- 1German Center for Neurodegenerative Diseases (DZNE), Greifswald, Germany
- 2Institute for Social Medicine, Occupational Medicine, and Public Health (ISAP) of the Medical Faculty, University of Leipzig, Leipzig, Germany
- 3Institute for Community Medicine, Section Epidemiology of Health Care and Community Health, University Medicine Greifswald (UMG), Greifswald, Germany
- 4Epidemiology, IQVIA, Frankfurt am Main, Germany
Background: The COVID-19 pandemic and the imposed lockdowns severely affected routine care in general and specialized physician practices.
Objective: To describe the long-term impact of the COVID-19 pandemic on the physician services provision and disease recognition in German physician practices and perceived causes for the observed changes.
Design: Observational study based on medical record data and survey data of general practitioners and specialists' practices.
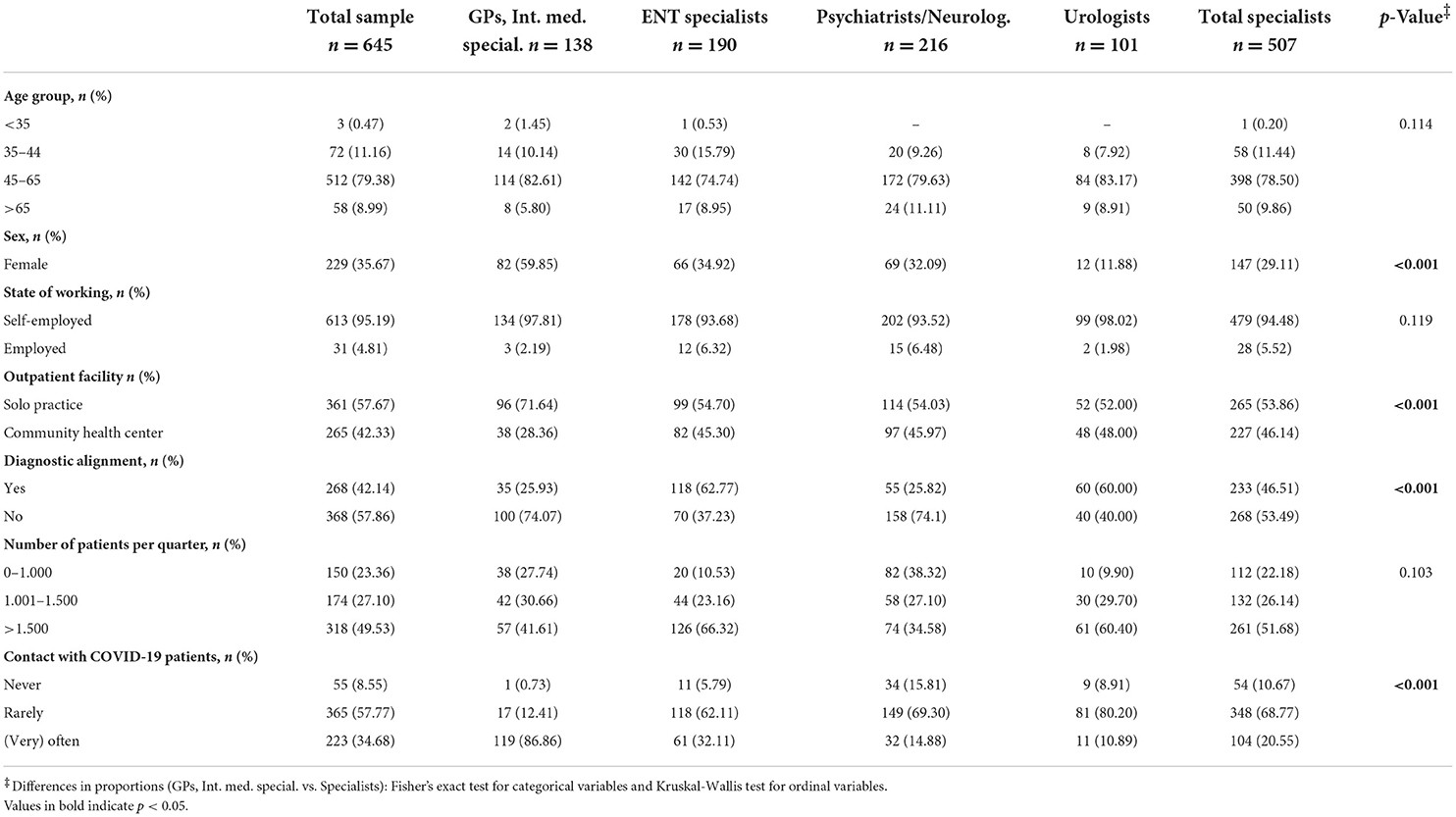
Participants: 996 general practitioners (GPs) and 798 specialist practices, who documented 6.1 million treatment cases for medical record data analyses and 645 physicians for survey data analyses.
Main measures: Within the medical record data, consultations, specialist referrals, hospital admissions, and documented diagnoses were extracted for the pandemic (March 2020–September 2021) and compared to corresponding pre-pandemic months in 2019. The additional online survey was used to assess changes in practice management during the COVID-19 pandemic and physicians' perceived main causes of affected primary and specialized care provision.
Main results: Hospital admissions (GPs: −22% vs. specialists: −16%), specialist referrals (−6 vs. −3%) and recognized diseases (−9 vs. −8%) significantly decreased over the pandemic. GPs consultations initially decreased (2020: −7%) but compensated at the end of 2021 (+3%), while specialists' consultation did not (−2%). Physicians saw changes in patient behavior, like appointment cancellation, as the main cause of the decrease. Contrary to this, they also mentioned substantial modifications of practice management, like reduced (nursing) home visits (41%) and opening hours (40%), suspended checkups (43%), and delayed consultations for high-risk patients (71%).
Conclusion: The pandemic left its mark on primary and specialized healthcare provision and its utilization. Both patient behavior and organizational changes in practice management may have caused decreased and non-compensation of services. Evaluating the long-term effect on patient outcomes and identifying potential improvements are vital to better prepare for future pandemic waves.
Introduction
Due to the COVID-19 pandemic and its rapid spread, governments worldwide initiated emergency lockdowns, mitigating infection rates and preventing the burden on the healthcare systems (1). Social distancing has become the standard practice in preventing the spread of COVID-19 infection (1–3).
Measures mitigating the infection rates resulted in side effects on the provision and utilization of routine care in worldwide healthcare systems. Healthcare utilization was affected due to efforts of reduced infection risk to prevent the older population and the overburden of the healthcare system (4). However, the infection risk and mortality rate also affected the provision of healthcare services during the pandemic, especially for general practitioners (GPs) (5).
Previous studies report that, initially, primary care physicians were unprepared for the new situation in their practices, especially regarding medical equipment, leading to significant concerns and fears among physicians, including being carriers of the virus or becoming infected (6, 7). GPs were concerned about the continuity of regular care due to COVID-19 measures and that these could affect the population's overall health (8). It can be assumed that the lack of medical equipment and the fear reflected in physicians' behavior entailed adjusting their practice management. However, evidence about related consequences at the individual practice level affecting healthcare provision is rare. Therefore, primary data are needed to fill this gap.
Despite several studies examining the impact of early imposed contact bans on the provision and utilization of primary and secondary healthcare services, indicating a tremendous decrease in physician consultations, specialist referrals, hospital admissions and disease recognition, there is presently a lack of knowledge about the compensation of the initial decline during the following course of the COVID-19 pandemic (9–14). Moreover, analyses of the causal background of changes in health service provision and the lack of compensation beyond the early COVID-19 contact bans are scarce.
Therefore, this study aimed to describe (i) the provision of healthcare services and disease recognition during the COVID-19 pandemic in Germany's primary and specialized care and (ii) to identify reasons for the change of both in the following course of the pandemic from an outpatient physician perspective.
Materials and methods
Study design
This study comprised a secondary data analysis to examine changes in healthcare service provision and an additional survey to assess perceived reasons for the changes in primary and specialized care provision.
The secondary data analysis was based on medical record data from the Disease Analyzer database (IQVIA), capturing consultations, drug prescriptions, specialist referrals, diagnoses made, and basic medical and demographic data directly and anonymously from the primary care and specialist practices via an interface to their respective practice management software (15). The database structure corresponds to the total number of physicians (i.e. statistical population) annually published by the German Medical Association in terms of demographic characteristics, diagnoses, and therapies for each specialty and covers about 3% of all outpatient practices in Germany (15). Diagnoses, prescriptions, and quality of the reported data are monitored by IQVIA using several criteria, such as completeness and plausibility (15). The analysis was based on data from a total of 6.1 million treatment cases per year (patients aged 18 years and older) documented by 996 GPs and internists or 798 specialist practices (n = 224 gynecologists, n = 147 orthopedists, n = 127 neurologists and psychiatrists, n = 133 ear, nose and throat (ENT) physicians, n = 83 dermatologists, and n = 84 urologists) in Germany between September 2019 and February 2020 (pre-pandemic period) as well as March 2020 and September 2021 (pandemic period).
The subsequent Germany-wide anonymous online survey was generated based on the previously conducted secondary data analysis results, daily developments, and internal expert consensus and comprised, in particular, the following steps: (i) review of the relevant literature, (ii) development of the first draft of the questionnaire by a previously formed core team of three researchers, (iii) consultation of the questionnaire with representatives (i.e. experts) of all participating professional associations as well as (iv) finalization and preparation for distribution. The questionnaire was distributed using the cloud-based open-source tool LimeSurvey (16). The following professional associations of practitioners shared the survey link between 04 December 2021 and 28 February 2022 with their members via different communication channels (e.g., e-mail distribution lists, newsletters, and homepages): German General Practitioners Association e.V., Professional Association of German Neurologists, Professional Association of German Urologists e.V., German Professional Association of Otolaryngologists e.V. Participating primary care physicians and specialists were informed about the changes in healthcare utilization during COVID-19 by the results of the secondary data analysis and were subsequently asked to fill in the questionnaire about their perceptions and reasons for the change in the provision and utilization of primary and specialized healthcare services. In total, n = 645 physicians responded to the online survey questionnaire, including n = 138 (21%) GPs and internal specialists as well as n = 507 (79%) specialists (n = 216 (34%) neurologists, n = 190 (30%) ENT specialists, n = 101 (16%) urologists). The survey was approved by the Ethical Committee of the Chamber of Physicians of Mecklenburg-Western Pomerania [registry number (BB 127/21)].
Observation period
The utilization and provision of healthcare services and recognized diseases were captured separately for each month from march 2019 to September 2021. According to Schilling et al. (17), the pandemic timeframe was subdivided into the following periods: 1st-COVID-19-Wave (March–May 2020), Summerplateau 2020 (June–September 2020), 2nd-COVID-19-Wave (October 2020–February 2021) 3rd-COVID-19-Wave (March–June 2021), Summerplateau 2021 (June–July 2021) and 4th-COVID-19-Wave (August–September 2021).
Study outcomes
Outcomes of the secondary data analysis
The main outcomes of the secondary data analysis to illustrate changes in health service utilization during the COVID-19 pandemic were the following: the number of (1) GPs and specialist consultations (telephone contacts and visits), (2) hospital admissions, (3) specialist referrals, and (4) recognized diseases. The following documented ICD-10 diagnoses were used to represent the recognition of diseases in the different practices: dementia (F01, F03, G30 and F06. 7), diabetes mellitus (E10–14), stroke (I63, I64, G45), epilepsy (G40), Parkinson's disease (G20, G21), depression (F32, F33), cancer (C00–C99), chronic bronchitis and chronic obstructive pulmonary disease (COPD; J42–J44), and myocardial infarction (MI; I21, I22) and coronary artery disease (CAD; I24, I25). All diagnoses must be the initial diagnosis. Healthcare utilization and disease recognition were presented as frequencies whereby the pandemic periods (2020 and 2021) were compared with the corresponding prepandemic periods in 2019. For this purpose, percentage differences were calculated for both the individual waves and overall pandemic course compared to the respective prepandemic period to assess the change during the COVID-19 pandemic in Germany.
Survey outcomes
The subsequent survey for the practitioners elicited the outpatient physicians' perspectives covering the following outcomes: (1) perceived causes for the decreased and non-compensated number of consultations and recognized diseases during the 1st-COVID-19-wave and the following waves, and (2) the changes made in practice management to reduce infection risk. To assess physicians' perceptions in more detail, two to five additional items assess on a 5-Point-Likert-type response scale (1= “does not apply” to 5= “applies”) whether the physicians thought that themselves or the patient caused the decrease or lack of compensation. Changes in practice management comprise eight items assessing whether the practices changed their management (1= “does not apply” to 5= “applies”) and 11 items assessing how often items were performed compared to pre-pandemic (1= “much rarer” to 5= “much more frequently”). Each of the six items represented measures for infection risk reduction and was assessed dichotomously (yes vs. no). In addition, sociodemographic characteristics of the physicians (age, sex) and the following characteristics of their practices were assessed: state of working (self-employed vs. employed), outpatient facility (solo practice vs. community health center), diagnostic alignment (yes vs. no), number of patients per quarter (0–1.000 vs. 1.001–1.500 vs. >1.500) and contact with designated COVID-19 patients (never vs. rarely vs. often vs. very often). The questionnaire is demonstrated in Supplementary Appendix 1.
Statistical analyses
Regarding primary and secondary data analysis, descriptive statistics were used. Group differences in proportions of sociodemographic and practice characteristics of the physicians, as well as in perception and views on causes, were determined using Fisher's exact Tests (GPs vs. Specialists). The reporting of the results followed the STROBE guidelines (18). Analyses were performed using SAS version 9.4 (Cary, NC: SAS Institute Inc) and STATA/IC 16 (19).
Results
Change in the provision of healthcare services
After an initial sharp decrease in the consultation rate during the first COVID-19 wave, GPs and internists (+2.6) have increased their consultations over the entire COVID-19 pandemic (2020–2021) in comparison to the pre-pandemic period (2019). However, the consultation rate for specialists was reduced (−1.7%) at the end of the fourth COVID-19 wave in September 2021. Neurologists and psychiatrists (+0.9%), urologists (+0.1%) and gynecologists (+3.3%) compensated for an initial consultation rate decrease, while orthopedists (−4.3%), dermatologists (−3.1%) and ENT specialists (−7.7%) had a decreased consultation rate at the end of 2021.
Over all COVID-19-waves, the specialists' referrals decreased in all practices, especially in GPs and less in specialist practices (−6.0 vs. −2.6%). The largest decrease was seen for ENT specialists (−6.1%). Hospital admissions decreased tremendously over the entire COVID-19 pandemic for both GPs (−21.5%) and specialists (−15.7%). While dermatologists (−32.7%) have demonstrated the largest, urologists (−11.1%) had the lowest decline. Figure 1 and Table 1 show the change in the consultation, specialists' referrals and hospital admission rate for each practitioner specialty over the entire COVID-19 pandemic. A detailed description of these changes can be found in Supplementary Appendix 2.
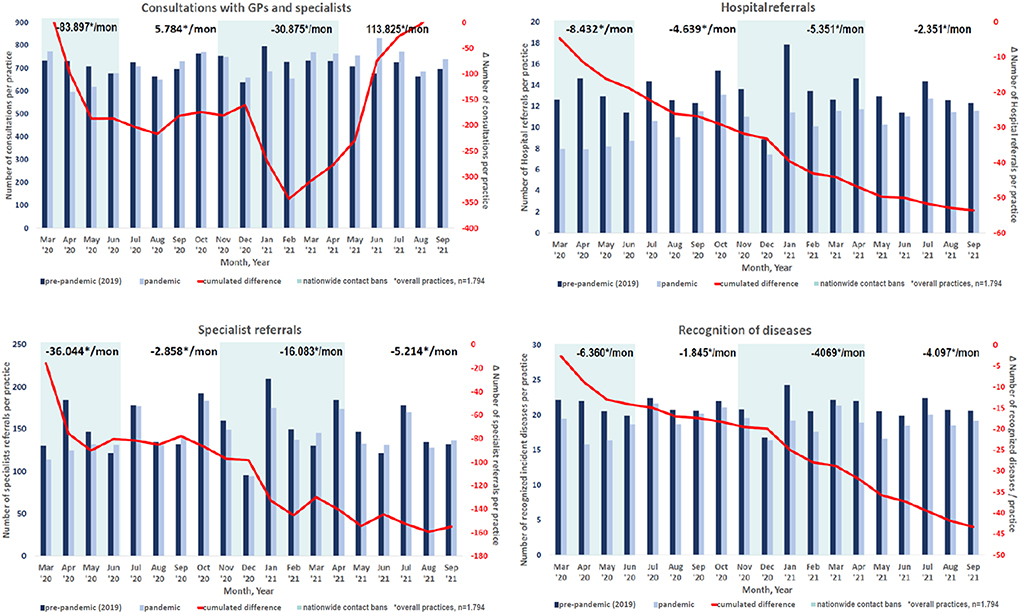
Figure 1. Change of consultation rate, specialist referrals, hospital admissions and detection of diseases over the COVID-19 pandemic.

Table 1. Utilization of healthcare services during the COVID-19 pandemic in Germany compared to the pre-pandemic time frame 2019/20.
Recognized diseases
During the COVID-19 pandemic, the number of recognized diseases decreased among GPs and specialist practices by −8.4% (GPs: −9.0% vs. specialists: −7.5%). The largest decline for GPs and internists accounted for COPD (−20.5%), Parkinson's disease (−13.0%) and CAD (−10.5%), followed by depression (−7.8%) and dementia (−7.1%). Acute strokes (−12.1%), diabetes (−10.4%), MI (−9.3%) and cancer (−8.5%) experienced the largest decrease among specialists. Table 2 demonstrates the change in recognized diseases. A detailed description of the changed recognition of diseases over time is also demonstrated in Supplementary Appendix 2.
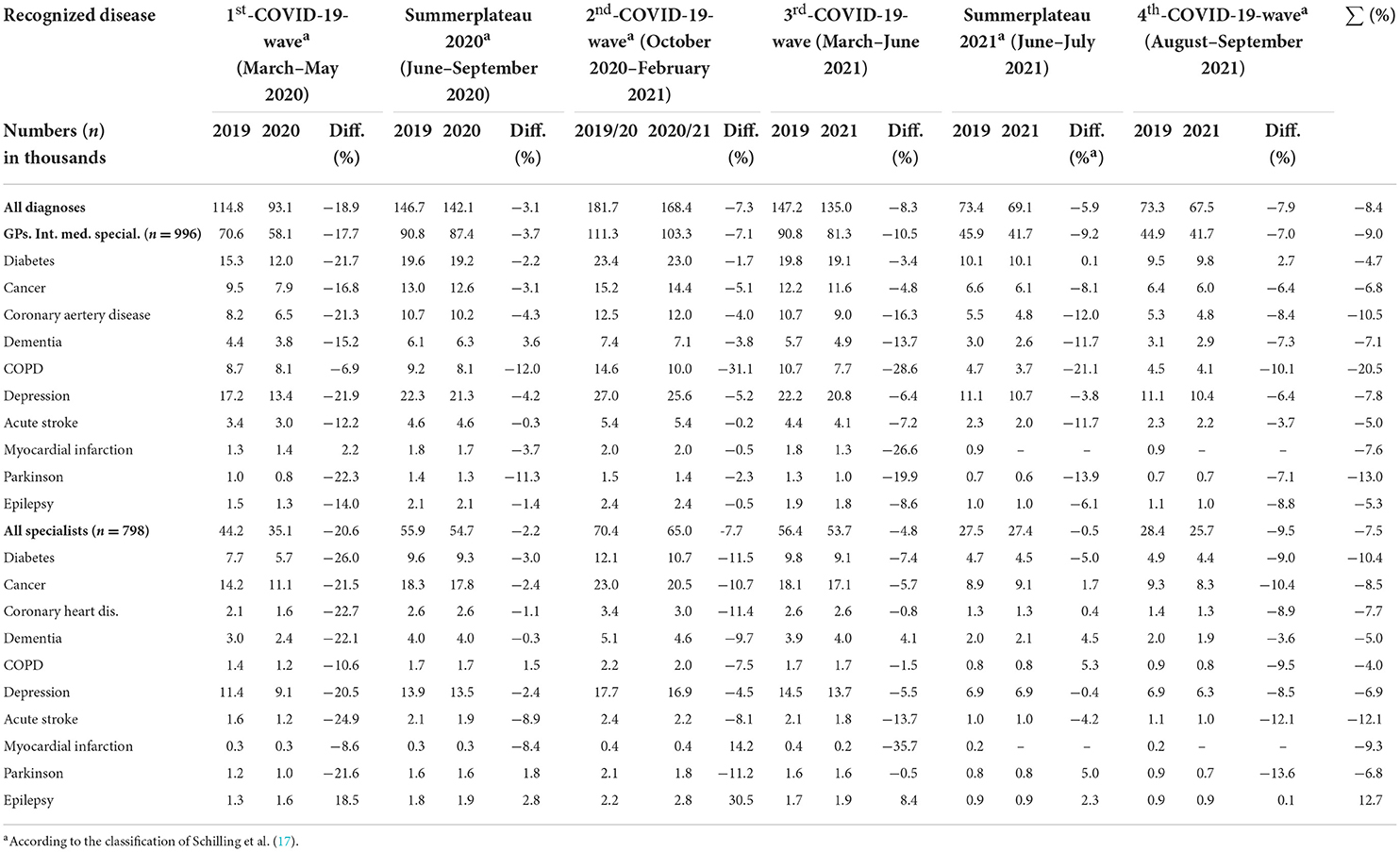
Table 2. Recognition of diseases during the COVID-19 pandemic in Germany compared to the pre-pandemic time frame 2019/20.
Practitioners' perception and causal reasons for the change in the healthcare provision and utilization
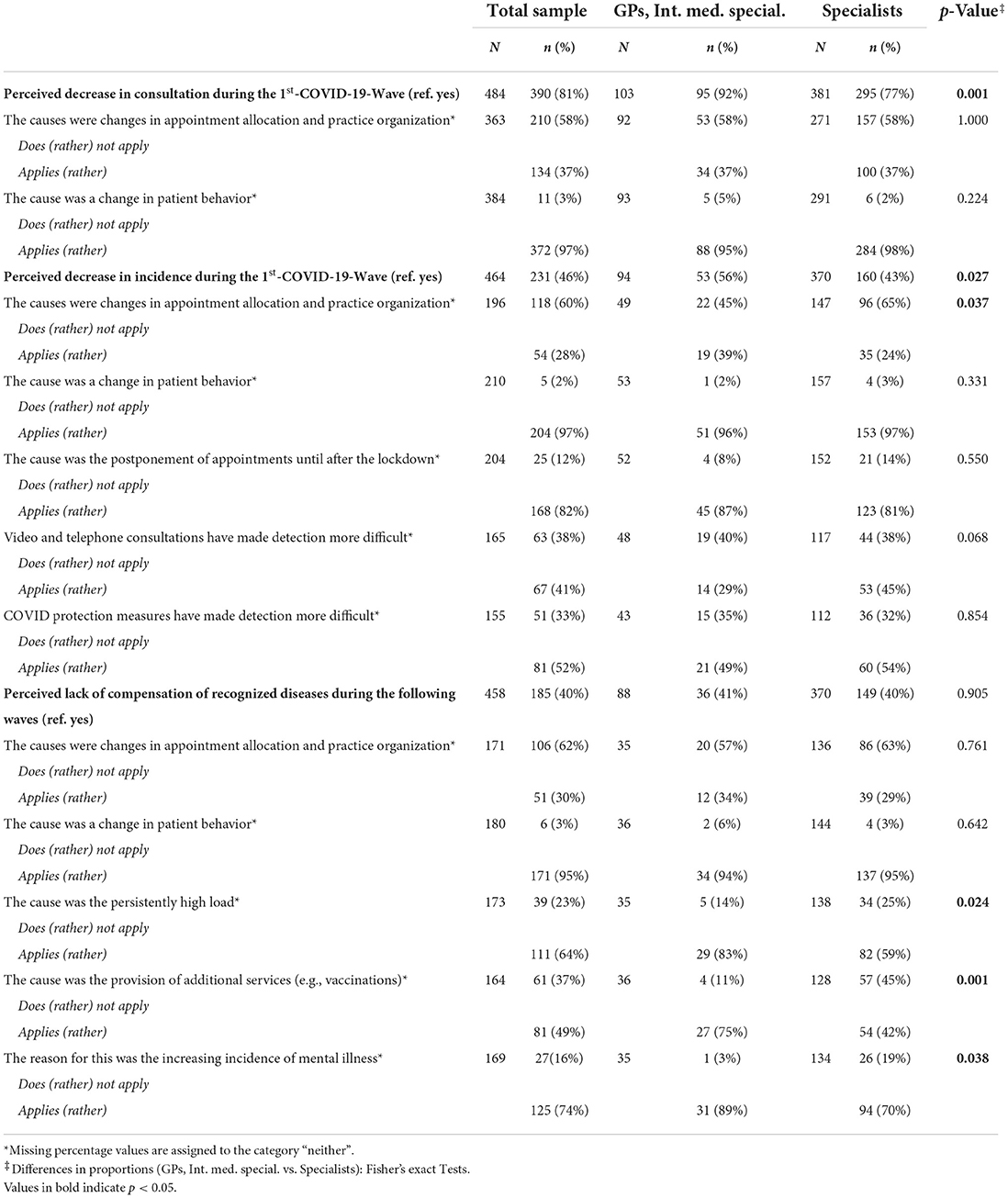
Table 3 summarizes the physicians' and practices' characteristics. The substantial decrease in primary care and specialist consultations was perceived by almost all physicians (81%), but especially in GPs practices (92 vs. 77%, p = 0.001). GPs and specialists surveyed saw the reasons for the decline primarily in changes in patient behavior (97% agreement). In contrast, less than half (48%) of physicians subjectively perceived the decline of the detection of diseases during the first lockdown - again, significantly more in GPs practices than in specialists' practices (56 vs. 43%, p = 0.027), also self-justified by changes in the patient behavior (97% agreement). In contrast, only 40% of physicians perceived a decline in the further course of the pandemic. Again, changed patient behavior (agreement in 95% of cases) was often considered the causative reason. Sixty-four perent of physicians, especially GPs (83 vs. 59%, p = 0.024), indicated the continued high burden, and the additional services such as vaccinations and corona testing prevented compensatory effects (75 vs. 42%, p = 0.001). Table 4 summarizes the survey results.
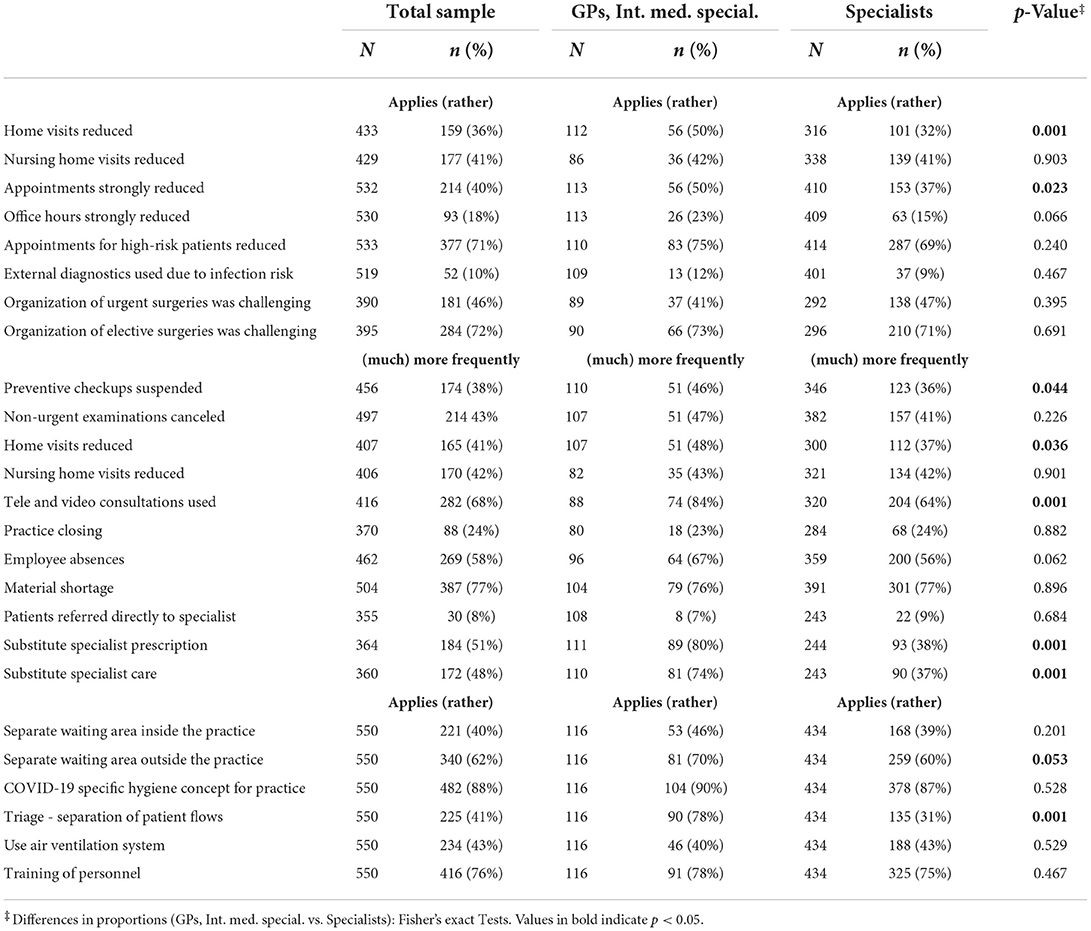
Change in practice management in primary care and specialist practices
Nearly half of the participating physicians stated that they reduced home visits (36%), nursing home visits (41%) and opening hours of the practice (40%) during the pandemic. This was seen more frequently in GP than in specialist practices. Thirty-eight percent and 43% of physicians reported that preventive checkups were suspended or non-urgent examinations canceled, respectively, more likely by GPs than specialists (46 vs. 36%, p = 0.044). 71% of surveyed GPs and specialists reported that appointments for high-risk patients for a more severe COVID-19 course were more likely canceled. GPs were also significantly more likely to use remote consultation (84 vs. 64%, p = 0.001). 80% of GPs also reported a provision of specialist prescriptions or specialist care in place of the specialists. Additionally, more than half of physicians (58%) experienced corona-related staff absences, and one in four practices were temporarily closed due to the absence and illnesses of practice personnel. Moreover, 62 and 40% of practices established a separate waiting area outside or within the practice. The changes in the practice segment are shown in Table 5.
Discussion
This analysis provided valuable evidence in healthcare services utilization and recognition of diseases in primary and specialized care during the COVID-19 pandemic and tried to illustrate physicians' perceived causes for the changes. The analysis elicited significant differences in the impact of the COVID-19 pandemic on the provision of routine care between primary and specialized practitioners. While GPs and internists could economically compensate the consultation rate over the entire pandemic due to additional services such as COVID-19 vaccinations, most specialists remained on a lower consultation rate. Specialist referrals, hospital admissions, and disease recognition decreased tremendously across all physicians but were stronger among GPs than specialists. Physicians perceived the decline in consultations but not the decrease in disease recognition. Nevertheless, reasons for the observed changes in healthcare utilization and disease recognition were seen by physicians in the changed patient behavior, especially in the postponement or cancellation of appointments during the COVID-19-related lockdowns. However, this study also revealed significant changes in practice management, like reducing nursing home visits and general home visits, shortened practice opening hours, suspended checkups and delayed consultations for high-risk patients. These changes could also impact the revealed changes in the healthcare provision, especially the detection of diseases.
Several studies have evaluated the impact of the early COVID-19 pandemic on primary care consultations, representing a dramatic decline (9, 11, 13, 14, 20). This analysis confirmed this decrease in outpatient consultations, especially at the beginning of the pandemic during the nationwide contact bans. However, the utilization of healthcare services provided by practitioners could partially be compensated over the further course. Schäfer et al. (13) found the effect was independent of specialty during the early stage of the pandemic, which is not in line with the results of this analysis, revealing tremendous differences between physician specializations. While GPs, internists, neurologists, urologists, and gynecologists could increase their consultations over the pandemic, orthopedists, dermatologists, and ENT specialists had a consultation rate deficit. For GPs and some other physician specializations, the upturn of the consultation rate correlated with the number of COVID-19 vaccinations given in primary and specialized care practices (21). The assumption of increased consultation rates due to COVID-19-related vaccinations is supported by the different perceptions of GPs and specialists. Moreover, prescription, hospital admission, specialists' referral, and disease detection rates did not compensate as the consultations did. On the contrary, these important rates decreased when the practices started with the vaccination. However, future studies need to confirm this assumption of increased COVID-19 vaccination-driven consultations and the coinciding occurrence of continuous negative trends regarding the other rates.
Additionally, the survey confirmed that the tremendous decline of consultations during the 1st-COVID-19-wave was perceived by the GPs (92%) and specialists (77%). However, while a patient-centered survey by Schuster et al. (22) revealed that the share of patient-initiated cancellations of primary care appointments was smaller than healthcare-initiated, only 37% of outpatient physicians surveyed in this study agreed that the decline could be traced back to the provider behavior, whereas 97% saw the cause in the changed patient behavior. Furthermore, recent studies support the thesis that the patient's behavior could be reasonable for the delay of outpatient service utilization regarding preventive care and visits for chronic diseases due to anxiety, reduced social activities, increased infection risk and a lack of perception of non-disabling symptoms (20, 23–26). The surveyed physicians supported these indications, confirming (97%) reasons for declined disease recognition remain in changed patient behavior. Moreover, 82% agreed with the cause that the postponement of appointments leads to this decrease. However, according to Bitzer et al. (27), patients lacked decision support to seek routine care during the COVID-19 pandemic, which could affect the demand for consultations under social distancing conditions. Further patient-centered research is, therefore, needed to evaluate the divergence and minimize the barriers to healthcare access in pandemic crises.
Further studies have already revealed a decrease in specialist referrals, hospital admissions and disease recognition during the first month of the COVID-19 pandemic (11, 13). The present analysis was in line with these findings. While the reduced number of hospital admissions was indicated by the limited number of beds in intensive care units, the decline in specialist referrals, especially by GPs and internists, could suggest a breach of the gatekeeping function usually associated with appropriate referral for specialty care (28, 29). This suggestion could be underlined by the not compensated decrease in disease recognition, which is also aligned with the literature, especially for diagnoses such as COPD, several types of cancer, dementia, acute stroke, CAD, and MI (23, 26, 30–33). However, not even half (46 and 40%) of physicians noticed this decline in recognition of diseases. A closer look at each physician's practice reveals that although these declines represent an enormous societal dimension, there were only −11.2 fewer diagnoses per GP practice and −6.4 fewer diagnoses per specialist practice over the entire pandemic. Therefore, whether individual practices or physicians could have perceived these decreases is questionable. These figures could likely be below a “perception threshold.” Alerting physician practices, indicating a significant declining trend, could be vital to impose countermeasures that aim to counteract the countervailing trend demonstrating a non-maintenance of routine primary care during pandemic times. Such solutions could be IT-based systems providing necessary information. Thus, further research about such interventions and the long-term impact of a reduced or delayed detection of diseases are highly relevant.
Limitations
It was not feasible to assess the extent to which emergency, urgent, and deferrable services were provided within the available diagnostic categories, limiting the assessment of whether individual physician practices properly prioritized diagnostic and treatment strategies in light of the high-risk situation and lockdown. While the reported results and discussion primarily comprise the summarized results over the entire study period, in-depth analyses of differences within waves were not the focus of this analysis. Further research is needed to highlight the differences between the respective stages of the pandemic, with greater attention to the various diagnoses and differences between age groups. Moreover, findings are related to treatment cases. Therefore, results do not allow conclusions to be drawn at the individual patient level because patient behavior was not captured in the available data.The primary data gained in the survey followed a cross-sectional design, limiting causal conclusions. In addition, the data is not representative of the statistical population of all physicians in Germany, especially regarding sociodemographic characteristics or the regional distribution, respectively. Furthermore, selection bias should be considered since data was collected via an online survey distributed by professional associations of specializations through their respective communication channels. The survey includes retrospectively asked questions drawn upon participants' memories. Therefore, possible recall bias should also be taken into account.
Conclusion
The COVID-19 pandemic significantly impacted primary and specialized care. Whereas specialist referral, hospital admission, and the diseases recognition rate steadily decreased over the COVID-19 pandemic, the initial decline in the physician consultation rate could be compensated at the end of 2021, probably due to additional service provisions such as COVID-19 vaccinations. GPs specialist referrals and hospital admissions also decreased much stronger than in specialist practices. Although most physician practices perceived the initial sharp decline of routine care, the number of non-detected diseases in each practice compared to the years before could be too minor for recognition in routine care practice. Physicians have seen patient behavior as the major contributor to this decline, comprising appointment cancellations or lacked decision support to seek routine care under social distancing conditions. However, changes in practice management may also have affected the tremendous decline in consultation, referrals, hospital admissions, and disease recognition. Mitigating the pandemic while maintaining routine care represents a major challenge for healthcare systems worldwide. Thus, decision-makers should divide responsibilities to ensure continued access to routine primary and specialty care on the one hand and to mitigate pandemics on the other. Furthermore, organizational and financial support for GPs and specialists' practices is urgently needed to prevent long-term adverse effects on patient outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The present study was reviewed and approved by the Ethical Committee of the Chamber of Physicians of Mecklenburg-Western Pomerania [Registry Number (BB 127/21)]. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
Author KK was an employee of IQVIA.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer AS declared a shared parent affiliation with the author JB to the handling editor at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1006578/full#supplementary-material
References
1. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. (2020) 395:1973–87. doi: 10.1016/S0140-6736(20)31142-9
2. Glass RJ, Glass LM, Beyeler WE, Min HJ. Targeted social distancing design for pandemic influenza. Emerg Infect Dis. (2006) 12:1671–81. doi: 10.3201/eid1211.060255
3. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. (2020) 27:taaa020. doi: 10.1093/jtm/taaa020
4. Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health. (2015) 105:1013–9. doi: 10.2105/AJPH.2014.302427
5. Lapolla P, Mingoli A, Lee R. Deaths from COVID-19 in healthcare workers in Italy-what can we learn? Infect Control Hosp Epidemiol. (2021) 42:364–5. doi: 10.1017/ice.2020.241
6. Bohlken J, Schömig F, Seehagen T, Köhler S, Gehring K, Roth-Sackenheim C, et al. [Experience of practice-based psychiatrists and neurologists during the COVID-19 pandemic]. Psychiatr Prax. (2020) 47:214–7. doi: 10.1055/a-1159-5575
7. Paffenholz P, Peine A, Hellmich M, Paffenholz SV, Martin L, Luedde M, et al. Perception of the 2020 SARS-CoV-2 pandemic among medical professionals in Germany: results from a nationwide online survey. Emerg Microbes Infect. (2020) 9:1590–9. doi: 10.1080/22221751.2020.1785951
8. Verhoeven V, Tsakitzidis G, Philips H, Van Royen P. Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish. GPs BMJ Open. (2020) 10:e039674. doi: 10.1136/bmjopen-2020-039674
9. Ekman B, Arvidsson E, Thulesius H, Wilkens J, Cronberg O. Impact of the Covid-19 pandemic on primary care utilization: evidence from Sweden using national register data. BMC Res Notes. (2021) 14:424. doi: 10.1186/s13104-021-05839-7
10. Howarth A, Munro M, Theodorou A, Mills PR. Trends in healthcare utilisation during COVID-19: a longitudinal study from the UK. BMJ Open. (2021) 11:e048151. doi: 10.1136/bmjopen-2020-048151
11. Michalowsky B, Hoffmann W, Bohlken J, Kostev K. Effect of the COVID-19 lockdown on disease recognition and utilisation of healthcare services in the older population in Germany: a cross-sectional study. Age Ageing. (2021) 50:317–25. doi: 10.1093/ageing/afaa260
12. Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. (2021) 11:e045343. doi: 10.1136/bmjopen-2020-045343
13. Schafer I, Hansen H, Menzel A, Eisele M, Tajdar D, Luhmann D, et al. The effect of COVID-19 pandemic and lockdown on consultation numbers, consultation reasons and performed services in primary care: results of a longitudinal observational study. BMC Fam Pract. (2021) 22:125. doi: 10.1186/s12875-021-01471-3
14. Xiao H, Dai X, Wagenaar BH, Liu F, Augusto O, Guo Y, et al. The impact of the COVID-19 pandemic on health services utilization in China: time-series analyses for 2016-2020. Lancet Reg Health West Pac. (2021) 9:100122. doi: 10.1016/j.lanwpc.2021.100122
15. Rathmann W, Bongaerts B, Carius HJ, Kruppert S, Kostev K. Basic characteristics and representativeness of the German Disease Analyzer database. Int J Clin Pharmacol Ther. (2018) 56:459–66. doi: 10.5414/CP203320
17. Schilling J, Buda S, Tolksdorf K. Zweite aktualisierung der “retrospektiven phaseneinteilung der COVID-19-pandemie in Deutschland”. Epid Bull. (2022) 10:3–5. doi: 10.25646/9787
18. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. (2007) 335:806–8. doi: 10.1136/bmj.39335.541782.AD
20. Velek P, Splinter MJ, Ikram MK, Ikram MA, Leening MJG, van der Lei J, et al. Changes in the diagnosis of stroke and cardiovascular conditions in primary care during the first 2 COVID-19 waves in the Netherlands. Neurology. (2022) 98:e564–72. doi: 10.1212/WNL.0000000000013145
21. Zentralinstitut für die kassenärztliche Versorgung (Zi). Current state of Vaccinations in Germany. (2022). Available online at: http://www.zidatasciencelab.de/covidimpfindex/ (accessed June 16, 2022).
22. Schuster NA, de Breij S, Schaap LA, van Schoor NM, Peters MJL, de Jongh RT, et al. Older adults report cancellation or avoidance of medical care during the COVID-19 pandemic: results from the Longitudinal Aging Study Amsterdam. Eur Geriatr Med. (2021) 12:1075–83. doi: 10.1007/s41999-021-00514-3
23. Maehl N, Bleckwenn M, Riedel-Heller SG, Mehlhorn S, Lippmann S, Deutsch T, et al. The impact of the COVID-19 pandemic on avoidance of health care, symptom severity, and mental well-being in patients with coronary artery disease. Front Med. (2021) 8:760265. doi: 10.3389/fmed.2021.760265
24. Stephenson E, Butt DA, Gronsbell J, Ji C, O'Neill B, Crampton N, et al. Changes in the top 25 reasons for primary care visits during the COVID-19 pandemic in a high-COVID region of Canada. PLoS ONE. (2021) 16:e0255992. doi: 10.1371/journal.pone.0255992
25. Thyrian JR, Kracht F, Nikelski A, Boekholt M, Schumacher-Schonert F, Radke A, et al. The situation of elderly with cognitive impairment living at home during lockdown in the Corona-pandemic in Germany. BMC Geriatr. (2020) 20:540. doi: 10.1186/s12877-020-01957-2
26. Uphaus T, Groschel S, Hayani E, Hahn M, Steffen F, Groschel K. Stroke care within the COVID-19 pandemic-increasing awareness of transient and mild stroke symptoms needed. Front Neurol. (2020) 11:581394. doi: 10.3389/fneur.2020.581394
27. Bitzer EM, Ansmann L, Horold M, Lyssenko L, Apfelbacher C. [“I better stay at home”-health system decisions to support the use of routine healthcare during the COVID-19 pandemic]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2021) 64:277–84. doi: 10.1007/s00103-021-03282-4
28. Sripa P, Hayhoe B, Garg P, Majeed A, Greenfield G. Impact of GP gatekeeping on quality of care, and health outcomes, use, and expenditure: a systematic review. Br J Gen Pract. (2019) 69:e294–303. doi: 10.3399/bjgp19X702209
29. Vincent JL, Creteur J. Ethical aspects of the COVID-19 crisis: how to deal with an overwhelming shortage of acute beds. Eur Heart J Acute Cardiovasc Care. (2020) 9:248–52. doi: 10.1177/2048872620922788
30. Axenhus M, Schedin-Weiss S, Tjernberg L, Wimo A, Eriksdotter M, Bucht G, et al. Changes in dementia diagnoses in Sweden during the COVID-19 pandemic. BMC Geriatr. (2022) 22:365. doi: 10.1186/s12877-022-03070-y
31. Borson S, Chen A, Wang SE, Nguyen HQ. Patterns of incident dementia codes during the COVID-19 pandemic at an integrated healthcare system. J Am Geriatr Soc. (2021) 69:3389–96. doi: 10.1111/jgs.17527
32. Jacob L, Loosen SH, Kalder M, Luedde T, Roderburg C, Kostev K. Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in germany. Cancers. (2021) 13:408. doi: 10.3390/cancers13030408
Keywords: COVID-19, healthcare utilization, disease recognition, hospitalization, primary care
Citation: Platen M, Bohlken J, Hoffmann W, Kostev K and Michalowsky B (2022) The long-term impact of the COVID-19 pandemic on primary and specialized care provision and disease recognition in Germany. Front. Public Health 10:1006578. doi: 10.3389/fpubh.2022.1006578
Received: 29 July 2022; Accepted: 31 October 2022;
Published: 17 November 2022.
Edited by:
Christos Lionis, University of Crete, GreeceReviewed by:
Anne Schrimpf, Leipzig University, GermanyGuenka Ivanova Petrova, Medical University Sofia, Bulgaria
Alexander Avian, Medical University of Graz, Austria
Copyright © 2022 Platen, Bohlken, Hoffmann, Kostev and Michalowsky. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bernhard Michalowsky, YmVybmhhcmQubWljaGFsb3dza3lAZHpuZS5kZQ==
 Moritz Platen
Moritz Platen Jens Bohlken2
Jens Bohlken2 Karel Kostev
Karel Kostev Bernhard Michalowsky
Bernhard Michalowsky