- 1School of Nursing, The University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 2School of Public Health, The University of Hong Kong, Hong Kong, Hong Kong SAR, China
Background: Delaying doctor consultation is harmful. Fear of COVID-19 leads to delays in seeking medical care at a time when pandemic information overflows. However, little is known about the role of COVID-19 related fear, attention to information, and fact-checking in such delay.
Objective: Under the Hong Kong Jockey Club SMART Family-Link Project, we examined the associations of delay in doctor consultation amidst the pandemic with sociodemographic characteristics, COVID-19 related fear, attention to information, and fact-checking.
Methods: We conducted a population-based online cross-sectional survey in May 2020 on Hong Kong Chinese adults. Respondents reported whether the pandemic caused any delay in doctor consultation (yes/no), level of COVID-19 related fear, attention to information and fact-checking (all on a scale of 0 to 10 and recoded into tertiles of low, moderate, high). Regression analyses were used to examine the associations of delay and fear with sociodemographic characteristics, attention and fact-checking, adjusting for covariates. Data were weighted by sex, age and education level of the population.
Results: Of 4,551 respondents (46.5% male, 59.7% aged over 45 years), 10.1% reported delay in doctor consultation. The mean score was 6.4 for fear, 8.0 for attention and 7.4 for fact-checking. Delay was more common in males and increased with age and fear. High vs. low level of fear was associated with delay [adjusted odd ratios (AOR) 2.68, 95% confidence interval (CI) 2.08, 3.47]. Moderate level of fact-checking was negatively associated with delay (AOR 0.72, 95% CI 0.56, 0.92). Females reported greater fear and fear decreased with age. Fear increased with attention to information and decreased with fact-checking. Fear substantially mediated the association of delay with attention (96%) and fact-checking (30%).
Conclusions: We have first shown that delay in doctor consultation increased with fear of COVID-19 and decreased with fact-checking amidst the pandemic. Fear also increased with attention to COVID-19 related information and decreased with fact-checking. Understanding these associations can help policymakers develop targeted communication and support to the public to reduce delayed doctor consultations and the associated COVID-19-related or unrelated morbidity and mortality in the community.
Introduction
Delay in doctor consultation can increase morbidity and mortality risk associated with various health conditions, and reduce the effectiveness of treatments (1, 2). Amidst the COVID-19 pandemic, such delay can result in more severe presentations and related excess deaths (3). Fear of infection in healthcare settings has led to delays in or avoidance of medical care, with negative health consequences (4–6). Understanding the environmental and psychosocial factors associated with such delay is needed to reduce fear and delay.
Meanwhile, the simultaneously ongoing infodemic, coined by the World Health Organization as an overabundance of information and rapid spread of misinformation, has also undermined the public's ability to discern the truth, thereby complicating public health responses to the pandemic (7, 8). Not only can misinformation fuel fear and confusion, frequent exposure to COVID-19-related information has been associated with mental distress, including fear, anxiety and depression (9–11). During a pandemic, individuals may not be able to obtain high-quality information, even if they regularly fact-check, and especially when they lack knowledge about science or are influenced by negative emotion or misinformation (12).
We used keywords of “COVID-19,” “coronavirus,” “delay,” “patient delay,” “seek” and “doctor consultation” to search PubMed and Cochrane Library up to 26 July 2021. Four surveys reported patient delays amidst the pandemic due to reasons including fear of infection, inability to get an appointment or access the care location, and being discouraged to access care to curb transmission (4, 13–15). We found no survey reports on the role of both fear of COVID-19 and COVID-19 information-related attitude (attention) and behavior (fact-checking) in delay in doctor consultation.
In Hong Kong, one of the most developed and westernized cities in China with a population of over 7 million, about 1,100 confirmed cases and 4 deaths were reported since the first case on 23 January until 31 May 2020 (around the end of the second wave of outbreak) (16). As of 3 November 2021, a total of 12,034 confirmed cases and 213 deaths were reported (17). This could be attributed to ubiquitous voluntary masking, hand hygiene and government public health measures including contact tracing and social distancing, but no lockdown. People were strongly advised against visiting places with high contact risk, including clinics and hospitals unless they had suspicious COVID-19 symptoms (18). Many hospitals also reduced non-emergency services. The prevalence and determinants of delay in doctor consultation in Hong Kong during the pandemic are unknown.
Under the Hong Kong Jockey Club SMART Family-Link Project, we conducted the Family Amidst COVID-19 (FamCov) survey in May 2020, after the second wave of the pandemic was under control. This paper reports (i) the associations of delay in doctor consultation and fear during COVID-19 with sociodemographic characteristics, (ii) the association of delay with fear and COVID-19 information-related attitude (attention) and behavior (fact-checking), (iii) the mediating effects of fear with information-related attitude and behavior on delay in doctor consultation in Hong Kong adults. We hypothesized that such delay is associated with fear of COVID-19 and COVID-19 information-related attitude and behavior, and that fear is a mediator of information-related attitude and behavior on delay in doctor consultation.
Methods
Study Design and Sampling
We conducted this online population-based cross-sectional survey by collecting as large a sample as possible with budget constraint and in a very short period of time (6 days from 26 May to 31 May 2020) when the second wave was under control and before another wave began.
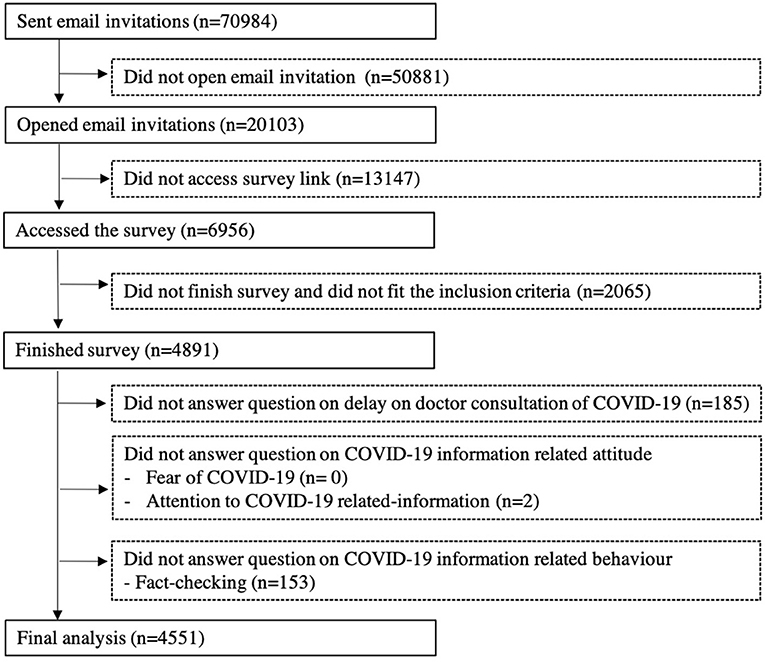
Detailed survey design and recruitment procedures have been published in our previous papers (19, 20). Briefly, email invitations were sent to 70,984 adults aged 18 years and above with valid email addresses from both probability and non-probability-based panels by the Hong Kong Public Opinion Research Institute (HKPORI), a well-known local survey agency. Four thousand eight hundred and ninety-one respondents who fit the inclusion criteria completed the survey. The response rate was 24.3% based on 20,103 respondents who opened the email. We excluded 185 respondents who did not answer the question on delay in doctor consultation, 2 respondents who did not answer the question on attention of COVID-19 information, and 153 respondents who did not answer the question on fact-checking of COVID-19 information, respectively. The remaining 4,551 were included in the present analyses. Figure 1 shows the flow diagram. Informed consent was obtained from all respondents before starting the survey. Ethics approval was obtained from the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (IRB reference no.: UW20-238).
Measurements
Delay in doctor consultation (delay) was assessed as one of 11 answer options to the question, “What harms have COVID-19 brought you?” One or more answer options could be selected. We analyzed “delay in doctor consultation” as “yes” vs. “no.”
Fear is an unpleasant natural emotional response to perceiving or recognizing a threat (such as the pandemic) and serves to keep people away from danger (20). Fear of COVID-19 (fear) was assessed by the question, “Has COVID-19 caused you fear?” on a scale of 0 (no fear at all) to 10 (very fearful), and was used in our previous paper (20). Higher scores indicated greater fear.
Two questions on COVID-19 information-related attitude (attention) and behavior (fact-checking) were asked. Attention is the cognitive process that makes it possible to position oneself toward relevant stimuli and respond to it. Fact-checking is a behavioral process to verify factual information, so as to promote the veracity and correctness of reporting. Attention to COVID-19 information (attention) was assessed by the question, “In general, how much attention do you pay to COVID-19-related information?” on a scale of 0 (none) to 10 (excessive). Higher scores indicated greater attention. Fact-checking of COVID-19 information (fact-checking) was assessed by the question, “When the outbreak was serious, how often did you fact-check COVID-19-related information before forwarding to family members?” on a scale of 0 (never) to 10 (always). Higher scores indicated more fact-checking.
We also collected information on sex, age group (18–24, 25–34, 35–44, 45–54, 55–64, and 65 years or above), education (primary or lower, secondary, diploma or certificate, associate degree, and degree or higher), and household monthly income (no income, less than HKD 4,000, 4,000–9,999, 10,000–19,999, 20,000–29,999, 30,000–39,999, and 40,000 or higher (USD 1 = HKD 7.8).
Statistical Analysis
Analyses were conducted using Stata version 15.0. Statistical significance was indicated by P < 0.05, and marginal statistical significance was indicated by P < 0.1. Results on respondent characteristics, presented as mean and standard deviation or number and percentage, were weighted by sex, age group and education of the Hong Kong general population to improve representativeness (21). Several variables were recoded: age (<35, 35–44, 45–54, 55–64 and 65 years or above), education (secondary or below, and post-secondary), household monthly income [lower (less than or equal to the median monthly household income per person) or higher] (19).
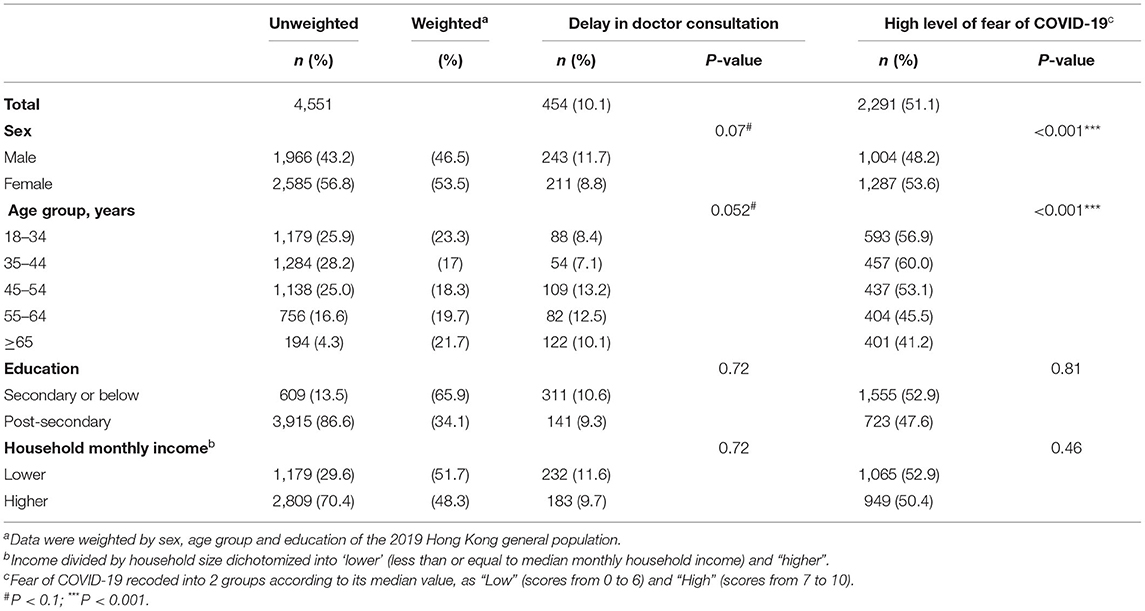
For ease of interpretation, we first examined the associations of delay (yes/no) and fear [high (median and above, scores from 7 to 10) / low (below median, scores from 0 to 6)] with sociodemographic characteristics (i.e., sex, age group, education, and household monthly income) by Chi square test, as shown in Table 1. Although only sex and age showed marginally significant associations with delay and fear, education was still considered as a potential confounding factor, as it is one of the key factors influencing health-related decisions and outcomes (22).
Second, we used logistic regression to examine the associations between delay (yes/no) and levels (high/moderate/low, according to their tertiles) of fear, COVID-19 information related attitude (attention) and behavior (fact-checking) with mutual adjustment and with potential confounding factors, as shown in Table 2. The level of fear was recoded as “Low” (scores from 0 to 5), “Moderate” (6 to 7), and “High” (9 to 10). The level of attention was recoded as “Low” (0 to 7), “Moderate” (8), and “High” (9 to 10). The level of fact-checking was recoded as “Low” (0 to 6), “Moderate” (7 to 8), and “High” (9 to 10).
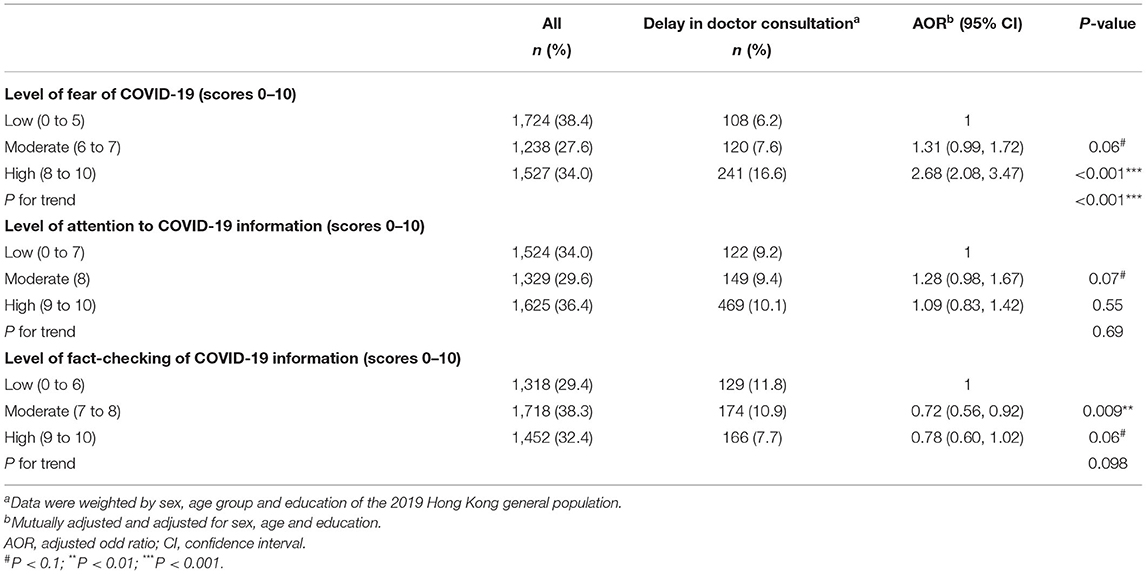
Table 2. The associations of delay in doctor consultation with COVID-19 related fear, attention to information and fact-checking.
We then used logistic regression to further examine the associations of high fear (vs. moderate/low) with levels (high/moderate/low) of attention and fact-checking, adjusting for each other and potential confounders, as shown in Table 3.
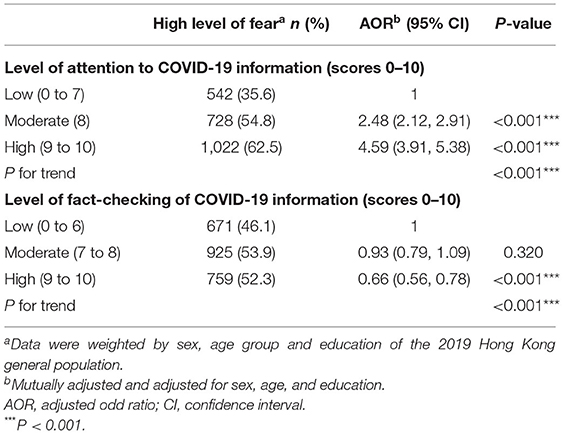
Table 3. The associations of level of fear of COVID-19 with attention to information and fact-checking.
Lastly, the associations of attention and fact-checking with delay were examined by Analysis of Moment Structures (AMOS; software version 25.0) using the asymptotically distribution free (ADF) method with no normal distribution assumption (23). The mediating effects of fear on attention and fact-checking on delay were performed by Sobel test (24), as shown in Table 4.
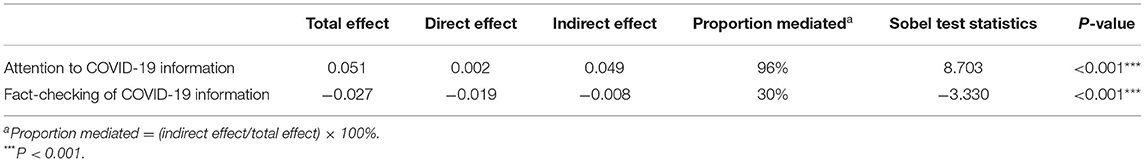
Table 4. The mediating effect of fear for the associations of attention and fact-checking with delay in consultation.
Results
Characteristics of the Survey Sample
Figure 1 shows the recruitment flow. Table 1 shows that of the 4,551 respondents, after weighting, 46.5% were male, 59.7% were aged 45 years or above, 34.1% had attained post-secondary education, and 48.3% had higher household income. 10.1% of respondents reported delay as a perceived harm amidst COVID-19. The mean ± SD score of fear was 6.4 ± 2.3. Of the two COVID-19 information questions, attention scored 8.0 ± 1.5 and fact-checking scored 7.4 ± 2.1.
The Associations of Delay in Doctor Consultation and Fear With Sociodemographic Characteristics
Table 1 shows that delay was more common in males (P = 0.07) and increased with age (P for trend = 0.052). No associations of delay with education and household income were reported. Females reported greater fear (P < 0.001) and fear decreased with age (P for trend < 0.001). No associations of delay and fear with education and household monthly income were reported.
The Associations of Delay in Doctor Consultation With Fear and Information-Related Attitude and Behavior
Table 2 shows that delay was reported by 6.2, 7.6, and 16.6% respondents with low, moderate and high levels of fear; 9.2, 9.4, and 10.1% respondents with low, moderate and high levels of attention; and 11.8, 10.9, and 7.7% respondents with low, moderate and high levels of fact-checking, respectively.
Delay increased with fear (P for trend < 0.001). More respondents with a moderate or high level of fear reported delay than those with a low level of fear [adjusted odd ratios (AOR), 95% confidence interval (CI): 1.31 (0.99, 1.72), P= 0.06 and AOR (95 CI): 2.68 (2.08, 3.47), P < 0.001, respectively]. More respondents with a moderate level of attention reported delay than those with a low level of attention [AOR (95% CI): 1.28 (0.98, 1.67), P = 0.07]. Delay decreased with fact-checking (P for trend < 0.1). Fewer respondents with a moderate or high level of fact-checking reported delay than those with a low level of fact-checking [AOR (95% CI): 0.72 (0.56, 0.92), P < 0.01 and AOR (95% CI): 0.78 (0.60, 1.02), P = 0.06, respectively].
The Associations of Level of Fear of COVID-19 With COVID-19 Information-Related Attitude and Behavior
Table 3 shows a high level of fear was reported in 35.6, 54.8, and 62.5% respondents with low, moderate and high levels of attention; and 49.4, 53.7, and 52.9% respondents with low, moderate and high levels of fact-checking, respectively. Fear increased with attention (P for trend < 0.001) and decreased with fact-checking (P for trend < 0.001). More respondents with a moderate or high level of attention reported a high level of fear than those with a low level of attention [AOR (95% CI): 2.48 (2.12, 2.91), P < 0.001 and 4.59 (3.91, 5.38), P < 0.001, respectively]. Fewer respondents with a high level of fact-checking reported a high level of fear than those with a low level of fact-checking [AOR (95% CI): 0.66 (0.56, 0.78), P < 0.001].
The Mediating Effects of Fear With Information-Related Attitude and Behavior on Delay in Doctor Consultation
Table 4 shows that fear substantially mediated associations of attention (96%) (Sobel test 8.73, P < 0.001) and fact-checking (30%) (Sobel test −3.33, P < 0.001) on delay.
Discussion
Our study is the first to show associations of delay in doctor consultation with fear of COVID-19 and COVID-19 information-related attitude (attention) and behavior (fact-checking) amidst the pandemic. Our findings show that one-tenth of respondents experienced delays in doctor consultation. Delay was more common in males and increased with age and fear. Fear was more common in females, decreased with age and fact-checking and increased with attention.
One-tenth of respondents also reported delay in doctor consultation as a perceived harm, which aligns with reports of decreased hospital admissions and visits for a wide spectrum of health conditions since the start of the pandemic in Hong Kong (25, 26) and elsewhere (27, 28). Respondents in Hong Kong reported delays in doctor consultation, which was relatively lower than the estimated 41% of U.S. adults who delayed or avoided medical care (13). This could be explained by the COVID-19 outbreaks that have been better controlled in Hong Kong compared with the U.S. (29).
Many studies report men are more likely to delay, or altogether avoid, doctor consultations, which is associated with the culture of masculinity and social structure of gender and power, including being conditioned to not show signs of weakness or dependence, with health issues (30, 31). Men are less likely to engage in behaviors that promote health and longevity (32), and traditional masculine ideals and a sense of self-worth tied to perceived masculinity are associated with healthcare avoidance and poorer health outcomes (30). Our results showed females and younger age groups had greater fear of COVID-19, consistent with pandemic-related reports including our previous paper (33–36).
Delay increasing with age could be explained by older people likely having more medical issues and appointments, and requiring assistance to seek care (37), which may result in a greater chance for delay. Older people may need more assistance (such as transportation and/or escorting) to attend medical appointments (37). As we hypothesized, greater fear was associated with delay, which is consistent with previous reports (4, 5, 13, 27).
Our results showed delay associated with moderate attention to COVID-19 information. This is consistent with other reports that show exposure and attention to COVID-19 information are positively associated with risk perception (38), including perceived susceptibility and severity, and mental distress (9–11, 39), which may result in delay. However, our findings showed no association of delay with too much attention, which could be due to differences in help-seeking behaviors for some individuals who independently search the internet for health-related information (40).
Our results also highlight the importance of fact-checking any received information related to the pandemic against trustworthy sources. Both the United Nations (UN) and World Health Organization (WHO) have led global efforts to combat misinformation (41, 42). In particular, the WHO has launched the joint “Stop the Spread” global campaign with the United Kingdom government to raise awareness about the risk of misinformation and encourage fact-checking with trusted sources such as national health authorities (43). In Hong Kong, distrust and criticism toward the government facilitated the rapid spread of false information and conspiracy theories (44, 45). With concerns that misinformation is spreading faster than the virus itself (46), fact-checking can help assure that people are using the correct information to make informed decisions (47).
There is also a need for simple, easily understandable, and evidence-based health education for the public to fight against misinformation and misunderstandings (48). As the world battles both a pandemic and concurrent infodemic, accurate and reliable information about the virus and related health information is of paramount importance. Authoritative and credible organizations need to lead and be more effective in the fight against the infodemic. Additionally, our results showed fear increased with attention and decreased with fact-checking, which is consistent with previous reports, and also mediated the associations of attention and fact-checking on delay (38, 49). Health messages need to be communicated in a clear and straightforward manner that does not exacerbate anxieties and irrational fears, and helps facilitate health-related decision-making.
The capacity burden on healthcare systems in various countries due to surging outbreaks have prompted governments to push for people to stay home, even when feeling unwell, which has exacerbated a crisis of increased preventable deaths (50, 51). While outbreaks in Hong Kong were relatively under control, with people voluntarily adhering to masking and social distancing guidelines, they were advised against visiting locations with high density and close contact risk (18). Seeking medical attention promptly amidst the pandemic can help with earlier identification of potential cases and prevent further transmission. There is a need for clear and consistent guidelines across all government and health agencies to warn against delay in doctor consultation and seeking medical care. Alternatively, telemedicine could offer a feasible solution to patients unwilling or unable to seek help in person (52).
More understanding on why people choose to delay care and how information-related attitude and behaviors can affect their decision-making is needed. Future studies should examine the underlying reasons for delay in doctor consultation to prevent further exacerbation of outbreaks and increased COVID-19-related or unrelated morbidity and mortality in the community.
Limitations
Our study had a few limitations. First, the short sampling time frame and online survey method had led to under sampling of older respondents and those without access to the internet. Online surveys commonly suffer from this methodological limitation. Online surveys are completed only by persons who are literate and have access to the internet, and by those who are sufficiently biased to be interested in the topic (53). However, this problem should not be substantial as the key variables showed only small differences between weighted and unweighted results. Second, it could be queried whether the use of a single-item can fully reflect the connotation of complex constructs. However, studies show that single-item measures have acceptable level reliability and reliability, and play its appropriate role in psychology and social science research (54, 55). Although multi-item measures are more preferred by researchers, single-item measures also have its legitimacy in academic research (54). Third, the cross-sectional design of this survey could only show associations and the current findings were based on our hypothesized pathways. Fourth, the self-reported data might be subject to recall and response biases. Fifth, the survey did not assess the reasons for delay and whether the delay actually occurred, as the question was framed as whether respondents viewed delay as a perceived harm of the pandemic, which should be more concerning than delay with no harm. However, the reported prevalence of those that answered yes is consistent with increased delays reported in recent reports (25, 26). Lastly, respondents' brief history of medical illness and COVID-19 related experience (e.g., having friends or family diagnosed with COVID-19) were not collected, which may influence their health-related attitude and behaviors.
Conclusions
We have first shown that delay in doctor consultation increased with fear of COVID-19 and decreased with fact-checking amidst the pandemic. Fear also increased with attention to COVID-19 related information and decreased with fact-checking. Understanding these associations can help policymakers develop targeted communication and support to the public to reduce delayed doctor consultations and the associated COVID-19-related or unrelated morbidity and mortality in the community.
Data Availability Statement
The dataset presented in this article is not readily available because the sharing of data to third parties was not mentioned in subjects' consent. Requests to access the dataset should be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AL and SS analyzed the data and wrote the first draft. AL, SS, SW, BW, M-PW, S-YH, and T-HL contributed to the conception and design of the study. AL, SS, SW, S-YH, and T-HL interpreted the results. All authors critically revised and approved the final manuscript.
Funding
The research was funded by the Hong Kong Jockey Club Charities Trust.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank the Hong Kong Jockey Club Charities Trust for funding this project, the Hong Kong Public Opinion Research Institute for the fieldwork, Jim Mai, and the Jockey Club SMART Family-Link Project team.
Abbreviations
COVID-19, the coronavirus disease 2019; FamCov, Family Amidst COVID-19 survey; CI, confidence interval; SD, standard deviation.
References
1. Dubayova T, van Dijk JP, Nagyova I, Rosenberger J, Havlikova E, Gdovinova Z, et al. The impact of the intensity of fear on patient's delay regarding health care seeking behavior: a systematic review. Int J Public Health. (2010) 55:459–68. doi: 10.1007/s00038-010-0149-0
2. Centers for Disease Control and Prevention. Excess Deaths Associated With COVID-19. (2020). Available online at: https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm (accessed August 25, 2021).
3. World Health Organization and the United Nations Children's Fund. Community-Based Health Care, Including Outreach and Campaigns, in the Context of the COVID-19 Pandemic. (2020). Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Comm_health_care-2020.1 (accessed August 25, 2021).
4. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. (2020) 4:e10–1. doi: 10.1016/S2352-4642(20)30108-5
6. Harvard TH, Chan School of Public Health, The Robert Wood Johnson Foundation, National Public Radio. The Impact of Coronavirus on U.S. Households Survey. (2020). Available online at: https://cdn1.sph.harvard.edu/wp-content/uploads/sites/21/2020/09/NPR-RWJF-Harvard-National-Report_092220_Final1-4.pdf (accessed August 25, 2021).
7. World Health Organization. Immunizing the Public Against Misinformation. (2020). Available online at: https://www.who.int/news-room/feature-stories/detail/immunizing-the-public-against-misinformation (accessed August 25, 2021).
8. The Lancet. The truth is out there, somewhere. Lancet. (2020) 396:291. doi: 10.1016/S0140-6736(20)31678-0
9. Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. (2020) 15:e0231924. doi: 10.1371/journal.pone.0231924
10. Riehm KE, Holingue C, Kalb LG, Bennett D, Kapteyn A, Jiang Q, et al. Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID-19 pandemic. Am J Prev Med. (2020) 59:630–8. doi: 10.1016/j.amepre.2020.06.008
11. Sasaki N, Kuroda R, Tsuno K, Kawakami N. Exposure to media and fear and worry about COVID-19. Psychiatry Clin Neurosci. (2020) 74:501–2. doi: 10.1111/pcn.13095
12. Yu W, Shen F. Does fact-checking habit promote COVID-19 knowledge during the pandemic? Evidence from China. Public Health. (2021) 196:85–90. doi: 10.1016/j.puhe.2021.05.005
13. Czeisler M, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1250–7. doi: 10.15585/mmwr.mm6936a4
14. Phillips GSA, Talwar C, Makaranka S, Collins DP. The impact and lessons learnt from the COVID-19 pandemic on a UK Burns Centre. Burns. (2021) 47. doi: 10.1093/bjsopen/zrab032.107
15. Wang AW, Prieto J, Ikeda DS, Lewis PR, Benzer EM, Van Gent JM. Perforated appendicitis: an unintended consequence during the coronavirus-19 pandemic. Mil Med. (2021) 186:e94–7. doi: 10.1093/milmed/usaa527
16. Centre for Health Protection. Latest Situation of Cases of COVID-19 (as of June 1 2020). (2020). Available online at: https://www.chp.gov.hk/files/pdf/local_situation_covid19_en_20200601.pdf (accessed October 1, 2021).
17. Centre for Health Protection. Latest Situation of Cases of COVID-19. (2021). Available online at: https://www.chp.gov.hk/files/pdf/local_situation_covid19_en_20211103.pdf (accessed Novemeber 3, 2021).
18. Yu YET, Leung WLL, Wong SOS, Liu KSN, Wan EYF, HKCFP Executive and Research Committee. How are family doctors serving the Hong Kong community during the COVID-19 outbreak? A survey of HKCFP members. Hong Kong Med J. (2020) 26:176–83. doi: 10.12809/hkmj208606
19. Wong BY, Lam TH, Lai AY, Wang MP, Ho SY. Perceived benefits and harms of the COVID-19 pandemic on family well-being and their sociodemographic disparities in Hong Kong: a cross-sectional study. Int J Environ Res Public Health. (2021) 18:1217. doi: 10.3390/ijerph18031217
20. Sit SM, Lam TH, Lai AY, Wong BY, Wang MP, Ho SY. Fear of COVID-19 and its associations with perceived personal and family benefits and harms in Hong Kong. Transl Behav Med. (2021) 11:793–801. doi: 10.1093/tbm/ibab018
21. Hong Kong Census and Statistics Department. Table 002 : Population by Age Group and Sex 2019, (Hong Kong) (2019).
22. Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. (2014) 129(Suppl. 2):19–31. doi: 10.1177/00333549141291S206
23. McDonald RP, Ho MH. Principles and practice in reporting structural equation analyses. Psychol Methods. (2002) 7:64–82. doi: 10.1037/1082-989X.7.1.64
24. Michael ES. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. (1982) 13:290–312. doi: 10.2307/270723
25. Chan KPF, Ma TF, Kwok WC, Leung JKC, Chiang KY, Ho JCM, et al. Significant reduction in hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in Hong Kong during coronavirus disease 2019 pandemic. Respir Med. (2020) 171:106085. doi: 10.1016/j.rmed.2020.106085
26. Leung WCY, Lau EHY, Kwan P, Chang RS-K. Impact of COVID-19 on seizure-related emergency attendances and hospital admissions - a territory-wide observational study. Epilepsy Behav. (2021) 115:107497. doi: 10.1016/j.yebeh.2020.107497
27. Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, et al. potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January-May 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:795–800. doi: 10.15585/mmwr.mm6925e2
28. Oseran AS, Nash D, Kim C, Moisuk S, Lai PY, Pyhtila J, et al. Changes in hospital admissions for urgent conditions during COVID-19 pandemic. Am J Manag Care. (2020) 26:327–8. doi: 10.37765/ajmc.2020.43837
29. World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. (2020). Available online at: https://covid19.who.int/ (accessed October 1, 2021).
30. Himmelstein MS, Sanche DT. Masculinity impediments: internalized masculinity contributes to healthcare avoidance in men and women. J Health Psychol. (2016) 21:1283–92. doi: 10.1177/1359105314551623
31. Cimons M. Many Men Avoid Doctors. That Can be Dangerous, Even Deadly, for Them. United States: The Washington Post (2019).
32. Courtenay WH. Constructions of masculinity and their influence on men's well-being: a theory of gender and health. Soc Sci Med. (2000) 50:1385–401. doi: 10.1016/S0277-9536(99)00390-1
33. Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol Trauma. (2020) 12:S17–21. doi: 10.1037/tra0000924
34. Bakioglu F, Korkmaz O, Ercan H. Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int J Ment Health Addict. (2020). doi: 10.1007/s11469-020-00331-y. [Epub ahead of print].
35. Campbell A. The evolutionary psychology of women's aggression. Philos Trans R Soc Lond B Biol Sci. (2013) 368:20130078. doi: 10.1098/rstb.2013.0078
36. Else-Ouest NM, Hyde JS, Goldsmith HH, Van Hulle CA. Gender differences in temperamet: ametanalysis. Psychol Bull. (2006) 132:33–72. doi: 10.1037/0033-2909.132.1.33
37. MacLeod KE, Ragland DR, Prohaska TR, Smith ML, Irmiter C, Satariano WA. Missed or delayed medical care appointments by older users of nonemergency medical transportation. Gerontologist. (2015) 55:1026–37. doi: 10.1093/geront/gnu002
38. Gardikiotis A, Malinaki E, Charisiadis-Tsitlakidis C, Protonotariou A, Archontis S, Lampropoulou A, et al. Emotional and cognitive responses to COVID-19 information overload under lockdown predict media attention and risk perceptions of COVID-19. J Health Commun. (2021) 26:434–42. doi: 10.1080/10810730.2021.1949649
39. Liu M, Zhang H, Huang H. Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC Public Health. (2020) 20:1649. doi: 10.1186/s12889-020-09761-8
40. Riel VR, Auwerx K, Debbaut P, Hees SV, Schoenmakers B. The effect of Dr Google on doctor–patient encounters in primary care: a quantitative, observational, cross-sectional study. BJGP Open. (2017) 1:bjgpopen17X100833. doi: 10.3399/bjgpopen17X100833
41. World Health Organization. How to Report Misinformation Online 2020. Available online at: https://www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/how-to-report-misinformation-online?gclid=Cj0KCQiA-aGCBhCwARIsAHDl5x_jIEGSE5OdwcipfrpAnYNYFXfl59N2uWhWImfYgVKENIBR_2Sm-kUaAtetEALw_wcB (accessed October 1, 2021).
42. United Nations. UN, News Organizations Artists Fight Against COVID-19 Fake News. (2020). Available online at: https://www.un.org/africarenewal/magazine/july-2020/un-news-organizations-and-artists-against-fake-news-covid-19 (accessed October 1, 2021).
43. World Health Organization. Countering Misinformation About COVID-19: A Joint Campaign With the Government of the United Kingdom. (2020). Available online at: https://www.who.int/news-room/feature-stories/detail/countering-misinformation-about-covid-19
44. Chan RKH. Tackling COVID-19 risk in Hong Kong: examining distrust, compliance and risk management. Curr Sociol. (2021) 69:1139212199002. doi: 10.1177/0011392121990026
45. Yam S,. Weaponising COVID-19: How State Suppression Breeds Distrust Disinformation in Hong Kong. (2020). Available online at: https://hongkongfp.com/2020/08/09/weaponising-covid-19-how-state-suppression-breeds-distrust-and-disinformation-in-hong-kong/ (accessed October 1, 2021).
46. Ebrahimji A. Doctors Say Coronavirus Myths on Social Media Are 'Spreading Faster Than the Virus Itself ' (2020). Available online at: https://edition.cnn.com/2020/09/01/business/coronavirus-myths-social-media-doctors-trnd/index.html (accessed October 1, 2021).
47. The University of Western Australia. How to Find Reliable and Accurate Sources of Information During COVID-19. (2020). Available online at: https://www.news.uwa.edu.au/archive/2020040811986/research/how-find-reliable-and-accurate-sources-information-during-covid-19/ (accessed October 1, 2021).
48. Freckelton QI. COVID-19: fear, quackery, false representations and the law. Int J Law Psychiatry. (2020) 72:101611. doi: 10.1016/j.ijlp.2020.101611
49. Liu PL, Huang LV. Digital disinformation about COVID-19 and the third-person effect: examining the channel differences and negative emotional outcomes. Cyberpsychol Behav Soc Netw. (2020) 23:789–93. doi: 10.1089/cyber.2020.0363
50. Coronavirus: UK Prepares to Ask Even Mildly Sick to Stay Home. (2020). Available online at: https://www.bbc.com/news/uk-51807781 (accessed October 1, 2021).
51. Bruggeman L, Bhatt J. ‘They Are Terrified’: Fearing Coronavirus, People With Potentially Fatal Conditions Avoid Emergency Care. (2020). Available online at: https://abcnews.go.com/Health/terrified-fearing-coronavirus-people-potentially-fatal-conditions-avoid/story?id=70306931 (accessed October 1, 2021).
52. Cheng L,. Telemedicine Offers Solutions to Hong Kong Patients Unwilling to Visit Hospitals for Check-Ups Amid Coronavirus Crisis. (2020). Available online at: https://www.scmp.com/news/hong-kong/health-environment/article/3078507/telemedicine-offers-solutions-hong-kong-patients (accessed October 1, 2021).
53. Andrade C. The limitations of online surveys. Indian J Psychol Med. (2020) 42:575–6. doi: 10.1177/0253717620957496
54. Zhang L, Wei X. Single-item measures: queries, responses and suggestions. Adv Psychol Sci. (2019) 27:1194–204. doi: 10.3724/SP.J.1042.2019.01194
Keywords: COVID-19, coronavirus, infodemic, infodemiology, delay in doctor consultation, patient delay, public health, information and communication technologies
Citation: Lai AY-K, Sit SM-M, Wu SY-D, Wang M-P, Wong BY-M, Ho S-Y and Lam T-H (2021) Associations of Delay in Doctor Consultation With COVID-19 Related Fear, Attention to Information, and Fact-Checking. Front. Public Health 9:797814. doi: 10.3389/fpubh.2021.797814
Received: 19 October 2021; Accepted: 16 November 2021;
Published: 13 December 2021.
Edited by:
Simon Ching Lam, Tung Wah College, Hong Kong SAR, ChinaReviewed by:
Hilda Ho, Children's Hospital of Orange County, United StatesMarques Shek Nam Ng, The Chinese University of Hong Kong, China
Copyright © 2021 Lai, Sit, Wu, Wang, Wong, Ho and Lam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sai-Yin Ho, c3lob0Boa3UuaGs=
†These authors share first authorship
 Agnes Yuen-Kwan Lai
Agnes Yuen-Kwan Lai Shirley Man-Man Sit
Shirley Man-Man Sit Socrates Yong-Da Wu
Socrates Yong-Da Wu Man-Ping Wang
Man-Ping Wang Bonny Yee-Man Wong2
Bonny Yee-Man Wong2 Sai-Yin Ho
Sai-Yin Ho Tai-Hing Lam
Tai-Hing Lam