
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 08 November 2022
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1020801
This article is part of the Research Topic The Impact of Non-Pharmaceutical Interventions (NPIs) on Communicable Diseases View all 9 articles
 Leonard Ngarka1,2
Leonard Ngarka1,2 Joseph Nelson Siewe Fodjo1,3
Joseph Nelson Siewe Fodjo1,3 Wepnyu Yembe Njamnshi1
Wepnyu Yembe Njamnshi1 John D. Ditekemena4
John D. Ditekemena4 Mohammed A. M. Ahmed5,6
Mohammed A. M. Ahmed5,6 Rhoda K. Wanyenze7
Rhoda K. Wanyenze7 Janet Dula8
Janet Dula8 Philippe Sessou9
Philippe Sessou9 Christian T. Happi10
Christian T. Happi10 John N. Nkengasong11
John N. Nkengasong11 Robert Colebunders3
Robert Colebunders3 Alfred K. Njamnshi1,2*†
Alfred K. Njamnshi1,2*†Introduction: While most governments instituted several interventions to stall the spread of COVID-19, little is known regarding the continued observance of the non-pharmaceutical COVID-19 preventive measures particularly in Sub-Saharan Africa (SSA). We investigated adherence to these preventive measures during the initial 6 months of the COVID-19 outbreak in some SSA countries.
Methods: Between March and August 2020, the International Citizen Project on COVID-19 consortium (www.icpcovid.com) conducted online surveys in six SSA countries: Benin, Cameroon, Democratic Republic of Congo, Mozambique, Somalia, and Uganda. A five-point individual adherence score was constituted by scoring respondents' observance of the following measures: mask use, physical distancing, hand hygiene, coughing hygiene, and avoiding to touch one's face. Community behaviors (going to public places, traveling during the pandemic) were also assessed. Data were analyzed in two time periods: Period 1 (March-May) and Period 2 (June-August).
Results: Responses from 26,678 respondents were analyzed (mean age: 31.0 ± 11.1 years; 54.1% males). Mean individual adherence score decreased from 3.80 ± 1.37 during Period 1, to 3.57 ± 1.43 during Period 2; p < 0.001. At the community level, public events/places were significantly more attended with increased travels during Period 2 compared to Period 1 (p < 0.001). Using linear mixed models, predictors of increased individual adherence included: higher age (Coef = 0.005; 95% CI: 0.003–0.007), female gender (Coef = 0.071; 95% CI: 0.039–0.104), higher educational level (Coef = 0.999; 95% CI: 0.885–1.113), and working in the healthcare sector (Coef = 0.418; 95% CI: 0.380–0.456).
Conclusion: Decreasing adherence to non-pharmaceutical measures over time constitutes a risk for the persistence of COVID-19 in SSA. Younger persons and those with lower education levels constitute target groups for improving adherence to such measures.
The coronavirus disease 2019 (COVID-19) has plagued the global scene for over 2 years. By June 16th 2022, the cumulative number of COVID-19 cases around the world stood at 535,248,141 with 6,313,229 deaths since the initial outbreak in Wuhan—China (1). While Europe and the Americas record the highest number of cases and deaths due to the deadly virus, the African continent accounts for <2% of the global COVID-19 burden (1). Initially it was predicted that the COVID-19 death toll would be enormous in Africa due to fragile health systems, precarious living conditions, and anticipated difficulties in observing the non-pharmaceutical preventive measures (2, 3). However, SSA cumulates fewer COVID-19 cases and deaths compared to other regions of the world. Among other reasons, the leading explanation for this relatively low COVID-19 numbers in SSA seems to be the demographic structure with several youths who are less susceptible to develop severe disease (4). Additionally, according to a recent genetic study, ACE2 genes (incriminated in COVID-19 physiopathology) show a rare variation among persons of African origin which may explain why most SSA populations are only mildly affected by the disease (5).
Most SSA countries reported their first case of COVID-19 in March 2020, justifying the World Health Organization's timing in recognizing COVID-19 as a pandemic during that same month (6). Consequently, many nations adopted unprecedented measures to limit viral transmission; such strategies included closure of international borders, closure of schools, and working from home when possible (7). The fact that the population's adherence to these preventive measures was not systematically monitored prompted the initiation of online surveys across several low- and middle-income countries via the International Citizen Project on COVID-19 (ICPCovid) (8).
Considering the unforeseen persistence of the pandemic during several years, it expected that adherence trends will vary over time. Moreover, the introduction of pharmaceutical measures against COVID-19 (for example, vaccines) may significantly impact adherence to the non-pharmaceutical strategies that were hitherto prioritized. Thus, understanding the determinants of adherence prior to COVID-19 vaccine deployment would inform public health authorities in SSA on the appropriate strategies to achieve high adherence to non-pharmaceutical measures in the general population during public health emergencies such as COVID-19.in pandemic. In the present paper, we sought to pool together adherence data from six ICPCovid countries in SSA to increase sample size and arrive at conclusions that hopefully would be relevant for most SSA settings. We specifically aimed to analyze the trends in adherence to COVID-19 preventive measures as well as the evolution of the COVID-19 prevalence during the first 6 months of the outbreak in the participating countries.
The data analyzed in this study were obtained during online surveys conducted by the ICPCovid consortium in six SSA countries between March and August 2020 (first 6 months of the outbreak in these SSA countries). Participating countries included: Benin, Cameroon, Democratic Republic of Congo (DRC), Mozambique, Somalia, and Uganda. The datasets used in this study are from (9–14).
In each country, investigators adapted the template ICPCovid questionnaire to the context of their countries and translated it to the national language(s). Thereafter the survey web-link was widely disseminated via social media and other platforms to invite consenting participants to fill in their responses through smartphones, tablets or computers. Data were collected on socio-demographic characteristics, as well as the self-reported experience of at least one of the following non-specific flu-like symptoms which constitute the COVID-19 clinical definition (15) during the past 2 weeks: fever, headaches, cough, sore throat, coryza, anosmia, ageusia, shortness of breath, myalgia, fatigue, nausea, or vomiting. The reported symptoms were used to identify participants who met the clinical criteria for suspected COVID-19 based on recommendations from the World Health Organization (WHO) (15).
To assess respondents' preventive behaviors during the pandemic, questions were also asked regarding observance of individual COVID-19 preventive measures (mask use, physical distancing, hand hygiene i.e., regular hand washing with soap and/or use of alcohol-based hand gel, not touching one's face, and covering the mouth when coughing/sneezing). as Adherence to community preventive measures against COVID-19 were also investigated; these included: having attended a gathering with more than 10 persons, having gone to a public gym/beauty center including hair/barbing saloon, been to a market, or having traveled, all within the past 7 days. All responses were anonymously submitted to the secure ICPCovid server (hosted in in Belgium), where they were stored until data extraction for analysis.
Collected data were exported to Microsoft Excel 2016 spreadsheets for cleaning and later transferred to R version 4.0.2 for analysis. Continuous variables (age and adherence score) were summarized as means and standard deviation (SD). Since the two continuous variables failed the Kolgomorov-Smirnov normality test, they were compared across groups using a Mann-Whitney U-test or Kruskal Wallis test as appropriate. Meanwhile, categorical variables (gender, educational level, marital status, profession, residential setting, healthcare worker/student, and adherence to individual preventive measures yes vs. no) were expressed as percentages, and comparisons done using the Chi-square test or Fisher exact test as appropriate. Adherence was measured by attributing a score of one when the respondent observed any of the preventive measures, and zero otherwise. A composite score for individual adherence was constructed by summing up scores from the five individual measures, since this combination of questions yielded the best performance (highest value for Cronbach alpha). In case of missing values for any of the above-mentioned individual preventive measures, the “partial” adherence scores were standardized to a 5-point scale using the formula below and rounded to the nearest whole number:
To investigate whether the level of adherence correlated with the prevalence of flu-like symptoms reported on a weekly basis in our study population, we constituted weekly clusters by grouping all data received during a given week in each country. Given that the reported flu-like symptoms had been experienced within the past 2 weeks, we used the rolling mean prevalence of suspected COVID-19 (considering two consecutive weeks: week n-1 and week n) for this analysis. Only weeks with ≥15 responses in the country-specific datasets were included when constituting the weekly clusters.
The internal consistency of the 5-item adherence score on the overall dataset was assessed using the Cronbach alpha, while its dimensionality was investigated using exploratory factor analysis (EFA). Determinants of individual adherence to COVID-19 preventive measures were investigated via a generalized linear mixed model using the 5-point adherence score as the dependent variable. The model was constructed using the lmer function (package: “lme4”) in the software R. The variable “country of residence” was introduced in the random part of the model, while all other variables were fixed covariates. Covariates for the final model were selected based on a p-value < 0.2 in univariate analysis. However, the variable “marital status” was excluded from the model due to several missing values (>4,000), despite the significant difference observed during the descriptive and univariate analysis. All p-values < 0.05 were considered statistically significant.
Pooled analysis of multi-country adherence scores was done using the software RevMan version 5.3. Surveys were sub-grouped based on the period during which the data was collected: Period 1 (early phase) included surveys that were conducted within the first 3 months March, April, May 2020; and Period 2 (later phase) for surveys conducted during the three remaining months (June, July, August 2020). To investigate whether pooled adherence scores varied by period, sub-group analysis was performed using a random effects model and a forest plot was generated.
The online ICPCovid platform used to conduct the surveys was approved by the Ethics Committee of the University of Antwerp, Belgium (Ref: 20/13/148). Additionally, the respective national ethical committees in each participating country provided their approval (see Author Statements section for details). Only responses from participants aged 18 years and above who provided an e-consent were retained for analysis. All data were collected anonymously and treated with absolute confidentiality.
Data from a total of 26,678 respondents from the six participating countries were analyzed (overall mean age: 31.0 ± 11.1 years, 54.1% males). Except for Cameroon which had no data for Period 1 and Uganda which had no data for Period 2, all other countries provided adherence data for both study periods. Table 1 presents the socio-demographic characteristics of the participants grouped by country and study period. For both Period 1 and Period 2, most participants resided in urban settings (68.1 and 74.8%, respectively) and had attained a university level of education (74.3 and 64.2%, respectively). There were more participants who reported at least one flu-like symptom during Period 2 (36.5%) than in Period 1 (20.1%); p < 0.001. Furthermore, the overall prevalence of suspected COVID-19 cases in our study population significantly increased from 8.7% in Period 1 to 9.8% in Period 2; p = 0.003. Of note, detailed flu-like symptoms were not available in the Ugandan survey hence it was not possible to identify suspected COVID-19 cases.
An overall decrease in the adherence to preventive measures was observed between Period 1 and Period 2 (Table 2). Pooled analysis by Period also showed a similar trend, with adherence scores decreasing from 3.85 in Period 1, to 3.82 in Period 2, albeit being non-significant statistically (Figure 1); of note, a high degree of heterogeneity was observed in the pooled analysis. Mean adherence score was higher among men (3.76) compared to women (3.58), p < 0.001; higher among participants in the healthcare sector (4.11) compared to other respondents (3.55), p < 0.001; higher among the more educated (postgraduate > undergraduate > secondary > primary), p < 0.001; and higher among rural residents (rural > suburban > urban), p < 0.001.
Regarding the internal consistency of the 5-item adherence score, the overall Cronbach alpha for the entire dataset was 0.669. Upon stratifying the data by country, disparities in internal consistency were observed; the following Cronbach alpha values were obtained: 0.521 for Benin (n = 969), 0.263 for Cameroon (n = 3,047), 0.661 for DRC (n = 7,230), 0.360 for Mozambique (n = 4,920), 0.725 for Somalia (n = 8,800), and 0.447 for Uganda (n = 1,712). Exploratory factor analysis (EFA) revealed that except for “mask use,” all other items loaded on one factor with factor loadings > 0.5. Mask use had a high loading (0.786) on a different factor (Supplementary Appendix 1).
There was an increase in non-observance of the community measures over time in our study population. Combined data from all participating countries show that compared to Period 1, Period 2 was characterized by more participants reporting that: they attended gatherings with ≥10 persons (from 12.7 to 39.4%, p < 0.001); they have been to public gym (from 3.5 to 12.1%, p < 0.001); they have been to a beauty center, hair/barbing saloon (from 22.4 to 35.8%, p < 0.001); they have been to a market (from 55.7 to 63.3%, p < 0.001); they traveled outside of their town of residence (from 8.4 to 18.1%, p < 0.001).
Regarding the analysis of the weekly adherence scores in relation to the rolling mean prevalence of suspected COVID-19, there was no correlation (Spearman rho = −0.035, p-value = 0.831). Figure 2 graphically presents the evolution of weekly adherence scores and suspected COVID-19 prevalence by country and by week (week numbers are given as per the 2020 yearly calendar). Based on rough estimates derived from the shape of the graphs, it appears that to produce a noticeable curb in the burden of COVID-19-like symptoms, the adherence scores must exceed the threshold value of four.
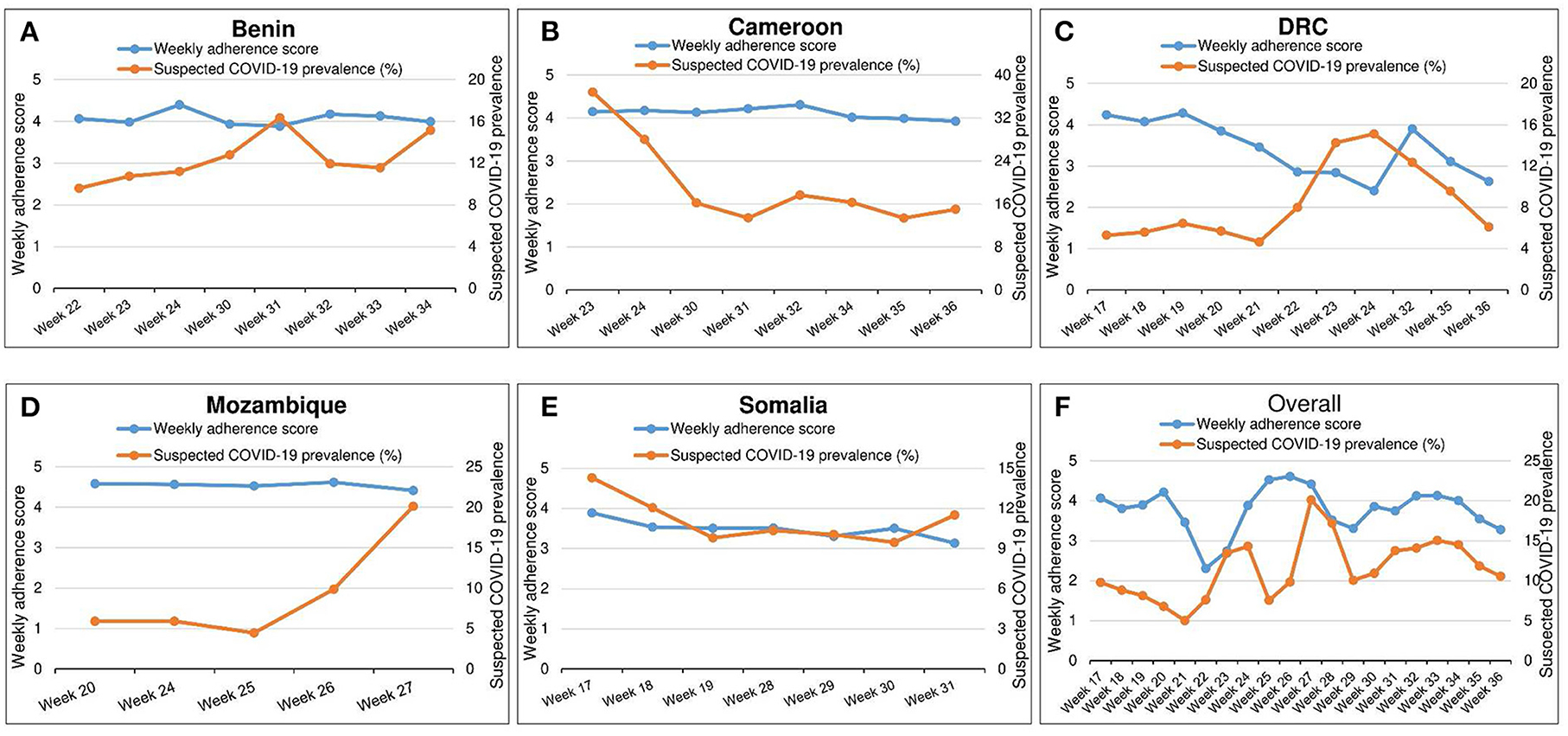
Figure 2. (A–F) Evolution of weekly adherence scores (for week n) and the rolling mean week-specific prevalence of suspected COVID-19 (for week n-1 and week n). Uganda is not included in this analysis because data on flu-like symptoms was not collected during the Ugandan ICPCovid survey.
The multivariable model showed that data collected during Period 2 was associated with lower adherence scores. Additionally, having experienced any flu symptoms during the past 2 weeks, residing in urban/sub-urban settings, and being unemployed/self-employed were also associated with reduced adherence to the preventive measures. Increasing age, female gender, higher educational level and working in the healthcare sector were all associated with increased adherence scores (Table 3). The random part of the model, represented by the variable “country of residence,” accounted for 11.6% of the variance in adherence score observed in our study population.
In this multi-country study, we examined adherence trends with respect to COVID-19 non-pharmaceutical preventive measures implemented in six SSA countries, and the concomitant evolution of the burden of COVID-19-like illness among the participants in these countries. We proposed a scoring system to best evaluate the population's adherence to these COVID-19 preventive measures. The adherence score showed an optimal overall Cronbach alpha value of 0.669 when the five individual preventive measures recommended by the WHO (16) were retained. Given that Cronbach alpha values for the 5-item adherence score varied greatly by country, and with the high heterogeneity observed during the pooled analysis, it is evident that the proposed scoring system still requires context-specific improvements and is hardly generalizable to different SSA countries.
We noted a significant drop in overall individual adherence over time, associated with an evident rise in the prevalence of COVID-19-like illness, which may have contributed to the resurgence (second wave) of the COVID-19 cases observed in Africa at the wake of 2021. Indeed, during the early months of the pandemic, many people were initially conscious and ready to adhere probably due to all the sensitizations on COVID-19 and its reported deleterious effects on human health. When individuals in the participating countries progressively noticed that they were not being decimated by the pandemic as per the predictions, coupled with the economic hardships engendered by the lockdown measures (17), they might have become more relaxed in observing the preventive measures just a few months after their implementation. Furthermore, governments might have become less strict about reinforcing the instituted measures after the first epidemic peak had passed in these countries. Although our web-based approach introduced a selection bias, the overall findings suggest that adherence to COVID-19 preventive measures gradually declined. This declining adherence possibly fostered the rise in COVID-19 incidence observed in numerous African countries (18, 19). Our findings corroborate with the occurrence of a second wave of COVID-19 in several African countries during the second half of the year 2020 (18, 19).
Although the overall drop in mean adherence score between Period 1 and Period 2 was significant, there were inter-country disparities. Countries such as the DRC and Somalia recorded a major drop in adherence scores, while Period 1 and Period 2 adherence scores were not significantly different for Benin and Mozambique. In Mozambique, the majority of the study population worked from home during both periods of the study, suggesting that community preventive measures were strictly observed by public and private institutions, possibly enhancing adherence to individual measures as well (11). Meanwhile in Benin, the government did not opt for a radical lockdown but rather insisted on more friendly barrier measures while allowing free movement of people (9); we presume that complying with this non-stringent strategy was not difficult, and therefore adherence scores remained more or less constant throughout the study duration in Benin. We further observed a rise in face mask usage during Period 2, and a decreased observance of other COVID-19 preventive measures, including physical distancing. This could be due to the fact that in SSA settings, distancing is not always easy in densely populated urban milieus, especially for individuals who work in the informal sector. Therefore, they tend to compensate the non-observance of distancing by increasing their face mask use in order to continue their professional duties amidst the pandemic. Additionally, face masks were in very limited supply during the early months of the pandemic (20), and this could explain why fewer persons wore masks in Period 1. Furthermore, the fact that “mask use” loaded on a different factor than other COVID-19 preventive measures during EFA suggests that it is perceived as a stand-alone intervention, with its own unique adherence trends. The increasing use of face masks is an encouraging finding, considering a recent meta-analysis which revealed that the protective effect of masking (using N95 or surgical masks) was comparable to that of observing distancing >1 meter (21). However, it is still necessary to promote physical distancing as this is a proven method to quell the COVID-19 pandemic by limiting inter-personal contacts (22).
Our study found that female gender was associated with an increase in individual adherence scores. Previous research in other SSA countries equally reported a more favorable attitude toward adherence to COVID-19 preventive measures in women (23, 24). Other studies have demonstrated that the psychological distress resulting from the COVID-19 pandemic and associated restrictions tend to affect females more than males (25), and that women are more concerned about their health and that of their family vis-à-vis COVID-19 (26). Additionally, males are more prone to non-adherence as they seek to provide for their families amidst the socio-economic hardship brought about by the pandemic, at the expense of observing the strict measures instituted to reduce viral transmission (27, 28).
From this study, we surmise that achieving an individual adherence score of at least four on five would noticeably curb the incidence of COVID-19-like illness in affected communities. This suggests that better adherence to the prescribed preventive measures may indeed contribute to limiting the risk of contracting COVID-19. Considering the modest internal consistency of the 5-item adherence score, we admit that it can hardly be used to accurately explain the variation in COVID-19 burden and transmission in different countries. Developing an ideal adherence score that would reflect the COVID-19 dynamics in a given community would indeed be a daunting task for a number of reasons: Firstly, fomite transmission of the coronavirus is currently being questioned (29, 30) thereby oppugning the role of handwashing or avoiding to touch one's face in preventing infection. Secondly, household transmission was identified as a major drive behind successive COVID-19 waves, notably in South Africa (31). High transmission within a given bubble highlights the difficulty of relying on community preventive measures to contain the infection. This certainly warrants further research.
We noted increased adherence scores among respondents who reported to be health personnel. As those at the frontline in the fight against the COVID-19 pandemic, health personnel are in constant contact with infected patients, including the hospitalized severe cases. Furthermore, persons in healthcare are more knowledgeable on COVID-19 scientific information updates with regards to prevention and treatment strategies and are best informed on the need for the strict respect of preventive measures. Hence, the compliance of healthcare workers could be leveraged to revamp adherence in the general population by using the health personnel as effective and trusted channels of communication and sensitization (10–13). We also observed that the participant's profession played a role in influencing adherence, similar to what was reported by another study in Ethiopia, where government and private organization workers were more likely to observe the preventive measures (32). In our own study, being unemployed or self-employed was associated with a lower adherence score with a trend of increasing adherence scores among those working in private or government institutions. One possible reason for this observation could be the reinforcement of preventive measures by private institutions and public workplaces via the provision of hand-washing stations, hand sanitizers, personal protective equipment, face masks, and imposing mandatory physical distancing as required by the government (21).
After more than 2 years into the COVID-19 pandemic, the implementation of measures to minimize transmission and curb COVID-19 incidence and prevalence has been shown to be effective when strictly respected. Currently, vaccines have become the centerpiece in the fight against COVID-19 (33). Available evidence reveals that although the approved COVID-19 vaccines are indeed effective at preventing the disease, the acquired immunity wanes with time especially when the newer variants of the virus are concerned (34). As such, vaccinated persons may still get infected and transmit the virus albeit to a lesser extent (35). While the non-pharmacological preventive measures might not produce the expected public health infection containment benefit (36), they are still crucial in limiting inter-person COVID-19 transmission even in the post-vaccination era.
Since our data were collected via an online approach, we recognize that only a particular group of individuals could participate (mostly educated persons, with good internet access and residing in urban settings) thereby introducing both selection and social desirability bias. However, although the findings are hardly generalizable to the general population of the included countries, they do highlight factors associated with adherence to the COVID-19 non-pharmaceutical preventive measures which are probably ubiquitous across most SSA countries. While the level of adherence to the preventive measures may be different among persons who did not participate in the survey (potentially worse as less educated persons, who tend to be less adherent, were under-represented in our study population), the adherence trends in the general population would most likely be similar to what we report in this paper. The proposed adherence score, constituted by purposeful selection of a few variables, may not fully capture the respondents' behavior vis-à-vis the national COVID-19 preventive measures in their country as this greatly varies in the different countries. Therefore, it may be worth investigating adherence scores that include other (combinations of) non-pharmaceutical measures against COVID-19 in the different countries, and that can also account for country-specific variables like number of COVID-19 tests done, strictness of confinement, and vaccination coverage.
We also admit that the WHO clinical case definition which we used to identify suspected cases of COVID-19 is far from accurate in estimating the real number of infected persons, as it does not take into account asymptomatic carriers whose impact in the COVID-19 transmission chain is undeniable (31). Indeed, studies have shown that COVID-19 burden estimates can vary greatly depending on the case definition used (37). With the onset of new COVID-19 waves even in communities with high adherence to non-pharmaceutical interventions (38), it remains unclear whether the latter, if not supplemented with other strategies, would be able to curb the COVID-19 burden in the long run. An additional limitation was the fact that we were unable to assess the external validity of our 5-item score; we therefore recommend that in future adherence surveys, specific questions should be asked that would provide relevant data for estimating the generalizability of a proposed score in a given country or community (39).
In conclusion, we report a decreasing trend in adherence to COVID-19 preventive measures in SSA countries. This represents a serious risk for resurgence of the virus as evidenced by second, third, and even fourth waves of COVID-19 in some African countries (40). While the advances in pharmaceutical tools against COVID-19 are laudable, proven non-pharmaceutical options can be still be adapted and implemented to ensure a persistent downward trajectory of COVID-19 incidence. Particularly, younger persons with lower education levels should be targeted to improve compliance to preventive measures in SSA settings. Finally, mass vaccination campaigns around the globe should not demotivate observance of non-pharmaceutical measures. Rather, the populations should be sensitized on the synergistic effects of vaccination and continued adherence to the preventive measures to contain the ongoing pandemic sooner rather than later.
Publicly available datasets were analyzed in this study. This data can be found at: Data available upon reasonable request from the ICPCovid consortium: aWNwY292aWRAdWFudHdlcnBlbi5iZQ==.
AN, LN, JS, WN, and RC conceived and designed this study. JDi, MA, RW, JDu, PS, and AN supervised data collection. JS cleaned and analyzed the data. LN, JS, and AN wrote the initial draft of the manuscript. All authors contributed to the editing of the initial draft and approved the final manuscript.
The establishment of the ICPCovid website to conduct the surveys was supported by a grant from the European Research Council (ERC 671055). No funding source supported the drafting and dissemination of this scientific article.
We thank the following ICPCovid research team members and partners in the different countries who were involved in the local organization/dissemination of the surveys:
• Benin: Guy Alain Alitonou, Director of Polytechnic School of Abomey-Calavi (University of Abomey-Calavi), Souaïbou Farougou and Charles Sossa Jérôme.
• Cameroon: Nfor L, Mengnjo M, Mendo EL, Angwafor S, Atchou Basseguin J, Nkouonlack C, Njit E, Ahidjo N, Chokote E, Dema F, Fonsah J, Tatah G, Palmer N, Seke Etet P, Palmer D, Nsagha D, Etya'ale D, Perrig S, Sztajzel R, Annoni JM, Bissek ACZK, Leke RG, and Abena Ondoa Obama MT (Brain Research Africa Initiative); The Prime Minister's Office for overall administrative support; The Ministry of Public Health, the Ministry of Communication and the Ministry of Post and Telecommunications of Cameroon and its partners for assisting in sensitization of the population and in disseminating the survey link.
• Democratic Republic of Congo: Hypolite Muhindo, Nkumba Mukadi Dalau (Faculty of Medicine, University of Kinshasa).
• Mozambique: António Júnior, Sérgio Mahumane, Sónia Enosse, Caroline Deschacht, and Sérgio Chicumbe (Instituto Nacional de Saúde, Ministry of Health).
• Somalia: Mohamed Shariff Osman, Ismail Omar Mohamed, Abdiwali Sheikh Mohamed, Mohamed Abdullahi Nor, Zakarie Arale, Aweis Ahmed Moalim Abdullahi, Ahmed Ahmed Mohamud Hussein, and Abdiasis Mohamed Ali (Mogadishu University).
• Uganda: Bob Omoda, Lillian Bulage, and Alex Ario (Uganda National Institute of Public Health).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1020801/full#supplementary-material
1. WHO. Coronavirus Disease (COVID-19) Dashboard. (2022). Available online at: https://covid19.who.int (accessed June 17, 2022).
2. Torti C, Mazzitelli M, Trecarichi EM, Darius O. Potential implications of SARS-CoV-2 epidemic in Africa: where are we going from now? BMC Infect Dis. (2020) 20:412. doi: 10.1186/s12879-020-05147-8
3. Makoni M. COVID-19 in Africa: half a year later. Lancet Infect Dis. (2020) 20:1127. doi: 10.1016/S1473-3099(20)30708-8
4. Adams J, MacKenzie MJ, Amegah AK, Ezeh A, Gadanya MA, Omigbodun A, et al. The conundrum of low COVID-19 mortality burden in sub-Saharan Africa: myth or reality? Glob Health Sci Pract. (2021) 9:433–43. doi: 10.9745/GHSP-D-21-00172
5. Zhang C, Verma A, Feng Y, Melo MCR, McQuillan M, Hansen M, et al. Impact of natural selection on global patterns of genetic variation and association with clinical phenotypes at genes involved in SARS-CoV-2 infection. Proc Natl Acad Sci USA. (2022) 119:e2123000119. doi: 10.1073/pnas.2123000119
6. World Health Organisation. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. (2020). Available online at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-−11-march-2020 (accessed March 20, 2020).
7. Umviligihozo G, Mupfumi L, Sonela N, Naicker D, Obuku EA, Koofhethile C, et al. Sub-Saharan Africa preparedness and response to the COVID-19 pandemic: a perspective of early career African scientists. Wellcome Open Res. (2020) 5:163. doi: 10.12688/wellcomeopenres.16070.2
8. ICPCovid Research Group. International Citizen Project Covid-19. (2020). Available online at: https://www.icpcovid.com/ (accessed May 11, 2020).
9. Sessou P, Siewe Fodjo JN, Sossa CJ, Farougou S, Colebunders R. Assessment of adherence to public health measures and their impact on the COVID-19 outbreak in Benin Republic, West Africa. Pan Afr Med J. (2021) 38.26843. doi: 10.11604/pamj.2021.38.293.26843
10. Siewe Fodjo JN, Ngarka L, Njamnshi WY, Nfor LN, Mengnjo MK, Mendo EL, et al. COVID-19 preventive behaviours in cameroon: a six-month online national survey. Int J Environ Res Public Health. (2021) 18:2554. doi: 10.3390/ijerph18052554
11. Ditekemena JD, Nkamba DM, Muhindo HM, Siewe JNF, Luhata C, Van den Bergh R, et al. Factors associated with adherence to COVID-19 prevention measures in the Democratic Republic of the Congo (DRC): results of an online survey. BMJ Open. (2021) 11:e043356. doi: 10.1136/bmjopen-2020-043356
12. Júnior A, Dula J, Mahumane S, Koole O, Enosse S, Fodjo JNS, et al. Adherence to COVID-19 preventive measures in mozambique: two consecutive online surveys. Int J Environ Res Public Health. (2021) 18:1091. doi: 10.3390/ijerph18031091
13. Ahmed MAM, Siewe Fodjo JN, Gele AA, Farah AA, Osman S, Guled IA, et al. COVID-19 in Somalia: adherence to preventive measures and evolution of the disease burden. Pathogens. (2020) 9:735. doi: 10.3390/pathogens9090735
14. Amodan BO, Bulage L, Katana E, Ario AR, Fodjo JNS, Colebunders R, et al. Level and determinants of adherence to COVID-19 preventive measures in the first stage of the outbreak in Uganda. Int J Environ Res Public Health. (2020) 17:8810. doi: 10.3390/ijerph17238810
15. WHO. COVID-19 Case Definition. Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2022.1 (accessed April 17, 2021).
16. WHO. Advice for the Public on COVID-19 – World Health Organization. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed April 17, 2021).
17. Lone SA, Ahmad A. COVID-19 pandemic – an African perspective. Emerg Microbes Infect. (2020) 9:1300–8. doi: 10.1080/22221751.2020.1775132
18. WHO. Rising Mortality as Africa Marks One Year of COVID-19. WHO Reg. Off. Afr. Available online at: https://www.afro.who.int/news/rising-mortality-africa-marks-one-year-covid-19 (accessed April 17, 2021).
19. Salyer SJ, Maeda J, Sembuche S, Kebede Y, Tshangela A, Moussif M, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet. (2021) 397:1265–75. doi: 10.1016/S0140-6736(21)00632-2
20. Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. (2020) 8:434–6. doi: 10.1016/S2213-2600(20)30134-X
21. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. (2020) 395:1973–87. doi: 10.1016/S0140-6736(20)31142-9
22. Tian H, Liu Y, Li Y, Wu C-H, Chen B, Kraemer MUG, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. (2020) 368:638–42. doi: 10.1126/science.abb6105
23. Azene ZN, Merid MW, Muluneh AG, Geberu DM, Kassa GM, Yenit MK, et al. Adherence towards COVID-19 mitigation measures and its associated factors among Gondar City residents: a community-based cross-sectional study in Northwest Ethiopia. PLoS ONE Public Libr Sci. (2021) 15:e0244265. doi: 10.1371/journal.pone.0256954
24. Majam M, Fischer A, Phiri J, Venter F, Lalla-Edward ST. International citizen project to assess early stage adherence to public health measures for COVID-19 in South Africa. PLoS ONE. (2021) 16:e0248055. doi: 10.1371/journal.pone.0248055
25. González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. (2020) 87:172–6. doi: 10.1016/j.bbi.2020.05.040
26. Apanga PA, Kumbeni MT. Adherence to COVID-19 preventive measures and associated factors among pregnant women in Ghana. Trop Med Int Health. (2021) 2021:13566. doi: 10.1111/tmi.13566
27. Ayanlade A, Radeny M. COVID-19 and food security in Sub-Saharan Africa: implications of lockdown during agricultural planting seasons. Npj Sci Food. (2020) 4:13. doi: 10.1038/s41538-020-00073-0
28. Nechifor V, Ramos MP, Ferrari E, Laichena J, Kihiu E, Omanyo D, et al. Food security and welfare changes under COVID-19 in Sub-Saharan Africa: impacts and responses in Kenya. Glob Food Secur. (2021) 28:100514. doi: 10.1016/j.gfs.2021.100514
29. Goldman E. Exaggerated risk of transmission of COVID-19 by fomites. Lancet Infect Dis. (2020) 20:892–3. doi: 10.1016/S1473-3099(20)30561-2
30. Horoho S, Musik S, Bryant D, Brooks W, Porter IM. Questioning COVID-19 surface stability and fomite spreading in three aeromedical cases: a case series. Mil Med. (2020) 2020:usaa548. doi: 10.1093/milmed/usaa548
31. Cohen C, Kleynhans J, von Gottberg A, McMorrow ML, Wolter N, Bhiman JN, et al. SARS-CoV-2 incidence, transmission, and reinfection in a rural and an urban setting: results of the PHIRST-C cohort study, South Africa, 2020–21. Lancet Infect Dis. (2022) 22:821–34. doi: 10.1016/S1473-3099(22)00069-X
32. Abeya SG, Barkesa SB, Sadi CG, Gemeda DD, Muleta FY, Tolera AF, et al. Adherence to COVID-19 preventive measures and associated factors in Oromia regional state of Ethiopia. PLoS ONE. (2021) 16:e0257373. doi: 10.1371/journal.pone.0257373
33. Liu X, Liu C, Liu G, Luo W, Xia N. COVID-19: progress in diagnostics, therapy and vaccination. Theranost Ivyspring. (2020) 10:7821–35. doi: 10.7150/thno.47987
34. Andrews N, Stowe J, Kirsebom F, Toffa S, Rickeard T, Gallagher E, et al. Covid-19 vaccine effectiveness against the omicron (B11529) variant. N Engl J Med. (2022) 386:1532–46. doi: 10.1056/NEJMoa2119451
35. Centers for Disease Control Prevention. Coronavirus Disease 2019 (COVID-19). Cent. Dis. Control Prev. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/fully-vaccinated-people.html (accessed May 7, 2021).
36. Parker A, Dawood H. SARS-CoV-2 transmission: time to rethink public health strategy. Lancet Infect Dis. (2022) 22:748–50. doi: 10.1016/S1473-3099(22)00137-2
37. Tsang TK, Wu P, Lin Y, Lau EHY, Leung GM, Cowling BJ. Effect of changing case definitions for COVID-19 on the epidemic curve and transmission parameters in mainland China: a modelling study. Lancet Public Health. (2020) 5:e289–96. doi: 10.1016/S2468-2667(20)30089-X
38. Reicher S, Drury J. Pandemic fatigue? How adherence to covid-19 regulations has been misrepresented and why it matters. Br Med J. (2021) 2021:372. doi: 10.1136/bmj.n137
39. Lazarus JV, Ratzan S, Palayew A, Billari FC, Binagwaho A, Kimball S, et al. COVID-SCORE: a global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10). PLoS ONE. (2020) 15:e0240011. doi: 10.1371/journal.pone.0240011
40. WHO. Cases Drop for First Time as Africa's Fourth COVID-19 Wave Ebbs. WHO Reg. Off. Afr. (2022). Available online at: https://www.afro.who.int/news/cases-drop-first-time-africas-fourth-covid-19-wave-ebbs (accessed May 23, 2022).
Keywords: COVID-19, Sub-Saharan Africa, barrier measures, adherence score, prevention
Citation: Ngarka L, Siewe Fodjo JN, Njamnshi WY, Ditekemena JD, Ahmed MAM, Wanyenze RK, Dula J, Sessou P, Happi CT, Nkengasong JN, Colebunders R and Njamnshi AK (2022) Adherence to COVID-19 preventive measures in Sub-Saharan Africa during the 1st year of the pandemic: Pooled analysis of the International Citizen Project on COVID-19 (ICPCovid) surveys. Front. Public Health 10:1020801. doi: 10.3389/fpubh.2022.1020801
Received: 16 August 2022; Accepted: 18 October 2022;
Published: 08 November 2022.
Edited by:
Ramy Mohamed Ghazy, Alexandria University, EgyptReviewed by:
Toluwase Asubiaro, University of Alberta, CanadaCopyright © 2022 Ngarka, Siewe Fodjo, Njamnshi, Ditekemena, Ahmed, Wanyenze, Dula, Sessou, Happi, Nkengasong, Colebunders and Njamnshi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alfred K. Njamnshi, YWxmcmVkLm5qYW1uc2hpQGJyYWluYWZyaWNhLm9yZw==
†ORCID: Alfred K. Njamnshi orcid.org/0000-0003-0052-1511
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.