
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Public Health , 24 October 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1010582
 Shengyi Min1†
Shengyi Min1† Yuxuan Zhou1†
Yuxuan Zhou1† Yuxuan Sun1
Yuxuan Sun1 Jiaquan Ye1
Jiaquan Ye1 Yongfei Dong2,3
Yongfei Dong2,3 Xichao Wang2,3
Xichao Wang2,3 Zhemin Zhou1
Zhemin Zhou1 Hanyu Zhou4*
Hanyu Zhou4* Heng Li1*
Heng Li1*This study described the knowledge, attitude, practice regarding antimicrobial resistance (AMR) among medical students between 2017 and 2022 in East China. A questionnaire-based survey was conducted with a total of 1,066 respondents. We highlighted that the undergraduates had a significant increase in the knowledge of antimicrobial resistance during the 5 years from 2017 to 2022 (p < 0.001). The majority of the assertions about the AMR were correctly identified by respondents. However, gaps were still observed in the issues of antimicrobial targets and bacterial transmission. In addition, overconfident attitudes and inappropriate behaviors of antimicrobial overuse and misuse were observed in the respondents. A number of 30.2% to 45.2% of the respondents asserted that there is no risk of AMR as long as the antimicrobials are taken correctly, and a proportion of the students (25.3% in 2022; 69.3% in 2017, p < 0.001) declared to buy antimicrobials from friends or family members to treat the same illness. Finally, spearman correlation coefficient was enrolled to compare the correlation of the student's KAP. Results showed that the students' knowledge of antimicrobials had a correlation with attitude (p = 0.0126) and practice (p < 0.001), suggesting that public education on knowledge could influence the behaviors among the medical students. Taken all together, our findings show a need to strengthen the medical students' cogitation on antimicrobial attitude and practice of appropriate usage as an essential strategy to reduce intractable public health problems. Additional curriculum reforms will be needed to add more specific AMR-related lectures to raise awareness amongst medical students in China.
Antimicrobial resistance (AMR) has emerged as one of the most pressing challenges over the last two decades (1). World Health Organization endorsed a global action plan in May 2015 to provide safer antimicrobials for the prevention and treatment of infectious diseases (2). However, AMR continues to spread in many parts of the world, including developing countries such as China, Pakistan, and India (3–6). As one of the world's largest producers and consumers of antimicrobials, the Chinese government has implemented a number of policy measures e.g., the “National Action Plan to Tackle Bacterial Resistance (NAPCBR, 2016–2020),” to address antimicrobial education in hospitals, community clinics, agricultural industry, and medical universities (7).
The purchase of antimicrobials is regulated by well-established legislation in China that antimicrobials can only be dispensed under the formal prescription from a medical practitioner (8). However, multidrug-resistant and extensively drug-resistant (XDR) bacterial strains were reported in the hospital (9). According to the China Antimicrobial Resistance Surveillance Trial Program (https://www.chinets.com), the isolation frequency of carbapenem-resistant Klebsiella pneumoniae had rapidly climbed from 2.9% in 2005 to 24.4% in 2021 (10). Additionally, extended-spectrum methicillin-resistant Staphylococcus aureus was detected in China and other countries as the emerging threat to public health (11–13).
To address the issues of AMR, previous studies have concentrated on the gap in knowledge, attitude, and practice (KAP) regarding antimicrobials among students (14–17). Previously, researchers investigated the KAP of Chinese undergraduates and discovered a large deficit in the knowledge section addressing the appropriate use of antimicrobials (15). The medical students' knowledge and attitude also drive their doctors' self-prescription of unneeded antimicrobials (18). Thus, advising future doctors and medical students on antimicrobial usage and dosage constitutes an important strategy to reduce bacterial drug resistance.
The Chinese NAPCBR (2016–2020) has counseled the public on appropriate AMR issues and antimicrobial prescribing for many years (7). To evaluate the awareness of antimicrobial resistance in medical education during the past 5-year, this study was conducted to investigate the KAP of medical students between 2017 and 2022. We hypothesized that the years of action on the necessity of antimicrobials had aided in raising awareness amongst medical students in East China.
This survey was questionnaire-based and aimed to assess the awareness of KAP among Chinese medical undergraduates between 2017 and 2022 in Yangtze River Delta region in eastern China. We selected one representative medical university in Suzhou as the research object. The sample size was measured by the online sample size calculator (https://www.calculator.net/) with a 50% population proportion, 5% margin of error, and 95% confidence level. The questionnaire was delivered to the students via Tencent forms on social media applications. The students were advised to fill out the questionnaire by clicking the link. A total of 1066 respondents were enrolled in this study with a response rate of 88.83% (1,066/1,200). The first round of the survey obtained 564 respondents during August and November 2017. The second round collected 502 feedbacks between August and October 2022 with either online or face-to-face interviews. All the respondents joined in with no incentives and signed the informed consents. Detailed characteristics were described in Table 1.
A structured questionnaire was prepared by reviewing questionnaires of validated surveys that were previously reported and was customized in such a way to reflect issues relevant to China (14–17). The questionnaire was divided into five sections with subdivided components. The first section was basic information about the students, gender, age and education level. The second section contained two multiple choices on the knowledge of AMR. The third section included eight questions of knowledge which were validated by WHO report and peer studies (2, 15). The fourth section recorded 12 questions which were set in the part of attitude relating to the severity of antimicrobial abuse in healthcare and the impact and responsibility of reduction based on the validated surveys used in both China and other countries (15, 17, 19–21). Finally, the fifth section of the questionnaire included five questions regarding the practices of antimicrobial overuse, misuse, and AMR transmission (Supplementary materials-questionnaire) (15, 17, 21). Questionnaire validation was ensured by an expert team (2 professors and 2 physicians) and 5 undergraduate medical students. The questionnaire was translated into Chinese and improved the accuracy on advice of relevant experts from the field of statistics and epidemiology before being finalized.
Grading standards were used to give each question specific scores. Standard answers such as “true” to “false” and “agree” to “disagree” were simultaneously determined corresponding to the suggestions from WHO (21). The grading standards were validated by similar surveys that were previously used in other research (15, 20). Specifically, 3 or 0 points were graded to the single or multiple-choice options and 1 to 5 points were allocated for five-answer responses as agree, agree slightly, neutral, disagree slightly, and disagree, respectively. All the questions and grading standards are presented in Supplementary materials-grading standard.
The grading scores were typed into SPSS 26.0 (IBM SPSS Statistics 26.0) and Graphpad prism 7 for statistical analysis (GraphPad Software Inc., San Diego, CA). For the data type of frequencies and percentages, descriptive statistics were used and were presented in tables. The median and IQR (Interquartile range defines the middle 50% of values from “lowest to highest” when ordered) were used to describe the data of attitude as appropriate. The difference of scores was determined through the Mann–Whitney statistical tests with p < 0.001 considered statistically significant (Figure 1). The categorical variables (such as the years) were done using Chi-square test to assess the association among these students toward antimicrobials (Table 2). Then rank sum test was enrolled for the analysis via Mann-Whitney U-test (Table 3). Finally, Spearman correlation coefficient was enrolled to compare the correlation of the student's knowledge, attitudes and practices between 2017 and 2022 with p < 0.001 as significant.
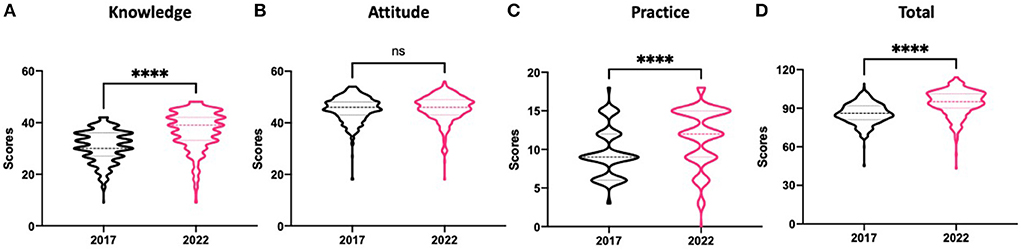
Figure 1. The grading graphs of respondents' knowledge, attitude, and practice on antimicrobials. Scores were calculated according to the grading standards and statistical test by Mann–Whitney with p-value < 0.001 (****) was considered statistically significant. Significances were observed in the scores of knowledge, practices and total respondents. (A) Knowledge scores were calculated based on the questions in Table 2A. Significances were observed among the respondents between 2017 and 2022 (p < 0.001). (B) Attitude scores were analyzed by evaluating the questions in Tables 2B and 3. No differences were found between the two groups (p = 0.2805). (C) Practice scores were computed based on the questions in Table 2C with significant differences detected (p < 0.001). (D) Total scores were statistically counted according to all the questions in Tables 2 and 3. Significances were observed among the two groups with regard to antimicrobial resistance (p < 0.001).
The present study assessed the knowledge, attitudes, and practices of medical undergraduates toward AMR between 2017 and 2022. In 2017, 564 medical students responded to the poll, with 63.3 percent of them being female and a median age of 21. In 2022, the second round of surveys included 502 participants, 59.2 percent of whom were female and had a median age of 21 (Table 1).
Table 2A shows the results of the knowledge assessment. The majority of the assertions about the emergence, transmission, and detriment of antimicrobial resistance were correctly identified by respondents. However, gaps in the issues contributing to AMR, such as Q1 and Q7, were still observed in our study, indicating that the confusion regarding the consequences of antimicrobial targets was still present among these medical students. “Antimicrobial resistance occurs when your body becomes resistant to antimicrobials and they no longer work as well,” according to WHO, is a false assertion (21). Only 67.3% and 45.6% of the respondents chose the correct answer in 2022 and 2017 (p < 0.001), respectively, down from the prior rate of 76% published by WHO in 2016. On the other hand, 76.5% and 77.8% of the respondents considered that bacteria could be transmitted from person to person, accompanied by a proportion of students holding the opposite opinion, indicating the importance of educating the students with regard to the basic knowledge of antimicrobial resistance and bacterial transmission.
The perspectives of the respondents concerning antimicrobial use and AMR transmission are shown in Tables 2B and 3. In 2017, over two-thirds (73.4%) of respondents agreed on antimicrobial abuse in China, and 77.5% considered that antimicrobials were widely used in agriculture. However, the survey of 2022 witnessed a dramatic drop in statistics that fewer than half of the students (44.6%) believed antimicrobials were applied broadly in agriculture and food-producing animals (p < 0.001). Following that, particular attitudes were evaluated to illustrate the variations in antimicrobial resistance. A majority of respondents (76.8% in 2022 and 77.5% in 2017) agreed on the current abuse of antimicrobials and would like to take responsibility for reducing them. However, still 30.2 to 45.2% (strongly agree% + agree%) of the respondents firmly asserted that there is no risk of antimicrobial resistance as long as the antimicrobials are taken correctly (Table 3). Significance was observed in other attitude responses such as the impact of AMR on health, and the prescription of antimicrobials, suggesting the present problems of overconfidence and inappropriate attitudes (Table 3, p < 0.001).
The respondents' practice on AMR was evaluated in Table 2C. Up to 80.9% and 77.1% of respondents claimed that they received antimicrobials from doctors in 2022 and 2017, respectively. Furthermore, only a tiny proportion of participants (4.8% in 2022; 6.2% in 2017) stated they would use antimicrobials to treat the common cold, which is not recommended by WHO. In addition, around 74.1% and 73.4% expressed their willingness to take all the antimicrobials as prescribed after they started therapy, as advised by WHO. However, a considerable proportion of respondents still contemplate buying antimicrobials on their own or through a doctor if they believe they are suffering from the same condition as previously (25.3% in 2022; 69.3% in 2017, p < 0.001), and some even buy antimicrobials from friends or family members to treat the same illness (28.9% in 2022; 66.8% in 2017, p < 0.001).
For current and future stakeholders, particularly university students in the fields of medicine and medical sciences, an overall awareness of the concept of AMR as well as KAP of underlying specific concerns such as proper usage is essential. Therefore, the grading standards were enrolled to evaluate the general KAP of students between 2017 and 2022. The scores were calculated according to the grading standards and statistical test by Mann–Whitney with p-value < 0.001 was considered statistically significant. Significances were observed in the scores of knowledge (p < 0.001), practices (p < 0.001) and total respondents (p < 0.001). The present results revealed that the knowledge and practice scores had significantly improved in 2022 (p < 0.001), whereas there was no significance in the attitude section compared to 2017 (p = 0.2805, Figure 1).
In addition, we calculated the correlation of the student's knowledge, attitudes and practices among all respondents. Results showed that the students' knowledge of antimicrobials had a correlation with attitude (p = 0.0126) and practice (p < 0.001), suggesting that public education on knowledge could influence the behaviors among the medical students. Similar surveys were conducted in China and other countries focusing on public education to improve the irrational and indiscriminate use of antimicrobials in the community. The public education that provides guidelines for medical practitioners may promote the cautious and rational use of antimicrobials (15, 22).
Antimicrobial resistance was reported to be transferred through agriculture, food-producing animals, irrational prescription, and others (23–25). Therefore, utilizing the medical school's key position in public education, introducing pharmaceutical lectures, and conducting publicity outreach would effectively boost the knowledge of antimicrobial resistance in universities (22). On the other hand, there was a small proportion of the respondents who believed that they were not at risk of AMR infection. Antimicrobials, however, are responsible for more than half of all medical adverse effects, according to the China Adverse Reaction Monitoring Center (26). The increasing cases of antimicrobial-resistant bacteria caused by improper use of antimicrobials have also been observed in recent years (27). Patients may be in danger of contracting antimicrobial-resistant bacteria if they seek medications for common cold and receive them without a prescription. Inadequate dosage, incomplete treatment, and drug abuse contribute to the emergence of AMR, which is a wake-up call for us to recognize the worldwide significance of antimicrobial resistance.
Another interesting research finding is that undergraduates' awareness of antimicrobial resistance has greatly risen over the 5 years from 2017 to 2022. This finding could be attributed to the following factors; Notably, the National Action Plan for Containment of Bacterial Resistance (2016–2020) emphasized the necessity of enhancing the medical knowledge popularization in the universities and raising the awareness of antimicrobial resistance as well as its responsible use (28, 29). Antimicrobial resistance is being widely debated and published on social media, which may enhance public awareness among university students, in addition to the identification of the topic within the university context and its implementation into the micro curriculum (30).
This study has some limitations. First, the results of KAP among medical undergraduates in Suzhou, East China, are limited to the study population, which may cause a negative impact on the generalizability of the study findings. Second, the limited number of questions cannot adequately capture all aspects of antimicrobial resistance. Third, this study aimed to understand the general perceptions of KAP among medical undergraduates, without taking into account the direct impact of other factors such as microbiology and pharmacology courses on cognitive outcomes. Despite these limitations, the present findings provide important information for evaluating and improving the knowledge, attitude, and practice of medical undergraduate students toward antimicrobial use.
We highlight those medical students surveyed had significantly increased the knowledge of antimicrobial resistance during the 5 years from 2017 to 2022 (p < 0.001). However, overconfident attitudes and inappropriate behaviors of AMR were still observed in the present respondents. Gaps were still observed in the issues of antimicrobial targets and bacterial transmission, indicating the importance of educating the students with regard to AMR. Additional curriculum reforms will be needed to add more specific AMR-related lectures and clinical practices to raise awareness amongst medical students in East China. The development of institutional treatment guidelines on antimicrobial resistance, and restrictions on self-prescription of unneeded antimicrobials were also urgent to reduce bacterial drug resistance in China.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethics Committees of Suzhou Medical College in Jiangsu Province, China. The patients/participants provided their written informed consent to participate in this study.
SM, HL, ZZ, and HZ wrote the main manuscript text. SM, YZ, YS, and JY prepared the tables. YD and XW analyzed the statistical data. All authors reviewed the manuscript.
This work was supported by grants from Extracurricular Scientific Research Project for Students of Suzhou Medical College (Pasteurien College), and Suzhou Science and Technology Project (N316460121).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1010582/full#supplementary-material
1. Dadgostar P. Antimicrobial resistance: Implications and costs. Infect Drug Resist. (2019) 12:3903–10. doi: 10.2147/IDR.S234610
2. Mendelson M, Matsoso MP. The World Health Organization Global Action Plan for antimicrobial resistance. S Afr Med J. (2015) 105:325. doi: 10.7196/SAMJ.9644
3. Chatterjee S, Hazra A, Chakraverty R, Shafiq N, Pathak A, Trivedi N, et al. Knowledge, attitude, and practice survey on antimicrobial use and resistance among Indian clinicians: A multicentric, cross-sectional study. Perspect Clin Res. (2022) 13:99–105. doi: 10.4103/picr.PICR_21_20
4. Bhardwaj K, Shenoy S, Baliga S, Unnikrishnan B, Baliga BS. Knowledge, attitude, and practices related to antibiotic use and resistance among the general public of coastal south Karnataka, India–A cross-sectional survey. Clin Epidemiol Glob Health. (2021) 11:100717. doi: 10.1016/j.cegh.2021.100717
5. Hayat K, Fatima N, Umer MF, Khan FU, Khan FU, Najeeb ZUR, et al. Understanding of future prescribers about antimicrobial resistance and their preparedness towards antimicrobial stewardship activities in Pakistan: Findings and implications. Front Pharmacol. (2022) 13:771083. doi: 10.3389/fphar.2022.771083
6. Hayat K, Jamshed S, Rosenthal M, Haq NU, Chang J, Rasool MF, et al. Understanding of pharmacy students towards antibiotic use, antibiotic resistance and antibiotic stewardship programs: A cross-sectional study from Punjab, Pakistan. Antibiotics (Basel). (2021) 10:66. doi: 10.3390/antibiotics10010066
7. Ying GG, He LY, Ying AJ, Zhang QQ, Liu YS, Zhao JL. China must reduce its antibiotic use. Environ Sci Technol. (2017) 51:1072–3. doi: 10.1021/acs.est.6b06424
8. Zhang T, Lambert H, Zhao L, Liu R, Shen X, Wang D, et al. Antibiotic stewardship in retail pharmacies and the access-excess challenge in China: A policy review. Antibiotics (Basel). (2022) 11:141. doi: 10.3390/antibiotics11020141
9. Wang Y, Lu D, Jin Y, Wang H, Lyu B, Zhang X, et al. Extensively drug-resistant (XDR) Salmonella typhi outbreak by waterborne infection - Beijing Municipality, China, January-February 2022. China CDC Wkly. (2022) 4:254–8. doi: 10.46234/ccdcw2022.062
10. Gao L, Lv Y, Li Y. Analysis of the drug resistance of carbapenem-resistant Klebsiella pneumoniae in the China antimicrobial resistance surveillance trial program, 2007-2018. Microb Drug Resist. (2020) 26:944–50. doi: 10.1089/mdr.2019.0299
11. Noorulamin MN, Zarafsah ZB, Janjua A, Iqbal A, Humerah S, Shaiq PA. Future trends in the treatment of MRSA in Pakistan. J Islamabad Med Dental College. (2022) 11:96–102. doi: 10.35787/jimdc.v11i2.672
12. Singhal T, Rodrigues C, Soman R, Wattal C, Swaminathan S, Nambi S, et al. Treatment of MRSA infections in India: Clinical insights from a Delphi analysis. Indian J Med Microbiol. (2022) 40:35–45. doi: 10.1016/j.ijmmb.2021.11.005
13. Chen Y, Sun L, Ba X, Jiang S, Zhuang H, Zhu F, et al. Epidemiology, evolution and cryptic susceptibility of methicillin-resistant Staphylococcus aureus in China: a whole-genome-based survey. Clin Microbiol Infect. (2022) 28:85–92. doi: 10.1016/j.cmi.2021.05.024
14. Hu Y, Wang X, Tucker JD, Little P, Moore M, Fukuda K, et al. Knowledge, attitude, and practice with respect to antibiotic use among Chinese medical students: A multicentre cross-sectional study. Int J Environ Res Public Health. (2018) 15:1165. doi: 10.3390/ijerph15061165
15. Huang Y, Gu J, Zhang M, Ren Z, Yang W, Chen Y, et al. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ. (2013) 13:163. doi: 10.1186/1472-6920-13-163
16. Lv B, Zhou Z, Xu G, Yang D, Wu L, Shen Q, et al. Knowledge, attitudes and practices concerning self-medication with antibiotics among university students in western China. Trop Med Int Health. (2014) 19:769–79. doi: 10.1111/tmi.12322
17. Wang Y, Guo F, Wei J, Zhang Y, Liu Z, Huang Y. Knowledge, attitudes and practices in relation to antimicrobial resistance amongst Chinese public health undergraduates. J Glob Antimicrob Resist. (2020) 23:9–15. doi: 10.1016/j.jgar.2020.07.023
18. Lin L, Fearon E, Harbarth S, Wang X, Lu C, Zhou X, et al. Decisions to use antibiotics for upper respiratory tract infections across China: a large-scale cross-sectional survey among university students. BMJ Open. (2020) 10:e039332. doi: 10.1136/bmjopen-2020-039332
19. André M, Vernby A, Berg J, Lundborg CS. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J Antimicrob Chemother. (2010) 65:1292–6. doi: 10.1093/jac/dkq104
20. Awad AI, Aboud EA. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS ONE. (2015) 10:e0117910. doi: 10.1371/journal.pone.0117910
21. World Health Organization. Antibiotic resistance: multi-country public awareness survey WHO Library (2015).
22. Ogunnigbo O, Nabiryo M, Atteh M, Muringu E, Olaitan OJ, Rutter V, et al. Exploring the antimicrobial stewardship educational needs of healthcare students and the potential of an antimicrobial prescribing app as an educational tool in selected African countries. Antibiotics (Basel). (2022) 11:691. doi: 10.3390/antibiotics11050691
23. Machowska A, Stålsby Lundborg C. Drivers of irrational use of antibiotics in Europe. Int J Environ Res Public Health. (2018) 16:27. doi: 10.3390/ijerph16010027
24. Patel SJ, Wellington M, Shah RM, Ferreira MJ. Antibiotic stewardship in food-producing animals: Challenges, progress, and opportunities. Clin Ther. (2020) 42:1649–58. doi: 10.1016/j.clinthera.2020.07.004
25. Thanner S, Drissner D, Walsh F. Antimicrobial resistance in agriculture. mBio. (2016) 7:e02227–15. doi: 10.1128/mBio.02227-15
26. Yan Z, Feng Z, Jiao Z, Chen C, Wang G, Feng D. The severity of adverse drug reactions and their influencing factors based on the ADR monitoring center of Henan Province. Sci Rep. (2021) 11:20402. doi: 10.1038/s41598-021-99908-3
27. Liu X, Cui D, Li H, Wang Q, Mao Z, Fang L, et al. Direct medical burden of antimicrobial-resistant healthcare-associated infections: empirical evidence from China. J Hosp Infect. (2020) 105:295–305. doi: 10.1016/j.jhin.2020.01.003
28. Xiao Y. Antimicrobial stewardship in China: Systems, actions and future strategies. Clin Infect Dis. (2018) 67:S135–41. doi: 10.1093/cid/ciy641
29. Yin J, Wang Y, Xu X, Liu Y, Yao L, Sun Q. The progress of global antimicrobial resistance governance and its implication to China: A review. Antibiotics (Basel). (2021) 10:1356. doi: 10.3390/antibiotics10111356
Keywords: antimicrobial resistance, medical education, antimicrobial use, knowledge, attitude and practice study, AMR awareness
Citation: Min S, Zhou Y, Sun Y, Ye J, Dong Y, Wang X, Zhou Z, Zhou H and Li H (2022) Knowledge, attitude, and practice associated with antimicrobial resistance among medical students between 2017 and 2022: A survey in East China. Front. Public Health 10:1010582. doi: 10.3389/fpubh.2022.1010582
Received: 03 August 2022; Accepted: 07 October 2022;
Published: 24 October 2022.
Edited by:
Suneela Garg, University of Delhi, IndiaReviewed by:
Jacob Kwada Kwaga, Ahmadu Bello University, NigeriaCopyright © 2022 Min, Zhou, Sun, Ye, Dong, Wang, Zhou, Zhou and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heng Li, aGxpQHN1ZGEuZWR1LmNu; Hanyu Zhou, bXJ6aHkxOTkyQDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.