- 1Università Cattolica del Sacro Cuore, Rome, Italy
- 2Azienda Ospedaliera San Camillo Forlanini, Rome, Italy
- 3DiagnostiCare ONLUS, Rome, Italy
- 4Scuola di Specializzazione in Psicologia della Salute–Università degli Studi di Roma “La Sapienza”, Rome, Italy
- 5Health Management IRCCS San Raffaele Roma, Rome, Italy
- 6Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
- 7Department of Medicine and Surgery, University of Perugia, Perugia, Italy
Cardiovascular diseases (CVDs) represent a major threat to health and primary prevention outstands as the most effective instrument to face this issue, addressing multiple risk factors at a time and influencing behavioral patterns. Community nurses have been involved in many interdisciplinary prevention activities, resulting in effective control of CV risk factors. We conducted a pilot study aiming at describing the impact on the CV risk profile of an 18-month interdisciplinary intervention on lifestyle habits. From September 2018 to May 2020, four general practitioners (GPs) working in the Roman neighborhood of Torresina recruited patients having a cardiovascular risk score (CRS) equal to or higher than 3% and lower than 20%; those patients were included in a nutritional, physical, and psychological counseling program. Assessments of patients' health status were led at baseline, 6, 12, and 18 months by a nutritionist, a physiotherapist, a psychologist, their GPs, and a community nurse. The CRS was estimated at every examination, based on the Italian Progetto Cuore algorithm. A total of 76 patients were included (mean age of 54.6 years; 33 men and 43 women). Mean CRS showed a significant reduction between baseline and 12 months (from 4.9 to 3.8); both total cholesterol and systolic blood pressure (SBP) significantly decreased at 6 months of follow-up (respectively, from 211.1 to 192 and from 133.1 to 123.1). Nonetheless, the reduction was later maintained only for SBP. However, during the last 6 months of the intervention, the COVID-19 pandemic broke out, thus, it is not possible to know how much the results achieved at 18 months were influenced by the restrictive measures introduced by the Italian government. When stratifying according to the presence of hypertension/diabetes and physical activity, no differences in the CRS could be highlighted between the two groups. Our pilot study proved that an interdisciplinary counseling intervention program can improve CV risk profile and could be further spread to people that, according to their CRS, would benefit more from changes in lifestyles.
1. Introduction
Cardiovascular diseases (CVDs) are a group of disorders affecting the heart and blood vessels (1), which represent the leading cause of death, premature death, and reduced quality of life globally: in 2019, they were responsible for an estimated 17.9 million deaths, among which 3.9 million in Europe alone (1). It has been estimated that one person dies every 36 s in the United States due to CVDs (2), with ischemic heart disease and stroke being the most frequent conditions (3). Moreover, not only do CVDs determine a significant and avoidable number of human lives lost, but they also outline a substantial economic burden, which cost the EU €210 billion a year in 2017, considering direct healthcare costs, productivity losses, and informal care of people with CVD (2).
“Progetto Cuore” is an Italian epidemiological project financed by the Italian Ministry of Health and aimed at recording CV events and the distribution of CV risk factors, in order to identify strategies to lower CV risk and consequent morbidity and mortality (4). In this regard, influencing behavioral patterns through primordial and primary prevention has been appointed as a decisive strategy (5, 6). As described in a systematic review by Sisti et al. addressing more than a single risk factor at a time can be more effective in CV risk reduction, particularly in individuals at risk: interventions on diet and physical activity, together with quitting tobacco use, are the ones that impact the most (7, 8).
Primary care is a suitable setting to identify patients who might be at risk of developing CVDs (9). Risk stratification is intended to target the intensity of the therapeutic or preventive measures to the severity of the patient's risk (10) and is complementary to the preventive population approach, which deals with population-wide strategies independently of individual risk (11). General practitioners (GPs) can assess CV risk by using validated risk scores (9, 10), such as SCORE (Europe) (12), Framingham (13), and ASCVD (US) (14), based on different combinations of modifiable risk factors that are also targets for prevention (15–19). By means of risk stratification, cardiovascular risk scores (CRS) allow one to plan lifestyle interventions, for instance, physical activity, diet, and smoking interventions (15). In several cases, interdisciplinary prevention activities have been coordinated by community nurses, creating bridges between primary care and hospitals (20): virtuous experiences have proved that primary prevention can be led outside of specialist centers and it can result in significant improvements in lifestyles and more effective control of risk factors (20).
This pilot study aims at describing the impact of a 12-month prevention and promotion, interdisciplinary program on lifestyle habits, and CV risk assessed through the CRS developed by “Progetto Cuore.” The intervention was led in a primary care setting in the Roman neighborhood of Torresina.
2. Materials and methods
2.1. Study design and population
“Cardiovascular Risk Prevention in the Neighborhood Torresina” is an 18-month interdisciplinary pilot pre-post observational study conducted among healthy individuals in the Roman neighborhood of Torresina [~5,000 inhabitants (21)] from December 2018 to May 2020.
The sample was recruited in September 2018 among the patients of the four GPs working in the Torresina neighborhood. The study envisaged the organization of an information campaign in order to sponsor the scientific initiative through the websites of the Torresina neighborhood and of the DiagnostiCare ONLUS Association, involved in the project. Posters about the project and the selection criteria of the participants were hung in the medical practices involved and in the most frequented strategic points of the neighborhood; moreover, flyers with the same information were placed in letterboxes in the neighborhood. Participants were recruited among all men and women aged between 35 and 69 years of age who presented at the GP practices in September 2018: among them, those who consented to enroll voluntarily and fulfilled the inclusion criteria took part in the study. The fact that a commitment was required for a medium to a long time further contributed to the self-selection of participants.
2.2. Parameters sampling
To estimate CRS, standardized methods were used to assess parameters according to “Progetto Cuore.” To standardize the measurements, blood samples were taken in a laboratory specifically identified for the study.
2.2.1. Fasting blood glucose
To determine fasting blood glucose, a blood venous withdrawal was carried out after at least a 12-h fasting. To be diagnosed with diabetes, the patient must have a fasting blood sugar level equal to or >126 mg/dL in 2 or more consecutive tests within a week or be treated with oral hypoglycemic drugs or insulin.
2.2.2. Blood pressure
Systolic blood pressure (SBP) was measured according to 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guidelines (22). It was determined two times within few minutes. The blood pressure value was calculated as the mean of the two readings.
2.2.3. Total, HDL, and LDL cholesterol and triglycerides
To determine total, high-density lipoprotein (HDL), and low-density lipoprotein (LDL) cholesterol and triglycerides, a blood venous withdrawal was carried out after at least a 12-h fasting.
2.2.4. Smoking habit
A smoker was defined as a person who smokes tobacco regularly every day (even only one cigarette) or has quitted for <12 months.
2.2.5. Physical activity
Physical activity was defined as having performed at least 150 min of moderate-intensity aerobic physical exercise, at least 75 min of vigorous-intensity aerobic physical exercise, or an equivalent combination of moderate- and vigorous-intensity activity throughout the week.
2.2.6. Alcohol consumption
Moderate drinkers were defined as those limiting their intake to 2 drinks or less per day for men and 1 drink or less per day for women when alcohol was consumed (23). Heavy drinkers were defined as men consuming more than 4 drinks on any day or more than 14 drinks per week, or women consuming more than 3 drinks on any day or more than 7 drinks per week (23).
2.2.7. Cardiovascular risk score determination
Global absolute CV risk is a parameter that defines the probability (in %) of the occurrence of a major CV event in the following 10 years in the adult population aged between 35 and 69 years. The software “Cuore.exe” (24), developed by the Italian National Institute of Health (ISS—Istituto Superiore di Sanità), was employed to determine the individual CRS, which is the best estimate of the global absolute CV risk. The software refers to 8 parameters, namely, age, gender, diabetes, smoking habit, SBP, total and HDL cholesterol, and antihypertensive drugs.
2.3. Data sources and management
All measurements, including the determination of the individual CRS, were carried out at baseline and at 6, 12, and 18 months by GPs and a community nurse.
Total blood glucose and cholesterol were assessed through laboratory testing. With respect to blood glucose, patients were not submitted to laboratory testing at baseline as GPs were already aware of their patient's status with respect to diabetes, thus, being allowed to gather the relevant information on the Cuore.exe software. Data concerning personal patient information (e.g., age, gender, educational level, profession, marital status, and nationality) and other relevant characteristics and prescriptions (e.g., smoking habits, diet, physical activity, and blood pressure) were collected by both GPs and community nurses. The 2016 “PASSI” questionnaire was used to collect information on lifestyles (25) while the Health Locus of Control (HLC) (26) and the Multidimensional Scale of Perceived Social Support (MSPSS) (27) were used to monitor behavioral changes. Participation in planned activities on lifestyle interventions was recorded by means of weekly diaries. All the information collected was organized in an Excel dataset, managed by the GPs: data were anonymized and identified through a univocal code.
The dataset was then handed over to the Institute of Public Health-Section of Hygiene of the Catholica University of the Sacred Heart of Rome for statistical analysis.
2.4. Health prevention and promotion intervention
The program was composed of three main interventions led by an interdisciplinary team at baseline, 6, and 12 months. Follow-up examinations were carried out at 6, 12, and 18 months.
2.4.1. Intervention 1: Nutritional counseling
The nutritional intervention aimed to convey basic nutrition information, focusing on the correct Mediterranean dietary habits to reduce the risk of CVD. At first, through simple general questions, the level of awareness of the sample population regarding nutrition was measured. Then, the nutritionist explained the different classes of macronutrients and focused on foods that may contribute to increasing or decreasing the risk of CVD. The main topics addressed were body hydration, salt consumption, consumption of saturated and polyunsaturated fatty acids, fruits and vegetables, and alcoholic and soft drinks. Finally, advice and guidance were given on how to shop for groceries, teaching how to read food labels to better evaluate the nutritional information of packaged products. In addition, the nutritionist evaluated weekly nutritional diaries completed by the patients in order to assess and correct the most frequent mistakes.
2.4.2. Intervention 2: Physical activity counseling
Relying on 2010 WHO “Global recommendations on Physical Activity for Health,” a physiotherapist and a motivational coach helped patients to develop an active lifestyle and organized group training activities.
In particular, training meetings were organized to make participants aware of their individual habits and to give advice and information on how to start and develop a training program based on walking.
Furthermore, a motivational coach set meetings to conduct outdoor group workouts and activities in the Torresina neighborhood area. These outdoor meetings were aimed at consolidating the group, creating an interrelationship among those involved, and sharing the benefits of doing physical activity together. This part of the program was carried out under the supervision of the physical therapist who provided professional support for the proper conduct of the practical activities.
2.4.3. Intervention 3: Psychological counseling
The psychological intervention was based on the transtheoretical model of health behavior change (28) and aimed to promote the change of unhealthy behaviors toward the adoption of better self-care.
Experiential group meetings aimed at exploring individual expectations and promoting behavioral change were organized. In addition, the psychologist evaluated the diaries completed by the patients in order to develop corrective suggestions for the most frequent and overall errors noted.
2.5. Statistical analysis
Data were described through means and standard deviation (SD) and absolute and relative frequencies as appropriate. The comparison of values of laboratory, anthropometric, and pressure parameters, and CRS at baseline, 6, 12, and 18 months was performed through repeated measures ANOVA with post-hoc Bonferroni multiple comparison test. The sphericity assumption has been evaluated with Mauchly's test; in the case of violation, corrections have been adopted. Either the Greenhouse-Geisser or the Huynh–Feldt correction was used according to the epsilon estimate. Interaction terms were not included in the model as only one group of patients was assessed. The repeated measures ANOVA relied on the central limit theorem. The Friedman test was used to address differences in the proportion of smokers over time. All the analyses considered only patients having complete data throughout the different points in time and were also stratified according to the presence of diabetes or/and hypertension at baseline, considering that these two diseases are included in the calculation of the CRS but are not fully and timely modifiable. Another stratified analysis was performed with regard to physical activity. People were classified as physical activity if they self-reported in answering the PASSI questionnaire to make intense physical activity for more than 1 day a week or moderate physical activity for at least 5 days a week. The significance level was set at 0.05 and the SPSS software (version 22) was used for the analysis.
3. Results
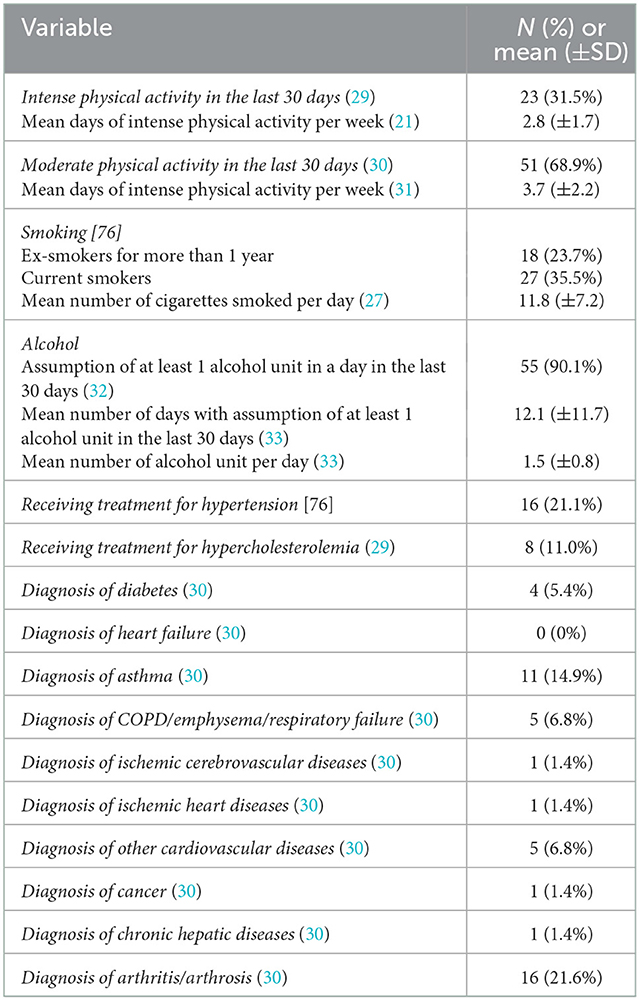
The study population included 76 individuals, 33 (43.4%) men and 43 (56.6%) women. The mean age was 54.6 (±7.6) years and 16 individuals held a bachelor's or master's degree (21.1%), 36 held a high school diploma (47.4%), and 24 held a middle school diploma (31.6%). Among 74 respondents to the PASSI questionnaire, 61 declared to work (82.4%). Participants' health status and risk factors are shown in Table 1. The results of the repeated measurement analysis are shown in Table 2.
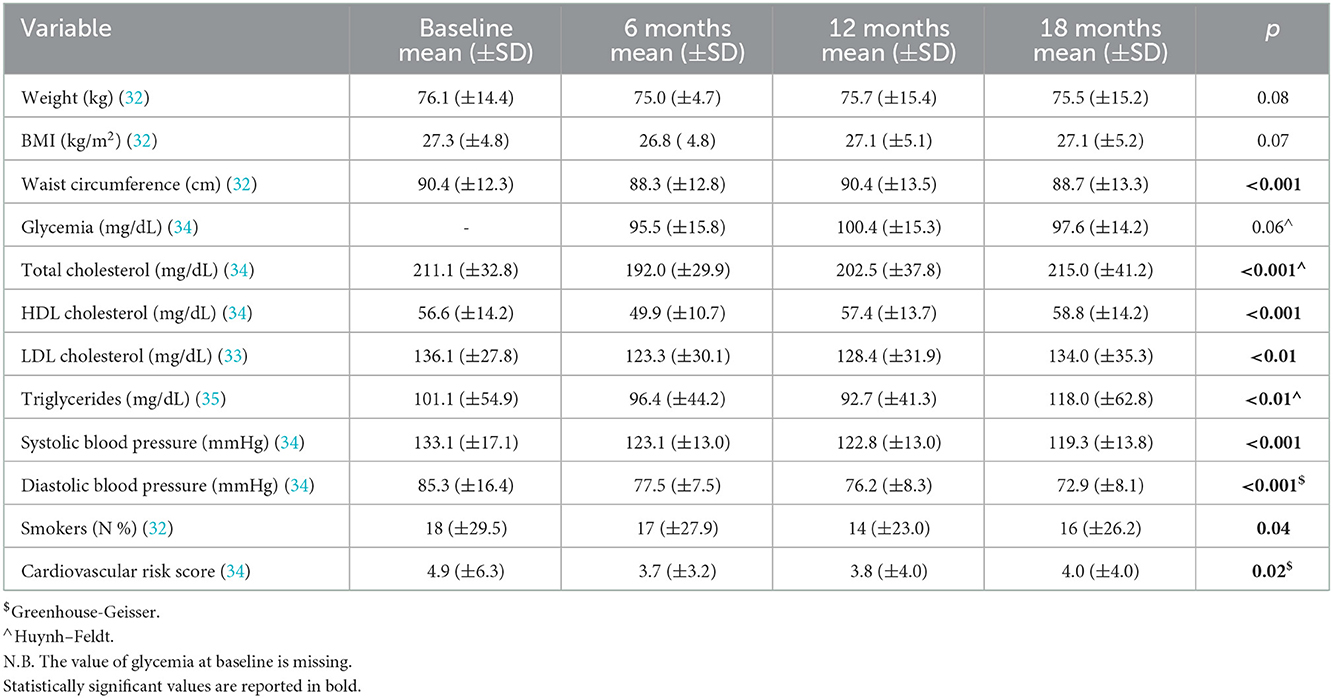
The mean CRS was 4.9 (±6.3) at baseline and showed a significant reduction in time. The relative decrease from baseline to 18 months (calculated as the ratio of the difference between the two values and the baseline value) was 18.4%. The post-hoc multiple comparison test revealed that a significant difference in CRS has established between baseline and 12 months. Considering modifiable variables included in the calculation of the CRS, namely, smoking, SBP, total cholesterol, and HDL cholesterol, it emerged that total cholesterol and SBP significantly decreased at 6 months of follow-up. Nonetheless, the reduction has been maintained in the remaining points in time only for SBP. Also, the prevalence of smokers slightly decreased, in particular, at 12 months.
The analysis stratified according to the presence of diabetes and/or hypertension showed that the CRS did not significantly change in the two groups considered separately (Table 3). This could be due to the increase in glycemia that was observed in people without diabetes and/or hypertension, which could have countered the decrease in total cholesterol and systolic pressure. On the other hand, in people with diabetes/hypertension, results should be considered with caution because of the very low sample size. Actually, a 9% relative decrease in mean CRS was observed from baseline to 18 months in people without diabetes and/or hypertension as compared to 26.7% in people with diabetes and/or hypertension.
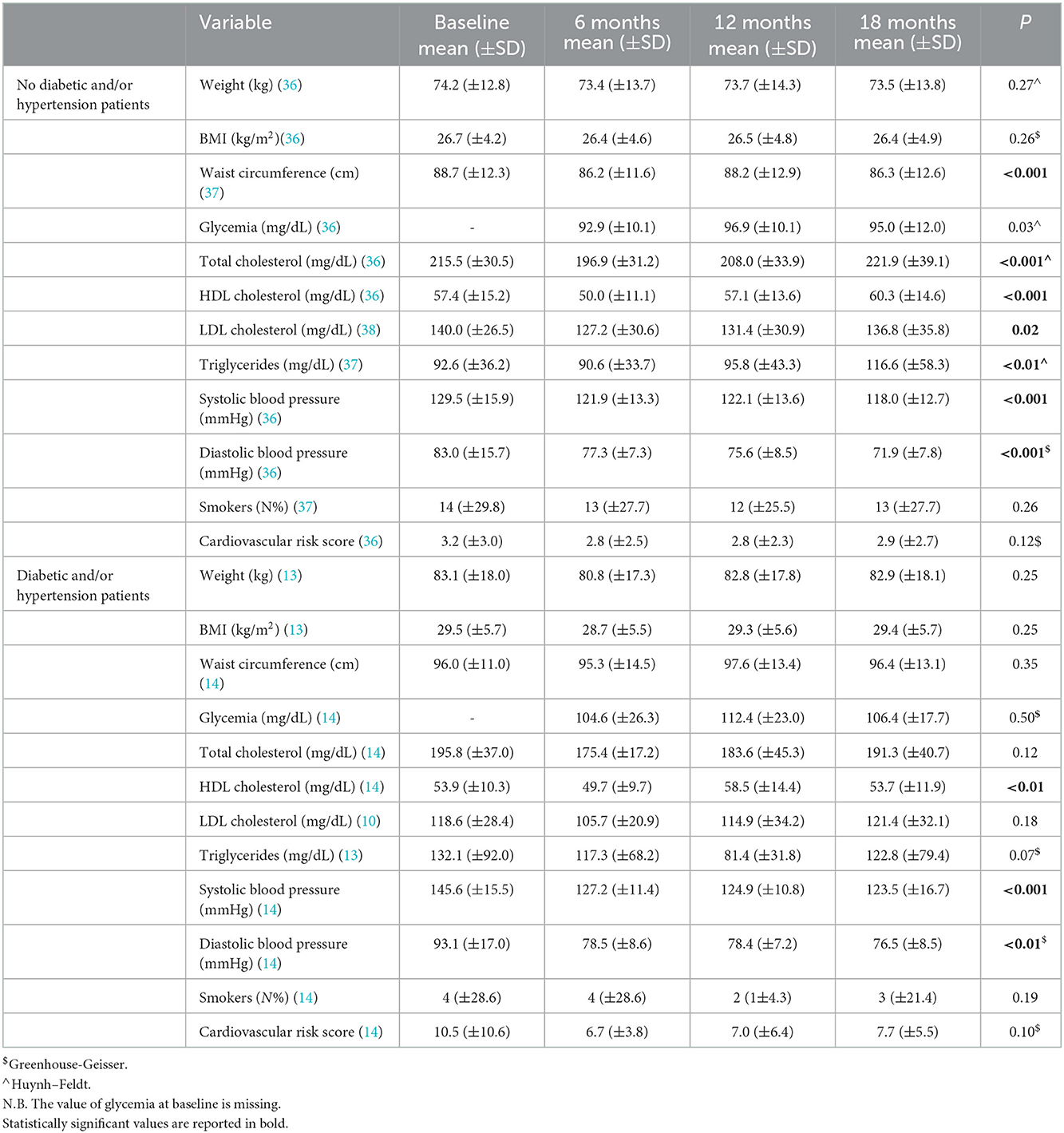
Table 3. Results of repeated measures ANOVA, stratified according to the presence of diabetes and/or hypertension.
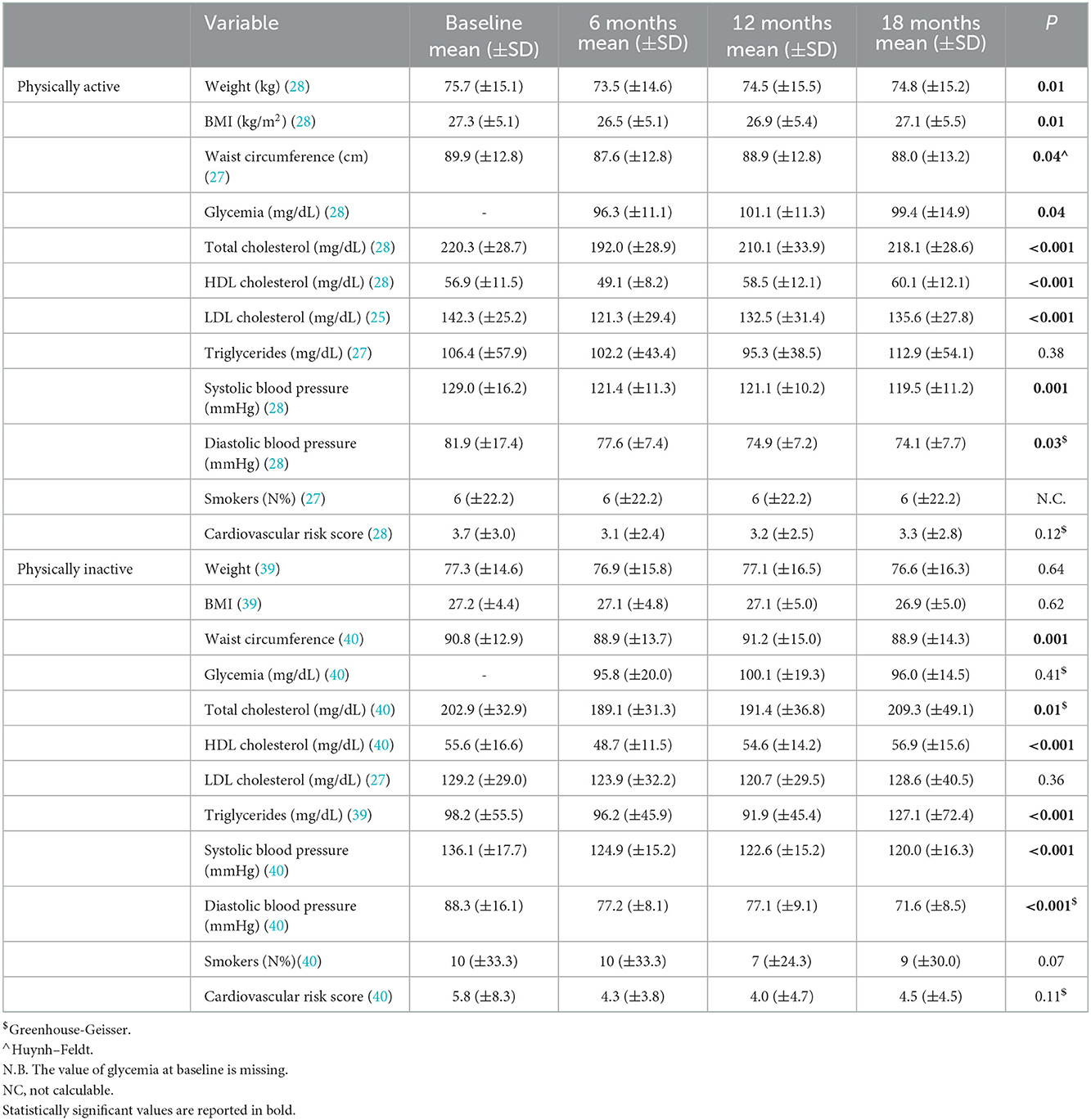
The analysis stratified according to physical activity showed that the CRS did not significantly change in the two groups considered separately (Table 4). The trend in total and HDL cholesterol as well as systolic pressure were confirmed with respect to the overall study population. A 10.8% relative decrease in mean CRS was observed from baseline to 18 months in physically active people as compared to 22.4% in physically inactive people. Interestingly, physically active people also showed a significant decrease in weight and BMI at 6 months.
4. Discussion
According to the “2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease,” the most important way to prevent CVDs is to promote a healthy lifestyle throughout life (39). Intervening on modifiable risk factors to reduce total CV risk is possible through regular physical activity (40), maintenance of adequate weight, proper nutrition (41, 42), and abstention from tobacco smoking (42–44). Such lifestyle modifications in many cases require changes in behavior, and it is, therefore, important that health professionals employ effective behavioral strategies for the overall lifestyle management of their patients (45). Addressing this issue requires building a coalition of health disciplines, including physicians, nurses, health professionals, and psychologists allied to help prevent and control non-communicable diseases (45, 46). To be effective, this type of approach must not stop at multidisciplinarity but aspire to interdisciplinarity, in which healthcare professionals with different backgrounds interpenetrate their knowledge at different levels to provide care that has the patient at its center (46, 47).
In our study, we represent an interdisciplinary community approach model of primary prevention through tailored educational interventions resulting in a significant reduction of CRS. This reduction, observed between baseline and 6–12 months, was due to a similar trend observed in some parameters that are used to calculate the CRS. In a systematic review, Pennant et al. identified 36 observational studies on community programs for the prevention of CVDs: these programs combined media, screening, and environmental changes. Although not via meta-analysis, they described an average net reduction of 9.08% in 10-year CVD risk (47); however, this value is lower than the one outlined in our study (22%). Stewart et al. (44) and Patnode et al. (48) showed that even a small reduction in SBP is associated with a significant reduction in CVD risk; to this proposition, Lewington et al. (49) showed that CVD risk doubles for every 20 mmHg increase in SBP and 10 mmHg increase in DBP in all age and ethnic groups. In a review of the literature, Sisti et al. reported a significant reduction in SBP and DBP of −5.20 and −4.53 mmHg, respectively, as a result of a lifestyle intervention at 6 months. Again, the reduction was also significant at 12 months (−3.34 and −2.98 mmHg, respectively) (7). These results are similar to ours; nevertheless, the change in pressure values was higher in our study both at 6 and 12 months. Patients in our study also showed better SBP reduction than those in a study by Lönnenberg et al. when compared after 12 months of follow-up (50). SBP and DBP are also impacted by diet and exercise as illustrated by Patnode et al. (48) in a primary care intervention, showing a decrease of approximately 1.3 and 0.5 mmHg in SBP and DBP at 6–12 months of follow-up compared with the usual care. Moreover, Sisti et al. assessed a significant reduction in total cholesterol (−0.26 and −0.21 mmol/L at 6 and 12 months, respectively) and triglycerides (−0.19 and −0.09 mmol/L at 6 and 12 months, respectively) (7): although this matches our results for cholesterol, we were not able to show significant changes in relation to triglycerides (7). Patnode et al. also outlined that dietary and physical activity counseling decreases LDL cholesterol level by approximately 2.6 mg/dl and total cholesterol level by approximately 2.8 mg/dl at 6–12 months of follow-up compared with usual care. In particular, they demonstrated that high-intensity interventions result in a greater reduction of LDL and total cholesterol, with no evidence of an effect on HDL cholesterol or triglyceride level (48). Quitting smoking is a relevant cost-effective intervention in primary prevention (51). As a consequence of our interdisciplinary program, we report an initial reduction in the number of smokers, which aligns with the net reduction in smoking prevalence of 1.7% described by Pennant et al. in their systematic review (47).
However, despite an initial improvement in values observed during the first 12 months of intervention, values at 18 months did not show significant differences with respect to baseline. In the last phase of our study, an external event such as the COVID-19 pandemic intervened to alter the effects of our program in the most critical phase, i.e., that of self-maintenance of patients of the results achieved. In light of the emergency situation, the Italian authorities have planned a series of restrictive measures, including a national lockdown in the period of March–April 2020, travel bans, the institution of work from home, and closures of shops and services (52): this resulted in an increase in sedentary behavior and increased CV risk by acting on modifiable risk factors (38, 53). In fact, a sedentary lifestyle is associated with increased oxidative stress and metabolic dysfunction that can result in hyperglycemia, reduced insulin sensitivity, hypertriglyceridemia, and hypertension, all of which increase CV risk (36, 37, 54). In line with these observations, we found an increase in CV risk in our study, in the opposite direction to its trend in the early stages of the multidisciplinary program. Perrone et al. showed that the reduction of daily physical activity during the lockdown period in dyslipidemic patients resulted in an increase in LDL-cholesterol levels of 15.8%, leading to an increased CV risk (55); this had already been shown by Sung et al. in healthy athletes following the interruption of physical activity for 1 month (56) and is also reflected in our results, which document an increase in total cholesterol levels after an initial improvement in the first year of intervention. Often, in addition to the worsening of laboratory parameters, an increase in body weight during lockdown has been documented, not infrequently linked to an increased caloric intake, which was not matched by increased physical activity, or to the worsening of diet quality (31, 57–59). In addition, home confinement has often also resulted in increased alcohol and tobacco consumption (33, 38, 60–62), as also highlighted in our study; on the contrary, indirectly, the pandemic has led to a worsening of hypertension, mainly due to reduced access to doctors' surgeries and pharmacies for the supply of drugs (32, 34, 35, 63); this aspect, on the other hand, does not seem to be correlated with confinement per se, as demonstrated by Pengo et al. who did not detect major changes in blood pressure levels during lockdown by means of a telemonitoring system for patients (64, 65); Similarly, in our study, SBP was the only CV risk factor that continued to improve during the pandemic phase.
The stratification of our results according to the presence of diabetes and/or hypertension and physical activity/inactivity did not issue any significant results, and this can be due to the limited number of people in different subgroups. Nonetheless, the relative reduction of CRS was higher in people with diabetes and/or hypertension and physically inactive patients but these results should be considered exploratory (8, 66). However, literature shows that the implementation of evidence-based guidelines in daily clinical practice may encounter difficulties, resulting in poor outcomes and less impact on CVD risk (67). This is reported by Kotseva et al. (67), who observed insufficient control of CVD risk factors such as blood pressure, cholesterol, and diabetes among patients followed over time in the EUROASPIRE studies, albeit reporting slightly more encouraging results than in the European EURIKA study (68). One of the aspects that can be highlighted in the EUROASPIRE studies is the absence of multidisciplinary follow-up by healthcare professionals: this may explain how our study, albeit on a considerably smaller sample, may have achieved better blood pressure control and an initial reduction in CVD risk, which then stopped when follow-up ceased.
In our analysis, we focused on individuals presenting at the GP's practice. The role of GPs is very important in patient care and is useful for risk assessment and communication at the individual level in order to guide lifestyle modification and treatment decisions (69, 70). Furthermore, primary healthcare and community nurses play a significant role in improving patients' self-management (71). Htay et al. (29), in a systematic review, highlighted the importance of the advanced nurse practitioner (ANP) in improving health outcomes and patient satisfaction in different care settings, including primary care. Therefore, the ANP plays the role of facilitator and, together with the physician, has a synergistic action in reducing mortality given by CVDs (30, 72). Community-based system interventions represent a promising but complex approach to preventive strategies. Existing studies suggest that the implementation of multiple actions by engaged community leaders (steering committees) is of critical importance to influence a complex system.
This study has several limitations. First, the main weakness of this study lies in the potential “self-selection bias,” as participation implied a willingness of the respondent to take an active part in the study and this willingness could be influenced by certain characteristics that could act as confounding factors. Furthermore, since the study has not foreseen a control group, observed changes should be commented on with caution as they could have also been attributable to factors other than the intervention. Moreover, not all patients included in the study were included in the analysis, due to missing data during the follow-up at 6, 12, and 18 months. Furthermore, our sample size was relatively small and no sample size determination or power analysis has been performed because it was a pilot study. Eventually, the generalizability of our findings is limited to people with a moderate risk profile. Furthermore, it should be observed that the pandemic outbreak and the following national lockdown (from March to May 2020) have probably affected results at 18 months; however, it is difficult to estimate their real influence and link them to changes in lifestyle and adherence to healthy behaviors.
Finally, although we documented at baseline the number of subjects on antihypertensive and cholesterolaemic-lowering therapy, we did not acquire information on the type of drugs nor on the dosage used: we are, therefore, unable to assess the impact of the program on the therapy of the patients involved by evaluating whether the dosage changed during the course of the study.
The results of this study corroborate the positive impact of health promotion and prevention interventions; however, randomized control trials are needed to further investigate the effectiveness of such kinds of interventions. This could guarantee actively taking charge of subjects by identifying potentially problematic situations and implementing policies for the prevention of risk factors of CVD and other non-communicable diseases.
Data availability statement
The datasets presented in this article are not readily available because only GPs hold patients' clinical data and they are responsible for them. Data have been anonymized and transmitted to the Section of Hygiene of Università Cattolica del Sacro Cuore, and they are available on request from the authors. Requests to access the datasets should be directed to PL, cGF0cml6aWEubGF1cmVudGlAdW5pY2F0dC5pdA==.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Committee Lazio 1 c/o San Camillo Forlanini Hospital (with protocol number 1817 / CE Lazio 1). The patients/participants provided their written informed consent to participate in this study.
Author contributions
PL, GD, AT, and SG: conceptualization and project administration. CG, EMaz, AL, EMar, and FD'A: investigation. CW, PL, and GD: methodology. AL, EMar, and FD'A: writing–original draft. AT, CG, PL, VG, AM, MP, and AB: writing–review and editing. CW: software and formal analysis. AT, CG, EMaz, and SG: data curation. PL and CW: validation. AT, CG, PL, VG, AM, MP, AB, and GD: supervision. All authors have read and agreed to the published version of the manuscript.
Acknowledgments
The authors would like to thank the students of the master's degree in Nursing Science and the support staff for their invaluable help in the collection of data throughout this project. We would also like to express our gratitude to the research participants who gave their valuable time and participated in this study voluntarily.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Cardiovascular Diseases (CVDs). Available online at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed October 12, 2022).
2. Heart Disease and Stroke Statistics-2021 Update A Report from the American Heart Association. Circulation. (2021) 134:E254–E743. doi: 10.1161/CIR.0000000000000950
3. Wilkins E, Wilson L, Wickramasinghe K, Bhatnagar P, Leal J, Luengo-Fernandez R, et al. European Cardiovascular Disease Statistics 2017. Brussels: European Heart Network (2017).
4. ISS. Il Progetto Cuore. Available online at: https://www.cuore.iss.it/altro/cuore (accessed December 31, 2021).
5. Pyörälä K. CHD prevention in clinical practice. Lancet. (1996) 348 (Suppl 1). doi: 10.1016/S0140-6736(96)98009-5
6. Perk J, de Backer G, Gohlke H, Graham I, Reiner Ž, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. (2012) 33:1635–701. doi: 10.1093/eurheartj/ehs092
7. Sisti LG, Dajko M, Campanella P, Shkurti E, Ricciardi W, de Waure C. The effect of multifactorial lifestyle interventions on cardiovascular risk factors: a systematic review and meta-analysis of trials conducted in the general population and high risk groups. Prev Med (Baltim). (2018) 109:82–97. doi: 10.1016/j.ypmed.2017.12.027
8. Rippe JM. Lifestyle Strategies for Risk Factor Reduction, Prevention, and Treatment of Cardiovascular Disease. Am J Lifestyle Med. (2019) 13:204. doi: 10.1177/1559827618812395
9. Harrison C, Britt H, Miller G, Henderson J. Prevalence of Chronic Conditions in Australia. PLoS ONE. (2013) 8:e67494. doi: 10.1371/journal.pone.0067494
10. Califf RM, Armstrong PW, Carver JR, D'Agostino RB, Strauss WE. 27th Bethesda Conference: matching the intensity of risk factor management with the hazard for coronary disease events. Task Force 5 Stratification of patients into high, medium and low risk subgroups for purposes of risk factor management. J Am Coll Cardiol. (1996) 27:1007–19. doi: 10.1016/0735-1097(96)87733-3
11. Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. (2010) 122. doi: 10.1161/CIR.0b013e3182051b4c
12. Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. (2003) 24:987–1003. doi: 10.1016/S0195-668X(03)00114-3
13. Lee MS, Flammer AJ, Li J, Lennon RJ, Delacroix S, Kim H, et al. Comparison of Time trends of cardiovascular disease risk factors and framingham risk score between patients with and without acute coronary syndrome undergoing percutaneous intervention over the last 17 years: from the mayo clinic percutaneous coronary intervention registry. Clin Cardiol. (2015) 38:747. doi: 10.1002/clc.22484
14. ASCVD Risk Estimator. Available online at: https://tools.acc.org/ldl/ascvd_risk_estimator/index.html#!/calulate/estimator/patient (accessed October 12, 2022).
15. Jancey J, James A, Lee A, Howat P, Hills AP, Anderson AS, et al. Metabolic syndrome in rural Australia: An opportunity for primary health care. Aust J Rural Health. (2019) 27:210–5. doi: 10.1111/ajr.12598
16. D'Agostino RB, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. (2001) 286:180–7. doi: 10.1001/jama.286.2.180
17. Anderson KM, Wilson PWF, Odell PM, Kannel WB. An updated coronary risk profile. A statement for health professionals. Circulation. (1991) 83:356–62. doi: 10.1161/01.CIR.83.1.356
18. Wilson PWF, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. (1998) 97:1837–47. doi: 10.1161/01.CIR.97.18.1837
19. de Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, et al. European guidelines on cardiovascular disease prevention in clinical practice. Third joint task force of european and other societies on cardiovascular disease prevention in clinical practice. Eur Heart J. (2003) 24:1601–10. doi: 10.1016/S0195-668X(03)00347-6
20. Haskell WL, Alderman EL, Fair JM, Maron DJ, Mackey SF, Superko HR, et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP). Circulation. (1994) 89:975–90. doi: 10.1161/01.CIR.89.3.975
21. Saggese L, Scala E. Comune di Roma. Il Contesto territoriale e il profilo socio-demografico del territorio e della comunità locale. (2015). Available online at: https://www.comune.roma.it/PCR/resources/cms/documents/cap_1_contesto_territoriale_profilo_socio_demografico.pdf (accessed April 20, 2022).
22. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults a report of the American College of Cardiology/American Heart Association Task Force on Clinical practice. Hypertension. (2018) 71: 13–115. doi: 10.1161/HYP.0000000000000065
23. Drinking Levels Defined | National Institute on Alcohol Abuse and Alcoholism (NIAAA). Available online at: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking (accessed April 20, 2022).
24. Istituto Superiore di Sanità. Il Progetto CUORE. Available online at: http://progettocuore.medisoft.it/cuore_exe/registration.aspx (accessed October 14, 2022).
25. Sorveglianza Passi. Available online at: https://www.epicentro.iss.it/passi/infoPassi/infoGen (accessed October 14, 2022).
26. Wallston BS, Wallston KA, Kaplan GD, Maides SA. Development and validation of the health locus of control (HLC) scale. J Consult Clin Psychol. (1976) 44:580–5. doi: 10.1037/0022-006X.44.4.580
27. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
28. Prochaska JO, di Clemente CC. Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy. (1982) 19:276–88. doi: 10.1037/h0088437
29. Htay M, Whitehead D. The effectiveness of the role of advanced nurse practitioners compared to physician-led or usual care: a systematic review. Int J Nurs Stud Adv. (2021) 3:100034. doi: 10.1016/j.ijnsa.2021.100034
30. Connolly SB, Kotseva K, Jennings C, Atrey A, Jones J, Brown A, et al. Outcomes of an integrated community-based nurse-led cardiovascular disease prevention programme. Heart. (2017) 103:840–7. doi: 10.1136/heartjnl-2016-310477
31. Özden G, Parlar Kiliç S. The effect of social isolation during COVID-19 pandemic on nutrition and exercise behaviors of nursing students. Ecol Food Nutr. (2021) 60:663–81. doi: 10.1080/03670244.2021.1875456
32. Burnier M. Controversies in the management of patients with arterial hypertension. Kardiol Polska. (2019) 77:902–7. doi: 10.33963/KP.15002
33. Dyal SR, Valente TW. A systematic review of loneliness and smoking: Small effects, big implications. Subst Use Misuse. (2015) 50:1697–716. doi: 10.3109/10826084.2015.1027933
34. Weber T. The corona-virus disease 2019 pandemic compromised routine care for hypertension: a survey conducted among excellence centers of the European Society of Hypertension. J Hypertens. (2021) 39:190–5. doi: 10.1097/HJH.0000000000002703
35. Kauppi M, Elovainio M, Stenholm S, Virtanen M, Aalto V, Koskenvuo M, et al. Social networks and patterns of health risk behaviours over two decades: a multi-cohort study. J Psychosom Res. (2017) 99:45–58. doi: 10.1016/j.jpsychores.2017.06.003
36. Gupta N, Hallman DM, Mathiassen SE, Aadahl M, Jørgensen MB, Holtermann A. Are temporal patterns of sitting associated with obesity among blue-collar workers? A cross sectional study using accelerometers. BMC Public Health. (2016) 16:1–10. doi: 10.1186/s12889-016-2803-9
37. Betts JA, Smith HA, Johnson-Bonson DA, Ellis TI, Dagnall J, Hengist A, et al. The energy cost of sitting versus standing naturally in man. Med Sci Sports Exerc. (2019) 51:726–33. doi: 10.1249/MSS.0000000000001841
38. Bérard E, Huo Yung Kai S, Coley N, Bongard V, Ferrières J. One-Year Impact of COVID-19 Lockdown-Related Factors on Cardiovascular Risk and Mental Health: A Population-Based Cohort Study. Int J Environ Res Public Health. (2022) 19. doi: 10.3390/ijerph19031684
39. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. (2019) 140:e596–646. doi: 10.1161/CIR.0000000000000678
40. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services (2018).
41. Cleeman JI. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. (2001) 285:2486–97. doi: 10.1001/jama.285.19.2486
42. American College of Lifestyle Medicine. Available online at: https://www.lifestylemedicine.org/ (accessed October 12, 2022).
43. Yusuf S, Wood D, Ralston J, Reddy KS. The World Heart Federation's vision for worldwide cardiovascular disease prevention. Lancet. (2015) 386:399–402. doi: 10.1016/S0140-6736(15)60265-3
44. Stewart J, Addy K, Campbell S, Wilkinson P. Primary prevention of cardiovascular disease: Updated review of contemporary guidance and literature. JRSM Cardiovasc Dis. (2020) 9:204800402094932. doi: 10.1177/2048004020949326
45. Jennings C, Astin F. A multidisciplinary approach to prevention. Eur J Prev Cardiol. (2017) 24:77–87. doi: 10.1177/2047487317709118
46. Jain A, Davis AM. Primary prevention of cardiovascular disease. JAMA. (2019) 322:1817–8. doi: 10.1001/jama.2019.15915
47. Pennant M, Davenport C, Bayliss S, Greenheld W, Marshall T, Hyde C. Community programs for the prevention of cardiovascular disease: a systematic review. Am J Epidemiol. (2010) 172:501–16. doi: 10.1093/aje/kwq171
48. Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. Behavioral Counseling to Promote a Healthful Diet and Physical Activity for Cardiovascular Disease Prevention in Adults Without Known Cardiovascular Disease Risk Factors: Updated Systematic Review for the U.S. Preventive Services Task Force. HRQ Publication No 15-05222-EF-1. Rockville, MD: Agency for Healthcare Research and Quality, JAMA. (2017). doi: 10.1001/jama.2017.3303
49. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. (2002) 360:1903–13. doi: 10.1016/S0140-6736(02)11911-8
50. Lönnberg L, Ekblom-Bak E, Damberg M. Reduced 10-year risk of developing cardiovascular disease after participating in a lifestyle programme in primary care. Ups J Med Sci. (2020) 125:250–6. doi: 10.1080/03009734.2020.1726533
51. Silagy C, Stead L. Physician advice for smoking cessation. Cochrane Database of Syst Rev. (2001). doi: 10.1002/14651858.CD000165
52. Coronavirus, le misure adottate dal Governo | www.governo.it. Available online at: https://www.governo.it/it/coronavirus-misure-del-governo (accessed October 4, 2022).
53. Chandrasekaran B, Ganesan TB. Sedentarism and chronic disease risk in COVID 19 lockdown - a scoping review. Scott Med J. (2021) 66:3–10. doi: 10.1177/0036933020946336
54. Saunders TJ, Atkinson HF, Burr J, MacEwen B, Skeaff CM, Peddie MC. The acute metabolic and vascular impact of interrupting prolonged sitting: a systematic review and meta-analysis. Sports Med. (2018) 48:2347–66. doi: 10.1007/s40279-018-0963-8
55. Perrone MA, Feola A, Pieri M, Donatucci B, Salimei C, Lombardo M, et al. The Effects of Reduced Physical Activity on the Lipid Profile in Patients with High Cardiovascular Risk during COVID-19 Lockdown. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18168858
56. Sung YC, Liao YH, Chen CY, Chen YL, Chou CC. Acute changes in blood lipid profiles and metabolic risk factors in collegiate elite taekwondo athletes after short-term de-training: a prospective insight for athletic health management. Lipids Health Dis. (2017) 16. doi: 10.1186/s12944-017-0534-2
57. Freiberg A, Schubert M, Starke KR, Hegewald J, Seidler A. A rapid review on the influence of COVID-19 lockdown and quarantine measures on modifiable cardiovascular risk factors in the general population. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18168567
58. Unubol M, Erdemir Z, Colak G, Guney E, Omurlu IK. Obesity pandemic triggered by the COVID-19 pandemic: experience from Turkey. Pol Arch Intern Med. (2021) 131:766–8. doi: 10.20452/pamw.16037
59. Kreutz R, Dobrowolski P, Prejbisz A, Algharably EAEH, Bilo G, Creutzig F, et al. Lifestyle, psychological, socioeconomic and environmental factors and their impact on hypertension during the coronavirus disease 2019 pandemic. J Hypertens. (2021) 39:1077–89. doi: 10.1097/HJH.0000000000002770
60. Kelly S, Olanrewaju O, Cowan A, Brayne C, Lafortune L. Alcohol and older people: A systematic review of barriers, facilitators and context of drinking in older people and implications for intervention design. PLoS ONE. (2018) 13. doi: 10.1371/journal.pone.0191189
61. Stanesby O, Labhart F, Dietze P, Wright CJC, Kuntsche E. The contexts of heavy drinking: A systematic review of the combinations of context-related factors associated with heavy drinking occasions. PLoS ONE. (2019) 14. doi: 10.1371/journal.pone.0218465
62. Seo DC, Huang Y. Systematic review of social network analysis in adolescent cigarette smoking behavior*. J Sch Health. (2012) 82:21–7. doi: 10.1111/j.1746-1561.2011.00663.x
63. Cuffee Y, Ogedegbe C, Williams NJ, Ogedegbe G, Schoenthaler A. Psychosocial risk factors for hypertension: an update of the literature. Curr Hypertens Rep. (2014) 16. doi: 10.1007/s11906-014-0483-3
64. Pengo M, Albini F, Guglielmi G, Mollica C, Soranna D, Zambra G, et al. Home blood pressure during COVID-19 related lockdown in patients with hypertension. Eur J Prev Cardiol. (2021) 28. doi: 10.1093/eurjpc/zwab061.142
65. Januszewicz A, Wojciechowska W, Prejbisz A, Dobrowolski P, Rajzer M, Kreutz R. Impact of the COVID-19 pandemic on blood pressure control and cardiovascular risk profile in patients with hypertension. Pol Arch Intern Med. (2021) 131. doi: 10.20452/pamw.16129
66. Moore SC, Patel AV., Matthews CE, Berrington de Gonzalez A, Park Y, Katki HA, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. (2012) 9. doi: 10.1371/journal.pmed.1001335
67. Kotseva K, de Backer G, de Bacquer D, Ryden L, Hoes A, Grobbee D, et al. Primary prevention efforts are poorly developed in people at high cardiovascular risk: a report from the European Society of Cardiology EURObservational Research Programme EUROASPIRE V survey in 16 European countries. Eur J Prev Cardiol. (2021) 28:370–9. doi: 10.1177/2047487320908698
68. Banegas JR, López-García E, Dallongeville J, Guallar E, Halcox JP, Borghi C, et al. Achievement of treatment goals for primary prevention of cardiovascular disease in clinical practice across Europe: the EURIKA study. Eur Heart J. (2011) 32:2143–52. doi: 10.1093/eurheartj/ehr080
69. Beganlic A, Pavljasevic S, Kreitmayer S, Zildzic M, Softic A, Selmanovic S, et al. Qualitative evaluation of cardiovascular diseases management in family medicine team in one year level. Med Arch. (2015) 69:140. doi: 10.5455/medarh.2015.69.140-144
70. Diederichs C, Neuhauser H, Rücker V, Busch MA, Keil U, Fitzgerald AP, et al. Predicted 10-year risk of cardiovascular mortality in the 40 to 69 year old general population without cardiovascular diseases in Germany. PLoS ONE. (2018) 13. doi: 10.1371/journal.pone.0190441
71. Simonetti V, Comparcini D, Tomietto M, Pavone D, Flacco ME, Cicolini G. Effectiveness of a family nurse-led programme on accuracy of blood pressure self-measurement: a randomised controlled trial. J Clin Nurs. (2021) 30:2409–19. doi: 10.1111/jocn.15784
Keywords: cardiovascular disease, cardiovascular risk score, risk reduction, primary care, primary prevention, health promotion
Citation: Lontano A, Marziali E, Galletti C, Mazza E, Gambioli S, Galasso V, Mingarelli A, D'Ambrosio F, Tamburrano A, Paolini M, Bande A, Damiani G, de Waure C and Laurenti P (2023) A real opportunity to modify cardiovascular risk through primary care and prevention: A pilot study. Front. Public Health 10:1009246. doi: 10.3389/fpubh.2022.1009246
Received: 01 August 2022; Accepted: 12 December 2022;
Published: 10 January 2023.
Edited by:
Christiane Stock, Charité Medical University of Berlin, GermanyReviewed by:
Željko Reiner, University Hospital Centre Zagreb, CroatiaGabriele Messina, University of Siena, Italy
Francesco Gianfagna, University of Insubria, Italy
Copyright © 2023 Lontano, Marziali, Galletti, Mazza, Gambioli, Galasso, Mingarelli, D'Ambrosio, Tamburrano, Paolini, Bande, Damiani, de Waure and Laurenti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eleonora Marziali,  ZWxlb25vcmEubWFyemlhbGkwMUBpY2F0dC5pdA==
ZWxlb25vcmEubWFyemlhbGkwMUBpY2F0dC5pdA==
 Alberto Lontano
Alberto Lontano Eleonora Marziali
Eleonora Marziali Caterina Galletti
Caterina Galletti Eduardo Mazza2
Eduardo Mazza2 Floriana D'Ambrosio
Floriana D'Ambrosio Andrea Tamburrano
Andrea Tamburrano Gianfranco Damiani
Gianfranco Damiani Chiara de Waure
Chiara de Waure Patrizia Laurenti
Patrizia Laurenti