
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 16 November 2022
Sec. Family Medicine and Primary Care
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1018686
This article is part of the Research TopicApplied Research in Primary Care: Improving Citizens' Health and Well-being in the Real WorldView all 36 articles
 Ahmed Hiko1*
Ahmed Hiko1* Nega Assefa1
Nega Assefa1 Zerihun Ataro2
Zerihun Ataro2 Addisu Sertsu1
Addisu Sertsu1 Elias Yadeta1
Elias Yadeta1 Teganu Balcha1
Teganu Balcha1 Abdulkerim Amano1
Abdulkerim Amano1 Henock Asfaw1
Henock Asfaw1 Deribe Bekele Dechasa1
Deribe Bekele Dechasa1 Kabtamu Nigussie1
Kabtamu Nigussie1 Lemesa Abdisa1
Lemesa Abdisa1Background: Coronavirus disease (COVID-19) is a viral-borne infection caused by the SARS-CoV-2 virus. Aside from the morbidity and mortality effects, it leaves the majority of hypertensive patients untreated and vulnerable to uncontrolled hypertension.
Objective: The purpose of this study was to assess follow-up conditions of care and its associated factors among adult hypertensive patients during COVID-19 in public health facilities of West Arsi, Southeastern Ethiopia.
Methods: A health facility-based retrospective cross-sectional study was conducted among 423 adult hypertensive patients in the West Arsi public health facilities from July 5 to August 6, 2021. A systematic random sampling technique was used to recruit the study participants. A pretested structured face-to-face interviewer and medical records were used to collect sociodemographic variables, basic clinical features, and follow-up data. The follow-up conditions of care were assessed using 12 items with “yes or no” questions. Then, based on the mean value of the items, the follow-up conditions of care were dichotomized into good and poor. As a result, the follow-up condition was good if the score was greater or equal to the mean, and poor unless otherwise. To investigate parameters related with follow-up conditions of care, bivariable and multivariable logistic regression analyses were used. A 95% confidence interval and a p-value of 0.05 were used to indicate a significant association.
Results: The rate of poor follow-up conditions of care during COVID-19 was 29% (95% confidence interval: 24.9–33.4%), according to this study. Age ≥ 60 years (AOR = 3.55; 95% CI: 2.09–6.03), transportation problem (AOR = 2.43; 95% CI: 1.28–4.61), fear of COVID-19 (AOR = 3.34; 95% CI: 1.59–7.01), co-morbidity (AOR = 1.93; 95% CI: 1.14–3.26) and physical distancing (AOR = 2.43; 95% CI: 1.44–4.12) were significantly associated with poor follow-up conditions of care.
Conclusions: In our study, 29% of the participants had poor follow-up care conditions. When compared to WHO recommendations, the findings of this study may explain poor follow-up care conditions. To enhance patients' follow-up treatment, evidence-based target interventions should be designed and executed, taking into account individuals at high risks, such as those over the age of 60 and those with comorbidities, and identifying additional risk factors.
COVID-19 is one of the most common causes of death associated with severe acute respiratory syndrome 2 (SARS-COVID-2) (1). Since its inception, the global shutdown has caused global population challenges in isolation and quarantine measures, affecting nearly 620 million confirmed cases and nearly 6.54 million deaths as of 25 September 2022 (2).
The non-communicable diseases worsen the severity of COVID-19 and raise the risk of death (3). Hypertension is the leading cause of global public health problems (4). It is the leading risk factor for global disease burden, accounting for 7% of global disability-adjusted life years (DALY) (5). Hypertension affects 31.1% of the worldwide population, with Ethiopia accounting for 30.2% (6). Hypertension is a risk factor for cardiovascular disease and the leading cause of mortality (7). According to the World Health Organization (WHO), its complications account for 94 million deaths worldwide, with ~17 million deaths from cardiovascular disease occurring each year (7). According to one study, hypertension complications cause 45% of heart disease deaths and 51% of stroke deaths (8).
Poor follow-up care is a situation in which patients are unable to receive the WHO-recommended usual follow-up care service within the planned appointment time frame for a variety of reasons. Typical follow-up treatment includes Bp measurement, medication refilling, lifestyle change recommendations, monitoring medication adherence, reviewing laboratory work, screening cardiovascular risks, and so on. When the target blood pressure was reached, WHO recommended varied checks at 3 to 6 month intervals, depending on the patients' health status. Individuals with higher BPs require shorter intervals (every 1 or 2 months), and an emergency visit is required if BP is 180/110 mmHg (9, 10).
Bp measurements are necessary for hypertension screening, diagnosis, and therapy. With restricted physical access to patients during COVID-19, healthcare providers are unsure how to measure blood pressure and analyze cardiovascular risk factors (11). Some patients avoid or postpone seeking care due to their fear of contracting COVID-19, and the ability to treat hypertensive patients has been jeopardized (12). Because of COVID-19, every system was altered, resulting in increased morbidity and mortality (13, 14).
According to the WHO disease burden and mortality estimates, non-communicable disease deaths in Africa increased from 22.8% in 2000 to 34.2% in 2016 (15). COVID-19, on the other hand, increases the burden of mortality by 13.7% in hypertensive patients (16). Border restrictions and lockdowns disrupted 64% of health services, lost patients from follow-up, and decreased medicine supplies, especially in low and middle-income countries (LMICs) (17, 18). Even for measured blood pressure status, there were 87.6% physical examinations, 47.6% laboratory tests, and 50% assessments of end-organ damage and cardiovascular risks (12). In addition, the epidemic increases the severity of hypertension problems such as ischemic heart disease, stroke, cardiovascular disease, and mortality (18, 19).
Around the world, uncontrolled hypertension causes 500,000 fatalities each year (4). According to research done in SSA, 77.4% of people had uncontrolled blood pressure. The incidence of uncontrolled hypertension varied significantly between studies, ranging from 11 to 70% (20, 21). When compared to before the COVID-19 epidemic, the prevalence of uncontrolled hypertension has skyrocketed (22). Despite COVID-19 challenges, numerous efforts have been implemented to enhance follow-up conditions of treatment and address other consequences of hypertension. A few of these included the use of telemedicine, connecting patients with neighboring medical centers, and extending the time between drug refills to reduce potential harm from subpar follow-up conditions of treatment (23–25). Despite various research on hypertension in Ethiopia, no investigations on follow-up care conditions and associated factors have been conducted. Again, the rate of follow-up care was unknown since the hypertensive patient treatment had been discontinued, drug supply had been disrupted, and all systems had changed as a result of COVI-19. Therefore, this study aims to evaluate the follow-up conditions of care and its associated factors among adult hypertensive patients during COVID-19 in public health facilities of the West Arsi zone, Southeastern Ethiopia.
A health facility-based retrospective cross-sectional study was conducted from July 5 to August 6, 2021. From all public health facilities, Kuyera specialized referral hospital, Melka Oda general hospital, Dodola general hospital, Abbosto health center, and Awasho health center were selected by simple random sampling method. The data retrieval period was from March 13, 2020, to March 14, 2021, for secondary data. Shashemene is the capital city of the West Arsi zone, which is located 250km from Addis Ababa. The overall population of this zone was estimated to be 2,520,875 according to the 2017 Central Statistical Agency population census, of whom 50.8% were women and 13.02% of those living there were urban residents (26).
The study included all adult hypertensive patients who had been taking anti-hypertensive medications for at least 6 months and were eligible for the study to assess follow-up conditions of care. But Patients with cognitive impairment, newly diagnosed, and incomplete medical records were excluded from the study. The sample size calculation was done using a single population formula. Since there was no previous research on the subject, the following assumptions were taken into account while determining the sample size: 95% confidence interval, 5% margin of error, and 50% prevalence of poor follow-up conditions of care since there was lack of published similar study on a similar topic. The total sample size increased to 423 after adding a 10% non-response rate. The following public health institutions had a total of 1,605 patients under follow-up care: Kuyera specialized referral hospital (520), Melka oda general hospital (352), Dodola general hospital (544), Abbosto health center (103), and Awasho health center (86). The average number of patients visiting a health institution each month was calculated by looking through the registration books of each facility's medical records, and then, 423 participants were proportionally allocated to each facility. Finally, from Kuyera referral hospital, Melka Oda general hospital, Dodola general hospital, Abbosto health center, and Awasho health center, respectively, 137, 93, 143, 27, and 23 people were hired. Following the determination of the K value, a systematic random sampling technique was used to choose research participants. The first case was chosen by lottery, and the remaining individuals were recruited and added one at a time.
Due to the lack of standard tools (24, 27), the questionnaires were created by evaluating prior research in a way that incorporated all the factors that may achieve the study objectives. They were then adapted for the local context. To gather information from research participants, it was written in English and then translated into Afan Oromo, the local language. The tool includes socio-demographic data (age, sex, religion, educational level, marital status, place of residence, and monthly income), fundamental clinical data (family history, comorbidity, and time since diagnosis), and follow-up conditions of care-related questions (patients attendance, medication refilled, inpatient visit, prior consultation, the form of consultation, access to medication, etc.). To evaluate patients' attendance at the medical institution, blood pressure measurements, and medication refills, a checklist was also employed to analyze their medical records. By using Cronbach's alpha (α), the internal consistency of the questionnaire was further examined, and 12 follow-up items received a score of 0.85. The data was gathered using a structured face-to-face interviewer-administered questionnaire. Two health officers served as facilitators and three BSc nurses served as data collectors. Throughout the data-collecting period, all COVID-19 safety procedures were followed.
There were two categories for the follow-up conditions of care: good and poor. Twelve “yes-no” questions were used to assess the follow-up conditions of care. From twelve items, two of them (unable to obtain prescription drugs and unable to obtain an in-person appointment) were negatively written, but before the analysis, they were recorded in the opposite direction to facilitate computation with other positive items. Following computation using SPSS, the mean cutoff follow-up conditions of care was eight with SD ± 0.1. Following that, the overall score for the follow-up conditions of care was divided into two categories: good for people who scored higher than or equal to the mean, and poor unless otherwise stated.
Good follow-up conditions: Participants in the study who achieve results above or equal to the mean on the follow-up conditions of care questions are in good follow-up circumstances (28, 29).
Poor follow-up conditions: Participants in the study who achieve results below the mean on the follow-up conditions of care questions are in poor follow-up circumstances (28, 29).
Medical disruptions: If an individual had to miss or cancel previously scheduled appointments or is unable to get an in-person appointment to see their provider (30).
Prescription drug disruption: If an individual is unable to obtain the prescription drugs they need or have to stop taking drugs exactly as prescribed to extend the supply (30).
Uncontrolled hypertension: If BP ≥150/90 mmHg in hypertensive patients aged 60 years or ≥140/90 mmHg for patients aged <60 years and all hypertensive patients with diabetes mellitus (DM) or chronic kidney disease (CKD) based on the average of three measurements (31).
Older: Those individuals with an age great or equal to 60 years.
Younger: Those individuals below the age of 60.
Physical distancing: Keeping a distance of 2 m from one another and limiting activities outside the home.
Fear of COVID-19: Anxiety and stress related to COVID-19 disease.
Isolation: Staying at home and avoiding contact with others.
To reduce prejudice, data collectors were hired from outside the data collection area. To ensure a common understanding, the principal investigator trained data collectors and supervisors for 2 days on the research's objectives, components, how to choose study participants, ethical issues, and a basic description of data gathering. Before the actual data collection, a pretest on 5% of the total sample was performed in the Negelle Arsi health center to improve data quality. Last but not least, significant input was included in the survey. The data collectors were under the supervision of supervisors. Every day, the supervisors rechecked the questionnaire's accuracy to address one issue at a time.
Epi data version 3.1 software was used to enter the data, which was then exported and analyzed using SPSS version 26. Variables were compiled using descriptive statistics (frequency distributions, mean, median, standard deviation, and calculation of variables). A descriptive frequency analysis was performed to look for any missing values and outliers. To determine the linear correlations among independent variables, multicollinearity was examined using variance inflation factors and a tolerance test. As a result, no variables in this study had a VIF > 10 or a tolerance test of 0.1. Hosmer-Lemeshow and Omnibus tests were used to assess the model's goodness of fit. Hosmer-Lemeshow (p = 0.473) and Omnibus tests (p = 0.000) showed a good model fit. To account for all potential confounders, in binary logistic regression, variables with p-values ≤ 0.25 at 95% confidence intervals (CI) were taken into consideration and integrated into the multivariable regression model. An adjusted odds ratio with a 95% confidence interval was deemed statistically significant in the multivariable model at a p-value of ≤0.05.
The research included a total of 409 participants, yielding a 96.69% response rate. More than half of the study participants 228 (55.7%) were male. The median age (±SD) was 52 ± 14.38 years and 142 (34.7%) fall within the age above 60 years. Around 26.9% attended Elementary school, 35.9% were farmers in occupation, and 53.1% were urban dwellers.
In terms of essential clinical characteristics, 91 (22.2%) people had a family history of hypertension. One hundred eighty-one responders (44.3%) reported co-morbidities with various conditions. The median illness duration for hypertensive patients was 4.98 years, with an interquartile range of 4.5 years (Q1 = 2.5 and Q3 = 7). The disease duration varied from 1 to 20 years. Of all responders, 343 (83.9%) were using one or more anti-hypertensive medications (Table 1).
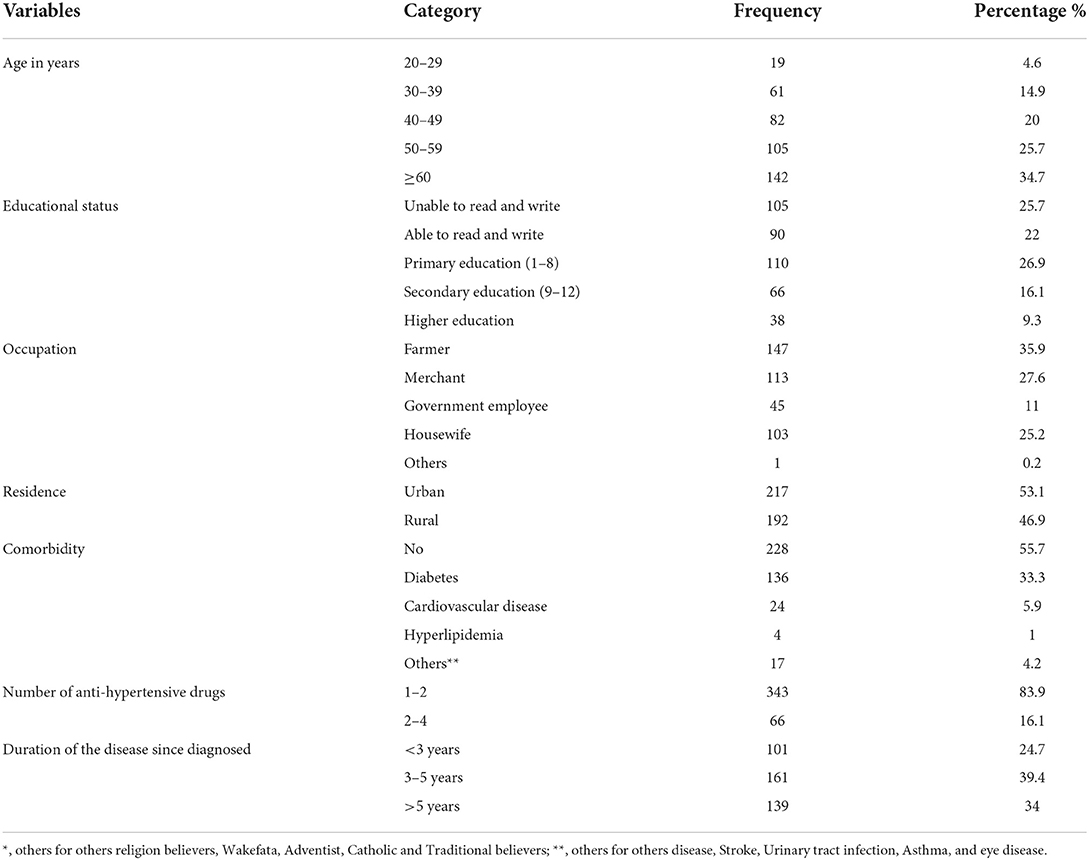
Table 1. Socio-demographic characteristics and basic clinical characteristics of hypertensive patients at West Arsi public health facilities, 2021 (N = 409).
Poor follow-up conditions of care had an overall rate of 29% (95% confidence interval: 24.9–33.4%). In terms of the follow-up conditions of care, 347 (84.8%) people visited a medical institution, 84.3% had their blood pressure taken, 84.1% had their prescriptions renewed, and 83.1% received counseling. Participants in the research who had a prior consultation <3 months ago totaled 359 (75.6%). Ninety-two (22.5%) people experienced medical issues, whereas 338 (82.6%) people were able to get prescription drugs. Seventy-four (18.1%) had to cease taking prescription medications exactly as directed. Three hundred forty (83.1%) had access to medicines from medical facilities, 375 (91.7%) had access to in-person consultations with medical experts, 384 (93.9%) had appointments for in-person consultations, and 171 (41%) had appointments for telephone consultations with medical professionals (Table 2).
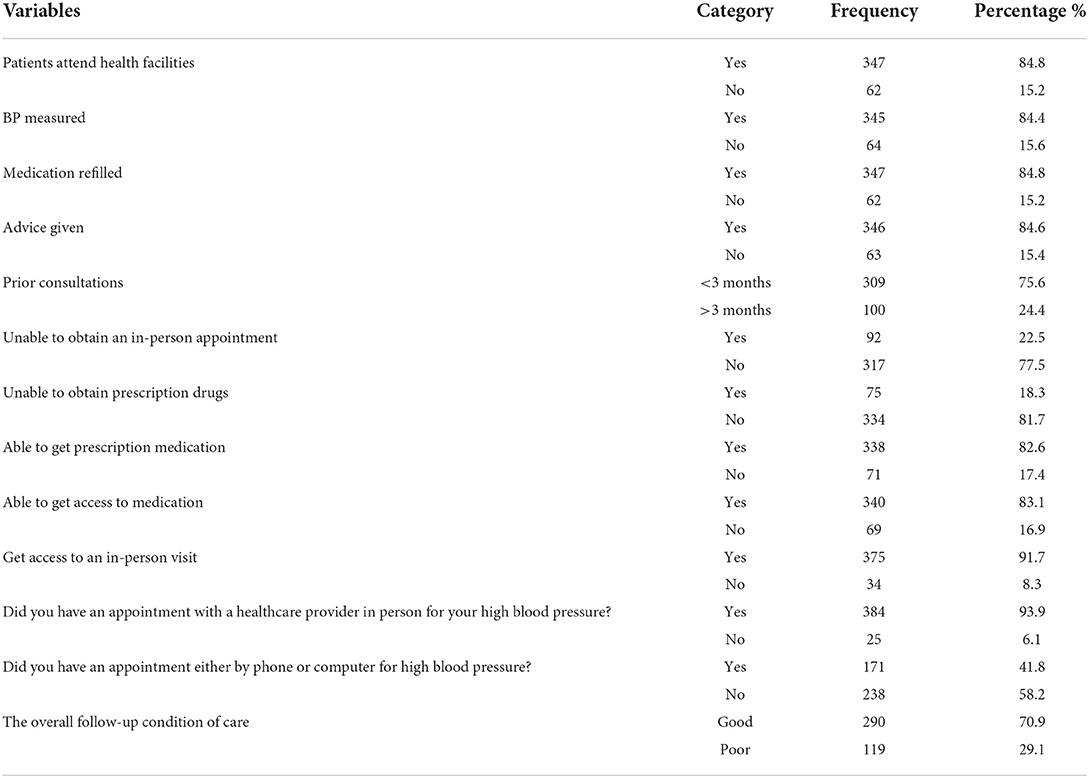
Table 2. Follow-up condition of care among adult hypertensive patients at West Arsi public health facilities during COVID-19, Ethiopia, 2021 (N = 409).
Of those who had to cease taking prescription medications exactly as directed or were unable to acquire them, 24 (32%), 72 (96%), 35 (46.7%), 51 (68%), and 42 (56%) were due to closed hospital/clinics, fear of COVID-19, closed pharmacy, fear of using public transit, and the rising cost of medications, respectively, as indicated in Table 3.
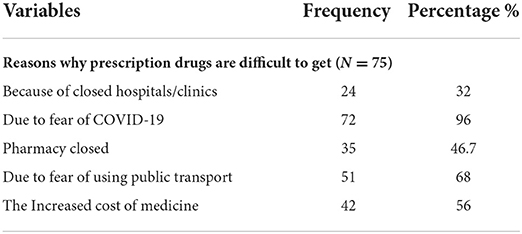
Table 3. Reasons why prescription drugs are difficult to get among adult hypertensive patients at West Arsi Public health facilities during COVID-19, Ethiopia, 2021 (N = 75).
Of all respondents, 340 (83.1%) needed to access medication from health facilities, while the remaining respondents were unable to do so for a variety of reasons, including difficulty accessing providers (38.2%), difficulty traveling (82.3%), inability to pay for medication costs (76.4%), and pharmacy closure (67.6%), as indicated in Figure 1.
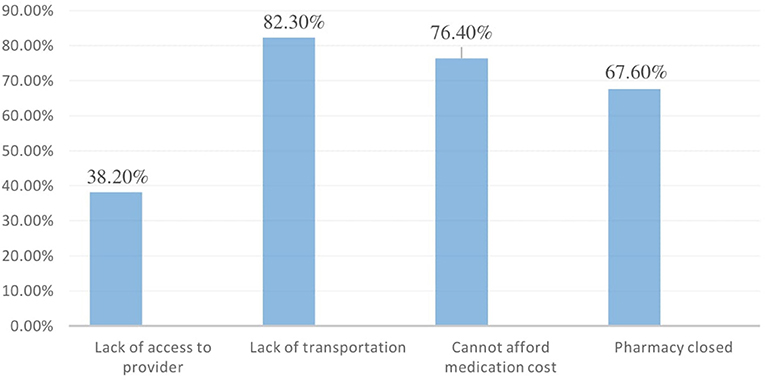
Figure 1. Reasons why some people cannot get medicine during COVID-19, among hypertensive patients at West Arsi public health facilities, Ethiopia, 2021.
Of all respondents, 204(49.9%) said their prescriptions were renewed every 3 months, while only 1.7% said they weren't (Figure 2).
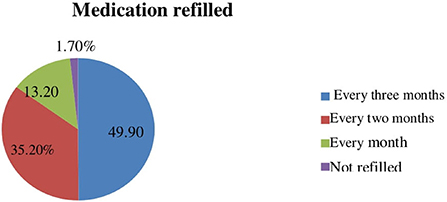
Figure 2. Medication refilled during COVID-19, among hypertensive patients at West Arsi public health facilities, Ethiopia, 2021.
According to the findings of this survey, 217 (53.1%) insufficient transportation, 169 (41.3%) pharmaceutical costs, 263 (63.3%) fear of COVID-19, and 138 (33.7%) shortage of necessary medicine and closure of some health facilities are possible reasons that reduce access to health care (Figure 3). One hundred twenty-nine (31.5%) reported that their health condition declined due to a lack of access to health care.
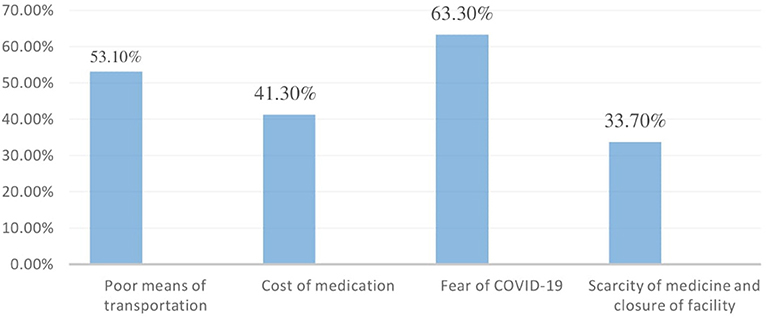
Figure 3. The potential cause of reduced access to healthcare among adult hypertensive patients on follow-up at West Arsi public health facilities, Ethiopia, 2021.
According to this study, 244 (59.7%) of study participants reported lockdown measures, followed by physical distancing 188 (46%), and isolation 76 (18.6%) were factors that affected seeking health care services.
In a binary logistic regression analysis, poor follow-up conditions of care were substantially correlated with age, educational status, monthly income, site of residence, comorbidities, transportation issues, fear of COVID-19, physical distance, and isolation. However, gender, religion, occupation, and marital status were not associated with the outcome variable. To control confounders, all variables with a p-value of <0.25 in the bivariable analysis were further considered in the multivariable logistic regression analysis.
Age, fear of COVID-19, transportation issues, comorbidities, and physical distance were all substantially linked with poor follow-up conditions of care on multivariable logistic regression analysis with a p-value < 0.05. Patients over the age of 60 were 3.55 times more likely than younger people to have poor follow-up conditions of care (AOR = 3.55, 95% CI: 2.09–6.03). Those who dread COVID-19 are 3.34 times more likely than their counterparts to have poor follow-up conditions of care (AOR = 3.34, 95% CI: 1.59–7.01). When compared to patients without transportation issues, patients with transportation issues had a 2.43 times higher likelihood of having poor follow-up conditions of care (AOR = 2.43, 95% CI: 1.28–4.61). Comorbidities increased the likelihood of having poor follow-up conditions of care by 1.93 times compared to counterparts (AOR = 1.93, 95% CI: 1.14–3.26). When the physical distance was present, the odds of poor follow-up conditions of care were 2.43 times greater than when it wasn't (AOR = 2.43, 95% CI: 1.44–4.12) at p-value 0.05 (Table 4).
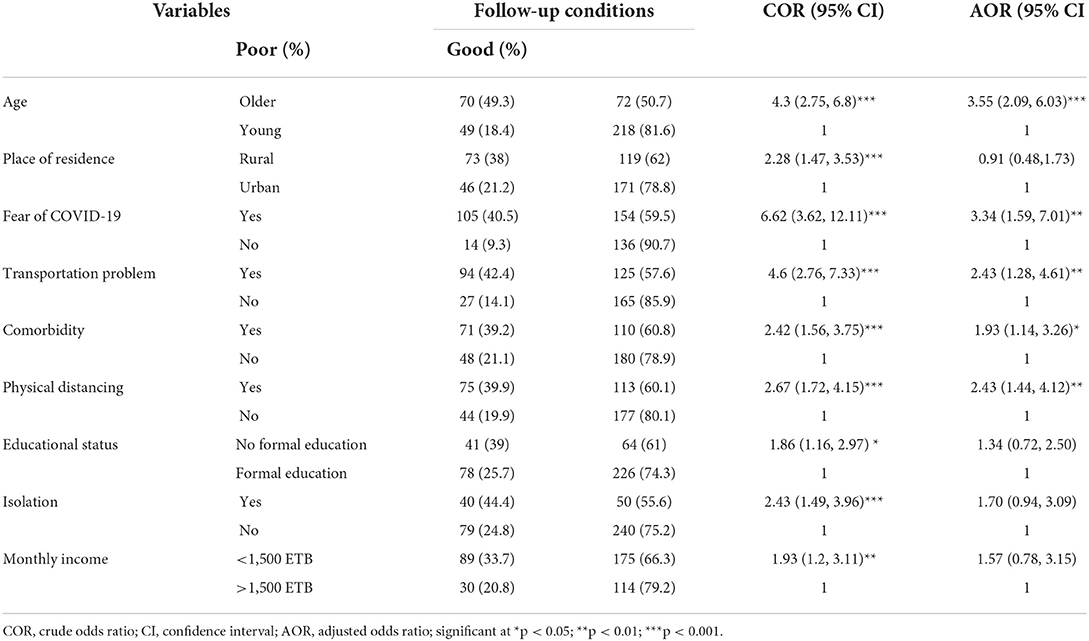
Table 4. Bivariable and multivariable logistic regression analysis depicting factors associated with poor follow-up conditions of care among adult hypertensive patients at West Arsi public health facilities, Ethiopia, 2021 (N = 409).
According to this study, 29% of patients had poor follow-up conditions. This discovery was consistent with observations from Northwest Ethiopia (32). However, the results of this study were lower (70%) than those of the Addis Ababa study (23). These may be explained by variations in temporary lockdown measures, attitudes about COVID-19, and methodological variations, particularly in terms of data collection techniques and research timeframe. In the current study, patients over the age of 60 years were more likely to have poor follow-up conditions of care. This matched the findings of the Addis Ababa investigation (23). The elderly are at a higher risk of COVID-19 case fatality, no caregivers are available for senior patients, and there are comorbid conditions present, which discourage the patients from attending treatment follow-up care (11, 32). Another reason for this might be the physiological outcome of weakened immunity in older persons, which increases the severity of COVID-19 risk factors and age-related reasonable comorbidity, both of which have a substantial influence (33–37). As a result, patients become concerned about the outbreak, and medical facilities are compelled to close. However, the findings of a research conducted in Islamabad, Pakistan, contradict our findings (38). This chasm may be produced by the patient's understanding of their ailment as well as the length of their therapy. For example, elderly patients getting long-term care adhere to their treatment plan and timeline. As a result, they have favorable follow-up medical conditions.
In this study, patients who dread COVID-19 were more likely than their counterparts to have poor follow-up conditions of treatment. This was in line with a prior investigation carried out in Addis Ababa (23). The outbreak provided ample evidence that anxiety, the high-risk perception among hypertension patients, and widespread media misinformation all played significant roles (39).
Patients with transportation problems had a greater risk of receiving subpar follow-up treatment than patients without such issues. This was consistent with the Addis Ababa study (23). The conceivable defense may be that there is a government lockdown and that there is a COVID-19 contracting scare. For instance, the government announced the COVID-19 preventive procedure after the pandemic emerged to stop the virus from spreading throughout the nation. The restriction of transportation services was one of the procedures. As a result of the risk posed by COVID-19, transportation services are drastically reduced. It was said that restrictions on transportation for health reasons had existed in the past (40). On the other hand, transportation and mobility have emerged as possible hotspots for the virus' transmission, particularly in areas with dense populations and few resources (41). The need for patient follow-up care may decline as a result. Another reason could be that most people travel from far-flung rural areas to get health care.
In this research, comorbidity increased the likelihood of having subpar follow-up conditions of care. This contradicted the findings of a study conducted in Islamabad, Pakistan (38). This disparity might be attributed to the research participants' differing degrees of knowledge about the risk of getting COVID-19 and its severity. Furthermore, COVID-19 is likely to impact those with underlying medical illnesses more frequently, hasten the course of the disease, and considerably increase mortality across all age groups, particularly those over the age of 60 (42). As a result, patients may become less reluctant to seek medical treatment.
Physical distance increased the likelihood of poor follow-up conditions of care compared to no physical distance. However, there were no research that supported this discovery. This might be due to physical separation, which encourages patients to stay at home, and medical personnel limiting the number of patients admitted to the hospital in order to prevent the coronavirus from spreading.
Another reason might be related to the reduction of essential clinical services, loss of patient follow-up, fragmentation of care, the decline in direct healthcare worker participation, and restrictions on patient access to health facilities because of enforced physical distance (43).
The results of our study have significant implications for practice and policy. Treatments that improve patients' follow-up care circumstances at health institutions must be designed and implemented. We discovered numerous characteristics linked with poor follow-up conditions of care in this study, including age, fear of COVID-19, transportation issues, the existence of comorbidities, and physical distance. As a result, any intervention aimed at enhancing follow-up care conditions might be beneficial. Interventions to improve follow-up conditions of care may include providing free medical care, educational interventions to educate patients about the benefits of regular treatment follow-up, providing awareness on COVID-19, family support, providing better services in healthcare settings, sending reminders to patients via phone calls, SMS, emails, and other means, linking patients to the nearby health facility, and so on (44–48).
To avoid the future advancement of their disease and its consequences, patients must be educated on how to carefully follow the directions offered by healthcare professionals. Because appropriate follow-up conditions of care result in optimal blood pressure control, healthcare practitioners should emphasize the necessity and purpose of attending follow-up appointments during first consultations. This would enable them to undertake required monitoring and medication optimization to provide the best potential treatment outcomes for patients (38). Because inpatient therapy was not possible due to the hazards of COVID-19 transmission, sending reminders through phone call, SMS, and email was an optional treatment approach to ensure continuity of care. Better health care was highly indicated by identifying persons at high risk, such as older patients and those with comorbidity, because this group of patients was extensively attacked by COVID-19 and the severity of the disease itself was worse in this group of patients. This results in better follow-up care. In general, during COVID-19, there is an urgent need for a systematic strategy to improve patient follow-up care, with a mix of a patient-centric approach and any digital and mobile technologies strongly suggested (49). The distribution and cause-effect relationship should be researched further in future studies.
The study's strength is that it involved many centers and included various hypertension individuals with various features. This broadens the applicability of the findings and the representativeness of sample groups. A whole dataset of medical records and in-person interviews were employed as data acquisition strategies to improve data accuracy and completeness. Physical distance was one of the variables that was included to determine how it affected the conditions of care for subsequent visits. However, there are certain limitations to this study. The study's design was its main shortcoming. Due to the retrospective nature of the study, memory bias may result from study participants' inability to recollect their former experiences. We employ a self-reported instrument that might introduce social desirability bias. Additionally, the study excluded adult hypertension patients who were receiving follow-up care at private medical institutions.
This study found that 29% of patients had poor follow-up conditions of treatment. When compared to WHO recommendations, the findings of this study may explain poor follow-up care conditions. To increase patients' follow-up care, evidence-based target interventions should be designed and implemented, taking into account individuals at high risks, such as those over the age of 60, those with comorbidity, and identifying other risk factors. And to stop the situation from getting worse, healthcare providers and other stakeholders should work in collaboration.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Haramaya University, College of Health and Medical Sciences, an Institute of the Health Research Ethics Review Committee (IHRER). The patients/participants provided their written informed consent to participate in this study. All research participants who were 18 years old at the time of the study gave their informed, voluntary, written, and signed permission after being informed of its goals, objectives, advantages, and disadvantages. Those who were unable to read have had their consent read to them and signed with their fingerprint.
AH, NA, ZA, and AS took part in the idea's inception, the proposal's development and revision, the analysis of data, and the writing up of the findings. EY, TB, AA, HA, DD, KN, and LA have participated in the analysis and manuscript write-up. All authors contributed to the article and approved the submitted version.
We appreciate Haramaya University for giving us the chance to perform this study. The West Arsi Health Bureau, all the workers at the medical facilities, and the study participants were also thanked.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1018686/full#supplementary-material
AOR, Adjusted Odds Ratio; BP, Blood Pressure; CI, Confidence Interval; CVD, Cardiovascular Disease; DALY, Global Disability-adjusted Life Years; HCW, Health Care Worker; LMCIs, Low and Middle-income Countries; NCD, Non-communicable Disease; SSA, Sab-Sahara Africa; WHO, World Health Organizations.
1. Dong X, Cao YY, Lu XX, Zhang JJ, Du H, Yan YQ, et al. Eleven faces of coronavirus disease 2019. Allergy. (2020) 75:1699–709. doi: 10.1111/all.14289
3. Palmer K, Monaco A, Kivipelto M, Onder G, Maggi S, Michel JP, et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy aging. Aging Clin Exp Res. (2020) 32:1189–94. doi: 10.1007/s40520-020-01601-4
4. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA. (2017) 317:165–82. doi: 10.1001/jama.2016.19043
5. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2224–60. doi: 10.1016/S0140-6736(12)61766-8
6. Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Laurence C, Adebamowo C, Ajayi I, et al. The burden of hypertension in sub-Saharan Africa: a four-country cross-sectional study. BMC Public Health. (2015) 15:1–8. doi: 10.1186/s12889-015-2546-z
7. WHO. A Global Brief On Hypertension: Silent killer, A Global Public Health Crisis. Geneva: World Health Organization (WHO) (2013).
8. Fraser-Bell S, Symes R, Vaze A. Hypertensive eye disease: a review. Clin Experiment Ophthalmol. (2017) 45:45–53. doi: 10.1111/ceo.12905
9. Akinniyi AA, Olamide OO. Missed medical appointment among hypertensive and diabetic outpatients in a tertiary healthcare facility in Ibadan, Nigeria. Trop J Pharm Res. (2017) 16:1417–24. doi: 10.4314/tjpr.v16i6.28
10. Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, et al. Hypertension Canada's 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. (2018) 34:506–25. doi: 10.1016/j.cjca.2018.02.022
11. Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, et al. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr. (2020) 14:965–7. doi: 10.1016/j.dsx.2020.06.042
12. Dawes M, Beerman S, Gelfer M, Hobson B, Khan N, Kuyper L, et al. The challenges of measuring blood pressure during COVID-19: how to integrate and support home blood pressure measurements. Can Fam Physician. (2021) 67:112–3. doi: 10.46747/cfp.6702112
14. Skeete J, Connell K, Ordunez P, DiPette DJ. Approaches to the management of hypertension in resource-limited settings: strategies to overcome the hypertension crisis in the post-COVID Era. Integr Blood Press Control. (2020) 13:125. doi: 10.2147/IBPC.S261031
15. Kraef C, Juma P, Kallestrup P, Mucumbitsi J, Ramaiya K, Yonga G. The COVID-19 pandemic and non-communicable diseases—a wake-up call for primary health care system strengthening in sub-Saharan Africa. J Prim Care Community Health. (2020) 11:948. doi: 10.1177/2150132720946948
16. Osibogun A, Abayomi A, Kanma-Okafor O, Idris J, Bowale A, Wright O, et al. Morbidity and Mortality Outcomes of COVID-19 Patients With and Without Hypertension in Lagos, Nigeria: A Retrospective Cohort Study (2020).
17. Seaton RA, Yinka-Ogunleye AF, Basu D, Mueller D, Sneddon J, Yinka-Ogunleye AF, et al. Response to the novel coronavirus (COVID-19) pandemic across Africa: successes, challenges, and implications for the future. Front Pharmacol. (2020) 11:1205. doi: 10.3389/fphar.2020.01205
19. Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. (2020) 146:110–8. doi: 10.1016/j.jaci.2020.04.006
20. Abegaz TM AOBhagavathula AS, et al. Magnitude and determinants of uncontrolled blood pressure among hypertensive patients in Ethiopia: a hospital-based observational study. Pharm Pract. (2018) 16:1173. doi: 10.18549/PharmPract.2018.02.1173
21. Yazzie D, Workineh S, Alebachew M, Beyene Berha A. Assessment of blood pressure control among hypertensive patients in Zewditu memorial hospital, Addis Ababa, Ethiopia: a cross-sectional study. J Bioanal Biomed. (2018) 10:80–7. doi: 10.4172/1948-593X.1000210
22. Sheppard JP, Nicholson BD, Lee J, McGagh D, Sherlock J, Koshiaris C, et al. Association between blood pressure control and coronavirus disease 2019 outcomes in symptomatic patients with hypertension. Hypertension. (2021) 77:846–55. doi: 10.1161/HYPERTENSIONAHA.120.16472
23. Aklilu TM, Abebe W, Worku A, Tadele H, Haile T, Shimelis D, et al. The Impact of COVID-19 on Care Seeking Behavior of Patients at Tertiary Care Follow-Up Clinics: A Cross-Sectional Telephone Survey. Addis Ababa, Ethiopia: medRxiv (2020). doi: 10.1101/2020.11.25.20236224
24. Mills TK, Peacock E, Chen J, Zimmerman A, He H, Cyprian A, et al. Experiences and beliefs of low-income patients with hypertension in louisiana and mississippi during the COVID-19 pandemic. J Am Heart Assoc. (2021) 10:e018510. doi: 10.1161/JAHA.120.018510
25. Nadar K S, Tayebjee MH, Stowasser M, Byrd JB. Managing hypertension during the COVID-19 pandemic. J Hum Hypertens. (2020) 34:415–7. doi: 10.1038/s41371-020-0356-y
26. WAZHB. Central Statistical Agency Population Projection of West Arsi Zonal Health Bureau (2017).
27. Samara B, Albawwab A. Adherence to hypertension medicine, patient follow-up and blood pressure monitoring in Jordanian hypertensive patients during the COVID-19 pandemic. Res Medicine Med Sci. (2020) 1:414. doi: 10.5281/zenodo.4420317
28. Nwabuo C, Dy SM, Weeks K, Young JH. Factors associated with appointment non-adherence among African-Americans with severe, poorly controlled hypertension. PLoS ONE. (2014) 9:e103090. doi: 10.1371/journal.pone.0103090
29. Ogedegbe G, Schoenthaler A, Fernandez S. Appointment-keeping behavior are not related to medication adherence in hypertensive African Americans. J Gen Intern Med. (2007) 22:1176–9. doi: 10.1007/s11606-007-0244-y
30. Evidation Health 2020. COVID-19 Pulse: Delivering Weekly Insights on the Pandemic from a 150,000+ Person Connected Cohort. Available online at: https://evidation.com/news/covid-19-pulse-first-data-evidation (accessed March 31, 2020).
31. Animut Y, Assefa AT, Lemma DG. Blood pressure control status and associated factors among adult hypertensive patients on outpatient follow-up at University of Gondar Referral Hospital, Northwest Ethiopia: a retrospective follow-up study. Integr Blood Press Control. (2018) 11:37–46. doi: 10.2147/IBPC.S150628
32. Ayele TA, Shibru H, Sisay M, Melese T, Fentie M, Azale T, et al. The effect of COVID-19 on poor treatment control among ambulatory Hypertensive and/or Diabetic patients in Northwest Ethiopia. PLoS ONE. (2022) 17:e0266421. doi: 10.1371/journal.pone.0266421
33. Jones TC, Biele G, Mühlemann B, Veith T, Schneider J, Beheim-Schwarzbach J, et al. Estimating infectiousness throughout SARS-CoV-2 infection course. Science. (2021) 373:eabi5273. doi: 10.1126/science.abi5273
34. Lee I, Hu L, Chen Y, Huang C, Hsueh R. Are children less susceptible to Covid-19? J. Microbiol Immunol Infect. (2020) 53:371–2. doi: 10.1016/j.jmii.2020.02.011
35. Liu K, Chen Y, Lin R, Han K. Clinical features of Covid-19 in elderly patients: a comparison with young and middle-aged patients. J Infect. (2020) 80:e14–8. doi: 10.1016/j.jinf.2020.03.005
36. Wang J, Zhu X, Xu Z, Yang G, Mao G, Jia Y, et al. Clinical and ct findings of covid-19: differences among three age groups. BMC Infect Dis. (2020) 20:1–11. doi: 10.1186/s12879-020-05154-9
37. Zhao M, Wang M, Zhang J, Gu J, Zhang P, Xu Y, et al. Comparison of clinical characteristics and outcomes of patients with coronavirus disease by 2019 at different ages. Aging. (2020) 12:10070. doi: 10.18632/aging.103298
38. Mahmood S, Jalal Z, Hadi MA, Shah KU. Association between attendance at outpatient follow-up appointments and blood pressure control among patients with hypertension. BMC. (2020) 20:458. doi: 10.1186/s12872-020-01741-5
39. Gaborone E, Oyeyemi SO, Wynn R. COVID-19-related misinformation on social media: a systematic review. Bull World Health Organ. (2021) 99:455. doi: 10.2471/BLT.20.276782
41. Liu L, Miller HJ, Scheff J. The impacts of the COVID-19 pandemic on public transit demand in the United States. PLoS ONE. (2020) 15:e0242476. doi: 10.1371/journal.pone.0242476
42. Adekunle S, Chuku O, Aleksandra M, Risha P, Kokab Y, Priyank D, et al. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. (2020) 2:1069–76. doi: 10.1007/s42399-020-00363-4
43. Vishala P, Keating JA, Carayon P, Safdar N. Physical distancing for care delivery in health care settings: Considerations and consequences. Am J Infect Control. (2021) 49: 1085–8. doi: 10.1016/j.ajic.2020.12.014
44. Reed M, Huang J, Graetz I, Muelly E, Millman A, Lee C. Treatment and follow-up care associated with patient-scheduled primary care telemedicine and in-person visits in a large integrated health system. JAMA Netw Open. (2021) 4:e2132793 doi: 10.1001/jamanetworkopen.2021.32793
45. Levin RP. How to manage the behavior of patients who disregard scheduled appointment times. J Am Dent Assoc. (2012) 143:172–3. doi: 10.14219/jada.archive.2012.0129
46. Lin H, Wu X. Intervention strategies for improving patient adherence to follow-up in the era of mobile information technology: a systematic review and meta-analysis. PLoS ONE. (2014) 9:e104266. doi: 10.1371/journal.pone.0104266
47. Vartanian KB, Holtorf M, Cox EJ, Diaz G, Khurana H, Schlegel S, et al. Patient experience and health care utilization for a COVID-19 telemedicine home monitoring program offered in English and Spanish. PLoS ONE. (2022) 17:e0270754. doi: 10.1371/journal.pone.0270754
48. Prasad S, Anand R. Use of mobile telephone short message service as a reminder: the effect on patient attendance. Int Dent J. (2012) 62:21–6. doi: 10.1111/j.1875-595X.2011.00081.x
Keywords: attendance and follow-up, hypertension, COVID-19, associated factors, Ethiopia
Citation: Hiko A, Assefa N, Ataro Z, Sertsu A, Yadeta E, Balcha T, Amano A, Asfaw H, Dechasa DB, Nigussie K and Abdisa L (2022) Follow-up conditions of care and associated factors among adult hypertensive patients during COVID-19 at West Arsi public health facilities, Southeastern Ethiopia: A multi-center cross-sectional study. Front. Public Health 10:1018686. doi: 10.3389/fpubh.2022.1018686
Received: 13 August 2022; Accepted: 26 October 2022;
Published: 16 November 2022.
Edited by:
Claire Collins, Irish College of General Practitioners, IrelandReviewed by:
Marilena Anastasaki, University of Crete, GreeceCopyright © 2022 Hiko, Assefa, Ataro, Sertsu, Yadeta, Balcha, Amano, Asfaw, Dechasa, Nigussie and Abdisa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmed Hiko, YWhtZWRoaWtvMTQyQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.