- 1Department of Environmental Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
- 2Department of Epidemiology and Biostatistics, University of California, San Francisco, San Francisco, CA, United States
Background: As the COVID-19 pandemic continues to ravage the world, the most pretentious sector besides the economy is the education system. Ethiopia is not equipped with the infrastructure and facilities to provide online classes for students at all levels. Hence, all institutions were re-opened with mandatory infection prevention and control (IPC) protocols such as the use of face masks, physical distancing, shifts in classes, and routine hand washing practices with soap and water to restrict the spread of the virus. Nevertheless, there has been no monitoring and follow- up and there is no data on IPC compliance among school children in the country. The purpose of this study was to examine the COVID-19 preventive practices and their associated factors among high and preparatory school students in Dessie City, Ethiopia.
Methods: A cross-sectional study was carried out by using a pre-tested face-to-face applied structured questionnaire and direct observations from March 8 to March 20, 2021, in five high and preparatory schools in Dessie City. The sample size was proportionally allocated in each school based on the students' total number registered in the first academic semester, then stratified by grade level, and proportionally allocated to each grade and section. Finally, a simple random sampling method was used to select study participants. Variables with p-values < 0.25 in the bivariate logistic regression analysis were entered into the multivariate logistic regression model.
Results: This study involved 422 students with a response rate of 98.8%. The level of good preventive practices was 43.7%. After adjusting for covariates, female, positive attitudes, received IPC training and clear accessible sharing of information and feedback with parents, students and teachers were identified as predictors of good precaution practices.
Conclusion: The prevalence of good prevention practices for COVID-19 among students was relatively very low. Therefore, the Department of Health and Education of Dessie City and each school should implement environmental health programs and promote prevention practices in high schools and preparatory schools.
Introduction
COVID-19, caused by severe acute respiratory syndrome-coronavirus 2 (SARS CoV-2 virus) was first detected in Hubei Province of China in December 2019 (1, 2). The contagious nature of the virus led WHO to declare it in March 2020 as a global pandemic (3, 4). By September 17, 2022, the virus had infected 493,429 people in Ethiopia (5). The most common initial COVID-19 symptoms include fever, dry cough, fatigue, breathing difficulties, and diarrhea (6, 7). These symptoms are normally mild, develop gradually and sometimes lead to serious complications such as cardiac and respiratory failures and death, especially in patients with comorbidities and in older people (8). The manifestation and symptoms change with new emerging variants of the virus (9). The virus is transmitted from person to person by respiratory droplets during sneezing, coughing, talking (10, 11) and through contact with people and surfaces (12, 13). The pandemic has spread at a slower pace in Africa than in other parts of the world (14, 15), apparently due to previous exposure of Africans to other infectious diseases such as Ebola virus disease and measles and the relatively young African population (15). However, due to lack of infrastructure, qualified personnel, and other resources, African health care systems experienced major difficulties in providing care for infected persons (16). Owing to the scarcity of vaccines, preventive measures promoting behavioral change continue to be more commonly used than vaccines in Africa, in contrast to Europe, East Asia, the USA and other industrialized countries (17).
After the outbreak of COVID-19 in early 2020, WHO proposed effective IPC, including the use of face masks and other personal protective equipment (PPE), alcohol-based sanitizers, social distancing, regular hand washing, contact tracing, and quarantine (18). Compliance with IPC protocols have been difficult in minimizing the risk of virus transmission (19) and the COVID-19 pandemic has disrupted public education (20). Stay-at-home pronouncements caused the closure of educational institutions across the world, prompting the shift to online teaching. Ethiopia, one of the least developed countries, does not have the resources for distant learning (13). As the schools and families do not have the resources for distant learning, the Ethiopian government recommends starting the teaching and learning processes in schools by implementing the COVID-19 prevention protocol. Hence, the government instructed all Ethiopian institutions to continue classroom teaching with the IPC directives. However, there is no detailed information on the enforcement, monitoring and compliance with these regulations and no COVID-19 prevention studies have been carried out in schools. This study examines the preventive practices and their associated factors for students in five high schools and preparatory schools in Dessie City, Ethiopia.
Materials and methods
Study area and study design
A cross-sectional study was carried out by using a pre-tested face-to-face applied structured questionnaire and direct observations from March 8 to March 20, 2021 in the five schools in Dessie City. Dessie is located in the highlands of Amhara Region. Of the city's five high schools and preparatory schools, three were government schools and two were private schools, with 9,024 students (4,341 males and 4,683 females) enrolled in March 2021.
Source population, inclusion and exclusion criteria
All Dessie City students in grades 9 through 12 enrolled from March 8 to March 20, 2021 were the source population and the sampled students who were available throughout the study period and willing to take part in the research were the study population. Students who were absent during the data collection period between March 8 and March 20 were excluded from the study.
Sample size determination
A single population proportion formula was used to obtain the sample size for this study.
The following assumptions were made: a 50% prevalence of preventive practices of students in high and preparatory schools since no study in Ethiopia on school students, a margin of error of 5%, a 95% CI, and a 10% non-response rate.
By adding a 10% non-response rate, the final sample size was 422 students.
Sampling technique
The sample size was allocated proportionally in each of the five schools studied based on the number of students enrolled in the first academic semester. The samples were then proportionally allocated to the 9th, 10th, 11th, and 12th grade levels, with each component of the relevant grade levels being further proportionally allocated. Finally, study participants were chosen by random sampling (lottery method) with classroom attendance as the sampling frame at the time of the survey.
Data collection methods and quality assurance
The face-to-face administered tools were adapted from the literature, the 2016 Ethiopian Demographic Health Survey (21), WHO (22), and UNICEF reports (23). Data were collected using structured questionnaire (self-reporting) and direct observation. The questionnaire consisted of five main sections: Section A contained 10 questions about socio-demographic status and sources of information on COVID-19; Section B contained 14 questions about water, sanitation, and hygiene behavior; Section C contained 17 questions about knowledge; Section D contained 15 questions about attitude, and Section E contained 22 questions about practice.
The data collectors were three environmental health professionals and three clinical nurses. One data collector was recruited for each school. The tool was prepared in English and then translated to Amharic, the local language, and back to English by two translators to check its consistency and completeness. The 2 days of training focused on instructing data collectors on how to collect data. The validity of the questionnaire was assessed by pretesting with 21 (5%) high and preparatory school students in nearby Kombolcha Town, and some amendments such as question order, avoiding less important questions, and editing questions that are unclear were made before the survey.
The reliability was determined by calculating the Cronbach's alpha method, which demonstrated satisfactory internal consistency. The Cronbach's alpha value for the preventive practice was 0.79, which indicates high reliability. No personal identifiers were obtained on the day of data collection, and COID-19 prevention measures were implemented throughout the procedure. The principal investigator supervised the process of data collection and supported the data collectors. Each questionnaire was checked daily for completeness and consistency before entering into computer data collectors. To check the quality of the entered data, 10% of the entered questionnaires were randomly selected and re-entered to identify potential data entry errors.
Outcome and explanatory variables
The outcome variable was preventive practices (good or poor) and the explanatory variables were socio-demographic status, water sanitation, hygiene (WASH), and sources of COVID-19 information. Four basic divisions were used to organize the explanatory variables. Section 1: Socio-demographic variables and source of information include age, sex, religion, grade, and household size, updated information from television, face book, internet Wi-Fi, families/friends, and received IPC training. Section 2: WASH variables; They include' number of students per class room, ventilation of class rooms and toilets, availability of alternative classes, posting of COVID-19 information in schools, sharing of information and feedback mechanisms between parents, students and teachers, information posts for events related to COVID- 19 in the schools, availability of psychosocial support, availability of piped water, availability of hand washing facilities, and availability of soap and alcohol-based hand sanitizer near wash basins. Section 3: Knowledge about coronavirus disease and its prevention and Section 4: Attitudes toward COVID-19 prevention.
Operational definitions
High school students: Students in grades 9 and 10 in 2020/21.
Preparatory school students: Students in 11th and 12th.
Knowledge: Respondents who scored equal to or above the mean value (≥14 out of 17 questions), were considered as having good knowledge, whereas a score of less than the mean value was considered as having poor knowledge about COVID-19 precautionary measures (Appendix 1).
Attitudes: Respondents who scored equal to or above the mean value (≥10 out of 15 questions), were considered to have a positive attitude, and scores of less than the mean value were considered to have a negative attitude about COVID-19 prevention (Appendix 1).
Practices: Respondents who scored equal to or above the mean value (≥11 out of 22 questions), were considered as having good preventive practices, whereas scores less than the mean value were classified as poor practices (see Table 4).
Data management and analysis
Prior to exporting the data to SPSS version 25.0 for analysis, it was cleaned, coded, and entered into EpiData version 3.1. Descriptive statistics were employed to evaluate the overall distribution, including means with standard deviations for continuous variables and frequencies and percentages for categorical variables. A binary logistic regression model with a 95% confidence interval was used to analyze the data (CI). A bivariate logistic regression analysis [crude odds ratio (COR)], as well as a regression of multivariate logistic analysis [adjusted odds ratio (AOR)], were carried out. Variables having a p < 0.250 were chosen for the analysis of multivariate logistic regression from the bivariate analysis (24). Variables having a significance level of <0.05 from the analysis of multivariate logistic regression were considered statistically significant and independently linked with good preventive measures among students.
Standard error with a cut-off value of 2 was used to check for multi-collinearity among independent variables. We discovered that the greatest standard error was 0.839, indicating that there was no multi-collinearity. The Hosmer Lemeshow test (24) was used to assess model fitness, yielding a p-value of 0.347, indicating that the model was fit.
Results
Socio-demographic characteristics of participants
Of the 422 students selected, 417 participated in the study, with a response rate of 98.8%. More than half of the students were Orthodox Christians [245 (58.8%)] and 89.4% of the participants were between 15 and 18 years old. The mean [±SD (standard deviation)] age of the students was 16.97 (±1.28), three-fifths [256 (61.4%)] were females and almost all (402, 96.4%)] were single. Nearly three-fourths (65.2%) of the participants were living in households with 4–6 members. Almost all participants got updated information on COVID-19 from television (377, 90.4%), families/and friends (395, 94.7%) (Table 1).
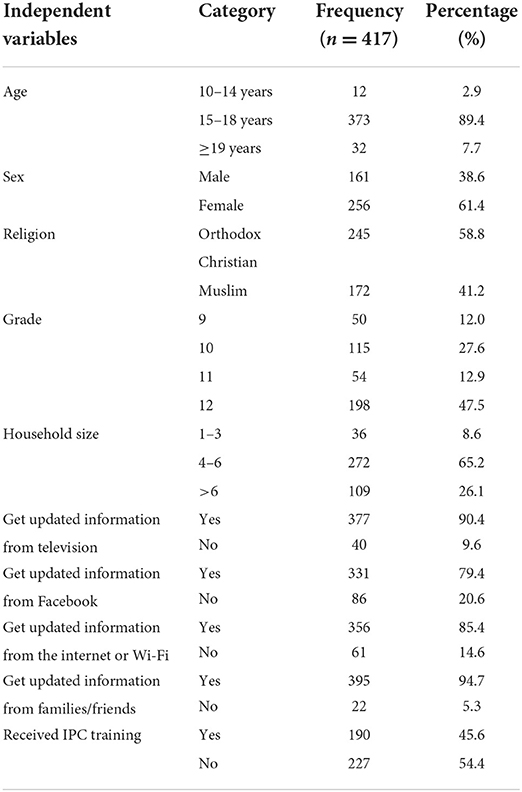
Table 1. Socio-demographic status and source of COVID-19 information utilized by high school and preparatory school students in Dessie City, Northeast Ethiopia.
WASH and preventive behavior
The main water source at all the schools was piped water in the school yards. There was no water interruption during the 2 weeks preceding the study (Table 2). The schools also posted some COVID-19 related information in its compounds (Table 3). There were hand-washing facilities in all five schools but no water and soap, and alcohol-based hand sanitizers were not available in any of the five schools during the observation period. Three-quarters (75.1%) of the students said that their classes had 39 or more students (Table 2), resulting in crowded conditions.
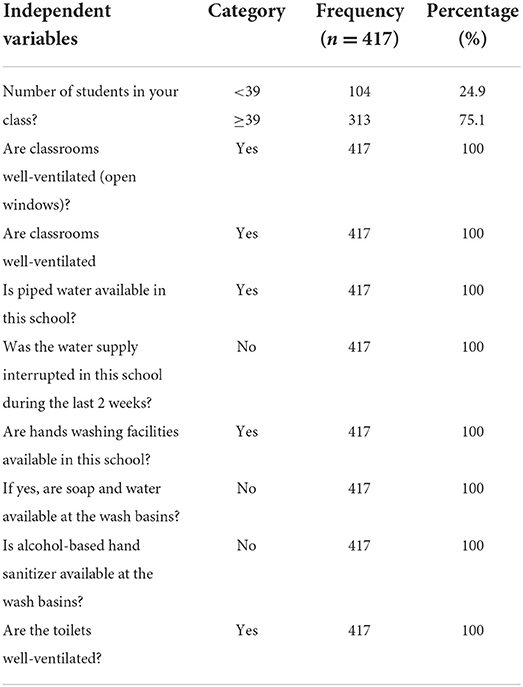
Table 2. Water, sanitation, and hygiene practices at high school and preparatory school students in Dessie City, Northeast Ethiopia.
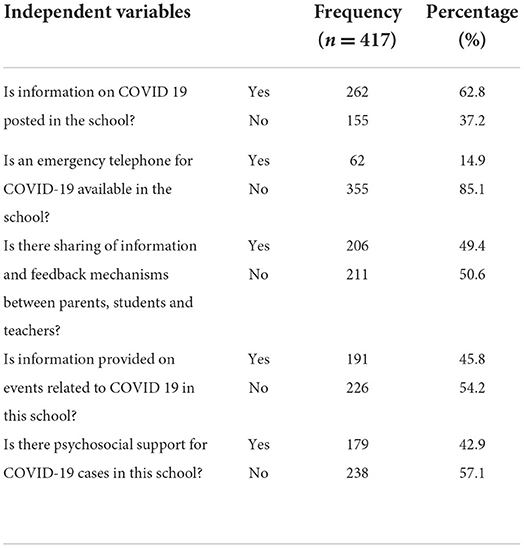
Table 3. COVID-19 related information posted at high schools and preparatory schools in Dessie City, Northeast Ethiopia.
More than half (247, 59.2%) of the students said that they always washed their hands using soap and water for a minimum of 20 s. Similarly, 218 (52.3%) allegedly used alcohol-based hand sanitizers. One-fourths (102, 24.5%) of the study participants washed their hands before entering the classroom, 94 (22.5%) before putting on and 92 (22.1%) after taking off a facemask and after sneezing and coughing (Table 2). Two-thirds (279, 66.9%) of the students supposedly wore a face mask or face covering cloth every time they left their home. Of the 417 participants, 145 (34.8%) stated that they always tried to maintain a 2- meter social distance when in public areas. Most of the study participants (345, 82.7%) had not reduced visits with friends and families, 254 (60.9%) continued to make non-essential trips outside their home and 238 (57.1%) and had no aversion to visiting crowded places. Nearly two-fifths (161, 38.6%) of the students avoided shaking hands, hugging and kissing during greetings since the advent of the coronavirus pandemic (Table 4).

Table 4. COVID-19 prevention measures among high school and preparatory school students in Dessie City, Northeast Ethiopia.
Overall, more than half (237, 56.8%) (95% CI: 52.3–61.9) of the students revealed that they had poor preventive practices and only 180 (43.2%) (95% CI: 38.1–47.7) had good practices (Table 4).
Factors associated with COVID-19 prevention
In the multivariable analysis, females, having received IPC training, sharing information and feedback established by parents, students and teachers who had a positive attitude were significantly associated with good preventive practices. Good preventive measures were 1.96 times more prevalent in females than in males (AOR = 1.96, 95% CI [1.24–3.10]). Students who received IPC training were 1.91 times more likely to practice prevention than those without training (AOR = 1.91, 95% CI [1.23–2.96]). Those who shared information and feedback with parents and teachers had a 2.11 times higher preventive practices score (AOR = 2.11, 95% CI [1.37–3.25]), and those with a positive perception of coronavirus precautionary measures were 3.33 times more likely to properly practice preventive practices (AOR = 3.33,95% CI [2.10–5.27]) than their counterparts (Tables 5, 6).
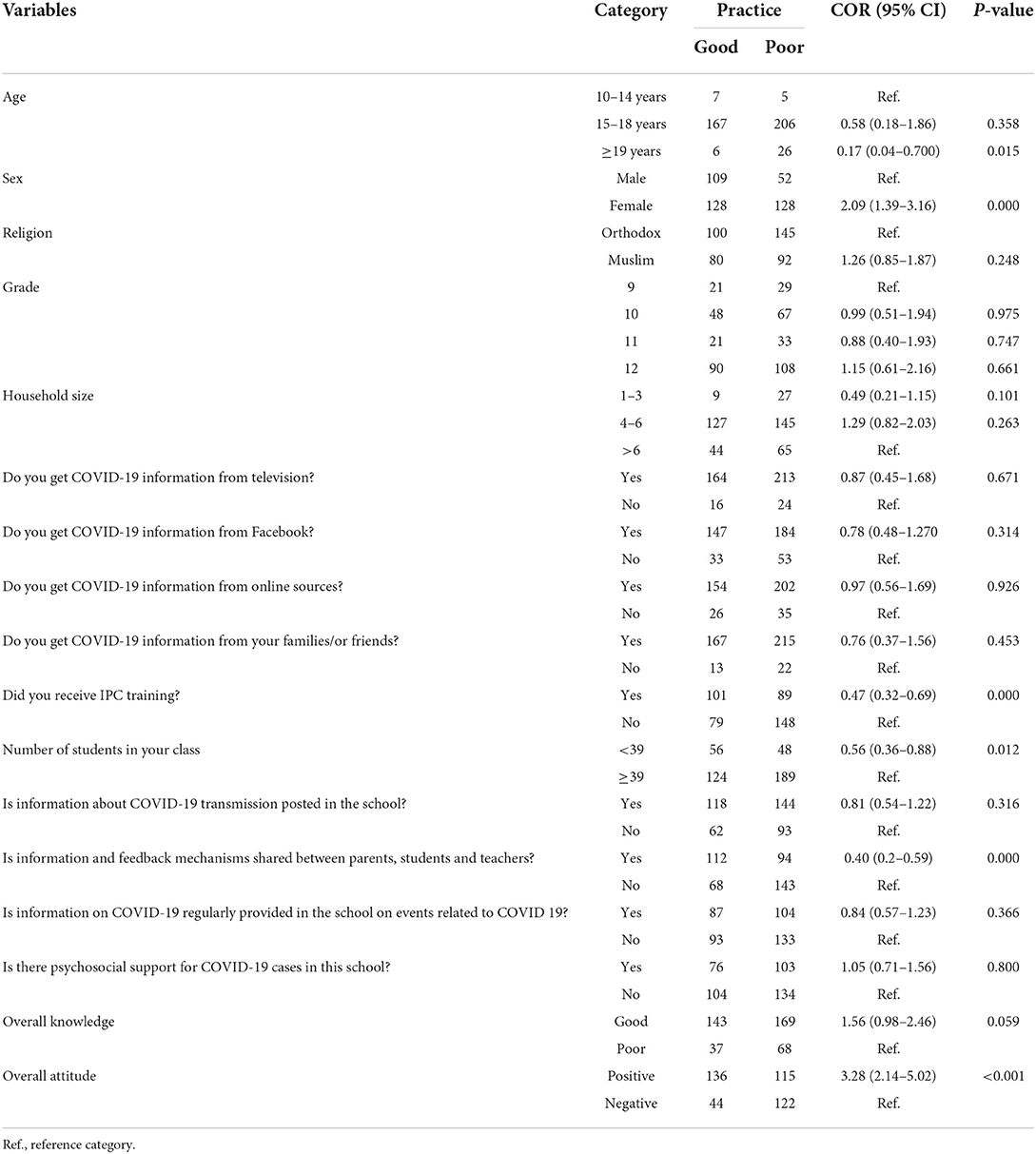
Table 5. Bivariate analysis of socio-demographic characteristics and sources of information on COVID-19 at high schools and preparatory schools in Dessie City, Northeast Ethiopia.
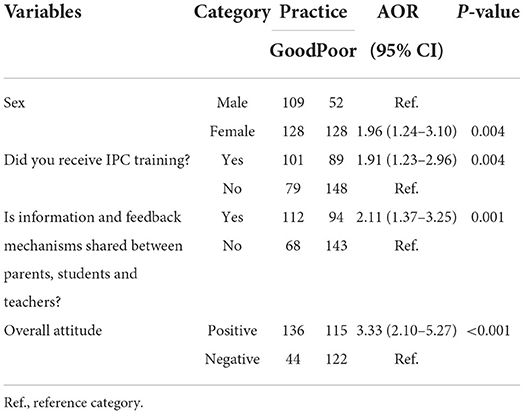
Table 6. Multivariate study of socio-demographic characteristics and sources of information regarding COVID-19 at high schools and preparatory schools in Dessie City, Northeast Ethiopia.
Discussion
The low prevalence (43.2%) of good preventive practices for COVID-19 among students in Dessie City is similar as in other studies in Ethiopia (25–28), Bangladesh (29), Sudan (30), and Egypt (31) and is lower than in other studies conducted in Ethiopia (32–35), Nepal (36), Syria (37), China (38), Uganda (39), and Pakistan (40). These discrepancies may be caused by variations in socio-demographic characteristics of the study populations, study areas, the time studies were carried out, occupation (health professionals vs. students), and the effectiveness of local COVID-19 programs. Probable reasons for the low preventive practices in this study may include the absence of an effective and comprehensive COVID-19 prevention program in the schools.
The higher prevalence of good preventive practices in Dessie schools than in three other communities in Ethiopia (41–43) is difficult to explain because they were carried out in general populations and among healthcare workers.
In this study, 247 (59.2%) participants allegedly washed their hands for a minimum of 20 s using soap and water, corroborating findings in Pakistan (56.0%) (44). But this rate is lower than those reported by two other studies in Ethiopia (81.4%) (32), (77.3%) (44) and studies in Pakistan (85.5%) (45), (94.0%) (46), Iran (82.2%) (47) and Beijing, China (91.3%) (48). These high rates were due to the relatively high socioeconomic level of participants, good WASH facilities, commitment of the government, and the recent study periods. The proportion of students washing their hands using soap and water after contacting any surface (176, 42.2%) was similar in our study as the one by Gebretsadik et al. among hospital visitors in another Ethiopian community (48.1%) (44).
The proportion of students reportedly wearing face masks when leaving home (66.9%) was similar to that reported by Jemal et al. (67.3%) (33) among Ethiopian health care workers and internet users in Nigeria (65.0%) (45), and high school students and young adults in Bangladesh (70.6%) (46). But our rate was higher than those reported for hospital patients (28) and a general population in Ethiopia (47), shoppers in the USA (41.0%) (48), a rural population in Egypt (47.3%) (49), and a general population in Syria (27.9%) (37). These variations may be due to differences in study dates and the effectiveness of local COVID-19 programs.
Only 38.6% of the students avoided shaking hands, hugging and kissing during greetings, a lower rate than those reported for Ethiopian health care workers (50), hospital visitors (48), and a predominantly rural population (44) and Syrian youth and adults on a social platform (92.5%) (37). Although the heterogeneity of these populations makes comparisons difficult, the absence of a COVID-19 prevention program in Dessie schools appears to be a significant factor in their low rates.
The rate of reporting good preventive practices was 1.9 times higher in females than in males. Similar ratios were reported by three other studies in Ethiopia (42, 51, 52) and by studies in Bangladesh (53), Uganda (54), Syria (37), Jordan (55), Iran (56), Beijing (57), Bangladesh (29), and in Saudi Arabia (58).
The positive attitude of the students about coronavirus prevention 3.33 times had better preventive practices than those who had a negative attitude. Similar rates were reported by a study in Sidama Region, Ethiopia (41), in northwest Ethiopia (52), Karachi, Pakistan (59), and north-central Nigeria (60), among primary, middle school students (57), and university students of China (38) and in the Sudanese population (30).
Students who had received IPC training were 1.91 times more likely to mention good preventive practices than those without IPC training, corroborating a study on health workers in Uganda (54) and frontline health workers in Nepal (61).
Study limitations
One possible limitation is that some students may appear to have given socially desirable response, mostly to questions about preventive behavior, although the extent of social desirability bias could not be determined.
Conclusion
This study revealed low rates of preventive behavior for COVID-19 and a wide gap between students' knowledge and practices. Scarcity of sanitary media, absence of accessible prevention and control training programs, and failure of parents and students to share information were major factors in the low prevention rates. We recommend that the Health and Education departments of Dessie City and administrations of the high schools and preparatory schools implement comprehensive COVID-19 prevention programs that address deficiencies in environmental health and promote health-enhancing behavior and attitudes. Furthermore, these entities should provide free personal protective equipment such as facemasks and alcohol-based hand sanitizer.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Review Committee of Wollo University's College of Medicine and Health Sciences gave their approval (Protocol number: CMHS/146/03/2021). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
All authors made a significant contribution to the work starting from the conception, study design, execution, acquisition of data, analysis and interpretation, in drafting, revising, or critically reviewing the manuscript. The authors also gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Acknowledgments
We acknowledge Dessie City Education Department and the school administrations for providing essential information and support. We also thank the data collectors, supervisors, and all respondents for participating in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1019584/full#supplementary-material
Abbreviations
AOR, Adjusted odds ratio; COR, Crude odds ratio; IPC, Infection prevention and control; WASH, Water, sanitation and hygiene.
References
1. Dzobo M, Hlongwa M, Denhere K, Kampira V, Mugoni M, Musuka G, et al. COVID-19 resurgence: lessons learnt to inform the South African response. Disaster Med Public Health Preparedness. (2021) 106:1–6. doi: 10.1017/dmp.2021.118
2. Li H, Wang Y, Ji M, Pei F, Zhao Q, Zhou Y, et al. Transmission routes analysis of SARS-CoV-2: a systematic review and case report. Front Cell Dev Biol. (2020) 8:618. doi: 10.3389/fcell.2020.00618
3. WHO. 2019-nCoV Outbreak' (Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV). (2020). Available online at: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-2019-ncov
4. Chandu VC, Lingamaneni KP, Pachava S, Baddam VRR, Marella Y. The influence of dissonance induction and assessment reactivity in improving adherence to COVID-19 precautionary measures: a cluster randomised controlled trial. Int Dental J. (2021) 72:141–8. doi: 10.1016/j.identj.2021.03.001
5. Worldometers. Coronovirus Statistics. (2022). Available online at: www.worldometers.info/coronavirus/
6. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
7. Chan JF-W, Yuan S, Kok K-H, To KK-W, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. (2020) 395:514–23. doi: 10.1016/S0140-6736(20)30154-9
8. Sofian M, Velayati AA, Banifazl M, Fotouhi F, Larijani MS, Afzali N, et al. SARS-CoV-2, a virus with many faces: a series of cases with prolonged persistence of COVID-19 symptoms. Wiener Med Wochenschr. (2021) 171:3–6. doi: 10.1007/s10354-020-00793-8
9. Clark A, Jit M, Warren-Gash C, Guthrie B, Wang HH, Mercer SW, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Global Health. (2020) 8:e1003–17. doi: 10.1016/S2214-109X(20)30264-3
10. Anfinrud P, Bax CE, Stadnytskyi V, Bax A. Could SARS-CoV-2 be transmitted via speech droplets? MedRxiv [Preprint]. (2020). 1–3. doi: 10.1101/2020.04.02.20051177
11. Georgiou GP, Kilani A. The use of aspirated consonants during speech may increase the transmission of COVID-19. Med Hypotheses. (2020) 144:109937. doi: 10.1016/j.mehy.2020.109937
12. Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, et al. Airborne transmission route of COVID-19: why 2 meters/6 feet of inter-personal distance could not be enough. Int J Environ Res. (2020) 18:2932. doi: 10.3390/ijerph17082932
13. Sahiledengle B, Tekalegn Y, Woldeyohannes D. The critical role of infection prevention overlooked in Ethiopia, only one-half of health-care workers had safe practice: a systematic review and meta-analysis. PLoS ONE. (2021) 16:e0245469. doi: 10.1371/journal.pone.0245469
14. Salyer SJ, Maeda J, Sembuche S, Kebede Y, Tshangela A, Moussif M, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet. (2021) 397:1265–75. doi: 10.1016/S0140-6736(21)00632-2
15. Musa HH, Musa TH, Musa IH, Musa IH, Ranciaro A, Campbell MC. Addressing Africa's pandemic puzzle: perspectives on COVID-19 transmission and mortality in sub-Saharan Africa. IntJ Infect Dis. (2021) 102:483–8. doi: 10.1016/j.ijid.2020.09.1456
16. Zenbaba D, Sahiledengle B, Takele A, Tekalegn Y, Yassin A, Tura B, et al. Compliance towards infection prevention measures among health professionals in public hospitals, southeast Ethiopia: a cross-sectional study with implications of COVID-19 prevention. Trop Med Health. (2021) 49:1–11. doi: 10.1186/s41182-021-00318-y
17. Hasan T, Beardsley J, Marais BJ, Nguyen TA, Fox GJ. The implementation of mass-vaccination against SARS-CoV-2: a systematic review of existing strategies and guidelines. Vaccines. (2021) 9:326. doi: 10.3390/vaccines9040326
18. WHO. Coronavirus, Prevention Measures. (2020). Available online at: https://www.who.int/health-topics/coronavirus#tab=tab_2
19. Ashinyo ME, Dubik SD, Duti V, Amegah KE, Ashinyo A, Asare BA, et al. Infection prevention and control compliance among exposed healthcare workers in COVID-19 treatment centers in Ghana: a descriptive cross-sectional study. PLoS ONE. (2021) 16:e0248282. doi: 10.1371/journal.pone.0248282
20. Rajab MH, Gazal AM, Alkattan K. Challenges to online medical education during the COVID-19 pandemic. Cureus. (2020) 12:e8966–e8976. doi: 10.7759/cureus.8966
21. Central Statistical Agency (CSA) [Ethiopia] ICF. Ethiopia Demographic and Health Survey. Addis Ababa; Rockville, MD: CSA and ICF (2016).
22. WHO. Coronavirus, Prevention Measures. Available online at: https://www.who.int/health-topics/coronavirus#tab=tab_2
23. UNICEF. COVID-19 and School Closures: Are Children Able to Continue Learning During School Closures?. UNICEF DATA (2020).
24. Hosmer J, Lemeshow S, Sturdivant R. Applied Logistic Regression. 3rd ed. Hoboken, NJ: John Wiley and Sons (2013).
25. Angelo AT, Alemayehu DS, Dacho AM. Knowledge, attitudes, and practices toward COVID-19 and associated factors among university students in Mizan Tepi University, 2020. Infect Drug Resistance. (2021) 14:349. doi: 10.2147/IDR.S299576
26. Desie Emiru T, Birlie TA, Tasew SF, Amare AT, Tibebu NS, Tiruneh CM. Assessment of knowledge, practice and associated factors towards prevention of novel corona virus among clients attending at Debre Tabor General Hospital Debre Tabor Town, North West Ethiopia, 2020: Institutional based cross-sectional study. J Commun Med Health Solut. (2020). doi: 10.2139/ssrn.3698545
27. Aynalem YA, Akalu TY, Gebresellassie B, Sharew NT, Assefa HK, Shiferaw WS. Assessment of undergraduate student knowledge, attitude, and practices towards COVID-19 in Debre Berhan University, Ethiopia. PLoS ONE. (2021) 16:e025044. doi: 10.1371/journal.pone.0250444
28. Akalu Y, Ayelign B, Molla MD. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen Hospital, Northwest Ethiopia. Infect Drug Resistance. (2020) 13:1949. doi: 10.2147/IDR.S258736
29. Ferdous MZ, Islam MS, Sikder MT, Mosaddek ASM, Zegarra-Valdivia J, Gozal D. Knowledge, attitude, and practice regarding COVID-19 outbreak in Bangladesh: an online-based cross-sectional study. PLoS ONE. (2020) 15:e0239254. doi: 10.1371/journal.pone.0239254
30. Sayedahmed AMS, Abdalla AAA, Khalid MHM. Knowledge, attitude and practice regarding COVID-19 among Sudanese population during the early days of the pandemic: online cross-sectional survey. Sci Afr. (2020) 10:e00652. doi: 10.1016/j.sciaf.2020.e00652
31. Kasemy ZA, Bahbah WA, Zewain SK, Haggag MG, Alkalash SH, Zahran E, et al. Knowledge, attitude and practice toward COVID-19 among Egyptians. J Epidemiol Global Health. (2020) 10:378. doi: 10.2991/jegh.k.200909.001
32. Tsegaye D, Shuremu M, Oljira D, Dubale S, Befekadu G, Bidira K. Knowledge and preventive practices towards COVID-19 and associated factors among healthcare workers in selected health facilities of Illu Aba Bor and Buno Bedelle Zones, Southwest Ethiopia. Preprints. (2020). doi: 10.20944/preprints2020110739
33. Jemal B, Ferede ZA, Mola S, Hailu S, Abiy S, Wolde GD, et al. Knowledge, attitude and practice of healthcare workers towards COVID-19 and its prevention in Ethiopia: a multicenter study. Sage Open Med. (2021) 9:1–10.: doi: 10.1177/20503121211034389
34. Desalegn Z, Deyessa N, Teka B, Shiferaw W, Hailemariam D, Addissie A, et al. COVID-19 and the public response: knowledge, attitude and practice of the public in mitigating the pandemic in Addis Ababa, Ethiopia. PLoS ONE. (2021) 16:e0244780. doi: 10.1371/journal.pone.0244780
35. Tadesse AW, Abebe NM, Tadesse SE, Wube MC, Abate AA. Preventive practice and associated factors towards COVID-19 among college students in Amhara Region, Ethiopia: a cross-sectional study. Ethiop J Health Sci. (2021) 31:3. doi: 10.4314/ejhs.v31i1.2
36. Limbu DK, Piryani RM, Sunny AK. Healthcare workers' knowledge, attitude and practices during the COVID-19 pandemic response in a tertiary care hospital of Nepal. PLoS ONE. (2020) 15:e0242126. doi: 10.1371/journal.pone.0242126
37. Al Ahdab S. A cross-sectional survey of knowledge, attitude and practice (KAP) towards COVID-19 pandemic among the Syrian residents. BMC Public Health. (2021) 21:296. doi: 10.1186/s12889-021-10353-3
38. Peng Y, Pei C, Zheng Y, Wang J, Zhang K, Zheng Z, et al. A cross-sectional survey of knowledge, attitude and practice associated with COVID-19 among undergraduate students in China. BMC Public Health. (2020) 20:1–8. doi: 10.1186/s12889-020-09392-z
39. Ssebuufu R, Sikakulya FK, Mambo SB, Wasingya L, Nganza SK, Ibrahim B, et al. Knowledge, attitude, and self-reported practice toward measures for prevention of the spread of COVID-19 among ugandans: a nationwide online cross-sectional survey. Front Public Health. (2020). 8:618731. doi: 10.3389/fpubh.2020.618731
40. Muhammad K, Saqlain M, Muhammad G, Hamdard A, Naveed M, Butt MH, et al. Knowledge, attitude, and practices (kaps) of community pharmacists regarding COVID-19: a cross-sectional survey in 2 provinces of Pakistan. Disaster Med Public Health Prep. (2021) 16:1864–72. doi: 10.1101/2020.05.22.20108290
41. Yoseph A, Tamiso A, Ejeso A. Knowledge, attitudes, and practices related to COVID-19 pandemic among adult populations in Sidama Regional State, Southern Ethiopia: a community based cross-sectional study. PLoS ONE. (2021) 16:e0246283. doi: 10.1371/journal.pone.0246283
42. Adane D, Yeshaneh A, Wassihun B, Gasheneit A. Level of community readiness for the prevention of COVID-19 pandemic and associated factors among residents of Awi Zone, Ethiopia: a community-based cross-sectional study. Risk Manage Healthc Policy. (2021) 14:1509. doi: 10.2147/RMHP.S302974
43. Mersha A, Shibiru S, Girma M, Ayele G, Bante A, Kassa M, et al. Health professionals practice and associated factors towards precautionary measures for COVID-19 pandemic in public health facilities of Gamo Zone, southern Ethiopia: a cross-sectional study. PLoS ONE. (2021) 16:e0248272. doi: 10.1371/journal.pone.0248272
44. Gebretsadik D, Ahmed N, Kebede E, Gebremicheal S, Belete MA, Adane M. Knowledge, attitude, practice towards COVID-19 pandemic and its prevalence among hospital visitors at Ataye district hospital, Northeast Ethiopia. PLoS ONE. (2021) 16:e0246154. doi: 10.1371/journal.pone.0246154
45. Isah MB, Abdulsalam M, Bello A, Ibrahim MI, Usman A, Nasir A, et al. Coronavirus disease 2019 (COVID-19): A cross-sectional survey of the knowledge, attitudes, practices (KAP) and misconceptions in the general population of Katsina State, Nigeria. UMYU J Microbiol Res. (2021) 6:24–37. doi: 10.1101/2020.06.11.20127936
46. Banik R, Rahman M, Sikder MT, Rahman QM, Pranta MUR. Knowledge, attitudes, and practices related to the COVID-19 pandemic among Bangladeshi youth: a web-based cross-sectional analysis. Z Gesundh Wiss. (2020) 1–11. doi: 10.21203/rs.3.rs-37946/v1
47. Afzal MS, Khan A, Qureshi UUR, Saleem S, Saqib MAN, Shabbir RMK, et al. Community-based assessment of knowledge, attitude, practices and risk factors regarding COVID-19 among Pakistanis residents during a recent outbreak: a cross-sectional survey. J Commun Health. (2020) 43:476–86. doi: 10.1007/s10900-020-00875-z
48. Haischer MH, Beilfuss R, Hart MR, Opielinski L, Wrucke D, Zirgaitis G, et al. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLoS ONE. (2020) 15:e0240785. doi: 10.1371/journal.pone.0240785
49. El-Gilany A-H, El-Bastawesy S, Ali SI. Knowledge, attitude and practices (KAP) of rural population about COVID-19: a community-based study in Talkha District, Egypt. Int J Novel Res Healthc Nursing. (2020) 7:525–32.
50. Twinamasiko N, Olum R, Gwokyalya AM, Nakityo I, Wasswa E, Sserunjogi E. Assessing knowledge, attitudes and practices towards COVID-19 Public Health preventive measures among patients at Mulago National Referral Hospital. Risk Manage Healthc Policy. (2021) 14:221. doi: 10.2147/RMHP.S287379
51. Kebede Y, Yitayih Y, Birhanu Z, Mekonen S, Ambelu A. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PLoS ONE. (2020) 15:e0233744. doi: 10.1371/journal.pone.0233744
52. Kassie BA, Adane A, Abebe Kassahun E, Ayele AS, Kassahun Belew A. Poor COVID-19 preventive practice among healthcare workers in Northwest Ethiopia. Adv Public Health. (2020) 2020. doi: 10.1155/2020/7526037
53. Sultana MS, Khan AH, Islam MR, Hossain S, Hasan MT, Kurasaki M, et al. Gender differences in knowledge, attitude and preparedness to respond to COVID-19 among adult population in Bangladesh: A Cross-Sectional Study 2020. Preprints. (2020). doi: 10.20944/preprints202011.0739.v1
54. Amanya SB, Nyeko R, Obura B, Acen J, Nabasirye C, Nakaziba R, et al. Knowledge and compliance with covid-19 infection prevention and control measures among health workers in regional referral hospitals in Northern Uganda: a cross-sectional online survey. F1000Research. (2021) 10:136. doi: 10.12688/f1000research.51333.2
55. Olaimat AN, Aolymat I, Elsahoryi N, Shahbaz HM, Holley RA. Attitudes, anxiety, and behavioral practices regarding COVID-19 among university students in Jordan: a cross-sectional study. Am J Trop Med Hyg. (2020) 103:1177–83. doi: 10.4269/ajtmh.20-0418
56. Honarvar B, Lankarani KB, Kharmandar A, Shaygani F, Zahedroozgar M, Haghighi MRR, et al. Knowledge, attitudes, risk perceptions, and practices of adults toward COVID-19: a population and field-based study from Iran. Int J Public Health. (2020) 65:731–9. doi: 10.1007/s00038-020-01406-2
57. Wen F, Meng Y, Cao H, Xia J, Li H, Qi H, et al. Knowledge, attitudes, practices of primary and middle school students at the outbreak of COVID-19 in Beijing: a cross-sectional online study. MedRxiv. (2020). doi: 10.1101/2020.06.29.20138628
58. Al-Hanawi MK, Angawi K, Alshareef N, Qattan AM, Helmy HZ, Abudawood Y, et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Front Public Health. (2020) 8:217. doi: 10.3389/fpubh.2020.00217
59. Jawed F, Manazir S, Zehra A, Riaz R. The novel Coronavirus disease (COVID-19) pandemic: knowledge, attitude, practice, and perceived stress among health care workers in Karachi, Pakistan. Med J Islamic Republic Iran. (2020) 34:132. doi: 10.47176/mjiri.34.132
60. Reuben RC, Danladi MM, Saleh DA, Ejembi PE. Knowledge, attitudes and practices towards COVID-19: an epidemiological survey in North-Central Nigeria. J Commun Health. (2020) 46:457–70. doi: 10.1007/s10900-020-00881-1
Keywords: COVID-19, preventive practices, high school and preparatory school students, Ethiopia, infection prevention and control
Citation: Feleke A, Gebrehiwot M, Kloos H, Embrandiri A, Daba C, Hassen S and Adane M (2022) COVID-19 preventive practices and associated factors among high school and preparatory school students in Dessie City, Ethiopia. Front. Public Health 10:1019584. doi: 10.3389/fpubh.2022.1019584
Received: 15 August 2022; Accepted: 25 October 2022;
Published: 21 November 2022.
Edited by:
Hasan Mahmud Reza, North South University, BangladeshReviewed by:
Mila Nu Nu Htay, Manipal University College Malaysia, MalaysiaArista Lahiri, Indian Institute of Technology Kharagpur, India
Copyright © 2022 Feleke, Gebrehiwot, Kloos, Embrandiri, Daba, Hassen and Adane. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alelgne Feleke, YWxlbGduZWZlQGdtYWlsLmNvbQ==; Mesfin Gebrehiwot, Z2VicmVoaXdvdG1lc2ZpbkB5YWhvby5jb20=; Metadel Adane, bWV0YWRlbC5hZGFuZTJAZ21haWwuY29t
 Alelgne Feleke1*
Alelgne Feleke1* Mesfin Gebrehiwot
Mesfin Gebrehiwot Chala Daba
Chala Daba