- 1Jinhua Eye Hospital, Jinhua, China
- 2School of Ophthalmology and Optometry, Eye Hospital of Wenzhou Medical University, Wenzhou, China
- 3State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center of Sun Yat-sen University, Guangzhou, China
Purpose: To identify the relationship between the increase in axial length (AL) and height in school-age children and explore the influence of refractive status on such a relationship.
Methods: In this 5-year cohort study, 414 Chinese children (237 boys) aged 6–9 years (mean 7.12) underwent measurements annually. AL was measured using the Lenstar; height with the children standing, without shoes; and refraction using subjective refraction without cycloplegia. Participants were divided according to the refractive status: persistent emmetropia, persistent myopia, and newly developed myopia. The measurement time points of the persistent emmetropia and persistent myopia groups were marked as T1, T2, T3, T4, and T5. The time of myopia onset in the newly developed myopia group was marked as t0; the preceding time points were marked as t−1, t−2, and so on, and the succeeding as t1, t2, and so on. The association between increase in AL and height was analyzed using simple correlation analysis.
Results: The mean changes in AL, height, and refraction were 1.39 mm, 23.60 cm, and −1.69 D, respectively, over 5 years in all children. The increase in AL and height were positively correlated for T1~T2, T1~T3, T1~T4, and T1~T5 (r = 0.262, P < 0.001; r = 0.108, P = 0.034; r = 0.165, P = 0.001; r = 0.174, P = 0.001, respectively). The changes in AL and height in the newly developed myopia group were significantly correlated (r = 0.289, P = 0.009) after myopia onset (t0~t2).
Conclusion: The increase in AL and height were positively correlated, especially in the newly developed myopia group after myopia onset. Thus, when children grow quickly, AL elongation should be monitored.
Introduction
In recent decades, the prevalence of myopia has rapidly increased (1). It is predicted that nearly half of the world's population will suffer from myopia by 2050 (2). The rate may be greater for eastern Asia, including China, Japan, South Korea, and Singapore (3–5), where the incidence of myopia is higher than in other areas. School-age children are the main group of people diagnosed with myopia (6), whose elongation of axial length (AL) plays a major role in the incidence and progression of myopia (7–10). Therefore, changes in AL may reflect changes in refractive status to some extent.
The association between height and AL has been demonstrated in previous cross-sectional studies (11–14) and longitudinal cohort studies (15–17). In 2002, Saw et al. (11) proved that taller children have longer AL by analyzing the height and AL of 1,449 children aged 7–9 years. Later, in 2011, Wang et al. (15) demonstrated the correlation between them through a longitudinal cohort study. They analyzed follow-up data of 553 children aged between 7 and 15 from 2006 to 2008 and concluded that height and AL are positively correlated. In brief, all previous studies agree with the statement that height and AL are positively correlated.
However, few studies have discussed the relationship between growth in height and AL. A previous study reported that the association between height and AL is largely attributable to shared genes (18). Therefore, we predicted that an association may also be present between the speed of the growth in height and AL. Huang et al. (19) proved that average changes in height and AL were correlated in a three-year follow-up experiment. However, they did not show such association at the different stages during follow-up, and the sample size was relatively small (N = 88). Later, Kearney et al. (20) and Li et al. (21) also explored the correlation between the increases in AL and height, but obtained different results. Kearney et al. argued that the association existed in persistent emmetropic children, while Li et al. found no association in the entire participant cohort during the 3-year follow up. This discrepancy may be ascribed to the differences in sample size (N = 140 and 452, respectively) and age range (5–20 and 6–8 years old, respectively). As the elongation of AL in myopic children differs from that of emmetropic children (22–24), the AL growth of those who will become myopic accelerates before the onset of myopia and slows down after it, while the annual AL change of emmetropic children is relatively stable (22). Thus, to explore the relationship between changes in height and AL, the refractive status should be considered.
In the present study we aimed to explore the association between the changes in height and AL in children through a five-year follow-up of children aged 6 to 9 years, and to determine whether the growth in height can predict the increase in AL. Furthermore, we aimed to explore the correlation between changes in height and AL in myopic children before and after the onset of myopia.
Methods
Participants
This was a five-year cohort study conducted from 2015 to 2020 in Jinhua, a city situated in eastern China. The subjects were students of 10 schools in the Wucheng District, Jindong District, and Jinhua Economic and Technological Development Zone. Children with systemic diseases that affect height growth or ocular health, strabismus, or amblyopia were excluded. Participants who received myopia control treatment such as orthokeratology lenses or low-concentration atropine, other than single vision lenses, were also excluded. In total, 456 children of grades 1–4 successfully completed the baseline ocular examinations, and 414 (90.8%) continuously attended their measurements in the following examinations. The age at baseline (date of first examination) of the participants ranged from 6 to 9 years.
The study was conducted in accordance with the Declaration of Helsinki of the World Medical Association. Informed consent was obtained from all participants or their parents.
Examinations
All participants underwent an examination at Jinhua Eye Hospital every 12 months since their first examination. The examination included height assessment and comprehensive eye examination. Height was evaluated without shoes: each child stood with the buttocks, shoulder blades, and back of the head against the wall. The doctor placed the headpiece firmly on the head and recorded the height (25). AL was measured using non-invasive, non-contact optical low-coherence reflectometry (Lenstar LS900; Haag-Streit AG, 3098 Koeniz, Switzerland) without pupil dilation. Three consecutive measurements were acquired, and the mean result was used (13). If the error of the three measurements was >0.1 mm, AL was remeasured. Refraction was measured using subjective refraction without cycloplegia by experienced optometrists. The child looked at the Standard Logarithmic Visual Acuity Chart 5 m away, while the optometrist presented a variety of lenses (including spherical lenses and cylinder lenses) and altered the power of lenses in the phoropter according to the child's subjective responses until the best-corrected visual acuity (BCVA) was achieved. The refraction was transformed into spherical equivalent (SE = sphere power + 0.5cylinder power). Refractive status was judged according to SE [myopia: SE ≤ −0.5D (26, 27); emmetropia: −0.5D < SE < +1.0D; hypertropia: SE ≥ 1.0D].
Data Analysis
SPSS (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, version 26.0. Armonk, NY: IBM Corp.) was used to analyze the data. Because data from the two eyes were highly correlated (the Spearman's rank correlation coefficient of AL and SE was 0.976 and 0.907, respectively, and both p-values were lower than 0.01), the data from the right eye were analyzed. The participants were classified according to the refractive status of each examination. Those who maintained emmetropia/myopia were grouped into the persistent emmetropia/persistent myopia groups. The newly developed myopia group included participants who had emmetropia or hyperopia at the first examination, became myopic in the following four examinations, and later maintained myopia. The time of each examination was marked as T1, T2, T3, T4, and T5 corresponding to the successive examinations for all participants/persistent emmetropia group/persistent myopia group. We then calculated the differences between the results of each examination and those at T1. For the newly developed myopia group, the time of first discovery of myopia was marked as t0. The previous time points were marked as t−1, t−2, …, and the following time points as t1, t2…. The difference between the results of each examination and those of t0 was calculated.
Data are presented as median (interquartile range). The correlation between the change in height and the change in AL was analyzed using simple correlation analysis. The bootstrap method was used to calculate the 95% confidence interval (95% CI) of the correlation coefficient (r-value). Age and sex were added as covariates in partial correlation analysis. Statistical significance was set at P < 0.05.
Results
Descriptive Data
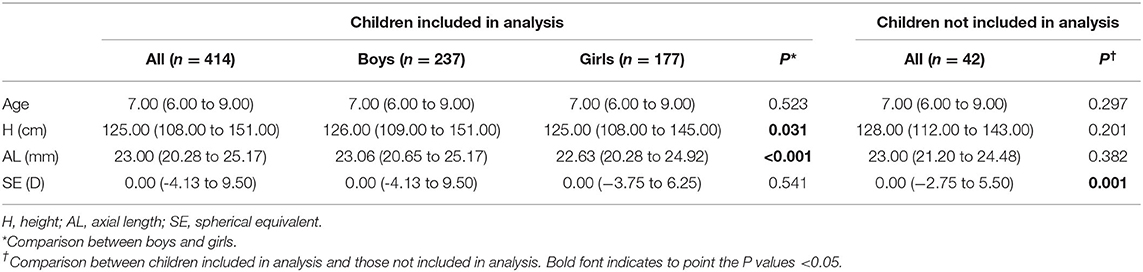
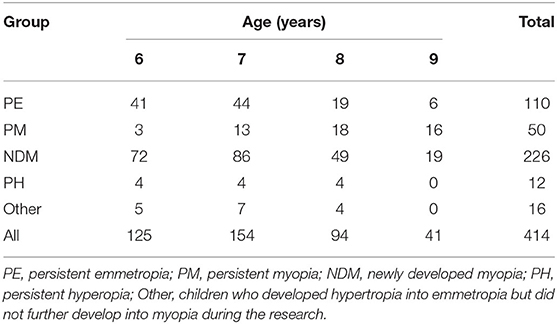
In total, 456 children (260 boys and 196 girls) participated in this study at baseline. Forty-two children were lost to follow-up in the following four examinations and were excluded from the analysis. The remaining 414 children (57.2% boys, 42.8% girls) completed the 5-year examination cycle, including 110 in the persistent emmetropia group, 50 in the persistent myopia group, and 226 in the newly developed myopia group. Twenty-eight children had hyperopia or developed from hyperopia to emmetropia but did not develop myopia. These children were taken into account when considering the correlation in all children but not analyzed separately as a specific sub-group. There was no significant difference between participants who dropped out and the remaining participants in terms of age at baseline (P = 0.297), height at baseline (P = 0.201), AL at baseline (P = 0.382), or sex (P = 0.757). Demographic characteristics of the participants at baseline are summarized in Table 1, while the age distribution at the first examination is presented in Table 2. Height, AL, and refraction at each examination are presented in Tables 3, 4.
During the five-year follow-up, on average, the children grew by 23.60 ± 4.65 cm in height, their AL increased by 1.39 ± 0.53 mm, and their SE change was −1.69 ± 1.29 D. The prevalence of myopia in each examination (from T1 to T5) was 12.1, 20.0, 32.9, 48.8, and 66.7%, respectively.
Correlation of Height With Axial Length and Refraction
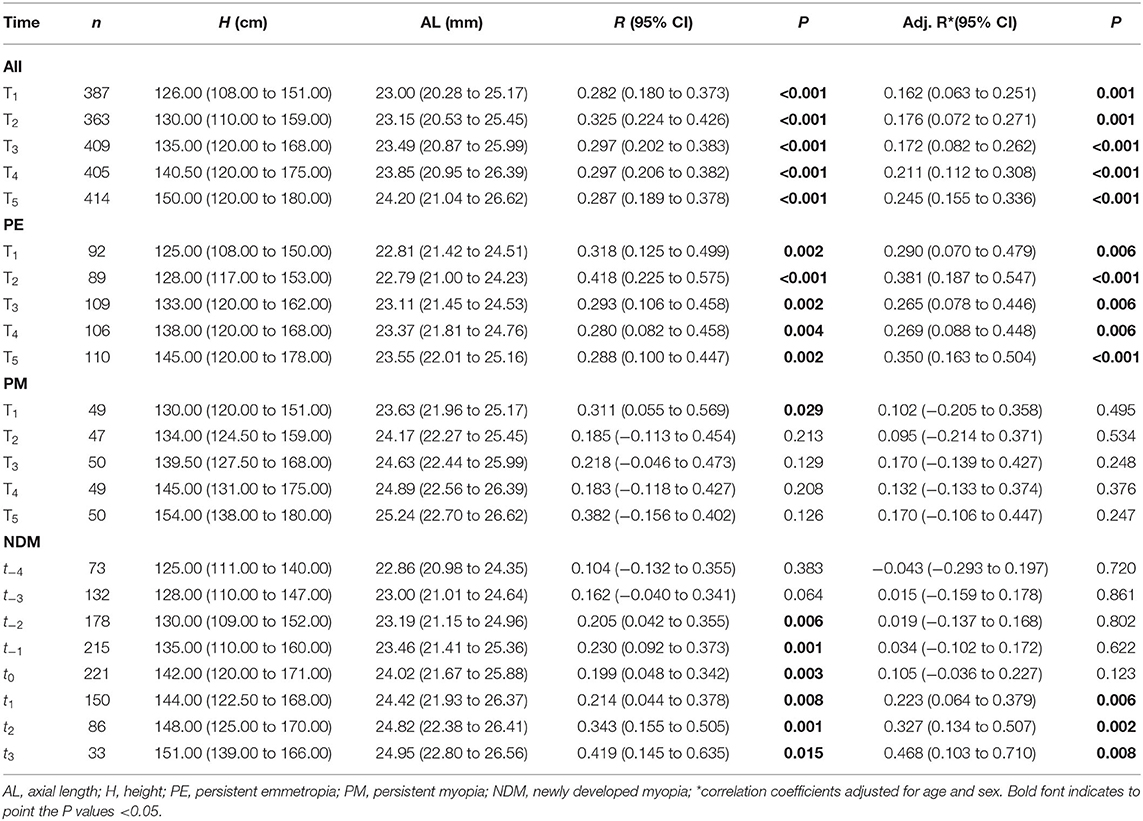
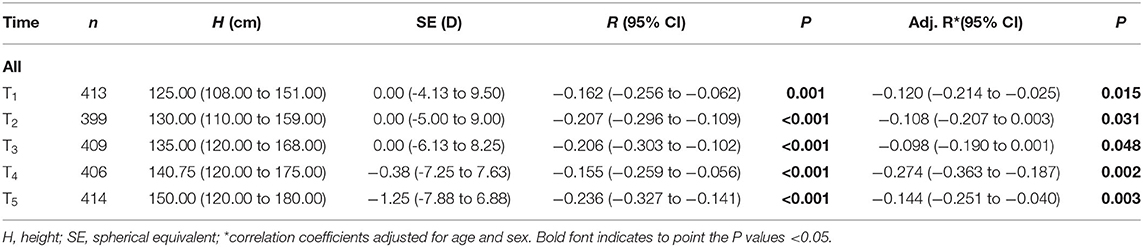
In each examination of all children, height and AL were positively and significantly correlated. The correlation was still statistically significant after adjusting for age and sex (Table 3). Conversely, height and refraction were negatively correlated before and after controlling for age and sex (Table 4).
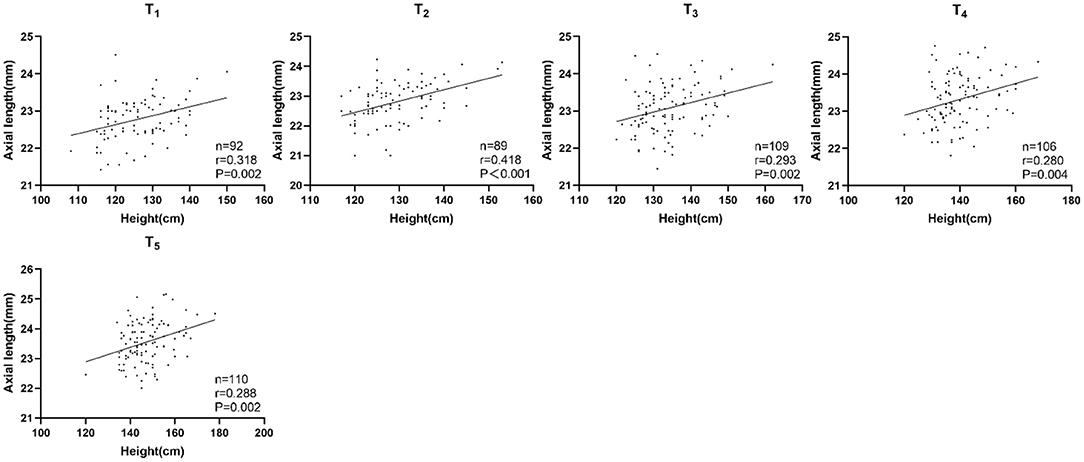
In the persistent emmetropia group, height and AL were positively correlated in each examination. The correlation was statistically significant with or without adjusting for sex and age (Table 3; Figure 1).
In the persistent myopia group, the correlation between height and AL only existed at T1, and was no longer present after correcting for age and sex (Table 3).
In the newly developed myopia group, height and AL were positively correlated at t−2, t−1, and t0 only before adjusting for confounding factors. From t1 to t3, height and AL were positively correlated both before and after controlling for sex and age (Table 3; Figure 2).
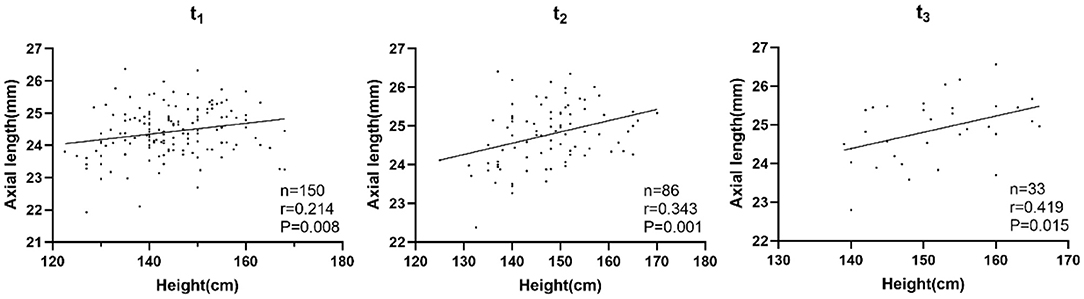
Correlation Between Changes in Height and Changes in Axial Length
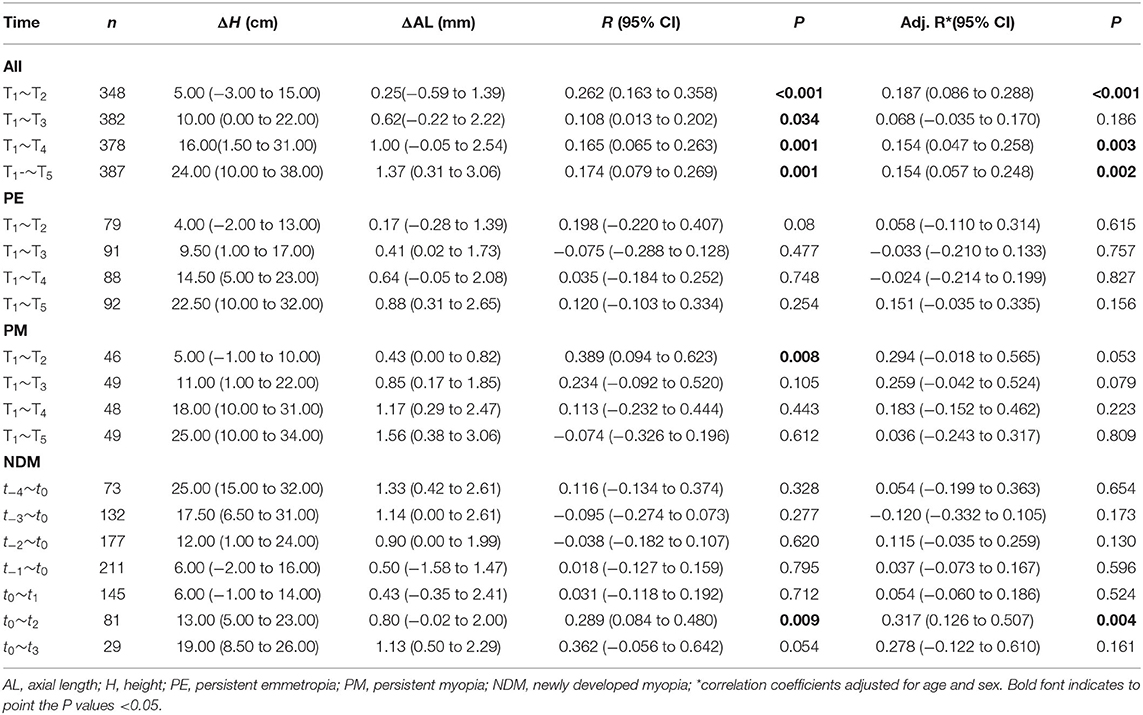
Correlations between the changes in height and AL were statistically significant for T1~T2, T1~T3, T1~T4, and T1~T5 (r = 0.262, P < 0.001; r = 0.108, P = 0.034; r = 0.165, P = 0.001; r = 0.174, P = 0.001, respectively). Furthermore, the correlations were still statistically significant for T1~T2, T1~T4, and T1~T5 after adjusting for age and sex (r = 0.187, P < 0.001; r = 0.154, P = 0.003; r = 0.154, P = 0.002; Table 5; Figure 3).
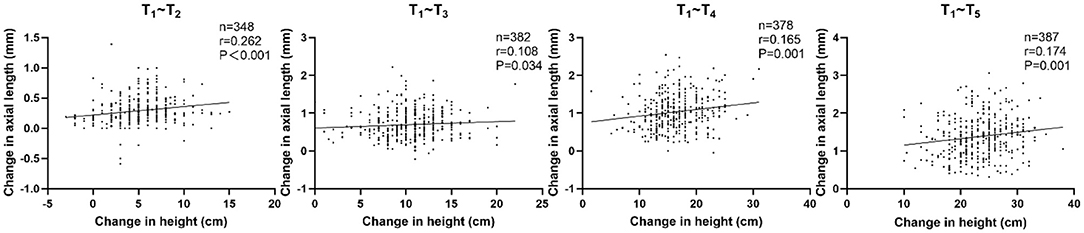
Significant correlations were found in the newly developed myopia group after the onset of myopia. Changes in height and AL were positively correlated both before and after correcting for age and sex for t0~t2 (r = 0.289, P = 0.009; r = 0.317, P = 0.004), while no significant correlations were found before myopia onset (Table 5; Figure 4).
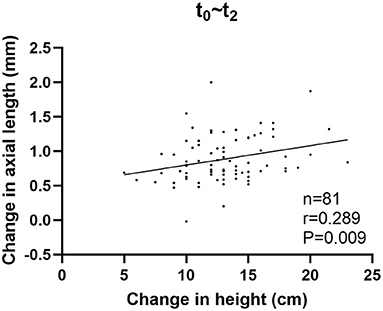
Figure 4. Correlation between changes in height and changes in axial length in the newly developed myopia group after the onset of myopia.
No significant correlation was observed between changes in AL and changes in height in the persistent emmetropia group. Similarly, no significant associations were found in the persistent myopia group, except for T1~T2 (r = 0.388, P = 0.008) before adjusting for the confounding factors (Table 5).
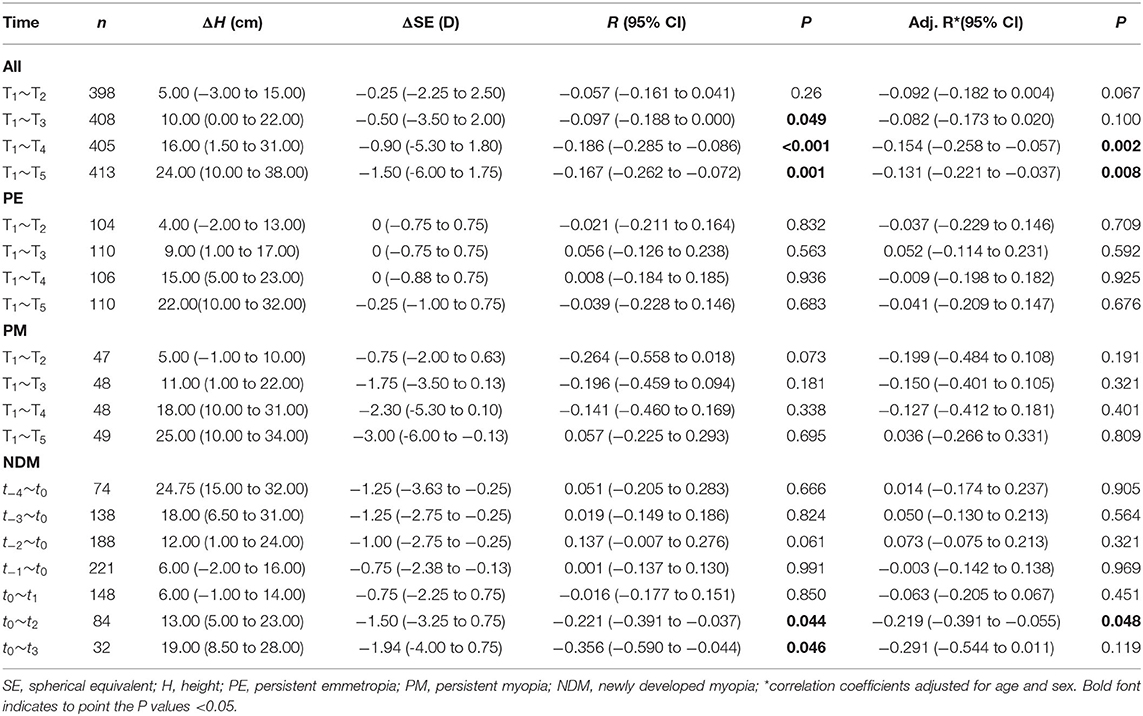
Correlation Between Changes in Height and Refraction
Table 6 shows the correlation between the changes in height and refraction. Changes in height and SE were negatively correlated for T1~T3, T1~T4, and T1~T5 (r = −0.097, P = 0.049; r = −0.186, P < 0.001; r = −0.167, P = 0.001). The pattern of correlation in the sub-groups was similar to that of changes in AL and height, but with negative correlation coefficients.
Discussion
This cohort study was conducted in Jinhua, a city located in eastern China, where the incidence of myopia is relatively high (28). In total, 414 children aged 6–9 participated in the study and completed a five-year series of follow-up examinations from 2015 to 2020, in which every child was examined every 12 months. A correlation was found between the growth in height and the increase in AL in children and adolescents, especially in the newly developed myopia group. Our results suggest that children may also experience increased AL growth when they present with rapid height growth.
We assessed the relationship between the changes in height and the increase in AL and found that they were positively correlated in children aged 6–9. This is essentially consistent with the results of Huang et al.'s study (19), which included 65 children aged 7–9 years old followed up every 6 months in a three-year period. They concluded that growth in height and AL during the research period were correlated. Compared with their study, the present one included more participants and had longer follow-up. Furthermore, we proved that the correlation existed not only in the whole period (T1~T5), but also at every follow-up time point (T1~T2, T1~T3, T1~T4, T1~T5).
However, the study by Li et al. did not find that the changes in height and AL were correlated (21). In their study, a total of 452 children aged 6–8 years accepted measurements every year during the 3-year follow-up period. They analyzed the relationship between the mean change in AL and the mean change in height through multivariate linear regression analysis, finding that they were not correlated at any point in the 3-year follow-up period (2015–2014, 2016–2014, or 2017–2014). This may be related to the lack of representativeness of the sample, composed of students of grades 1 and 2 from a single school. It may also be related with the shorter follow-up time (3 years) and the fact that refractive status was not considered. Kearney et al. (20) concluded that changes in height and AL were correlated in the persistent emmetropia group (n = 55), but not in the newly developed myopia group, in 105 subjects aged 5–20 years, with examination conducted every 2 years for 4 years. The disagreement between the results of the study by Kearney et al. and ours may result from the difference in the age of the participants and the follow-up time intervals.
We also found a positive correlation between changes in height and AL after myopia onset in the newly developed myopia group. That might be due to the fact that children have a peak incidence of myopia at the age of growth spurt at least in Chinese. A previous study reported that the onset of myopia and the peak of its progression may be associated with growth spurts (16). Moreover, AL elongation and growth in height may be partially mediated by the same genes (18). The changes in height are the result of both genetic and environmental factors (29, 30), and the same applies to AL (31, 32). The experiment by He proved that the correlation between AL and height is largely (89%) attributable to shared genes (18). In addition to genes, hormones play an important role: many hormones involved in height growth, such as GH, IGF-1, and TH, have also been shown to accelerate the growth of eyes (33–36). Although there may be shared genes and hormones related to both growths, height is more susceptible to nutritional environmental factors and gastrointestinal infection, while AL growth is more susceptible of being modified by illumination and visual cues.
In the present study, we also explored the relationship between height and AL for different refractive status. Selovic et al. found that height and AL were positively correlated in persistent emmetropes by analyzing the data of 1,600 pupils (37). However, they neither investigated the correlation in newly developed or persistent myopes, nor conducted a follow-up study. Our further exploration also revealed that height and AL were positively correlated in every examination in the persistent emmetropia group as well as in the newly developed myopia group after the onset of myopia. However, the association did not exist in any examination in the newly developed myopia group before the onset of myopia or in the persistent myopia group. Whether the onset of myopia plays a role in the relationship between height and AL in children and adolescents, further researches are required.
Similar results were obtained for the correlation between height and refraction, because refraction is largely determined by the AL (38, 39). Though AL plays an important role in refraction, a longer AL doesn't necessarily mean more myopic. Emmetropia is a balance between AL, corneal power and lens power (40). That means longer eyes can be compensated by less lens power or flatter corneas to keep emmetropic (41–45). So future studies should take lens power and corneal radius of curvature into consideration to account for their possible compensation of greater axial growth.
The current research has proved that changes in height and AL are positively correlated in the transition from childhood to adolescence. Myopia gradually becomes prevalent from the age of 6–9 years old (6, 46–49), when height also grows relatively fast (50). Yip et al. (16) argued that children who experienced peak height velocity earlier may also become myopic earlier. Our study further found that when children grow fast in height, their AL may also elongate quickly, just at the time they may be more likely to become myopic in this environment. Thus, observing the growth rate of children can serve as an indicator to monitor the growth velocity of their AL. When a child is in a stage of rapid height growth, we may need to be aware that his/her AL is also in a period of easy elongation. The elongation of the AL is closely related to the occurrence and development of myopia. As to whether the strengthening of myopia prevention and control measures can slow the growth of AL in the period of rapid height growth, further research is warranted.
Based on prior studies, we further proved the correlation between changes in height and changes in AL. However, there are some limitations to our study. First, we did not produce genetic data or measure hormone levels. Therefore, we cannot directly prove whether the correlation between height and AL is mediated by genes or hormones. Second, we did not use a questionnaire to acquire information that may be associated with the onset of myopia, such as reading and writing distance, and time spent outdoors. Such information will help us better understand the development of myopia in our participants. Third, some of the subjects in our study may have grown into adolescence later in the follow-up period. Adolescents are likely to grow faster than children (51). However, we didn't have the exact puberty parameters such as age of maximum height velocity, age of menarche and voice changes. Although, in agreement with Yip et al. (16), we could observe a correlation between the time of rapid growth of AL and height, to adjust for antecedents of the pubertal peak, detailed information of puberty and a longer follow up time would be required. Finally, the follow up time is still too short to include the whole period of accelerated growth. We chose children aged 6–9 years old and followed up for 5 years which covers the time of rapid change of refraction based on our previous study (52). However, some subjects may be outside the peak of accelerated growth. A longer follow up period would be necessary to clarify the relationship between the peak of accelerated growth and the progression of myopia, and changes in AL and height after the onset of myopia in future studies.
Ulaganathan et al. (53) previously described that the mean amplitude of daily variations in AL is 0.029± 0.007 mm, thus, minor variations could be neglected when considering yearly AL changes. So, the AL was not measured at the same time each day in this study. The non-cycloplegic refraction may render an overestimation of myopia. However, it may have less effect in a longitudinal study such as our own, which monitored the progression of refraction in the same population (6).
In summary, we suggest that during the growth of school-age children, a significant correlation exists not only between AL and height, but also between AL growth and height growth, especially in children with newly developed myopia. This indicates that during the period of rapid height growth, the elongation of AL also needs to be considered. Whether the strengthening of outdoor activities or other myopia control measures can delay the elongation of AL during the rapid height growth period may be an urgent question that needs to be answered.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Jinhua Eye Hospital. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
LT: research design and collect data. CW, YP, MX, and MW: technical assistance and guidance. XY: research and academic guidance. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China Grant 82070995.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank Shi-ming Li at Beijing Tongren Hospital for his advice on this study.
References
1. Morgan IG, Ohno-Matsui K, Saw S-M. Myopia. Lancet. (2012) 379:1739–48. doi: 10.1016/S0140-6736(12)60272-4
2. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. (2016) 123:1036–42. doi: 10.1016/j.ophtha.2016.01.006
3. Morgan IG, French AN, Ashby RS, Guo X, Ding X, He M, et al. The epidemics of myopia: Aetiology and prevention. Prog Retin Eye Res. (2018) 62:134–49. doi: 10.1016/j.preteyeres.2017.09.004
4. Xiang ZY, Zou HD. Recent epidemiology study data of myopia. J Ophthalmol. (2020) 2020:4395278. doi: 10.1155/2020/4395278
5. Ding B-Y, Shih Y-F, Lin LLK, Hsiao CK, Wang IJ. Myopia among schoolchildren in East Asia and Singapore. Surv Ophthalmol. (2017) 62:677–97. doi: 10.1016/j.survophthal.2017.03.006
6. Wang J, Li Y, Zhao Z, Wei N, Qi X, Ding G, et al. School-based epidemiology study of myopia in Tianjin, China. Int Ophthalmol. (2020) 40:2213–22. doi: 10.1007/978-981-13-7896-6
7. Hyman L, Gwiazda J, Hussein M, Norton TT, Wang Y, Marsh-Tootle W, et al. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. (2005) 123:977–87. doi: 10.1001/archopht.123.7.977
8. Jones LA, Mitchell GL, Mutti DO, Hayes JR, Moeschberger ML, Zadnik K. Comparison of ocular component growth curves among refractive error groups in children. Invest Ophthalmol Vis Sci. (2005) 46:2317–27. doi: 10.1167/iovs.04-0945
9. Hou W, Norton TT, Hyman L, Gwiazda J, Group C. Axial elongation in myopic children and its association with myopia progression in the correction of myopia evaluation trial. Eye Contact Lens. (2018) 44:248–59. doi: 10.1097/ICL.0000000000000505
10. Tideman JWL, Polling JR, Vingerling JR, Jaddoe VWV, Williams C, Guggenheim JA, et al. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. (2018) 96:301–9. doi: 10.1111/aos.13603
11. Saw S-M, Chua W-H, Hong C-Y, Wu H-M, Chia K-S, Stone RA, et al. Height and its relationship to refraction and biometry parameters in Singapore Chinese children. Invest Ophthalmol Vis Sci. (2002) 43:1408–13.
12. Ojaimi E, Morgan IG, Robaei D, Rose KA, Smith W, Rochtchina E, et al. Effect of stature and other anthropometric parameters on eye size and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci. (2005) 46:4424–9. doi: 10.1167/iovs.05-0077
13. Ye S, Liu S, Li W, Wang Q, Xi W, Zhang X. Associations between anthropometric indicators and both refraction and ocular biometrics in a cross-sectional study of Chinese schoolchildren. BMJ Open. (2019) 9:e027212. doi: 10.1136/bmjopen-2018-027212
14. Goss DA, Cox VD, Herrin-Lawson GA, Nielsen ED, Dolton WA. Refractive error, axial length, and height as a function of age in young myopes. Optom Vis Sci. (1990) 67:332–8. doi: 10.1097/00006324-199005000-00006
15. Wang D, Ding X, Liu B, Zhang J, He M. Longitudinal changes of axial length and height are associated and concomitant in children. Invest Ophthalmol Vis Sci. (2011) 52:7949–53. doi: 10.1167/iovs.11-7684
16. Yip VC, Pan CW, Lin XY, Lee YS, Gazzard G, Wong TY, et al. The relationship between growth spurts and myopia in Singapore children. Invest Ophthalmol Vis Sci. (2012) 53:7961–6. doi: 10.1167/iovs.12-10402
17. Northstone K, Guggenheim JA, Howe LD, Tilling K, Paternoster L, Kemp JP, et al. Body stature growth trajectories during childhood and the development of myopia. Ophthalmology. (2013) 120:1064–73 e1. doi: 10.1016/j.ophtha.2012.11.004
18. Zhang J, Hur Y-M, Huang W, Ding X, Feng K, He M. Shared genetic determinants of axial length and height in children: the Guangzhou twin eye study. Arch Ophthalmol. (2011) 129:63–8. doi: 10.1001/archophthalmol.2010.323
19. Huang CY, Hou CH, Lin KK, Lee JS, Yang ML. Relationship of lifestyle and body stature growth with the development of myopia and axial length elongation in Taiwanese elementary school children. Indian J Ophthalmol. (2014) 62:865–9. doi: 10.4103/0301-4738.141047
20. Kearney S, Strang NC, Cagnolati B, Gray LS. Change in body height, axial length and refractive status over a four-year period in caucasian children and young adults. J Optom. (2020) 13:128–36. doi: 10.1016/j.optom.2019.12.008
21. Li T, Jiang B, Zhou X. Axial length elongation in primary school-age children: a 3-year cohort study in Shanghai. BMJ Open. (2019) 9:e029896. doi: 10.1136/bmjopen-2019-029896
22. Mutti DO, Hayes JR, Mitchell GL, Jones LA, Moeschberger ML, Cotter SA, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. (2007) 48:2510–9. doi: 10.1167/iovs.06-0562
23. Xiang F, He M, Morgan IG. Annual changes in refractive errors and ocular components before and after the onset of myopia in Chinese children. Ophthalmology. (2012) 119:1478–84. doi: 10.1016/j.ophtha.2012.01.017
24. Rozema J, Dankert S, Iribarren R, Lanca C, Saw SM. Axial growth and lens power loss at myopia onset in singaporean children. Invest Ophthalmol Vis Sci. (2019) 60:3091–9. doi: 10.1167/iovs.18-26247
25. Louer AL, Simon DN, Switkowski KM, Rifas-Shiman SL, Gillman MW, Oken E. Assessment of Child Anthropometry in a Large Epidemiologic Study. J Vis Exp. (2017) 120:e54895. doi: 10.3791/54895
26. Wong YL, Yuan Y, Su B, Tufail S, Ding Y, Ye Y, et al. Prediction of myopia onset with refractive error measured using non-cycloplegic subjective refraction: the WEPrOM Study. BMJ Open Ophthalmol. (2021) 6:e000628. doi: 10.1136/bmjophth-2020-000628
27. Flitcroft DI, He M, Jonas JB, Jong M, Naidoo K, Ohno-Matsui K, et al. IMI—Defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. (2019) 60:M20–30. doi: 10.1167/iovs.18-25957
28. Wu GY, Huang TQ, Hospital JE. Correlation analysis of the development of children's myopia and the length of axial length in Jinhua. Chin J Strabismus Pediatric Ophthalmol. (2017).
29. Andrade AC, Jee YH. Nilsson O, New genetic diagnoses of short stature provide insights into local regulation of childhood growth. Horm Res Paediatr. (2017) 88:22–37. doi: 10.1159/000455850
30. Baron J, Sävendahl L, De Luca F, Dauber A, Phillip M, Wit JM, et al. Short and tall stature: a new paradigm emerges. Nat Rev Endocrinol. (2015) 11:735–46. doi: 10.1038/nrendo.2015.165
31. Pozarickij A, Williams C, Hysi PG, Guggenheim JA, Eye UKB, Vision C. Quantile regression analysis reveals widespread evidence for gene-environment or gene-gene interactions in myopia development. Commun Biol. (2019) 2:167. doi: 10.1038/s42003-019-0387-5
32. Harb EN, Wildsoet CF. Origins of refractive errors: environmental and genetic factors. Annu Rev Vis Sci. (2019) 5:47–72. doi: 10.1146/annurev-vision-091718-015027
33. Liu YX, Sun Y. MMP-2 participates in the sclera of guinea pig with form-deprivation myopia via IGF-1/STAT3 pathway. Eur Rev Med Pharmacol Sci. (2018) 22:2541–8.
34. Prashar A, Hocking PM, Erichsen JT, Fan Q, Saw SM, Guggenheim JA. Common determinants of body size and eye size in chickens from an advanced intercross line. Exp Eye Res. (2009) 89:42–8. doi: 10.1016/j.exer.2009.02.008
35. Rada JA, Wiechmann AF. Ocular expression of avian thymic hormone: changes during the recovery from induced myopia. Mol Vis. (2009) 15:778–92.
36. Seko Y, Tanaka Y, Tokoro T. Influence of bFGF as a potent growth stimulator and TGF-beta as a growth regulator on scleral chondrocytes and scleral fibroblasts in vitro. Ophthalmic Res. (1995) 27:144–52. doi: 10.1159/000267651
37. Selovic A, Juresa V, Ivankovic D, Malcic D, Selovic Bobonj G. Relationship between axial length of the emmetropic eye and the age, body height, and body weight of schoolchildren. Am J Hum Biol. (2005) 17:173–7. doi: 10.1002/ajhb.20107
39. Young TL, Metlapally R, Shay AE. Complex trait genetics of refractive error. Arch Ophthalmol. (2007) 125:38–48. doi: 10.1001/archopht.125.1.38
40. Ip JM, Huynh SC, Kifley A, Rose KA, Morgan IG, Varma R, et al. Variation of the contribution from axial length and other oculometric parameters to refraction by age and ethnicity. Invest Ophthalmol Vis Sci. (2007) 48:4846–53. doi: 10.1167/iovs.07-0101
41. Iribarren R, Morgan IG, Hashemi H, Khabazkhoob M, Emamian MH, Shariati M, et al. Lens power in a population-based cross-sectional sample of adults aged 40 to 64 years in the Shahroud Eye Study. Invest Ophthalmol Vis Sci. (2014) 55:1031–9. doi: 10.1167/iovs.13-13575
42. Iribarren R, Hashemi H, Khabazkhoob M, Morgan IG, Emamian MH, Shariati M, et al. Hyperopia and lens power in an adult population: the Shahroud eye study. J Ophthalmic Vis Res. (2015) 10:400–7. doi: 10.4103/2008-322X.158895
43. Iribarren R. Crystalline lens and refractive development. Prog Retin Eye Res. (2015) 47:86–106. doi: 10.1016/j.preteyeres.2015.02.002
44. He X, Sankaridurg P, Naduvilath T, Wang J, Xiong S, Weng R, et al. Normative data and percentile curves for axial length and axial length/corneal curvature in Chinese children and adolescents aged 4-18 years. Br J Ophthalmol. (2021). doi: 10.1136/bjophthalmol-2021-319431
45. Muralidharan G, Martínez-Enríquez E, Birkenfeld J, Velasco-Ocana M, Pérez-Merino P, Marcos S. Morphological changes of human crystalline lens in myopia. Biomed Opt Express. (2019) 10:6084–95. doi: 10.1364/BOE.10.006084
46. Wang SK, Guo Y, Liao C, Chen Y, Su G, Zhang G, et al. Incidence of and factors associated with myopia and high myopia in chinese children, based on refraction without cycloplegia. JAMA Ophthalmol. (2018) 136:1017–24. doi: 10.1001/jamaophthalmol.2018.2658
47. Tsai DC, Fang SY, Huang N, Hsu CC, Chen SY, Chiu AW, et al. Myopia development among young schoolchildren: the myopia investigation study in Taipei. Invest Ophthalmol Vis Sci. (2016) 57:6852–60. doi: 10.1167/iovs.16-20288
48. Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. (2016) 100:882–90. doi: 10.1136/bjophthalmol-2015-307724
49. Dong YH, Liu HB, Wang ZH, Yang ZP, Xu RB, Yang ZG, et al. Prevalence of myopia and increase trend in children and adolescents aged 7-18 years in Han ethnic group in China, 2005-2014. Zhonghua Liu Xing Bing Xue Za Zhi. (2017) 38:583–7. doi: 10.3760/cma.j.issn.0254-6450.2017.05.005
50. Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. (1976) 51:170–9. doi: 10.1136/adc.51.3.170
51. Li H, Ji CY, Zong XN, Zhang YQ. Height and weight standardized growth charts for Chinese children and adolescents aged 0 to 18 years. Zhonghua Er Ke Za Zhi. (2009) 47:487–92. doi: 10.3760/cma.j.issn.0578-1310.2009.07.003
52. Qin Z, Peng T, Zhang Z, Lou J, Wang C, Deng R, et al. Myopia progression and stabilization in school-aged children with single-vision lenses. Acta Ophthalmol. (2021). doi: 10.1111/aos.15038. [Epub ahead of print].
Keywords: axial length (AL), height, myopia, correlation, school-age children
Citation: Tao L, Wang C, Peng Y, Xu M, Wan M, Lou J and Yu X (2022) Correlation Between Increase of Axial Length and Height Growth in Chinese School-Age Children. Front. Public Health 9:817882. doi: 10.3389/fpubh.2021.817882
Received: 18 November 2021; Accepted: 29 December 2021;
Published: 20 January 2022.
Edited by:
Rafa Iribarren, Drs. Iribarren Eye Consultants, ArgentinaReviewed by:
Sebastián Eduardo Dankert, Centro Oftalmólogico de Diagnóstico, ArgentinaAbel José Szeps, Hospital Posadas, Argentina
Copyright © 2022 Tao, Wang, Peng, Xu, Wan, Lou and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiangtao Lou, bG91X2ppYW5ndGFvQDE2My5jb20=
 Lixia Tao1
Lixia Tao1 Meiping Xu
Meiping Xu Jiangtao Lou
Jiangtao Lou Xinping Yu
Xinping Yu