
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 30 September 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1001282
This article is part of the Research TopicPublic Perspectives on Health and WellbeingView all 24 articles
Introduction: Shared decision-making (SDM) and trust building through continuity of care are known to play a pivotal role in improving appropriate antibiotic prescribing and use.
Problem: However, less is known about how to effectively leverage these factors when present—or overcome them when not—to address community needs and improve patient liaison.
Methods: We addressed this question using a convergent parallel mixed-methods design. Focus group discussions (N = 13; August 2018–September 2020), were analyzed alongside a nationally-representative cross-sectional survey (N = 2004; November 2020–January 2021), in Singapore. Descriptive quantitative analyses and multivariable logistic regression were undertaken to examine antibiotic knowledge and factors associated with preference for SDM. Qualitative applied thematic analysis was integrated with these data to further explain the findings.
Findings: Poor knowledge and misbeliefs on appropriate antibiotic use and antimicrobial resistance (AMR) were identified. For example, only 9% of the surveyed population understood that AMR occurs when the bacteria, not the human body, become resistant to antibiotics. Qualitative data corroborated the survey findings and suggested a shared value was placed on public education to avoid the fallout from resistant bacterial strains on current and future generations. This study also identified the opportunity to harness community trust in primary care doctors, who were described as highly valued educators for antibiotic use and AMR. Those who had trust in doctors were 75% more likely to prefer SDM (aOR 1.75, 95% CI 1.10–2.77, P = 0.017), especially adults aged ≥50 years who were receiving continued care with a regular doctor (aOR 1.83, 95% CI 1.18–2.86, P = 0.007). Continuity of care was observed to value-add SDM by building trusting relationships, though it was often absent in younger populations.
Conclusion: This study highlights the long-term value-add of building on cultural capital pertaining to appropriate antibiotic use and AMR, by leveraging on the role of trust in doctors, desire for SDM and anchoring these in continuity of care when possible.
Recommendations: Using focused messaging and exploring alternative channels of communications such as annual check-ins or tele-consultations with a regular doctor, and emphasizing continuity of care across all age groups would help bridge the identified gaps.
Global annual mortality attributable to antimicrobial resistance (AMR) was projected to reach 10 million by 2050 (1). This estimated number is comparable with the annual global excess death count of an average of 7.5 million reported for the coronavirus disease 2019 (COVID-19) in the first 2 years of the pandemic (2), suggesting an urgent need to slow down AMR progression before it becomes the next pandemic.
Overprescribing of antibiotics is one of the major causes of AMR (3). Reasons include patient demands, clinical uncertainties, fear of missing diagnosis, and fear of medico-legal issues (4–10). However, one-sided information delivery through educational materials focused on encouraging doctors to improve appropriate antibiotic prescribing and nationwide campaigns to raise public awareness on AMR have limited effects (11–13). In contrast, systematic reviews have shown that shared decision-making (SDM) between patients and doctors enables better chances of reducing inappropriate antibiotic prescribing and use (11, 14, 15). Furthermore, the process of SDM is known to be buoyed up by receiving continuity of care from a regular doctor, and having mutual trust (7, 16–18). The importance of these relationships has been explored in a qualitative study conducted amongst primary care doctors practicing in Singapore, which has positioned these constructs at the core of a VALUE model of SDM for antibiotic prescribing (18).
The model highlights the importance of starting with—building up when lacking or drawing on when present—the doctor's own values and organizational culture to adhere to recommended practice and optimal patient care. Nevertheless, not every context will present the opportunity to influence or leverage such values. Continuity of care is not always possible, and trust takes time. In some cases, trust may be hard to win, if ever. To better navigate such scenarios, the central role of patients in navigating decisions around antibiotic use and adherence needs to be better understood. So far, existing literature indicates that the public's perceptions of SDM have been less explored, in favor of appraising satisfaction with clinical consultations post-SDM (11, 14).
Accordingly, the current study aims to better understand how to support the VALUE model's application in the primary care setting by accounting for the community's perspective and how to improve patient liaison around recommended antibiotic practices. We use a mixed-methods design informed by social and behavior change communication (SBCC) traditions (19) to firstly, assess gaps in knowledge, as well as intentions and behavioral follow-through to inform related messaging needs. Next, we examine for whom trust in doctors, continuity of care and SDM are valued to inform targeting for practitioner-led intervention design. Lastly, we explore the role of trust, how it is established and in particular how trusted sources can be leveraged via multiple channels to share information.
Our study defines SDM, following Elwyn et al. as a three-step process: (a) providing reasonable options to patients, (b) using decision aids to describe these, and (c) exploring patient preferences and making choices together with the doctor (20). The planned analysis acknowledges these steps, starting with defining specific knowledge and intentions or behavioral gaps that help to define how “reasonable options” to use antibiotics appropriately should be messaged and communicated. In addition, we opted to dig deeper on understanding how to target these decision aids, building on a previous study conducted in Singapore, which highlighted that poor knowledge of antibiotic use and AMR in younger age groups drives larger extents of inappropriate antibiotic practices (21). Lastly, best channels through which related information may be strategically used are assessed. Existing channels and campaigns in our present context are discussed below.
Overall, these analyses will help us identify areas for theory-informed intervention design and strategic implementation to improve antibiotic use in the primary care setting, via SDM processes, adding to what is already know from the practitioner's perspective, based on the existing identified VALUE-driven model (18).
This is a convergent parallel mixed-methods study. A nationally-representative community-based survey was conducted (November 2020–January 2021) on a randomly selected sample of Singapore residents (citizens and permanent residents) aged 21 years and above. The sampling frame and data collection methods are fully reported elsewhere (21). Separately, 13 focus group discussions (FGDs) were conducted (August 2018–September 2020). The Standards for Reporting Qualitative Research (SRQR) (22) was used to report qualitative methods, and quantitative procedures were integrated within.
All study methods and procedures were reviewed and approved by the National Healthcare Group Domain Specific Review Board of Singapore (Reference Number: 2017/01179).
The survey was conducted during the COVID-19 pandemic (November 2020–January 2021), after a national lockdown was lifted. Working adults, who were previously office-based, remained mostly in a “work-from-home” mode. Majority of students enrolled in higher learning institutes were attending classes online. On the other hand, FGD recruitment was disrupted by the COVID-19 pandemic (January 2020–August 2020) due to the early stages of national containment of community COVID-19 transmission. FGDs were resumed and completed in September 2020 with strict compliance to the nation's safe management measures.
Between 2018 and 2020, the annual AMR campaign message by the Singapore Health Promotion Board was “Fighting the flu virus is not my battle. Talk to your doctor for the treatment you need” (23). It was intensively disseminated through posters at public areas (bus stops, rapid transit system stations), brochures, tissue packs, television advertisements, social media posts and YouTube advertisements during the annual World Antibiotics Awareness Week in November.
The survey questionnaire addressed antibiotic use and AMR. These included questions on knowledge, trust in information sources and doctors, as well as continuity of care, which were selected for analysis.
Knowledge questions were presented as True/False/Don't know. Questions on attitude and trust in doctors were presented in a 5-point Likert scale (strongly disagree to strongly agree) and dichotomized in the manner described below. Trust in information sources for health-related matters or medicines was presented in a 5-point Likert scale (never to completely) and dichotomized into 2 categories: trust (moderately/a lot/completely) vs. do not trust (never/rarely). Additional demographic information was also collected.
The dependent variable was defined by the statement “I would want my doctor to discuss with me and make the decision on antibiotic prescribing with me” (24). Respondents who agreed to this statement (strongly agree/agree) would be categorized as preferring SDM on antibiotic prescribing with their doctors. The independent variable on patient-acquired, all-round trust in doctors was tabulated using a composite score. It was composed of a 9-statement scale developed by Hall et al. (25), and agreement (strongly agree/agree) to all 7 positive statements, and disagreement (neither agree or disagree/disagree/strongly disagree) to both negative statements.
Positive statements included: (1) doctors in general care about their patients' health just as much as their patients do, (2) doctors are extremely thorough and careful, (3) I completely trust doctors' decisions about which medical treatments are the best, (4) doctors are totally honest in telling their patients about all the different treatment options available for their conditions, (5) doctors think only about what is best for their patients, (6) doctors always use their very best skill and effort on their patients, and (7) I have no worries about putting my life in the hands of doctors.
Negative statements were: (1) sometimes doctors care more about what is convenient for them than about their patients' medical needs, and (2) sometimes doctors do not pay full attention to what patients are trying to tell them.
Lastly, another independent variable on continuity of care was defined as reportedly seeking medical attention from a regular doctor.
Proportions were tabulated and chi-squared test was used to compare differences between them. Multivariable logistic regression was then performed to determine the independent factors associated with preference for SDM on antibiotic prescribing with doctors. Covariates were selected through assessing the Akaike information criteria, Bayesian information criteria and likelihood ratios, and included in the final regression model to adjust for potential confounding. Interactions between covariates were individually explored and product terms were also included in the final model. Effect measure modification due to socio-demographic factors was further assessed. Statistical significance was defined as P-value < 0.05. Statistical analyses were conducted in Stata version 14.0 (StataCorp LLC, College Station, Texas US).
A semi-structured topic guide (Supplementary File Annex 1) was developed by HG (Female, MPH, Research Fellow) based on previous findings from the literature (26–32). Pilot interviews were conducted with co-workers of varying educational levels and with no prior medical knowledge to ensure content validity and proper phrasing of questions. Three research assistants, all females, bilingual graduates and trained in qualitative fieldwork, facilitated or took notes for the FGDs in the preferred language of the participants (English, Mandarin, Malay or Tamil).
Invitation letters were disseminated to the community through community networks or recruitment drives. Interested members of the community left their contact details with the study team and were later contacted via email or telephone. Informed consent and basic demographic details were collected on the day of the FGD. Each FGD lasted for 90 mins. The topic guide consisted of questions pertaining to knowledge, attitudes and perceptions toward antibiotic use and AMR, antibiotic practices and also interactions with primary care doctors on the use of antibiotics.
Singapore residents (citizens and permanent residents) aged 21 years and above were purposively sampled with maximum variation to ensure representation from different ethnic (Chinese, Malay and Indian) and age (21–49 years old and ≥50 years old) groups. A good mix of education level was also considered. To reach data and meaning saturation (33), at least two focus groups were required per stratum (i.e., older Chinese, younger Chinese, older Malay, younger Malay, older Indian and younger Indian). Hence, in this study, a minimum total number of 12 focus groups was planned. All potential participants were screened and included in the study if they were able to answer the question “Do you know what are antibiotics?.”
Each FGD was audio-recorded and data were transcribed verbatim. Applied thematic analysis was undertaken (34). Steps included data familiarization, segmenting the data according to topics pertinent to the current study objectives, and agreeing on a coding framework, as well as describing emergent themes. The coding framework was guided by identification of elements of VALUE model for antibiotic prescribing in the primary care setting (18). These included knowledge and understanding of antibiotic use and AMR, the presence and role of continuity of care, trusting patient-doctor relationship and active liaison with patients that lead to SDM processes on antibiotic prescribing. ATLAS.ti 9 was used to manage the qualitative data and record emergent themes.
Regular meetings were conducted with a senior member of the team. Emergent themes and sub-themes were discussed and a consensus reached on the meaning of the data. Saturation was judged to have been achieved at over two-thirds of the way through the coding process.
Both datasets were analyzed separately and integrated at the reporting stage as appropriate. Qualitative main themes are reported by highlighting these in bold-italics, while supporting themes are narrated alongside these. Each objective is addressed in turn.
Out of 4791 households approached, 2004 (41.8%) respondents took part in the survey. They were representative of the Singapore population in 2020 (35), and most sought antibiotics from a GP and had a regular doctor (Supplementary Tables S1, S2). Thirteen FGDs were conducted, with a good distribution of ethnic groups and balance of education level, diversity of gender and ages was also achieved (Supplementary Table S3).
Descriptive quantitative analyses are summarized in Figures 1A–D. These findings are integrated with qualitative thematic analyses, summarized in Tables 1, 2 with illustrative quotes.
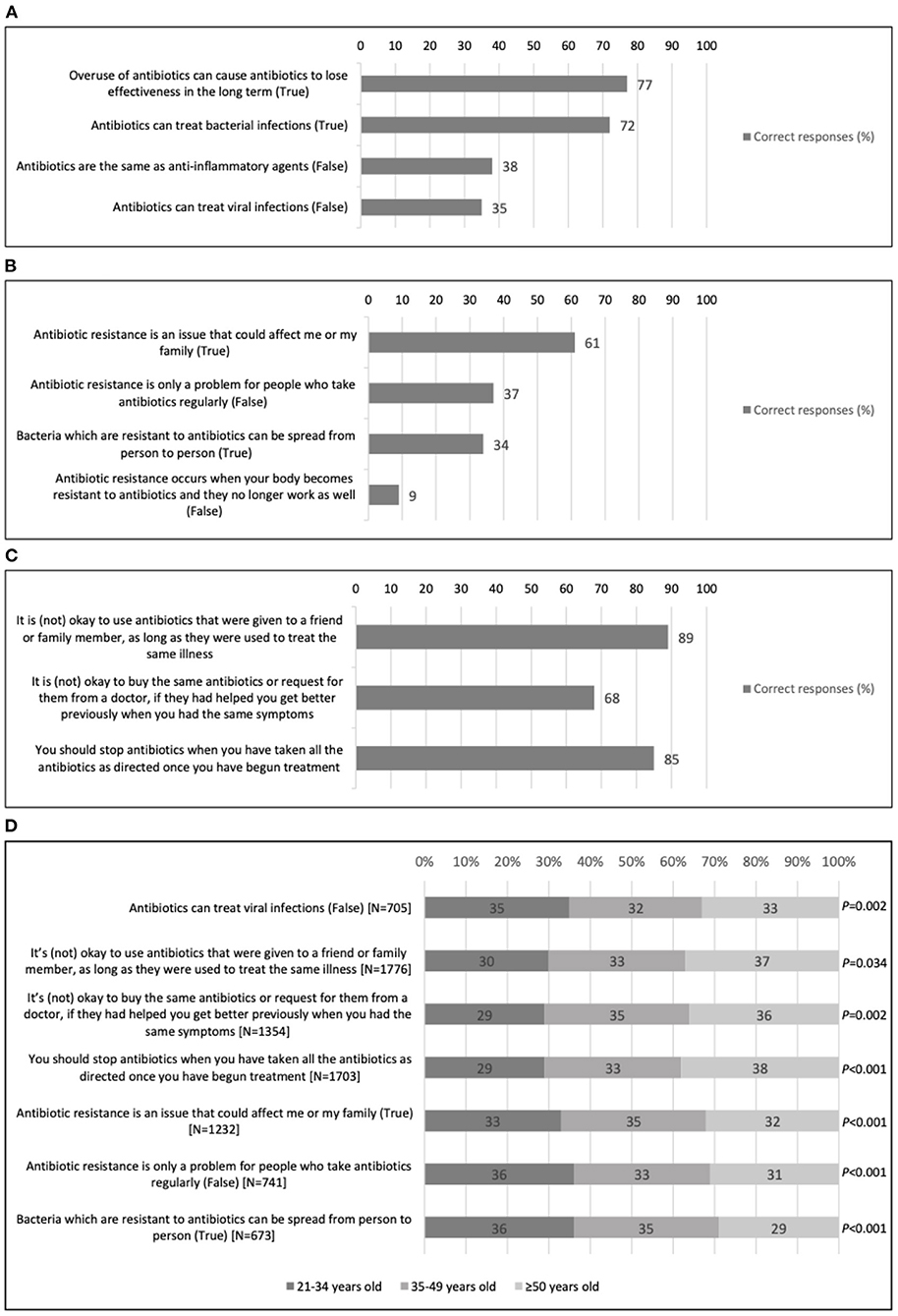
Figure 1. Proportion of correct responses from 2004 Singapore residents on statements pertaining to antibiotic use and antimicrobial resistance (AMR), surveyed between November 2020 and January 2021. (A) Knowledge of statements related to understanding how antibiotics work. (B) Knowledge of statements related to antimicrobial resistance (AMR). (C) Knowledge related to appropriate ways of obtaining and taking antibiotics. (D) Understanding differences in correct response in (A–C), stratified by age (only significant trends reported).
Quantitative data showed a good understanding surrounding the need for using antibiotics cautiously and intentionally (Figure 1A). For instance, a large proportion knew that overuse of antibiotics can cause them to lose effectiveness in the long term (77%). It was also largely known that antibiotics are for the treatment of bacterial infection (72%), even though other misconceptions existed. These misconceptions centered on far fewer recognizing the falsehood that antibiotics could be used to treat viral infection (35%) and believing that antibiotics had anti-inflammatory properties (38%).
Qualitatively, see Table 1A, we identified specific gaps in the community's knowledge around reasons to take and minimize antibiotic use where appropriate, which corroborated with the above.
These included the explicit inability to differentiate between bacteria and viruses. Also, the misconception that an antibiotic is the same as a painkiller, or an anti-inflammatory agent. Furthermore, the underlying rationale as to why the overuse of antibiotics would interfere with their effectiveness in the long term was misunderstood: it was seen as leading to the “body building immunity” against the antibiotics, not the bacteria itself becoming resistant. Relatedly, one participant also had the erroneous thought that antibiotics are taken to strengthen one's immune system. These beliefs had influence over how antibiotics were taken, as explained below.
In general, the term “antibiotic resistance” was incomprehensible to the community (Figure 1B). Echoing previously shared qualitative findings, only 9% of the respondents realized that it is erroneous to believe that AMR occurs when the body becomes resistant to antibiotics. Relatedly, just 34% were aware that bacteria which are resistant to antibiotics can spread from person to person. Overarchingly, qualitative findings showed a poor understanding of AMR and indicated that lay beliefs rather than scientific consensus were commonly being used to define the term “antibiotic resistance.”
The term was being used to infer mechanisms that only affect those who overdose on or overuse antibiotics, and therefore would need even more antibiotics to achieve an effect or the body itself had developed resistance to the antibiotic. Some expressed that the effects of antibiotic resistance were cumulative by age, since older adults would have taken more of such medications over their life time. Such rationales may explain why 61% of survey respondents reported that antibiotic resistance was an issue that may affect them or their families, despite most not understanding the mechanism by which this occurred.
Most respondents in the survey reported that they understood that antibiotics should not be shared with others (89%) and that they should be taken as directed (85%) (Figure 1C). Despite these quantitative results, focus group participants commonly shared that it was not unusual for them or their family members to not finish a full course of antibiotics once they started to feel better. Qualitative data highlights while the best ways to obtain antibiotics and the advice on taking them was generally known, this did not always translate to good practices (Table 1B). The misconception that the body, not the bacteria, became resistant was one reason why the full dose of prescribed antibiotics might not be completed.
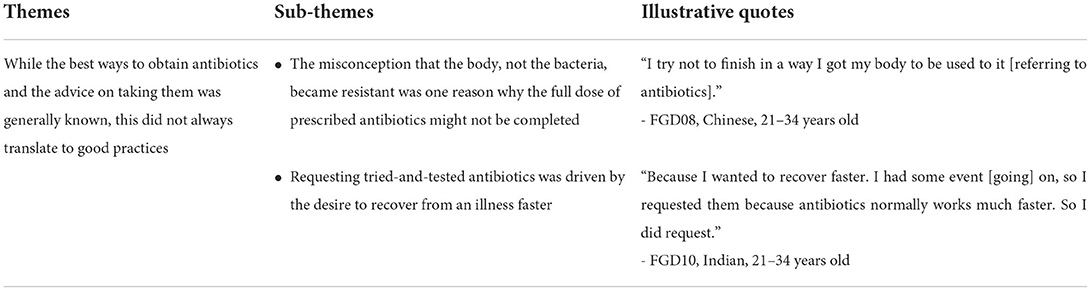
Table 1B. Intentions and behavioral follow-through, themes collated from focus group discussion data.
In addition, 68% of survey respondents correctly responded that it would not be advisable to buy the same antibiotics or request them from doctors simply because these had helped with similar symptoms previously (Figure 1C); while focus group participants often described such a request as being reasonable because it was driven by the need to recover from an illness faster. There were small differences by age in knowledge (Figure 1D); in general, those aged 35 years and older were more apt at answering correctly on the appropriate ways of obtaining antibiotics while younger people had marginally better understanding of statements relating to AMR.
Quantitative descriptive results are collated in Figure 2 and regression analyses are summarized in Tables 2A,B. Analyses are presented by stratifying age, and they also built on existing findings which have shown that poor knowledge of antibiotic use and AMR and inappropriate antibiotic use in the general population are modified by age; with younger adults being less informed and likely to have worse outcomes (21).
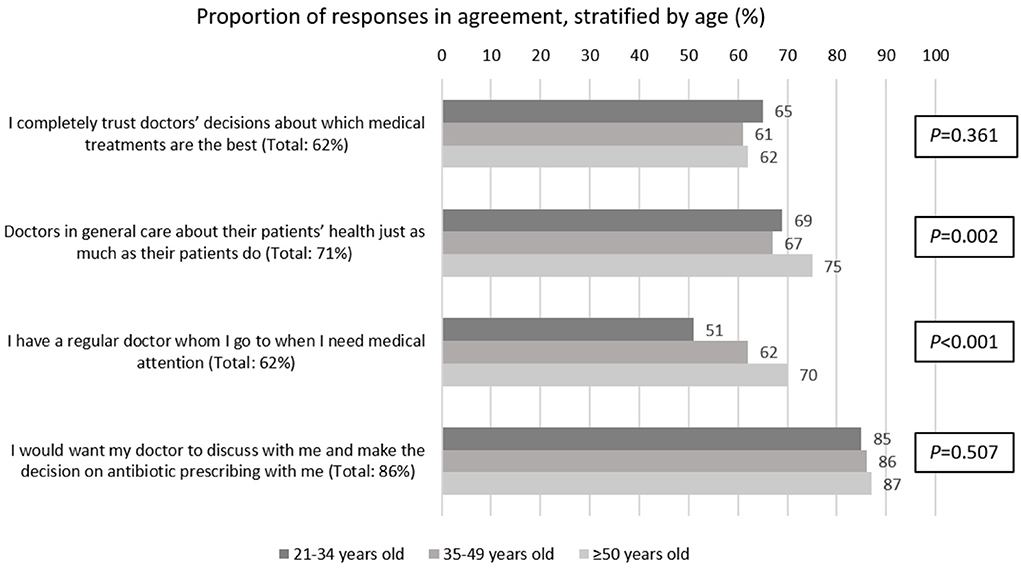
Figure 2. Proportion of responses from 2004 Singapore residents, surveyed between November 2020 and January 2021, agreeing to these statements pertaining to trust in doctors, continuity of care and shared decision-making (SDM) for antibiotic prescribing, stratified by age.
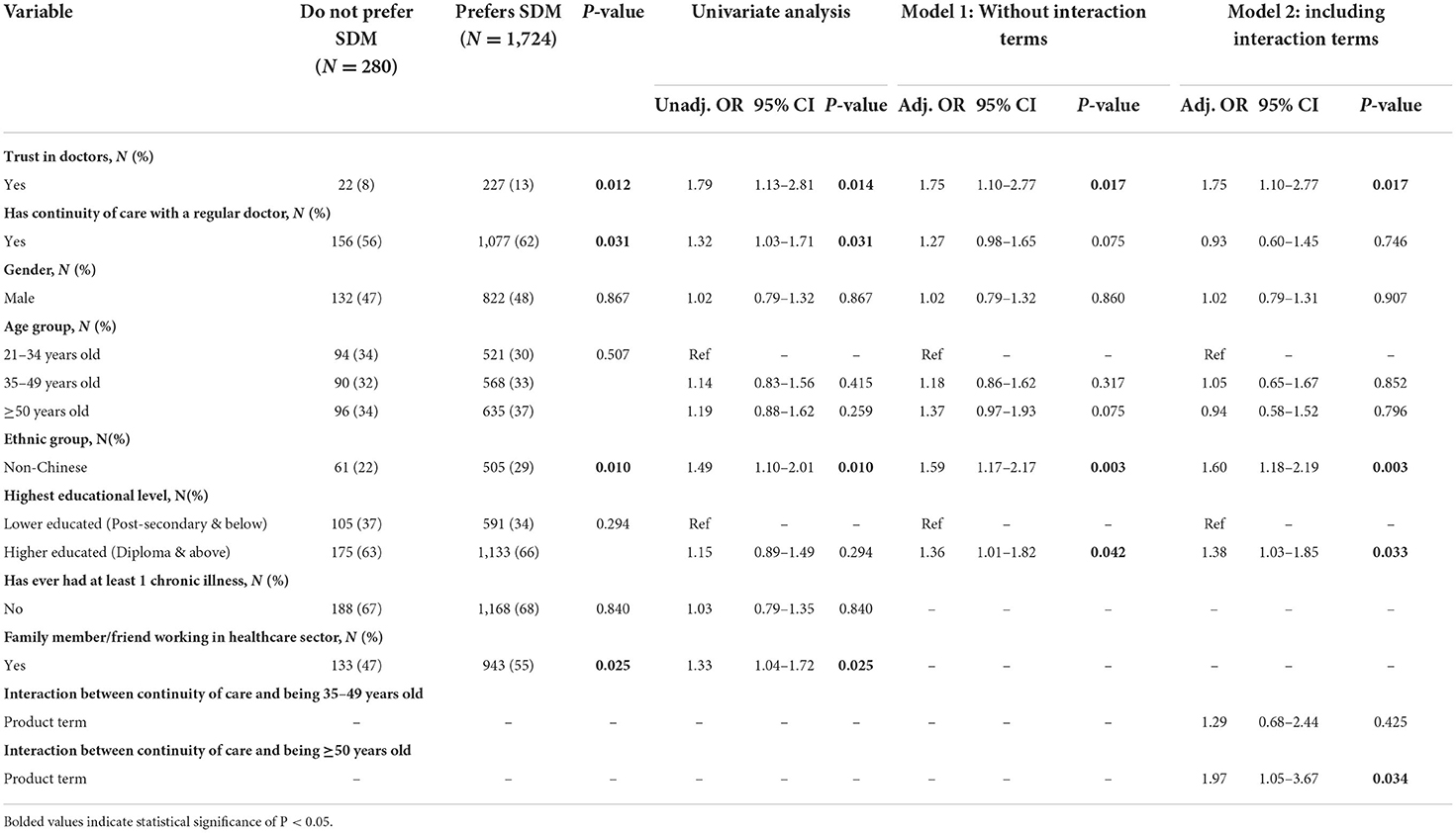
Table 2A. Univariate and multivariable logistic regression examining factors associated with preference for shared decision-making on antibiotic prescribing, N = 2004.

Table 2B. Association between preference for shared decision-making on antibiotic prescribing and continuity of care, according to age group, N = 2004.
Overall, in the present study, only a small majority of 62% reported having complete trust in doctors' decisions about which medical treatments are the best (Figure 2). Descriptive data showed a small effect of age relating to general trust in doctors, with those aged ≥50 years being most likely to believe that doctors in general care about their patients' health just as much as their patients do (21–34 years old: 69%; 35–49 years old: 67%; ≥50 years old: 75%, P = 0.002). Similarly, amongst the 62% of respondents who had continuity of care with a regular doctor, there were larger proportions of older respondents who medically attended with a regular doctor (21–34 years old: 51%; 35–49 years old: 62%; ≥50 years old: 70%, P < 0.001). In contrast, quite a few more (86%) reported a preference for SDM but there was no statistically significant difference between age groups on such preference (21–34 years old: 85%; 35–49 years old: 86%; ≥50 years old: 87%, P = 0.507).
Upon adjusting for potential confounders, respondents who scored as trusting their doctors based on the scale measuring all-round trust in doctors, as developed by Hall et al. (25), were 75% more likely to prefer SDM when seeking antibiotic prescriptions (aOR 1.75, 95% CI 1.10–2.77, P = 0.017) (Table 2A). Though there was no significant effect from continuity of care on preference for SDM after adjusting for potential confounders, there was a significant multiplicative effect of age on these associations (Table 2B). In those aged 50 years and above, it was found that when seeking antibiotics, those with continuity of care were 83% more likely to prefer SDM with their doctors, compared to those without it (aOR 1.83, 95% CI 1.18–2.86, P = 0.007).
Descriptive quantitative analyses stratified by age are listed in Figure 3. These findings are supplemented with qualitative thematic analysis, summarized with illustrative quotes in Tables 3A–C.
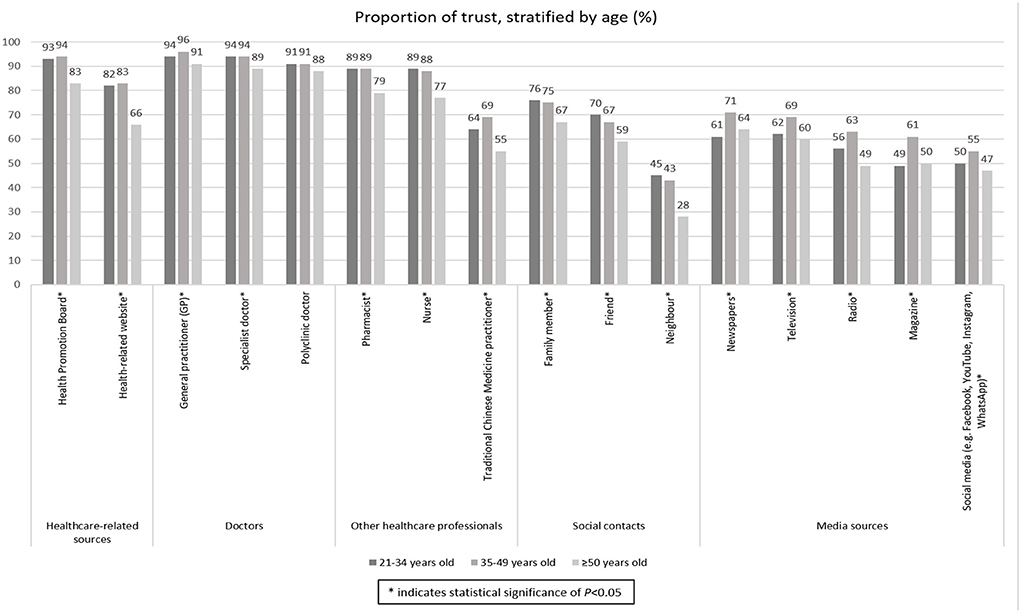
Figure 3. Proportion of trust on different health information sources of 2004 Singapore residents surveyed between November 2020 and January 2021, stratified by age. The * was used to denote categories with statistical significance.
Though older people were shown to have better continuity of care and apparent interpersonal relationships with their doctors, trust in doctors was cross-cutting across age bands, see Figure 2, which shows no significant difference across age bands for having complete trust in doctors' decisions about medical treatments. Similarly, when asked about preferences for trusted sources to gain information on health-related matters or medicines (Figure 3), there were very small differences across age bands on preferences for doctors. Indeed, general practitioners (GPs) were reported as most trusted by all age bands compared to all other proposed channels of acquiring information. However, younger people were more receptive to information by other health professionals such as nurses, as well as social contacts such as friends and family, than those over 50 years of age.
Qualitatively, consensus across the age bands emerged pertaining to main themes such as the value-add through taking time to build trust (Table 3A) and enable SDM, as shown in Table 2A. It was shared that in some cases, trust between patients and doctors was not a given. Ways of doing this pivoted around better communication and sharing of knowledge. There was a clear demand for and expression toward valuing of public education on appropriate antibiotic use and AMR. The importance of twinning trusted role of doctor with outreach and scientific information dissemination was pointed out as a basis for protecting current and future generations from the risks of antibiotics being rendered ineffective. This was corroborated by an observed lack of public outreach on AMR as compared to other chronic or lifestyle diseases, e.g., diabetes.
The valuing of SDM on antibiotic prescribing (Table 3B) was also notable by the expressed desire to have healthcare professionals as main focal point of education, supplemented by the use of other channels of communication and use of decision aids. In addition, it was shared throughout the focus groups that initiation of SDM was experienced as a “matter of course”—it may or may not happen. Interestingly, communication to redress this lack of SDM, for instance tackling poor knowledge and empowering patients, was perceived as the doctor's responsibility.
Lastly, the valuing of continuity of care (Table 3C) was directly connected to valuing existing relationships with ones' doctors. Continuity of care was also enabled or hindered by practical factors, such as proximity, waiting times, speed and efficiency of diagnosis etc. It was clear that continuity of care, though often preferred, may not always be possible. Models of primary care provision will need to account for such situations and enable ways of encouraging seeking and receiving medically sound advice when the potential need for antibiotics presents, despite these limitations.
This study provides important insights on what were the community's needs which should be addressed before and during SDM. It emphasizes the role of trust on educating patients to address their needs, promoting continuity of care and influencing their acceptance and desire for SDM with their doctors on antibiotic prescribing in primary care settings. The central role of trust in driving the community's preference for SDM with their doctors on antibiotic prescribing was evident, with those who trusted their doctors being far more likely to prefer SDM, as compared to those who did not trust their doctors.
SDM was not an unfamiliar concept within the community, with many wanting this to happen when seeking antibiotics and others sharing that primary care doctors were already practicing this. However, the community lacked empowerment to actively take part in SDM, despite their desires, due to a lack of medical knowledge, as self-perceived and as shown in current and previous quantitative findings (21). Being equipped with right information to make informed choices is key during SDM (20). There were obvious knowledge gaps of both antibiotic use and AMR, and presence of misbeliefs surrounding these topics amongst the community, which translated to inappropriate antibiotic use.
These study findings are reflective of existing literature (21, 36–38), though our qualitative findings further revealed that there could be reasonable intentions behind undesirable antibiotic practices. Our study also informs a model of how to build on the community's valuing of SDM and leverage the importance of following appropriate antibiotic behaviors to minimize the potential for AMR development and preserve present and future generations' access to effective antibiotic treatments. Desired antibiotic behaviors include seeking medical consultation before taking antibiotics, rather than demanding them; following doctor's advice on how to take them; and not sharing them with others or stocking them for future use unnecessarily.
The mixed-methods data informs a model of strategic planning by using cultural capital to value-add, and build on what is known, using: tailored message content design following the 7Cs of public health communications (39) (see Supplementary Table S4, for suggested message content); funneling these into desired behaviors using appropriate, age-segmented, targeted, multi-channel intervention aids extracted from our findings (Figure 4). Message content needs to be clear and consistent regardless of communication modality used and, we suggest, spearheaded or endorsed by the highly trusted medical professionals, especially GPs, partnering with the Health Promotion Board or the Regional Health Systems through community-based campaigns. Traditional modes of communication such as hardcopy decision aids (including pamphlets) and newspaper articles are preferred and recommended for older adults (21, 40) but innovations to digitalize and/or gamify these materials and place at social locations should be considered to reach the tech-savvy and highly social younger adults.

Figure 4. A strategic implementation model to guide the designing of interventions to improve appropriate antibiotic use in the general public.
At the interpersonal level, first and foremost, the investment in building trusting relationships between patients and doctors will also value-add and is well known to make medical consultations more effective. The cyclical interdependency between continuity of care and trust is key to enabling SDM processes and must not be underestimated. The practices of enrolling with one primary care doctor should be recommended at the national level and patients making annual check-in visits (especially for older adults) or having tele-consultations with a regular doctor (particularly for younger adults) should be encouraged. These touch points should be harnessed to distribute decision aids or message cards with focused and consistent evidence-based messages on appropriate antibiotic use and AMR. These can also be made available on “café cards” or posters through identified community networks with messages crafted to spark discussion, social engagement and awareness of AMR, and the potential effects of this on current and future generations.
In fact, the strategy of engaging healthcare professionals as educators and SDM facilitators was well supported. As highlighted in a recent systematic review conducted to assess the role of education in antibiotic stewardship (41), the distribution of passive educational materials to educate patients on antibiotic use without the presence of an active educator yielded negligible effects on improving antibiotic prescribing in the primary care setting (42–45). In contrast, the active involvement of adult patients and parents in SDM processes, through the use of a visual tool to clarify their values and preferences on antibiotics via conversations with their doctors, resulted in a 25% reduction of unnecessary antibiotics prescribed for upper respiratory tract infections (46). Educational tools were found to be impactful only when used as SDM decision aids; public engagement and education were also recommended to involve both doctors and community partners (41).
Such a strategy should aim to consciously streamline and design information flow, appealing to both younger and older generations, and especially drawing in younger adults. Younger adults are known to passively gather a variety of information via personal and friendship networks (47–50), including the Internet. Campaigns focused on inter-generational benefits and encouraging sharing about how to avoid AMR will increase the diffusion of messages and effectiveness of campaigns.
Coincidentally, our recommended strategic model aligns with a recent national healthcare reform in the community to build a healthier population in Singapore. From 2023 onwards, enrolment to a single preferred primary care provider will commence under the “Healthier SG” initiative to encourage continuity of care to address different health needs of Singapore residents at different stages of life, with the involvement of multiple care and community partners to promote healthy living for different age sub-populations (51). Riding on this initiative, it would spare the arduous process of lobbying for policy change prior to implementing our strategy. Instead, our implementation model can be applied immediately to the Singaporean context, leveraging on the affirmative infrastructure which will be established through this upcoming healthcare reform.
Our study had several strengths. Firstly, the use of mixed methods provided in-depth qualitative understanding on the complexities surrounding the community context and constructs known to be of interest in persuading patients to take antibiotics appropriately, namely, trust building, continuity of care, and SDM (18). Furthermore, for the survey component, we employed a robust sampling method to proportionately stratify and randomize accordingly, ensuring generalizability of quantitative results. Purposive, maximum variation sampling by age and ethnicity was used for the FGDs, to ensure a range of voices were captured for in-depth analysis, enabling transferability of findings. However, there was a low representation of participants aged 35–49 years from the Malay ethnic group.
Furthermore, we acknowledge the possibility of social desirability bias, which may have led study respondents to reduce their sharing of inappropriate antibiotic practices, though steps were taken to encourage open sharing, and emphasis placed on anonymity throughout data collection procedures. Finally, there could also be unknown confounders which were not adjusted for in the final logistic regression model.
The current study demonstrates how building trust with a consistent provider opens up opportunities to educate the community on appropriate antibiotic use and AMR. The use of focused and consistent messaging in the community, the enablement of continuity of care with a regular primary care doctor, and leverage on the cultural capital of valuing SDM, to protect current and future generations from the fallout of AMR, is emphasized.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Domain Specific Review Board, National Healthcare Group, Singapore. The patients/participants provided their written informed consent to participate in this study.
HG designed the FGD topic guide, co-designed the survey questionnaire, arranged and conducted training with the surveyors, analyzed the data, and drafted the manuscript. ZH provided guidance on data analysis and critically revised the manuscript. AC conceived the study, provided overall direction and planning for the study, co-designed the survey questionnaire, and critically revised the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the National Medical Research Council Singapore, Health Services Research Grant (NMRC/HSRG/0083/2017).
The study team would like to thank all members of the public who participated in our study, Nur Azzriyani Bte Roslan, Aysha Farwin and Jeanette Yeo for facilitating the FGDs, Dr Mathew Mathews, Tan Gek Jee, Hong Gao Qiang, Er Kea Wee, Tang Hwee Noy and surveyors from Institute of Policy Studies Social Lab for their administrative and logistical support to complete the household survey, and Evonne Tay for her research administrative support to ensure the proper design and layout of the final survey booklet.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1001282/full#supplementary-material
AMR, Antimicrobial resistance; COVID-19, Coronavirus disease 2019; FGD, Focus group discussion; GP, General practitioner; SDM, Shared decision-making; SRQR, Standards for Reporting Qualitative Research.
1. Review on Antimicrobial Resistance. Antimicrobial Resistance: Tackling a Crisis for the Health Wealth of Nations. (2014). Available online at: https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf (accessed January 21, 2022).
2. World Health Organization. 14.9 Million Excess Deaths Associated With the COVID-19 Pandemic in 2020 and 2021 (2022). Available online at: https://www.who.int/news/item/05-05-2022-14.9-million-excess-deaths-were-associated-with-the-covid-19-pandemic-in-2020-and-2021 (accessed May 6, 2022).
3. World Health Organization. Antibiotic Resistance. (2020). Available online at: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed January 21, 2022).
4. Zetts RM, Stoesz A, Garcia AM, Doctor JN, Gerber JS, Linder JA, et al. Primary care physicians' attitudes and perceptions toward antibiotic resistance and outpatient antibiotic stewardship in the USA: a qualitative study. BMJ Open. (2020) 10:e034983. doi: 10.1136/bmjopen-2019-034983
5. Rose J, Crosbie M, Stewart A, A. qualitative literature review exploring the drivers influencing antibiotic over-prescribing by GPs in primary care and recommendations to reduce unnecessary prescribing. Perspect Public Health. (2021) 141:19–27. doi: 10.1177/1757913919879183
6. O'Connor R, O'Doherty J, O'Regan A, Dunne C. Antibiotic use for acute respiratory tract infections (ARTI) in primary care; what factors affect prescribing and why is it important? a narrative review. Ir J Med Sci. (2018) 187:969–86. doi: 10.1007/s11845-018-1774-5
7. Germeni E, Frost J, Garside R, Rogers M, Valderas JM, Britten N. Antibiotic prescribing for acute respiratory tract infections in primary care: an updated and expanded meta-ethnography. Br J Gen Pract. (2018) 68:e633–45. doi: 10.3399/bjgp18X697889
8. Lee TH, Wong JG, Lye DC, Chen MI, Loh VW, Leo YS, et al. Medical and psychosocial factors associated with antibiotic prescribing in primary care: survey questionnaire and factor analysis. Br J Gen Pract. (2017) 67:e168–77. doi: 10.3399/bjgp17X688885
9. Patel A, Pfoh ER, Misra Hebert AD, Chaitoff A, Shapiro A, Gupta N, et al. Attitudes of high vs. low antibiotic prescribers in the management of upper respiratory tract infections: a mixed methods study. J Gen Intern Med. (2020) 35:1182–8. doi: 10.1007/s11606-019-05433-5
10. Yates TD, Davis ME, Taylor YJ, Davidson L, Connor CD, Buehler K, et al. Not a magic pill: a qualitative exploration of provider perspectives on antibiotic prescribing in the outpatient setting. BMC Fam Pract. (2018) 19:96. doi: 10.1186/s12875-018-0788-4
11. Tonkin-Crine SK, Tan PS, van Hecke O, Wang K, Roberts NW, McCullough A, et al. Clinician-targeted interventions to influence antibiotic prescribing behavior for acute respiratory infections in primary care: an overview of systematic reviews. Cochrane Database Syst Rev. (2017) 9:CD012252. doi: 10.1002/14651858.CD012252.pub2
12. Price L, Gozdzielewska L, Young M, Smith F, MacDonald J, McParland J, et al. Effectiveness of interventions to improve the public's antimicrobial resistance awareness and behaviors associated with prudent use of antimicrobials: A systematic review. J Antimicrob Chemother. (2018) 73:1464–78. doi: 10.1093/jac/dky076
13. Lim JM, Singh SR, Duong MC, Legido-Quigley H, Hsu LY, Tam CC. Impact of national interventions to promote responsible antibiotic use: a systematic review. J Antimicrob Chemother. (2020) 75:14–29. doi: 10.1093/jac/dkz348
14. Coxeter P, Del Mar CB, McGregor L, Beller EM, Hoffmann TC. Interventions to facilitate shared decision making to address antibiotic use for acute respiratory infections in primary care. Cochrane Database Syst Rev. (2015) 2015:CD010907. doi: 10.1002/14651858.CD010907
15. Blyer K, Hulton L. College students, shared decision making, and the appropriate use of antibiotics for respiratory tract infections: a systematic literature review. J Am Coll Health. (2016) 64:334–41. doi: 10.1080/07448481.2015.1099105
16. Brookes-Howell L, Wood F, Verheij T, Prout H, Cooper L, Hood K, et al. Trust, openness and continuity of care influence acceptance of antibiotics for children with respiratory tract infections: a four country qualitative study. Fam Pract. (2014) 31:102–10. doi: 10.1093/fampra/cmt052
17. Barrera SC, Cancino RS, Barreto TW. The impact of continuity of care on antibiotic prescribing in acute otitis media. Int J Pediatr Otorhinolaryngol. (2019) 126:109616. doi: 10.1016/j.ijporl.2019.109616
18. Guo H, Hildon ZJ, Loh VWK, Sundram M, Ibrahim MAB, Tang WE, et al. Exploring antibiotic prescribing in public and private primary care settings in Singapore: a qualitative analysis informing theory and evidence-based planning for value-driven intervention design. BMC Fam Pract. (2021) 22:205. doi: 10.1186/s12875-021-01556-z
19. Nancy S, Dongre AR. Behavior change communication: past, present, and future. Indian J Community Med. (2021) 46:186–90. doi: 10.4103/ijcm.IJCM_441_20
20. Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. (2012) 27:1361–7. doi: 10.1007/s11606-012-2077-6
21. Guo H, Hildon ZJ, Lye DCB, Straughan P, Chow A. The associations between poor antibiotic and antimicrobial resistance knowledge and inappropriate antibiotic use in the general population are modified by age. Antibiotics (Basel). (2022) 11:47. doi: 10.3390/antibiotics11010047
22. O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. (2014) 89:1245–51. doi: 10.1097/ACM.0000000000000388
23. Health Promotion Board. Programmes: Antibiotics do Not Treat Flu. (2021). Available online at: https://healthhub.sg/programmes/146/use-antibiotics-right (accessed January 21, 2022).
24. Center for Health Protection Department of Health. General Public's Knowledge, Attitude and Practice Survey on Antimicrobial Resistance 2016/17. (2017).
25. Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. (2002) 37:1419–39. doi: 10.1111/1475-6773.01070
26. Cals JW, Boumans D, Lardinois RJ, Gonzales R, Hopstaken RM, Butler CC, et al. Public beliefs on antibiotics and respiratory tract infections: an internet-based questionnaire study. Br J Gen Pract. (2007) 57:942–7. doi: 10.3399/096016407782605027
27. Hawkings NJ, Butler CC, Wood F. Antibiotics in the community: a typology of user behaviors. Patient Educ Couns. (2008) 73:146–52. doi: 10.1016/j.pec.2008.05.025
28. Brooks L, Shaw A, Sharp D, Hay AD. Toward a better understanding of patients' perspectives of antibiotic resistance and MRSA: a qualitative study. Fam Pract. (2008) 25:341–8. doi: 10.1093/fampra/cmn037
29. Brookes-Howell L, Elwyn G, Hood K, Wood F, Cooper L, Goossens H, et al. 'The body gets used to them': patients' interpretations of antibiotic resistance and the implications for containment strategies. J Gen Intern Med. (2012) 27:766–72. doi: 10.1007/s11606-011-1916-1
30. Hoffmann K, Ristl R, Heschl L, Stelzer D, Maier M. Antibiotics and their effects: what do patients know and what is their source of information? Eur J Public Health. (2014) 24:502–7. doi: 10.1093/eurpub/ckt112
31. Gualano MR, Gili R, Scaioli G, Bert F, Siliquini R. General population's knowledge and attitudes about antibiotics: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. (2015) 24:2–10. doi: 10.1002/pds.3716
32. Pan DS, Huang JH, Lee MH Yu Y, Chen MI, Goh EH, et al. Knowledge, attitudes and practices toward antibiotic use in upper respiratory tract infections among patients seeking primary health care in Singapore. BMC Fam Pract. (2016) 17:148. doi: 10.1186/s12875-016-0547-3
33. Hennink MM, Kaiser BN, Weber MB. What influences saturation? estimating sample sizes in focus group research. Qual Health Res. (2019) 29:1483–96. doi: 10.1177/1049732318821692
36. Choo SJ, Chang CT, Lee JCY, Munisamy V, Tan CK, Raj JD, et al. A cross-sectional study on public belief, knowledge and practice toward antibiotic use in the state of Perak, Malaysia. J Infect Dev Ctries. (2018) 12:960–9. doi: 10.3855/jidc.10723
37. Lim JM, Chhoun P, Tuot S, Om C, Krang S, Ly S, et al. Public knowledge, attitudes and practices surrounding antibiotic use and resistance in Cambodia. JAC Antimicrob Resist. (2021) 3:dlaa115. doi: 10.1093/jacamr/dlaa115
38. Gillani AH, Chang J, Aslam F, Saeed A, Shukar S, Khanum F, et al. Public knowledge, attitude, and practice regarding antibiotics use in Punjab, Pakistan: a cross-sectional study. Expert Rev Anti Infect Ther. (2021) 19:399–411. doi: 10.1080/14787210.2021.1823216
39. World Health Organization. Effective Communications: Participant Handbook: Communications Training Programme for WHO Staff. London: Geneva (2015).
40. Guo H, Lim HY, Chow A. Health information orientation profiles and their association with knowledge of antibiotic use in a population with good Internet access: a cross-sectional study. Antibiotics. (2022) 11:769. doi: 10.3390/antibiotics11060769
41. Satterfield J, Miesner AR, Percival KM. The role of education in antimicrobial stewardship. J Hosp Infect. (2020) 105:130–41. doi: 10.1016/j.jhin.2020.03.028
42. Gonzales R, Sauaia A, Corbett KK, Maselli JH, Erbacher K, Leeman-Castillo BA, et al. Antibiotic treatment of acute respiratory tract infections in the elderly: effect of a multidimensional educational intervention. J Am Geriatr Soc. (2004) 52:39–45. doi: 10.1111/j.1532-5415.2004.52008.x
43. Mainous AG, Diaz VA, Carnemolla M. A community intervention to decrease antibiotics used for self-medication among Latino adults. Ann Fam Med. (2009) 7:520–6. doi: 10.1370/afm.1061
44. Smeets HM, Kuyvenhoven MM, Akkerman AE, Welschen I, Schouten GP, van Essen GA, et al. Intervention with educational outreach at large scale to reduce antibiotics for respiratory tract infections: a controlled before and after study. Fam Pract. (2009) 26:183–7. doi: 10.1093/fampra/cmp008
45. Vinnard C, Linkin DR, Localio AR, Leonard CE, Teal VL, Fishman NO, et al. Effectiveness of interventions in reducing antibiotic use for upper respiratory infections in ambulatory care practices. Popul Health Manag. (2013) 16:22–7. doi: 10.1089/pop.2012.0025
46. Légaré F, Labrecque M, Cauchon M, Castel J, Turcotte S, Grimshaw J. Training family physicians in shared decision-making to reduce the overuse of antibiotics in acute respiratory infections: a cluster randomized trial. CMAJ. (2012) 184:E726–34. doi: 10.1503/cmaj.120568
47. Wrzus C, Hänel M, Wagner J, Neyer FJ. Social network changes and life events across the life span: a meta-analysis. Psychol Bull. (2013) 139:53–80. doi: 10.1037/a0028601
48. Carstensen LL. Socioemotional selectivity theory: Social activity in life-span context. Annu Rev Gerontol Geriatr. (1991) 11:195–217.
49. Carstensen LL. Social and emotional patterns in adulthood: Support for socioemotional selectivity theory. Psychol Aging. (1992) 7:331–8. doi: 10.1037/0882-7974.7.3.331
50. Carstensen LL. Evidence for a life-span theory of socioemotional selectivity. Curr Dir Psychol Sci. (1995) 4:151–6. doi: 10.1111/1467-8721.ep11512261
51. Ministry of Health Singapore. News Highlight: Promoting Overall Healthier Living While Targeting Specific Sub-Populations. (2022). Available online at: https://www.moh.gov.sg/news-highlights/details/promoting-overall-healthier-living-while-targeting-specific-sub-populations (accessed September 6, 2022).
Keywords: antimicrobial resistance, shared decision-making, trusting relationships, continuity of care, community values, public engagement
Citation: Guo H, Hildon ZJ-L and Chow A (2022) “Antibiotics are for everyone, our past and our future generations, right? If antibiotics are dead, we will be in big trouble”: Building on community values for public engagement on appropriate use of antibiotics in Singapore. Front. Public Health 10:1001282. doi: 10.3389/fpubh.2022.1001282
Received: 23 July 2022; Accepted: 14 September 2022;
Published: 30 September 2022.
Edited by:
Anat Gesser-Edelsburg, University of Haifa, IsraelReviewed by:
Krushna Chandra Sahoo, Regional Medical Research Center (ICMR), IndiaCopyright © 2022 Guo, Hildon and Chow. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zoe Jane-Lara Hildon, emhpbGRvbkBudXMuZWR1LnNn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.