- 1Department of Epidemiology, Mailman School of Public Health, Columbia University Irving Medical Center, New York, NY, United States
- 2Department of Anesthesiology, Vagelos College of Physicians and Surgeons, Columbia University Irving Medical Center, New York, NY, United States
- 3Transportation Research Institute, University of Michigan, Ann Arbor, MI, United States
- 4Department of Emergency Medicine, School of Medicine, University of Colorado, Aurora, CO, United States
- 5Department of Epidemiology, Colorado School of Public Health, University of Colorado Denver, Aurora, CO, United States
- 6Department of Family Medicine and Public Health, School of Medicine, University of California, San Diego, San Diego, CA, United States
- 7Department of Health, Behavior and Society, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States
- 8Bassett Research Institute, Mary Imogene Bassett Hospital, Cooperstown, NY, United States
Introduction: Social isolation is a modifiable risk factor for negative health outcomes among older adults. This work assessed the relationship between geography (i.e., urban vs. non-urban residence) and social isolation in a cohort of older drivers.
Methods: The AAA LongROAD cohort with 2,989 older adult drivers from across the country were included. Social isolation was measured at baseline and at two subsequent annual follow-ups using PROMIS v2.0 Social Isolation 4a. The effect of geographic location with social isolation was assessed through with multivariable regression using a generalized estimating equation model.
Results: The rate of social isolation in urban areas was 21% lower (adjusted RR 0.79, 95% CI 0.46, 1.36) compared to non-urban areas after adjusting for covariates, though not significant.
Discussion: Social isolation is a predictor of poor health outcomes and geographic considerations have been lacking in the literature. The panel data in this analysis provides more evidence for causality though the under-representation of non-urban areas potentially reduces the power for the results.
Conclusions: It is important to understand the needs and risk of social isolation in various geographic settings to ensure resources and interventions are appropriately modified for a greater public health impact.
Introduction
The older adult population in the United States (US) is steadily growing, with adults over 65 projected to outnumber those under 18 for the first time in US history (1, 2). The rapidly growing older adult population is affected by age-related functional decline, increased prevalence of acute and chronic diseases, and the prospect of a loss of independence through driving cessation. The latter is associated with significant health decline including worsening physical function and increased depression (1, 3–5). It was founded that a modifiable risk factor associated with mortality and increased medical costs is social isolation (6–8). A national assessment found that 24% of older adults in the United States are socially isolated (6). The construct of social isolation assesses social network, community connections and participation in society (5, 6, 8, 9).
We assessed if geography was associated with social isolation with a more precise measure of social isolation to build on this conversation in the literature. Social isolation is a more objective and comprehensive domain compared to loneliness. Along with mortality, social isolation is associated with increased medical costs (7, 8).
To date there has not been consensus on whether social isolation varies by geography. A study measuring prevalence of social isolation found no difference between urban and non-urban areas in the adjusted model where social isolation was measured as physical separation (6). A subsequent cross-sectional study more broadly defining social isolation by rurality found that urban residents had fewer close relatives and friends, and were less able to rely on them than residents of non-metropolitan areas (10). Interestingly, residents in the least populated and most isolated rural places had similar levels of loneliness to their urban counterparts, despite reporting more social connections.
Other research has shown that older adults utilize health care services more than younger patients, and particularly for older adults experiencing loneliness, interactions with the health system can be very important for social and physical health (11). Rural dwelling individuals also have been shown to have poorer access to healthcare, which may be exacerbated by the loss of the ability to drive with advanced age, particularly in settings with poor public transportation infrastructure more common in non-urban settings (12, 13). This creates a challenging situation for older drivers who may be experiencing loneliness or isolation but have a reduced ability to seek care.
Using the AAA Longitudinal Research on Aging Drivers (AAA LongROAD) cohort, we assessed the rate of social isolation among older adults using precise measures normed to the US average. The Patient-Reported Outcomes Measurement Information System (PROMIS) measure for social isolation is a concise and validated measure developed by the National Institutes of Health. It was derived from a loneliness scale which is more focused on the feeling of distress that is associated with social isolation vs. loneliness (14, 15). We hypothesized an increased rate of social isolation with a less pronounced change in more rural areas.
Methods
The study population is from the AAA LongROAD prospective cohort study. Participants ranged from 65 to 79 years old at baseline and were recruited in one of five sites across the US: Ann Arbor, MI, Baltimore, MD, Cooperstown, NY, Denver, CO, and San Diego, CA. To be included in the study, participants had to reside in one of the above-referenced locations for 80% of the year, have a valid driver's license and have no major cognitive deficits. A total of 2,990 were enrolled in the cohort; more detailed methods are described in the LongROAD methods paper (2). Because we are assessing population averages, participants needed at least one measure of social isolation across the three time intervals (baseline 7/7/2015 to second year follow-up 6/8/2019); one participant did not meet this criterion and was excluded. The study population for this analysis was 2,989.
The self-reported PROMIS v2.0 Social Isolation 4a data was collected at baseline and annually (16). This measure for social isolation is derived from the following four questions: “I feel left out,” “I feel that people barely know me,” “I feel isolated from others” and “I feel that people are around me but not with me” (15, 17). Participants reported the degree to which they agreed with the statements, using Likert response categories which are summed and converted to a standardized T-score. The continuous T-score is normed to the US Census population with the mean being a T-score of 50 and a T-score of 40 being one standard deviation less isolated than the population mean.
Geography based on address of primary residence was dichotomized to urban and non-urban using Rural Urban Commuting Area (RUCA) codes. The original ten RUCA codes based on census tract, population density, and commuting were categorized into urban (1, 1.1), suburban (1.3, 2.2), and rural (>2.2) for the LongROAD study. For this analysis, the categories were dichotomized into urban and non-urban, the latter including the suburban population due to the small sample size. Potential confounders were age group, gender (male/female), race/ethnicity, marital status, education, measures of health and driving exposure (18). Marriage was categorized for the model and included as a dichotomous variable: married or live-in partner; divorced, separated, never married or widowed. Race/ethnicity was analyzed using the following categories: White Non-Hispanic (85.9%), Black Non-Hispanic, Asian, Hispanic and other non-Hispanic. Education categories were advanced degrees (41.6%), Bachelor's; some college, Associates' or vocational; and high school or less. Race/ethnicity, education and miles driven per week were included in the model as dummy variables. Physical status was measured with PROMIS SF v.1.0- Physical Function 4a dichotomized at the mean; scores <50 indicated worse than average physical function. Vision and hearing were dichotomized self-reported measures (Very Good to Excellent vs. Poor to Good) (10, 19). Social role (PROMIS Item Bank v2.0- Ability to Participate in Social Roles and Activities) and depressive symptoms (PROMIS Short Form v1 Depression 4a) both produce T-scores, with higher scores indicating increased depressive symptoms and increased ability to participate in social roles (20). Life satisfaction was measured on a scale from one to five with five representing the highest satisfaction (21). Driving frequency was self-reported miles driven per week. This variables was included because driving status is associated with social isolation (3, 8, 22).
Baseline characteristics were stratified by exposure status, i.e., urban or non-urban, and compared using χ2 and T-tests. To account for correlation from repeated measures within individuals, a generalized estimating equation (GEE) was used to assess the rate of social isolation using an identity link, Gaussian distribution and unstructured correlation structure. Life satisfaction and social role were highly correlated with one another and therefore excluded from modeling to increase the model's precision. Their collinearity approached 0.4. Time-varying covariates included in the model were age, race/ethnicity, marital status, education, depression, physical function, hearing and driving exposure.
Results
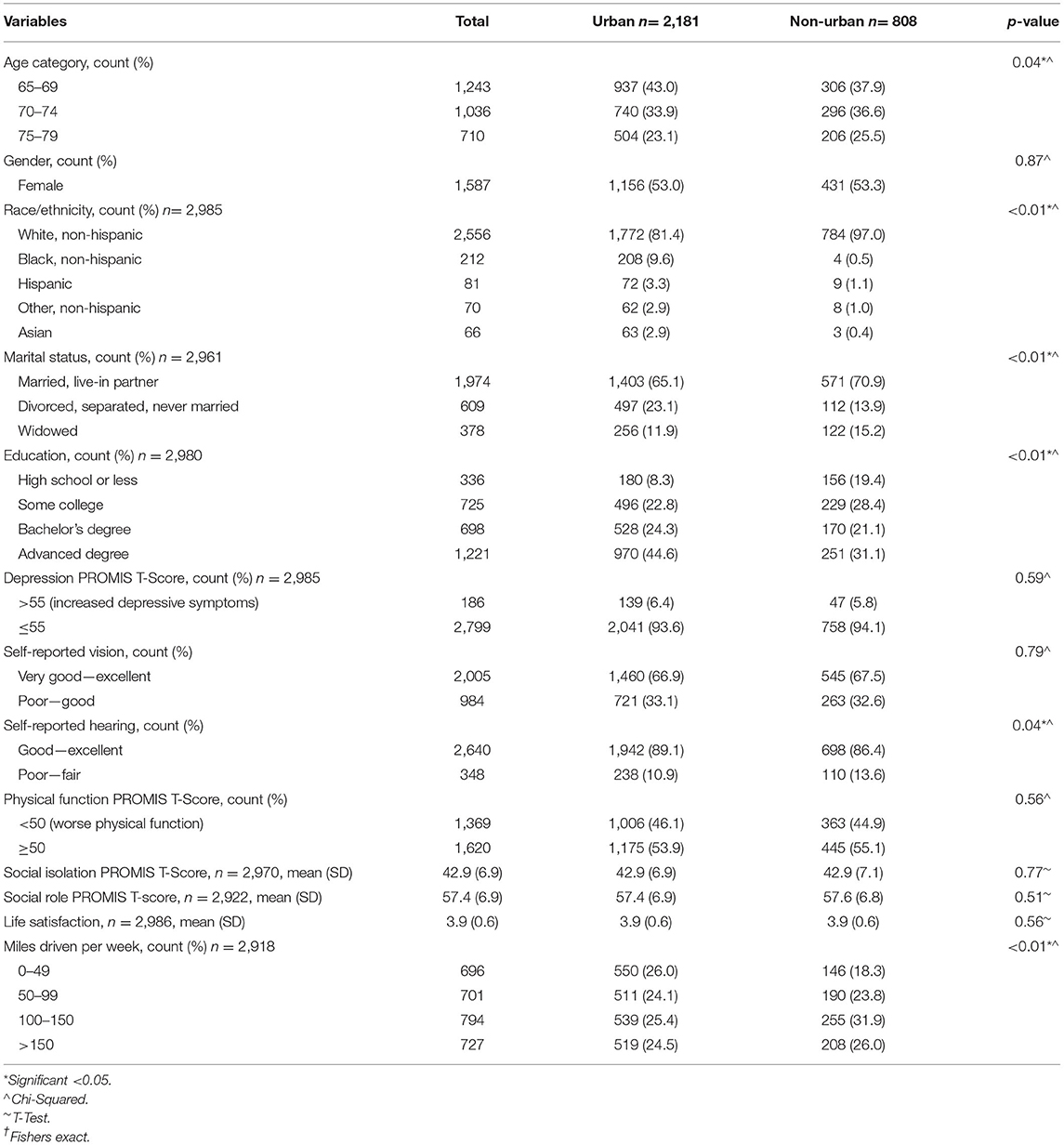
The population in this analysis was predominantly white (85.5%), married (66.0%) and held advanced degrees (40.8%) (Table 1). Below average depression (93.6%) and social isolation (mean 42.0, SD 6.9) were reported as well as higher levels of life satisfaction (mean 3.9, SD 0.6) (Table 1). Physically this cohort self-reported very good vision (67.1%) and hearing (88.3%) with 54.2% scoring better than average on physical function (Table 1).
Of the 2,989 participants 13.2% reported social isolation at baseline and the average T-score measures was 42.9, lower than average social isolation. A T-score of 50 is the mean and a T-score of 40 indicates one standard deviation below the mean corresponding with less social isolation. Variables from univariate testing as seen in Table 1 that were statistically significantly different between urban and non-urban settings were included in the model. Those were age (p = 0.04), race and ethnicity (p < 0.01), marital status (p < 0.01), education (p < 0.01), hearing (p = 0.04) and miles driven per week (p < 0.01). Depression, vision and hearing were significantly related to social isolation and also included in the full model.
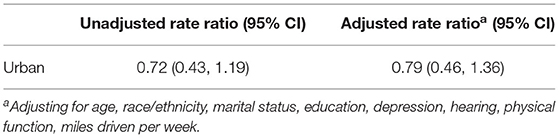
Participants in urban areas appeared to be 28% less likely to be socially isolated than participants in non-urban areas in the unadjusted model (unadjusted rate ratio 0.72, 95% CI 0.43, 1.19) (Table 2). That gap narrowed to 21% in the adjusted model (adjusted rate ratio 0.79, 95% CI 0.46, 1.36) (Table 2). Neither rate was statistically significant. The adjusted model was globally significant in being able to meaningfully assess the relationship between geography and social isolation (χ2= 384.7, p-value < 0.01). Gender and vision were excluded as they did not contribute to the adjusted rate ratio.
Discussion
Social isolation is gaining increased attention as a predictor of poor health outcomes, now associated with increased risk of death and increased Medicare expenses, although geographic considerations have been lacking in this literature (7, 23). Disparities in health outcomes and health care access by geographic location have been documented extensively, as have the associations between isolation and health care utilization, suggesting that these complex relationships require further examination (8, 11). Assuming that social isolation is a modifiable risk factor for poor outcomes, more detailed information can support more tailored interventions.
These results align with a larger cross-sectional study in that social isolation was not significantly different between urban and non-urban areas (6). Cudjoe et al. (6) had sufficient power for its conclusions; however, it was limited by the cross-sectional nature of the data. In this analysis, we similarly saw no significant difference in social isolation between urban and non-urban areas. A subsequent study assessing social isolation by geography found increased social isolation in urban areas and found an association in rural areas with the potential to buffer the effects of social isolation: friends that can be relied upon, number of close family members, number of living children and grandchildren, number of friends (10). A major limitation in social isolation research is a lack of consensus in construct operationalization.
A strength of this study is the increased precision of the PROMIS Social Isolation SFv2.0 short form which is normed to US census data allowing for increased comparability. Panel data from three time periods provided more evidence for causality. A limitation was that the sample is not demographically diverse, although it was not designed to be a nationally representative sample. Alternate transportation use was excluded in this analysis as it was not operationalized to include rideshare but could be a potential confounder when assessing geographic differences (24). The suburban and rural categories, combined to represent non-urban areas were under-represented in this study compared to urban areas, potentially reducing study power for these results.
Conclusions
The importance of social isolation is gaining more traction in research and it will be important to have a nuanced understanding of the experience in the geographically diverse areas of the US to ensure effective policies are implemented. Although geographic differences in social isolation were not statistically significant in this analysis, the evidence can build on the conversation in the literature regarding social isolation and rurality. This research was done prior to the COVID-19 pandemic; more research is needed to better understand the effect the pandemic may have had on social isolation, specifically older adults. Geographic location could potentially play a greater role in the setting of a pandemic and it needs further analysis.
Data Availability Statement
Restrictions apply to the availability of these data. Data are available from the author with permission from the AAA Foundation for traffic safety and upon execution of a data use agreement.
Ethics Statement
The studies involving human participants were reviewed and approved by IRB of the Columbia University Medical Center (IRB-AAAN9950). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
TM and LL: conceptualization, formal analysis, and writing—original draft preparation. TM, LL, GL, and DS: methodology. TM, DS, CD, MB, LM, DE, VJ, LH, and GL: data curation. TM, LL, DS, CD, MB, LM, DE, VJ, LH, and GL: writing—review and editing. TM: supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the AAA Foundation for Traffic Safety. This research was supported in part by Grant 1 R49 CE002096- 01 from the Centers for Disease Control and Prevention, National Center for Injury Prevention and Control to the Center for Injury Epidemiology and Prevention at Columbia University.
Author Disclaimer
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health and Centers for Disease Control and Prevention.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chihuri S, Mielenz TJ, Dimaggio CJ, Betz ME, Diguiseppi C, Jones VC, et al. Driving cessation and health outcomes in older adults. J Am Geriatr Soc. (2016) 64:332–41. doi: 10.1111/jgs.13931
2. Census U,. (2018). Available online at: https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html (accessed November 22, 2021).
3. Li G, Eby DW, Santos R, Mielenz TJ, Molnar LJ, Strogatz D, et al. (2017). Longitudinal Research on Aging Drivers (LongROAD): study design and methods. Injury Epidemiology, 4. doi: 10.1186/s40621-017-0121-z
4. Mezuk B, Rebok GW. Social integration and social support among older adults following driving cessation. J Gerontol B Psychol Sci Soc Sci. (2008) 63:S298–303. doi: 10.1093/geronb/63.5.S298
5. Schryer E, Boerner K, Horowitz A, Reinhardt JP, Mock SE. The social context of driving cessation: understanding the effects of cessation on the life satisfaction of older drivers and their social partners. J Appl Gerontol. (2019) 38:1661–86. doi: 10.1177/0733464817741683
6. Cudjoe TKM, Roth DL, Szanton SL, Wolff JL, Boyd CM, Thorpe RJ. The epidemiology of social isolation: national health and aging trends study. J Gerontol B Psychol Sci Soc Sci. (2018) 75:107–13. doi: 10.1093/geronb/gby037
7. Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. (2013) 103:2056–62. doi: 10.2105/AJPH.2013.301261
8. Qin W, Xiang X, Taylor H. Driving cessation and social isolation in older adults. J Aging Health. (2019) 089826431987040. doi: 10.1093/geroni/igz038.3048
9. Kruk ME, Ling EJ, Bitton A, Cammett M, Cavanaugh K, Chopra M, et al. Building resilient health systems: a proposal for a resilience index. BMJ. (2017) 357:j2323. doi: 10.1136/bmj.j2323
10. Henning-Smith C, Moscovice I, Kozhimannil K. Differences in social isolation and its relationship to health by rurality. J Rural Health. (2019) 35:540–9. doi: 10.1111/jrh.12344
11. National Academies of Sciences, Engineering, and Medicine (NASEM); Division of Behavioral and Social Sciences and Education; Health and Medicine Division; Board on Behavioral, Cognitive, and Sensory Sciences; Board on Health Sciences Policy; Committee on the Health and Medical Dimensions of Social Isolation and Loneliness in Older Adults. Washington, DC: National Academies Press (US) (2020).
12. Caldwell JT, Ford CL, Wallace SP, Wang MC, Takahashi LM. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am J Public Health. (2016) 106:1463–9. doi: 10.2105/AJPH.2016.303212
13. Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. (2015) 129:611–20. doi: 10.1016/j.puhe.2015.04.001
14. Henriksen J, Larsen ER, Mattisson C, Andersson NW. Loneliness, health and mortality. Epidemiol Psychiatr Sci. (2019) 28:234–9. doi: 10.1017/S2045796017000580
15. Manemann SM, Chamberlain AM, Roger L, Griffin JM, Boyd CM, Cudjoe TKM, et al. Perceived social isolation and outcomes in patients with heart failure. J Am Heart Assoc. (2018) 7:e008069. doi: 10.1161/JAHA.117.008069
16. Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. Initial item banks and first wave testing of the Patient–Reported Outcomes Measurement Information System (PROMIS) network: 2005-2008. J Clin Epidemiol. (2010) 63:1179–94. doi: 10.1016/j.jclinepi.2010.04.011
17. Kieny MP, Bekedam H, Dovlo D, Fitzgerald J, Habicht J, Harrison G, et al. Strengthening health systems for universal health coverage and sustainable development. Bull World Health Organ. (2017) 95:537–9. doi: 10.2471/BLT.16.187476
18. Strogatz D, Mielenz TJ, Johnson AK, Baker IR, Robinson M, Mebust SP, et al. Importance of driving and potential impact of driving cessation for rural and urban older adults. J Rural Health. (2019) 36:88–93. doi: 10.1111/jrh.12369
19. Crowe CL, Kannoth S, Andrews H, Strogatz D, Li G, DiGuiseppi C, et al. Associations of frailty status with low-mileage driving and driving cessation in a cohort of older drivers. Geriatrics. (2020) 5:19. doi: 10.3390/geriatrics5010019
20. Health Measures. (2017). Retrieved from NIH Toolbox website: http://www.healthmeasures.net/explore-measurement-systems/promis (accessed November 22, 2021).
21. Campbell A, Converse P, Rodgers W. Quality of American Life, The: Perceptions, Evaluations, and Satisfactions. New York, NY: Russell Sage Foundation (1976).
22. Man C, Ng LS, Molnar LJ, Eby DW, Ryan LH, DiGuiseppi C, et al. Frailty phenotype and self-reported crashes and driving space: baseline AAA LongROAD. J Transport Health. (2019) 15:100626. doi: 10.1016/j.jth.2019.100626
23. Shaw JG, Farid M, Noel-Miller C, Joseph N, Houser A, Asch SM, et al. Social isolation and medicare spending: among older adults, objective isolation increases expenditures while loneliness does not. J Aging Health. (2017) 29:1119–43. doi: 10.1177/0898264317703559
Keywords: geography, modifiable risk, driving, social isolation, older adults
Citation: Lynch L, Mielenz TJ, Li G, Eby DW, Molnar LJ, Betz ME, DiGuiseppi C, Hill LL, Jones V and Strogatz D (2021) Rate of Social Isolation by Geographic Location Among Older Adults: AAA LongROAD Study. Front. Public Health 9:791683. doi: 10.3389/fpubh.2021.791683
Received: 08 October 2021; Accepted: 15 November 2021;
Published: 10 December 2021.
Edited by:
Moon Choi, Korea Advanced Institute of Science and Technology, South KoreaReviewed by:
Birute Strukcinskiene, Klaipėdax University, LithuaniaVictoria Ramos Gonzalez, Instituto de Salud Carlos III (ISCIII), Spain
Copyright © 2021 Lynch, Mielenz, Li, Eby, Molnar, Betz, DiGuiseppi, Hill, Jones and Strogatz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thelma J. Mielenz, dGptMjE0MUBjdW1jLmNvbHVtYmlhLmVkdQ==
 Laura Lynch
Laura Lynch Thelma J. Mielenz
Thelma J. Mielenz Guohua Li1,2
Guohua Li1,2 David Strogatz
David Strogatz