- 1Anesthesia Technology Department, Prince Sultan Military College of Health Sciences, Dhahran, Saudi Arabia
- 2College of Applied Medical Sciences, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
- 3King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia
- 4College of Applied Sciences, AlMaarefa University, Riyadh, Saudi Arabia
- 5Prince Mohammed Bin Abdulaziz Hospital, Riyadh, Saudi Arabia
- 6Armed Forces Hospital Southern Region, Khamis Mushayt, Saudi Arabia
- 7King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia
- 8Prince Sultan Military Medical City, Riyadh, Saudi Arabia
- 9Department of Radiology, King Saud Medical City, Riyadh, Saudi Arabia
Background: Evidence-based practice (EBP) plays a crucial role in improving the quality of healthcare services by ensuring the delivery of the highest and safest level of patient care since EBP helps in justifying treatment choices to patients. Studies that examine the levels of EBP knowledge, attitudes toward EBP, and use of the use of EBP within anesthetic teams' practice are lacking, hence it is necessary to explore this.
Aim: To evaluate anesthesia teams' levels of knowledge, attitude toward and use of the evidence-based practice in a local hospital in Saudi Arabia.
Method: In one hospital, a cross-sectional survey was conducted using a convenience sampling technique using a validated questionnaire instrument called the Evidence-Based Practice EBP Questionnaire. The questionnaire was distributed through an online method to 173 participants. Descriptive and inferential statistics Tests were utilized to analyse the retrieved data using the SPSS program.
Results: One hundred and forty questionnaires were completed and returned, yielding a response rate of 80.9%. Overall, anesthesia teams showed a high positive attitude toward EBP but low levels of knowledge and use of EBP. Participants with higher levels of education and/or work experience exhibited significantly higher levels of knowledge and use of EBP than those who had lower education levels and/or work experience. Also, higher levels of education and/or work experience exhibited a significant positive association toward a higher level of knowledge and use of EBP. However, attitude levels toward EBP did not exhibit either significant or associated. Physicians showed significantly higher knowledge and use of EBP than non-physicians. Lack of knowledge and lack of time due to workload were the leading barriers encountered by anesthesia teams ATs.
Conclusion: Education level, work experience and job position affect the knowledge, attitude, and use of EBP. Continuous education and minimizing barriers are recommended to enhance the knowledge, attitude, and use of EBP among anesthesia teams in Saudi Arabia.
Background
In the past, Healthcare Professionals (HCP) based their medical judgments on daily practice, expert sources, or textbooks, and not on scientific evidence-based studies (1). However, in the early 21st century, the picture changed totally due to the huge increase in the quantity of clinical research evidence available (2). Annually about 2.5 million papers are published (3). However, the increase in the quantity of clinical research evidence does not automatically translate into improved patient treatment and care (4). Moreover, rapid changes in the methods of treatments and technologies within the last two decades have made it difficult for HCP to ensure that the available evidence has sufficiently high validity to be implemented into their clinical practice (5). Therefore, EBP exists to play the main role in providing the practitioner with the essential skills to be able to distinguish whether the available evidence is trustworthy (6).
Evidence-based practice is outlined as the process of decision-making by integrating the finest scientific research evidence with clinical experience and the patient's preferences and values (7). The principle of EBP comprises five phases: it starts with formulating a clinical question, searching for the best evidence that answers the question formulated, critically appraising the evidence retrieved to assess its validity and reliability, and implementing the findings with HCPs' expertise and patients' preferences, and finally, evaluating the entire process with the findings of patients' outcomes (8). EBP aims to deliver the most efficient healthcare service where HCPs' decisions are made according to the evaluation of the best evidence rather than depending on traditional treatments (9). Hence, EBP is considered crucial to delivering safe practice with high-quality care to enhance patient outcomes (10).
In the past three decades, EBP has become a global concern for HCPs and administrative staff as well as researchers and policymakers, since it is found to be effective in reducing costs without affecting the quality of care (11). Most healthcare organizations globally have found that EBP offers remarkable outcomes in terms of reducing mortality, morbidity, and medical errors while improving cost-effectiveness (12). Healthcare institutions globally could reduce their expenses by 30% if patients received evidence-based care (13). The World Health Organization (WHO) revealed that employing EBP in daily practice can save a minimum of £4.5 million annually in each hospital (14). In the United Kingdom (UK), EBP reduced around 63% of the total cost of a surgical procedure for carpal tunnel syndrome, which is among the most common surgical procedures performed (15), while in the US, EBP has increased the recovery rate by 30% and saved about 35% of the total cost of treatment for oncology patients suffering from lung cancer, which is the second most common disease diagnosed in the United State (US) (16–18). Accordingly, both national and international healthcare organizations have highlighted the significance of evidence-based care to ensure that patients receive appropriate, high-quality care (19).
Unfortunately, although EBP has proved its effectiveness in different clinical organizations, HCPs' uptake is below optimum levels (14). The gap between the amount of research evidence that exists and the application of such evidence in clinical practice is huge (19). In anesthesia, 30% of clinical decisions taken by ATs have been found to be either unnecessary or potentially harmful to patients (20). For instance, 40% of anesthetists are found to perform the cricoid pressure technique while intubating patients undergoing either emergency or cesarean section procedures, although this technique has been shown to cause esophageal rupture (21). Also, around 80% of medication error events are avoidable if the anesthesia practitioner applied actual evidence-based care (22).
Practitioners have reported encountering several obstacles with the use of EBP in clinical practice (23). Many studies have found that insufficient knowledge about EBP, lack of time due to workload, level of academic qualifications and level of work experience were the main barriers to the use of EBP during clinical practice (24–28). Healthcare organizations also found that HCPs' attitude toward EBP plays a fundamental role in the use of EBP principles in clinical practice (29). This is critical, since applying evidence to clinical practice can take a decade, which could delay the provision of a high-quality healthcare service (30).
To date, limited studies have explored the knowledge, attitudes, and use of EBP among Anesthesia Teams (AT) worldwide. Unfortunately, no studies have investigated these aspects among ATs in Saudi Arabia (SA). Thus, the presence of this gap highlights the need to establish at least a baseline measurement to provide a clear picture to establish strategies to address any future problems that may appear. The study findings would thus underline the knowledge, attitude, and use of EBP among ATs in their respective practices. This could also lead to further research into potential methods for implementing EBP in SA. Hence, the current study aimed to explore the level of knowledge, attitude, and use of evidence-based practice among anesthesia teams in a single hospital in SA. Also, an assessment was performed to investigate the contributing factors that affect the level of knowledge, attitude, and use of EBP within anesthesia teams' professional practice.
Methods
Study design
This was a descriptive quantitative cross-sectional survey design. The questionnaire link was sent to the participants' emails via an accredited and secured web page platform (SurveyMonkey) to anesthesia staff.
Target population
The target population was 173 (all anaesthesiologists and anesthesia technologists/technicians who are officially registered in the Saudi Commission for Health Specialities and currently working in Prince Sultan Military Medical City Riyadh Saudi Arabia). A gatekeeper who has access to the contacts of the registered anesthesia staff was utilized to identify the eligible population. Since the data collection period was for 4 weeks between January and February 2020. An auto-reminder was sent asking participants to complete the questionnaire 2 weeks after sending the first link to improve the response rate.
Sampling
This study used a non-probability convenience sampling method since it reaches all eligible participants who are available and accessible to participants. Importantly, a power calculation was utilized to calculate the needed sample size, to ensure that the sample of the current study would be representative of all anesthesia practitioners in the targeted hospital. The G*power programme (version 3.1.9.2) was utilized with a significant value of p ≤ 0.05, power of 0.95 and medium effect size of 0.3. This calculation revealed that a sample size of 138 participants was required.
Data collection
Data were collected by using the Evidence-Based Practice Questionnaire (EBPQ) tool which is considered a valid and reliable self-reported questionnaire (31). The EBPQ comprises closed-ended questions within three subscales: knowledge about, attitude toward, and use of EBP.
Each item of the EBPQ takes the form of a seven-point Likert scale ranging from (1 to 7), and the participants were asked to choose where they found themselves between these seven points. For the knowledge subscale, a score of (1) indicated “Poor,” whereas a score of (7) indicated “Best,” while for the use subscale, a score of (1) indicated “Never” whereas a score of (7) indicated “Frequently.”
However, in the attitude subscale, the participants were asked to indicate where they found themselves between two opposite statements (for instance, “I resent having my clinical practice questioned” to “I welcome questions on my practice”): a score of number (1) means the statement is negative and a score of (7) means the statement is positive. The respondents were asked to indicate their level for each subscale, where (1) indicated the lowest score and (7) indicated the highest. Subsequently, the average score was calculated to determine the level of each subscale. Higher scores indicated higher use of knowledge about and a more positive attitude toward EBP.
In the fourth section, six demographic questions were added to the questionnaire such as gender, age, specialization, job position, academic qualifications, and work experience. Therefore, the questionnaire had four sections with a total of 30 questions. A pilot study was conducted with eight qualified anesthesia professionals (four anaesthesiologists and four technologists) who are not from the targeted population. Piloting was performed to ensure face validity prior to sending the questionnaire to the target population.
Data analysis
Both descriptive and inferential statistical approaches were utilized to analyse the data collected for this study. These statistical methods were applied using the Statistical Package for Social Sciences (SPSS) program (version 25). Frequency, percentage, mean, and Standard Deviation (SD) were used for the descriptive statistics, and these were presented in tables and charts to simplify explaining the participants' data. Normality test was used, and the data showed that the data were normally distributed; therefore, parametric statistical tests were used for the study's results. Thereafter, inferential statistical tests were used. Both t-test and one-way Analysis of Variance (ANOVA) were utilized. Pearson's Correlation test was used to examine whether associations existed between the participants' responses and the variables.
In this study, the cut-off level was determined as follows: mean scores from 1 to 3 were considered low, whereas a score of 4 was considered moderate and 5–7 was considered high.
Ethical considerations
Ethical approval was obtained from the targeted hospital, in SA, giving the researcher permission to conduct the study in the anesthesia department. Participants have received an information sheet that contains the aim and objectives of the study. Implied consent was the method for obtaining informed consent for this study, and this was clearly stated and explained to the participants in the information sheet. When the participant presses the “submit” button and the questionnaire has been sent, this acts as informed consent. Also, no names or numbers were requested in the questionnaire to ensure the anonymity and confidentiality of the participants.
Ethical approval project code: 1233, 31 Jul Series 2019.
Results
Response rate
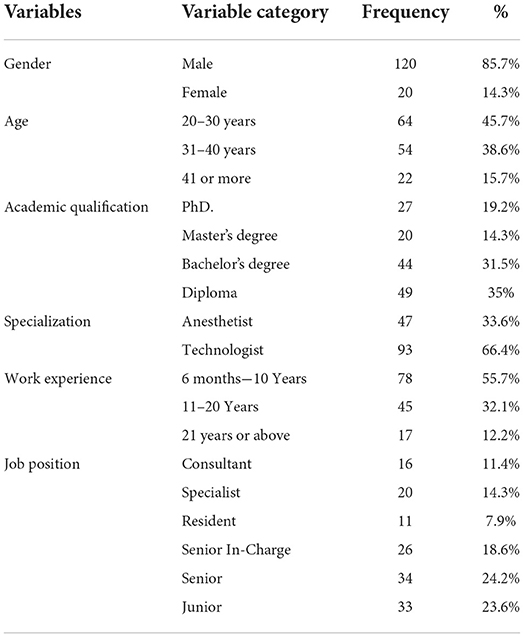
Out of 173 questionnaires sent, a total of 140 questionnaires were completed presenting a response rate of 80.9%. Of 140 questionnaires, 64 (45.7%) of participants were between 20 and 30 years old, 54 (38.6%) were aged between 31 and 40 years, and 22 (15.7%) were aged 41 or above. The majority of respondents 49 (35%) held diplomas, while 44 (31.5%) held bachelor's degrees, 27 (19.2%) held PhD degrees and finally, 20 (14.3%) held master's degrees. Regarding specialization, most of the respondents were technologists 93 (66.4%), while 47 (33.6%) were anesthetists (Table 1).
Furthermore, more than half of the respondents 78 (55.7%) had between 6 months and 10 years of experience, while 45 (32.1%) had between 11 and 20 years, and only 17 (12.2%) had 21 or more years of experience. As for the job position variable, the majority of participants were in senior positions 34 (24.2%), followed by 33 (23.6%) who were in junior positions, while 26 (18.6%) were senior in charge, 20 (14.3%) were specialists, 16 (11.4%) were consultants and 11 (7.9%) were residents. The majority of respondents were male (85.7%), while 20 (14.2%) were female, and PhD and master's holders were all Anesthetists (Table 1).
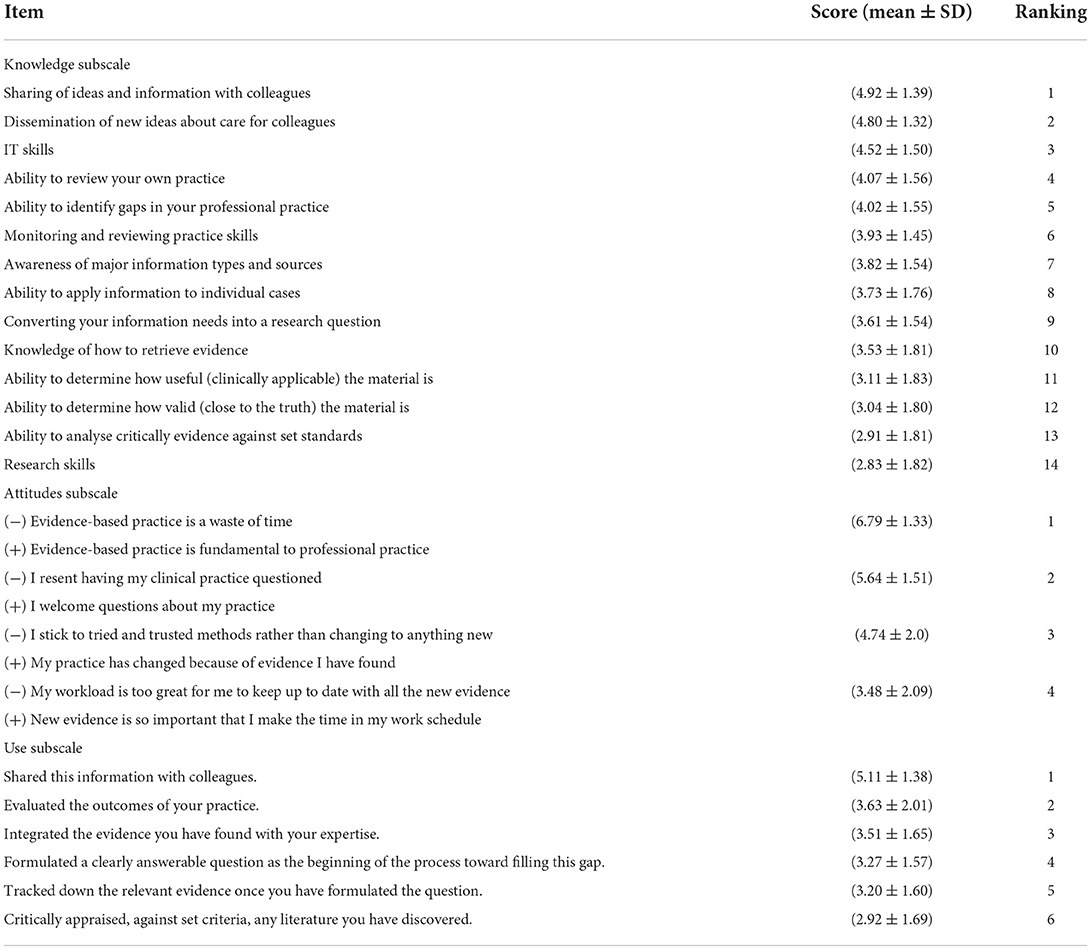
Knowledge of EBP
Overall, ATs revealed a low level of knowledge about EBP, with a mean score of (3.77) out of 7. In this context, participants show a moderate level of knowledge toward sharing and disseminating new ideas about care with colleagues, with a mean score of (4.92; 4.52) respectively. However, ATs' research skills and ability to critically analyse the evidence against set standards were the lowest among the questionnaire items, with an average score of (2.83; 2.91) respectively (Table 2).
Attitude toward EBP
ATs exhibited a high positive attitude toward EBP, with a mean score of (5.16) out of 7. The participants show a high positive attitude toward the importance of EBP to clinical practice, with a mean score of (6.79). However, ATs show a negative attitude level in “workload is too great for me to keep up to date with new evidence,” with a mean score of (3.48) (Table 2).
Use of EBP
ATs exhibited a low level of use of EBP, with a mean score of (3.60) out of 7. In this context, ATs show a high use level in sharing information with colleagues, with a mean score of (5.11). However, ATs show poorness in critically appraise literature, with a mean score of (2.92) (Table 2).
Statistically significant results
Within demographic characteristics, anesthetists have higher levels of knowledge, attitude, and use of EBP than technologists. However, only the knowledge and use levels reveal statistically significant differences between anesthetists and technologists (both at p = 0.001). For attitude level, no statistically significant results were found between anesthetists and technologists (p = 0.092). Likewise, the results show that levels of knowledge and use of EBP significantly increased as work experience increased among ATs (both at p = 0.001). However, although the attitude level increased with work experience among ATs, the result did not reveal a statistically significant difference (p = 0.249). This indicates that there is convergence in ATs' level of attitude toward EBP depending on the work experience variable. Regarding academic qualifications, the ATs' levels of knowledge, attitude, and use of EBP increased as academic qualifications increased. However, only knowledge and use levels exhibited statistically significant differences (both at p = 0.001). Within the results, the study results show that levels of knowledge, attitude and use of EBP increased as job positions increased. Further, the results show that there were statistically significant differences between levels of knowledge and use among ATs (both at p = 0.001). However, for attitude level, there were no significant difference p = 0.221 (Table 3).
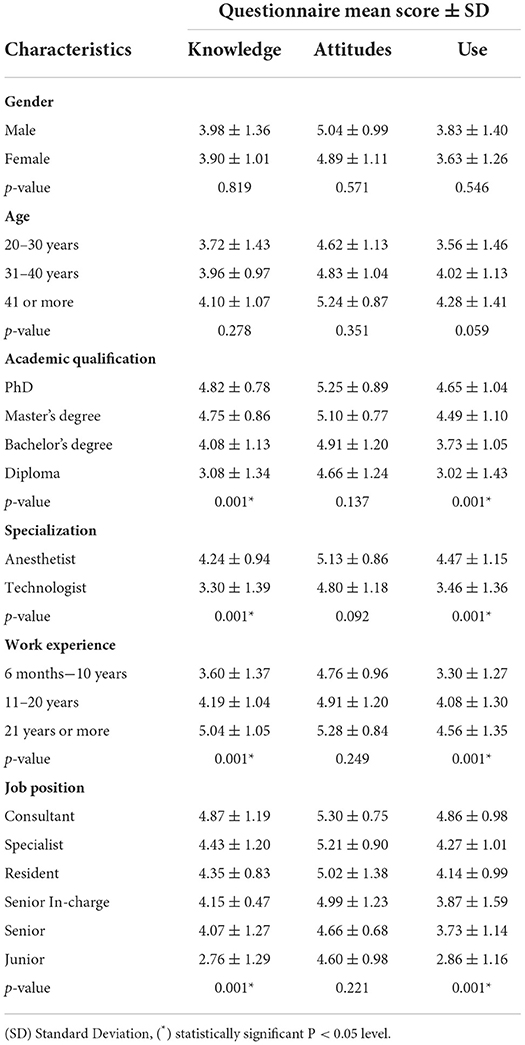
Table 3. Statistical differences and correlations for knowledge, attitude, and practice or use levels according to demographic characteristics (n = 140).
Associations according to demographic characteristics
Results reveal that there were no associations between attitude levels and any of the demographic variables. However, there were positive, statistically significant associations between the level of knowledge about EBP among ATs and academic qualification (R = 0.503) and work experience (R = 0.363). These findings indicate that ATs' knowledge increased with the increment of academic qualification and/or work experience. Also, there were positive, statistically significant associations between the levels of use of EBP among ATs and academic qualifications (R = 0.483), work experience (R = 0.199) and job position (R = 0.409), indicating that ATs' use of EBP increases in line with each of these variables. Regarding gender, age and specialization, the results show no significant association (Table 4).
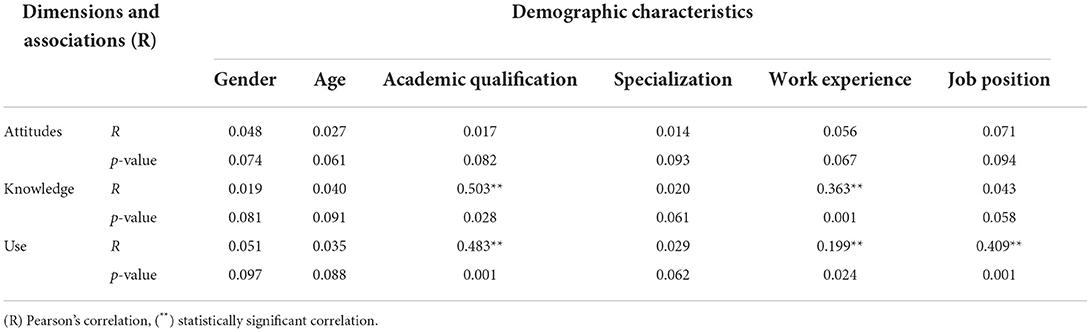
Table 4. Associations of knowledge, attitude and use levels according to demographic characteristics (n = 140).
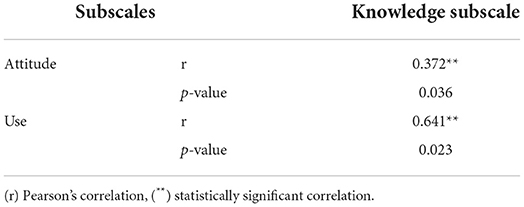
Association between the attitude and use subscales toward the knowledge subscale
Results exhibit that there was a significant positive association between the levels of attitude and knowledge toward EBP among ATs (R = 0.372, p = 0.036), which indicates that the ATs' attitude toward EBP increased with the increment of knowledge level. Similarly, there was a significant positive association between the level of use of EBP among ATs and the level of knowledge (R = 0.641, p = 0.023), showing that the ATs' use of EBP increased with the increment of knowledge level (Table 5).
Discussion
The study aimed to investigate the level of ATs' knowledge, attitude, and use of EBP in a large local hospital in SA. The current study revealed that amongst the three subscales, attitude achieved the highest score, followed by knowledge, while the lowest score was for the use of EBP. The current study's findings suggest that ATs overall have a low level of knowledge about EBP. This result was similar to the findings of previous studies (24, 26, 32, 33). However, it contradicts the findings of previous studies (25, 34, 35).
Within the knowledge subscale, the highest items scored by ATs related to sharing and dissemination of evidence to colleagues, whereas the lowest scoring items were in “research skills,” “ability to critically appraise literature,” and “ability to determine how valid the material is” and “ability to determine how useful the material is.” This is interesting since the highest and lowest scoring items were also similarly ranked in previous studies (24–26). The similarities in the results reported by the latter studies indicate that the lack of knowledge could be attributed to the weakness of the teaching approaches in terms of providing sufficient teaching modules to explain the principles of EBP during academic studies. This was clear in the current study's significant difference in the level of knowledge as academic qualifications increased. In this study, participants with diplomas showed the lowest score, while those with PhD degrees had the highest level of knowledge about EBP. This could be because the diploma curriculum for anesthesia practitioners in SA does not contain any research modules to teach students how to read and evaluate research findings (36). The current study also found a significant positive association between level of knowledge and academic qualification, meaning that higher qualifications were related to higher knowledge. This is congruent with the previous studies (33, 35). Importantly, although the latter two studies reported different overall results regarding the level of knowledge about EBP, these studies showed similar results regarding the association between qualifications and level of knowledge. The findings of this study also revealed that work experience exhibited a significant positive association with a high level of knowledge. The increase was comparable with the findings of previous studies (24–26, 32).
Attitude toward EBP was highly positive amongst ATs in this study. This was comparable to previous studies (37–40). This highly positive attitude could be because the targeted hospital undergoes annual evaluation by the Saudi Central Board for Accreditation of Healthcare Institutions (CBAHI) and the Joint Commission (JCI), and these organizations play a main role in enhancing the use of EBP. This high positive attitude indicates that ATs have good use of- the significance of EBP in delivering the highest quality of healthcare. On the other hand, the lowest attitude level reported by ATs was toward the statement “My workload is too great for me to keep up to date with all the new evidence,” which could be considered as a barrier not only to the level of attitude but also toward the use of EBP at the bedside. The presence of this barrier is critical, since attitudinal barriers toward EBP can be more difficult to overcome than knowledge barriers, and thus could affect the application of retrieved evidence in actual practice (41). The current study found a statistically significant positive association between the attitude and knowledge subscales, meaning that attitude level increases as knowledge level increases.
Results from the current study revealed that ATs have low levels of use of EBP. This finding concurred with previous studies (28, 42, 43). However, it contrasted with previous studies (26, 27). This might be because the former three studies and the present study reported a lack of knowledge about EBP. In this study, a significant positive association between the use and knowledge subscales, meaning that level of use of EBP increases with the increase of knowledge. This is interesting since this can be the main influence toward the low use level. Additionally, the current study's results found that the use of EBP among ATs showed a significant increase as their academic qualification increased.
The current study also found that work experience influences the level of use of EBP. The use of EBP increased significantly with higher work experience. This was comparable to the previous studies (28, 42, 43). However, it contradicted the previous studies (26, 27). It could be because HCPs with more than 10 years of experience become more confident in using EBP in clinical practice, whereas those with < 10 years of experience have limited practical knowledge (44). Moreover, the current study found a significant increase in the practice of EBP as the seniority of job positions increases. This result was comparable with the findings of previous studies (28, 43). In fact, the tasks, and duties of anesthesia practitioners in senior positions tend to be more administrative than clinical, allowing more time to search for and evaluate evidence (45). In contrast, residents and juniors have huge workloads, such as covering on-calls duties, attending cardiac arrest events, and visiting patients before and after surgery, which makes the use of EBP in clinical practice difficult (46).
Limitations
Limitations of the current study could be attributed to the fact that the data collection instrument utilized in the study was a self-reported questionnaire, which might be subject to self-reporting bias. Also, conducting a cross-sectional study in a single hospital with a relatively small sample size limits the ability to generalize the results to all ATs in SA.
Conclusion
This study was conducted to investigate ATs' levels of knowledge, attitude, and use of EBP in a single hospital in SA. Generally, the findings show that ATs had poor knowledge and use of EBP. However, ATs showed high positive attitudes toward EBP. Also, the study revealed that certain demographic characteristics influenced the overall results within the three subscales levels. Anesthesia practitioners' academic qualifications, Job positions, and work experience revealed a significant result with a positive correlation higher level of knowledge and use of EBP. In this study, lack of knowledge about EBP principles and lack of time due to workload were reported by ATs as the main barriers that affected their attitude and use levels toward EBP. Therefore, providing training and workshops about research skills, critical appraisal skills and research utilization to all ATs should be implemented, as this would reinforce their knowledge, which in turn would reflect on the high use of EBP in clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Prince Sultan Military Medical City Scientific Research Center. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Acknowledgments
Special appreciation and recognition to the participants who joined in the study and delivered their data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Angelis RM, Avezum Júnior Á, Cavalcanti AB, Carvalho RT. Evidence-based anesthesiology: what is it and how to practice it. Rev Bras Anestesiol. (2004) 54:582–94. doi: 10.1590/S0034-70942004000400014
2. Bhatt A. Evolution of clinical research: a history before and beyond James Lind. Perspect Clin Res. (2010) 1:6.
3. International International Association of Scientific Technical Medical Publishers. An Overview of Scientific and Scholarly Journal Publishing. (2015). Available online at: https://www.stm-assoc.org/2015_02_20_STM_Report_2015.pdf (accessed October, 2022).
4. Rangachari P, Rissing P, Rethemeyer K. Awareness of evidence-based practices alone does not translate to implementation: insights from implementation research. Qual Manag Healthcare. (2013) 22:117–25. doi: 10.1097/QMH.0b013e31828bc21d
5. Greig PR, Higham HE, Darbyshire JL, Vincent C. Go/no-go decision in anaesthesia: wide variation in risk tolerance amongst anaesthetists. Br J Anaesth. (2017) 118:740–6. doi: 10.1093/bja/aew444
6. The Information Standard. Finding the Evidence, A Key Step in the Information Production Process. (2013). Available online at: https://www.england.nhs.uk/tis/wp-content/uploads/sites/17/2014/09/tis-guide-finding-theevidence-07nov.pdf (accessed October, 2022).
7. Tilson JK, Kaplan SL, Harris JL, Hutchinson A, Ilic D, Niederman R, et al. Sicily statement on classification and development of evidence-based practice learning assessment tools. BMC Med Educ. (2011) 11:1–0. doi: 10.1186/1472-6920-11-78
9. Facilitating Evidence-Based Practice in Nursing and Midwifery in the WHO European Region. Available online at: http://www.euro.who.int/__data/assets/pdf_file/0017/348020/WH06_EBP_report_complete.pdf?ua=1 (accessed October, 2022).
10. Lehane E, Leahy-Warren P, O'Riordan C, Savage E, Drennan J, O'Tuathaigh C, et al. Evidence-based practice education for healthcare professions: an expert view. BMJ Evid Based Med. (2019) 24:103–8. doi: 10.1136/bmjebm-2018-111019
11. Mathieson A, Grande G, Luker K. Strategies, facilitators and barriers to implementation of evidence-based practice in community nursing: a systematic mixed-studies review and qualitative synthesis. Primary Health Care Res Dev. (2019) 20:e6. doi: 10.1017/S1463423618000488
12. Department of Health. The Evidence Base of the Public Health Contribution of Nurses and Midwives. (2017). Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/208842/Evidence.pdf (accessed October, 2022).
13. Melnyk BM, Gallagher-Ford L, Long LE, Fineout-Overholt E. The establishment of evidence-based practice competencies for practicing registered nurses and advanced practice nurses in real-world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews Evid Based Nurs. (2014) 11:5–15. doi: 10.1111/wvn.12021
14. World Health Organization. Facilitating Evidence-Based Practice in Nursing and Midwifery in the WHO European region. (2017). Available online at: http://www.euro.who.int/__data/assets/pdf_file/0017/348020/WH06_EBP_report_complete.pdf?ua=1 (accessed October, 2022).
15. Williamson M, Sehjal R, Jones M, James C, Smith A. How critical cost analysis can save money in today's NHS: a review of carpal tunnel surgery in a district general hospital. BMJ Open Quality. (2018) 7:e000115. doi: 10.1136/bmjoq-2017-000115
16. Neubauer MA, Hoverman JR, Kolodziej M, Reisman L, Gruschkus SK, Hoang S, et al. Cost effectiveness of evidence-based treatment guidelines for the treatment of non–small-cell lung cancer in the community setting. J Oncol Pract. (2010) 6:12–8. doi: 10.1200/JOP.091058
17. American Cancer Society. Cancer Facts Figures. (2018). Available online at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf
18. Royal College of Midwives. Evidence-Based Midwifery. (2015). Available online at: https://www.rcm.org.uk/media/2778/evidence-based-midwifery-september-2015.pdf
19. Dimidjian S. Evidence-Based Practice in Action: Bridging Clinical Science and Intervention. New York, NY: Guilford Publications. (2019).
20. Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. (2012) 7:1–7. doi: 10.1186/1748-5908-7-50
21. Difficult Airway Society. Guidelines for the Management of Unanticipated Difficult Intubation in Adults: Not Just Another Algorithm. (2015). Available online at: https://bjanaesthesia.org/article/S0007-0912(17)31426-5/pdf (accessed October, 2022).
22. Nanji KC, Patel A, Shaikh S, Seger DL, Bates DW. Evaluation of perioperative medication errors and adverse drug events. Anesthesiology. (2016) 124:25–34. doi: 10.1097/ALN.0000000000000904
23. Mahmoud MH, Abdelrasol ZF. Obstacles in employing evidence-based practice by nurses in their clinical settings: a descriptive study. Front Nurs. (2019) 6:123–33. doi: 10.2478/FON-2019-0019
24. Heydari A, Mazlom SR, Ranjbar H, Scurlock-Evans L. A study of Iranian nurses' and midwives' knowledge, attitudes, and implementation of evidence-based practice: The time for change has arrived. Worldviews Evid Based Nurs. (2014) 11:325–31. doi: 10.1111/wvn.12052
25. Zhou F, Hao Y, Guo H, Liu H. Attitude, knowledge, and practice on evidence-based nursing among registered nurses in traditional Chinese medicine hospitals: a multiple center cross-sectional survey in China. Evid Based Complement Altern Med. (2016) 2016:5478086. doi: 10.1155/2016/5478086
26. Aburuz ME, Hayeah HA, Dweik G, Alakash H. Knowledge, attitudes, and practice about evidence-based practice: A jordanian study. Health Sci J. (2017) 11:2. doi: 10.21767/1791-809X.1000485
27. Nalweyiso DI, Kabanda J, Mubuuke AG, Sanderson K, Nnyanzi LA. Knowledge, attitudes and practices towards evidence based practice: a survey amongst radiographers. Radiography. (2019) 25:327–32. doi: 10.1016/j.radi.2019.03.004
28. Worku T, Yeshitila M, Feto T, Leta S, Mesfin F, Mezmur H. Evidence-based medicine among physicians working in selected public hospitals in eastern Ethiopia: a cross-sectional study. BMC Med Inform Decis Mak. (2019) 19:1–8. doi: 10.1186/s12911-019-0826-8
29. Li S, Cao M, Zhu X. Evidence-based practice: knowledge, attitudes, implementation, facilitators, and barriers among community nurses—systematic review. Medicine. (2019) 98:e17209. doi: 10.1097/MD.0000000000017209
30. Dilling JA, Swensen SJ, Hoover MR, Dankbar GC, Donahoe-Anshus AL, Murad MH, et al. Accelerating the use of best practices: the Mayo Clinic model of diffusion. Jt Comm J Qual Patient Saf. (2013) 39:AP1–2. doi: 10.1016/S1553-7250(13)39023-0
31. Upton D, Upton P. Development of an evidence-based practice questionnaire for nurses. J Adv Nurs. (2006) 53:454–8. doi: 10.1111/j.1365-2648.2006.03739.x
32. Chiu YW, Weng YH, Lo HL, Hsu CC, Shih YH, Kuo KN. Comparison of evidence-based practice between physicians and nurses: a national survey of regional hospitals in Taiwan. J Contin Educ Health Prof. (2010) 30:132–8. doi: 10.1002/chp.20070
33. Alshehri AA, Al-Khowailed MS, Alnuaymah FM, Alharbi AS, Alromaihi MS, Alghofaili RS, et al. Knowledge, attitude, and practice toward evidence-based medicine among hospital physicians in Qassim region, Saudi Arabia. Int J Health Sci. (2018) 12:9.
34. Yahui HC, Swaminathan N. Knowledge, attitudes, and barriers towards evidence-based practice among physiotherapists in Malaysia. Hong Kong Physiother J. (2017) 37:10–8. doi: 10.1016/j.hkpj.2016.12.002
35. Abdel-Kareem A, Kabbash I, Saied S, Al-Deeb A. Knowledge, practices and attitudes of physicians towards evidencebased medicine in Egypt. East Mediterr Health J. (2019) 25:82–9. doi: 10.26719/emhj.18.010
36. Takrouri MS, Takrouri FM. Historical report account on the development of anesthesiology and medical services in Kingdom Saudi Arabia 1956-1987: MI Al-Khawashki's letter dated April 25th 1997. Anesth Essays Res. (2011) 5:236. doi: 10.4103/0259-1162.94794
37. Davies KS. Evidence-based medicine: UK doctors' attitudes and understanding. Int J Evid Based Healthcare. (2011) 9:265–73.
38. Elarab HS, El Salam SA, Behalik SG, Eltayeb HE. Nurses, practice, knowledge and attitude towards evidence-based practice at Yanbu general hospital-kingdom of Saudi Arabia. Life Sci J. (2012) 9:1062–71.
39. Ammouri AA, Raddaha AA, Dsouza P, Geethakrishnan R, Noronha JA, Obeidat AA, et al. Evidence-based practice: Knowledge, attitudes, practice and perceived barriers among nurses in Oman. Sultan Qaboos Univ Med J. (2014) 14:e537.
40. Attar AA, Khereldeen MM, Refaat B, Saleh HA. Knowledge and Attitude of Physicians toward Evidence-Based Medicine. Int J Pure Appl Sci Technol. (2014) 21:17.
41. Melnyk BM, Fineout-Overholt E. Evidence-based Practice in Nursing & Healthcare: A Guide to Best Practice. New York, NY: Lippincott Williams & Wilkins. (2018).
42. Adamu A, Naidoo JR. Exploring the perceptions of registered nurses towards evidence-based practice in a selected general hospital in Nigeria. Afr J Nurs Midwifery. (2015) 17:33–46.
43. Baig M, Sayedalamin Z, Almouteri O, Algarni M, Allam H. Perceptions, perceived barriers, and practices of physicians' towards evidence-based medicine. Pak J Med Sci. (2016) 32:49.
44. Bertram R, Kerns S. Selecting and Implementing Evidence-based Practice: A Practical Program Guide. Switzerland: Springer. (2019).
45. Leedal JM, Smith AF. Methodological approaches to anaesthetists' workload in the operating theatre. Br J Anaesth. (2005) 94:702–9. doi: 10.1093/bja/aei131
Keywords: evidence based practice, attitudes, use, knowledge, anesthesia teams, Healthcare Professionals
Citation: Al Anazi SK, Al Zahrani WA, Alsanad MA, Alzahrani MS, Al Ghamdi IS, Alotaibi AA, Al maliki MA, Asiri HM, Alshehri GM, Alanazi AS and Al Anazi AK (2022) A cross-sectional survey exploring the attitude, knowledge, and use of anesthesia teams toward evidence-based practice in Riyadh Saudi Arabia. Front. Public Health 10:1017106. doi: 10.3389/fpubh.2022.1017106
Received: 11 August 2022; Accepted: 05 October 2022;
Published: 31 October 2022.
Edited by:
Russell Kabir, Anglia Ruskin University, United KingdomReviewed by:
Himel Mondal, Saheed Laxman Nayak Medical College, IndiaJamileh Farokhzadian, Kerman University of Medical Sciences, Iran
Copyright © 2022 Al Anazi, Al Zahrani, Alsanad, Alzahrani, Al Ghamdi, Alotaibi, Al maliki, Asiri, Alshehri, Alanazi and Al Anazi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdulmueen Awadh Alotaibi, YW90YWliaUBtY3N0LmVkdS5zYQ==; Salem Khalaf Al Anazi, c2thbGFuYXppODVAZ21haWwuY29t
 Salem Khalaf Al Anazi1*
Salem Khalaf Al Anazi1* Waleed Abdullah Al Zahrani
Waleed Abdullah Al Zahrani Abdulmueen Awadh Alotaibi
Abdulmueen Awadh Alotaibi