all four domains (75). Environmental QoL may be lower among HCWs with low income due to poorer living conditions, financial issues, and physical insecurities (61, 73).
The study results showed that there were no differences in terms of burnout, resilience, and QoL among HCWs who had been infected or not infected by the COVID-19 virus. The results are not consistent with extant literature, where those who had been infected by the COVID-19 virus reported higher burnout levels (36, 76). Infection status may also lead to physical and psychological ramifications, eventually leading to lower QoL (35). However, a study conducted among the Italian general population found that COVID-19 infection did not significantly predict resilience (77). As this study was carried out during the later stages of the COVID-19 pandemic when most HCWs had been vaccinated against the virus, having been infected by the virus may not have affected the HCWs in terms of their burnout, resilience, and QoL.
The results of this study have significance on identifying HCWs who may be at risk of burnout, low resilience, and low QoL during the COVID-19 pandemic and beyond. It is important to identify the related demographic and work factors in order to more effectively screen HCWs for the presence of these conditions, and to provide age-, gender-, and specialty-appropriate interventions. Healthcare authorities should be mindful of the negative consequences of long working hours on HCW's QoL. Attention should be paid to younger HCWs' and doctors' QoL, to find out the specific work, physical or psychological characteristics contributing to lower QoL. Issues pertaining to the environmental health of HCWs with lower income should also be identified and addressed.
This study has a few limitations. Being a cross-sectional study, we could not infer a cause-and-effect relationship between the variables. Since the participants were not randomly sampled, we could not rule out the presence of bias in this study. Other aspects which possibly contribute to burnout, resilience, and QoL among HCWs were not explored, such as the influence of religion, workload, and psychological distress. Future studies can be conducted to understand the role of resilience and coping in mediating burnout and QoL among HCWs. A combination of quantitative and qualitative methodology in future studies would be able to provide in-depth information on the possible causes that led to our findings.
This study explored demographic and work-related factors associated with burnout, resilience, and QoL among HCWs in Malaysia during the COVID-19 pandemic. The findings of this study call out for some specific interventions from policy makers. Nurses were more prone to report poor scores on burnout and resilience than doctors. However, they reported higher mean score on various dimensions of QoL than doctors. Age of the HCWs was an important factor in determining resilience as HCWs with higher age reported high resilience. Though inferential but low age of the HCWs means they are new to the profession and therefore overburdened and not experienced as compared to their senior counterparts who have years of experience, that works as a coping strategy for them. The study confirmed that higher income level leads to better resilience and longer work duration leads to low level of QoL. It is imperative that healthcare practitioners and policy makers adopt and implement interventions to promote a healthy workplace environment, address ethical concerns, and prevent burnout among healthcare workers during and beyond the COVID-19 pandemic. Managing the issue of long working hours could possibly result in improved resilience, burnout, and QoL among HCWs. Though this study may be able to inform some policy specific areas where interventions are needed, identifying effective solutions and evaluating their effectiveness will require larger and interventional studies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of Management and Science University. The patients/participants provided their written informed consent to participate in this study.
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
This work was supported by the Special Projects of the Central Government Guiding Local Science and Technology Development, China (No. 2021L3018). The funder was not involved in study design, in the collection, analysis and interpretation of data, in the writing of the manuscript, and nor in the decision to submit the manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kanchanachitra C, Lindelow M, Johnston T, Hanvoravongchai P, Lorenzo FM, Huong NL, et al. Human resources for health in Southeast Asia: shortages, distributional challenges, and international trade in health services. Lancet. (2011) 377:769–81. doi: 10.1016/S0140-6736(10)62035-1
2. Reith TP. Burnout in United States healthcare professionals: a narrative review. Cureus. (2018) 10:3681. doi: 10.7759/cureus.3681
3. Chew QH, Chia FLA, Ng WK, Lee WCI, Tan PLL, Wong CS, et al. Perceived stress, stigma, traumatic stress levels and coping responses amongst residents in training across multiple specialties during COVID-19 pandemic—a longitudinal study. Int J Environ Res Public Health. (2020) 17:6572. doi: 10.3390/ijerph17186572
4. Chirico F, Ferrari G, Nucera G, Szarpak Ł, Crescenzo P, Ilesanmi O. Prevalence of anxiety, depression, burnout syndrome, and mental health disorders among healthcare workers during the COVID-19 pandemic: a rapid umbrella review of systematic reviews. J Health Soc Sci. (2021) 6:209–20. Available online at: https://journalhss.com/wp-content/uploads/jhhs_62_209-220.pdf
5. Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. (2020) 66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007
6. Kamberi F, Sinaj E, Jaho J, Subashi B, Sinanaj G, Jaupaj K, et al. Impact of COVID-19 pandemic on mental health, risk perception and coping strategies among health care workers in Albania - evidence that needs attention. Clin Epidemiol Glob Health. (2021) 12:824. doi: 10.1016/j.cegh.2021.100824
7. Htay MNN, Marzo RR, Bahari R, AlRifai A, Kamberi F, El-Abasiri RA, et al. How healthcare workers are coping with mental health challenges during COVID-19 pandemic? - a cross-sectional multi-countries study. Clin Epidemiol Glob Health. (2021) 11:759. doi: 10.1016/j.cegh.2021.100759
8. Marzo RR, Singh A, Mukti RF. A survey of psychological distress among Bangladeshi people during the COVID-19 pandemic. Clin Epidemiol Glob Health. (2021) 10:693. doi: 10.1016/j.cegh.2020.100693
9. Marzo RR, Vinay V, Bahari R, Chauhan S, Ming DAF, Fernandez SFAN, et al. Depression and anxiety in Malaysian population during third wave of the COVID-19 pandemic. Clin Epidemiol Glob Health. (2021) 12:868. doi: 10.1016/j.cegh.2021.100868
10. Marzo RR, Khanal P, Ahmad A, Rathore FA, Chauhan S, Singh A, et al. Quality of life of the elderly during the COVID-19 pandemic in Asian countries: a cross-sectional study across six countries. Life. (2022) 12:365. doi: 10.3390/life12030365
11. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory. 3rd ed. In:MD Lanham, editor, Evaluating Stress: A Book of Resources. Lanham, MD: Scarecrow Education (1997). p. 191–218.
12. WHO. ICD-11. Available online at: https://icd.who.int/en (accessed November 14, 2022).
13. Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians: a systematic review. J Am Med Assoc. (2018) 320:1131–50. doi: 10.1001/jama.2018.12777
14. Woo T, Ho R, Tang A, Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J Psychiatr Res. (2020) 123:9–20. doi: 10.1016/j.jpsychires.2019.12.015
15. Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare. (2020) 8:421. doi: 10.3390/healthcare8040421
16. Ching SM, Ng KY, Lee KW, Yee A, Lim PY, Ranita H, et al. Psychological distress among healthcare providers during COVID-19 in Asia: systematic review and meta-analysis. PLoS ONE. (2021) 16:e0257983. doi: 10.1371/journal.pone.0257983
17. Ghahramani S, Lankarani KB, Yousefi M, Heydari K, Shahabi S, Azmand S, et al. Systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Front Psychiatry. (2021) 12:758849. doi: 10.3389/fpsyt.2021.758849
18. de Garcia CL, de Abreu LC, Ramos JLS, de Castro CFD, Smiderle FRN, dos Santos JA, et al. Influence of burnout on patient safety: systematic review and meta-analysis. Medicina. (2019) 55:553. doi: 10.3390/medicina55090553
19. Dugani S, Afari H, Hirschhorn LR, Ratcliffe H, Veillard J, Martin G, et al. Prevalence and factors associated with burnout among frontline primary health care providers in low- and middle-income countries: a systematic review. Gates Open Res. (2018) 2:4. doi: 10.12688/gatesopenres.12779.1
20. Amoafo E, Hanbali N, Patel A, Singh P. What are the significant factors associated with burnout in doctors? Occup Med. (2015) 65:117–21. doi: 10.1093/occmed/kqu144
21. Roslan NS, Yusoff MSB, Asrenee AR, Morgan K. Burnout prevalence and its associated factors among Malaysian healthcare workers during covid-19 pandemic: an embedded mixed-method study. Healthcare. (2021) 9:10090. doi: 10.3390/healthcare9010090
22. Bozdag F, Ergün N. Psychological resilience of healthcare professionals during COVID-19 pandemic. Psychol Rep. (2021) 124:2567–86. doi: 10.1177/0033294120965477
23. Luthans F. The need for and meaning of positive organizational behavior. J Organ Behav. (2002) 23:695–706. doi: 10.1002/job.165
24. Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. Am J Crit Care. (2015) 24:412–20. doi: 10.4037/ajcc2015291
25. Schreiber M, Cates DS, Formanski S, King M. Maximizing the resilience of healthcare workers in multi-hazard events: lessons from the 2014–2015 Ebola Response in Africa. Milit Med. (2019) 184(Suppl.1):114–20. doi: 10.1093/milmed/usy400
26. Mealer M, Jones J, Meek P. Factors affecting resilience and development of posttraumatic stress disorder in critical care nurses. Am J Crit Care. (2017) 26:184–92. doi: 10.4037/ajcc2017798
27. McKinley N, Karayiannis PN, Convie L, Clarke M, Kirk SJ, Campbell WJ. Resilience in medical doctors: a systematic review. Postgrad Med J. (2019) 95:140–7. doi: 10.1136/postgradmedj-2018-136135
28. Yu F, Raphael D, Mackay L, Smith M, King A. Personal and work-related factors associated with nurse resilience: a systematic review. Int J Nurs Stud. (2019) 93:129–40. doi: 10.1016/j.ijnurstu.2019.02.014
29. Serrão C, Duarte I, Castro L, Teixeira A. Burnout and depression in portuguese healthcare workers during the COVID-19 pandemic—the mediating role of psychological resilience. Int J Environ Res Public Health. (2021) 18:636. doi: 10.3390/ijerph18020636
30. WHO. WHOQOL - Measuring Quality of Life. (2022). Available online at: https://www.who.int/tools/whoqol (accessed August 2, 2022).
31. Haraldstad K, Wahl A, Andenæs R, Andersen JR, Andersen MH, Beisland E, et al. A systematic review of quality of life research in medicine and health sciences. Qual Life Res. (2019) 28:2641–50. doi: 10.1007/s11136-019-02214-9
32. Ibrahim NK, Alzahrani NA, Batwie AA, Abushal RA, Almogati GG, Sattam MA, et al. Quality of life, job satisfaction and their related factors among nurses working in king Abdulaziz University Hospital, Jeddah, Saudi Arabia. Contemp Nurse. (2016) 52:486–98. doi: 10.1080/10376178.2016.1224123
33. Suryavanshi N, Kadam A, Dhumal G, Nimkar S, Mave V, Gupta A, et al. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. (2020) 10:e01837. doi: 10.1002/brb3.1837
34. Aalaa M, Sanjari M, Tootee A, Mirzabeigi G, Salemi S. Assessment of quality of life of Iranian nurses. Nurs Rep. (2012) 2:e10. doi: 10.4081/nursrep.2012.e10
35. Jin YH, Huang Q, Wang YY, Zeng XT, Luo LS, Pan ZY, et al. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID-19 infected healthcare workers in a tertiary acute care hospital in Wuhan: a cross-sectional survey. Milit Medical Res. (2020) 7:24. doi: 10.1186/s40779-020-00254-8
36. Chavez S, Long B, Koyfman A, Liang SY. Coronavirus Disease (COVID-19): a primer for emergency physicians. Am J Emerg Med. (2021) 44:220–9. doi: 10.1016/j.ajem.2020.03.036
37. Noorshahrizam SA. As Omicron Cases Spike, Health Coalition Calls for Reinforced Plan Against COVID-19. (2022). Available online at: https://malaysia.news.yahoo.com/omicron-cases-spike-health-coalition-040155133.html (accessed July 31, 2022).
38. New Straits Times. KJ: Malaysia Fully Into Omicron Wave. NST Online. (2022). Available online at: https://www.nst.com.my/news/nation/2022/02/769160/kj-malaysia-fully-omicron-wave (accessed July 31, 2022).
39. Ying TP. Omicron BA.2 to Become Dominant Coronavirus Variant in Malaysia. NST Online. (2022). Available online at: https://www.nst.com.my/news/nation/2022/03/781780/omicron-ba2-become-dominant-coronavirus-variant-malaysia (accessed July 31, 2022).
40. Anand R. PM Muhyiddin Receives First COVID-19 Vaccine as Malaysia Kicks Off Mass Inoculation Campaign. The Straits Times. (2021). Available online at: https://www.straitstimes.com/asia/se-asia/pm-muhyiddin-receives-first-covid-19-vaccine-as-malaysia-kicks-off-mass-inoculation (accessed July 31, 2022).
41. Ministry of Health, Malaysia. COVIDNOW in Malaysia. (2021). Available online at: https://covidnow.moh.gov.my/ (accessed July 31, 2022).
42. Cochran WG. Note on an approximate formula for the significance levels of z. Ann Math Statist. (1940) 11:93–5. doi: 10.1214/aoms/1177731945
43. Chen WS, Haniff J, Siau CS, Seet W, Loh SF, Jamil MHA, et al. Translation, cross-cultural adaptation and validation of the Malay version of the Maslach Burnout Inventory (MBI) in Malaysia. Int J Soc Sci Stud. (2014) 2:66. doi: 10.11114/ijsss.v2i2.309
44. Chen WS, Haniff J, Siau CS, Seet W, Loh SF, Jamil MHA. Pilot study of the Malay maslach burnout inventory and Malay work-related quality of life scale in Malaysia. Stud Asian Soc Sci. (2014) 1:20–6. doi: 10.5430/sass.v1n1p20
45. WHO. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment: Field Trial Version, December 1996. Geneva: World Health Organization (1996).
46. Cheung YB, Yeo KK, Chong KJ, Khoo EY, Wee HL. Reliability and validity of the English-, Chinese-and Malay-language versions of the World Health Organization quality of life (WHOQOL-BREF) questionnaire in Singapore. Ann Acad Med Singap. (2017) 46:461–9. doi: 10.47102/annals-acadmedsg.V46N12p461
47. Hasanah CI, Naing L, Rahman ARA. World Health Organization quality of life assessment: brief version in Bahasa Malaysia. Med J Malaysia. (2003) 58:79–88. Available online at: http://www.e-mjm.org/2003/v58n1/WHO_Quality_of_Life_Assessment.pdf
48. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. (2008) 15:194–200. doi: 10.1080/10705500802222972
49. World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bullet World Health Org. (2001) 79:373. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2566407/pdf/11357217.pdf
50. Sull A, Harland N, Moore A. Resilience of health-care workers in the UK; a cross-sectional survey. J Occup Med Toxicol. (2015) 10:20. doi: 10.1186/s12995-015-0061-x
51. Coco M, Guerrera CS, Santisi G, Riggio F, Grasso R, Di Corrado D, et al. Psychosocial impact and role of resilience on healthcare workers during COVID-19 pandemic. Sustainability. (2021) 13:7096. doi: 10.3390/su13137096
52. Huang L, Wang Y, Liu J, Ye P, Cheng B, Xu H, et al. Factors associated with resilience among medical staff in radiology departments during the outbreak of 2019 novel coronavirus disease (COVID-19): a cross-sectional study. Med Sci Monit. (2020) 26:e925669. doi: 10.12659/MSM.925669
53. Gök A, Kogar EY. A meta-analysis study on gender differences in psychological resilience levels. Kibris Türk Psikiyatri ve Psikoloji Dergisi. (2021) 3:132–43. doi: 10.35365/ctjpp.21.2.15
54. Hirani S, Lasiuk G, Hegadoren K. The intersection of gender and resilience. J Psychiatr Ment Health Nurs. (2016) 23:455–67. doi: 10.1111/jpm.12313
55. Wilks SE. Resilience amid academic stress: the moderating impact of social support among social work students. Adv Soc Work. (2008) 9:106–25. doi: 10.18060/51
56. Ong HL, Vaingankar JA, Abdin E, Sambasivam R, Fauziana R, Tan ME, et al. Resilience and burden in caregivers of older adults: moderating and mediating effects of perceived social support. BMC Psychiatry. (2018) 18:27. doi: 10.1186/s12888-018-1616-z
57. Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. (2018) 18:156. doi: 10.1186/s12888-018-1736-5
58. Çelmeçe N, Menekay M. The effect of stress, anxiety and burnout levels of healthcare professionals caring for COVID-19 patients on their quality of life. Front Psychol. (2020) 11:597624. doi: 10.3389/fpsyg.2020.597624
59. Ortega-Galán ÁM, Ruiz-Fernández MD, Lirola MJ, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, et al. Professional quality of life and perceived stress in health professionals before COVID-19 in Spain: primary and hospital care. Healthcare. (2020) 8:484. doi: 10.3390/healthcare8040484
60. Li Y, Zhang H, Feng Z, Chen S, Liu T, Chen X, et al. Life events, anxiety and depression among doctors and nurses in the emergency department: a study from eleven General Hospital in Hunan Province, China. J Psychiatry Brain Sci. (2016) 1:2. doi: 10.20900/jpbs.20160002
61. Rashid MU, Khan MAS, Dalal K, Sagar SK, Hossian M, Barsha SY, et al. Quality of life (QoL) among COVID-19 recovered healthcare workers in Bangladesh. BMC Health Serv Res. (2022) 22:716. doi: 10.1186/s12913-022-07961-z
62. Hayne AN, Gerhardt C, Davis J. Filipino nurses in the United States: recruitment, retention, occupational stress, and job satisfaction. J Transcult Nurs. (2009) 20:313–22. doi: 10.1177/1043659609334927
63. Arora S, Kalra R. Quality of life (QOL) of people living with substance users in urban and rural community of Delhi. Curr Med Res Practice. (2018) 8:96–9. doi: 10.1016/j.cmrp.2018.05.010
64. Asante JO Li MJ, Liao J, Huang YX, Hao YT. The relationship between psychosocial risk factors, burnout and quality of life among primary healthcare workers in rural Guangdong province: a cross-sectional study. BMC Health Serv Res. (2019) 19:1–10. doi: 10.1186/s12913-019-4278-8
65. Gholami A, Jahromi LM, Zarei E, Dehghan A. Application of WHOQOL-BREF in measuring quality of life in health-care staff. Int J Prev Med. (2013) 4:809. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3775221/pdf/IJPVM-4-809.pdf
66. Zheng M, Jin H, Shi N, Duan C, Wang D, Yu X, et al. The relationship between health literacy and quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. (2018) 16:1–10. doi: 10.1186/s12955-018-1031-7
67. Woon LSC, Mansor NS, Mohamad MA, Teoh SH, Leong Bin Abdullah MFI. Quality of life and its predictive factors among healthcare workers after the end of a movement lockdown: the salient roles of COVID-19 stressors, psychological experience, and social support. Front Psychol. (2021) 12:652326. doi: 10.3389/fpsyg.2021.652326
68. Williams GA, Maier CB, Scarpetti G, de Belvis AG, Fattore G, Morsella A, et al. What strategies are countries using to expand health workforce surge capacity during the COVID-19 pandemic? Eurohealth. (2020) 26:51–7. Available online at: https://apps.who.int/iris/bitstream/handle/10665/336296/Eurohealth-26-2-51-57-eng.pdf
69. Fu C, Wang G, Shi X, Cao F. Social support and depressive symptoms among physicians in tertiary hospitals in China: a cross-sectional study. BMC Psychiatry. (2021) 21:1–11. doi: 10.1186/s12888-021-03219-w
70. Arca M, Dönmezdil S, Durmaz ED. The effect of the COVID-19 pandemic on anxiety, depression, and musculoskeletal system complaints in healthcare workers. Work. (2021) 69:47–54. doi: 10.3233/WOR-205014
71. Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. (2020) 105:2. doi: 10.1016/j.jhin.2020.03.002
72. González-Blanch C, Hernández-de-Hita F, Muñoz-Navarro R, Ruíz-Rodríguez P, Medrano LA, Cano-Vindel A. The association between different domains of quality of life and symptoms in primary care patients with emotional disorders. Sci Repo. (2018) 8:1–10. doi: 10.1038/s41598-018-28995-6
73. Gou Z, Xie X, Lu Y, Khoshbakht M. Quality of Life (QoL) survey in Hong Kong: Understanding the importance of housing environment and needs of residents from different housing sectors. Int J Environ Res Public Health. (2018) 15:219. doi: 10.3390/ijerph15020219
74. Moutinho ILD, Lucchetti ALG, da Silva Ezequiel O, Lucchetti G. Mental health and quality of life of Brazilian medical students: incidence, prevalence, and associated factors within two years of follow-up. Psychiatry Res. (2019) 274:306–12. doi: 10.1016/j.psychres.2019.02.041
75. Thangiah G, Said MA, Majid HA, Reidpath D, Su TT. Income inequality in quality of life among rural communities in Malaysia: a case for immediate policy consideration. Int J Environ Res Public Health. (2020) 17:8731. doi: 10.3390/ijerph17238731
76. Asghar MS, Akram M, Yasmin F, Najeeb H, Naeem U, Gaddam M, et al. Comparative analysis of neutrophil to lymphocyte ratio and derived neutrophil to lymphocyte ratio with respect to outcomes of in-hospital coronavirus disease 2019 patients: a retrospective study. Front Med. (2022) 9:951556. doi: 10.3389/fmed.2022.951556
77. Sampogna G, Del Vecchio V, Giallonardo V, Luciano M, Albert U, Carmassi C, et al. What is the role of resilience and coping strategies on the mental health of the general population during the COVID-19 pandemic? Results from the Italian multicentric comet study. Brain Sci. (2021) 11:1231. doi: 10.3390/brainsci11091231
Keywords: burnout, resilience, quality of life, influencing factors, healthcare workers, Malaysia
Citation: Marzo RR, ElSherif M, Abdullah MSAMB, Thew HZ, Chong C, Soh SY, Siau CS, Chauhan S and Lin Y (2022) Demographic and work-related factors associated with burnout, resilience, and quality of life among healthcare workers during the COVID-19 pandemic: A cross sectional study from Malaysia. Front. Public Health 10:1021495. doi: 10.3389/fpubh.2022.1021495
Received: 17 August 2022; Accepted: 16 November 2022;
Published: 16 December 2022.
Edited by:
Ozden Gokdemir, Izmir University of Economics, TurkeyReviewed by:
Adriano Friganovic, University Hospital Centre Zagreb, CroatiaCopyright © 2022 Marzo, ElSherif, Abdullah, Thew, Chong, Soh, Siau, Chauhan and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yulan Lin, eXVsYW5saW5AZmptdS5lZHUuY24=; Roy Rillera Marzo, cnJtdGV4YXNAeWFob28uY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.