
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 17 December 2021
Sec. Public Health Education and Promotion
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.779107
 Farhan Alshammari1
Farhan Alshammari1 Ahmed Alobaida1
Ahmed Alobaida1 Abdulhadi Alshammari2
Abdulhadi Alshammari2 Atheer Alharbi2
Atheer Alharbi2 Adel Alrashidi2
Adel Alrashidi2 Asma Almansour2
Asma Almansour2 Amal Alremal2
Amal Alremal2 Kashif Ullah Khan2*
Kashif Ullah Khan2*Background: Self-medication is an important issue for health authorities around the world. It is also a common practice among university students.
Objective: This study aimed to assess the prevalence of and reasons for self-medication among university students.
Methods: A descriptive, cross-sectional community based survey design was adopted for the current study. All the students enrolled in Hail University, Saudi Arabia were selected to include in the study. Data was collected from February to April 2020 using a validated questionnaire and were analyzed using IBM SPSS Statistics, Version 22.0. Using convenient sampling technique, the total sample size calculated was 370 participants. A descriptive analysis was performed. Chi-square test and binary logistic regression was used for analyzing the data where statistical significance was set at p ≤ 0.05.
Results: A total of 373 participants completed the questionnaire. The response rate was 84%. The overall prevalence of self-medication among the students was 98.2%. Of the 373 participants, 40.8% were men, and 59.2% were women. Furthermore, 56% were in fields other than health sciences, 23.1% were in preparatory foundation courses, and 20.9% were from the health and medical sciences. The most frequent medical condition that led to self-medication was headaches (92.85%), followed by coughs (37.5%), colic (31.9%) and influenza (30.3%). On univariate analysis, it is revealed that for both abdominal colic [OR 0.54 (0.34–0.86), p = 0.01] and constipation [OR 0.57 (0.32–1.02), p 0.05], female gender was observed significantly with low prevalence than male. However, for influenza, the self-medication prevalence [OR 1.86 (1.19–2.91), p = 0.006] observed was significantly higher in female participants than male. A significant association (p = 0.011) between the self-medication factors and gender was shown in the current study results.
Conclusion: An alarming prevalence of self-medication among the students was recorded. Health care providers can increase awareness of the issue by educating individuals about the harmful effects of irresponsible self-medication.
Medication consumption trends are an important health predictor. The awareness of trends can lead to the identification and determination of disease prevalence, as well as the ability to gain insights into the use of clinical services (1). Self-medication is a major concern because it can hinder diagnosis and lead to the proliferation of resistant microorganisms and iatrogenic illnesses (2). Previous studies in various countries have reported an increase in self-medication (3), which has been described as a patient's decision to take medication on their own or on the advice of a pharmacist or layperson rather than consult a medical practitioner (1). Generally, over-the-counter drugs are involved, but prescription-only medicines have also been used (4, 5). Age, gender, financial position, self-care attitude, education level, medical literacy, happiness and non-seriousness of illness are influential factors in self-medication behaviors (6, 7).
Self-medication has been found to be very common among university students. Previous studies have reported a high self-medication prevalence (55–98%) among university students in Egypt and Palestine (8, 9). A high self-medication prevalence (86.6%) was found among male university students at Al-Qassim University (10). A study at Taibah University revealed that a considerably high proportion (64.8%) of students used non-prescription medications (11). Most medications can cause severe side effects that could have serious health implications and even be life-threatening. Therefore, a physician's evaluation is critical for effective care (12). Community pharmacists play a significant role in facilitating self-medication. Patients who can be prescribed medicines by pharmacists and those who should be advised to contact physicians should be differentiated by the pharmacist (12). According to the World Health Organization, pharmacists are central players in the supply and distribution of drugs to the public (13). In their clinical capacity, pharmacists are qualified to provide guidance on the medications they provide. Individuals are increasingly treating a significant number of illnesses without the aid of doctors or pharmacists. Pharmacists can play an important role in helping them to make well-informed self-care decisions (12).
Few studies have addressed the prevalence of self-medication among Saudi university students. The influential factors in self-medication behaviors are still being debated; thus, more research is needed. The study aimed to determine the prevalence of self-medication among Saudi university students. Self-medication for the most common disease states in north-eastern Saudi Arabia and pharmacists' involvement were assessed.
This study was based on a descriptive, cross-sectional community based survey. Current study was carried out in all the enrolled students of Hail University, Saudi Arabia, from February to April 2020. Hail, located in the north of the Kingdom of Saudi Arabia has an estimated population of 356,770 Saudi nationals and expatriates and a capital of Hail Region among 1 of the 13 regions of the Kingdom of Saudi Arabia. The University of Hail is a public institute located in main city of Hail where the student population is rated medium.
The validated structured questionnaire contained total 31 close-ended questions with “yes and no response about self-medication practices and pharmacists” roles was adopted for the current study. The questionnaire had three sections. Part I elicited participant sociodemographic characteristics e.g., age, gender and nationality, university program and university course etc. Part II had two sub-parts, where subpart A contained 13 questions about the influential factors, including medical conditions, in self-medication, while subpart B had 04 questions about the factors that contribute to self-medication. Whereas, the third and final section had 6 questions used for evaluating the contribution of pharmacist in self-medication. The study questionnaire was adapted from various similar studies conducted previously and pre-tested on a sample of 10 participants, any ambiguities in the questions or responses were removed before its implementation (12, 14). In addition, the questionnaire was distributed to the male and female sections. Before the administration of the questionnaire, the students provided informed consent and received information about the study. The purpose of study was explained to all study participants and a consent form had been signed before the questionnaire would be given to students. Appropriate time were given to respondents to complete the questionnaire and return back. Students were with written informed consent and willing to participate in the study was included in study. To ensure diversity, all registered students, regardless of their social and demographic backgrounds, were eligible for inclusion in the study.
Convenient sampling technique was used to collect data from study population. Sample size of current study was calculated based on Raosoft sample size calculator, Where margin of error is 5%, confidence level is 95%, population size of university students is 10,000 available at the university website and response distribution is 50%. The total sample calculated was 370 (15).
The data were analyzed using IBM SPSS Statistics, Version 22.0. A descriptive analysis was performed. The data are reported as percentages. The chi-square test was used, and statistical significance was set at p ≤ 0.05.
The University of Hail research and ethics committee reviewed the research study proposal for any ethical issues. The study was approved by the committee (Nr. 41/213/43602). The students were given an assurance of confidentiality before being asked to provide written informed consent.
A total of 444 students were approached, and 373 completed the questionnaire. The response rate was 84%. Most were women (59.2%), a majority (55.2%) of whom were aged 21–25 years. In addition, 97.6% were Saudi nationals. A majority (75.6%) of the participants were undergraduates (Table 1).
The most common symptoms and diseases reported by participants who practiced self-medication were headaches (92.8%, n = 346), coughs (37.5%, n =140), colic (31.9%; n =119) and influenza ([flu] 30.3%, n =113; Table 2). There was a statistically significant relationship between medical conditions, including flu and colic and gender (Table 2). The prevalence of self-medication for colic was higher among women (22%, p = 0.009); however, for flu (15.5%, p = 0.006), it was higher among men (Table 2). Upon binary logistic regression (univariate analysis), the results showed that for both abdominal colic and constipation, female gender was observed significantly with low prevalence than male with the odd ratios and p-value of (OR 0.54, p 0.01) and (OR 0.57, p 0.05) respectively. However, for influenza, the self-medication prevalence (OR 1.86, p = 0.006) observed was significantly higher in female participants (Table 3).
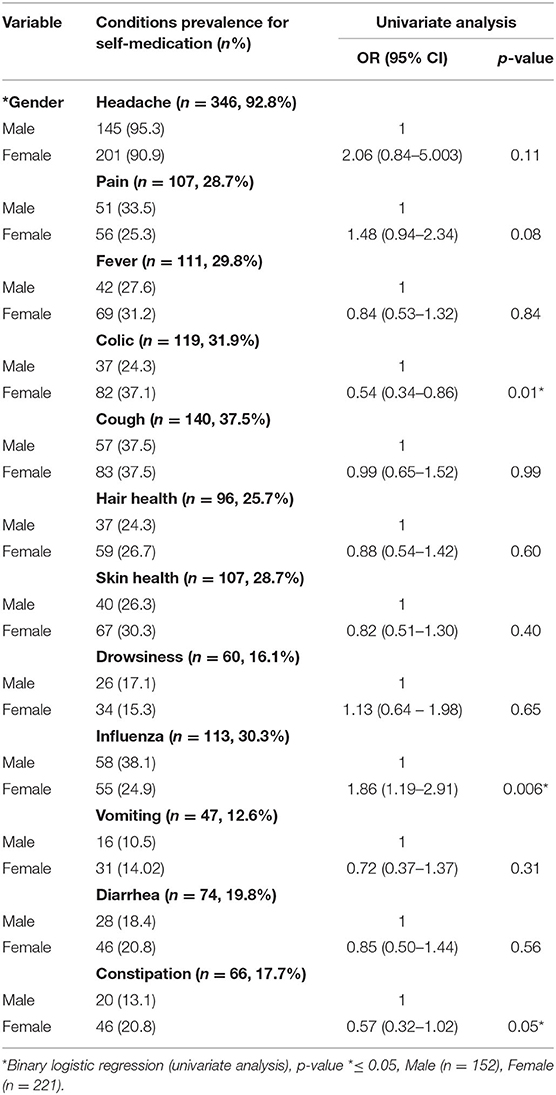
Table 3. Gender related prevalence of self-medication conditions among the study population (n = 373).
The most common justifications for university students to indulge in self-medication were “mild illness” and “time-saving option” where followed by other options that was urgency to self-medicate and cost-effectiveness. There was a statistically significant difference between the genders regarding the reasons for self-medication (p = 0.011; Table 4). Women identified more influential factors than did men.
Table 5 presents the data on pharmacist consultations for self-medication and as a drug consultant among University of Hail students. The results of the chi-square test indicated that the university program had a significant influence on the participants who sought pharmacists' opinions when taking more than one drug (76.4%, n =285; p = 0.010; Table 5). A statistically significant difference was observed between the academic program and pharmacist consultations regarding increasing the duration of drug consumption (n = 244, 65.4%; p = 0.011). The chi-square test indicated a lack of statistical significance between age and pharmacist consultation.
The appropriate use of self-medication, with full knowledge about the drugs and the condition to be treated, could be beneficial for mild illnesses. However, the risks cannot be ignored. They include dosage errors and the inappropriate duration of drug use. In addition, the occurrence of drug–drug interactions could negatively affect health.
This study was conducted in the Hail region to estimate the incidence and prevalence of self-medication among University of Hail students. The incidence of self-medication among the students was very high. In a study in Al-Qassim Province in Saudi Arabia, Saeed et al. reported that 86.2% of university students were self-medicated. However, at Taibah University Medina, 64.8% of the students were practiced self-medication (10, 11). According to Albusalih et al., the self-medication prevalence in the medicine and pharmacy colleges in Dammam city was 26%, the lowest in Saudi medical colleges (16). The high prevalence of self-medication is not unique to Saudi Arabia. A study conducted in Rio Grande, Brazil indicated that 86.4% of the students were self-medicated. Zafar et al. found that 76% of university students in Karachi, Pakistan were self-medicated (14, 17). The prevalence among Palestinian university students was 98%, which is the highest (9). In Slovenia, 92.3% of Ljubljana University students were found to be self-medicated (7). In Oman, 94% of university students were self-medicated. However, in Islamabad, Pakistan, the prevalence of self-medication among university students was 42% (18, 19).
In the current study, all 373 participants reported being self-medicated. The prevalence was higher among male students where 148 (97.3%) male student self-medicate out total 152 students participated in the study. Out of total 221 female students participated in the study survey, 207 (93.6%) used self-medication. In a study of students at Taibah University in Madinah, Saudi Arabia, Aljaouni et al. found that 65.5% of self-medicated students were women. In Oman, Egypt and Ethiopia, the prevalence was higher among women than men; thus, gender could be a factor in self-medication (11, 18, 20, 21).
The results of the present study (Table 2) support those of Saeed et al. in Dammam and Zafar et al. in Karachi regarding headaches being the most reported reason (59.9 and 72.4%, respectively) for seeking self-medication (14, 16). According to Alshogran et al., the most common indication (81.9%) for self-medication among students in Jordan was headaches (22). Because of the availability of free healthcare services in Saudi Arabia, the high prevalence of self-medication could be patients' believing that these diseases are mild and do not require treatment by a physician. Pharmacists are not only drug suppliers and distributors; they are also healthcare providers. They can play a major role in patients' decisions about self-medication by providing information. Thus, the focus should be on disease management and survival rather than sales and profit.
Especially for over-the-counter products, pharmacists can play a very important role by providing patients with the necessary information about medications and dosage. Their role in patient care services should include providing advice, building awareness about medical products and providing detailed information about medication effects, dosage and duration and possible side effects and drug–drug interactions, in addition to monitoring patients. The present study found that 65% to 79% of the university students practicing self-medication sought the assistance of a pharmacist. This suggests pharmacists' high confidence in the community and awareness of their active role in health care.
The results indicated that the students' main reasons for self-medication were as follows: mild illness (61%), time-saving option (22%), urgency (13%) and cost-effectiveness (2.9%). A study at a Dammam public university found that 35.1% of the medical and pharmacy students sought self-medication for mild problems (16). However, Sharif et al. reported that 72% of Sharjah university students self-medicated for mild disease (23).
It was assumed that the prevalence of self-medication among medical college students would be lower than that among other students because of their awareness of the drugs and their side effects. However, the results indicated that there was no difference between the medical and non-medical students. In a Jordanian university, the prevalence among medical and non-medical students was similar (22). The percentage of students who consulted pharmacists about drugs for self-medication (Table 3) revealed the students' awareness of the pharmacist's important role and their concerns about the drugs they had sought or used. The results indicated that 79.6% of the students sought pharmacist recommendations; thus, they were aware of dose variations. More women (59.2%) than men (40.8%) consulted pharmacists before taking drugs. Most (76.4%) of the students sought a pharmacist's advice about taking more than one drug; thus, they were aware of drug interactions.
The prevalence of self-medication among the university students and the pharmacists' contribution to this behavior were high. The occurrence of self-medication is concerning. Pharmacists can play a significant role by providing advice on rational options, increasing awareness about the care to be taken in medicine use, providing data on side effects and examining patients for their illnesses. Healthcare organizers should educate the public about the negative effects of irresponsible self-medication.
The questionnaire was self-reported and this could have led to under or over reporting of the self-medication practices. Furthermore, the study sample size calculation was through a convenient sampling technique, which is inferior to probability sampling in its representativeness. Moreover, the sample size of the study was not so large to generalize the results over the whole kingdom population.
Implications of the awareness and education regarding the self-medication practices can be useful in future.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
FA contributed to the study conceptualization, data curation, methodology and project administration, and manuscript editing. AAlo contributed to formal analysis, manuscript revision, and resources. AAls contributed to formal analysis, investigation, and data curation. AAlh contrinuted to formal analysis, data collection, investigation, and software. AAlra contributed to the data collection, formal analysis, writing, and revision. AAlm contributed to the methodology, study design, and manuscript revision. AAlre contributed to the data collection, software, data retrieving, and writing. KK is the scientific coordinator of this study and has developed the concept and made substantive intellectual contributions to the manuscript. All authors contributed to the study concept and design, manuscript revision for intellectual concepts and final approval for manuscript submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.779107/full#supplementary-material
2. Wajngarten M. Editorial. Rev Assoc Med Bras. (2001) 47:269–95. doi: 10.1590/S0104-42302001000400001
3. Blenkinsopp A, Bradley C. Patients, society, and the increase in self-medication. BMJ. (1996) 312:629–32. doi: 10.1136/bmj.312.7031.629
4. WHO Guidelines for the Regulatory Assessment of Medical Products for Use in Self-Medication. (2000). Available online at: http://www.who.int/medicine/library/qsm/whoedm-qsm-2000-l/who-edm-qsm-00_l.htm (accessed November 16, 2021).
5. Pereira FSVT, Bucaretchi F, Stephan C, Cordeiro R. Self-medication in children and adolescents. J Pediatria. (2007) 83:453–8. doi: 10.2223/JPED.1703
6. Abay SM, Amelo W. Assessment of self-medication practices among medical, pharmacy, and health science students in GondarUniversity, Ethiopia. J Young Pharm. (2010) 2:306–10. doi: 10.4103/0975-1483.66798
7. Klemenc-Ketis Z, Hladnik Z, Kersnik J. A cross sectional study of sex differences in self-medication practices among university students in Slovenia. CollegiumAntropologicum, (2011) 35:329–34.
8. El Ezz N, Ez-Elarab H. Knowledge, attitude and practice of medical students towards self-medication at Ain Shams University, Egypt. J Prev Med Hyg. (2011) 52:196–200.
9. Sawalha AF. A descriptive study of self-medication practices among Palestinian medical and nonmedical university students. Res Soc Adm Pharm. (2008) 4:164–72. doi: 10.1016/j.sapharm.2007.04.004
10. Saeed MS, Alkhoshaiban AS, Al-Worafi A, Mohammed Y, Long CM. Perception of self-medication among university students in Saudi Arabia. Arch Pharm Pract. (2014) 5:49. doi: 10.4103/2045-080X.142049
11. Aljaouni ME, Hafiz AA, Alalawi HH, Alahmadi GA, AlKhawaja I. Self-medication practice among medical and non-medical students at Taibah University, Madinah, Saudi Arabia. Int J Acad Sci Res. (2015) 3:54–65.
12. Al-Hussaini M, Mustafa S, Ali S. Self-medication among undergraduate medical students in Kuwait with reference to the role of the pharmacist. J Res Pharm Pract. (2014) 3:23. doi: 10.4103/2279-042X.132706
13. WHO Consultive Group. Report of the 4th. The Role of the Pharmacist in Self-care and Selfmedication. Hague: WHO Consultive Group (1998).
14. Zafar SN, Syed R, Waqar S, Zubairi AJ, Vaqar T, Shaikh M, et al. Self-medication amongst university students of Karachi: prevalence, knowledge and attitudes. J Pak Med Assoc. (2008) 58:214.
15. Sample Size Calculator by Raosft. Available online at: http://www.raosoft.com/samplesize.html (accessed November 16, 2021).
16. Albusalih FA, Naqvi AA, Ahmad R, Ahmad N. Prevalence of self-medication among students of pharmacy and medicine colleges of a public sector university in Dammam City, Saudi Arabia. Pharmacy. (2017) 5:51. doi: 10.3390/pharmacy5030051
17. Da Silva MGC, Soares MCF, Muccillo-Baisch AL. Self-medication in university students from the city of Rio Grande, Brazil. BMC Public Health. (2012) 12:339. doi: 10.1186/1471-2458-12-339
18. Al Flaiti M, Al Badi K, Hakami WO, Khan SA. Evaluation of self-medication practices in acute diseases among university students in Oman. J Acute Dis. (2014) 3:249–52. doi: 10.1016/S2221-6189(14)60056-1
19. Hussain A, Khanum A. Self-medication among university students of Islamabad, Pakistan-a preliminary study. Southern Med Rev. (2008) 1:14–6.
20. Helal R, Abou-ElWafa H. Self-medication in university students from the city of Mansoura, Egypt. J Environ Public Health. (2017) 2017:9145193. doi: 10.1155/2017/9145193
21. Sado E, Kassahun E, Bayisa G, Gebre M, Tadesse A, Mosisa B. Epidemiology of self-medication with modern medicines among health care professionals in Nekemte town, western Ethiopia. BMC Res Notes. (2017) 10:1–5. doi: 10.1186/s13104-017-2865-5
22. Alshogran OY, Alzoubi KH, Khabour OF, Farah S. Patterns of self-medication among medical and nonmedical University students in Jordan. Risk Manag Healthc Policy. (2018) 11:169. doi: 10.2147/RMHP.S170181
Keywords: students, pharmacists, Hail University, Saudi Arabia, self-medication
Citation: Alshammari F, Alobaida A, Alshammari A, Alharbi A, Alrashidi A, Almansour A, Alremal A and Khan KU (2021) University Students' Self-Medication Practices and Pharmacists' Role: A Cross-Sectional Survey in Hail, Saudi Arabia. Front. Public Health 9:779107. doi: 10.3389/fpubh.2021.779107
Received: 17 September 2021; Accepted: 24 November 2021;
Published: 17 December 2021.
Edited by:
Marcus Tolentino Silva, University of Sorocaba, BrazilReviewed by:
Victor C. W. Hoe, University of Malaya, MalaysiaCopyright © 2021 Alshammari, Alobaida, Alshammari, Alharbi, Alrashidi, Almansour, Alremal and Khan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kashif Ullah Khan, a2FzaGlmMDBraGFuQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.