- 1Department of Psychiatry, Duke University School of Medicine, Duke University Health System, Durham, NC, United States
- 2Duke Center for Healthcare Safety and Quality, Duke University Health System, Durham, NC, United States
- 3Division of Neonatal and Developmental Medicine, Department of Pediatrics, Stanford University School of Medicine and Lucile Packard Children's Hospital, Palo Alto, CA, United States
- 4California Perinatal Quality Care Collaborative, Palo Alto, CA, United States
- 5Division of Pediatric Critical Care Medicine, Department of Pediatrics, Stanford University School of Medicine and Lucile Packard Children's Hospital, Palo Alto, CA, United States
Importance: Problems with the wellbeing of healthcare workers (HCWs) are widespread and associated with detrimental consequences for the workforce, organizations, and patients.
Objective: This study tested the effectiveness of the Web-based Implementation for the Science of Enhancing Resilience (WISER) intervention, a positive psychology program, to improve six dimensions of the wellbeing of HCWs.
Design: We conducted a randomized controlled trial of HCWs between 1 April 2018 and 22 July 2019. Cohort 1 received WISER daily for 10 days. Cohort 2 acted as a waitlist control before receiving WISER.
Setting: Web-based intervention for actively employed HCWs across the United States.
Participants: Eligibility criteria included being ≥18 years old and working as a HCW. Each participant was randomized to start the intervention or serve as a waitlist control for 14 days before starting the intervention.
Interventions: Cohorts received links via 10 texts exposing them to introductory videos and positive psychology exercises (3 good things, cultivating awe, random acts of kindness, cultivating relationships, and gratitude letters).
Main outcomes and measures: The primary outcome was emotional exhaustion; secondary outcomes included depressive symptoms, work-life integration, happiness, emotional thriving, and emotional recovery. All outcomes were assessed at baseline, 1-week post-intervention (primary endpoint), and 1, 6, and 12-month post-intervention. Outcomes were measured using six validated wellbeing instruments, rescaled to 100-point scales for comparison. Six items assessed participants' WISER experience. The analysis employed mixed-effects models.
Results: In cohorts 1 and 2, 241 and 241 initiated WISER, and 178 (74%) and 186 (77%) completed the 6-month follow-up, respectively. Cohort populations were similar at baseline, mostly female (81; 76%) and nurses (34; 32%) or physicians (22; 23%), with 1–10 years of experience in their current position (54; 52%). Relative to control, WISER significantly improved depressive symptoms [−7.5 (95%CI: −11.0, −4.0), p < 0.001], work-life integration [6.5 (95%CI: 4.1, 8.9), p < 0.001], happiness [5.7 (95%CI: 3.0, 8.4), p < 0.001], emotional thriving [6.4 (95%CI: 2.5, 10.3), p = 0.001], and emotional recovery [5.3 (95%CI: 1.7, 8.9), p = 0.004], but not emotional exhaustion [−3.7 (95%CI: −8.2, 0.8), p = 0.11] at 1 week. Combined cohort results at 1, 6, and 12 months showed that all six wellbeing outcomes were significantly improved relative to baseline (p < 0.05 for all). Favorable impressions of WISER were reported by 87% of participants at the 6-month post-assessment.
Conclusion and relevance: WISER improved HCW depressive symptoms, work-life integration, happiness, emotional thriving, and emotional recovery. Improvements in all HCW wellbeing outcomes endured at the 1-, 6-, and 12-month follow-ups. HCW's impressions of WISER were positive.
Clinical trials number: https://clinicaltrials.gov/ct2/show/, identifier: NCT02603133. Web-based Implementation for the Science of Enhancing Resilience Study (WISER).
Introduction
Safe and reliable healthcare was unambiguously linked to the wellbeing of healthcare workers (HCWs) before there was a global health crisis (1–4). The COVID-19 pandemic has caused historic levels of psychological distress in HCWs in particular (5–8), revealing the additional burdens of social isolation, fear of contracting the disease, economic strain, unpredictable childcare, uncertainty about the future, prolonged bouts of physical and emotional exhaustion, and moral distress. Maintaining a healthy workforce requires not only a sufficient number of HCWs but also maximizing the ability of each one to meet the needs of patients (9).
Before the pandemic, problems with HCW wellbeing were already disturbingly common [e.g., 30–40% of physicians and nurses report burnout (10–12)] and expensive (13), while traditional workplace wellness efforts are costly and often ineffective (14, 15). Longstanding difficulties with work-life integration, challenges with the electronic health record, and a difficult work culture remain largely unaddressed (16–18). Poor HCW wellbeing has been linked to adverse patient events, including increased rates of infections (1, 3) and self-reported errors (1, 2). Furthermore, struggling HCWs are more likely to drop out of the workforce, increasing costly turnover (19–21) and further exacerbating staffing shortages (22).
Although they are not a panacea against the rising tide of HCW burnout, evidence that web-based wellbeing programs are effective is growing (23–26). Unfortunately, feasible interventions to improve wellbeing are uncommon (27). We have developed and refined an engaging, low-burden program [Web-based Implementation for the Science of Enhancing Resilience (WISER)] to enable rapid and enduring improvements in wellbeing (28). This stepwise program uses updated versions of evidence-based interventions drawn from positive psychology that have been effective in improving wellbeing and reducing depression symptoms, which are delivered via mobile platforms (24–26, 28).
Wellbeing intervention uptake by busy HCWs requires evidence-based tools that are accessible, easy to use, and engaging. We have adapted WISER considerably in response to these needs (28). In the original WISER trial, we found equivalent efficacy for a 6 vs. 1-month intervention duration. From qualitative feedback, we were encouraged to further reduce the user participation burden. In addition, the original study randomized entire newborn intensive care units. Such clustering (by work setting) may have supported the intervention's efficacy but may limit scalability. Therefore, the objective of this study was to test the efficacy of an abbreviated WISER in 10 texts intervention for improving HCW wellbeing (emotional exhaustion, depressive symptoms, work-life integration, happiness, emotional thriving, and emotional recovery) using an individual-level randomized design in which participants were randomized into one of the following two cohorts: the intervention or waitlist control. The efficacy of WISER was tested using the randomized trial 1-week endpoint, but the persistence of effects was tested up to a year later. Given the bite-sized nature of this brief 10-day intervention, evidence supporting the sustainability of improvements to wellbeing is warranted.
Hypothesis 1 (randomized controlled trial, RCT): Efficacy of WISER in 10 texts: The intervention will improve HCW wellbeing compared with waitlist control by the 1-week post-intervention primary endpoint.
Hypothesis 2 (endurance of effects): The benefits of WISER will endure at 1-, 6-, and 12-month post-intervention.
Materials and methods
Design
HCWs were randomly assigned to one of the two cohorts in the investigator-initiated, randomized controlled study (RCT) known as WISER in 10 texts. Cohort 1 completed the baseline assessment and received the intervention on 9 July 2018, while cohort 2 acted as a waitlist control and provided an initial (“waitlist control”) assessment on 23 July (14 days later). Cohort 2 completed their baseline assessment and received the intervention. The RCT portion of the study used the 1-week post-assessment results as the primary endpoint to minimize the duration of the waitlist period for HCWs looking to do something about their wellbeing in the near term. The wherewithal necessary to do something about wellbeing of HCWs is increasingly challenging (8). Specifically, this difference-in-differences approach was calculated as follows: (cohort 1: 1-week post-intervention—baseline)—(cohort 2: baseline—waitlist control). A sensitivity analysis using t-tests compared 1-week cohort 1 post-intervention with the baseline of cohort 2. The remaining time points were used to test whether benefits endured at 1, 6, and 12 months. The QualtricsTM platform was used for enrollment, data collection, randomization of individual enrollees to study cohorts, and delivery of text messages with links to WISER activities.
Participants
The US inpatient and outpatient HCWs were enrolled from 1 April to 9 July 2018 using a link on our website (https://www.hsq.dukehealth.org/), labeled bit.ly/3WISER, or were provided the link during continuing education talks and webinars. Generally, people who seek the content on our website and/or attend our continuing education activities have a background or interest in patient safety, quality improvement, and/or wellbeing. There was also a brief explanation of the WISER intervention during enrollment that provided an overview of the prevalence and severity of wellbeing issues in healthcare, as well as the length and nature of WISER in 10 texts as a method for “pausing and reflecting on what is going well.”
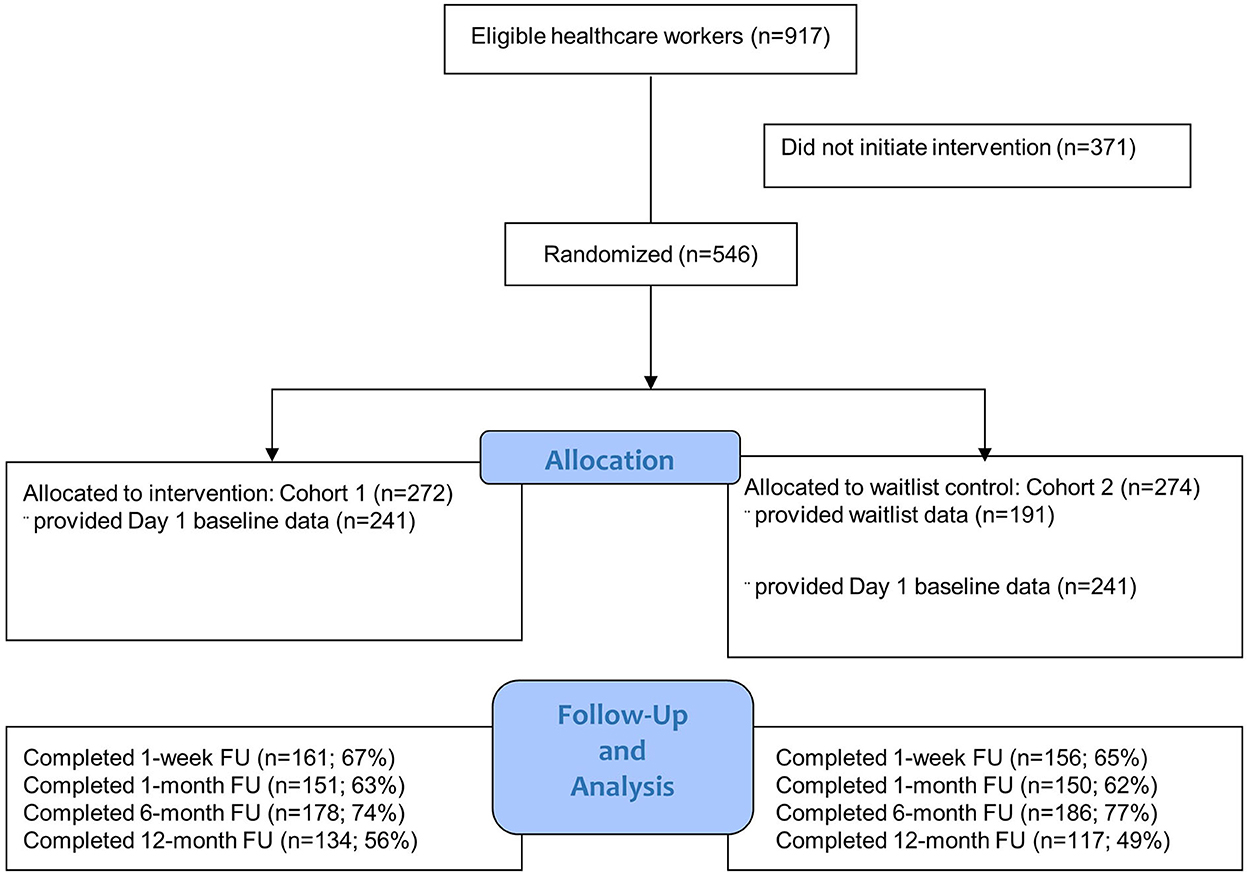
Participants were informed of the start date and follow-up dates during enrollment. We assessed cohorts at five time points: day 1 (baseline, prior to starting the intervention), and 1, 1, 6, and 12-month post-intervention (Figure 1). Cohort 2 had one additional assessment at the beginning of their waitlist period (titled “waitlist control”) to allow for RCT analyses. Each cohort received the intervention; therefore, blinding was not feasible.
Intervention
WISER in 10 texts is comprised of five guided wellbeing modules based on adult learning principles, combining educational material with practice-based learning (28). Individual modules have been favorably evaluated as brief, feasible, and practical (24–26). Links to each module of the intervention were delivered via text message at 7 pm local time each evening for 10 days. Modules were introduced with an 8–10 min evidence-based educational video and included simple and engaging reflective activities lasting from 2 to 7 min. Every module included a prompt for doing three good things; texts 2–4 and 6–10 included a second “positive reflections” activity to complete. The structure was given as follows:
Text 1: 3 Good Things.
Text 2: 3 Good Things; Cultivate Awe.
Text 3: 3 Good Things; Random Act of Kindness.
Text 4: 3 Good Things; 1 Good Chat/Cultivate Relationships.
Text 5: 3 Good Things; inform the participant that next text they choose the tool they want to use in addition to continuing Three Good Things.
Text 6: 3 Good Things; Choice of Awe/Kindness/ Relationships.
Text 7: 3 Good Things; Choice of Awe/Kindness/ Relationships.
Text 8: 3 Good Things; Choice of Awe/Kindness/ Relationships.
Text 9: 3 Good Things; Choice of Awe/Kindness/ Relationships.
Text 10: 3 Good Things; Cultivate Gratitude.
Three Good Things asks participants to reflect on and briefly describe three positive experiences that occurred that day (24, 29). Cultivate Awe provided an opportunity to learn about and experience the benefits of awe and wonder through a series of visually and conceptually stunning images followed by an exercise to reflect on one of their own experiences of awe (30). Random Acts of Kindness provided an opportunity to learn, practice, and reflect on the power of providing unsolicited kindness to others by documenting acts of kindness that were witnessed, committed, and/or received (31). Relationship Resilience promoted an understanding of beneficial relationship patterns, including reflections on recent positive interactions and experiences (32). Gratitude provided a structured opportunity to express gratitude toward others through a guided letter-writing exercise (29, 33).
Measures
The multidimensional nature of wellbeing makes it difficult to summarize in one domain. In addition to the four wellbeing domains (emotional exhaustion, depression, work-life integration, and subjective happiness) used in the original WISER RCT (28), two domains (emotional thriving and emotional recovery) were added. Given the contemporary relevance to HCWs, responsiveness to interventions, and psychometric validity, we chose the primary outcome of emotional exhaustion (EE). EE was assessed by a widely used (8, 16, 17, 24, 25, 34, 35) 5-item derivative of the emotional exhaustion scale of the Maslach Burnout Inventory (36), shown to have excellent psychometric properties (24–26, 34, 35, 37, 38), external validity (16, 17, 34), and responsiveness to interventions (18, 24–26, 37). Details of each wellbeing domain are in the Supplementary material.
Randomization
Participants enrolled using Qualtrics, which consecutively randomized participants into two cohorts. Participants received details of the intervention and their start date in an email for their records.
Statistical analyses
For comparability across the six wellbeing domains, we rescaled outcome measures to 100-point scales. Hypotheses tested included the efficacy of WISER in cohort 1 (intervention) vs. cohort 2 (waitlist control) and combined cohort changes from baseline to 1-week, 1-month, 6-month, and 12-month post-assessments. The randomized trial and endurance of effects portions of the study were evaluated using generalized linear mixed-effects modeling that included fixed effects for time and random effects for participants to account for within-participant correlation (39). To facilitate statistical power and interpretation of the long-term follow-up results, we combined the two cohorts and used percent concerning thresholds. This technique is commonly used in safety culture and wellbeing research when looking across a set of metrics (some positively and some negatively balanced) such that a “low percent concerning,” or a reduction in percent concerning was easier to interpret (16, 17, 34, 40).
Mixed-model hypothesis tests were conducted in SAS 9.4 using PROC GLIMMIX. A p-value of <0.05 was considered statistically significant. We considered EE improvement of at least 10% from baseline to be meaningful based on previous studies (24, 26, 28, 41). This translated to a decrease in EE from 50/100 to 45/100, a 5-point decline, or an effect size of 0.25, assuming a standard deviation of 20, needing 253 participants in each arm of the intervention to have 80% power to detect this effect size.
Results
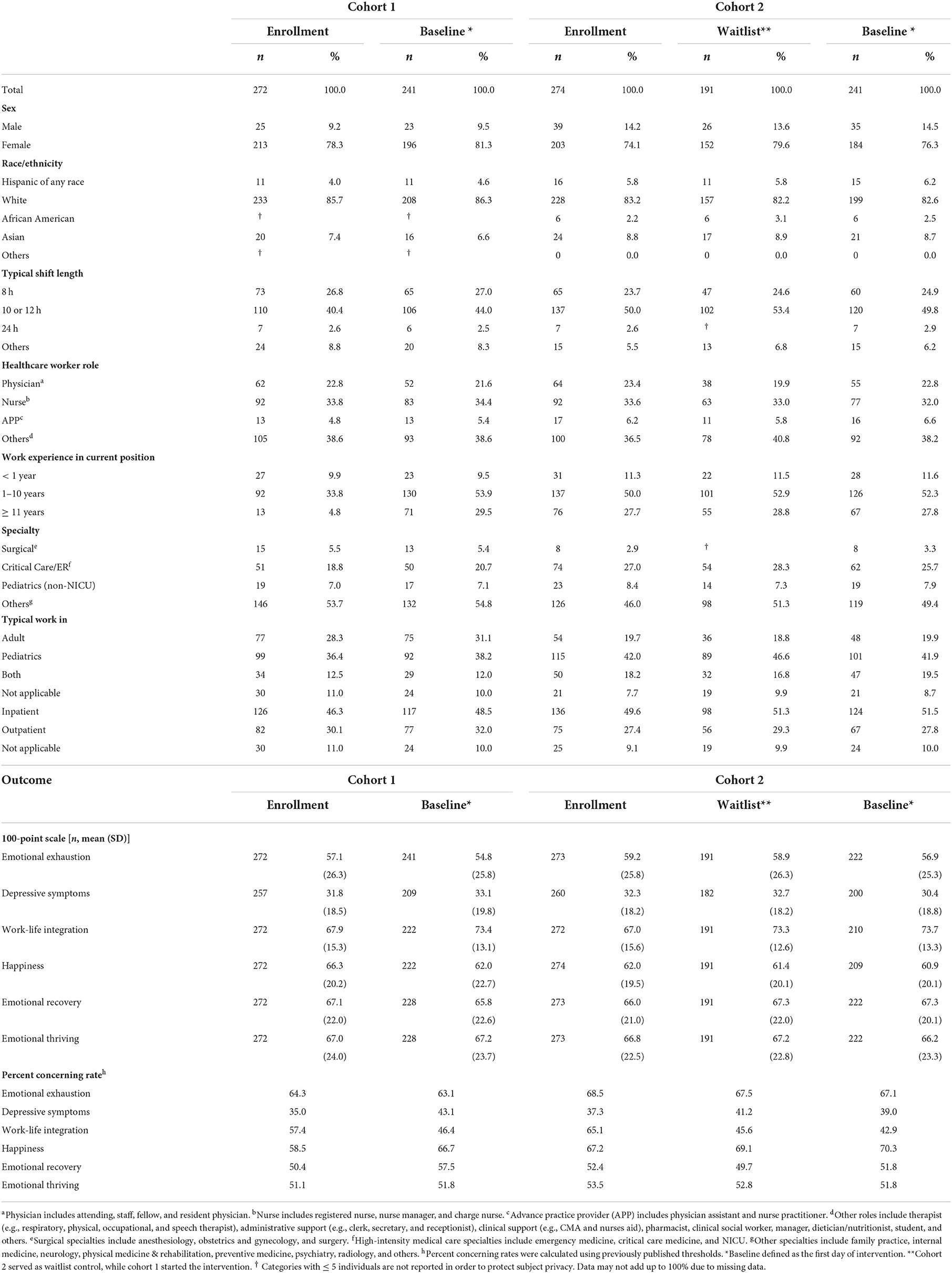
Enrollment and participation in the trial are shown in Figure 1 (the CONSORT diagram). In cohort 1, 241 respondents initiated the intervention, with 161 (67%) in the follow-up at 1 week, 151 (63%) at 1 month, 178 (74%) at 6 months, and 134 (56%) at 12 months. In cohort 2, 241 respondents initiated the intervention, with 156 (65%) in the follow-up at 1 week, 150 (62%) at 1 month, 186 (77%) at 6 months, and 117 (49%) at 12 months. Table 1 displays the characteristics of the study population by cohort prior to the intervention. Cohorts 1 and 2 had similar demographics at baseline. No adverse events were reported. The six dimensions of HCW wellbeing exhibited good psychometric reliability (Cronbach's α): emotional exhaustion (α = 0.84), depression (α = 0.83), happiness (α = 0.86), work-life integration (α = 0.80), emotional thriving (α = 0.81), and emotional recovery (α = 0.82).
RCT Efficacy: The intervention will improve HCW's emotional exhaustion, depression, work-life integration, happiness, emotional thriving, and emotional recovery compared with the waitlist control by the 1-week post-intervention primary endpoint (Hypothesis 1). On a 100-point scale, compared with cohort 2 (waitlist control), the WISER intervention in cohort 1 reduced depression (−7.5, 95% CI −11.0–−4.0, p <0 .001) and improved work-life integration (6.5, 95% CI 4.1–8.9, p < 0.001), happiness (5.7, 95% CI 3.0–8.4, p < 0.001), emotional thriving (6.4, 95% CI 2.5–10.3, p = 0.004), and emotional recovery (5.3, 95% CI 1.7–8.9, p < 0.001), but emotional exhaustion did not reach significance (−3.7, 95% CI −8.2–0.8, p = 0.11; see Table 2). The sensitivity analysis using t-tests compared 1-week cohort 1 post-intervention with the baseline of cohort 2 showing significant improvements in all wellbeing outcomes (p ≤ 0.005) except for emotional thriving and emotional recovery (p = 0.13; see Table 2).
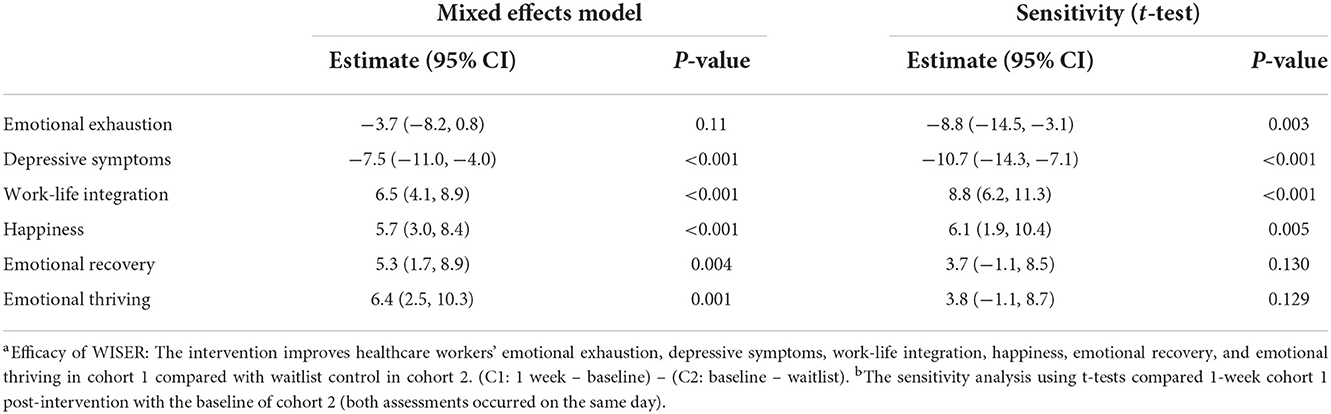
Table 2. Efficacy of WISER intervention at 1 week in mixed-effects modela and sensitivity analysesb.
Endurance of effects: The effects of WISER will endure at 1-, 6-, and 12-month post-intervention (Hypothesis 2).
In combined cohorts on a 100-point scale, at 1-, 6-, and 12-month post-intervention, WISER was associated with reduced emotional exhaustion (p < 0.001), reduced depressive symptoms (p < 0.001), improved work-life integration (p < 0.001), improved happiness (p < 0.001), improved emotional recovery (p < 0.001), and improved emotional thriving (p < 0.001 to 0.03), relative to baseline (Table 3; Figures 2, 3). In combined cohorts using % concerning, WISER was similarly associated with improvements in all outcomes at all time points (Table 4).
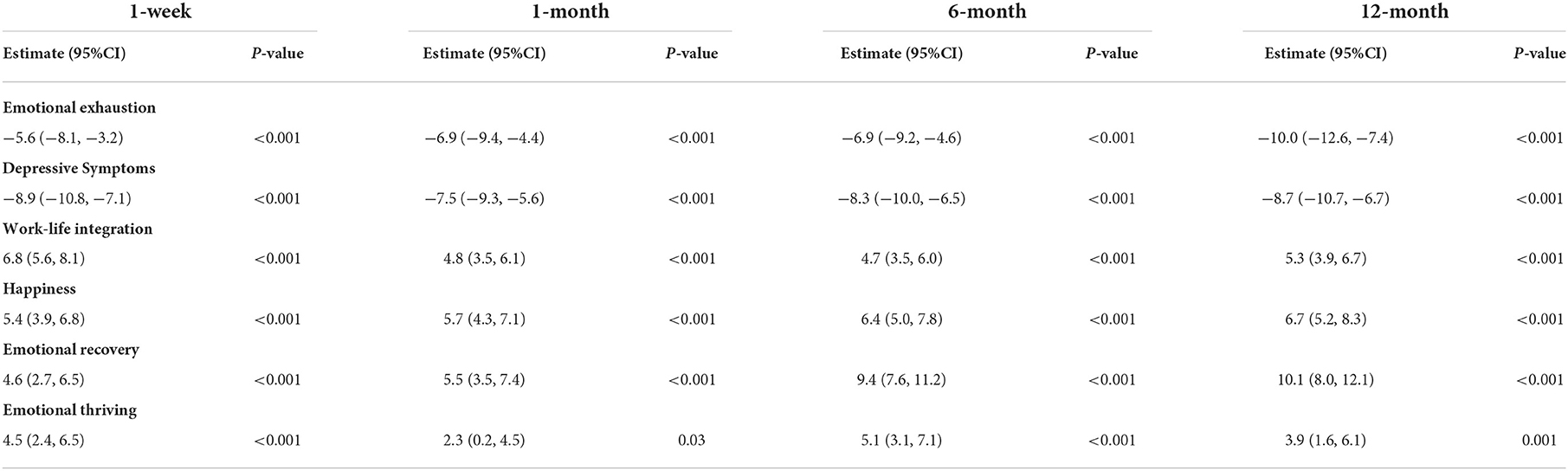
Table 3. Effectiveness of WISER at 1-week, 1-, 6-, and 12-month post-intervention (100-point scale), combined cohorts.
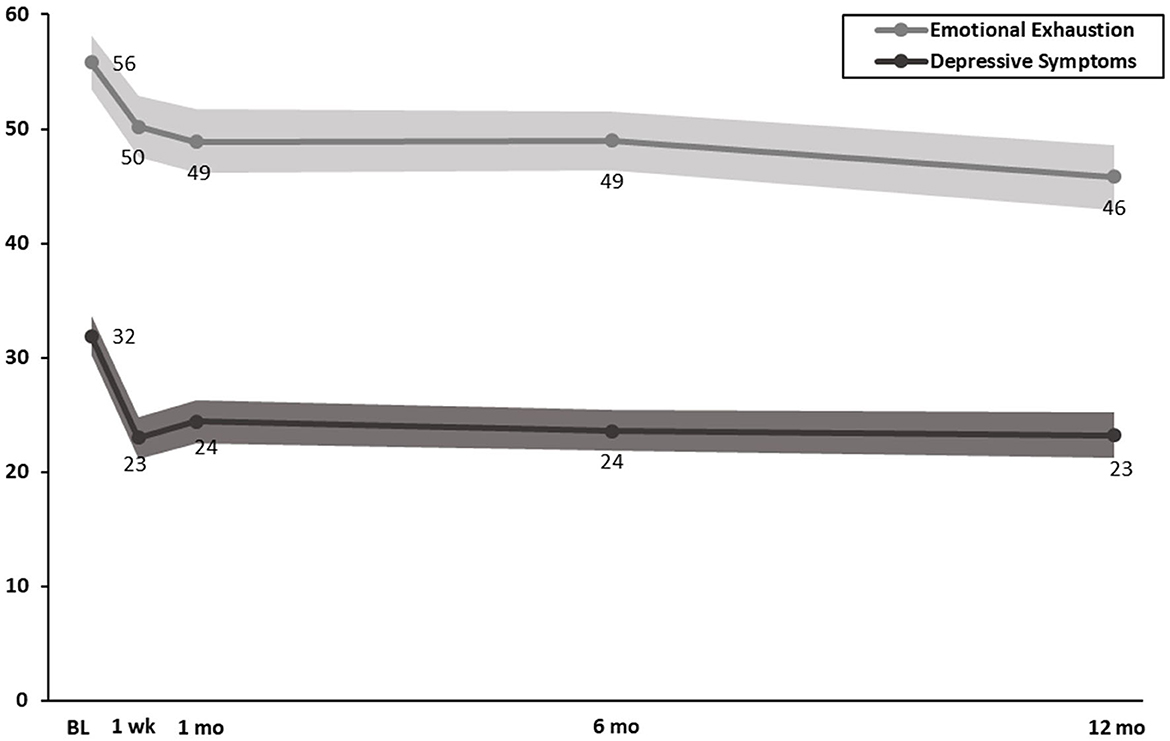
Figure 2. Effect of WISER for emotional exhaustion and depressive symptoms at 1-week, 1-, 6-, and 12-month post-intervention (100-point scale). Dots in the middle line: point estimates from mixed-effects models for each time point; shaded areas: 95% confidence intervals from mixed-effects models. BL, baseline; 1 wk, 1-week post-intervention; 1 mo, 1-month post-intervention; 6 mo, 6-month post-intervention; 12 mo, 12-month post-intervention.
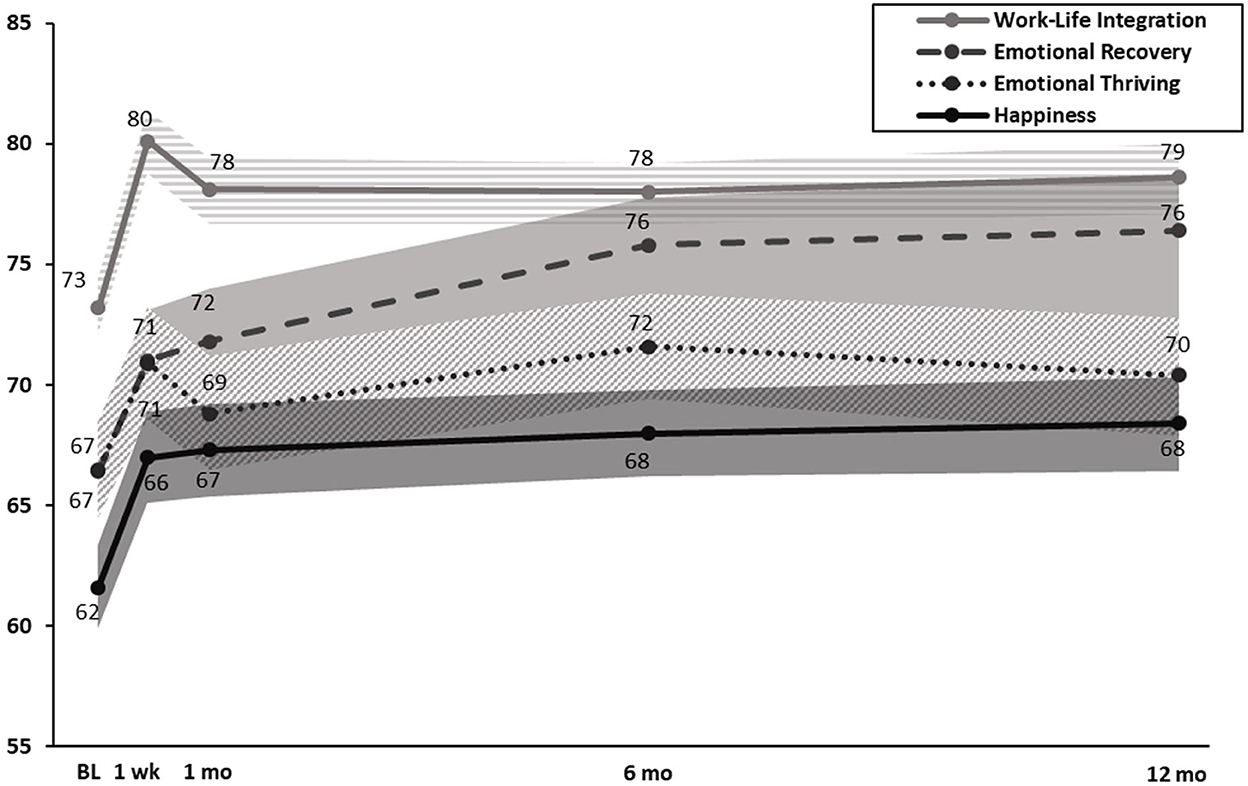
Figure 3. Effect of WISER for work-life integration, emotional recovery, emotional thriving, and happiness at 1-week, 1-, 6-, and 12-month post-intervention (100-point scale). Note: Dots in the middle line: point estimates from mixed-effects models for each time point; shaded areas: 95% confidence intervals from mixed-effects models. BL, baseline; 1 wk, 1-week post-intervention; 1 mo, 1-month post-intervention; 6 mo, 6-month post-intervention; 12 mo, 12-month post-intervention.
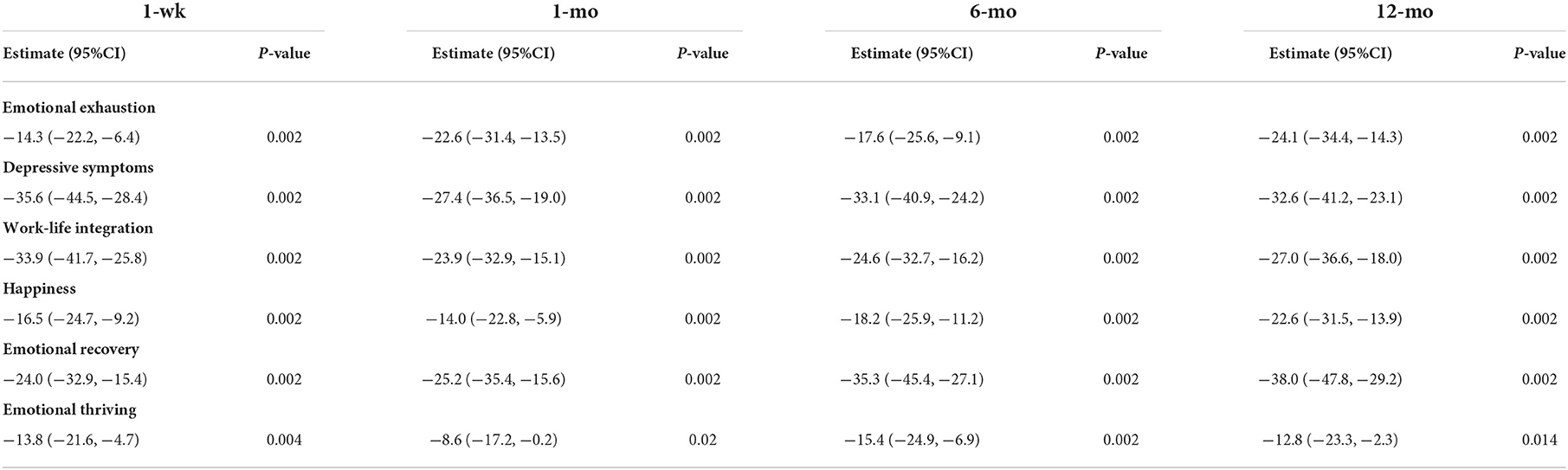
Table 4. Effectiveness of WISER at 1-week, 1-, 6-, and 12-month post-intervention (% concerning), combined cohorts.
Neither RCT efficacy nor endurance of effects results changed meaningfully after adjusting for covariates.
Participant evaluation of WISER at the 6-month post-intervention was positive, with 87% reporting overall favorable impressions (see Supplementary material for Participant Evaluation of WISER).
Discussion
In this RCT, WISER in 10 texts demonstrated robust evidence of efficacy across 5 of 6 wellbeing outcome measures by 1 week and was associated with enduring improvements for all 6 wellbeing outcomes at the 1-, 6-, and 12-month post-assessment of emotional exhaustion, depressive symptoms, work-life integration, happiness, emotional thriving, and emotional recovery. WISER demonstrated a significant and enduring effect among neonatal intensive care unit HCWs in the original RCT (28), and here we find similar results despite a significantly compressed intervention period from 6 months to only 10 days. The magnitude of the program's wellbeing improvements is favorable relative to a meta-analysis of interventions to improve HCW wellbeing (27).
Implementation of WISER demonstrated efficacy for 5 of the 6 outcomes at the 1-week post-intervention (emotional exhaustion did not reach statistical significance), and it demonstrated enduring effects for all outcomes at all subsequent follow-up time points. Emotional exhaustion was significantly lower by the 1-month follow-up and that reduction continued at 6 and 12 months. In retrospect, our efforts to shorten WISER, including the follow-up period of 1-week post-intervention, may have been too early to detect a significant change in emotional exhaustion. Previous studies using the 1-month follow-up timeframe have shown significant reductions in HCW emotional exhaustion (24–26, 28), and it may take several weeks for the increases in access to positive emotions attained through WISER to accrue. Although the mixed effects model RCT analysis of emotional exhaustion at 1 week did not reach significance, the added statistical power to detect improvements in combined cohort analyses (Tables 3, 4) demonstrated significant improvements for all wellbeing outcomes across all time periods (including the 1-week post-intervention). The first RCT of WISER used a 1-month post-intervention and found that WISER reduced emotional exhaustion by 1 month, and the effect continued at the 6-month follow-up. Future studies should consider extending the post-intervention beyond 1 week when EE is used.
Wellbeing interventions based on positive psychology (42) research may help alleviate some of the growing problems with HCWs' wellbeing, which is especially salient during the unprecedented and prolonged demands of the COVID-19 pandemic (5, 8, 43). The durability and increase of effect sizes in wellbeing outcomes over time suggest that our results are clinically meaningful and compare favorably with longer and more resource-dependent interventions intended to improve wellbeing and mental health, such as individualized coaching or meditation (41, 44–46). The HCW WISER user experience was positive, with 87% reporting overall favorable impressions. Consistent with the first RCT (28) of WISER showing improvements at 1- and 6-month post-intervention, the current RCT showed that a simple, low-resource intervention can cause robust improvements in individual HCW wellbeing that are enduring for at least a year. As of this writing, WISER in 10 texts is still available as a research study to all US HCWs at bit.ly/3WISER.
Notwithstanding the efficacy of WISER, we wish to avoid a false dichotomy on how to address HCW wellbeing. It is tempting to polarize the topic of individual vs. institutional resources for HCW wellbeing and to advocate for institutional reforms almost exclusively (47). Understandably frustrated HCWs who have experienced repeated upheavals from broken systems are correct to insist on improvements. However, this mindset only focuses on part of the solution because we also need individual-level solutions for the plurality of HCWs (5) who are struggling with wellbeing right now (48). Fixing the system takes time, and obvious targets for sources of burnout such as the electronic health record account for less than one-tenth of the burnout variance in comparison to work culture (18). A more practical, responsive, and nuanced approach would be to “empower HCWs to fix the system and give them some useful wellbeing resources to choose from because they are profoundly stressed here and now.” This dual approach would also be responsive to the significant differences in wellbeing by HCW role, gender, years of experience, specialty, and individual proclivity (8).
Most participants (87%) reported that WISER helped them to recognize more opportunities for positive emotions, potentially elucidating the psychological pathways that underlie WISER's effectiveness. People who struggle with wellbeing experience decreased ability to notice and pay attention to positive stimuli (49). Rigorous psychological research has consistently shown that experiencing positive emotion is central to building consequential personal resources like wellbeing (50), as well as helping to find meaning after adversity (51), and accelerating recovery after emotional upheavals (52). Positive emotions like hope, gratitude, and serenity may recharge depleted batteries (53), and experiencing positive emotions has both psychological and physiological benefits (54). Despite the well-documented descriptions of burnout in healthcare, few interventions have been tested in randomized trials, and fewer still have used multiple theory-driven interventions. The WISER intervention packages tools that promote noticing and savoring positive emotions, require only a mobile phone, and is scalable and free, and its 10-day version is quite feasible.
Limitations
This study should be viewed in light of its design. In line with other wellbeing behavioral intervention studies (55–60), we experienced non-initiation and attrition in both study cohorts, which may introduce selection bias. The number of participants who initiated the intervention by providing baseline data (n = 482) was considerably smaller than the number who expressed interest (n = 917) in this study by clicking the study description link, meaning 53% initiated WISER. This challenge of initiation rates among busy HCWs was exemplified in a recent innovative RCT of professional coaching (41) for physicians that showed similar efficacy to our study, yet with only 88 of 764 (11.5%) eligible physicians choosing to participate. This study compares favorably to this and other interventions, including dieting, smoking cessation, and other web-based wellbeing interventions (55, 56, 61), which tend to have low rates of initiation (~20%) even when financial incentives are provided (55). Similarly, the Centers for Disease Control and Prevention recognized in-person lifestyle change programs such as the National Diabetes Prevention Program average over 60% attrition by week 44 (62), and web-based weight-loss programs report 65–70% of their initiators are no longer using the web-based program by the 52-week mark (63). Emotional exhaustion itself may contribute to a lack of initiation energy (8) and may explain the lack of effectiveness found in workplace wellbeing programs (14). It is unknown if participants who were lost to follow-up experienced similar improvements to those who completed the study, suggesting that our results should be interpreted with caution but those who completed the intervention derived significant benefits. Statistical power was good for the combined cohorts but slightly underpowered for individual cohort analyses (this could explain why emotional exhaustion did not reach significance at 1-week by cohort but did in the combined cohort analyses). This lack of statistical power to compare individual cohorts across follow-ups is a significant limitation, and future studies should recruit to the point of overpowered samples given the growing problems of loss to follow-up in HCW wellbeing studies. Using an enrollment process with a fixed starting date provided predictability for participants, but future studies may consider rolling enrollments and start dates to allow for adequately powered analyses to be used. Finally, our participants were mostly white females, which reflects the workforce demographics in many large academic centers. We know that female HCWs report significantly worse wellbeing than their male counterparts (64), and that female, racial, and ethnic minority HCWs experience more mistreatment and discrimination by patients, families, and visitors in ways that deteriorate wellbeing (65). It is uncertain whether our findings are generalizable to settings with more diverse workforces, and the extent to which particular HCW demographic groups benefit from wellbeing interventions is an area ripe for future research.
Conclusion
WISER in 10 texts significantly improved the wellbeing of HCWs relative to a waitlist control, and improvements were sustained over 1 year for emotional exhaustion, depressive symptoms, work-life integration, happiness, emotional thriving, and emotional recovery. Participants reported enjoyment of the intervention, with four out of five evaluating WISER favorably. Although initiating the intervention among busy HCWs can be a challenge, WISER provides an ongoing low-intensity positive psychology wellbeing resource as HCWs continue to respond to the COVID-19 pandemic.
Data availability statement
The authors will share raw data from the study upon reasonable request to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Duke University Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
JS created WISER, conceptualized and designed the study, assisted in data analysis and interpretation, critically reviewed the manuscript, and approved the final manuscript as submitted. KA consulted on tool development and study design, assisted in the analysis and interpretation of the data, critically reviewed the manuscript, and approved the final manuscript as submitted. XC coordinated the data management and carried out the initial data analyses, critically reviewed the manuscript, and approved the final manuscript as submitted. DT assisted in the interpretation of the data, critically reviewed the manuscript, and approved the final manuscript as submitted. JP conceptualized and designed the study, assisted in data analysis and interpretation, critically reviewed the manuscript, and approved the final manuscript as submitted. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This work was supported by the National Institute of Child Health and Human Development (R01 HD084679-01, Co-PIs: JS and JP), the Agency for Healthcare Research and Quality (K08 HS027837-01, PI: DT), and the Health Resources and Services Administration (5 U3NHP45396-02-00, PI: JS).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1016407/full#supplementary-material
References
1. Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Ann Surg. (2010) 251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3
2. Tawfik DS, Profit J, Morgenthaler TI, Satele DV, Sinsky CA, Dyrbye LN, et al. Physician burnout, wellbeing, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. (2018) 93:1571–80. doi: 10.1016/j.mayocp.2018.05.014
3. Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care–associated infection. Am J Infect Control. (2012) 40:486–90. doi: 10.1016/j.ajic.2012.02.029
4. Tawfik DS, Scheid A, Profit J, Shanafelt T, Trockel M, Adair KC, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. (2019) 171:555. doi: 10.7326/M19-1152
5. Haidari E, Main EK, Cui X, Cape V, Tawfik DS, Adair KC, et al. Maternal and neonatal health care worker well-being and patient safety climate amid the COVID-19 pandemic. J Perinatol. (2021) 41:961–9. doi: 10.1038/s41372-021-01014-9
6. Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. (2020) 3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185
7. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
8. Sexton JB, Adair KC, Proulx J, Profit J, Cui X, Bae J, et al. Emotional exhaustion among US healthcare workers before and during the COVID-19 pandemic, 2019–2021. JAMA Network Open. (2022) 5:e2232748. doi: 10.1001/jamanetworkopen.2022.32748
9. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. (2020) 323:2133–4. doi: 10.1001/jama.2020.5893
10. Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Satele DV, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. (2019) 94:1681–94. doi: 10.1016/j.mayocp.2018.10.023
11. Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse burnout and quality of care: cross-national investigation in six countries. Res Nurs Health. (2010) 33:288–98. doi: 10.1002/nur.20383
12. Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. (2012) 344(mar20 2):e1717–e1717. doi: 10.1136/bmj.e1717
13. Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, Fiscus LC, et al. Estimating the Attributable Cost of Physician Burnout in the United States. Ann Intern Med. (2019) 170:784–90. doi: 10.7326/M18-1422
14. Song Z, Baicker K. Effect of a workplace wellness program on employee health and economic outcomes: a randomized clinical trial. JAMA. (2019) 321:1491–501. doi: 10.1001/jama.2019.3307
15. Reif J, Chan D, Jones D, Payne L, Molitor D. Effects of a workplace wellness program on employee health, health beliefs, and medical use: a randomized clinical trial. JAMA Intern Med. (2020) 180:952–60. doi: 10.1001/jamainternmed.2020.1321
16. Sexton JB, Schwartz SP, Chadwick WA, Rehder KJ, Bae J, Bokovoy J, et al. The associations between work-life balance behaviours, teamwork climate and safety climate: cross-sectional survey introducing the work-life climate scale, psychometric properties, benchmarking data and future directions. BMJ Qual Saf. (2017) 26:632–40. doi: 10.1136/bmjqs-2016-006032
17. Schwartz SP, Adair KC, Bae J, Rehder KJ, Shanafelt TD, Profit J, et al. Work-life balance behaviours cluster in work settings and relate to burnout and safety culture: a cross-sectional survey analysis. BMJ Qual Saf. (2019) 28:142–50. doi: 10.1136/bmjqs-2018-007933
18. McPeek-Hinz E, Boazak M, Sexton JB, Adair KC, West V, Goldstein BA, et al. Clinician burnout associated with sex, clinician type, work culture, and use of electronic health records. JAMA Netw Open. (2021) 4:e215686. doi: 10.1001/jamanetworkopen.2021.5686
20. Schloss EP, Flanagan DM, Culler CL, Wright AL. Some hidden costs of faculty turnover in clinical departments in one academic medical center. Acad Med. (2009) 84:32–6. doi: 10.1097/ACM.0b013e3181906dff
21. Sinsky CA, Shanafelt TD, Dyrbye LN, Sabety AH, Carlasare LE, West CP. Health care expenditures attributable to primary care physician overall and burnout-related turnover: A cross-sectional analysis. Mayo Clin Proc. (2022) 97:693–702. doi: 10.1016/j.mayocp.2021.09.013
22. Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. (2016) 91:422–31. doi: 10.1016/j.mayocp.2016.02.001
23. Karyotaki E, Efthimiou O, Miguel C, Bermpohl FMG, Furukawa TA, Cuijpers P, et al. Internet-based cognitive behavioral therapy for depression: A systematic review and individual patient data network meta-analysis. JAMA Psychiatry. (2021) 78:361–71. doi: 10.1001/jamapsychiatry.2020.4364
24. Sexton JB, Adair KC. Forty-five good things: a prospective pilot study of the Three Good Things wellbeing intervention in the USA for healthcare worker emotional exhaustion, depression, work-life balance and happiness. BMJ Open. (2019) 9:e022695. doi: 10.1136/bmjopen-2018-022695
25. Adair KC, Rodriguez-Homs LG, Masoud S, Mosca PJ, Sexton JB. Gratitude at work: prospective cohort study of a web-based, single-exposure wellbeing intervention for health care workers. J Med Internet Res. (2020) 22:e15562. doi: 10.2196/15562
26. Adair KC, Kennedy LA, Sexton JB. Three good tools: Positively reflecting backwards and forwards is associated with robust improvements in well-being across three distinct interventions. J Posit Psychol. (2020) 15:613–22. doi: 10.1080/17439760.2020.1789707
27. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272–81. doi: 10.1016/S0140-6736(16)31279-X
28. Profit J, Adair KC, Cui X, Mitchell B, Brandon D, Tawfik DS, et al. Randomized controlled trial of the “WISER” intervention to reduce healthcare worker burnout. J Perinatol. (2021) 41:2225–34. doi: 10.1038/s41372-021-01100-y
29. Seligman MEP, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol. (2005) 60:410–21. doi: 10.1037/0003-066X.60.5.410
30. Rudd M, Vohs KD, Aaker J. Awe expands people's perception of time, alters decision making, and enhances wellbeing. Psychol Sci. (2012) 23:1130–6. doi: 10.1177/0956797612438731
31. Pressman SD, Kraft TL, Cross MP. It's good to do good and receive good: The impact of a ‘pay it forward' style kindness intervention on giver and receiver well-being. J Posit Psychol. (2015) 10:293–302. doi: 10.1080/17439760.2014.965269
32. Kok BE, Coffey KA, Cohn MA, Catalino LI, Vacharkulksemsuk T, Algoe SB, et al. How positive emotions build physical health: perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol Sci. (2013) 24:1123–32. doi: 10.1177/0956797612470827
33. Emmons RA, McCullough ME. Counting blessings vs. burdens: an experimental investigation of gratitude and subjective well-being in daily life. J Pers Soc Psychol. (2003) 84:377–89. doi: 10.1037/0022-3514.84.2.377
34. Sexton JB, Adair KC, Leonard MW, Frankel TC, Proulx J, Watson SR, et al. Providing feedback following Leadership WalkRounds is associated with better patient safety culture, higher employee engagement and lower burnout. BMJ Qual Saf. (2018) 27:261–70. doi: 10.1136/bmjqs-2016-006399
35. Adair KC, Quow K, Frankel A, Mosca PJ, Profit J, Hadley A, et al. The improvement readiness scale of the SCORE survey: A metric to assess capacity for quality improvement in healthcare. BMC Health Serv Res. (2018) 18:975. doi: 10.1186/s12913-018-3743-0
36. Maslach C, Jackson S. Maslach Burnout Inventory. Palo Alto, CA: Consulting Psychologists Press, Inc. (1981).
37. Sexton JB, Adair KC, Profit J, Milne J, McCulloh M, Scott S, et al. Perceptions of institutional support for “second victims” are associated with safety culture and workforce well-being. Jt Comm J Qual Patient Saf . (2021) 47:306–12. doi: 10.1016/j.jcjq.2020.12.001
38. Sexton JB, Adair KC, Profit J, Bae J, Rehder K, Gosselin T, et al. Safety culture and workforce well-being associations with positive leadership WalkRounds. Jt Comm J Qual Patient Saf . (2021) 47:403–11. doi: 10.1016/j.jcjq.2021.04.001
39. Turner EL, Li F, Gallis JA, Prague M, Murray DM. Review of recent methodological developments in group-randomized trials: part 1-design. Am J Public Health. (2017) 107:907–15. doi: 10.2105/AJPH.2017.303706
40. Rehder KJ, Adair KC, Hadley A, McKittrick K, Frankel A, Leonard M, et al. Associations between a new disruptive behaviors scale and teamwork, patient safety, work-life balance, burnout, and depression. Jt Comm J Qual Patient Saf . (2020) 46:18–26. doi: 10.1016/j.jcjq.2019.09.004
41. Dyrbye LN, Shanafelt TD, Gill PR, Satele DV, West CP. Effect of a professional coaching intervention on the well-being and distress of physicians: A pilot randomized clinical trial. JAMA Intern Med. (2019) 179:1406–14. doi: 10.1001/jamainternmed.2019.2425
42. Rehder K, Adair KC, Sexton JB. The science of health care worker burnout: assessing and improving health care worker wellbeing. Arch Pathol Lab Med. (2021) 145:1095–109. doi: 10.5858/arpa.2020-0557-RA
43. Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. (2020) 66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007
44. West CP, Dyrbye LN, Satele DV, Shanafelt TD. Colleagues meeting to promote and sustain satisfaction (COMPASS) groups for physician well-being: A randomized clinical trial. Mayo Clin Proc. (2021) 96:2606–14. doi: 10.1016/j.mayocp.2021.02.028
45. Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. (2009) 302:1284–93. doi: 10.1001/jama.2009.1384
46. Dyrbye LN, Gill PR, Satele DV, West CP. Professional coaching and surgeon wellbeing. A randomized controlled trial. Ann Surg. (2022). doi: 10.1097/SLA.0000000000005678. [Epub ahead of print].
47. National Academies of Sciences E. Taking Action Against Clinician Burnout: A Systems Approach to Professional Wellbeing. Washington, DC: Washington, DC: National Academies Press (US). (2019).
48. Lebares CC, Greenberg AL, Ascher NL, Delucchi KL, Reilly LM, van der Schaaf M, et al. Exploration of individual and system-level well-being initiatives at an academic surgical residency program: a mixed-methods study. JAMA Netw Open. (2021) 4:e2032676. doi: 10.1001/jamanetworkopen.2020.32676
49. Bianchi R, Laurent E. Emotional information processing in depression and burnout: an eye-tracking study. Eur Arch Psychiatry Clin Neurosci. (2015) 265:27–34. doi: 10.1007/s00406-014-0549-x
50. Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. J Pers Soc Psychol. (2008) 95:1045–62. doi: 10.1037/a0013262
51. Fredrickson BL, Kurtz LE. Cultivating Positive Emotions to Enhance Human Flourishing. In: Applied Positive Psychology: Improving Everyday Life, Health, Schools, Work, and Society. New York, NY, US: Routledge/Taylor & Francis Group. (2011). p. 35–47.
52. Fredrickson BL, Mancuso RA, Branigan C, Tugade MM. The undoing effect of positive emotions. Motiv Emot. (2000) 24:237–58. doi: 10.1023/A:1010796329158
53. Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional wellbeing. Psychol Sci. (2002) 13:172–5. doi: 10.1111/1467-9280.00431
54. Fredrickson BL, Levenson RW. Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cogn Emot. (1998) 12:191–220. doi: 10.1080/026999398379718
55. Halpern SD, Harhay MO, Saulsgiver K, Brophy C, Troxel AB, Volpp KG. A pragmatic trial of E-cigarettes, incentives, and drugs for smoking cessation. N Engl J Med. (2018) 378:2302–10. doi: 10.1056/NEJMsa1715757
56. Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. (2005) 82:222S−5S. doi: 10.1093/ajcn/82.1.222S
57. Crichton GE, Howe PR, Buckley JD, Coates AM, Murphy KJ, Bryan J. Long-term dietary intervention trials: critical issues and challenges. Trials. (2012) 13:111. doi: 10.1186/1745-6215-13-111
58. Miller BML, Brennan L. Measuring and reporting attrition from obesity treatment programs: a call to action! Obes Res Clin Pract. (2015) 9:187–202. doi: 10.1016/j.orcp.2014.08.007
59. Dalle Grave R, Calugi S, Compare A, El Ghoch M, Petroni ML, Tomasi F, et al. Weight loss expectations and attrition in treatment-seeking obese women. Obes Facts. (2015) 8:311–8. doi: 10.1159/000441366
60. Bahadir A, Iliaz S, Yurt S, Ortakoylu MG, Bakan ND, Yazar E. Factors affecting dropout in the smoking cessation outpatient clinic. Chron Respir Dis. (2016) 13:155–61. doi: 10.1177/1479972316629953
61. Colombo O, Ferretti VVV, Ferraris C, Trentani C, Vinai P, Villani S, et al. Is drop-out from obesity treatment a predictable and preventable event? Nutr J. (2014) 13:13. doi: 10.1186/1475-2891-13-13
62. Cannon MJ, Masalovich S, Ng BP, Soler RE, Jabrah R, Ely EK, et al. Retention among participants in the national diabetes prevention program lifestyle change program, 2012-2017. Diabetes Care. (2020) 43:2042–9. doi: 10.2337/dc19-2366
63. Neve MJ, Collins CE, Morgan PJ. Dropout, nonusage attrition, and pretreatment predictors of nonusage attrition in a commercial web-based weight loss program. J Med Internet Res. (2010) 12:e69. doi: 10.2196/jmir.1640
64. Tawfik DS, Shanafelt TD, Dyrbye LN, Sinsky CA, West CP, Davis AS, et al. Personal and professional factors associated with work-life integration among US physicians. JAMA Netw Open. (2021) 4:e2111575. doi: 10.1001/jamanetworkopen.2021.11575
Keywords: emotional exhaustion, wellbeing, burnout, wellbeing intervention, bite-sized wellbeing, positive psychology intervention, WISER
Citation: Sexton JB, Adair KC, Cui X, Tawfik DS and Profit J (2022) Effectiveness of a bite-sized web-based intervention to improve healthcare worker wellbeing: A randomized clinical trial of WISER. Front. Public Health 10:1016407. doi: 10.3389/fpubh.2022.1016407
Received: 29 August 2022; Accepted: 07 November 2022;
Published: 08 December 2022.
Edited by:
Markus M. Luedi, Bern University Hospital, SwitzerlandReviewed by:
Mariana Kaiseler, Leeds Beckett University, United KingdomThomas Heidegger, Bern University Hospital, Switzerland
Copyright © 2022 Sexton, Adair, Cui, Tawfik and Profit. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: J. Bryan Sexton, QnJ5YW4uU2V4dG9uQER1a2UuZWR1
 J. Bryan Sexton
J. Bryan Sexton Kathryn C. Adair
Kathryn C. Adair Xin Cui
Xin Cui Daniel S. Tawfik
Daniel S. Tawfik Jochen Profit3,4
Jochen Profit3,4